Abstract
Dementia arising in patients with Parkinson disease or parkinsonian neurodegeneration comprises a heterogeneous neuropathology. Clinical labeling of patients with both dementia and Parkinson disease is dichotomous, depending on the temporal development of cognitive impairment and motor parkinsonism. Patients with dementia arising first (or within the first year of PD) are classified as dementia with Lewy bodies; patients with PD for more than 1 year before cognitive decline are classified as Parkinson disease with dementia. Despite this differential clinical classification, autopsy studies demonstrate variable admixtures of cortical synuicleinopathy, Aβ-amyloidopathy and tau neurofibrillary tangle deposition. There are no routine clinical diagnostic measures that accurately distinguish the underlying neuropathologies in individual patients. In the present paper, we review the published literature describing characteristics of fibrillary Aβ-amyloid deposition on the basis of PET radiotracer imaging in patients with Parkinson disease and in parkinsonian dementia syndromes. Although individual reports often include only small-to-modest subject numbers, there is overall suggestion that PD patients have a lower incidence of Aβ-amyloid deposition than seen amongst elderly normal subjects, and that Parkinson disease with dementia patients have a lower incidence of Aβ-amyloid deposition than do patients with dementia with Lewy bodies. These apparent features contrast the findings of Aβ-amyloid-PET imaging in normal aging and the development of Alzheimer disease, where Aβ-amyloid deposition arises asymptomatically and apparently many years before development of signs or symptoms of dementia. It is proposed that focused, prospective studies are needed to further address and understand the complex role(s) of Aβ-amyloid pathology in Parkinson disease, and that this understanding will be critical to the development of targeted disease-modifying therapy for dementia in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive impairment and dementia in synucleinopathies
Parkinson disease (PD) is the most common human neurodegenerative movement disorder, and is overall the second most common neurodegenerative disorder after Alzheimer disease (AD). PD is characterized by the intraneuronal deposition of α-synuclein (α-Syn) aggregates (Lewy bodies) and degeneration of monoaminergic brainstem nuclei (particularly the substantia nigra pars compacta). Parkinson disease affects approximately 1 % of the population over the age of 60 [1]. Cognitive impairment is common in PD, and the risk of developing dementia in patients with PD is 2–6-fold higher than in the general population, corresponding to lifetime risk estimates of 30–80 % [2–4]. Clinical diagnosis of dementia in patients with PD is dichotomized into two conditions. Parkinson disease with dementia (PDD) is related closely to an increasingly recognized syndrome, dementia with Lewy bodies (DLB). DLB is in fact the second most common neurodegenerative dementia, accounting for up to 20 % of all neurodegenerative dementia cases [5–7]. The key similarity between PDD and DLB is the requirement for PD neuropathologic changes, together with dementia. Several expert consensus meetings on DLB, its diagnosis, and its management have been convened by investigators at Newcastle upon Tyne [8–10]. Recommendation from the first DLB workshop [8] was that diagnostic classification of DLB be applied to patients in whom dementia preceded the clinical onset of PD, or when dementia occurred within 1 year after PD diagnosis. Classification as PDD was recommended when dementia developed more than 1 year after PD diagnosis.
Overlapping features of PDD and DLB
Although it was hoped that the PDD vs. DLB clinical classification rule would improve diagnostic homogeneity and identify distinctions between these two syndromes, subsequent studies have shown substantial overlap of PDD and DLB clinical phenotypes in numerous ancillary, biomarker and neuropathology studies. Thus, neuropsychological, neuropathological and neuroimaging studies do not show reliable differences between subjects classified clinically as PDD vs. those with DLB. Neuropsychometric evaluations may identify prominent visual dysfunction in pure DLB, however, there is no reliable neuropsychometric distinction between DLB and PD [11–13]. Similar visual psychometric abnormalities are found in PDD patients [14]. Features that may distinguish DLB form AD, including parkinsonism, visual illusions/hallucinations, fluctuating cognitive deficits, sensitivity to dopaminergic medications and striatal dopaminergic deficits on molecular neuroimaging studies [10] are manifest also in PDD. Most importantly, neuropathological studies of both PDD and DLB reveal similar admixtures of protein deposition abnormalities. By definition, both DLB and PDD are characterized by intraneuronal α-Syn aggregates and nigrostriatal degeneration. The degree and nature of the basal ganglia pathology, however, does not distinguish the disorders [15, 16]. Neuropathological studies focusing on cortical pathology identify advanced stages of α-Syn pathology (corresponding to Braak PD stages 5 and 6 [17] or equivalent [18] as well as AD neuropathologies including extracellular Aβ-amyloid plaques and intracellular neurofibrillary tangles (NFTs) in significant subsets of both PDD and DLB cases [19–28]. “Pure” α-Syn changes (without Aβ deposits or NFTs) are observed in approximately 25–35 % of cases, with additional Aβ-plaques in the remainder. Amongst those subjects with Aβ-plaques, up to half demonstrate additional NFT pathology sufficient for diagnosis of AD. In several series, the presence and severity of dementia are not predicted on the basis of the α-Syn stage or Braak AD stage [29] alone, but are best characterized by combinations of α-Syn and AD pathologies, particularly NFT extent [27, 28]. Neuroimaging studies reveal severe nigrostriatal dopamine projection losses in both PDD and DLB [30, 31], and the presence of Aβ-amyloid marker binding is reported variably in PET studies of both disorders (see below).
Amyloidopathy in Alzheimer disease and normal aging
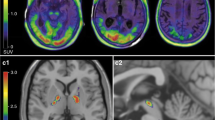
Recently developed molecular imaging approaches now permit the detection of pathological accumulations of Aβ–amyloid plaques [32], and are a subject of several manuscripts in this issue of Clinical and Translational Imaging. PET studies of fibrillary Aβ–amyloid deposition with the thioflavin derivative ligand [11C]Pittsburgh compound-B (PiB) and related clinically-approved radiofluorinated tracers including [18F]Florbetapir, [18F]Florbetaben and [18F]Flutemetamol, reveal important, new biomarker evidence for the role(s) of amyloid deposition in AD and aging (see [33] for review). To summarize the current understanding, Aβ–amyloid deposition is imaged with PET in virtually all patients with autopsy-confirmed AD. The few subjects diagnosed clinically with probable AD with “negative” amyloid scans are believed to be due to clinical misdiagnoses of frontotemporal dementia or of pure DLB as probable AD [30]. Comparative amyloid imaging and pathological confirmatory studies support the image-based classification of individual subject Aβ–amyloid status [34, 35]. The amyloid cascade hypothesis, that extracellular amyloidosis precedes the development of tau-based intracellular NFT pathology in AD, is supported by PiB-PET findings from several investigations. First, the intensity of amyloid deposition does not correlate with the severity of dementia amongst AD patients with “positive” amyloid-PET scans [36]. Second, there is high frequency of AD-range “PiB-positive” findings in pre-AD patients diagnosed with mild cognitive impairment (MCI). Amyloid-positive MCI subjects have very high rates of progression to AD over 3 years [37]. Finally, there is a substantial age-related prevalence of AD-range amyloid tracer binding amongst asymptomatic normal elderly subjects [38–40], and increased risk for development of MCI and AD in these amyloid-positive individuals [41]. These findings in normal elderly and sporadic AD subjects are recapitulated in a recent study of dominant, monogenetic AD. This report indicates the onset of amyloid deposition more than a decade before symptomatic memory deficits, supporting a long asymptomatic lag period between AD-range amyloid deposition and the onset of significant neurodegeneration [42]. Once cognitive impairment and decline develop, there was little further amyloid binding in PET imaging with [18F]Florbetapir. On this construct background, amyloid-PET findings in subjects with synucleinopathy were researched and are summarized below.
Literature review
In this manuscript, we report the results of literature searches for published amyloid-PET studies in patients with parkinsinism, including PD, PD with mild cognitive impairment (PD-MCI), PDD and DLB. We conducted an OVID-Medline search of the published literature, seeking articles identified by the intersection of {Parkinson disease.mp OR exp Parkinson Disease OR exp Lewy Body Disease} AND {florbetapir.mp OR florbetaben.mp OR flutemetamol.mp OR AV-1.mp OR AV-45.mp OR F-PIB.mp OR PIB.mp}. This search strategy identified 48 references. The authors reviewed each of these by title and abstract content, seeking original reports of PET amyloid tracer binding in patients with synucleinopathies. Papers reporting fewer than three subjects per parkinsonian diagnosis group were excluded, as were those failing to provide detailed description of the tracer binding levels that could be related to established normal and probable AD subject groups. Review articles identified in this search were not included in the analysis, but the citations therein were reviewed for possible additional original reports of amyloid binding in parkinsonian subjects. Reports that were identified as overlapping in subject content were excluded. After inclusion of these additional citations and application of exclusion criteria, 19 reports met our screening [30, 43–60].
Amyloidopathy in PD, PD-MCI, PDD and DLB
A number of prior studies have examined Aβ–amyloid deposition imaging, each involving limited numbers of PD, PDD and DLB subjects [30, 43–60]. Studies employing [11C]PiB predominate in the reported literature. We extracted from the reports the incidence of pathological (AD-range intensity) Aβ–amyloid deposition in these groups (Table 1). Most papers described the numbers of subjects with this intensity range of cortical amyloid tracer binding. However, at least one early publication reported subjects with vs. without any cortical binding above background (see Fig. 2 in [45]). In this case, we revised the authors’ estimates of amyloid incidence by imposing a cutoff threshold of 1.4:1 (cerebral cortex-to-cerebellar cortex ratio), as identified in other studies using this same tracer methodology.
Although there is a wide range of positive Aβ–amyloid incidences and relatively few subjects in most individual studies, there is general agreement that the incidence of AD-range amyloid positivity in PD with normal cognition is very low (individual study range 0–13 %; average 6 %). Within 7 individual reports including cognitively normal, non-parkinsonian subjects, the average incidence of Aβ–amyloid positivity in PD is lower than that in the normals (normal 15 %; PD 6 %). In subjects with PD-MCI, the incidence of Aβ–amyloid positivity ranges between 0 and 11 % (average 8 %), and in 3 of these 4 reports that include also cognitively normal PD groups, the incidence of amyloid positivity is no higher than in PD. Subjects with PDD have higher incidence of Aβ–amyloid positivity than do normals, PD and PD-MCI, ranging from 0 to 80 % in individual reports (average 27 %), while the incidence in DLB ranges between 33 and 100 % in individual reports (average 59 %).
Owing to the small sample sizes in some individual reports, and also potentially to differing image analysis approaches and definitions of AD-range Aβ–amyloid deposition, the individual study ranges within diagnostic groups across studies are relatively broad. However, there is general agreement both within and across virtually all reports on some aspects. First, PD and PD-MCI have similar incidences of Aβ–amyloid positivity, and these are lower than age-comparable normal subjects. Large studies of elderly subjects indicate an average of 30 % of normal subjects between ages 60 and 90 are amyloid-positive [61–63]. Parkinson disease with dementia subjects have higher than normal incidence of amyloid positivity, and DLB subjects have even higher incidence. Dementia with Lewy body subjects, however, demonstrate lower incidence of Aβ–amyloid positivity than do other large studies of probable Alzheimer disease [36, 40, 41, 43, 53, 63].
An apparent association in PD and PD-MCI subjects, not predicted by parallel studies in non-parkinsonian subjects, is the relationship of below-AD-range cortical amyloid tracer binding with measures of cognitive function. In non-parkinsonian subjects, there is no significant relationship found between intensity of amyloid tracer binding and cognitive measures, including amongst MCI and AD subjects; amyloid burden estimated in PET imaging correlates neither with severity of cognitive impairment, nor with its progression. However, a recent study in PD-MCI suggests that cortical PiB binding may correlate with global cognitive function [57].
Discussion
There are several important limitations of our Aβ–amyloid imaging literature summary in PD and related dementias. The most obvious problem is the lack of a standardized approach to data collection, processing and analysis across the many laboratories reporting original data. Most investigators to date have employed [11C]PiB as the amyloid-binding radiotracer. However, there is a dichotomy of scanning procedures, with some investigators employing tracer kinetic approaches to the estimation of tracer distribution volume (DV) measures; some with use of arterial plasma reference and others with the use of a reference brain region such as the cerebellar cortex. Other laboratories use the simple late tracer distribution (SUV) as the primary imaging outcome, again scaling the cerebral values to a reference region, most often the cerebellar cortex. While this diversity of approaches often leads to very similar binary classification of individual subject amyloid burden (positive vs. negative), there are systematic biases and distinctions that preclude our ability to impose a quantitative threshold across all studies. For this reason, we have relied heavily on each reporting laboratory to characterize the parkinsonian subjects in relation to normal and probable AD studies performed at their site and in similar fashion. Nevertheless, there are very likely classification inconsistencies between laboratories when individual subjects have scan results near to the pathologic AD threshold. An additional source of variability across studies concerns the method of cerebral cortical VOI definition. Some approaches rely on anatomic imaging (usually MRI) for stereotaxic direction of cortical and cerebellar volumes, while others may rely on PET image data alone. Some investigators report an average cerebrocortical binding measure, while others focus on cortical regions with highest and most prevalent amyloid binding in probable AD such as the precuneus and posterior cingulate cortex. Finally, there is likely a significant recruitment bias, both within and between laboratories, related to identification of PDD vs. DLB subjects. The former are most often seen in movement disorders clinics, while the latter are likely to arise in cognitive disorders clinics. Differing thresholds for determination of the movement and cognitive clinical abnormalities in the patients identified and referred for imaging may certainly contribute to the apparent imaging differences observed.
Our literature review and synthesis suggests unpredicted aspects of Aβ–amyloidopathy in PD and associated cognitive impairment syndromes. First, it appears that intense Aβ–amyloid deposition in PD patients with MCI may not anticipate by many years the development of PDD, while it does predict conversion to AD in non-PD-MCI patients. Second, there is suggestion that there may be concomitant behavioral effects of Aβ–amyloid deposition in PD as compared to the asymptomatic and behaviorally silent accumulations in non-PD elderly subjects. Both of these observations raise the possibility that the neurobiological salience of cortical Aβ–amyloid deposition differs in conjunction with neuronal α-Syn accumulation, although cellular mechanism(s) for this interaction are not yet established. This suggests an area in need of further, direct investigation, as mechanism(s) involved in this hypothetical interaction could offer novel therapeutic targets. A final unusual aspect of the Aβ–amyloid studies in parkinsonism suggests an overall lower prevalence in cognitively normal PD and in PD-MCI than in elderly subjects without neurologic abnormalities. This might suggest that synucleinopathy is in some manner protective against the mechanism(s) underlying cerebral Aβ–amyloid deposition. Although the available data do not exclude this possibility, we think it unlikely. Rather, we favor the construct that neurologically normal subjects begin asymptomatic accumulation of cerebral Aβ–amyloid deposits with increasing incidence at advancing age. If a subject with existing Aβ–amyloid deposition develops α-Syn pathology, they rapidly manifest both cognitive impairment and motor parkinsonism, and are classified clinically as DLB. Whereas, subjects who develop α-Syn pathology without antecedant Aβ–amyloid deposition are more likely to develop cognitive decline much later in the course of PD, and are more likely to have Aβ–amyloid depositions less intense than is typical of probable AD. Future studies focusing on the presymptomatic molecular imaging of DLB would be particularly informative in testing this construct.
An important descriptive result of most individual studies and of our summary is that the known pathological heterogeneity within patients classified clinically as DLB vs. PDD is reflected in the apparent heterogeneity of Aβ–amyloid positivity in these groups. It was originally hoped that clinical distinction according to the timing of movement and cognitive deficits would lead to homogeneity in underlying pathophysiologies in parkinsonian dementias. However, it has emerged that there is little evidence for clinical, behavioral or other routine diagnostic assessment that supports distinction of DLB and PDD. Results of molecular endophenotype imaging, as summarized herein, suggest an alternative classification approach: Patients could be classified according to the presence or absence of protein misfolding and aggregate deposition characteristics. At the present time, there are sensitive and specific imaging biomarkers for fibrillary Aβ–amyloid deposition, but not yet specific probes for the other potential targets in DLB and PDD. Misfolded protein aggregates containing α-Syn (in Lewy bodies and Lewy neurites), could theoretically be depicted in biomarker imaging of novel ligands, yet to be introduced and validated [64]. In addition, probes targeting the accumulations of misfolded tau proteins (including NFT tau accumulations) have been recently pursued, and several promising ligands are under active investigation [65]. Biomarker imaging with these multiple approaches could result in future imaging distinctions more closely related to underlying pathophysiologic disease mechanisms. Overall, the search for effective disease-modifying therapy for dementia in PD is likely to require this classification for appropriate selection of patients for clinical trials.
Conclusions
The pathophysiologic processes underlying dementia in patients with concomitant parkinsonian neurodegenerations are heterogeneous, involving cortical α-Syn, Aβ–amyloid and tau NFTs in varied combination. The currently established clinical classification of DLB vs. PDD is insufficient to identify and separate processes that may contribute to dementia. It is conceivable that PDD and DLB represent phenotypic variations of the same underlying process. Another possibility is that the neuropathologic resemblance of PDD and DLB represents convergence of different initial pathophysiologic pathways at advanced stages in the disease processes. A final and more likely consideration, however, may be that the heterogeneity (even at end-stage) among patients with either PDD or DLB reflects distinct neuropathologic processes that are present in some individuals across both clinical diagnostic groups—that is; the “clinical one-year rule” may be suboptimal or even inappropriate for distinguishing subtypes of dementia pathologies in synucleinopathies. Many interesting and potentially important aspects of amyloidopathy suggested in the parkinsonian dementias will require a focused, more homogeneous approach for confirmation and extension that addresses technical inconsistencies in future studies. It is hoped that molecular imaging-based classifications will fill a critical gap in our present understanding, and provide a basis for future development of novel-targeted interventions and their assessments.
References
de Lau LM, Breteler MM (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5(6):525–535
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23(6):837–844
Aarsland D, Andersen K, Larsen JP, Lolk A, Kragh-Sorensen P (2003) Prevalence and characteristics of dementia in Parkinson disease: an 8-year prospective study. Arch Neurol 60(3):387–392
Halliday G, Hely M, Reid W, Morris J (2008) The progression of pathology in longitudinally followed patients with Parkinson’s disease. Acta Neuropathol 115(4):409–415
Zaccai J, McCracken C, Brayne C (2005) A systematic review of prevalence and incidence studies of dementia with Lewy bodies. Age Ageing 34(6):561–566
Boot B (2013) The incidence and prevalence of dementia with Lewy bodies is underestimated. Psychol Med 43(12):2687–2688
Vann Jones SA, O’Brien JT (2014) The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Psychol Med 44(4):673–683
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D, Jansen EN, Ballard C, de Vos RA, Wilcock GK, Jellinger KA, Perry RH (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop (1996). Neurology 47(5):1113–1124
McKeith IG, Perry EK, Perry RH (1999) Report of the second dementia with Lewy body international workshop: diagnosis and treatment. Consortium on dementia with Lewy bodies. Neurology 53(5):902–905
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A, Kosaka K, Lee VM, Lees A, Litvan I, Londos E, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ, Yamada M (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB consortium. Neurology 65(12):1863–1872
Yoshizawa H, Vonsattel JP, Honig LS (2013) Early neuropsychological discriminants for Lewy body disease: an autopsy series. J Neurol Neurosurg Psychiatry 84(12):1326–1330
Reid WG, Hely MA, Morris JG, Loy C, Halliday GM (2011) Dementia in Parkinson’s disease: a 20-year neuropsychological study (Sydney Multicentre Study). J Neurol Neurosurg Psychiatry 82(9):1033–1037
Lippa CF, Duda JE, Grossman M, Hurtig HI, Aarsland D, Boeve BF, Brooks DJ, Dickson DW, Dubois B, Emre M, Fahn S, Farmer JM, Galasko D, Galvin JE, Goetz CG, Growdon JH, Gwinn-Hardy KA, Hardy J, Heutink P, Iwatsubo T, Kosaka K, Lee VM, Leverenz JB, Masliah E, McKeith IG, Nussbaum RL, Olanow CW, Ravina BM, Singleton AB, Tanner CM, Trojanowski JQ, Wszolek ZK (2007) DLB and PDD boundary issues: diagnosis, treatment, molecular pathology, and biomarkers. Neurology 68(11):812–819
Mosimann UP, Rowan EN, Partington CE, Collerton D, Littlewood E, O’Brien JT, Burn DJ, McKeith IG (2006) Characteristics of visual hallucinations in Parkinson disease dementia and dementia with lewy bodies. Am J Geriatr Psychiatry 14:153–160
Suzuki M, Desmond TJ, Albin RL, Frey KA (2002) Striatal monoaminergic terminals in Lewy body and Alzheimer’s dementias. Ann Neurol 51(6):767–771
Tsuboi Y, Uchikado H, Dickson DW (2007) Neuropathology of Parkinson’s disease dementia and dementia with Lewy bodies with reference to striatal pathology. Parkinsonism Relat Disord 13(Suppl 3):S221–S224
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24(2):197–211
Beach TG, Adler CH, Lue L, Sue LI, Bachalakuri J, Henry-Watson J, Sasse J, Boyer S, Shirohi S, Brooks R, Eschbacher J, White CL 3rd, Akiyama H, Caviness J, Shill HA, Connor DJ, Sabbagh MN, Walker DG (2009) Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol 117(6):613–634
Braak H, Braak E (1990) Cognitive impairment in Parkinson’s disease: amyloid plaques, neurofibrillary tangles, and neuropil threads in the cerebral cortex. J Neural Transm Park Dis Dement Sect 2(1):45–57
Dickson DW (2002) Dementia with Lewy bodies: neuropathology. J Geriatr Psychiatry Neurol 15(4):210–216
Braak H, Rub U, Jansen Steur EN, Del Tredici K, de Vos RA (2005) Cognitive status correlates with neuropathologic stage in Parkinson disease. Neurology 64(8):1404–1410
Oinas M, Sulkava R, Polvikoski T, Kalimo H, Paetau A (2007) Reappraisal of a consecutive autopsy series of patients with primary degenerative dementia: Lewy-related pathology. APMIS 115(7):820–827
Lowe J (2008) Neuropathology of dementia with Lewy bodies. Handb Clin Neurol 89:321–330
Jellinger KA (2009) Significance of brain lesions in Parkinson disease dementia and Lewy body dementia. Front Neurol Neurosci 24:114–125
Ubhi K, Peng K, Lessig S, Estrella J, Adame A, Galasko D, Salmon DP, Hansen LA, Kawas CH, Masliah E (2010) Neuropathology of dementia with Lewy bodies in advanced age: a comparison with Alzheimer disease. Neurosci Lett 485(3):222–227
Halliday GM, Holton JL, Revesz T, Dickson DW (2011) Neuropathology underlying clinical variability in patients with synucleinopathies. Acta Neuropathol 122(2):187–204
Compta Y, Parkkinen L, O’Sullivan SS, Vandrovcova J, Holton JL, Collins C, Lashley T, Kallis C, Williams DR, de Silva R, Lees AJ, Revesz T (2011) Lewy- and Alzheimer-type pathologies in Parkinson’s disease dementia: which is more important? Brain 134(Pt 5):1493–1505
Irwin DJ, White MT, Toledo JB, Xie SX, Robinson JL, Van Deerlin V, Lee VM, Leverenz JB, Montine TJ, Duda JE, Hurtig HI, Trojanowski JQ (2012) Neuropathologic substrates of Parkinson disease dementia. Ann Neurol 72(4):587–598
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82(4):239–259
Burke JF, Albin RL, Koeppe RA, Giordani B, Kilbourn MR, Gilman S, Frey KA (2011) Assessment of mild dementia with amyloid and dopamine terminal positron emission tomography. Brain 134(Pt 6):1647–1657
Koeppe RA, Gilman S, Junck L, Wernette K, Frey KA (2008) Differentiating Alzheimer’s disease from dementia with Lewy bodies and Parkinson’s disease with (+)-[11C]dihydrotetrabenazine positron emission tomography. Alzheimers Dement 4(1 Suppl 1):S67–S76
Rowe CC, Villemagne VL (2011) Brain amyloid imaging. J Nucl Med 52(11):1733–1740
Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, Bergstrom M, Savitcheva I, Huang GF, Estrada S, Ausen B, Debnath ML, Barletta J, Price JC, Sandell J, Lopresti BJ, Wall A, Koivisto P, Antoni G, Mathis CA, Langstrom B (2004) Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol 55(3):306–319
Sojkova J, Driscoll I, Iacono D, Zhou Y, Codispoti KE, Kraut MA, Ferrucci L, Pletnikova O, Mathis CA, Klunk WE, O’Brien RJ, Wong DF, Troncoso JC, Resnick SM (2011) In vivo fibrillar beta-amyloid detected using [11C]PiB positron emission tomography and neuropathologic assessment in older adults. Arch Neurol 68(2):232–240
Wolk DA, Grachev ID, Buckley C, Kazi H, Grady MS, Trojanowski JQ, Hamilton RH, Sherwin P, McLain R, Arnold SE (2011) Association between in vivo fluorine 18-labeled flutemetamol amyloid positron emission tomography imaging and in vivo cerebral cortical histopathology. Arch Neurol 68(11):1398–1403
Fodero-Tavoletti MT, Cappai R, McLean CA, Pike KE, Adlard PA, Cowie T, Connor AR, Masters CL, Rowe CC, Villemagne VL (2009) Amyloid imaging in Alzheimer’s disease and other dementias. Brain Imaging Behav 3(3):246–261
Okello A, Koivunen J, Edison P, Archer HA, Turkheimer FE, Nagren K, Bullock R, Walker Z, Kennedy A, Fox NC, Rossor MN, Rinne JO, Brooks DJ (2009) Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology 73(10):754–760
Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, Mintun MA (2010) APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol 67(1):122–131
Mielke MM, Wiste HJ, Weigand SD, Knopman DS, Lowe VJ, Roberts RO, Geda YE, Swenson-Dravis DM, Boeve BF, Senjem ML, Vemuri P, Petersen RC, Jack CR Jr (2012) Indicators of amyloid burden in a population-based study of cognitively normal elderly. Neurology 79(15):1570–1577
Rowe CC, Ellis KA, Rimajova M, Bourgeat P, Pike KE, Jones G, Fripp J, Tochon-Danguy H, Morandeau L, O’Keefe G, Price R, Raniga P, Robins P, Acosta O, Lenzo N, Szoeke C, Salvado O, Head R, Martins R, Masters CL, Ames D, Villemagne VL (2010) Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging 31(8):1275–1283
Rowe CC, Bourgeat P, Ellis KA, Brown B, Lim YY, Mulligan R, Jones G, Maruff P, Woodward M, Price R, Robins P, Tochon-Danguy H, O’Keefe G, Pike KE, Yates P, Szoeke C, Salvado O, Macaulay SL, O’Meara T, Head R, Cobiac L, Savage G, Martins R, Masters CL, Ames D, Villemagne VL (2013) Predicting Alzheimer disease with beta-amyloid imaging: results from the Australian imaging, biomarkers, and lifestyle study of ageing. Ann Neurol 74(6):905–913
Fleisher AS, Chen K, Quiroz YT, Jakimovich LJ, Gomez MG, Langois CM, Langbaum JB, Ayutyanont N, Roontiva A, Thiyyagura P, Lee W, Mo H, Lopez L, Moreno S, Acosta-Baena N, Giraldo M, Garcia G, Reiman RA, Huentelman MJ, Kosik KS, Tariot PN, Lopera F, Reiman EM (2012) Florbetapir PET analysis of amyloid-beta deposition in the presenilin 1 E280A autosomal dominant Alzheimer’s disease kindred: a cross-sectional study. Lancet Neurol 11(12):1057–1065
Rowe CC, Ng S, Ackermann U, Gong SJ, Pike K, Savage G, Cowie TF, Dickinson KL, Maruff P, Darby D, Smith C, Woodward M, Merory J, Tochon-Danguy H, O’Keefe G, Klunk WE, Mathis CA, Price JC, Masters CL, Villemagne VL (2007) Imaging beta-amyloid burden in aging and dementia. Neurology 68(20):1718–1725
Edison P, Rowe CC, Rinne JO, Ng S, Ahmed I, Kemppainen N, Villemagne VL, O’Keefe G, Nagren K, Chaudhury KR, Masters CL, Brooks DJ (2008) Amyloid load in Parkinson’s disease dementia and Lewy body dementia measured with [11C]PIB positron emission tomography. J Neurol Neurosurg Psychiatry 79(12):1331–1338
Gomperts SN, Rentz DM, Moran E, Becker JA, Locascio JJ, Klunk WE, Mathis CA, Elmaleh DR, Shoup T, Fischman AJ, Hyman BT, Growdon JH, Johnson KA (2008) Imaging amyloid deposition in Lewy body diseases. Neurology 71(12):903–910
Johansson A, Savitcheva I, Forsberg A, Engler H, Langstrom B, Nordberg A, Askmark H (2008) [(11)C]-PIB imaging in patients with Parkinson’s disease: preliminary results. Parkinsonism Relat Disord 14(4):345–347
Maetzler W, Reimold M, Liepelt I, Solbach C, Leyhe T, Schweitzer K, Eschweiler GW, Mittelbronn M, Gaenslen A, Uebele M, Reischl G, Gasser T, Machulla HJ, Bares R, Berg D (2008) [11C]PIB binding in Parkinson’s disease dementia. NeuroImage 39(3):1027–1033
Maetzler W, Liepelt I, Reimold M, Reischl G, Solbach C, Becker C, Schulte C, Leyhe T, Keller S, Melms A, Gasser T, Berg D (2009) Cortical PIB binding in Lewy body disease is associated with Alzheimer-like characteristics. Neurobiol Dis 34(1):107–112
Burack MA, Hartlein J, Flores HP, Taylor-Reinwald L, Perlmutter JS, Cairns NJ (2010) In vivo amyloid imaging in autopsy-confirmed Parkinson disease with dementia. Neurology 74(1):77–84
Foster ER, Campbell MC, Burack MA, Hartlein J, Flores HP, Cairns NJ, Hershey T, Perlmutter JS (2010) Amyloid imaging of Lewy body-associated disorders. Mov Disord 25(15):2516–2523
Jokinen P, Scheinin N, Aalto S, Nagren K, Savisto N, Parkkola R, Rokka J, Haaparanta M, Roytta M, Rinne JO (2010) [(11)C]PIB-, [(18)F]FDG-PET and MRI imaging in patients with Parkinson’s disease with and without dementia. Parkinsonism Relat Disord 16(10):666–670
Claassen DO, Lowe VJ, Peller PJ, Petersen RC, Josephs KA (2011) Amyloid and glucose imaging in dementia with Lewy bodies and multiple systems atrophy. Parkinsonism Relat Disord 17(3):160–165
Villemagne VL, Ong K, Mulligan RS, Holl G, Pejoska S, Jones G, O’Keefe G, Ackerman U, Tochon-Danguy H, Chan JG, Reininger CB, Fels L, Putz B, Rohde B, Masters CL, Rowe CC (2011) Amyloid imaging with (18)F-florbetaben in Alzheimer disease and other dementias. J Nucl Med 52(8):1210–1217
Gomperts SN, Locascio JJ, Marquie M, Santarlasci AL, Rentz DM, Maye J, Johnson KA, Growdon JH (2012) Brain amyloid and cognition in Lewy body diseases. Mov Disord 27(8):965–973
Graff-Radford J, Boeve BF, Pedraza O, Ferman TJ, Przybelski S, Lesnick TG, Vemuri P, Senjem ML, Smith GE, Knopman DS, Lowe V, Jack CR Jr, Petersen RC, Kantarci K (2012) Imaging and acetylcholinesterase inhibitor response in dementia with Lewy bodies. Brain 135(Pt 8):2470–2477
Kantarci K, Lowe VJ, Boeve BF, Weigand SD, Senjem ML, Przybelski SA, Dickson DW, Parisi JE, Knopman DS, Smith GE, Ferman TJ, Petersen RC, Jack CR Jr (2012) Multimodality imaging characteristics of dementia with Lewy bodies. Neurobiol Aging 33(9):2091–2105
Petrou M, Bohnen NI, Muller ML, Koeppe RA, Albin RL, Frey KA (2012) Abeta-amyloid deposition in patients with Parkinson disease at risk for development of dementia. Neurology 79(11):1161–1167
Gomperts SN, Locascio JJ, Rentz D, Santarlasci A, Marquie M, Johnson KA, Growdon JH (2013) Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia. Neurology 80(1):85–91
Ossenkoppele R, Prins ND, Pijnenburg YA, Lemstra AW, van der Flier WM, Adriaanse SF, Windhorst AD, Handels RL, Wolfs CA, Aalten P, Verhey FR, Verbeek MM, van Buchem MA, Hoekstra OS, Lammertsma AA, Scheltens P, van Berckel BN (2013) Impact of molecular imaging on the diagnostic process in a memory clinic. Alzheimers Dement 9(4):414–421
Shimada H, Shinotoh H, Hirano S, Miyoshi M, Sato K, Tanaka N, Ota T, Fukushi K, Irie T, Ito H, Higuchi M, Kuwabara S, Suhara T (2013) Beta-amyloid in Lewy body disease is related to Alzheimer’s disease-like atrophy. Mov Disord 28(2):169–175
Morris JC, Roe CM, Xiong C, Fagan AM, Goate AM, Holtzman DM, Mintun MA (2010) APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol 67(1):122–131
Mielke MM, Wiste HJ, Weigand SD, Knopman DS, Lowe VJ, Roberts RO, Geda YE, Swenson-Dravis DM, Boeve BF, Senjem ML, Vemuri P, Petersen RC, Jack CR Jr (2012) Indicators of amyloid burden in a population based study of cognitively normal elderly. Neurology 79(15):1570–1577
Rowe CC, Ellis KA, Rimajova M, Bourgeat P, Pike KE, Jones G, Fripp J, Tochon-Danguy H, Morandeau L, O’Keefe G, Price R, Raniga P, Robins P, Acosta O, Lenzo N, Szoeke C, Salvado O, Head R, Martins R, Masters CL, Ames D, Villemagne VL (2010) Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging 31(8):1275–1283
Shah M, Seibyl J, Cartier A, Bhatt R, Catafau AM (2014) Molecular imaging insights into neurodegeneration: focus on α-synuclein radiotracers. J Nucl Med 55:1397–1400
Shah M, Catafau AM (2014) Molecular imaging insights into neurodegeneration: focus on tau PET radiotracers. J Nucl Med 55:871–874
Conflict of interest
Dr. Frey lists grant support from General Electric and consulting activities with Siemens, Avid Radiopharmaceuticals and MIM Software. He holds general stock interests in Bristol Myers Squibb, Medtronic, Merck and Novo-Nordisk. Dr. Petrou lists no potential conflicts.
Compliance with ethical standard
No direct participation of human or experimental animal subjects was involved in this reporting; all data discussed and presented are derived from previously published scientific reports.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frey, K.A., Petrou, M. Imaging amyloidopathy in Parkinson disease and parkinsonian dementia syndromes. Clin Transl Imaging 3, 57–64 (2015). https://doi.org/10.1007/s40336-015-0104-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-015-0104-4