Abstract
Introduction
The most recent European guidelines on hypertension redefined office blood pressure (BP) treatment targets according to age strata and cardiovascular (CV) risk profile.
Aim
To evaluate proportions of adult outpatients achieving office BP treatment targets recommended by current compared to previous hypertension guidelines.
Methods
We extracted data from medical databases of adult outpatients followed in three excellence centers in hypertension (Rome, Italy; L’Aquila, Italy; Valencia, Spain). Office BP treatment targets were defined according to either 2013 ESH/ESC guidelines (< 140/90 mmHg in non-diabetic individuals aged 18–80 years, < 150/90 mmHg in those aged ≥ 80 years, and < 140/85 mmHg in diabetic individuals), or 2018 ESC/ESH guidelines: (< 130/80 mmHg in individuals aged 18–65 years, < 140/80 mmHg in those aged 65–79 and ≥ 80 years). SCORE risk was assessed in all patients.
Results
From an overall sample of 14,229 adult subjects, 4049 (28.5%) resulted normotensive individuals, 3088 (21.7%) were untreated and 7092 (49.8%) treated hypertensive outpatients. Treated hypertensives showed significantly higher ESC score risk (8.3 ± 13.0% vs. 3.9 ± 8.4%; P < 0.001) and lower systolic/diastolic BP (140.6 ± 18.8/83.9 ± 11.5 vs. 148.3 ± 14.2/94.7 ± 10.1 mmHg; P < 0.001) than untreated hypertensives. Compared to previous guidelines, BP control significantly lowered in non-diabetic outpatients (n = 5847) of all age groups [18–65 years: (13.1% vs. 42.9%), 65–79 years (25.8% vs. 42.5%) and ≥ 80 years (29.1% vs. 66.0%); P < 0.001 for all comparisons]; similar reductions were observed in diabetic outpatients (n = 1245) [18–65 years (32.7% vs. 14.8%), 65–79 years (37.3% vs. 24.7%) and ≥ 80 years (47.1% vs. 27.9%); P < 0.001].
Conclusions
According to the recommended new office BP treatment targets, the proportions of treated uncontrolled hypertensive patients substantially increased. These findings should prompt a tighter application of therapeutic recommendations and, thus, highlight the need for improving hypertension management and control strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hypertension represents one of the most relevant and frequent cardiovascular (CV) risk factors for coronary artery disease (CAD), chronic kidney disease (CKD), stroke, and congestive heart failure. It has been counted that in less than 5 years, about 1.4 billion people worldwide will be affected by hypertension [1]. Despite the efforts to promote CV health and to fight against major CV risk factors, uncontrolled BP levels can be observed in more that 40% of treated hypertensive patients [2,3,4]. Poor rates of blood pressure (BP) control have relevant socio-economic consequences, as well as important health implications, considering that elevated BP accounts for more than 54% of deaths from ischemic heart disease at world level [5].
New guidelines from European Society of Cardiology/European Society of Hypertension (ESC/ESH) are based on the most recent studies and are issued with the aim of improving the diagnosis and control of essential hypertension [6]. One of the most important novel aspect of these guidelines was the re-definition of office BP treatment targets compared to the previous ones [7]. According to new guidelines, the optimal systolic/diastolic BP goals should be 130–139/70–79 mmHg in individuals aged > 65 years and < 130 mmHg or lower, if tolerated (not < 120 mmHg), in those aged 18–65 years, with the only exception of CKD patients, in whom systolic BP treatment target should be < 140 mmHg to 130 mmHg [6]. Similar targets have been also proposed by the new American College of Cardiology/American Heart Association (ACC/AHA) United States hypertension guidelines [8], which identified patients with stage 1 hypertension in the presence of systolic BP ≥ 130 and ≤ 139 mmHg and/or diastolic BP ≥ 80 and ≤ 89 mmHg.
Redefining office BP targets has relevant implications for the daily clinical management of hypertension. Indeed, several reports have already showed how setting more ambitious BP treatment goals substantially increase the proportions of treated uncontrolled hypertensive outpatients, who are at increased risk of developing major CV outcomes compared to normotensive individuals [9,10,11]. The final goal of these more stringent therapeutic strategies is to improve management of high BP and to reduce the hypertension-related burden of disease.
On the basis of these considerations, the aim of this study was to achieve a real-life appraisal of BP control in three European hypertension excellence centers to find out whether current practice, which was turned on the BP targets recommended by previous guidelines, meets the current guidelines and, if not, how far they are. For this purpose, we explored the potential differences in the proportions of adult treated hypertensive outpatients achieving the office BP treatment targets according to previous or new European guidelines on hypertension. Secondary aim was to analyse the individual CV risk profile of treated uncontrolled outpatients, in order to evaluate how new office BP treatment targets might impact on global CV risk estimation in hypertension.
2 Methods
2.1 Methodology of the Study
This is an observational, cross-sectional, multicentre study designed to evaluate the proportions of patients achieving the office BP treatment targets recommended by 2018 ESC/ESH [6] compared to the proportions obtained by adopting the BP thresholds proposed by 2013 ESH/ESC [7] guidelines in hypertensive outpatients followed by three excellence centers in hypertension, located in low-risk areas of Southern Europe (Rome, Italy; L’Aquila, Italy; Valencia, Spain).
The entire data collection was completed on-site and then delivered to the data collection centre (Rome, IT) by on-line access to remote database. At each study site, data collection was conducted between January and April 2019. Data collection included full medical history and physical examination. Information was obtained on current therapy for hypertension, dyslipidaemia, diabetes and comorbidities, including CAD, stroke, and CKD, as well as any concomitant medications. Office systolic and diastolic BP and serum creatinine levels were extracted from available clinical records.
All BP measurements were performed according to recommendations by European guidelines [6]. Office BP measurements were performed in the Hypertension Clinics during the morning section. Sequential BP measurements were performed in a quiet room, after 5 min of rest, on the same arm and with the participant in the sitting position, by using validated devices [6]. The average of three consecutive BP measurements and heart rate was considered as clinic systolic/diastolic BP levels [6]. All BP measurements were attended. BP levels used for the analysis were derived from the last available visits.
The study conformed to the Declaration of Helsinki and its subsequent modifications, and was authorized by the reference Ethical Committee. The confidentiality of the data was carefully and strictly protected. Physicians who completed the program did not receive any compensation for their participation.
2.2 Definition of Risk Factors and Comorbidities
Diagnosis of hypercholesterolemia was defined in the presence of total cholesterol levels ≥ 190 mg/dl or low-density lipoprotein cholesterol (LDL-C) levels ≥ 130 mg/dl or stable lipid-lowering treatment in both conditions [12,13,14]. Obesity was defined in the presence of body mass index (BMI) ≥ 30 kg/m2 [15]. Diabetes was defined in the presence of plasma glucose levels ≥ 126 mg/dl or stable glucose-lowering therapy [16,17,18].
CKD was assessed by measuring plasma creatinine concentration and defined by the presence of either estimated glomerular filtration rate (eGFR) less than 60 ml/min/1.73 m2, calculated according to the Cockcroft–Gault formula, or creatinine clearance (CrCl) less than 60 ml/min/1.73 m2 [7].
CAD was defined according to the presence of the two of the following three items: symptoms (e.g. chest pain) lasting longer than 15 min, transient increase in serum concentrations of enzymes indicating cardiac damage (more than twice the upper limit of normal) and electrocardiographic changes typical of myocardial ischemia (new persistent ST-segment elevation or pathological Q waves in two contiguous leads) [19, 20]. However, the diagnosis of CAD may also include other coronary events, for example acute coronary syndrome, recurrent angina and coronary revascularization, which were distinguished in the case-report form [21]. Stroke, was defined as a neurological deficit with sudden onset and persistence of symptoms for more than 24 h or leading to death with no apparent causes other than vascular ones [22]. Transient ischemic attack was defined as a neurological event with the signs and symptoms of stroke, but which resolves within a short period of time (less than 24 h) [23].
2.3 Risk Score Models
CV risk was estimated by using European SCORE risk equation in those patients aged between 40 and 65 years and without comorbidities (primary prevention) [24]. In the presence of diabetes, SCORE risk has been corrected according to gender groups. Since study population was composed by adult Caucasian individuals, the low-risk score charts have been applied [24]. Patients with valid SCORE risk have been stratified into four groups: (1) low CV risk (SCORE < 1%); (2) moderate CV risk (SCORE ≥ 1% − < 5%); (3) high CV risk (SCORE ≥ 5% − < 10%); (4) very high CV risk (SCORE ≥ 10%).
2.4 Statistical Analysis
All data were entered into Microsoft Excel for Windows (Microsoft Office, Microsoft Corp, Redmond, Wash). Baseline characteristics of patients are presented as number and percentage for dichotomous variables and mean ± standard deviation (SD) of the mean for continuous variables. Normal distribution of data was assessed using histograms and Kolmogorov–Smirnov test. Continuous variables were tested with t-Student test, whereas dichotomous variables were tested by chi square test. All tests were two-sided, and a P value of less than 0.05 was considered statistically significant. All calculations were generated using SPSS, version 20.0 for MacOs (SPSS Inc., Chicago, Illinois).
3 Results
From an overall sample of 14,229 individuals who underwent first BP assessment or follow-up visits at the three excellence centers for hypertension, 4049 (28.5%) fell in the normotensive area, 3088 (21.7%) were untreated hypertensive patients, and 7092 (49.8%) were receiving antihypertensive drug therapies (treated hypertensive patients). General characteristics of the study population are reported on Table 1. Demographic and clinical parameters of hypertensive outpatients did not show significant differences among three centers.
As expected, treated hypertensive outpatients were significantly older and had more CV risk factors and comorbidities compared to untreated hypertensive individuals. SCORE risk estimation was significantly higher in the former than in the latter group (3.9 ± 8.4 vs 8.3 ± 13.0; P < 0.001). Conversely, average office systolic/diastolic BP levels were significantly lower in treated than in untreated hypertensive individuals (140.6 ± 18.8/83.9 ± 11.5 mmHg; vs. 148.3 ± 14.2/94.7 ± 10.1 mmHg; P < 0.001).
In treated hypertensive patients, 1245 (17.6%) were diabetics, among whom 244 (19.6%) older than 80 years, 603 (48.4%) aged between 65–79 years and 398 (32.0%) aged between 18–65 years. In non-diabetic hypertensive patients under pharmacological therapies (n = 5847; 82.4%), 802 (13.7%) were older than 80 years, 2.100 (35.9%) aged between 65–79 and 2.945 (50.4%) aged between 18–65 years.
Among treated hypertensive patients, 33.7% were on angiotensin-converting enzyme inhibitors, 43.7% received angiotensin-receptor blockers, 26.6% calcium-channel blockers, 36.4% beta-blockers and 12,8% diuretics. Treated hypertensive patients received 1.70 ± 0.9 antihypertensive drugs on average; 46.1% were on monotherapies, whilst 51.2% were treated with combination therapies (2.7% data on drug therapies not available).
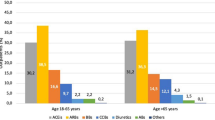
3.1 Blood Pressure Control Rates
Overall rates of BP control according to different guidelines are illustrated in Fig. 1. Proportions of treated hypertensive outpatients achieving the recommended office BP treatment targets stratified by age classes and diabetes are reported in Tables 2 and 3, respectively. Overall, about 45% of treated patients achieved office BP treatment targets proposed by previous guidelines [7], whereas only 20% of treated patients showed office BP levels within the normal ranges according to new guidelines [6]. Similar reductions in the proportions of treated controlled hypertensive patients were observed in both diabetic and non-diabetic outpatients.
Proportions of treated hypertensive patients achieving the recommended therapeutic targets according to either 2013 or 2018 European Hypertension Guidelines. In panel a, data are presented in the overall population and in subjects with or without diabetes. In panel b, data are presented according age class and presence or absence of diabetes
The proportions of non-diabetic hypertensive patients who achieved the recommended office BP treatment targets were 66% in those aged ≥ 80 years, 42.5% in those aged between 65–79 years and 42.9% in the group aged between 18–65 years, according to 2013 ESH/ESC guidelines [7]; the same proportions were 29.1%, 25.8% and 13.1% in the three age class groups of non-diabetic patients, respectively, according to 2018 ESC/ESH guidelines [6]. On the other hand, 47.1% of diabetic hypertensive patients aged ≥ 80 years, 37.3% of those aged 65–79 years and 32.7% of those aged between 18–65 years showed BP levels within the office BP treatment targets recommended by previous guidelines [7], whilst these proportions were 27.9%; 24.7% and 14.8% in the three age class groups of diabetic patients, respectively, according to new guidelines [6].
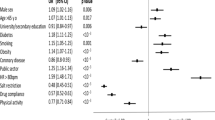
3.2 Global Cardiovascular Risk Assessment
Distribution of risk SCORE strata in treated uncontrolled hypertensive outpatients aged 40–65 years and without comorbidities (primary prevention) according to different European Guidelines is illustrated in Electronic Figure 1 (online available). As shown, there was no significant difference in the distribution of patients at high or very high CV risk between previous [7] or current [6] guidelines. At the same time, proportions of patients at low or moderate CV risk resulted slightly higher in treated uncontrolled hypertensive outpatients according to 2018 ESC/ESH guidelines [6] compared to those identified by using 2013 ESH/ESC guidelines [7]. Similar trends have been observed for both non-diabetic (panel A) and diabetic (panel B) treated hypertensive patients.
4 Discussion
Hypertension control is a key element for achieving effective CV protection and reducing the burden of hypertension-related CV diseases. In view of the mounting prevalence and increasing incidence of this condition in both high and low-income countries, mostly in Europe [25,26,27,28,29], closer attention has been devoted for implementing therapeutic strategies aimed at improving BP control in treated hypertensive patients.
Evidence from randomized controlled clinical trials have consistently demonstrated the beneficial effects of achieving the BP goals of less than 140/90 mmHg in all classes of adult hypertensive outpatients and less than 150/90 mmHg in elderly (> 65 years) hypertensive patients under pharmacological therapies [30,31,32,33,34]. More recent evidence from large clinical trials, however, have questioned these goals and proposed more stringent BP treatment targets, which have been associated with significantly lower incidence of major CV outcomes and hospitalizations compared to that obtained with conventional ones [35,36,37,38]. Following these evidence, international guidelines on hypertension now recommend the achievement of lower BP treatment targets than those promoted by the previous editions [6, 8]. However, there are limited information about the proportions of treated hypertensive patients achieving the new office BP treatment targets in the setting of real clinical practice. This may produce several socio-economic consequences and cause potentially relevant clinical implications
This first consequence of this reclassification is that a high percentage of hypertensive patients who had been considered “under control” is now reclassified as “uncontrolled”. In our study population, we confirmed that BP control was relatively poor, and this seems to be independent by the applied criteria for BP treatment targets. A possible explanation of this poor BP control might be due the frequent concomitant presence of additional comorbidities and/or difficult-to-treat hypertension among hypertensive patients referred to Excellence Hypertension Centers. Of note, BP control rate further reduced from about 45–20% in the overall population sample of treated hypertensive outpatients, by adopting new BP treatment target criteria. In particular, marked reductions of BP control were observed in non-diabetic individuals (from 46 to 19%) compared to diabetic patients (from 38 to 22%). Recent studies have reported similar results by testing the BP control rates according to previous or current US guidelines for hypertension management and control [9, 10]. These findings highlight the urgent need to implement both pharmacologic and non-pharmacologic antihypertensive treatment strategies, in order to improve the BP control rates and achieve the recommended BP treatment targets in both diabetic and non-diabetic hypertensive patients.
A second relevant consequence is the fact that a larger proportion of apparently “low risk” individuals are now potentially candidate for receiving antihypertensive drug therapies than that considered by the previous guidelines. Indeed, in our study, the most relevant drop-out of BP control has been observed in non-diabetic individuals aged between 18–65 years, in whom the proportion of patients achieving the recommended BP treatment targets falls from about 43 to 13%. This implies that a larger amount of treated hypertensive outpatients should receive more drugs and combination therapies, in order to improve the BP control rates and reduce the risk of hypertension-related complications also in low risk categories of patients without diabetes or comorbidities. In addition, among untreated normotensive individuals without comorbidities (primary prevention) (n = 1212), about 7% were at high CV risk and 5% were at very high CV risk according to European SCORE risk equation, thus requesting pharmacological interventions for reducing the risk of having major CV events.
Untreated patients correspond to about 22% of patients and they are mostly in the 18–65 years of age stratum. This was probably due to the fact that relatively young individuals at low-to-moderate cardiovascular risk profile received non-pharmacological interventions (i.e. life-style changes, diet, weight reduction, etc).
In this latter regard, the analysis of the distribution of treated uncontrolled hypertensive outpatients according to European SCORE risk categories in our population sample showed no relevant differences for those individuals at high or very high risk between previous or current guidelines. At the same time, however, new guidelines identify a larger proportion of treated uncontrolled individuals at low-to-moderate risk, for whom adoption of life-style interventions and antihypertensive treatment optimization should be implemented for ameliorating BP control rates. This aspect highlights the relevance of preventive strategies to be applied in adult hypertensive patients, who are apparently at “low risk” of experiencing major CV events, in order to reduce the burden of diseases and costs related to hypertension and its complications.
4.1 Potential Limitations
The present study is based on a cross-sectional, descriptive survey. The results presented are to be considered substantially expected as the new definition of office BP treatment targets proposed by new guidelines is shifted from higher to lower BP values than those proposed by previous guidelines. Information on out-of-office BP levels, particularly 24-h ambulatory BP monitoring, were available in a relatively limited number of patients included in the analysis, thus we cannot provide data on proportions of patients with normal (white-coat hypertension) or above normal (sustained hypertension) out-of-office BP. No data were available for the use of other antihypertensive drug classes, such as alpha-blockers and antialdosterone agents, which might be considered in difficult-to-treat hypertension to ameliorate BP control rates. This has been recently demonstrated in the Prevention And Treatment of Hypertension With Algorithm based Therapy (PATHWAY-2) trial, a randomised, double-blind crossover trial performed in the United Kingdom, which enrolled adult outpatients with resistant hypertension [39]. The use of mineralocorticoid agents (namely spironolactone 25–50 mg) was associated with significant BP reductions compared to those obtained with beta-blockers or amiloride, on top of the optimal antihypertensive therapy [39]. New hypertension guidelines have a major emphasis on initial use of single-pill combinations of at least two different antihypertensive medications as a key component of the pharmacological strategy for improving hypertension control. Given the relatively limited time elapse between publication of new guidelines and data analysis, it cannot be excluded that treating physicians have not modified their practice according to new recommendations for the clinical management of hypertension.
5 Conclusions
Our study showed that the adoption of the BP treatment targets proposed by 2018 ESC/ESH guidelines increased proportions of uncontrolled hypertensive patients across all age classes, and mostly in diabetic patients at high CV risk. Indeed, by adopting these BP treatment targets, in our sample about 80% of treated hypertensive patients need more drugs to achieve the recommended BP goals. That means that the vast majority of hypertensive outpatients needs to start antihypertensive therapy or to improve their BP lowering therapies in order to achieve the new recommended BP treatment targets. Given the fact that these findings have been reported in three excellence centers in hypertension, it might be argued that even higher proportions of treated uncontrolled hypertensive patients can be observed in the setting of general practice.
Thus, reclassification of treated hypertensive patients who did not achieve the recommended treatment goals allows us to identify substantially higher proportions of patients at low-to-moderate risk, in whom life-style measures and drug treatment optimization should be adopted, in order to ameliorate hypertension management and control and reduce the burden of hypertension-related CV diseases.
References
Egan BM, Kjeldsen SE, Grassi G, Esler M, Mancia G. The global burden of hypertension exceeds 1.4 billion people: should a systolic blood pressure target below 130 become the universal standard? J Hypertens. 2019;37(6):1148–53.
Cooney MT, Storey S, Taylor L, Dudina A, Hall M, Hemeryck L, et al. EUROASPIRE (European Action on Secondary Prevention through Intervention to Reduce Events) III—a comparison of Irish and European results. Ir Med J. 2009;102(4):113–6.
Tocci G, Ferrucci A, Pontremoli R, Ferri C, Rosei EA, Morganti A, et al. Blood pressure levels and control in Italy: comprehensive analysis of clinical data from 2000 to 2005 and 2005 to 2011 hypertension surveys. J Hum Hypertens. 2015;29(11):696–701.
Borghi C, Tubach F, De Backer G, Dallongeville J, Guallar E, Medina J, et al. Lack of control of hypertension in primary cardiovascular disease prevention in Europe: results from the EURIKA study. Int J Cardiol. 2016;01(218):83–8.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA. 2017;317(2):165–82.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219.
Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017 Nov 13.
Tocci G, Presta V, Figliuzzi I, Miceli F, Citoni B, Coluccia R, et al. Reclassification of hypertensive outpatients according to new United States guidelines on high blood pressure. Am J Hypertens. 2019;32(1):77–87. https://doi.org/10.1093/ajh/hpy139.
Lee JH, Kim SH, Kang SH, Cho JH, Cho Y, Oh IY, et al. Blood pressure control and cardiovascular outcomes: real-world implications of the 2017 ACC/AHA hypertension guideline. Sci Rep. 2018;8(1):13155.
Ruilope LM, Ruiz-Hurtado G, Barderas MG, de la Cruz JJ, Lucia A, de la Sierra A, et al. Frequency and prognosis of treated hypertensive patients according to prior and new blood pressure goals. Hypertension. 2019;74(1):130–6.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97.
Sesti G, Volpe M, Cosentino F, Crepaldi G, Del Prato S, Mancia G, et al. Metabolic Syndrome: Diagnosis and Clinical Management, an Official Document of the Working Group of the Italian Society of Cardiovascular Prevention (SIPREC) Guest Editor: E. Agabiti Rosei, President of the Italian Society of Hypertension. High Blood Pressure & Cardiovascular Prevention. 2006;13(4):185–98.
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–8.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52.
Ryden L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28(1):88–136.
Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9.
Volpe M, Borghi C, Cavallo Perin P, Chiariello M, Manzato E, Miccoli R, et al. Cardiovascular prevention in subjects with impaired fasting glucose or impaired glucose tolerance. High Blood Press Cardiovasc Prev. 2010;17(2):89.
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29(23):2909–45.
Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernandez-Aviles F, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28(13):1598–660.
Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–38.
Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(6):1583–633.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40(6):2276–93.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003.
Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289(18):2363–9.
Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–27.
de Burgos-Lunar C, Jimenez-Garcia R, Salinero-Fort MA, Gomez-Campelo P, Gil A, Abanades-Herranz JC, et al. Trends in hypertension prevalence, awareness, treatment and control in an adult type 2 diabetes Spanish population between 2003 and 2009. PLoS One. 2014;9(1):e86713.
Bromfield SG, Bowling CB, Tanner RM, Peralta CA, Odden MC, Oparil S, et al. Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and older, 1988–2010. J Clin Hypertens (Greenwich). 2014;16(4):270–6.
Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8):e003423.
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022–31.
Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):1004–10.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98.
Drawz PE, Pajewski NM, Bates JT, Bello NA, Cushman WC, Dwyer JP, et al. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) Ambulatory Blood Pressure Study. Hypertension. 2017;69(1):42–50.
Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. 2011;29(7):1253–69.
Weir MR, Hsueh WA, Nesbitt SD, Littlejohn TJ 3rd, Graff A, Shojaee A, et al. A titrate-to-goal study of switching patients uncontrolled on antihypertensive monotherapy to fixed-dose combinations of amlodipine and olmesartan medoxomil +/− hydrochlorothiazide. J Clin Hypertens (Greenwich). 2011;13(6):404–12.
Group SR, Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Data analysis has been supported by unrestricted grant from Menarini International.
Conflict of interest
Authors have no conflict of interest to disclose.
Additional information
This article is part of the topical collection on Epidemiology of Hypertension.
Electronic supplementary material
Below is the link to the electronic supplementary material.

40292_2020_359_MOESM1_ESM.jpg
Distribution of risk SCORE strata in either non-diabetic (panel A) or diabetic (panel B) uncontrolled hypertensive outpatients aged 40-65 years and without comorbidities (primary prevention) according to 2013 vs 2018 European Guidelines. (JPEG 85 kb)

Rights and permissions
About this article
Cite this article
Tocci, G., Presta, V., Ferri, C. et al. Blood Pressure Targets Achievement According to 2018 ESC/ESH Guidelines in Three European Excellence Centers for Hypertension. High Blood Press Cardiovasc Prev 27, 51–59 (2020). https://doi.org/10.1007/s40292-020-00359-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-020-00359-0