Abstract
Introduction
The use of unattended automated office blood pressure (uAutoOBP) versus attended automated (aAutoOBP) and manual auscultatory office blood pressure (AuscOBP) measurements is a topic of current controversy.
Aim
To evaluate the differences between OBP measurements methods in the general practice (GP) setting.
Methods
We first compared aAutoOBP and uAutoOBP in 42 consecutive patients with hypertension (group 1). Secondly, we compared AuscOBP to uAutoOBP measurements in 133 consecutive patients with hypertension (group 2). In addition, we analyzed the achieved OBP targets as recommended in the 2018 European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) guidelines in group 2.
Results
The mean age of patients in group 1 was 71 years (range 34–89 years, 54.8% females). The aAutoOBP and uAutoOBP systolic (131.7 and 131.6 mmHg) and diastolic (83.4 and 82.4 mmHg) mean values were not significantly different. The patient characteristics in group 2 were similar to group 1. We observed a significant difference between AuscOBP and uAutoOBP measurement for both systolic (149.4 versus 129.5 mm Hg) and diastolic (85.4 versus 81.6 mm Hg, p < 0.0001, respectively). Accordingly, 20.3% and 45.9% of patients reached the overall 2018 ESC/ESH systolic and diastolic OBP targets of < 140/80 mmHg according to AuscOBP and uAutoOBP (p < 0.0001).
Conclusion
The attended versus unattended status of automated OBP measurements had no impact on OBP values in GP. However, significantly higher OBP values and lower rates of achieved target OBP were observed by using AuscOBP measurements by physicians in comparison to automated OBP recordings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hypertension is a global public health issue that affects more than 1 billion individuals [1] and a strong risk factor for cardiovascular diseases [2]. The 2018 European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Guidelines for the management of arterial hypertension define hypertension as systolic blood pressure (SBP) values ≥ 140 mmHg, and/or diastolic BP (DBP) values ≥ 90 mmHg [2]. This definition is based on conventional office BP (OBP) measurements that are usually carried out by measuring OBP with auscultatory measurements with a conventional stethoscope or more recently with oscillometric semiautomatic or automatic methods. These measurements of OBP are typically carried out by a physician or a nurse during the visit to the office [3]. There is, however, an ongoing controversy and intensive discussion about the differences in OBP values as obtained not only by the different techniques but by also as to how the presence or absence of an attending person, e.g., physician or nurse, might affect the OBP values [4,5,6,7,8,9,10,11,12,13,14]. The fact that OBP measurements by a doctor or nurse might contribute to a pressure response resulting in higher OBP values due to an alerting reaction [15,16,17] is a well know phenomenon referred to as the “white-coat effect” [2, 18]. Consequently, the difference between the higher OBP and lower out-of- OBP values have been at least in part [19] attributed to this effect and thus to the attending vs. unattended status of OBP measurements [2].
The discussion on the differences between aAutoOBP and uAutoOBP measurements has recently been intensified after the report of the Systolic Blood Pressure Intervention Trial (SPRINT), that was conducted in 102 clinical sites in the United States and in which the OBP was measured by an unattended automated measurement technique [4, 20]. However, the method used for OBP monitoring in the study and its applicability in a real-world clinical setting in daily routine management has subsequently been a matter of controversy [2, 5, 21].
Two important studies by Filipovský et al. [22, 23]. comparing the uAutoOBP with AuscOBP measurement technique in a specialized hypertension healthcare center [22] and the other taking place in four academic hypertension centers [23], reported a significant difference between both measurements. In another critical study, however, Bauer et al. [21] used the same measurement protocol as in SPRINT [4] but in a GP office setting. Unlike, the studies by Filipovský et al. [22, 23], this study showed no significant differences between uAutoOBP readings and AuscOBP measurements.
The primary objective of the current study was to evaluate differences between aAutoOBP and uAutoOBP measurements and to compare uAutoOBP measurements with AuscOBP differences in hypertensive patients in the GP setting. In addition, we analyzed the potential implications for hypertension management based on the 2018 ESC/ESH Guidelines recommendations for target OBP in the management of arterial hypertension [2].
2 Methods
2.1 Study design
We conducted a single-center study in a large GP office in Germany (Audorfer Gemeinschaftspraxis, Oberaudorf, Germany). The Audorfer GP office treats approximately 10,000 patients per year, offering wide range of preventive, diagnostic and therapeutic services, with a particular focus on chronic diseases, such as cardiovascular diseases, diabetes and obesity. Four GPs working in this office participated in the study. All consecutive patients with hypertension during the study period between April/2018 and October/2018 were initially invited to participate during their routine clinical examination, by one of the four GPs.
Informed consent was obtained from each participant, after receiving a complete explanation about the nature of the present study. Only patients who gave their informed consent were included. Their personal information was protected following the regulations of personal data confidentiality and data pseudonomisation for analysis in agreement with the local General Data Protection Legislation (“Datenschutz-Grundverordnung”, DSGVO). The protocol was in accordance with the 1975 Helsinki Declaration and approved by the Charité ethics committee. In total, 133 consecutive patients with a diagnosis of arterial hypertension that attended the GP office for routine clinical examinations were included. All patients had been visiting the GP office for at least 1 year. Patients with hypertensive emergencies or any other severe illness or emergencies at the time of presentation were excluded.
2.2 OBP measurement
In agreement with a previous report [21], our study protocol did not interfere with the routine AuscOBP measurements used for routine patient care by the participating GPs. Thus, the number of measurements used was at the discretion of the physician (one in the majority of patients), and the devices used included OSO Kll, ERKA 2517, and BOSO Profitest sphygmomanometers.
For both aAutoOBP and uAutoOBP measurements, we used the validated Mobil-O-Graph® NG device (I.E.M GmbH, Stolberg, Germany) [24, 25]. During automated OBP measurements with the Mobil-O-Graph, OBP was measured three times in 30-s intervals. We used the mean of these three measurements for statistical analysis. All OBP measurement devices were calibrated within a year prior to the study.
In group 1, which included 42 patients (age range 34–89 years, 54.8% females and 45.2% males), automated OBP was measured with the Mobil–O- Graph using a proper size cuff bladder that was placed on the patient’s upper arm. The following protocol for aAutoOBP and uAutoOBP measurements was used:
- 1.
All patients were seated with the Mobil-O-Graph cuff in place in the same patient room, on an ergonomic examination chair, with their back and arms supported, with their feet placed flat on the floor, and without speaking during 5 min of rest.
- 2.
For the aAutoOBP measurements, the device program was started after 5 min of rest by the medical assistance staff in the patient room by pressing the Start key of the device in front of the patient and with the staff personal remaining in the patient room throughout the measurements.
- 3.
For the uAutoOBP measurements, an additional separate staff room was used in which a computer for remote control of the Mobil-O-Graph device by Bluetooth was available. First, the medical assistance staff selected the patient from the patient list on the computer, went inside the patient's room and activated the PAIr mode on the Mobil-O-Graph device. The patient was seated in the patient room and the Mobil-O-Graph cuff was placed as stated above. The entire medical assistance staff left the room. In the staff room, the Mobil-O-Graph device and the computer being in Bluetooth communications mode were paired and the measurements were started after the patient rested for 5 min in the patient room.
- 4.
The aAutoOBP and uAutoOBP measurements were performed in random order.
In the second group, including 133 patients (age range 32–93 years, 62.4% females, and 37.6% males) the participating GPs performed their routine AuscOBP measurements in the examination room. In addition, the patient was taken to a separate room to perform the uAutoOBP measurements with the Mobil-O-Graph using the same procedure described above for group 1.
The differences between aAutoOBP and uAutoOBP values were regarded as the primary endpoint of the study; we expected a maximal difference of 10 mmHg in SBP in the GP setting [21]. Thus, a sample size of 34 was required with a power of 80% power to detect this difference through a paired t test assuming that the standard SD is 20 mmHg with a α-significance level of 0.05. We increased the sample number to 42 patients (group 1).
Secondly, in an explorative analysis, we compared uAutoOBP to AuscOBP measurements by GPs (133 patients, group 2). In addition, we analyzed the OBP control rates in group 2, as recommended in the 2018 ESC/ESG guidelines [2]. Thus, we analyzed the percentage of patients achieving the overall recommended target of systolic OBP (SOBP) and diastolic OBP (DOBP) values below 140 and 80 mmHg; and the frequency of patients who achieved the lower target below 130 and 80 mmHg in the group of patients younger than 65 years and without chronic kidney disease (CKD). Finally, we determined the frequency of patients with resistant hypertension, i.e., as defined by OBP values of systolic ≥ 140 mmHg and/or diastolic ≥ 90 mmHg in response to combination therapy with three first-line drugs including a diuretic [2].
2.3 Statistical Analysis
All statistical analyses were performed using version 25 IBM SPSS Statistics Software, Armonk, NY: IBM Corp and GraphPad Prism version 8 for Windows, GraphPad Software, La Jolla California, USA. Numeric data are presented as the arithmetic mean ± SD or as a proportion (percentage). We compared the OBP values using paired 2-sided t student tests in both studies. We constructed Bland–Altmann plots to compare aAutoOBP to uAutoOBP and AuscOBP to uAutoOBP. Bias (i.e., mean of the differences) and limits of agreement of 95% were derived from Bland-Altmann analysis. Additionally, we applied Pearson’s correlation analyses to assess the association between variables. A stepwise multivariate regression analysis was then performed; using as dependent variables the SOBP and DOBO differences (Δ).Pearson's Chi-squared test was used for the analysis of control rates according to the recommended target OBP in the recent European guidelines. P values < 0.05 were regarded as statistically significant.
3 Results
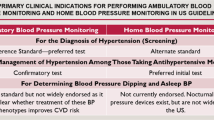
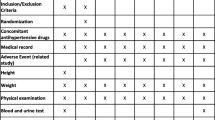
Demographic and clinical characteristics of patients in group 1 (aAutoOBP vs. uAutoOBP, 42 patients) and group 2 (AuscOBP vs. uAutoOBP, 133 patients) are summarized in Table 1. The mean age in group 1 and group 2 was 71 and 72 years, and 54.8% and 62.4% of the patients were females. The most common concomitant diseases in both groups were dyslipidemia, diabetes mellitus, stroke or transient ischemic attack, and coronary heart disease. In both groups, more than 90% of patients were treated with antihypertensive drugs, while the minority (28.6%) were treated with only one medication. As compared to males, female patients in group 1 were older (73 ± 11 vs. 64 ± 14 years, p = 0.03) but demonstrated similar SOBP (130.7 ± 15.3 vs. 132.8 ± 13.7 mmHg, p = 0.64) and DOBP (80.8 ± 11.1 vs. 85.6 ± 10.6 mmHg, p = 0.17). In group 2, male and female patients had similar age (72 ± 12 vs. 69 ± 10 years, p = 0.14) and demonstrated similar SOBP (139.9 ± 16.9 vs. 138.9 ± 16.1 mmHg, p = 0.74) and DOBP (82.4 ± 11.4 vs. 85.4 ± 11.4 mmHg, p = 0.15).
3.1 Group 1: aAutoOBP vs. uAutoOBP
No significant differences between the two methods of aAutoOBP vs. uAutoOBP measurements were detected for both SOBP (131.7 ± 14.1 mmHg vs. 131.6 ± 15.2 mmHg, p = 0.84) and DOBP (83.4 ± 10.8 mm Hg vs. 82.4 mmHg, p = 0.05). The individual OBP values of the patients are shown in Fig. 1a. The coefficient of correlation between the two methods showed a highly significant correlation for both SOBP (r = 0.93, p < 0.001) and DOBP (r = 0.96, p < 0.0001, Online Resource 1a). ΔSOBP (0.1 ± 5.7 mmHg) was significantly correlated with uAutoSOBP (r = 0.38, p < 0.0001), but not with age and gender. ΔDOBP (0.9 ± 3.2 mmHg) was not significantly correlated with age, gender, aAutoDOBP or uAutoDOBP. Δ SOBP was similar in males and females (0.2 ± 6.6 and 0.5 ± 4.5 mmHg, p = 0.7). ΔDOBP was also similar in males and females (2.4 ± 2.1 mmHg and 2.7 ± 2.2 mmHg, p = 0.6). In a stepwise multivariate analysis including age and gender in the model, ΔSOBP remained independently correlated with uAutoSOBP (beta = − 0.1, p = 0.02). Bland –Altman plot illustrates the small inter-individual differences between attended and unattended automated SOBP and DOBP values (Fig. 2a). Limits of agreement were − 10.8 mmHg to 11.1 mmHg for SOBP and − 5.2 mmHg to 7.1 mmHg for DOBP.
Individual a systolic office blood pressure (SOBP) and diastolic office blood pressure (DOBP) values of attended-automated and unattended-automated measurements in group 1 (n = 42) and b SOBP and DOBP values of manual auscultatory and unattended-automated measurements in group 2 (n = 133). *P < 0.0001 vs. other group in panel
Bland-Altman plots a comparing systolic office blood pressure (SOBP) and diastolic office blood pressure (DOBP) values of attended-automated versus unattended-automated measurements in group 1 (n = 42) and b comparing SOBP and DOBP values of auscultatory versus unattended-automated measurements in group 2 (n = 133). Solid lines, mean bias; dashed lines, 95% limits of agreement
3.2 Group 2: AuscOBP vs. uAutoOBP
Significant differences between the two methods of AuscOBP vs. uAutoOBP measurements were detected for both SOBP (149.4 ± 20.1 vs. 129.5 ± 15.8 mmHg, p < 0.0001, Fig. 1b) and DOBP (85.4 ± 12.1 vs. 81.6 ± 12.3 mmHg, p < 0.0001, Fig. 1b). The coefficient of correlation revealed significant correlations between AuscOBP and uAutoOBP measurements for both SOBP (r = 0.69, p < 0.0001) and DOBP (r = 0.73, p < 0.0001; Online Resource 1b). ΔSOBP (19.9 ± 14.8 mmHg) was positively correlated with AuscSOBP (r = 0.63, p < 0.0001), but not with age (r = 0.13, p = 0.14) and gender (r = 0.01, p = 0.90). ΔDOBP (3.9 ± 8.9 mmHg) was positively correlated with AuscDOBP (r = 0.34, p < 0.0001) and inversely correlated with uAutoDOBP (r = − 0.39, p < 0.0001), but not with age (r = 0.03, p = 0.75) and gender (r = 0.15, p = 0.08).ΔSOBP in females and males was similar (19.7 ± 13.3 and 19.9 ± 15.7 mmHg, p = 0.91). ΔDOBP was numerically but not significantly lower in females than in males, (2.1 ± 8.5 and 4.9 ± 9.0 mmHg, p = 0.08). In a stepwise multivariate analysis including age and gender in the model, ΔSOBP remained independently correlated with AuscSOBP (beta = 1.00, p < 0.0001) and ΔDOBP remained independently correlated with AuscDOBP (beta = 0.3, p < 0.0001). The corresponding Bland-Altman plots illustrate in Fig. 2b the inter-individual variability between AuscOBP and uAutoOBP for both, SOBP (a) and DOBP (b) values. The limits of agreement were wide, i.e. between − 9.2 and 48.8 mmHg for SOBP and − 13.6 and 21.2 mmHg for DOBP. In a further analysis, we evaluated the achieved OBP targets as recommended in the 2018 ESC/ESH guidelines in group 2. When AuscOBP measurements were considered, the observed systolic and diastolic OBP were below the overall recommended target of 140 and 80 mmHg in 27 patients (20.3%), while 5 of 38 patients (13.2%) achieved OBP values below the lower target of 130 and 80 mmHg in the corresponding group (Fig. 3). Resistant hypertension was observed in 13 patients (9.8%, Fig. 3). In contrast, when the uAutoOBP measurements were considered 61 patients (45.9%) and 11 patients (28.9%) of patients were controlled with values below 140/80 and 130/80 mmHg, while 5 patients (3.8%) were diagnosed with resistant hypertension (Fig. 3). Thus, control rates of hypertension were significantly lower based on the AuscOBP measurements, while the percentage of patients with resistant hypertension was higher (Fig. 3, p < 0.0001, respectively).
Percentage Patients in group 2 that achieve blood pressure control or exhibit resistant hypertension. OBP, office blood pressure; CKD, chronic kidney disease. For the definition of resistant hypertension, see text [2]. *P < 0.0001 vs. other group in panel (Pearson’s Chi-square test)
4 Discussion and Conclusion
The recent 2018 ESC/ESH Guidelines encourage, in contrast to the time-honored approach to rely only on OBP for the diagnosis on hypertension, the additional use of out-of-office BP measurement for the management of hypertension [2]. Hence, the guidelines recommend for the first time to base the diagnosis of hypertension on repeated OBP measurements or out-of-office BP measurement with ambulatory BP measurement (ABPM) and/or home BP measurement (HBPM) if logistically and economically feasible [2]. Among others, one important limitation of OBP measurements is based on the well-known “white-coat-effect” [1, 17]. The term white-coat hypertension, although originally defined for untreated individuals only, is now also used to describe discrepancies between OBP and out-of-office BP in patients treated for hypertension [2].
It is known that white-coat-hypertension can be present in up to 30–40% of the patients (> 50% in the very old patients) and its prevalence is higher in women, non-smokers and with increasing age [26, 27]. However, many studies suggest that the diagnosis of whit-coat-hypertension can be reduced or even eliminated with automated multiple OBP readings, and particularly when a doctor or nurse is not involved in the BP measurement, i.e., during uAutoOBP measurements [11,12,13, 26, 27]. An important study highlighting the potential to detect lower OBP values by uAutoOBP measurements was previously reported [22]. In this single-center study reported by Filipovský et al. [22] uAutoOBP measurements resulted in significantly lower systolic (− 15.0 mmHg) and diastolic (− 8.0 mmHg) OBP values as compared to AuscOBP measurements. Our results are thus in agreement with this study although our data with four participating physicians were obtained in a single-center GP setting, while the previous study was performed with three participating physicians in a single-center hypertension specialist clinic [22]. In a subsequent multicenter study involving 172 patients, the authors reported albeit still statistically significant, a smaller difference of 8.5 mmHg and 3.0 mm Hg between systolic and diastolic AuscOBP and uAutoOBP values [23]. However, in the previous studies yielding a difference of 15/8 mmHg automated measurements were conducted after five minutes of rest, while in the more recent study the conduction of the uAutoOBP measurements was carried out after only a short (one minute) rest period. This highlights the importance of the resting time preceding the measurements, even in the setting of measuring OBP in a separate room [28]. Nevertheless, the recent data reported by other authors [22, 23, 29] and our current data are at variance with the results obtained in a recent study in Germany involving 4 GPs´ offices [21]. In this study, no significant OBP differences between AuscOBP and uAutoOBP measurements were found in 107 subjects. Concerning the AuscOBP measurements, the measurements took place right before the automated OBP measurements in our study and the study by Bauer et al. [21]. However, in the latter study, the same person that performed the conventional OBP measurement was also responsible for the automated measurement and was also trained to use the device (i.e., Omron 907 BP monitor) and protocol of uAutoOBP measurement. Thus, this might have introduced bias by influencing at the same time, the performance of the physician during AuscOBP measurements. In contrast, in our study, the participating GPs who performed the AuscOBP measurements were not involved in automated OBP measurements, which was exclusively done by the medical staff (nurses) of the GP office. Therefore, by avoiding any interference with the conventional OBP measurements by GPs as much as possible, our study might better reflect the routine measurements of OBP as being applied by GPs in clinical routine. The potential impact on BP management between the different methods used is highlighted by our data on achieved OBP targets and the percentage of patients with resistant hypertension. Hence, the rates of achieved OBP targets were significantly higher, and the percentage of patients with resistant hypertension significantly lower when uAutoOBP measurements were considered. It appears appropriate to point out at this point that we obtained in parallel with a previous study [22] a pronounced difference between AuscOBP and automated OBP, while other recent studies observed smaller differences [23, 29]. Nevertheless, our data are compatible with a recent meta-analysis that identified a substantial pooled mean difference of +14.5 mmHg in routine, AuscSOBP compared to automated OBP measurements [11]. Thus, it seems well established that AuscOBP measurements give in general higher OBP values than automated OBP determinations [7, 11], which can have a substantial impact on hypertension management as shown. Furthermore, our study in the GP setting is in agreement with a recent meta-analysis demonstrating that, when the same measurement protocol and device are used, aAutoOBP provides similar OBP values as uAutoOBP [7].
However, some limitations of our study should be noted. First, although our study involved a large GP office with four participating physicians it nevertheless represents a single-center study with a small number of patients. Thus, a multi-center study and the enrollment of a large number of patients would have increased the validity of our findings. Moreover, we did not schedule multiple visits for OBP measurements as reported by Filipovský et al. [22]. This is a further limitation, because repeated visits allow a better determination of the reproducibility and potential impact of differences between OBP measurements, particularly regarding the white-coat effect during AuscOBP. Another limitation of the present study is the lack of standardization of the AuscOBP measurements in group 2. The rationale for this was based on our intention not to interfere with the routine procedures of the participating GPs [21].Thus, the conduction of AuscOBP measurements by the GPs should reflect their routine clinical practice. Consequently, based on our intention a bias was introduced into the comparison between the non-standardized AuscOBP and the very well standardized aAutoOBP measurements in group 2.
Hence, not only a potential white-coat affect due to the presence of the attending GP but also the less stringent methodology during the performance of AuscOBP might have contributed to the higher OBP values obtained by GPs. First, the number of AuscOBP measurements performed was only one in the majority of cases rather than three as recommended in the European guidelines [2]. Second, additional important factors such as the recommendation to investigate the patient seated in a quiet environment for 5 min before beginning the OBP measurements might have also not applied. This could have also contributed to the higher AuscOBP values observed in group 2. This limitation of AuscOBP measurements seems particularly relevant, since a large proportion of the global population spends overall only a few (less than five) minutes with their primary care physicians during their office visits [30].
Thus, in addition to the new concept that supports a wider use of out-of-office BP measurement in the 2018 ESC/ESH guidelines [2], the careful use of automated measurements- and for practical reasons possibly in the attended setting—should be the preferred method for OBP monitoring in routine clinical practice as suggested [7, 11].
References
Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. The Lancet. 2017;389(10064):37–55.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Paini A, Salvetti M, Bertacchini F, Stassaldi D, Maruelli G, Arnoldi C, et al. Unattended vs attended Bp measurement: mean values and determinants of the difference. J Hypertens. 2018;36:e70.
Group SR. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Lüscher TF, Kjeldsen SE, Mancia G, Papademetriou V. From ‘essential’ hypertension to intensive blood pressure lowering: the pros and cons of lower target values. Eur Heart J. 2017;38(44):3258–71. https://doi.org/10.1093/eurheartj/ehx643.
Stergiou GS, Kyriakoulis KG, Kollias A. Office blood pressure measurement types: different methodology—different clinical conclusions. J Clin Hypertens. 2018;20(12):1683–5.
Kollias A, Stambolliu E, Kyriakoulis KG, Gravvani A, Stergiou GS. Unattended versus attended automated office blood pressure: systematic review and meta-analysis of studies using the same methodology for both methods. J Clin Hypertens. 2019;21(2):148–55.
Nasothimiou EG, Tzamouranis D, Rarra V, Roussias LG, Stergiou GS. Diagnostic accuracy of home vs. ambulatory blood pressure monitoring in untreated and treated hypertension. Hypertens Res. 2012;35(7):750.
Quer G, Nikzad N, Chieh A, Normand A, Vegreville M, Topol EJ, et al. Home monitoring of blood pressure: short-term changes during serial measurements for 56398 subjects. IEEE J Biomed Health Inf. 2017;22(5):1691–8.
Kjeldsen SE, Mancia G. Unattended automated office vs. ambulatory blood pressure in people with high cardiovascular risk: implications for understanding the SPRINT results. J Hypertens. 2019;37(1):6–8.
Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Internal Med. 2019;179(3):351–62.
Myers MG, Parati G. Self-measurement of blood pressure in the office and at home. J Hypertens. 2003;21(12):2223–5.
Parati G, Pomidossi G, Casadei R, Mancia G. Lack of alerting reactions to intermittent cuff inflations during noninvasive blood pressure monitoring. Hypertension. 1985;7(4):597–601.
Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Grant FC, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286.
Mancia G, Bombelli M, Cuspidi C, Facchetti R, Grassi G. Cardiovascular risk associated with white-coat hypertension: pro side of the argument. Hypertension. 2017;70(4):668–75.
Mancia G, Parati G, Pomidossi G, Grassi G, Casadei R, Zanchetti A. Alerting reaction and rise in blood pressure during measurement by physician and nurse. Hypertension. 1987;9(2):209–15.
Franklin SS, Thijs L, Asayama K, Li Y, Hansen TW, Boggia J, et al. The cardiovascular risk of white-coat hypertension. J Am Coll Cardiol. 2016;68(19):2033–43.
Mancia G, Zanchetti A. Editors’ Corner: White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do. J Hypertens. 1996;14(9):1049–52.
Parati G, Omboni S, Staessen J, Thijs L, Fagard R, Ulian L, et al. Limitations of the difference between clinic and daytime blood pressure as a surrogate measure of the ‘white-coat’effect. J Hypertens. 1998;16(1):23–9.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–248.
Bauer F, Seibert FS, Rohn B, Bauer KA, Rolshoven E, Babel N, et al. Attended versus unattended blood pressure measurement in a real life setting. Hypertension. 2018;71(2):243–9.
Filipovský J, Seidlerová J, Kratochvíl Z, Karnosová P, Hronová M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 2016;25(4):228–34.
Filipovský J, Seidlerová J, Ceral J, Vysočanová P, Špác J, Souček M, et al. A multicentre study on unattended automated office blood pressure measurement in treated hypertensive patients. Blood Press. 2018;27(4):188–93.
Wei W, Tölle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Pressure Monit. 2010;15(4):225–8.
Weiss W, Gohlisch C, Harsch-Gladisch C, Tölle M, Zidek W, van der Giet M. Oscillometric estimation of central blood pressure: validation of the Mobil-O-Graph in comparison with the SphygmoCor device. Blood Pressure Monit. 2012;17(3):128–31.
Brinker S, Pandey A, Ayers C, Price A, Raheja P, Arbique D, et al. Therapeutic drug monitoring facilitates blood pressure control in resistant hypertension. J Am Coll Cardiol. 2014;63(8):834–5.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Handler J. The importance of accurate blood pressure measurement. Permanente J. 2009;13(3):51.
Andreadis EA, Geladari CV, Angelopoulos ET, Savva FS, Georgantoni AI, Papademetriou V. Attended and unattended automated office blood pressure measurements have better agreement with ambulatory monitoring than conventional office readings. J Am Heart Assoc. 2018;7(8):e008994.
Irving G, Neves AL, Dambha-Miller H, Oishi A, Tagashira H, Verho A, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902. https://doi.org/10.1136/bmjopen-2017-017902.
Acknowledgements
We are very grateful for the outstanding support of the entire staff of the Audorfer Gemeinshaftspraxis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol was in accordance with the 1975 Helsinki Declaration and approved by the Charité ethics committee.
Informed consent
Informed consent was obtained from all participants before inclusion into the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Höller, J., Villagomez Fuentes, L.E., Matthias, K. et al. The Impact of Measurement Methods on Office Blood Pressure and Management of Hypertension in General Practice. High Blood Press Cardiovasc Prev 26, 483–491 (2019). https://doi.org/10.1007/s40292-019-00347-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-019-00347-z