Abstract
Background and Objectives
Macrolide-resistant Mycoplasma pneumoniae (MR-MP) have been reported worldwide. Strategies for the treatment of MR-MP are a key focus of research. The GENECUBE® is a novel, fully automated rapid genetic analyzer. The goals of this study were to assess the macrolide sensitivity of M. pneumoniae (MP) isolates by analyzing 23S ribosomal RNA (rRNA) gene sequences using a GENECUBE®-based system and to determine the validity of this system in determining clinical treatment options for MP pneumonia.
Methods
This was an observational retrospective study including 150 children with MP pneumonia. We used quenching probe polymerase chain reaction (Q-probe PCR) as implemented in the GENECUBE® system to detect macrolide resistance-causing mutations in the MP 23S rRNA gene. We compared the duration of fever between patients receiving initial empirical antibiotic treatment (Empirical T group) and those receiving treatment after Q-probe PCR (PCR First group) diagnosis.
Results
Selecting antibiotic treatment after Q-probe PCR significantly shortened the duration of fever compared to empirical antibiotic treatment (PCR First group, median: 6.0 days [n = 32]; Empirical T group, median: 7.5 days [n = 66]; p = 0.002). Comparison of macrolide sensitivity using Q-probe PCR and clinical diagnosis showed that the reliability of Q-probe PCR was nearly validated for macrolide sensitivity.
Conclusion
Q-probe PCR as implemented by GENECUBE® is a useful tool for the diagnosis of MP pneumonia and enables optimization of the selection of antibiotics in order to rapidly improve the clinical course of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cases of Mycoplasma pneumoniae (MP) pneumonia were pre-screened with the GENECUBE® system to identify macrolide-resistant isolates. |
Pre-screening MP cases with the GENECUBE® system before antibiotic treatment led to a significant reduction in the duration of fever among MP patients. |
The GENECUBE®-based method exhibited high sensitivity, specificity, and reliability, making it a useful tool for antibiotic selection for treatment of MP infections. |
1 Introduction
Mycoplasma pneumoniae (MP) is one of three species of Mycoplasma that frequently produce infections in humans. Many pathogenic features of MP infection are presumed to be immune-mediated rather than induced directly by the bacterium [1]. Although MP infections are often associated with mild-to-moderate pneumonia [2], they can also cause serious life-threatening disease, with around a quarter of patients experiencing extrapulmonary complications [3, 4]. MP is transmitted from person to person by infected respiratory droplets during close contact.
Macrolides are usually the first-line treatment for macrolide-sensitive (MS)-MP infection. Treatment of MP infections with clarithromycin or azithromycin results in clinical benefits equal to those of erythromycin treatment [5, 6]. In 2000, pneumonia-causing MP isolates exhibiting macrolide resistance were isolated from patients with community-acquired pneumonia (CAP), and macrolide resistance has since become widespread in Japan [7, 8]. Macrolide-resistant (MR)-MP has also been reported in Asia, France, Italy, Israel, and the USA [8,9,10,11,12,13,14,15,16]. The prevalence of MR-MP infection varies among countries: for example, 9.8% in France [9], 26.0% in Italy [13], 32.1% in Israel [10], and 8.2% in 2012 [11] and 13.2% in 2015 in the USA [15]. In Japan, the highest prevalence of MR-MP was 81.6% in 2012, which gradually decreased to 59.3% in 2014 and 43.6% in 2015 [16].
Diagnosis of MP infection is usually confirmed retrospectively, such as following clinical improvement with empirical treatment, or via serological tests using enzyme immunoassays of paired acute and convalescent MP samples. Recently, direct polymerase chain reaction (PCR) has been used to detect MP genomic DNA and may be highly sensitive and specific for MP in patients with respiratory tract infections [18,19,20,21,22]. The Infectious Diseases Society of America suggests serological or PCR-based tests for the laboratory diagnosis of MP infection [17]. Serological tests and DNA detection by PCR are typically employed as diagnostic methods for MP infections, but have limitations; for example, serology can show negative results, mainly in the early disease stages, and PCR does not allow researchers to distinguish between MP infection and asymptomatic carriage. In one cross-sectional study, MP DNA was detected with similar frequency in children with and without symptoms of upper respiratory tract infection [23]. At present, we need comprehensive analysis to ascertain an accurate diagnosis of MP pneumonia, using clinical symptoms, chest X-ray, serological tests, and DNA detection by PCR, because the etiological diagnosis of respiratory infections caused by MP is a constantly challenging issue due to the current lack of a rapid, sensitive, and specific diagnostic gold standard [24].
The GENECUBE® is a novel, fully automated rapid genetic analyzer capable of extracting nucleic acids from biological material, preparing reaction mixtures, and amplifying target genes rapidly (all within 50 min) [25, 26]. Assays with this instrument are based on the hybridization of an allele-specific, fluorescence-conjugated probe and PCR amplification by melting point analysis. We thus speculated that the GENECUBE® could be used to detect MP genes rapidly. The goals of this study were to use a GENECUBE®-based system for the simultaneous detection of the presence and macrolide sensitivity of pneumonia-causing MP isolates by sequencing the 23S ribosomal RNA (rRNA) gene and to compare these results with the clinical efficacy of macrolide therapy to determine the utility of this new system in selecting antibiotics for MP treatment.
2 Subjects and Methods
This study was carried out at the Chutoen General Medical Center, a tertiary referral hospital in Shizuoka, Japan, from May 2013 to December 2017. The center covers an area with a population of about 460,000, including 64,000 children younger than 15 years old. In the present study, we retrospectively reviewed medical records to identify children suspected of having MP pneumonia.
2.1 GENECUBE® Assay and Quenching Probe (Q-Probe) Polymerase Chain Reaction (PCR) for Mycoplasma pneumoniae (MP) Detection
The GENECUBE® (TOYOBO, Ltd., Osaka, Japan) is a device that can be used for automated gene analysis, including nucleic acid extraction, amplification, and detection. This device can handle a maximum of eight samples at a time and analyze up to four items at the same time. After installing the reagents and consumables, nucleic acid extraction requires approximately 20 min, and amplification and detection can be completed in 30 min. To determine macrolide sensitivity, this method was used to detect the 23S rRNA gene of MP and identify base mutations at positions 2063 and 2064, which are the main mutations responsible for macrolide resistance [8, 9]. These can be clearly distinguished via melting curve analysis (Fig. 1).

Reproduced from Kawashima et al. [42], with permission
Melting curve analysis for detecting macrolide-resistant Mycoplasma pneumoniae and macrolide-sensitive M. pneumoniae. Negative control: result obtained after analysis of the negative control sample; Positive (wild-type): result obtained after analysis of a plasmid containing a partial wild-type M. pneumoniae 23S rRNA gene; Positive (A2063G): result obtained after analysis of a plasmid containing a partial M. pneumoniae 23S rRNA gene with the A2063G substitution; Positive (A2064G): result obtained after analysis of a plasmid containing a partial M. pneumoniae 23S rRNA gene with the A2064G substitution.
DNA extraction was performed using the GENECUBE® Prep module. PCR was carried out using the TEST BASIC KIT, which contains primers and probe dilution mixture (PPD mix, TOYOBO, Ltd., Osaka, Japan), primers, and probe. The PCR protocol involved denaturation at 94 °C for 30 s, followed by 60 cycles of denaturation at 97 °C for 1 s, annealing at 58 °C for 3 s, and extension at 63 °C for 5 s. The PCR products were then automatically subjected to melting temperature (Tm) analysis, which consisted of denaturation at 94 °C for 30 s, annealing at 39 °C for 30 s, and then heating to 75 °C at a rate of 0.09 °C/s. Q-probe fluorescence was quenched by the guanine bases in the target [25, 26].
2.2 Diagnosis of MP Pneumonia and Lower Respiratory Tract Infections
In the present study, before the diagnosis of MP pneumonia, we identified other viral and bacterial pathogens causing pneumonia using a bacterial culture test and kit for the identification of viral antigens, such as those of influenza A and B, human metapneumovirus, respiratory syncytial virus, and adenovirus. The diagnosis of MP pneumonia was based on clinical signs and symptoms of lower respiratory tract infections (cough, fever, productive sputum, dyspnea, chest pain, or abnormal breath sounds) and the presence of new infiltrates on chest radiographs that were at least segmental and were not caused by pre-existing or other known causes. The diagnosis of MP pneumonia was confirmed using quenching probe PCR (Q-probe PCR) of nasopharyngeal or oropharyngeal samples or through testing for a four-fold increase in the levels of MP antibodies in blood samples of acutely infected and convalescent (2 or 3 weeks after fever onset) patients. Antibodies to M. pneumoniae were measured using particle agglutination (PA) tests (Serodia-Myco II kit, Fujirebio, Tokyo, Japan; the manufacturers claim that the Serodia-Myco II PA test exclusively detects IgM antibody) [27]. If patients who met the criteria for MP pneumonia were suspected to also have secondary respiratory infections or other disease, we discussed and finally diagnosed the patient during a daily conference with staff doctors.
2.3 Outcomes
The primary outcome was the duration of fever, defined by the period from fever onset to the afebrile state, and this was compared between the group of children administered empirical antibiotic treatment first (Empirical T group), followed by Q-probe PCR diagnosis of MP pneumonia, and the group administered antibiotics after Q-probe PCR diagnosis of MP pneumonia (Q-probe PCR First group). Antibiotic regimens included erythromycin 25–50 mg/kg/day in four or six divided doses; clarithromycin 10–15 mg/kg/day in two or three divided doses; azithromycin 10 mg/kg in one dose (maximum dose 500 mg) on 3 days; tosufloxacin 12 mg/kg per day in two divided doses; minocycline 2–4 mg/kg/day in two divided doses; and garenoxacin 400 mg/day in one dose. The Empirical T group comprised those patients administered empirical antibiotics, including erythromycin, azithromycin, clarithromycin, tosufloxacin, minocycline, and garenoxacin, before Q-probe PCR examination. Patients administered penicillin or cephalosporin antibiotics before Q-probe PCR examination were excluded. The choice of antibiotics depended on the institutes or physicians attending the patients. The Q-probe PCR first group (PCR First) was defined as those patients administered erythromycin, azithromycin, clarithromycin, tosufloxacin, and minocycline after Q-probe PCR examination. Based on the results of Q-probe PCR, MS-MP patients were administered clarithromycin or azithromycin, MR-MP patients younger than 8 years were administered tosufloxacin, and MR-MP patients older than 8 years were administered minocycline. We compared the duration of fever, clinical course, and blood characteristics, such as white blood cells, red blood cells, hemoglobin, hematocrit, platelets, total protein, albumin, aspirate aminotransferase, alanine aminotransferase (ALT), lactate dehydrogenase, blood urea nitrogen, creatinine, total bilirubin, and C-reactive protein between the Empirical T group and the PCR First group. In the Empirical T group, blood examination was performed after macrolide or tetracycline treatment; in the PCR First group, blood examination was performed at the time of PCR examination. Corticosteroids were administered if the patient experienced a prolonged fever of more than 1 week after antibiotic therapy. Patients who were administered antibiotics with corticosteroids as the initial treatment were excluded.
The secondary outcome was the diagnosis of macrolide sensitivity in MP cases, for which clinical diagnosis was compared with Q-probe PCR detection. An MP-macrolide responder (MP-M responder) diagnosis was given to patients who were afebrile with improvements in clinical symptoms after administration of clarithromycin or azithromycin. An MP-macrolide non-responder (MP-M non-responder) diagnosis was given to patients who were not afebrile with improvements in clinical symptoms after administration of macrolide antibiotics or patients who were afebrile with improvements in clinical symptoms after administration of minocycline, tosufloxacin, or garenoxacin. Fever was defined as a maximum axillary temperature of ≥ 37.5 °C (measured two or three times) during the day. Afebrile was defined by a maximum axillary temperature of less than 37.5 °C, which was maintained for more than 48 h. Antibiotic resistance was defined as an axillary temperature of more than 37.5 °C, maintained for more than 48 h after administration of antibiotics.
2.4 Data Analysis
Results are expressed as the median and interquartile range. Two-sided comparisons between groups were conducted using the Mann–Whitney U test, Chi-square test, or Fisher’s exact test, as appropriate. Three-sided comparisons were tested using a one-way analysis of variance (ANOVA). Post hoc analyses were performed using the Bonferroni test. We calculated sensitivity, specificity, and kappa statistics with respective 95% confidence intervals (CIs) to compare the MP-M responder isolates and MS-MP isolates detected through Q-probe PCR. Kappa coefficients varied between 0 and 1. We used the following semi-quantitative scale to determine the extent of agreement: > 0.8 (very good), 0.61–0.80 (good), 0.41–0.60 (moderate), 0.21–0.40 (fair), or < 0.21 (slight) [28].
For all statistical analyses, p < 0.05 was considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Tochigi, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing) [29]. More precisely, it is a modified version of R Commander that was designed to add statistical functions frequently used in biostatistics.
3 Results
3.1 Prevalence of Macrolide-Resistant MP
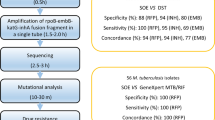
The study design is shown in Fig. 2. In total, 346 children were suspected to have MP pneumonia during the study period. Of these, 156 were excluded as they were found to be negative for MP via PCR and to not exhibit increasing mycoplasma PA. The study group therefore included 190 children suspected to have MP pneumonia. Forty cases were excluded based on the exclusion criteria, Q-probe PCR positive with no MP pneumonia, including 27 without chest X-rays, one complicated with asthma, one complicated with acute appendicitis, one complicated with Kawasaki disease, one complicated with Streptococcus pyogenes infection, and nine with symptoms of cough with no fever. In 150 children, the diagnosis of MP pneumonia was confirmed: 139 Q-probe PCR positive with MP pneumonia and 11 Q-probe negative with MP pneumonia through testing for a four-fold increase in the level of MP antibodies (PA method) in blood samples of acutely infected and convalescent patients. There were 53 patients in the hospital and 97 were outpatients. The decision to hospitalize a patient was made on a case-by-case basis depending upon age, underlying medical problems, and clinical factors including severity of illness. The selection of the hospital was determined by the institute at which members of our clinical working group were based. Of the 139 Q-probe PCR-positive MP cases, 60 were positive for MR-MP (40.0%). Table 1 shows a comparison of the clinical courses and blood examinations between MR-MP and MS-MP cases and sensitivity of Q-probe PCR for MP using the GENECUBE® method. In the Q-probe PCR-positive samples collected between 2013 and 2015, 18 of 57 (31.6%) were MR-MP positive, whereas among those collected between 2016 and 2017, 42 of 82 were (51.2%) MR-MP positive, indicating a significant increase in the prevalence over time (p = 0.025).
3.2 Empirical Treatment Versus Treatment After Detection with Q-Probe PCR
For the comparison of empirical treatment and treatment after Q-probe PCR, 41 patients were further excluded: nine patients who were administered antibiotics and corticosteroids at initial treatment, 12 patients for whom the number of afebrile days could not be confirmed because they did not follow the proper antibiotic regimen, and six and 14 patients who were administered penicillin and cephalosporin, respectively, before Q-probe PCR examination. Among the remaining patients, there was a significant difference in the duration of fever between the Empirical T and PCR First groups (Fig. 3, Table 2). There were also significant differences in the sex, number of PCR examination days, and macrolide sensitivity between the two groups. The first antibiotic therapy is shown in Table 3. In the PCR First group, there were 24 MS-MP isolates, with eight cases effectively treated with azithromycin and 13 cases effectively treated with clarithromycin. Although clarithromycin or azithromycin was indicated for two patients (a 12-year-old female and a 9-year-old male), they could not take clarithromycin or azithromycin powder and were instead administered a tablet of minocycline, leading both cases to be afebrile. One case of MS-MP was found to be resistant to azithromycin, and this patient was administered corticosteroids for prolonged fever. Also, in the PCR First group, there were eight MR-MP cases, with four effectively treated with minocycline and three effectively treated with tosufloxacin. One MR-MP case was resistant to tosufloxacin, and this patient was administered corticosteroids for prolonged fever.
Comparison of duration of fever between the Empirical T and PCR First groups. Selection of antibiotic treatment after Q-probe PCR significantly shortened the duration of fever when compared to empirical antibiotic treatment. First PCR group, median: 6.0 days (n = 32, IQR 5.0–8.0 days); Empirical T group, median: 7.5 days (n = 66, IQR 6.3–9.0 days), p = 0.002. IQR interquartile range, PCR polymerase chain reaction, Q-Probe PCR quenching probe polymerase chain reaction
In the Empirical T group, there were 22 MS-MP cases. Among these, three received empirical administration of azithromycin, including one that was resistant to azithromycin; ten received clarithromycin, including five that were resistant; two received erythromycin, including two that were resistant; one received garenoxacin and was resistant; and six received tosufloxacin, including five that were resistant. Fourteen of the 22 MS-MP cases in the Empirical T group (63.6%) were resistant to the first antibiotic used for treatment, especially those who received tosufloxacin first, with five of six being resistant. There were 44 cases of MR-MP in the Empirical T group. Among these, 14 received empirical administration of Azithromycin (AZX), all of which were resistant; two received azithromycin first and tosufloxacin second, both of which were resistant; 15 received clarithromycin, all of which were resistant; one received clarithromycin first and azithromycin second and was resistant; three received clarithromycin first and tosufloxacin second, all of which were resistant; two received minocycline, none of which were resistant; and seven received tosufloxacin, four of which were resistant. Thirty-nine of the 44 MR-MP cases in the Empirical T group (88.6%) were resistant to the first antibiotic used.
In the end, among the 22 MS-MP cases in the Empirical T group, azithromycin was effective in seven cases, clarithromycin was effective in ten cases, garenoxacin was effective in one case, and tosufloxacin was effective in two cases. Azithromycin was only partially effective in two MS-MP cases, requiring the administration of corticosteroids. Among the 44 MR-MP cases, azithromycin was effective in one case, clarithromycin was effective in one case, minocycline was effective in 22 cases, and tosufloxacin was effective in 11 cases. There were nine cases of MR-MP in the Empirical T group in which antibiotics were only partially effective (four patients administered minocycline and five administered tosufloxacin), and these patients received corticosteroids for prolonged fever.
3.3 Q-Probe PCR Versus Clinical Diagnosis of Macrolide Sensitivity
Among the patient samples, 11 were Q-probe PCR negative and 139 were Q-probe PCR positive. Of these, 21 patients were excluded, including nine patients administered antibiotics and corticosteroids at initial treatment and 12 patients for whom the number of afebrile days could not be confirmed because they did not follow the proper antibiotic regimen. Clinical diagnosis of macrolide sensitivity was therefore performed in 129 patients, with a clinical diagnosis of MP-M responders in 59 cases and a clinical diagnosis of MP-M non-responders in 70 cases. Table 4 compares rates of clinical and Q-probe PCR diagnosis of macrolide sensitivity. Those cases that were Q-probe PCR negative tended to exhibit a clinical course similar to that of MP-M non-responder cases. Among the three Q-probe PCR-negative cases that were clinically diagnosed as MP-M responders, azithromycin was effective in one case, and clarithromycin was effective in two cases. Of the eight Q-probe PCR-negative cases that were clinically diagnosed as MP-M non-responders, tosufloxacin was effective in four cases; among the other four cases, two were resistant to minocycline and two were resistant to tosufloxacin, and all received corticosteroids. Of the 11 cases diagnosed as MS-MP by Q-probe PCR but diagnosed clinically as MP-M non-responders, minocycline was effective in three cases, tosufloxacin was effective in two cases, and garenoxacin was effective in one case. The remaining five cases were resistant to azithromycin and received corticosteroids. There were 51 cases diagnosed as MR-MP using both Q-probe PCR and clinical diagnosis; among these, minocycline was effective in 27 cases, and tosufloxacin was effective in 14. Among the remaining ten cases, four were resistant to minocycline, six were resistant to tosufloxacin, and all were administered corticosteroids. Table 5 shows the validation of Q-probe PCR detection when compared to clinical diagnosis in the present study. According to this validation, for MS-MP cases, the sensitivity of Q-probe PCR was 91.5% (95% CI 81.3–97.2), specificity was 84.3% (95% CI 71.7–91.2), positive predictive value (PPV) was 83.1% (95% CI 71.7–91.2), negative predictive value (NPV) was 92.2% (95% CI 82.7–97.4), and kappa was 0.75 (95% CI 0.64–0.87). For MR-MP cases, sensitivity was 72.9% (95% CI 60.9–82.8), specificity was 96.6% (95% CI 88.3–99.6), PPV was 96.2% (95% CI 87.0–99.5), NPV was 75.0% (95% CI 63.7–84.2), and kappa was 0.68 (95% CI 0.55–0.80).
4 Discussion
Prolonged fever of more than 48 h after the initiation of antibiotic treatment has been reported in children with MR-MP who were treated with macrolide antibiotics [12, 30]. In the present study, we retrospectively compared the duration of fever between patients who received initial empirical antibiotic treatment and those who received antibiotic treatment after Q-probe PCR diagnosis. Our results showed that selecting the antibiotic for treatment after Q-probe PCR significantly shortened the duration of fever compared to empirical antibiotic treatment. No significant differences were observed between MS-MP and MR-MP in terms of clinical symptoms or examination results.
In Japan, the highest prevalence of MR-MP was 81.6% in 2012, which gradually decreased to 59.3% in 2014 and 43.6% in 2015 [16]. However, during the study period of this experiment, the prevalence of MR-MP among children in the Chutoen area increased significantly. Thus, the possibility of MR-MP should be considered in children with suspected MP infection who do not respond as expected to macrolide treatment, and strategies for MR-MP treatment should be a key area of research. Pharmacokinetic and clinical data indicate that both tetracyclines and fluoroquinolones are highly effective in the treatment of MS-MP and MR-MP [3, 7, 31,32,33]. Currently, macrolides are the only practical option for treatment of MP pneumonia in young children, since both fluoroquinolones and tetracyclines are relatively contraindicated for patients younger than 18 and 8 years of age, respectively, due to safety and toxicity concerns [34, 35]. In Japan, guiding principles for treating MP pneumonia were recently published (2014) [36]. According to this guideline, macrolides are recommended as the first-line drug for treating MP pneumonia because their minimal inhibitory concentrations (MICs) against MS-MP are quite low. In contrast, the MICs of tosufloxacin and minocycline against MP are relatively high, and in some patients infection may persist in the airways and become disseminated after treatment. Generally, children who are hospitalized with pneumonia are initially treated empirically. Empirical treatment is encouraged in the 2011 and 2014 guidelines for the treatment of MP infection [35, 36]. However, evidence has shown that the excessive and uncontrolled use of long-acting, broad-spectrum macrolides may be the main driver of the development of macrolide resistance [37], and inappropriate use or overuse of antibiotics is a major factor in the development of antibiotic resistance [38]. However, prompt initiation of antibiotic treatment is crucial in children with CAP. With changes in the prevalence of MR-MP, the optimization of antibacterial use is important, both in the care of individual patients and within strategies to address the wider problem of antibacterial resistance. This has prompted the need for methods allowing the rapid diagnosis of MP infections and the proper use of antibiotics in the treatment of outpatients. Our results show that the Q-probe PCR as implemented by the GENECUBE® system can enable the optimization of antibacterial selection and be used to rapidly improve the clinical course of MP pneumonia.
Previous research reported a PCR method for MP detection with a sensitivity of 92% [21]. In the present study, the sensitivity of the Q-probe PCR for detecting MP infection was unclear. Recently, inconsistencies have been reported between PCR-based and PA tests for MP laboratory diagnosis, indicating that PA tests may exhibit high false-positive rates and that PCR-based tests may be more accurate in detecting true MP infection [39]. Moreover, no single diagnostic test is considered optimal for MP detection, and improved assays are required [24]. We validated the ability of Q-probe PCR to determine the macrolide sensitivity of MP isolates by comparing it with the clinical diagnosis of macrolide sensitivity. The reliability of Q-probe PCR in determining macrolide sensitivity was nearly validated. Thus, our results showed that the sensitivity, specificity, and reliability of the Q-probe PCR as implemented by GENECUBE® were sufficient for the detection of macrolide sensitivity in MP pneumonia. The sensitivity and accuracy of Q-probe PCR are dependent on the design of primers with high amplification efficiency, and several sets of PCR primers have been designed for Q-probe PCR of MP. The Q-probe PCR GENECUBE® system allows for the rapid, simple, non-invasive detection of 23S rRNA gene mutations within 50 min from start to finish.
A 2014 systematic review of 17 studies (4294 patients) found insufficient evidence for the efficacy of antimicrobial treatment of MP in reducing respiratory tract infections or improving symptoms, including the duration of fever [39]. This analysis, however, was limited by publication bias; heterogeneity; and the lack of blinding, consistent diagnostic methods, reliable outcome measures, and information on duration of symptoms or mixed infections in the included studies [40, 41]. We suggest that the Q-probe PCR by GENECUBE® is a useful tool for the clinical and epidemiological control of MP pneumonia.
There are several limitations of the present study. This study was conducted with a relatively small number of patients and used a retrospective, cross-sectional study design. There may be selection bias, as all cases of MP pneumonia were derived from a single tertiary referral hospital. There were significant differences in macrolide sensitivity between the Empirical T and PCR First groups. One reason for this difference could be that some children with MP pneumonia who were administered empirical antibiotic treatment improved before being referred our hospital; these children were therefore excluded from the present study. In the present study, the empirical therapeutic use of fluoroquinolones and tetracyclines was conducted in only three patients: one was administered garenoxacin and two were administered minocycline. Although the sample size was small, we considered that there was no bias in the analysis of primary outcomes of the empirical therapeutic use of fluoroquinolones and tetracyclines. The GENECUBE® method cannot detect the macrolide resistance-causing mutation at position 2617 in the 23S rRNA gene of MP, and thus MP pneumonia cases with this mutation were included in the MS-MP group. However, the most frequent MR-MP-causing mutation in Japan is the mutation at position 2063 [16]. Cases of MR-MP pneumonia caused by the 2617 mutation may be very rare, and this source of study bias can largely be ignored. Fourth, we did not analyze mutations in the 23S rRNA gene by direct sequencing to confirm the results of Q-probe PCR. However, previous studies validated the 23S rRNA gene mutation using Q-probe PCR [42]. ALT levels were significantly different between the MR-MP and MS-MP cases. The reason for this is unknown but may involve bias due to the limited number of study subjects. There was a distinct difference in the collection timing of initial blood samples between the Empirical T group and PCR First group. Comparisons between these datasets may have introduced bias. Another limitation was the complete exclusion of secondary respiratory infections.
5 Conclusion
In spite of the limitations mentioned, and although decisions regarding empirical treatment are complicated by substantial differences in the clinical presentation of MP pneumonia, Q-probe PCR by GENECUBE® can be useful for optimizing antibacterial selection and rapidly improving the clinical course of disease. Further studies of the Q-probe PCR by the GENECUBE® system, including prospective randomized trials, are needed given the frequent use of macrolide antibiotics in children.
References
Baseman JB, Reddy SP, Dallo SF. Interplay between mycoplasma surface proteins, airway cells, and the protean manifestations of mycoplasma-mediated human infections. Am J Respir Crit Care Med. 1996;154:S137–44.
File TM. The science of selecting antimicrobials for community-acquired pneumonia (CAP). J Manag Care Pharm. 2009;15:S5–11.
Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004;17:697–728.
Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol Rev. 2008;32:956–73.
Cassell GH, Drnec J, Waites KB, Pate MS, Duffy LB, Watson HL, McIntosh JC. Efficacy of clarithromycin against Mycoplasma pneumoniae. J Antimicrob Chemother. 1991;27:47–59.
Schönwald S, Skerk V, Petricevic I, Car V, Majerus-Misic L, Gunjaca M. Comparison of three-day and five-day courses of azithromycin in the treatment of atypical pneumonia. Eur J Clin Microbiol Infect Dis. 1991;10:877–80.
Miyashita N, Akaike H, Teranishi H, Ouchi K, Okimoto N. Macrolide-resistant Mycoplasma pneumoniae pneumonia in adolescents and adults: clinical findings, drug susceptibility, and therapeutic efficacy. Antimicrob Agents Chemother. 2013;57:5181–5.
Kawai Y, Miyashita N, Kubo M, Akaike H, Kato A, Nishizawa Y, et al. Therapeutic efficacy of macrolides, minocycline, and tosufloxacin against macrolide-resistant Mycoplasma pneumoniae pneumonia in pediatric patients. Antimicrob Agents Chemother. 2013;57:2252–8.
Peuchant O, Ménard A, Renaudin H, Morozumi M, Ubukata K, Bébéar CM, et al. Increased macrolide resistance of Mycoplasma pneumoniae in France directly detected in clinical specimens by real-time PCR and melting curve analysis. J Antimicrob Chemother. 2009;64:52–8.
Averbuch D, Hidalgo-Grass C, Moses AE, Engelhard D, Nir-Paz R. Macrolide resistance in Mycoplasma pneumoniae, Israel, 2010. Emerg Infect Dis. 2011;17:1079–82.
Yamada M, Buller R, Bledsoe S, Storch GA. Rising rates of macrolide-resistant Mycoplasma pneumoniae in the central United States. Pediatr Infect Dis J. 2012;31:409–11.
Kawai Y, Miyashita N, Yamaguchi T, Saitoh A, Kondoh E, Fujimoto H, et al. Clinical efficacy of macrolide antibiotics against genetically determined macrolide-resistant Mycoplasma pneumoniae pneumonia in paediatric patients. Respirology. 2012;17:354–62.
Chironna M, Sallustio A, Esposito S, Perulli M, Chinellato I, Di Bari C, et al. Emergence of macrolide-resistant strains during an outbreak of Mycoplasma pneumoniae infections in children. J Antimicrob Chemother. 2011;66:734–7.
Okada T, Morozumi M, Tajima T, Hasegawa M, Sakata H, Ohnari S, et al. Rapid effectiveness of minocycline or doxycycline against macrolide-resistant Mycoplasma pneumoniae infection in a 2011 outbreak among Japanese children. Clin Infect Dis. 2012;55:1642–9.
Zheng X, Lee S, Selvarangan R, Qin X, Tang YW, Stiles J, et al. Macrolide-resistant Mycoplasma pneumoniae, United States. Emerg Infect Dis. 2015;21:1470–2.
Tanaka T, Oishi T, Miyata I, Wakabayashi S, Kono M, Ono S, et al. Macrolide-resistant Mycoplasma pneumoniae infection, Japan, 2008–2015. Emerg Infect Dis. 2017;23:1703–6.
Baron EJ, Miller JM, Weinstein MP, Richter SS, Gilligan PH, Thomson RB Jr, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2013 recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM)(a). Clin Infect Dis. 2013;57:e22–121.
Tjhie JH, van Kuppeveld FJ, Roosendaal R, Melchers WJ, Gordijn R, MacLaren DM, et al. Direct PCR enables detection of Mycoplasma pneumoniae in patients with respiratory tract infections. J Clin Microbiol. 1994;32:11–6.
Blackmore TK, Reznikov M, Gordon DL. Clinical utility of the polymerase chain reaction to diagnose Mycoplasma pneumoniae infection. Pathology. 1995;27:177–81.
Ramirez JA, Ahkee S, Tolentino A, Miller RD, Summersgill JT. Diagnosis of Legionella pneumophila, Mycoplasma pneumoniae, or Chlamydia pneumoniae lower respiratory infection using the polymerase chain reaction on a single throat swab specimen. Diagn Microbiol Infect Dis. 1996;24:7–14.
Xu D, Li S, Chen Z, Du L. Detection of Mycoplasma pneumoniae in different respiratory specimens. Eur J Pediatr. 2011;170:851–8.
American Academy of Pediatrics. Mycoplasma pneumoniae and other Mycoplasma species infections. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red book: 2015 report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village: American Academy of Pediatrics; 2015. p. 568.
Spuesens EB, Fraaij PL, Visser EG, Hoogenboezem T, Hop WC, van Adrichem LN, et al. Carriage of Mycoplasma pneumoniae in the upper respiratory tract of symptomatic and asymptomatic children: an observational study. PLoS Med. 2013;10:e1001444.
Montagnani F, Rossetti B, Vannoni A, Cusi MG, De Luca A. Laboratory diagnosis of Mycoplasma pneumoniae infections: data analysis from clinical practice. New Microbiol. 2018;41(3):203–7.
Hida Y, Hisada K, Shimada A, Yamashita M, Kimura H, Yoshida H, et al. Rapid detection of the Mycobacterium tuberculosis complex by use of quenching probe PCR (geneCube). J Clin Microbiol. 2012;50:3604–8.
Furuta T, Soya Y, Sugimoto M, Nishino M, Yamade M, Uotani T, et al. Rapid automated genotyping of CYP2C19 and Helicobacter pylori 23S rRNA gene in gastric juice. J Gastroenterol Hepatol Res. 2013;2:508–12.
Barker CE, Sillis M, Wreghitt TG. Evaluation of Serodia Myco II particle agglutination test for detecting Mycoplasma pneumoniae antibody: comparison with mu-capture ELISA and indirect immunofluorescence. J Clin Pathol. 1990;43(2):163–5.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Kanda Y. Investigation of the freely-available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Yoo SJ, Kim HB, Choi SH, Lee SO, Kim SH, Hong SB, et al. Differences in the frequency of 23S rRNA gene mutations in Mycoplasma pneumoniae between children and adults with community-acquired pneumonia: clinical impact of mutations conferring macrolide resistance. Antimicrob Agents Chemother. 2012;56:6393–6.
Cao B, Zhao CJ, Yin YD, Zhao F, Song SF, Bai L, et al. High prevalence of macrolide resistance in Mycoplasma pneumoniae isolates from adult and adolescent patients with respiratory tract infection in China. Clin Infect Dis. 2010;51:189–94.
File TM Jr, Schlemmer B, Garau J, Cupo M, Young C, 049 Clinical Study Group. Efficacy and safety of gemifloxacin in the treatment of community-acquired pneumonia: a randomized, double-blind comparison with trovafloxacin. J Antimicrob Chemother. 2001;48:67–74.
Hoeffken G, Talan D, Larsen LS, Peloquin S, Choudhri SH, Haverstock D, et al. Efficacy and safety of sequential moxifloxacin for treatment of community-acquired pneumonia associated with atypical pathogens. Eur J Clin Microbiol Infect Dis. 2004;23:772–5.
Bradley JS, Jackson MA, Committee on Infectious Diseases; American Academy of Pediatrics. The use of systemic and topical fluoroquinolones. Pediatrics. 2011;128:e1034–45.
Ouchi K, Kurosaki T, Okada K, editors. Guidelines for management of respiratory infectious diseases in children in Japan 2011, Joint Committee of Japanese Society of Pediatric Infectious Disease and Japanese Society of Pediatric Pulmonology. Pneumonia [in Japanese]. Tokyo: Kyowa Kikaku Ltd.; 2011. p. 44.
Kohno S, Ishida T, Izumikawa K, Iwata S, Kadota J, Tanaka H, The Committee of Japanese Society of Mycoplasmology, et al. Guiding principles* for treating Mycoplasma pneumoniae pneumonia. Japan; 2014. http://square.umin.ac.jp/jsm/Eng%20shisin.pdf#search=%27Guiding+principles%2A+for+treating+Mycoplasma+pneumoniae+pneumonia%27.
Odonkor ST, Addo KK. Bacteria resistance to antibiotics: recent trends and challenges. Int J Biol Med Res. 2011;2:1204–10.
van de Sande-Bruinsma N, Grundmann H, Verloo D, Tiemersma E, Monen J, Goossens H, European Antimicrobial Resistance Surveillance System Group; European Surveillance of Antimicrobial Consumption Project Group, et al. Antimicrobial drug use and resistance in Europe. Emerg Infect Dis. 2008;14:1722–30.
Wang L, Feng Z, Zhao M, Yang S, Yan X, Guo W, et al. A comparison study between GeXP-based multiplex-PCR and serology assay for Mycoplasma pneumoniae detection in children with community acquired pneumonia. BMC Infect Dis. 2017;17:518.
Biondi E, McCulloh R, Alverson B, Klein A, Dixon A, Ralston S. Treatment of Mycoplasma pneumonia: a systematic review. Pediatrics. 2014;133:1081–90.
Colin AA, Yousef S, Forno E, Korppi M. Treatment of Mycoplasma pneumoniae in pediatric lower respiratory infection. Pediatrics. 2014;133:1124–5.
Kawashima Y, Uekura Y, Yamashita K, Notake S, Nakamura K, Kimata S, et al. Construction and evaluation of a method for detecting genetic mutations for macrolide resistance in Mycoplasma pneumoniae with an auto gene analyzer, GENECUBE [in Japanese]. J Jpn Soc Clin Microbiol. 2018;28:98–105.
Acknowledgements
The authors thank the Committee of Chutoen General Medical Center for their assistance in the treatment of patients admitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yutaka Ito, Satoru Iwashima, Satoshi Hayano, Tomohiro Nishio, Ryosuke Shiozawa, Soichiro Yata, Toshiko Kubota, Akira Kubota, and Keiichi Uemura do not have any potential, perceived, or real conflicts of interest, in particular any financial arrangements relevant to this article.
Funding
The authors have no financial relationships relevant to this article to disclose. The equipment of the Chutoen General Medical Center was used for this study.
Ethical approval and informed consent
The study protocol was approved by the Ethics Committee of Chutoen General Medical Center (approval date: 31 May 2018; approval number: 75) and was conducted according to the principles of the Declaration of Helsinki. Prior consent was obtained via opt-out and inclusion agreements based on the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects. We posted an explanation of this study on the internet homepages of the participating institutions, and when a participant stated their intention to withhold consent, we excluded the corresponding data from this study.
Rights and permissions
About this article
Cite this article
Ito, Y., Iwashima, S., Hayano, S. et al. Rapid Detection of the Macrolide Sensitivity of Pneumonia-Causing Mycoplasma pneumoniae Using Quenching Probe Polymerase Chain Reaction (GENECUBE®). Mol Diagn Ther 22, 737–747 (2018). https://doi.org/10.1007/s40291-018-0360-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-018-0360-x