Abstract
Objective
To evaluate the cost effectiveness of genetic screening for the apolipoprotein (APOE) ε4 allele in combination with preventive donepezil treatment in comparison with the standard of care for amnestic mild cognitive impairment (AMCI) patients in Canada.
Methods
We performed a cost-effectiveness analysis using a Markov model with a societal perspective and a time horizon of 30 years. For each strategy, we calculated quality-adjusted life-years (QALYs), using utilities from the literature. Costs were also based on the literature and, when appropriate, Ontario sources. One-way and probabilistic sensitivity analyses were performed. Expected value of perfect information (EVPI) analysis was conducted to explore the value of future research.
Results
The base case results in our exploratory study suggest that the combination of genetic testing and preventive donepezil treatment resulted in a gain of 0.027 QALYs and an incremental cost of $1,015 (in 2009 Canadian dollars [Can$]), compared with the standard of care. The incremental cost-effectiveness ratio (ICER) for the base case was Can$38,016 per QALY. The ICER was sensitive to the effectiveness of donepezil in slowing the rate of progression to Alzheimer’s disease (AD), utility in AMCI patients, and AD and donepezil treatment costs. EVPI analysis showed that additional information on these parameters would be of value.
Conclusion
Using presently available clinical evidence, this exploratory study illustrates that genetic testing combined with preventive donepezil treatment for AMCI patients may be economically attractive. Since our results were based on a secondary post hoc analysis, our study alone is insufficient to warrant recommending APOE genotyping in AMCI patients. Future research on the effectiveness of preventive donepezil as a targeted therapy is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Alzheimer’s disease (AD) is a degenerative brain disease that impairs cognitive function, memory, and activities of daily living [1]. According to estimates for the year 2008, management of AD in Canada cost $15 billion (in Canadian dollars [Can$]) in direct, indirect, and unpaid caregiver opportunity costs, and required 231 million hours of informal care time [2]. There has been limited success in treating AD, which motivates scientists to find solutions to delay the onset of AD at an earlier stage. Mild cognitive impairment (MCI) represents a transitional state between the cognitive abilities of normal aging and early-stage AD [3]. Therefore, there is a national and global imperative to prevent the progression of MCI to AD. Amnestic mild cognitive impairment (AMCI) is a subtype of MCI involving impaired memory but otherwise intact cognitive function, and patients with this condition are at increased risk of developing AD [4]. Progression to AD may also accelerate in the presence of one or more apolipoprotein (APOE) ε4 alleles [5–7]. Approximately 24% of the AMCI population in Canada carry the ε4/ε4 APOE genotype [8], and AMCI patients who carry two APOE ε4 alleles have a 94% chance of developing AD by the age of 80 years [9]. Genetic testing for the presence of APOE ε4 alleles may be an efficient way to target a therapy to a group that has a higher risk of progressing to AD and is likely to benefit from the health intervention.
Scientists have been investigating different ways to delay and prevent AD. One method includes the use of therapeutics such as cholinesterase inhibitors (donepezil, rivastigmine, galantamine, memantine) to slow cognitive decline; these treatments are currently used for mild to moderate AD. Although the current standard of care in the treatment of MCI does not include these medications [10], there may be some clinical benefit from using pharmacotherapy at an earlier stage as preventive treatment. A systematic search of the literature in Medline retrieved only two randomized controlled trials (RCTs) that investigated the effect of the drug donepezil in AMCI patients. In the first study, 132 AMCI patients who received donepezil treatment for 24 weeks did not show significant improvement in primary efficacy measures but did show improvement in secondary ones [11]. The second study compared the effectiveness of donepezil treatment with a placebo in delaying the onset of AD among AMCI patients [4]. Although the study found that donepezil delayed the onset of AD during the first 12 months of treatment, the difference in the progression rate did not persist after 3 years. In a secondary post hoc analysis, however, the benefit of donepezil was evident among carriers of one or more APOE ε4 alleles throughout the 3-year follow-up period.
The second study showed the potential of identifying APOE ε4 allele carriers through genetic testing as a more effective way of screening for AMCI patients who are most likely to benefit from targeted therapeutics. Although several studies have assessed the cost effectiveness of donepezil in AD and MCI patients [12–15], there has been no economic evaluation of APOE ε4 genetic testing in combination with preventive donepezil therapy in patients with AMCI. Those studies focused only on the economic evaluation of donepezil treatment and did not consider the association between gene polymorphisms and potential outcomes.
Since personalized medicine and pharmacogenomics are relatively new areas of research, the benefits of new genetic tests and their impact on the cost effectiveness of treatment remain uncertain. The RCT mentioned earlier, which evaluated genetic testing in AMCI patients, could not make a strong recommendation, because of insufficient data. Specifically, it only examined treatment effects in separate groups of APOE ε4 carriers and non-carriers in a secondary post hoc analysis [4]. Despite this shortcoming, an effort to model the combination of genetic testing and preventive donepezil treatment for AMCI patients can still prove useful because it can generate the framework necessary to analyze different treatment scenarios in anticipation of the influx of more robust clinical evidence.
The primary objective of this study, therefore, was to evaluate the potential cost effectiveness of APOE ε4 testing in combination with preventive donepezil treatment (the “targeted therapy” strategy). We compared the proposed strategy with the standard of care for AMCI patients in Canada: specifically, routine monitoring until progression to AD without genetic testing and preventive treatment (the “standard of care” strategy). Because of the uncertainty in the available data, this type of study is exploratory and relies on secondary post hoc analysis. Consequently, another objective of the study was to understand the impact of these uncertainties on the estimates of the cost effectiveness of the aforementioned test and treatment strategy.
Definitive conclusions drawn from the results of economic evaluations should be met with some caution. Because of its exploratory nature, by itself this study may not be useful for decision makers who decide on funding. Rather, this study, while providing significant insight into a proposed health intervention, more importantly can inform future clinical research as well as form the basis of further economic research when more clinical evidence is available. A study of genetic testing in combination with preventive treatment for AMCI patients has not been conducted before and, additionally, resource use for AMCI patients has never been investigated in a North American setting.
2 Methods
2.1 Outline of the Model
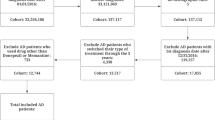
A Markov model was designed to simulate the natural history of AMCI over a 30-year time horizon (reflecting the life expectancy of the cohort). Health effects were expressed as quality-adjusted life-years (QALYs), which weigh length-of-life with quality-of-life data—specifically, health-state utilities. The model simulates a hypothetical cohort of 70-year-old AMCI patients with problems in the memory domain (a Mini-Mental State Examination [MMSE] score in the range of 27–30), subdivided into APOE ε4 carriers and non-carriers. Each year, patients can either progress to AD or die from other causes (Fig. 1). Transition probabilities define the movement between health states and were estimated using data from published literature (Table 1). Patients accrue costs and QALYs on the basis of the amount of time spent in each health state, which are assigned unique cost and utility estimates. This analysis was conducted from a societal perspective in a Canadian setting. A 1-year cycle length was used, and both costs and effects were discounted by 5% per year.
In the targeted therapy strategy, the model begins with the hypothetical cohort receiving an APOE genetic test during a visit to a memory clinic or a neurologist. If the test identifies a patient as a carrier of one or more APOE ε4 alleles, the patient receives donepezil as a preventive treatment to delay the onset of AD. Non-carriers are monitored until they develop AD. Since the genetic test works on any good-quality DNA, and the procedure itself and interpretation of the result are straightforward and transparent (0.01% attributable to human error), we assumed the APOE ε4 allele genetic test specificity and sensitivity to be 100%. In the standard of care strategy, patients receive neither APOE genetic testing nor preventive treatment and are only monitored until progression to AD. In both scenarios, once patients progress to AD, we assumed they receive a drug of similar cost and effectiveness to donepezil until they die.
Using guidelines [16], we conducted a systematic review in Medline for every model parameter, including the prevalence of APOE ε4 allele in AMCI patients and the mortality risk, health-state utilities, and costs of both AMCI and AD patients. To conduct a systematic review of the effectiveness of preventive donepezil treatment among APOE ε4 carriers and non-carriers, we searched Medline and Cochrane Reviews databases. We used Grading of Recommendations Assessment, Development and Evaluation (GRADE) quality assessment methods [17] to appraise estimates for clinical parameters.
2.2 Prevalence of the Apolipoprotein ε4 Allele Among Patients with Amnestic Mild Cognitive Impairment
We obtained the prevalence of the APOE ε4 allele among AMCI patients in Canada (24%) from the Canadian Study of Health and Aging (CSHA), which investigated the epidemiology of dementia in Canada [8]. The CSHA study uses a definition termed “cognitive impairment and no dementia” (CIND), which has clinical characteristics similar to those of AMCI [18]. One European study of APOE ε4 prevalence in cognitively impaired individuals attending memory clinics reported statistics of 15% in controls and 36% in patients with AMCI [19]. Another memory clinic sample replicated a tendency for a North–South gradient in APOE e4 prevalence in Europe, which had been noted previously in population studies. It cited 31.5% prevalence in Southern Europe and up to 62.7% prevalence in patients with MCI or subjective complaints [20]. We explored the effect of prevalence in a sensitivity analysis to assess the generalizability of our results to a higher-prevalence setting.
2.3 Transition Probabilities
We obtained the annual risk of death of the general population in Canada from Canadian life tables [21]. We assumed that the mortality rate from AMCI is the same as that of the general population. The annual mortality risk of patients with AD was calculated using the relative risk from age-matched annual mortality rates for AD patients from the US Monongahela Valley Independent Elders Survey (MoVIES) [23], which suggested that AD patients have a higher mortality risk than MCI patients. In a sensitivity analysis, we ran a scenario where the mortality risk of AD patients was the same as that of AMCI patients. We also assumed that the mortality risk is independent of APOE carrier status.
We obtained the rates of progression from AMCI to AD for the first 3 years and the effectiveness of preventive donepezil treatment in delaying the onset of AD from a multicenter RCT investigating the effectiveness of preventive donepezil treatment in North American AMCI patients [4]. The trial used the onset of AD as the primary outcome and defined AD according to the clinical criteria of the National Institute of Neurological and Communicative Diseases and Stroke and the Alzheimer’s Disease and Related Disorders Association [4]. The trial compared the progression from AMCI to AD between those who received 10 mg of donepezil daily as preventive treatment (the donepezil group) and those who received no preventive treatment (the placebo group) every 6 months over 3 years. A secondary post hoc analysis from the RCT showed that donepezil had a treatment benefit in APOE ε4 carriers over the 3-year period but had a limited effect on non-carriers. We estimated the transition probabilities from the conditional probabilities of developing AD (using Kaplan-Meier estimates of the rate of progression from MCI to AD as shown in Fig. 1 in the original trial publication) [4]. In the primary analysis, which combined APOE ε4 carriers and non-carriers, the donepezil group had a lower rate of progression to AD than the placebo group in the first year, but their progression rate increased in subsequent years and converged with that of the placebo group after 3 years. We recognize that there is some uncertainty in generalizing the results from the secondary post hoc analysis to the AMCI population in the Canadian setting, and thus we also conducted extensive sensitivity and scenario analyses on the slowing of the rate of progression to AD and the effectiveness of donepezil. We did not adjust the effectiveness estimates for dropouts, because the trial estimates we used were analyzed with an intention-to-treat principle, which takes into account the effect of dropouts.
Since there is little evidence on the effectiveness of donepezil beyond 3 years, we assumed that after year 3, donepezil does not delay cognitive decline. To be conservative, we assumed that those who receive donepezil have a higher rate of progression to AD in the fourth year (18.9% per year) than those who do not receive donepezil (8.1% per year), and so they have an equivalent cumulative probability of developing AD by the end of year 4. In subsequent years, all groups have the same annual probability of developing AD (8.1%), estimated from a meta-analysis of rates of progression from MCI to AD, which included 29 robust inception cohort studies [24].
2.4 Quality of Life
We obtained health-state utilities for AMCI and AD (Table 1) from a study that elicited quality-of-life estimates from 679 North American patients at various stages of AD (from “questionable AD” to terminal AD), using the Health Utilities Index 2 (HUI2) method [25–27]. The study categorized patients by using the Clinical Dementia Rating (CDR) scale [28]. We estimated the health-state utility score of AMCI from the mean score of 52 patients with questionable AD (CDR score 0.5), and we used utility values from the mild, moderate, and severe categories for the AD health states [28].
2.5 Resource Use and Costs
We estimated the costs from standard costing sources in Ontario, Canada, and published literature [29–31]. Currently, the APOE ε4 genetic test is not publicly available in Canada, and we had to use several sources to generate an estimate. In our base case, we assumed that each genetic test costs Can$325. This estimate is the average of the service fee from a medical laboratory services company in the US [32] and the genetic test cost retrieved from a recent Ontario report [33]. We conducted a sensitivity analysis using a higher cost estimate for genetic testing. For the targeted therapy strategy, we assumed that APOE ε4 carriers receive 10 mg of donepezil daily as a preventive treatment. Gastrointestinal side effects such as diarrhea and nausea are the most common adverse events associated with donepezil; we assumed that 10% of those receiving donepezil would experience gastrointestinal adverse events per year [4] and that management would require three visits to a general physician, with visit costs being estimated using the Ontario physician fee schedule [34].
Our systematic search found one study on the cost associated with MCI from a German societal perspective, which was inflated and converted to Can$ [48]. For the genetic screening strategy, we assumed that patients identified as APOE ε4 carriers would have several extra physician visits for surveillance compared with non-carriers, because they are at higher risk of developing AD. The annual cost of AD includes the costs of nursing home care, medication, community support services, and caregivers’ productivity loss. We abstracted the costs associated with different stages of AD from an earlier Canadian costing study that focused on AD [35]. We expressed all costs in 2009 Can$, inflated using the medical component of the Canadian Consumer Price Index, when necessary [37].
2.6 Sensitivity Analysis
We conducted deterministic and probabilistic sensitivity analyses to assess the uncertainty of all parameters. We varied all parameters separately in one-way sensitivity analyses (ranges shown in Table 1). For the probabilistic sensitivity analyses, we used gamma distributions to represent uncertainty in the cost parameters because cost data are skewed and cannot be negative. We used beta distributions for the probabilities and utilities because these estimates are confined to a 0–1 range (Table 1). All parameters were randomly sampled from their assigned distributions, and 1,000 simulations were performed. We estimated the likelihood of each treatment strategy being the more favorable across a range of willingness-to-pay (WTP) thresholds. To assess the value of additional information, we calculated the expected value of perfect information (EVPI) with a 20-year lifespan of the testing technology and a partial EVPI (EVPPI) for the input parameters at various WTP thresholds [38]. From the 24% prevalence of AMCI and population estimates in Canada, we estimated the number of AMCI patients aged 70 years and older in Canada to be 275,000. Using this population estimate, we estimated the population EVPI at different WTP thresholds.
3 Results
3.1 Base Case
In AMCI patients, genetic testing in combination with preventive donepezil treatment for APOE ε4 carriers was more effective (0.027 QALY gained) and more costly (an additional Can$1,015) than the standard of care strategy. The incremental cost-effectiveness ratio (ICER) of the genetic test strategy was Can$38,016 per QALY gained (Table 2). Over the course of the model, 68% of the cohort developed AD.
3.2 Sensitivity Analysis
One-way sensitivity analysis revealed that the results were most sensitive to the effectiveness of donepezil in slowing the rate of progression to AD, utility in AMCI patients, and AD and donepezil treatment costs (Fig. 2). The effects of changes in other parameters, such as utility values in AD, the prevalence of the APOE ε4 allele, discount rates, and genetic test and AMCI surveillance costs, were less pronounced.
We explored a scenario where the progression rate differs only on the basis of treatment and not APOE ε4 carrier status, using the rates of progression to AD observed in the RCT among placebo- and donepezil-treated groups without APOE carrier status stratification. In this scenario, the ICER increased to Can$113,647 per QALY gained. In another scenario where we limited the time horizon of the analysis to 3 years, the ICER decreased slightly to Can$36,229 per QALY gained. One study found that individuals with MCI were 1.74 times more likely to die than those without cognitive impairment [22]. If the annual mortality risk of patients with AMCI was 1.74 times higher than that of the general population, the ICER decreased to Can$25,876 per QALY gained. In a scenario with no differential mortality between AMCI and AD patients, the ICER was Can$1,714 per QALY gained. When we increased the genetic test cost by a factor of 3, assuming a combination of new genes and other yet to be discovered AD risk factors, the ICER using the more expensive genetic test increased to Can$62,366 per QALY gained. Changing the analytical perspective to the health system payer changed the ICER to Can$50,182 per QALY gained.
Probabilistic sensitivity analysis revealed that most of the 1,000 simulated ICERs were located mainly in the northeast quadrant and some in the southwest quadrant, with a center close to the origin of the cost-effectiveness plane (Fig. 3). If one QALY gained is valued at Can$50,000, then 55% of the simulated ICERs were considered cost effective (Figs. 3, 4). The genetic testing strategy had a higher chance of being cost effective (66%) if the WTP was Can$100,000 per QALY (Fig. 4).
3.3 Expected Value of Perfect Information
The overall EVPIs were Can$667, Can$856, and Can$900 per patient at WTP thresholds of Can$20,000, Can$50,000, and Can$100,000 per QALY, respectively (Fig. 5). The EVPI for a target population size of 275,000 is considerable at Can$255 million if the WTP threshold is Can$35,000, and also steadily increases above Can$65,000, as shown in Fig. 6. The partial EVPI for parameters varied with WTP thresholds (Fig. 5). At a WTP threshold of Can$50,000 per QALY, additional information on the natural progression to AD, efficacy of preventive treatment, donepezil treatment costs and post-progression AD treatments costs would be valuable. Although there is little uncertainty around the unit cost of donepezil, there are uncertainties around the dose, frequency, and duration of preventive treatment. With corresponding partial EVPIs being quite low, conducting additional research on quality-of-life estimates, surveillance costs, and adverse event costs would be of little value.
4 Discussion
In our model, APOE ε4 genetic testing with preventive donepezil treatment was more costly and more effective than the standard of care strategy. The benefit of the targeted therapy strategy, conferred through a reduction in progression to AD among APOE ε4 allele carriers during the first 3 years, translated into an average gain equivalent to 10 days of quality-adjusted life per patient. Although the effect size may appear small, it is comparable to QALYs gained in studies for other recognized health interventions, such as pharmacogenetic testing in the clinical management of schizophrenia (4 days) [39] or adjuvant treatment in postmenopausal women with breast cancer (25 days) [40]. The additional cost of Can$1,015 per patient combined with the effectiveness estimate results in an ICER of Can$38,016 per QALY gained. This suggests that the targeted therapy strategy could be a cost-effective intervention if the WTP exceeds Can$39,000 per QALY gained.
Our sensitivity analysis results suggest that the ICER varies somewhat with changes in parameters that may be specific to jurisdictions, such as the prevalence of APOE ε4 alleles in the AMCI population and costs. Our estimates of the prevalence of APOE ε4 alleles in AMCI and of the cost of AD are lower than published estimates from other countries [19, 41, 42]. Overall, this implies that our results are likely to be generalizable to other jurisdictions as long as the country-specific values are within the ranges tested in our sensitivity analysis; if the estimates of the prevalence of APOE ε4 alleles in AMCI and of the cost of AD were higher in other jurisdictions, the ICER would likely be lower.
The comparative benefit of the targeted therapy strategy versus the standard of care strategy in AMCI patients is based on two important clinical parameters: (i) an elevated risk of developing AD among carriers of APOE ε4 alleles compared with non-carriers; and (ii) delayed progression to AD with preventive donepezil treatment specifically among APOE ε4 allele carriers. Studies have found an association between APOE ε4 carriage and development of AD [6, 43–45]. However, the accuracy of APOE ε4 genotyping in predicting progression of MCI to AD is not high enough on its own to warrant its use in clinical practice, because not all ε4 carriers will develop AD, and many non-carriers may develop AD. Although we obtained our effectiveness estimates from a large, multicenter RCT [4], the estimates were from a secondary post hoc analysis, and the authors did not feel that their results were statistically powered to make a policy recommendation around the targeted therapy strategy. Also, the effectiveness of donepezil treatment among APOE ε4 carriers is still debatable, especially considering that a separate RCT that investigated the effectiveness of another cholinesterase inhibitor among APOE ε4 carriers [46] did not publish its findings. Our EVPI analysis suggests that additional research on the effectiveness estimate would be valuable to reduce this uncertainty.
The weighted annual baseline rate of progression (12%) in our study, combining APOE ε4 carriers and non-carriers, was based on the RCT [4]. This rate is similar to the rate (13%) reported in a recent study among patients seen in a memory disorder clinic [47]. The same study also reported a 3% progression rate among a community-based sample. Although our baseline rate is higher than the rate in the community setting, we are modeling a scenario of offering APOE genetic testing to patients at a memory disorder clinic, which justifies the appropriateness of this higher rate.
To date, this is the first economic evaluation of genetic testing in combination with preventive donepezil treatment in AMCI patients. It would not be appropriate to compare our results with the results from other economic evaluations of donepezil treatment in AD patients; in our study, the incremental benefit from the new intervention for APOE ε4 carriers was gained in the “pre-dementia” MCI state before progression to AD. The only previously published economic evaluation of donepezil treatment in MCI patients did not stratify patients by their APOE ε4 carrier status and only used hypothetical efficacy and utility values instead of estimates from the published literature [15]. The results of that evaluation also suggested that preventive donepezil treatment is less attractive in the absence of a mechanism to identify and direct therapy to high-risk individuals.
Our study had several limitations. First, there is limited evidence on the effectiveness of donepezil treatment in delaying progression from AMCI to AD among APOE ε4 carriers. However, our study showed the framework of evaluating a targeted therapy in preventing the onset of AD from MCI, and may be useful when more evidence on effective targeted therapies in this area appears. Second, we used surveillance costs for AMCI patients from a German study of costs associated with MCI in primary care [48]. That study was undertaken using an older patient population (average age 81 years) than our starting cohort, and it was conducted in a different health care system, which means that certain cost components could potentially have differed. However, the impact of any such differences would be small, since surveillance costs were not a key driver in the model. Third, we did not model a higher mortality rate among AD patients who carry APOE ε4 alleles, as was observed in one study, because that study may have had selection biases that limited the generalizability of the results [49]. However, if a higher mortality rate does exist for APOE ε4 patients with AD, slowing the progression of AD with testing and early treatment among this subgroup may be even more favorable than we estimated. Finally, widely accepted and validated criteria for diagnosing MCI are unavailable. The differences between this term and other clinical definitions suggested for cognitive dysfunction associated with aging, such as “cognitive impairment no dementia”, “mild cognitive decline”, and “age-associated cognitive decline”, are not clear [50]. In addition, flexibility in the interpretation of AMCI, in combination with differences in the mean age of samples and variability in the diagnostic criteria and method of recruitment, have resulted in prevalence estimates ranging from 1% to 26% among elderly participants in epidemiologic studies [51]. Incorrect AMCI diagnoses were not considered in the model, but a substantial rate of incorrect diagnoses would increase direct medical costs for testing, resulting in an increased ICER. We also would not capture those who are not seen and diagnosed with AMCI before development of AD, and thus this strategy would not benefit such patients. More effort may be required in implementing standard diagnostic criteria and estimating the frequency of AMCI diagnosis in the elderly population.
In the future, APOE genotypes may be useful in combination with other clinical measures or genetic variations. Notably, recent genome-wide association studies undertaken by large genetics consortia reported nine novel AD loci [52], each of which adds to the risk of dementia later in life; however, the largest effect on the risk of late-onset AD is observed for the APOE ε4 allele. This information provides great insight into the cause of AD, since the gene discovery will contribute to predicting who will develop AD, which will be important when preventive measures become available. In addition, recent pharmacogenomic studies have shown that carriers of some genotypes have worse responses to conventional anti-dementia drugs [53], highlighting the potential of targeted therapy in preventing and treating AD. Although our study is exploratory in nature, it is the first economic evaluation of pharmacogenomics in delaying the onset of AD, which may offer insights for future studies evaluating technologies for use in a similar disease area in light of more evidence of effective target therapies.
5 Conclusion
Our study was prompted in part by the hypothesis that among APOE ε4 carriers, preventive donepezil treatment could potentially delay progression from AMCI to AD. Given this possibility, we created a model to explore genetic testing for APOE ε4 in combination with preventive donepezil treatment for carriers of this allele, using a Canadian context. The incremental cost effectiveness of this new intervention is strongly dependent on the effectiveness of preventive donepezil treatment in delaying progression from AMCI to AD among APOE ε4 carriers, for which there is currently limited evidence. Such data limitations should be kept in mind when interpreting our exploratory results. As more evidence of effective targeted therapy in delaying progression to AD becomes available, the economic evaluation estimates can be updated with new data.
References
Alzheimer’s Disease Education and Referral Centre, National Institute on Aging About Alzheimer’s disease: Alzheimer’s basics. http://www.nia.nih.gov/alzheimers/topics/alzheimers-basics. Accessed 25 Oct 2012.
Alzheimer Society Canada. Rising tide: the impact of dementia on Canadian society. http://www.alzheimer.ca/en/Get-involved/Raise-your-voice/Rising-Tide/Rising-tide-summary. Accessed 25 Oct 2012.
Petersen RC. Mild cognitive impairment: aging to Alzheimer’s disease. New York: Oxford University Press; 2003.
Petersen RC, Thomas RG, Grundman M, et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352(23):2379–88.
Korovaitseva GI, Shcherbatykh TV, Selezneva NV, et al. Genetic association between the apolipoprotein E (ApoE) gene alleles and various forms of Alzheimer’s disease [in Russian]. Genetika. 2001;37(4):529–35.
Goldman JS, Hou CE. Early-onset Alzheimer disease: when is genetic testing appropriate? Alzheimer Dis Assoc Disord. 2004;18(2):65–7.
Tierney MC, Szalai JP, Snow WG, et al. A prospective study of the clinical utility of ApoE genotype in the prediction of outcome in patients with memory impairment. Neurology. 1996;46(1):149–54.
Hsiung GY, Sadovnick AD, Feldman H. Apolipoprotein E epsilon4 genotype as a risk factor for cognitive decline and dementia: data from the Canadian Study of Health and Aging. CMAJ. 2004;171(8):863–7.
Fleck LM. Just caring: the moral and economic costs of APOE genotyping for Alzheimer’s disease. Ann NY Acad Sci. 1996;802:128–38.
Chertkow H, Massoud F, Nasreddine Z, et al. Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. CMAJ. 2008;178(10):1273–85.
Salloway S, Ferris S, Kluger A, et al. Efficacy of donepezil in mild cognitive impairment: a randomized placebo-controlled trial. Neurology. 2004;63(4):651–7.
Neumann PJ, Hermann RC, Kuntz KM, et al. Cost-effectiveness of donepezil in the treatment of mild or moderate Alzheimer’s disease. Neurology. 1999;52(6):1138–45.
O’Brien BJ, Goeree R, Hux M, et al. Economic evaluation of donepezil for the treatment of Alzheimer’s disease in Canada. J Am Geriatr Soc. 1999;47(5):570–8.
Feldman N, Gauthier S, Hecker J, et al. Economic evaluation of donepezil in moderate to severe Alzheimer disease. Neurology. 2004;63:644–50.
Kasuya M, Meguro K. Health economic effect of donepezil treatment for CDR 0.5 converters to Alzheimer’s disease as shown by the Markov model. Arch Gerontol Geriatr. 2010;50(3):295–9.
Khan KS, Kunz R, Kleijnen J, et al. Systematic reviews to support evidence-based medicine: how to review and apply findings of healthcare research. London: Royal Society of Medicine Press; 2003.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Davis HS, Rockwood K. Conceptualization of mild cognitive impairment: a review. Int J Geriatr Psychiatry. 2004;19(4):313–9.
van der Flier WM, Pijnenburg YA, Schoonenboom SN, et al. Distribution of APOE genotypes in a memory clinic cohort. Dement Geriatr Cogn Disord. 2008;25(5):433–8.
Norberg J, Graff C, Almkvist O, et al. Regional differences in effects of APOE epsilon4 on cognitive impairment in non-demented subjects. Dement Geriatr Cogn Disord. 2011;32(2):135–42.
Statistics Canada. Census: population and dwelling counts. http://www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97-550/Index.cfm?TPL=P1C&Page=RETR&LANG=Eng&T=101. Accessed 29 Oct 2012.
Bennett DA, Wilson RS, Schneider JA, et al. Natural history of mild cognitive impairment in older persons. Neurology. 2002;59(2):198–205.
Dodge HH, Shen C, Pandav R, et al. Functional transitions and active life expectancy associated with Alzheimer disease. Arch Neurol. 2003;60(2):253–9.
Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia: meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119(4):252–65.
Neumann PJ, Sandberg EA, Araki SS, et al. A comparison of HUI2 and HUI3 utility scores in Alzheimer’s disease. Med Decis Making. 2000;20(4):413–22.
Jonsson L, Andreasen N, Kilander L, et al. Patient- and proxy-reported utility in Alzheimer disease using the EuroQoL. Alzheimer Dis Assoc Disord. 2006;20(1):49–55.
Kerner DN, Patterson TL, Grant I, Kaplan RM. Validity of the quality of well-being scale for patients with Alzheimer’s disease. J Aging Health. 1998;10(1):44–61.
Morris JC. The clinical dementia rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412–4.
Ministry of Health and Long-Term Care. Ontario drug benefit formulary/comparative drug index no. 41. http://www.health.gov.on.ca/english/providers/program/drugs/formulary/edition_41.pdf. Accessed 25 Oct 2012.
Ministry of Health and Long-Term Care. Schedule of benefits for physician services under the Health Insurance Act. http://www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/physserv_mn.html. Accessed 25 Oct 2012.
Ministry of Health and Long-Term Care. Schedule of benefits for laboratory services: April 1, 1999. http://www.health.gov.on.ca/english/providers/program/ohip/sob/lab/lab_services_sched_01_19990401.pdf. Accessed 29 Oct 2012.
SpectraCell Laboratories. SpectraCell Laboratories offers apolipoprotein E genetic testing [media release]. http://www.spectracell.com/media/press-release-apo-e.pdf. Accessed 25 Oct 2012.
Miller F, Hurley J, Morgan S, et al. Predictive genetic tests and health care cost: final report prepared for the Ontario Ministry of Health and Long Term Care. http://www.health.gov.on.ca/fr/common/ministry/publications/reports/geneticsrep02/chepa_rep.pdf. Accessed 25 Oct 2012.
Wong CL, Bansback N, Lee PE, Anis AH. Cost-effectiveness: cholinesterase inhibitors and memantine in vascular dementia. Can J Neurol Sci. 2009;36(6):735–9.
Hux MJ, O’Brien BJ, Iskedjian M, et al. Relation between severity of Alzheimer’s disease and costs of caring. CMAJ. 1998;159(5):457–65.
Hogan DB, Thierer DE, Ebly EM, Parhad IM. Progression and outcome of patients in a Canadian dementia clinic. Can J Neurol Sci. 1994;21(4):331–8.
Statistics Canada. Consumer price index, health and personal care. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/cpis01a-eng.htm. Accessed 25 Oct 2012.
Oostenbrink JB, Al MJ, Oppe M, Rutten-van Molken MP. Expected value of perfect information: an empirical example of reducing decision uncertainty by conducting additional research. Value Health. 2008;11(7):1070–80.
Perlis RH, Ganz DA, Avorn J, et al. Pharmacogenetic testing in the clinical management of schizophrenia: a decision-analytic model. J Clin Psychopharmacol. 2005;25(5):427–34.
Lonning PE. Comparing cost/utility of giving an aromatase inhibitor as monotherapy for 5 years versus sequential administration following 2–3 or 5 years of tamoxifen as adjuvant treatment for postmenopausal breast cancer. Ann Oncol. 2006;17(2):217–25.
Rice DP, Fox PJ, Max W, et al. The economic burden of Alzheimer’s disease care. Health Aff (Millwood). 1993;12(2):164–76.
Fagnani F, Lafuma A, Pechevis M, et al. Donepezil for the treatment of mild to moderate Alzheimer’s disease in France: the economic implications. Dement Geriatr Cogn Disord. 2004;17(1–2):5–13.
Mayeux R, Saunders AM, Shea S, et al. Utility of the apolipoprotein E genotype in the diagnosis of Alzheimer’s disease. Alzheimer’s Disease Centers Consortium on Apolipoprotein E and Alzheimer’s Disease. N Engl J Med. 1998;338(8):506–11.
Lindsay J, Laurin D, Verreault R, et al. Risk factors for Alzheimer’s disease: a prospective analysis from the Canadian Study of Health and Aging. Am J Epidemiol. 2002;156(5):445–53.
Elias-Sonnenschein LS, Viechtbauer W, Ramakers IH, et al. Predictive value of APOE-epsilon4 allele for progression from MCI to AD-type dementia: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(10):1149–56.
Novartis Clinical Trial Results Database. A prospective, randomized, multicenter, double blind, placebo-controlled, parallel-group study of the effect of rivastigmine on the time to clinical diagnosis of Alzheimer’s disease in subjects with mild cognitive impairment (MCI). http://www.novctrd.com/ctrdWebApp/clinicaltrialrepository/displayFile.do?trialResult=1886. Accessed 25 Oct 2012.
Farias ST, Mungas D, Reed BR, et al. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66(9):1151–7.
Luppa M, Heinrich S, Matschinger H, et al. Direct costs associated with mild cognitive impairment in primary care. Int J Geriatr Psychiatry. 2008;23:963–71.
Williams MM, Xiong C, Morris JC, Galvin JE. Survival and mortality differences between dementia with Lewy bodies vs Alzheimer disease. Neurology. 2006;67(11):1935–41.
Raschetti R, Albanese E, Vanacore N, Maggini M. Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomized trials. PLoS Med. 2007;4(11):e338.
Lopez OL, Jagust WJ, DeKosky ST, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study, part 1. Arch Neurol. 2003;60:1385–9.
Naj AC, Jun G, Beecham GW, et al. Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet. 2011;43(5):436–41.
Cacabelos R, Martinez-Bouza R. Genomics and pharmacogenomics of dementia. CNS Neurosci Ther. 2011;17(5):566–76.
Funding statements
This research was supported by grant no. RE01-061 from the Ontario Research Fund. Katherine Siminovitch is supported by a Canada Research Chair award and the Sherman Family Chair in Genomic Medicine. The Pharmacoeconomics Research Unit is supported by Cancer Care Ontario and the Ministry of Health. This research does not reflect the views of the funders.
Conflict of interest disclosures
Dr. Sandra Black has received speaker’s honoraria from Pfizer, Eisai, and Novartis, and ad hoc consulting fees from Pfizer, Novartis, GlaxoSmithKline, Roche, Bristol-Myers Squibb, and Elan. Dr. Black’s research unit has received research funds from Pfizer, GlaxoSmithKline, Lundbeck, Roche, and Novartis. The others authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Djalalov, S., Yong, J., Beca, J. et al. Genetic Testing in Combination with Preventive Donepezil Treatment for Patients with Amnestic Mild Cognitive Impairment. Mol Diagn Ther 16, 389–399 (2012). https://doi.org/10.1007/s40291-012-0010-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-012-0010-7