Abstract
Background
Direct patient reporting (DPR) is a system where patients report suspected adverse drug reactions (ADRs) directly to competent bodies. Studies have shown the added advantages of DPR of ADRs. In August 2012, the National Pharmacovigilance Centre (NPC) commenced implementation of a Pharmacovigilance Rapid Alert System for Consumer Reporting (PRASCOR) under the spontaneous reporting system, with the aim of facilitating direct consumer reporting of suspected ADRs to the drug regulatory authority.
Objectives
This study aims to examine the performance of PRASCOR by determining its quantitative contribution to spontaneous reporting of ADRs in Nigeria from inception in August 2012 to February 2017.
Method
In the PRASCOR system, consumers of medicines who experience an untoward effect are encouraged to send a prepaid short text message with the name of the medicine and the reaction to a short code (20543). This message with the consumer’s phone number is forwarded as an email alert to the National Agency for Food and Drug Administration and Control (NAFDAC) for follow-up. Logs of text messages from the PRASCOR system obtained from the service provider were reviewed to determine the number of consumer alerts and ‘reportable alerts’ received during the review period. Furthermore, the NPC local database was reviewed to determine the number of individual case safety reports (ICSRs) from PRASCOR and characterize them.
Results
A total of 47,071 hits were logged by the PRASCOR server. There were 3594 ‘consumer complaints’, of which 94% were ‘reportable alerts’. Fifty-two per cent (n = 1758) of ‘reportable alerts’ contained information on both a medicine and a suspected ADR. A total of 353 ICSRs in the local database were attributed to PRASCOR, but only 247 (70%) of these were successfully matched to the originating PRASCOR alert. For the period under review, PRASCOR contributed 3.9% of reports in the NPC local database.
Conclusion
We conclude that, quantitatively, PRASCOR contributed minimally to the number of ADR reports received under the spontaneous reporting system, but has potential for performing better and adding value to the reporting of ADRs and pharmacovigilance in Nigeria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Consumers are willing to share their medicine-related experiences with the drug regulatory authority in Nigeria through the Pharmacovigilance Rapid Alert System for Consumer Reporting (PRASCOR). |
PRASCOR contributed quantitatively to adverse drug reactions reported in the local database, albeit minimally. |
Strengthening and improving the PRASCOR system will provide greater benefit to the Nigerian pharmacovigilance system. |
1 Introduction
Adverse drug reaction (ADR) reporting is a fundamental part of a pharmacovigilance (PV) system as it provides knowledge that is critical for improving the safe use of medicines. The safety information on which marketing authorization is granted to medicines is usually limited due to the inherent limitations of clinical trials, such as a highly selected and limited number of trial participants, and incomplete or a lack of information about rare but serious ADRs, drug interactions, and safety in special population groups, such as pregnant women and children. For this reason it is crucial to continue monitoring and collecting information on patients’ experiences after marketing of medicines through post-marketing surveillance activities, including prompt reporting of ADRs.
ADR reports are collected in two major ways—spontaneous reporting and active surveillance. Active surveillance uses methods such as cohort event monitoring (CEM), prescription event monitoring (PEM), registries and data linkages to generate safety data including ADR reports. Spontaneous reporting on the other hand relies on voluntary reporting of ADRs by healthcare providers, marketing authorization holders and patients, and is the bedrock of PV systems [1]. ADRs are estimated to contribute between 4.5 and 6.7% of all patient hospitalizations and/or prolongation of hospital admissions in different countries. They are said to be the fourth to sixth leading cause of death in the USA [2,3,4,5,6]. Notwithstanding evidence of underreporting of ADRs through spontaneous reporting systems [7, 8], reported cases give evidence that ADRs are a significant cause of morbidity and mortality [3, 9, 10].
From inception, spontaneous reporting of ADRs in many countries was traditionally done by healthcare providers, until the early 2000s when a paradigm shift led to direct patient reporting (DPR) of ADRs to relevant bodies. Implementation of the new European Union (EU) PV legislation in 2012 that mandates Member states to encourage DPR of suspected ADRs to the relevant bodies saw more countries adopting DPR of ADRs [11,12,13,14]. By this legislation, patients in the EU have additional avenues to actively participate in their healthcare by directly reporting their experiences with medicines. Patients in many resource-limited settings may not have a similar formal system to directly report adverse reactions from their medications. PV systems in developing countries need to institute similar systems for patients (consumers) to directly report ADRs to relevant bodies.
DPR refers to a system where patients report suspected ADRs directly to relevant bodies without interfacing with a healthcare provider. There is ample evidence that patient reports are as valuable as reports from healthcare professionals and can sometimes help early detection of potential ADR problems and generate signals [15,16,17,18,19,20,21,22]. Furthermore, experience from countries implementing DPR shows that patient reports have qualitative value as patients specify the circumstances in which the reaction occurred and give more detailed descriptions that could help in determining causality. Also, patients tend to report different types of drug reactions from those reported by healthcare providers and provide details of how the reactions impact their lives [15, 16].
A survey of 11 countries implementing DPR revealed three major ways through which patients can report: electronic (web-based), telephone and paper/fax-based reporting. Some countries use a combination of these methods [11]. To support countries willing to implement DPR, the Uppsala Monitoring Centre (UMC) developed a web-based electronic patient reporting tool (eReporting) that allows national centres to capture individual case safety reports (ICSRs) directly from patients into VigiFlow® [23].
There is currently either no formal system for DPR in many African countries participating in international drug safety monitoring or there is no documentation for those that exist. Some authors have studied patients’ perspectives on ADR reporting [24], while others have advocated direct involvement of patients in spontaneous reporting as a positive force for improving reporting of ADRs in developing countries [25, 26]. In Nigeria, patients previously reported suspected ADRs only through their healthcare providers or sources of the medicine [27]. PV systems in resource-constrained settings, especially in Africa, are therefore challenged to establish low-cost, high-impact systems for DPR.
In August 2012, the National Pharmacovigilance Centre (NPC) in Nigeria initiated a programme named Pharmacovigilance Rapid Alert System for Consumer Reporting (PRASCOR), with support from the Global Fund for HIV/AIDS, Tuberculosis and Malaria (GFATM) through the National Malaria Elimination Programme (NMEP). The programme was designed to enhance spontaneous reporting of ADRs by allowing consumers to directly alert the NPC of ADRs suspected to have arisen from use of a medicine. It takes advantage of one of the most readily accessible, widely available and frequently used technological tools—the mobile phone. Recent information puts mobile phone penetration in Nigeria at 94% [28].
1.1 How PRASCOR Works
A consumer who uses a medicine and experiences an untoward or unexpected effect sends a prepaid short text message (SMS) containing the name of the medicine and the reaction to a short code (20543) on any of the four major mobile networks in the country. The message, along with the consumer’s phone number is forwarded as an email alert to a dedicated National Agency for Food and Drug Administration and Control (NAFDAC) webmail account (webmail.nafdac.gov.ng) managed and maintained by staff of the NPC. Simultaneously, the system also sends an automatic acknowledgment to the consumer, informing that the consumer will be contacted for more information. This email alerts the NPC of a potential case of suspected ADR. The service provider maintains a log of all hits to the PRASCOR server.
Although the PRASCOR system was established primarily to collect information on possible ADRs that consumers might experience, it quickly became clear that the service needed to be extended to alerts on all NAFDAC-regulated products and processes. Thus if an alert contained information about any NAFDAC-regulated product or process, it was considered a valid consumer complaint and potentially useful. Upon receipt of an email alert from the PRASCOR service, a staff member in the NPC reviews the email to determine if it is a ‘consumer complaint’, i.e. if it contains information related to any of the seven products (drugs, food, cosmetics, chemicals, detergent, medical devices and packaged water) regulated by NAFDAC. Based on this review, the staff member follows up with a phone call to the consumer to obtain all the information necessary to fill the NPC ADR reporting form, also known as the ‘Yellow form’ (available as electronic supplementary material), which includes patient identifier (name/initials and age), description of ADR, suspect medicine, outcome of reaction, etc. The source of medicine is often provided by or solicited from the consumer and included on the filled ADR form during the follow-up call.
If an alert contains information on a medicine, suspected ADR or both, it is termed a ‘reportable alert’. If sufficient information for a valid report (an identifiable patient, a description of the suspected ADR, a suspected medicine and reporter information) is obtained from the consumer, the reportable alert is converted to an ICSR and entered into the ADR database as a ‘PRASCOR ICSR’. Other non-drug-related consumer complaints are forwarded to relevant divisions for further action.
This work aims to examine the performance of PRASCOR by determining its quantitative contribution to spontaneous reporting of ADRs in Nigeria from inception in August 2012 to February 2017. We assessed consumer complaints and reportable alerts received through PRASCOR to understand how well the system was able to convert alerts from patients to ICSRs to enhance knowledge about medicines and improve health outcomes. Finally, we analysed PRASCOR ICSRs in the local database to characterize patient demographics and know the most reported drug classes, the system organ classes (SOCs) most affected by reported ADRs, the outcome of ADR experiences, and the most common sources of drugs for those reporting through PRASCOR.
2 Methods
2.1 Study Design
This was a retrospective, descriptive, non-interventional study that reviewed all alerts received by the PRASCOR system and suspected ADR reports emanating from the PRASCOR system in the national ADR database.
For this study, the file of all hits logged by the PRASCOR service from inception to February 2017 was obtained in a MicroSoft Excel® file. A three-level data extraction approach was applied to identify and filter alerts that could be relevant for analysis.
2.2 Data Extraction
The PRASCOR log file was cleaned to remove all non-PRASCOR-related messages, such as junk messages and advertisements.
The cleaned log file was reviewed to retain only hits with information on any of the seven NAFDAC-regulated products (drugs, food, cosmetics, chemicals, detergent, medical devices and packaged water), i.e. consumer complaints. Duplicate messages (messages received from the same phone number, on the same date and at about the same time) were eliminated. Messages which appeared to be the same in content but from different phone numbers were treated as different alerts and included in the count.
The second level of extraction involved the review of all consumer complaints to extract all reportable alerts, i.e. alerts containing the name of a medicine, a suspected ADR or both. If an alert contained only the name of a medicine or only information on a suspected ADR, it was included in the count at this stage. All non-drug-related consumer complaints were eliminated.
The third level of data extraction involved review of all reportable alerts to extract alerts containing information on both the suspected medicine and at least one suspected ADR, i.e. ‘medicine–suspected ADR combination’. All alerts with information on only a medicine or the suspected ADR were eliminated. It is believed that alerts with the name of a medicine and description of a suspected ADR are more likely to be converted to ICSRs and will be easier to match with reports in the database.
2.3 NPC ADR Databases
The NPC maintains two different ADR databases for spontaneous reporting: a Microsoft Access®-based ‘local database’ and the VigiFlow® database. The local database contains all suspected ADR reports submitted to the NPC whether or not they contain all the information required for a valid report, i.e. an identifiable patient, description of the suspected ADR, suspected medicine and information on reporter, and whether or not they have been assessed for causality. The local database is administered and managed by staff of the NPC. The VigiFlow® database on the other hand contains only valid ADR reports that have been assessed and assigned a causality assessment grade. This means that ICSRs in the VigiFlow® database contain more complete information than some of the ICSRs in the local database. For this study, the local database was used to extract ICSR data for further analysis.
Potentially, all reportable alerts can be converted to ICSRs, as they ought to trigger a call from the NPC to obtain more information from the consumer to fill an ADR form. Hence, a systematic search of the NPC local database using the unique code assigned to each ICSR in the database was undertaken to extract all ICSRs emanating from the PRASCOR service (PRASCOR ICSRs). Each report received by the NPC is assigned a unique code before it is entered into the local database. Information contained in the code include the date and year it was received and the reporting institution, among other things. In the case of reports obtained from PRASCOR, the reporting institution is indicated as PRASCOR. Hence, all ICSRs emanating from PRASCOR in the local database were extracted into a Microsoft Excel® sheet to determine the extent to which ‘PRASCOR alerts’ were converted to ICSRs.
2.4 Data Analysis
Data extraction, handling and counting were done using Microsoft Excel®. All PRASCOR ICSRs were manually checked against the reportable alerts with information on medicine–suspected ADR combination using the name of the medicine, the reaction(s) and the year the report was received to determine the level to which alerts from PRASCOR were converted to ICSRs.
In addition, all PRASCOR ICSRs from the local database were exported to IBM SPSS® statistics software, version 20, and analysed using descriptive statistics to characterize them by patient demographics (age and sex), most frequently reported medicines and ADRs, the SOC most affected, the outcome of ADRs, and sources of medicines. The most reported medicines and ADRs were analysed using proxy indicators, such as the class of medicines and the SOC.
3 Results
From August 2012 to February 2017, a total of 47,071 hits were logged by the PRASCOR server. After removing blank text messages, 41,585 hits were retained. Further cleaning of the hits to remove junk messages, advertisements, goodwill/political messages, requests for employment and confirmation of NAFDAC product registration number, and other irrelevant messages, 3836 consumer complaints, i.e. alerts with information on at least one NAFDAC-regulated product, were identified. Removal of duplicate alerts led to 3594 consumer complaints (including 138 messages with similar contents, but sent from different phone numbers) being retained for analysis.
3.1 Reportable Alerts from PRASCOR
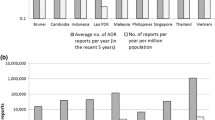
A total of 3379 consumer complaints (94%) were reportable alerts, i.e. alerts containing either the name of a medicine, a suspected ADR or both. Fifty-two per cent of reportable alerts (n = 1758) contained information on both a medicine and at least one suspected ADR, i.e. medicine–suspected ADR combination. The annual distribution of consumer complaints and reportable alerts based on information contained is shown in Figs. 1 and 2.
3.2 PRASCOR ICSRs in NPC Local Database
The local database contained a total of 22,370 ICSRs submitted to the NPC from September 2004 to February 2017. Between August 2012 and February 2017, the number of ICSRs submitted to the local database was 9133. ICSRs attributed to PRASCOR were 353. Thus within the period under review, PRASCOR quantitatively contributed 3.9% of spontaneous reports in the local database. Its overall contribution to total reports in the local database was 1.6%. The 353 PRASCOR ICSRs in the local database give a conversion rate of 10.4% when compared against the 3379 reportable alerts identified from PRASCOR.
Seventy per cent of the 353 PRASCOR ICSRs (n = 247) were successfully matched to a reportable alert with information on medicine–suspected ADR combination. No match was found for 30% (n = 106). Table 1 gives the annual break down of reportable alerts and the number of PRASCOR ICSRs in the local database successfully matched to an originating reportable alert with information on medicine–suspected ADR combination. On average, about 14% of PRASCOR ICSRs in the local database were successfully matched to an originating reportable alert with information on both medicine and suspected ADR combination.
3.3 Characterization of PRASCOR ICSRs
3.3.1 Patient Demographics
Although only 247 PRASCOR ICSRs were successfully matched to reportable alerts with information on medicine–ADR combination, analysis to characterize PRASCOR ICSRs was done on all 353 reports tagged as PRASCOR reports in the local database.
Fifty-five percent (n = 195) of patients were male, while 43% (n = 153) were female. Gender was not recorded for 2% of patients (n = 5).
Patients were categorized into three broad age categories: 1–5 years, 6–17 years and 18 years and above. This categorization was used because a sizeable number of reports (n = 123, 35%) recorded ‘adult’ as the age of the patient. All reports with age as ‘adult’ were categorized as 18 years and above. The median age of patients was 18 years, with an interquartile range of 10. The highest number of reports (n = 271, 77%) were from patients 18 years and above, while the lowest number of reports (n = 23, 7%) were from those 6–17 years of age. Age was not recorded for 30 patients.
3.3.2 Pharmacological Drug Classification
A total of 96 different medicines involving 25 pharmacological drug classes were reported (Table 2). Antimalarials (n = 111, 31.4%) were the most reported drug class followed by antibiotics (n = 83, 23.5%), analgesics (n = 50, 14.2%) and anti-retrovirals (ARVs) (n = 14, 4.0%).
3.3.3 Source of Medicine
A total of 255 reports (72%) had information on source of the suspected medicine. Forty-two percent (n = 149) were from community pharmacies, while 26% (n = 90) were from hospital pharmacies (Table 3). No information was provided for 28% (n = 98) of reports.
3.3.4 SOC affected by Reaction
A total of 145 distinct ADRs involving 14 SOCs were reported. General disorders (n = 128, 36%) were the most affected SOC, followed by skin and subcutaneous tissue disorder (n = 121, 34%) (Table 4).
3.3.5 Outcome of Reaction
Two hundred and twenty-seven (64%) reports had information on outcome of the reaction. One hundred and eighty-five (82%) of these reported the ADRs as resolved completely. Two cases (0.9%) reported death and two reported life-threatening conditions, respectively, as the outcome of the reactions (Table 5).
4 Discussion
We found that PRASCOR quantitatively contributed 3.9% of spontaneous reports in the NPC local database during the period under review, indicating a willingness of consumers in Nigeria to use PRASCOR to share their drug-related concerns with NAFDAC. This is buttressed by the 94% of consumer complaints that were drug related.
A review of the methods used for DPR in other countries showed that patients could report their ADRs directly either electronically, by telephone/fax and/or via post, without human interface [11, 12]. This ensures that every ADR experience shared by patients is captured as an ICSR. The Nigerian DPR system on the other hand is a two-phased system: a short text message (alert) is sent first, which is then followed by a phone call from PV staff to convert alerts to ICSRs. No system was similar to this short code alert system used in Nigeria, making comparison with other systems difficult. However, with the Nigerian system, there is the danger of some alerts not being converted to ICSRs, as seen in the 10.4% conversion rate from reportable alerts to PRASCOR ICSRs in this study. This represents missed opportunities to convert consumer experiences to data that could inform regulatory decisions and improve the outcome of use of medicines for consumers. Given the potential role of electronic health systems in signal detection [29, 30], it will be worthwhile for NAFDAC to consider transiting to electronic reporting for patients without the need for human interface. This has the potential of increasing the quantity and quality of patient reports from spontaneous reporting. Many studies have already documented the qualitative value of direct patient reports [15, 17, 18, 20, 22, 31]. The proposed electronic system may be in the form of a web-based application, as used by several countries [11, 12], or a mobile application that patients can use to directly send reports from their smartphones, given the penetration of smartphones, in Africa and Nigeria in particular [28, 32, 33].
A review of available records and discussions with PV staff revealed numerous factors responsible for the low conversion of reportable alerts to ICSRs. These are broadly grouped into three categories: connectivity (mobile network) issues and consumer- and PV staff-related factors. Poor network connectivity that made it difficult to reach consumers accounted for about 85% of PV staff members’ inability to convert alerts to ICSRs. After several attempts to reach a consumer with no success, staff usually move on to other tasks, leading eventually to the alert being lost to follow-up. A consumer-related factor included consumers not picking up follow up calls. There are also instances when consumers have denied sending any message to NAFDAC. Given the large percentage of females (40%) and males (30%) with no formal education in Nigeria [34], it is possible that some consumers could not comprehend what was said by the PV staff during follow-up calls. This is supported by an observed poor grammar and spelling of words seen in some of the messages, suggesting a low level of education of senders of such alerts. This underscores the need to continuously train PV staff on effective communication. A PV staff-related factor was the time lag between receiving a consumer alert and placing a follow-up call. Considerable time lag between the two activities, perhaps due to the pressure of work or other factors, makes it more likely for a consumer to forget that she/he sent a message and the details of the reaction when eventually contacted. A substantial number of reportable alerts could be converted to ICSRs with diligent follow-up.
Thirty per cent of PRASCOR ICSRs were not successfully matched to a reportable alert with information on medicine–suspected ADR combination. An explanation for this is that PV staff are required to follow-up all reportable alerts, i.e. all alerts with information on either the medicine or the ADR or both. The data extraction process for this study, however, eliminated alerts with information on only the medicine or the ADR, since it would have been very difficult to accurately match such alerts to any PRASCOR ICSR, as PRASCOR ICSRs do not have information on the date and time of receipt of the alert to facilitate reliable matching. A well designed electronic reporting application with mandatory fields will eliminate this challenge of converting reportable alerts to ICSRs.
4.1 Characterization of ICSRs
Looking at the characteristics of the PRASCOR ICSRs, we found a slightly higher reporting rate among males (55%) than females. This is in line with the reported higher mobile phone ownership among men (87.8%) than women in Nigeria [35], which makes it easier for men to access and use the service.
Similarly, the highest number of reports came from patients in the 18 years and above age category. This is expected for two reasons. First, 35% of patients recorded their age as ‘adult’, leading to the placement of a large number of patients in the age category ‘18 years and above’, which may have skewed the result. Second, consumers in this age category are also more likely to own and use mobile phones compared to those in the other age categorizations used in this study [35].
4.2 Classes and Sources of Reported Medicines
Antimalarials were the highest reported medicines, followed by antibiotics and analgesics. Nigeria has a 45% rapid diagnostic test (RDT) prevalence of malaria, which is responsible for 60% of annual outpatient visits [36]. Furthermore, antimalarial medicines are classified as over-the-counter drugs and are therefore widely available and readily accessible [37].
A community pharmacy was the most frequently reported source of medicines. This is expected given the over-the-counter status of the most frequently implicated drug class (antimalarials) in the study and the well documented fact that many patients first seek care for illnesses, particularly malaria, from the private sector [30, 38, 39]. An unexpected finding, however, was the low number of consumers that indicated sourcing their medicines from patent and proprietary medicine vendor (PPMV) shops, given the high proliferation of these shops across the country [39,40,41]. A possible explanation may be found in the terminology used by consumers to describe medicine stores. ‘Pharmacy’ and ‘chemist’ are used interchangeably by some consumers to describe both a community pharmacy and a PPMV store.
Antibiotics were the second most frequently reported drug class. Several studies have documented evidence of extensive self-medication, misuse and unregulated access to antibiotics by patients in Nigeria [42,43,44,45,46,47].
4.3 SOCs Affected by ADRs and Outcomes of Reactions
General disorders and administrative site disorders (36%) and skin and subcutaneous tissue disorders (34%) were the SOCs most frequently involved in the ADRs reported by patients. Skin and appendage disorders are some of the most frequently involved SOC in other studies [48,49,50]. Since consumers may not be able to objectively and scientifically describe their ADRs, the high number of ADRs classified as general disorders is not unexpected. Similarly, skin disorders are very hard to miss and easy to describe, making it possible for patients to clearly report on their skin-related issues.
Eighty-two per cent of patients with information on outcome of their reaction recovered fully. This is considered a positive outcome that could be used to reassure patients of the possibility of complete recovery after their ADR experience. Two cases each of death and life-threatening outcomes were reported, but not followed up, as this was outside of the scope of this study.
4.4 Limitations
The generalizability of findings from this study is limited by several factors, including PRASCOR alerts containing similar or the same messages but originating from different phone numbers being treated as separate messages, with the consequence of a higher number of alerts and a lower conversion rate. Another issue was that reportable alerts with information on only the medicine or suspected ADR are usually followed up by PV staff, but in this study, such alerts were not used for matching of PRASCOR ICSRs, with a consequence of under-matching of PRASCOR ICSRs to originating alerts. Furthermore, at the commencement of the PRASCOR service in 2012, converted ICSRs were not explicitly coded as emanating from the PRASCOR service, thus leading to under-estimation of the contribution of the PRASCOR service to ICSRs in the database. Finally, this study did not look at the cost of the PRASCOR service, and therefore could not make deductions about the cost effectiveness of PRASCOR in the Nigerian PV system. This might be an interesting area for future studies to guide countries looking to implement a similar system.
5 Conclusions
Reviewing the PRASCOR system showed that patients are willing to share their medicine-related experiences with NAFDAC. For the review period, the PRASCOR system quantitatively contributed 3.9% of reports in the NPC local database. Although low, this initial result is encouraging. Given the potential benefits that direct patient reports can contribute both quantitatively and qualitatively to increasing our understanding of drug safety issues, the system needs to be improved. Training and retraining of PV staff on prompt and effective communication will help to improve data collection and should be a short-term goal for the system. Migrating to electronic reporting that allows direct capture of patient reports without human interface should be considered a long-term plan for harnessing the full potential of PRASCOR as a DPR tool, improving its contribution to spontaneous reporting and sustaining the system. We conclude that patient reporting of ADRs in Nigeria using PRASCOR has contributed quantitatively to ADR reporting and has potential for adding greater value to PV in Nigeria if properly harnessed.
References
Pal S, Dodoo A, Mantel A, Olsson S. The world medicines situation 2011. Pharmacovigilance and safety of medicines. Geneva: WHO; 2011.
Davies EC, Green CF, Taylor S, Williamson PR, Mottram DR, et al. Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. https://doi.org/10.1371/journal.pone.0004439.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients. A meta analysis of prospective studies. JAMA. 1998;279:1200–5.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329:15–9.
Tumwikirize WA, Ogwal-Okeng JW, Vernby A, Anokbonggo WW, Gustafsson LL, Lundborg SC. Adverse drug reactions in patients admitted on internal medicine wards in a district and regional hospital in Uganda. Afr Health Sci. 2011;11(1):72–7.
Mehta UC. Pharmacovigilance: the devastating consequences of not thinking about adverse drug reactions. CME. 2011;29(6). http://www.ajol.info/index.php/cme/article/view/72000. Accessed 28 Nov 2012.
Hazell L, Shakir SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29(5):385–96 (abstract).
Alvarez-Requejo A, Carvajal A, Bégaud B, Moride Y, Vega T, Arias LH. Under-reporting of adverse drug reactions. Estimate based on a spontaneous reporting scheme and a sentinel system. Eur J Clin Pharmacol. 1998;54(6):483–8 (abstract).
Wiffen P, Gill M, Edwards J, Moore A. Adverse drug reactions in hospital patients: a systematic review of the prospective and retrospective studies. Bandolier Extra June 2002 from http://www.ebandolier.om. Accessed 28 Nov 2012.
Wu C, Bell CM, Wodchis WP. Incidence and economic burden of adverse drug reactions among elderly patients in Ontario emergency departments: a retrospective study. Drug Saf. 2012;35(9):769–81.
van Hunsel F, Harmark L, Pal S, Olsson S, van Grootheest K. Experiences with adverse drug reaction reporting by patients: an 11-country survey. Drug Saf. 2012;35(1):45–60.
Herxheimer A, Crombag R, Alves TL. Direct patient reporting of adverse drug reactions: a fifteen-country survey and literature review [online]. Health Action International (Europe) Amsterdam, Netherlands. 2010. https://consumers.cochrane.org/ Accessed 5 May 2017.
World Health Organization. Safety monitoring of medical products: reporting system for the general public. Switzerland: WHO; 2012.
Ancel.la Santos. Direct Patient reporting in the European Union. A snapshot of reporting systems in seven member states. Health Action International, Amsterdam, The Netherlands. http://www.apps.who.int/medicinedocs/en/d/Js22088en/. Accessed 8 May 2017.
Avery AJ, Anderson C, Bond CM, Fortnum H, Gifford A, Hannaford PC, et al. Evaluation of patient reporting of adverse drug reactions to the UK ‘Yellow Card Scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess. 2011;15(20):1–234, iii–iv. https://doi.org/10.3310/hta15200.
Egberts TCG, Smulders M, de Koning FHP, Meyboom RHB, Leuflens HGM. Can adverse drug reactions be detected earlier? A comparison of reports by patients and professionals. BMJ. 1996;313:530–1.
Farcas AM, Farah C, Bojita MT. Patients reporting of suspected adverse reactions to antidepressants. A pilot methodological study. Farmacia. 2010;58(3):255–63.
Vihelmsson A, Svensson T, Meeuwisse A, Carlsten A. What can we learn from consumer reports on psychiatric adverse reports to a consumer association. BMC Clin Pharmacol. 2011;11:16. http://www.biomedcentral.com/1472-6904/11/16.
van Hunsel F, van der Well C, Passier A, van Puijenbroek E, van Grootheest K. Motives for reporting adverse drug reactions by patients in The Netherlands. Eur J Clin Pharmacol. 2010. https://doi.org/10.1007/s00228-010-0865-7.
de Langen J, van Hunsel F, Passier A, de Jong-van den Berg L, van Grootheest K. Adverse drug reaction reporting by patients in The Netherlands: three years of experience. Drug saf. 2008;31(6):515–24.
Durrieu G, Palmaro A, Pourcel L, Caillet C, Faucher A, Jacquet A, et al. First French experience of ADR reporting by patients after a mass immunization campaign with influenza A (H1N1) pandemic vaccination. A comparison of reports by patients and healthcare professionals. Drug Saf. 2012;35(10):845–54.
Gawert L, Hierse F, Zink A, Strangfeld A. How well do patient reports reflect adverse drug reactions reported by rheumatologists? Agreement of physician-and patient—reported adverse events in patients with rheumatoid arthritis observed in the German biologics register. Rheumatol Adv Access. 2010. https://doi.org/10.1093/rheumatology/keq300. http://rheumatology.oxfordjournals.org Accessed 22 Nov 2012.
eReporting. A new module for VigiFlow (2014). https://www.who-umc.org/media/1207/e-reporting-vigiflow.pdf. Accessed 4 April 2017.
Sabblah GT, Darko DM, Mogtari H, et al. Drug Saf. 2017;40:911. https://doi.org/10.1007/s40264-017-0563-9 (abstract).
Kiguba R, Karamagi C, Waako P, Ndagije HB, Bird SM. Recognition and reporting of suspected adverse drug reactions by surveyed healthcare professionals in Uganda: key determinants. BMJ Open. 2014;4(11):e005869. https://doi.org/10.1136/bmjopen-2014-005869.
Balogun SH, Adeleye OA. Patient reporting practices of suspected adverse drug reactions to antiretroviral drugs in a tertiary health facility in Nigeria. Niger Postgrad Med J. 2014;21(4):331–7 (abstract).
Federal Ministry of Health. Nigerian National Pharmacovigilance Policy and Implementation Framework. Abuja: Federal Ministry of Health; 2012. ISBN: 978-978-931-754-7. http://nafdac.gov.ng/images/Nigerian_National_Pharmacovigilance_Policy_and_Implementation_February_2012_Abuja.pdf.
Adeyemi Adepetun. Smart phone penetration hits 30% in Nigeria. The Guardian Business. 2016. https://guardian.ng/business-services/smartphone-penetration-hits-30-in-nigeria/. Accessed 13 May 2017.
Cederholm S, Hill G, Asiimwe A, Bate A, Bhayat F, Persson Brobert G, et al. Structured assessment for prospective identification of safety signals in electronic medical records: evaluation in the health improvement network. Drug Saf. 2015;38(1):87–100. https://doi.org/10.1007/s40264-014-0251-y.
Suku CK, Hill G, Sabblah G, Darko M, Muthuri G, Abwao E, Pandit J, Osakwe AI, Elagbaje C, Nyambayo P, Khoza S, Dodoo AN, Pal SN. Experiences and lessons from implementing cohort event monitoring programmes for antimalarials in four African countries: results of a questionnaire-based survey. Drug Saf. 2015. https://doi.org/10.1007/s40264-015-0331-7.
Mohammed AA, Mohamed IMI, Subish P, Mohamed AAH. Importance of consumer reporting of adverse drug reactions in malaysia. Discipline of social and administrative pharmacy. Gelugor: School of Pharmaceutical Sciences, Universiti Sains Malaysia; 2010. ISBN 978-967-394019-6.
Bahk CY, Goshgarian M, Donahue K, Freifeld CC, Menone CM, Pierce CE, Rodriguez H, Brownstein JS, Furberg R, Dasgupta N. Increasing patient engagement in pharmacovigilance through online community outreach and mobile reporting applications: an analysis of adverse event reporting for the Essure device in the US. Pharm Med. 2015;29(6):331–40.
de Vries ST, Wong L, Sutcliffe A, Houÿez F, Ruiz CL, Mol PGM. Factors influencing the use of a mobile app for reporting adverse drug reactions and receiving safety information: a qualitative study. Drug Saf. 2017;40:443–55. https://doi.org/10.1007/s40264-016-0494-x.
National Population Commission (NPC) [Nigeria] and ICF International. Nigeria Demographic and Health Survey 2013. Abuja: NPC and ICF International; 2014.
Broadcasting Board of Governors. Contemporary media use in Nigeria. https://www.bbg.gov/wp-content/media/2014/05/Nigeria-research-brief.pdf Accessed 8 Jan 2018.
National Malaria Elimination Programme (NMEP), National Population Commission (NPopC), National Bureau of Statistics (NBS), and ICF International. Nigeria Malaria Indicator Survey 2015. Abuja: NMEP, NPopC, and ICF International; 2016.
Bassi PU, Osakwe AI, Suku C, Kalat M, Elagbaje C, Isah A, et al. Cohort event monitoring of patients treated for uncomplicated malaria with artemisinin-based combination therapies in selected hospitals and community pharmacies in Nigeria. Niger Postgrad Med J. 2016;23:172–81.
Roll Back Malaria. Community involvement in rolling back malaria. WHO/CDS/RBM/2002.42. Geneva: World Health Organization; 2002.
Beyeler N, Liu J, Sieverding M. A systematic review of the role of proprietary and patent medicine vendors in healthcare provision in Nigeria. PLoS One. 2015;10(1):e0117165. https://doi.org/10.1371/journal.pone.0117165.
Prach LM, Treleaven E, Isiguzo C, Liu J. Care-seeking at patent and proprietary medicine vendors in Nigeria. BMC Health Serv Res. 2015. https://doi.org/10.1186/s12913-015-0895-z.
Liu J, Prach LM, Treleaven E, Hansen M, Anyanti J, Jagha T, Seaman V, Ajumobi O, Isiguzo C. The role of drug vendors in improving basic health-care services in Nigeria. Bull World Health Organ. 2016;94:267–75. https://doi.org/10.2471/BLT.15.154666.
Eshiet UI, Essien EG, Effiong GS, Ekwueme C. Self-medication with antibiotics amongst civil servants in Uyo, Southern Nigeria. J Adv Med Pharm Sci. 2015;2(3):89–97 (article no.JAMPS.2015.012).
Sanya TE, Titilayo OF, Adisa R, Segun JS. Use of antibiotics among non-medical students in a Nigerian university. Afr Health Sci. 2013;13(4):1149–55. https://doi.org/10.4314/ahs.v13i4.41.
Akinyandenu O, Adeniyi A. Irrational use and non-prescription sale of antibiotics in Nigeria: a need for change. J Sci Innov Res. 2014;3(2):251–7.
Igbeneghu OA. Knowledge and practices in the use of antibiotics among a group of Nigerian university students. Int J Infect Control. 2013;v9:i1. https://doi.org/10.3396/ijic.v9i1.007.13.
Yah SC, Yusuf OE, Eghafona NO. Pattern of antibiotic usage by adult populations in the city of Benin, Nigeria. Sci Res Essays. 2008;3(3):081–5.
Auta A, Banwat SB, David S, Dangiwa DA, Ogbole E, Tor-anyiin AJ. Antibiotic use in some Nigerian communities: knowledge and attitudes of consumers. Trop J Pharm Res. 2013;12(6):1087–92.
Oreagba IA, Oshikoya KA, Ogar C, Adefurin AO, Ibrahim A, Awodele O, Oni Y. Adverse reactions to fluoroquinolones in the Nigerian population: an audit of the reports submitted to the National Pharmacovigilance Centre from 2004 to 2016. Pharma Res Per. 2017;5(2):e00297. https://doi.org/10.1002/prp2.297.
Prajapati K, Desai M, Shah S, Panchal J, Kapadia J, Dikshit R. An analysis of serious adverse drug reactions at a tertiary care teaching hospital. Perspect Clin Res. 2016;7(4):181–6.
Jose J, Rao PG. Pattern of adverse drug reactions notified by spontaneous reporting in an Indian tertiary care teaching hospital. Pharmacol Res. 2006;54(3):226–33.
Acknowledgements
We appreciate the support of the National Malaria Elimination Programme, principal recipient to the Global Fund for AIDS, Tuberculosis and Malaria (GFATM), through which the funds for establishing the PRASCOR service was made available to NAFDAC as a sub-recipient in 2012. We also thank GFATM, whose continued funding of NAFDAC ensures that consumers continue to have a voice in their healthcare. We acknowledge Mr. Anthony Obieze, whose creative thinking coined the acronym PRASCOR, and finally, our thanks goes to all PV staff, including past and present interns and corp members, who go the extra mile to follow-up all reportable alerts with a call.
Author information
Authors and Affiliations
Contributions
CKO conceived the work, analysed the data and drafted the manuscript. CKO, AAKA and KA extracted and cleaned the data. AIO, AI, FJ, AAKA, KA and YO reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Comfort Ogar, Ali Ibrahim, Adeline Osakwe, Fatima Jajere, Ashega Kigbu-Adekunle, Kemi Alonge and Yetunde Oni have no conflicts of interest that are directly related to this review work and the content of this study.
Funding
No funding was received for conducting this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogar, C.K., Ibrahim, A., Osakwe, A.I. et al. Pharmacovigilance Rapid Alert System for Consumer Reporting (PRASCOR): A Look at Its Quantitative Contribution to Spontaneous Reporting in Nigeria from August 2012 to February 2017. Pharm Med 32, 131–141 (2018). https://doi.org/10.1007/s40290-018-0228-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-018-0228-8