Abstract
Background
Regulation of postprandial hyperglycemia is a major concern for individuals with type 2 diabetes. Exercise can reduce postprandial hyperglycemia by increasing contraction-mediated glucose uptake. However, there is no consensus with which to develop guidelines for optimal postprandial exercise timing and prescription.
Objective
The current systematic review was conducted to consolidate the literature surrounding the effects of postprandial exercise on glucose regulation in individuals with type 2 diabetes.
Methods
Electronic databases were searched on 17 February 2017. Inclusion criteria were: (1) trial was a randomized crossover trial; (2) subjects were diagnosed with type 2 diabetes; (3) a standardized meal was given; (4) exercise was initiated within three hours of the meal; (5) subjects were not treated with insulin.
Results
Twelve studies met the inclusion criteria, involving 135 participants (108 males, 20 females, seven unknown). The included studies varied greatly in their timing, duration, intensity, modality, and glucose measures. Postprandial aerobic exercise (11 studies) decreased short-term glucose area under the curve by 3.4–26.6% and 24-h prevalence of hyperglycemia by 11.9–65%. Resistance exercise (two studies) decreased the short-term glucose area under the curve by 30% and 24-h prevalence of hyperglycemia by 35%.
Conclusion
Postprandial exercise may be an effective way to improve glucose control in individuals with type 2 diabetes. The most consistent benefits were seen in long-duration (≥ 45 min), moderate-intensity aerobic exercise. Resistance training also appears to be an effective modality. We recommend that individuals with type 2 diabetes focus on increasing energy expenditure after the largest meal of the day. More research is needed in this area to confirm the results of this systematic review and to provide clinicians with specific exercise recommendations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Postprandial exercise appears to effectively improve glucose control in individuals with type 2 diabetes. |
The most consistent benefits were seen with long-duration, moderate-intensity, aerobic exercise. |
Future studies should examine resistance training, which may be particularly effective in this population, as well as match for energy expenditure in their study design. |
1 Introduction
For patients with type 2 diabetes (T2D), a condition that has reached pandemic proportions, a primary focus of treatment is the reduction in hyperglycemia. Prevention of hyperglycemia is particularly important following a meal, when glucose concentrations are highest. For example, elevated blood glucose 2 h after lunch increases the risk for cardiovascular events by 50% and the risk for mortality by 89% [1]. One potentially promising and safe strategy for reducing postprandial (i.e., following a meal) hyperglycemia is repeated muscle contractions through exercise [2].
Although individuals with T2D have impaired insulin sensitivity, muscular contraction-mediated glucose uptake provides a means for glucose to exit the bloodstream and enter the muscle tissue independent of insulin [3]. Exercise can be used to induce post-prandial contraction-mediated glucose uptake. Unfortunately, the optimal timing and prescription of postprandial exercise to maximally reduce postprandial hyperglycemia have not been clearly elucidated [4]. The purpose of this systematic review was to consolidate the literature surrounding the effects of postprandial exercise on glucose regulation in individuals with T2D.
2 Methods
This systematic review was carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [5].
2.1 Searches
Electronic databases (PubMed, Google Scholar) were searched on 15 February 2017 using the keywords: type 2 diabetes, exercise, postprandial or meal, and glycemic or glycaemic or glucose. The reference lists of all identified trials and relevant reviews were also examined.
2.2 Selection Criteria
Two authors (AB, GZ) initially screened each article based on the title and abstract. Full versions of potentially eligible articles were then obtained for review. The following inclusion criteria were used: (1) trial was a randomized crossover trial; (2) subjects were diagnosed with type 2 diabetes; (3) a standardized meal was given; (4) exercise was initiated within 3 h of a meal; (5) the subjects were not treated with insulin. Articles were not limited by exercise intensity or modality. Studies were excluded if subjects had co-morbid cardiovascular disease.
2.3 Data Synthesis
The characteristics and design of each study were entered into a spreadsheet along with the outcome measures and findings. The studies were separated into aerobic exercise and resistance exercise interventions. Percent changes (%∆) between non-exercise controls and exercise conditions were calculated in order to make meaningful comparisons between studies.
Study quality was assessed on a percentage rating scale using a modified version of the Jadad scale, shown in Electronic Supplementary Material Table S1 [6]. The percentage was calculated by dividing the number of “yes” scores by the total number of applicable items. This modified version was more appropriate than the original Jadad scale due to the nature of randomized crossover exercise interventions. In addition to items from the Jadad scale, four items from the PEDro scale and three from the Delphi List were included, as well as three recommendations from the CONSORT statement [7,8,9]. Lastly, it must be noted that while the current scoring system has not been thoroughly evaluated or validated, it has been used by a previous exercise-based systematic review [10].
3 Results
3.1 Article Selection
A total of 382 potentially eligible articles were identified through electronic databases, and an additional 12 articles were identified through manual searches of reference lists. Of the 394 total articles, 360 were excluded after title and abstract screening. Subsequently, 34 full-text articles were acquired and assessed for eligibility, of which 22 did not meet the inclusion criteria. Figure 1 depicts the article selection process along with reasoning for the excluded trials.
3.2 Characteristics of Included Studies
Included study characteristics are summarized in Table 1. The number of participants in each trial ranged from seven to 20. Seven studies included only males [11,12,13,14,15,16, 22] and five studies included males and females [17,18,19,20,21]. One study reported lean participants [19], one study reported obese participants [21], five studies reported sedentary participants [13, 14, 18, 20, 22], two studies reported obese and sedentary participants [11, 12], and three studies did not use these subject characterizations [15, 17]. In eight of the trials, participants continued their normal medications [11, 15,16,17,18,19,20,21], in three studies, no medications were taken on testing days, and in one study medication use was not mentioned [12]. Six studies took place in Europe [11,12,13, 15, 16, 22], four in North America [14, 17, 18, 21], and two in Japan [19, 20].
The timing of exercise following the meal and specific outcome measures varied among the studies, making consolidation of the findings difficult. The timing of exercise initiation ranged from immediately after to 2.5 h after the meal. The most common outcome measures included postprandial glucose concentration [14, 17,18,19,20, 22], 3- or 4-h glucose area under the curve (AUC) [11, 12, 17,18,19, 21], 24-h average glucose concentration [11, 16, 18, 22], and 24-h prevalence of hyperglycemia [15, 16, 22]. Five studies utilized continuous glucose monitoring [11, 15, 16, 18, 22] for their measures and nine used blood draws [12,13,14, 16, 17, 19,20,21, 23].
3.2.1 Study Quality Assessment
The quality of the studies ranged from 38 to 58%, with the average being 49% (Table 1). Higher quality scores were not attained due to the majority of studies not reporting: (1) methods of intervention randomization, (2) a justification of sample size, (3) details regarding reasons for subject dropout, and (4) the reproducibility of primary outcome measurements.
3.2.2 Exercise Interventions
Table 1 outlines the exercise interventions in the included trials. Seven trials assessed the effects of moderate-intensity aerobic exercise [11, 12, 14,15,16,17, 23], five trials used high-intensity aerobic exercise [13, 18,19,20, 22], six trials used intermittent aerobic exercise bouts [11, 13, 15, 18,19,20], and two trials utilized resistance training [16, 21]. Intensity of the exercise bouts ranged from 35% of maximum workload to 90% of maximum heart rate. The length of the individual intermittent aerobic exercise bouts ranged from 1 to 15 min. The total duration of intermittent bouts ranged from 6 to 45 min. Continuous aerobic exercise bouts ranged from 20 to 60 min. One of the studies using resistance training had a duration of 45 min, while the other study noted that three sets of ten repetitions were performed, but did not specify an exact duration. For aerobic exercise modality, four studies used walking [11, 15, 17, 20], seven studies used cycling [12,13,14,15,16, 18, 22], and two studies used stair climbing [19, 20].
3.2.3 Effects of Exercise on Glucose Measures
The findings are summarized in Table 1. Tables 2 and 3 show the percent changes in glucose measures based on intensity and timing of exercise initiation, respectively. Table 4 compares the percent changes for high-intensity interval training (HIIT) and continuous aerobic exercise.
3.2.4 Timing of Exercise Initiation
In the one study that compared a split pre- and post-lunch exercise session to continuous postprandial exercise, similar effects were seen for 24-h prevalence of hyperglycemia, (control: 131.3 ± 20.7 mg/dl; split: 128.2 ± 28.5 mg/dl; continuous: 129.8 ± 17.2 mg/dl), which is arguably the most important measure [11]. However, in the two studies directly comparing pre- and postprandial exercise, postprandial had a greater glucoregulatory effect. In one of the studies, 20 min of walking after dinner decreased blood glucose immediately following exercise and the 3-h AUC, whereas walking before dinner non-significantly increased blood glucose (immediate glucose concentration: control: 7.8 ± 0.7 mmol/L; post: 6.1 ± 0.4 mmol/L; pre: 8.8 ± 1.0 mmol/L; 3-h AUC: control: 11.7 ± 2.0 mmol/L; post: 11.3 ± 3.7 mmol/L; pre: 13.7 ± 2.2 mmol/L) [17]. In the final study comparing pre- and post-prandial exercise, pre-prandial resistance training resulted in an 18% decrease in 4-h AUC, whereas postprandial resistance training resulted in a 30% decrease in the same measure (absolute values not reported) [21]. Although pre-prandial did show glucoregulatory effects, postprandial exercise seemed to be more consistently effective at mitigating hyperglycemia.
3.2.5 Modality
All aerobic exercise modalities, including walking, cycling, and stair climbing/descending seemed to be effective at reducing hyperglycemia [11,12,13,14,15,16,17,18,19,20]. One study directly compared resistance training to aerobic exercise and found comparable beneficial effects on the 24-h prevalence of hyperglycemia [16]. There are only two studies that examined the effects of resistance training on glycemic control in individuals with T2D, and the results suggest that resistance training may also be an effective modality [16, 21]. However, more studies are needed to confirm or refute this possibility. Postprandial resistance training was found to be more effective than pre-prandial resistance training, though both bouts significantly reduced glucose concentrations. Table 2 shows glucose changes among studies using resistance training compared to aerobic exercise at various intensities.
3.2.6 Intensity
Overall, continuous moderate-intensity aerobic exercise was the most common type of intervention. Postprandial moderate-intensity exercise had a greater glucoregulatory effect than non-exercise controls [11, 12, 15, 16, 23]. A bout as simple as 20 min of self-paced walking induced a 21.8% reduction in blood glucose (exercise: 6.1, control: 7.8–6.1 mmol/L) immediately following exercise compared to a non-exercise control [17].
High-intensity exercise was also found to be effective for reducing postprandial glucose concentrations [18,19,20, 22]. High intensity exercise as short as 3 min demonstrated a beneficial effect [19]. One study directly compared high-intensity to low-intensity exercise, and the low-intensity bout had a greater effect on reducing the prevalence of hyperglycemia throughout the 24-h period following the meal [22]. However, another study showed that moderate-intensity exercise was more beneficial than low-intensity activities of daily living (ADLs) [15]. These results suggest that moderate may be the most consistently effective intensity to reduce hyperglycemia in individuals with T2D.
4 Discussion
The purpose of this systematic review was to investigate the literature surrounding the effects of exercise following a meal on glucose regulation in individuals with T2D. Arguably, the most clinically meaningful measurement of glucose control is the prevalence of hyperglycemia throughout the day, as this directly relates to further disease progression, cardiovascular risk, and mortality [24, 25]. While not all studies measured prevalence of hyperglycemia, the available evidence indicates that engagement in any mode and intensity of exercise appears to reduce postprandial hyperglycemia. On average, low-intensity aerobic, moderate-intensity aerobic, high-intensity aerobic, and resistance training reduced the 12- to 24-h prevalence of hyperglycemia by 30.8, 33.5, 41.8, and 35%, respectively [15, 16, 18, 22].
Although any mode and intensity of exercise seems to have a beneficial effect on hyperglycemia, increased energy expenditure seems to be the driving factor behind exercise-induced decreases in hyperglycemia in individuals with T2D. We suggest that continuous moderate-intensity aerobic exercise, regardless of modality and beginning approximately 1 h after a meal is a safe, realistic, and effective strategy to decrease blood glucose and increase energy expenditure. The following sections elaborate on prescription recommendations for the timing, modality, and intensity of exercise.
4.1 Timing
Postprandial exercise appears to be a more effective exercise strategy than pre-prandial exercise for managing postprandial hyperglycemia in individuals with T2D for several reasons [11, 17, 21]. First, postprandial exercise increases glucose uptake into the muscle when blood glucose is peaking, resulting in a blunted glucose peak and a reduction in hyperglycemia [13, 26, 27]. Second, in postprandial exercise, the contraction-mediated glucose uptake may be complemented by the endogenous insulin secretion stimulated by the meal [17].
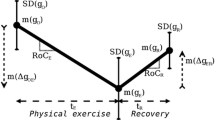
While postprandial exercise is beneficial for reducing hyperglycemia, the optimal timing for exercise initiation following a meal is not clear. Prior studies have reported a rapid glucose rebound when short duration exercise was performed less than 60 min after a meal [13, 20, 28]. One potential reason for this is decreased insulin secretion due to sympathetic activity associated with the acute thermic effect of food [13, 29]. As insulin and exercise both stimulate the sympathetic nervous system, they may confound the sympathetic response of food. In spite of this, the intensity and durations varied greatly in the current review, making firm timing recommendations difficult. In general, exercising within a 3-h window after a meal seems to positively impact glucose control.
4.2 Modality
The included studies provide strong evidence that walking or cycling following a meal reduces postprandial hyperglycemia [17, 18, 22, 30]. Stair climbing and descending has also showed positive effects, though more research is needed regarding this modality [15, 20]. Intermittent postprandial exercise also appears to be beneficial, but future research should compare intermittent to continuous exercise while matching for energy expenditure [11, 15]. Discontinuous exercise may be particularly effective for populations with poor cardiorespiratory fitness, such as obese or elderly individuals, who are unable to perform continuous exercise.
Only two studies utilized protocols with resistance training [16, 21]. One of these studies reported a 30% decrease in short-term glucose AUC [21], the other reported a decrease from 9.6 mmol/L to 8.6 mmol/L in 24-h average glucose concentration [16]. Unfortunately, as far as we know, the correlation between glucose reductions and improvements in specific clinical outcomes has not been established. However, a decrease in glycated hemoglobin (HbA1C) to 7%, which corresponds to a blood glucose level of 8.6 mmol/L, is associated with a reduced risk of macrovascular events including cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke [31].
Progressive resistance training is known to be especially beneficial for the T2D population due to increases in lean muscle mass and type II fiber type recruitment [32]. Resistance training may be a feasible modality to implement since it is well tolerated in many populations [33]. It may also be preferable to aerobic exercise following a meal given the relatively minimal degree of associated gastrointestinal distress. Van Dijk et al. directly compared aerobic exercise to resistance training and found that both modalities reduced 24-h average glucose concentrations by ~ 10%. In the same study, 24-h prevalence of hyperglycemia was also reduced by 33 and 35% for aerobic exercise and resistance training, respectively [16]. The strength of this evidence leads us to recommend 2–3 days per week of resistance training following the largest meal of the day. However, future studies are warranted to compare the acute and chronic effects of resistance and aerobic training on postprandial hyperglycemia.
4.3 Intensity
For the purpose of the current review, exercise intensity was classified according to the American College of Sports Medicine (ACSM) criteria, whereby low, moderate, and high intensity are defined as < 40, 40–59, and 60–89% volume of oxygen uptake reserve (VO2R) or percent of heart rate reserve (%HRR), respectively. Some studies described exercise intensity using percentage of work capacity and maximum heart rate [15, 16, 18, 19, 22]. While these units are not identical, there is a general consensus among exercise physiologists that these intensities correlate to the corresponding ACSM categories.
Low- and moderate-intensity exercise had beneficial effects on postprandial hyperglycemia. However, high-intensity exercise showed inconsistent results depending on the timing of the specific glucose measurement. Five studies showed beneficial decreases in the 24-h prevalence of hyperglycemia (18.6–65%) [15, 16, 18, 22, 24]—it must be noted that the study with a 65% decrease had only seven subjects and a large standard deviation (40%) [18]. On the other hand, one study showed a slight increase in glucose concentration (1.1%) when the measurement was taken immediately following exercise [22]. One potential reason for this is that high-intensity exercise may elicit a more substantial endocrine response than moderate-intensity exercise [34]. This could theoretically stimulate a glucose rebound due to increases in gluconeogenesis and glycogenolysis [35]. Therefore, oxygen uptake and ventilatory threshold testing in individuals with T2D may be helpful for clinicians to accurately prescribe exercise intensity and minimize the likelihood of a glucose rebound. It is also important to consider that high-intensity exercise may not be well tolerated following a large meal.
In terms of moderate-intensity exercise, long-term (24-h) glucose measures were consistently reduced by 17–34% (Table 2) [11, 12, 15,16,17]. There was mixed evidence for the short-term benefits of moderate-intensity, potentially due to variations in postprandial timing and duration of exercise. The findings were more stable for low-intensity exercise. Manders et al. directly compared low intensity to high intensity while matching for energy expenditure and observed a 49.7% decrease in 24-h prevalence of hyperglycemia following low-intensity exercise, compared to only 18.6% following high-intensity exercise [22]. Another study showed that a 15-min bout of walking after each meal of the day did not induce a significant reduction in hyperglycemia, potentially due to the short duration [15]. Taken together, these findings suggest that increasing the duration, and thus the energy expenditure, may be particularly important for low-intensity exercise.
4.4 Energy Expenditure
The current evidence indicates that energy expenditure may be the most critical factor in reducing postprandial hyperglycemia in the T2D population [12, 13, 15, 22]. In support of this theory, Larsen et al. found that a reduction in energy intake had the same impact on glucose control as equivalent exercise-induced energy expenditure [12]. In light of this, moderate-intensity exercise may be the most realistic means of reducing hyperglycemia because it requires more energy than low-intensity exercise for a given amount of time. Ideally, intensity should be dependent on the time available to exercise, in which less time available for exercise necessitates increases in intensity.
As energy balance is a key factor that can be modified by both energy intake and expenditure, it is clear that eating a balanced diet and avoiding over-eating are essential for T2D management [26]. However, excessive focus on caloric reduction may lead to disordered eating, higher glucocorticoid levels, and a failure to maintain long-term weight loss [36]. Thus, exercise may be a more important lifestyle behavior to regulate energy balance. Future studies should report energy expenditure and examine the intensity, type, and timing of postprandial exercise while matching for energy expenditure.
4.5 Clinical Implications and Recommendations
Based on the evidence, we recommend individuals with T2D adhere to the current ACSM guidelines for the general population, which are similar to the exercise guidelines released by the American Diabetes Association (ADA). These guidelines recommend achieving 150 min of moderate-intensity aerobic exercise per week (30 min five times per week), 1 h of vigorous intensity aerobic exercise per week (20 min three times per week) or some equivalent combination [4, 37]. The guidelines also recommend 2–3 non-consecutive days of resistance training per week at intensities varying between 50 and 80% of 1-repetition maximum (1RM), targeting all major muscle groups using a scheme of 1–4 sets of 8–15 repetitions per exercise [4, 37]. Importantly, these recommendations also state that no more than 2 days should pass without any exercise participation due to the transient glucose uptake mechanism stimulated by exercise [37].
We recommend that this exercise is initiated after the largest meal of the day, and that individuals should progress toward 60 min of moderate-intensity activity per day to maximize energy expenditure. For most individuals in this population, a brisk walk (7–10 metabolic equivalent of tasks (METs)) would be considered moderate-intensity exercise. In addition, resistance training should also be performed following the largest meal on 2–3 days of the week. Despite the paucity of literature regarding resistance training in individuals with T2D, we recommend that the volumes for resistance training described in the previous paragraph should be followed to ensure adequate energy expenditure.
In addition to exercising after the largest meal of the day, we have several other recommendations that differ slightly from the current guidelines. First, for resistance training, we suggest remaining in the moderate-intensity range (50–60% 1-RM) to prevent large increases in blood pressure and minimize delayed-onset muscle soreness (DOMS). Minimizing DOMS, in particular, may help to maximize adherence. Secondly, while the current guidelines advise no more than two consecutive days without exercise, we suggest that there should be no more than 1 day per week without exercise. Again, this shift in frequency is recommended due to the transient nature of contraction-mediated glucose uptake. A sample weekly exercise schedule may consist of 4 days per week of aerobic exercise and 3 days per week of resistance training.
These guidelines are ideals and rigid adherence to them may be unrealistic. Therefore, prioritizing the most important underlying themes of lifestyle-based glycemic regulation (any type of physical activity every day surrounding large meals) should be promoted. For example, clinicians and other health professionals should recommend increasing physical activity following a meal, even if it as simple as walking the dog after the largest meal of the day. Additionally, clinicians and health professions must be versed in prescribing patient-focused, creative strategies to overcome barriers. If designating 60 min for exercise is not attainable due to work or family responsibilities, incorporating physical activity into these responsibilities (e.g., a family walk after dinner or using a stand-up desk for 60 min after lunch at work) may be a feasible option when time is a barrier. Exercise prescription should focus on progressively increasing energy expenditure following large meals, while maintaining adherence, and empowering the individual. Ultimately, clinicians should help patients work toward the goal of 60 min of moderate-intensity aerobic exercise or resistance training following the largest meal of the day.
5 Conclusion
Postprandial hyperglycemia is a significant problem for individuals with T2D. The current evidence indicates that postprandial exercise may help reduce hyperglycemia, thus preventing the progression of T2D and associated complications. Although the optimal intensity and timing of initiation are not clear, energy expenditure seems to be the most critical factor. Based on this, we suggest updating the current ACSM and ADA guidelines to prescribe low–moderate-intensity daily exercise during the 3-h period following the largest meal of the day.
References
Cavalot F, Pagliarino A, Valle M, Di Martino L, Bonomo K, Massucco P, et al. Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: lessons from the San Luigi Gonzaga Diabetes Study. Diabetes Care. 2011;34(10):2237–43.
Bacchi E, Negri C, Trombetta M, Zanolin ME, Lanza M, Bonora E, et al. Differences in the acute effects of aerobic and resistance exercise in subjects with type 2 diabetes: Results from the RAED2 Randomized Trial. Earnest CP, editor. PLoS One. 2012;7(12):e49937.
Huang S, Czech MP. The GLUT-4 glucose transporter. Cell Metab [Internet]. 2007 [cited 2017 May 22];5(4):237–52. http://www.sciencedirect.com/science/article/pii/S1550413107000678.
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–67.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev [Internet]. 2015;4(1):1. http://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials [Internet]. 1996[cited 2017 Aug 3];17(1):1–12. http://www.ncbi.nlm.nih.gov/pubmed/8721797.
Maher CG, Moseley AM, Sherrington C, Elkins MR, Herbert RD. A description of the trials, reviews, and practice guidelines indexed in the PEDro database. Phys Ther. 2008;88(9):1068–77.
Verhagen AP, de Vet HCW, de Bie RA, Kessels AGH, Boers M, Bouter LM, et al. The Delphi list: a criteria for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(98):1235–41.
Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet [Internet]. 2001;357(9263):1191–4. http://www.sciencedirect.com/science/article/pii/S0140673600043373.
Van Rosendal SP, Osborne MA, Fassett RG, Coombes JS. Guidelines for glycerol use in hyperhydration and rehydration associated with exercise. Sports Med. 2010;40:113–39.
Haxhi J, Leto G, di Palumbo AS, Sbriccoli P, Guidetti L, Fantini C, et al. Exercise at lunchtime: effect on glycemic control and oxidative stress in middle-aged men with type 2 diabetes. Eur J Appl Physiol. 2016;116(3):573–82.
Larsen JJS, Dela F, Kjaer M, Galbo H. The effect of moderate exercise on postprandial glucose homeostasis in NIDDM patients. Diabetologia. 1997;40(4):447–53.
Larsen JJS, Dela F, Madsbad S, Galbo H. The effect of intense exercise on postprandial glucose homeostasis in type II diabetic patients. Diabetologia. 1999;42(11):1282–92.
Poirier P, Mawhinney S, Grondin L, Tremblay A, Broderick T, Cleroux J, et al. Prior meal enhances the plasma glucose lowering effect of exercise in type 2 diabetes. Med Sci Sport Exerc. 2001;33(8):1259–64.
van Dijk J-W, Venema M, van Mechelen W, Stehouwer CDA, Hartgens F, van Loon LJC. Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care [Internet]. 2013[cited 2017 Feb 12];36(11):3448–53. http://www.ncbi.nlm.nih.gov/pubmed/24041682.
van Dijk J-W, Manders RJF, Tummers K, Bonomi AG, Stehouwer CDA, Hartgens F, et al. Both resistance- and endurance-type exercise reduce the prevalence of hyperglycaemia in individuals with impaired glucose tolerance and in insulin-treated and non-insulin-treated type 2 diabetic patients. Diabetologia [Internet]. 2012 [cited 2017 Feb 12];55(5):1273–82. http://springerlink.bibliotecabuap.elogim.com/10.1007/s00125-011-2380-5.
Colberg SR, Zarrabi L, Bennington L, Nakave A, Thomas Somma C, Swain DP, et al. Postprandial walking is better for lowering the glycemic effect of dinner than pre-dinner exercise in type 2 diabetic individuals. J Am Med Dir Assoc. 2009;10(6):394–7.
Gillen JB, Little JP, Punthakee Z, Tarnopolsky MA, Riddell MC, Gibala MJ. Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Diabetes Obes Metab. 2012;14(6):575–7.
Honda H, Igaki M, Hatanaka Y, Komatsu M, Tanaka S, Miki T, et al. Stair climbing/descending exercise for a short time decreases blood glucose levels after a meal in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2016;4(1):e000232.
Takaishi T. Stair climbing/descending exercise-immediate effect against postprandial hyperglycemia in older people with type 2 diabetes mellitus. Ann Sport Med Res. 2015;2(3):1023.
Heden TD, Winn NC, Mari A, Booth FW, Rector RS, Thyfault JP, et al. Postdinner resistance exercise improves postprandial risk factors more effectively than predinner resistance exercise in patients with type 2 diabetes. J Appl Physiol. 2015;118(5):624–34.
Manders RJF, van Dijk J-WM, van Loon LJC. Low-intensity exercise reduces the prevalence of hyperglycemia in type 2 diabetes. Med Sci Sport Exerc [Internet]. 2010[cited 2017 Feb 12];42(2):219–25. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005768-201002000-00001.
Tobin LWL, Kiens B, Galbo H. The effect of exercise on postprandial lipidemia in type 2 diabetic patients. Eur J Appl Physiol [Internet]. 2007[cited 2017 Feb 12];102(3):361–70. http://www.ncbi.nlm.nih.gov/pubmed/17952452.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. [cited 2017 May 27]. https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/jcem/87/3/10.1210_jcem.87.3.8341/2/jcem0978.pdf.
Pistrosch F, Natali A, Hanefeld M. Is hyperglycemia a cardiovascular risk factor? Diabetes Care [Internet]. 2011 [cited 2017 May 27];34 Suppl 2(Suppl 2):S128–31. http://www.ncbi.nlm.nih.gov/pubmed/21525443.
Larsen JJS, Dela F, Kjaer M, Galbo H. The effect of moderate exercise on postprandial glucose homeostasis in NIDDM patients. Diabetologia. 1997;40:447–53.
Poirier P, Tremblay A, Catellier C, Tancrède G, Garneau C, Nadeau A. Impact of time interval from the last meal on glucose response to exercise in subjects with type 2 diabetes. J Clin Endocrinol Metab [Internet]. 2000[cited 2017 Feb 12];85(8):2860–4. http://press.endocrine.org/doi/10.1210/jcem.85.8.6760.
Høstmark AT, Ekeland GS, Beckstrøm AC, Meen HD. Postprandial light physical activity blunts the blood glucose increase. Prev Med (Baltim) [Internet]. 2006 [cited 2017 May 28];42(5):369–71. http://linkinghub.elsevier.com/retrieve/pii/S0091743505001623
Tappy L. Thermic effect of food and sympathetic nervous system activity in humans. Reprod Nutr Dev [Internet]. 1996 [cited 2017 May 28];36(4):391–7. http://www.ncbi.nlm.nih.gov/pubmed/8878356.
Haxhi J, Scotto di Palumbo A, Sacchetti M. Exercising for metabolic control: is timing important? Ann Nutr Metab. 2013;62(1):14–25.
Zoungas S, Chalmers J, Ninomiya T, Li Q, Cooper ME, Colagiuri S, et al. Association of HbA1c levels with vascular complications and death in patients with type 2 diabetes: evidence of glycaemic thresholds. Diabetologia [Internet]. 2012[cited 2017 Jul 11];55(3):636–43. http://www.ncbi.nlm.nih.gov/pubmed/22186981.
Laughlin MH. Physical activity-induced remodeling of vasculature in skeletal muscle: role in treatment of type 2 diabetes. J Appl Physiol. 2016;120(1):1–16.
Falck RS, Davis JC, Milosevic E, Liu-Ambrose T. How much will older adults exercise? A feasibility study of aerobic training combined with resistance training. Pilot Feasibility Stud [Internet]. 2017[cited 2017 Jun 2];3(1):2. http://www.ncbi.nlm.nih.gov/pubmed/28138396.
Hill EE, Zack E, Battaglini C, Viru M, Viru A, Hackney AC. Exercise and circulating cortisol levels: the intensity threshold effect. J Endocrinol Invest. 2008;31(7):587–91.
Hackney AC, Walz EA. Hormonal adaptation and the stress of exercise training: the role of glucocorticoids. 2013 [cited 2017 Apr 2];4(420):165–71. http://www.tss.awf.poznan.pl/files/Vol_4_Hackney_-_Walz.pdf
Tomiyama AJ, Mann T, Vinas D, Hunger JM, Dejager J, Taylor SE. Low calorie dieting increases cortisol. Psychosom Med [Internet]. 2010 [cited 2017 Jun 2];72(4):357–64. http://www.ncbi.nlm.nih.gov/pubmed/20368473
Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care [Internet]. 2016 [cited 2017 Dec 4];39(11):2065–79. http://care.diabetesjournals.org/content/39/11/2065.
Funding
No sources of funding were used to assist in the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Andrew Borror, Gabriel Zieff, Claudio Battaglini, and Lee Stoner declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borror, A., Zieff, G., Battaglini, C. et al. The Effects of Postprandial Exercise on Glucose Control in Individuals with Type 2 Diabetes: A Systematic Review. Sports Med 48, 1479–1491 (2018). https://doi.org/10.1007/s40279-018-0864-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-018-0864-x