Abstract
Low energy availability, functional hypothalamic amenorrhea, and low bone mineral density are three interrelated conditions described in athletic women. Although described as the female athlete triad (Triad), males experience similar health concerns. The literature suggests that individuals with a disability may experience altered physiology related to these three conditions when compared with the able-bodied population. The goal of this review is to describe the unique implications of low energy availability, low bone mineral density, and, in females, menstrual dysfunction in individuals with a disability and their potential impact on the para athlete population. A literature review was performed linking search terms related to the three conditions with six disability categories that are most represented in para sport. Few articles were found that directly pertained to athletes, therefore, the review additionally characterizes literature found in a non-athlete population. Review of the available literature in athletes suggests that both male and female athletes with spinal cord injury demonstrate risk factors for low energy availability. Bone mineral density may also show improvements for wheelchair athletes or athletes with hemiplegic cerebral palsy when compared with a disabled non-athlete population. However, the prevalence of the three conditions and implications on the health of para athletes is largely unknown and represents a key gap in the sports medicine literature. As participation in para sport continues to increase, further research is needed to understand the impact of these three interrelated health concerns for athletes with a disability, accompanied by educational initiatives targeting athletes, coaches, and health professionals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of low energy availability, menstrual dysfunction, and impaired bone health in athletes with a disability is largely unknown. |
Susceptibility towards low energy availability and impaired bone health is dependent on disability type and severity in many cases. |
Participation in Paralympic and community-based adaptive sport competition is growing at a rapid pace. Therefore, more research is needed to better understand the implications of low energy availability, menstrual dysfunction, and impaired bone health in athletes with a disability. |
1 Introduction
Nutritional deficits are known to affect many physiological processes in athletes, and the importance of optimal nutrition has been recognized by major sports governing bodies and organizations. The term female athlete triad (Triad) was initially outlined in 1993 as a syndrome consisting of disordered eating, amenorrhea, and osteoporosis [1]. In 2007, a position stand from the American College of Sports Medicine (ACSM) updated the diagnostic criteria for the Triad, characterizing it as a spectrum ranging from optimal health to disease for the three following interrelated conditions: energy availability, menstrual function, and bone mineral density (BMD) [2]. It was noted that low energy availability accounted for both intentional and unintentional energy deficits that drive symptomatology, and the diagnostic criteria were also amended to acknowledge that athletes and active women may experience one or more of the three components [2]. In 2014, these definitions were preserved and expanded for purposes of assigning a risk assessment score and guiding clinicians making decisions for return to play [3].
Additionally, the impact of energy status on multiple physiological processes has been recognized by the International Olympic Committee (IOC) in a recent consensus statement, supporting that energy deficiency may contribute to menstrual dysfunction and impaired bone health [4]. While low energy availability has been shown to alter metabolic and reproductive hormones in healthy females, analogous consequences such as hormonal imbalance or low BMD have been identified in male athletes [5–7].
Although the systemic impact of low energy availability has been studied rather extensively in able-bodied athletes, little is currently known regarding its prevalence or effects on athletes with a disability [4]. It must be recognized that this population of athletes may have energy requirements, bone health considerations, and menstrual function differences that vary from the norms of the general athlete population. These variations may be multifactorial and attributable to the characteristics of the disability itself, behavioral and training changes due to the nature of adaptive sports competition, or both. Additionally, it is important to recognize that sports-related injury and illness may have heightened functional consequences for athletes with a disability when compared with their able-bodied peers [8, 9]. The paucity of literature available to inform evidence-based practice on the prevention and treatment of low energy availability, menstrual dysfunction, and impaired bone health in athletes with disability means that current standards of care are usually extrapolated from what is known in the able-bodied population.
Concurrently, participation in community-based adaptive sport and Paralympic sport continues to rapidly expand. Although relatively young in sports history, the Paralympic movement has grown into significant international recognition and is now considered one of the premier elite sporting events in the world. The London 2012 Summer Paralympic Games featured over 4000 athletes who competed across 20 sports, a significant increase from the first official Paralympic games in 1960 [10, 11]. This sharp increase in elite para sport participation also likely reflects the accelerated growth of grassroots sports opportunities for athletes with disabilities. As with able-bodied athletes, the medical community must be prepared to provide optimal care to these individuals.
Therefore, the aim of this narrative review is to synthesize the available literature on energy status, menstrual function, and bone health in female athletes with disability. We also examine literature that pertains to energy status and bone health in male athletes with a disability. Where a paucity of literature exists regarding the athlete population, information regarding non-athletic individuals with a disability is provided to create a framework for future investigations and discuss implications for the athletic population. This review provides a basis for further research and the development of clinical assessment tools and treatment algorithms. In all cases, athletes, coaches, athletic trainers, physicians, and other support personnel must be educated about the causes and consequences of low energy availability in athletes with disabilities to better recognize and prevent known consequences such as hormonal imbalance and low BMD.
2 Literature Search Methodology
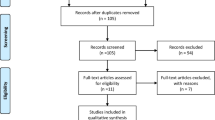
A review of the literature was performed in July–August 2015 using PubMed, cross-linking terms related to energy availability, menstrual function, and bone health with six major disability categories: spinal cord injury (SCI), spina bifida (SB), central neurologic injury [cerebral palsy (CP) or acquired brain injury], amputee, short stature or achondroplasia, and visual impairment (Table 1). The specific search terms used for the literature review are located in Table 1. These disability categories were selected given their high prevalence in the population of athletes with disabilities and to ensure that a breadth of information regarding various types of impairments was captured [12]. Given the paucity of data in this area, original research, reviews, and applicable book chapters were all included in the initial search. This resulted in a total of 1565 search results, many of which were not directly applicable to our research scope. References were then screened by two authors utilizing the following inclusion criteria: articles were written in English; relevance to energy availability, menstrual function, or BMD; and relevance to one of the six major disability categories selected in either an athlete or non-athlete population. This screening process yielded 63 original research papers, eight reviews, and five chapters, which were included in the analysis (Table 1). Notably, only five original research papers and one review article were specific to athletes (Table 2) [13–18].
2.1 Definitions
2.1.1 Energy Availability
Energy availability is commonly defined as energy intake (kcal) minus exercise energy expenditure (kcal), divided by kilograms of fat free mass (FFM) [19]. Energy availability is a product of three components—energy intake, energy expenditure, and stored energy—and can be altered by changes in any of these components. In individuals with a disability, FFM may change as a result of the impairment, further increasing the challenge of determining energy availability in this cohort. Additionally, the term low energy availability, based on healthy females without known medical conditions, is defined as a threshold of 30 kcal/kg FFM per day [6], however it remains unclear how this may change based upon impairment type. Despite these challenges, it is important to explore what is known regarding influences of energy status on the overall health of athletes with disability.
2.1.2 Menstrual Function
Menstrual function is an important aspect of overall health in females, and menstrual dysfunction is important to recognize and address in athletes of all backgrounds. Menstrual dysfunction refers to development of oligomenorrhea (nine or fewer menstrual periods in 12 months), primary amenorrhea (first menstrual period at age ≥15 years) or secondary amenorrhea (defined as cessation of menses for ≥3 months) [2]. These definitions apply equally to able-bodied and disabled individuals.
2.1.3 Bone Mineral Density
BMD is a common measure of overall skeletal health. The ACSM defines “low BMD” in young female athletes participating in weight-bearing sports as BMD Z scores between −1.0 and −2.0 with other risk factors [2]. The International Society for Clinical Densitometry (ISCD) indicates a Z score below −2.0 as abnormal for premenopausal women and for males [20]. How these thresholds may vary for athletes with disability is currently unknown.
3 Findings
3.1 Energy Availability
3.1.1 Spinal Cord Injury
The literature search yielded two articles that examined dietary habits and nutrient intake among athletes with SCI (Table 2). One study reported that Canadian athletes with SCI competing in wheelchair sports may monitor or restrict food intake to maintain an ideal body weight for elite sport competition. Of interest, this behavior was found to be more prevalent in male athletes [14]. In contrast, female athletes with SCI may be at particular risk for other nutrient deficiencies. A second study reported that more than 25% of female athletes with SCI had a daily dietary intake that did not meet the estimated average requirement in the general population for nutrients, including calcium, magnesium, folate, and vitamin D [13]. Furthermore, one review article indicated that, for both males and females, energy expenditure of individuals with SCI is typically reduced by between 25 and 75% during exercise when compared with able-bodied individuals, with the greatest energy expenditure reduction in athletes with tetraplegia or those participating in static wheelchair sports [17, 21].
The reason for this reduction is likely multifactorial. In the non-athlete population of individuals with SCI, it has been noted that basal metabolic rate and energy expenditure are significantly affected by SCI and vary according to lesion level and whether the injury is complete or incomplete [22]. For example, energy needs are reduced for individuals with SCI because everyday movements use a smaller muscle mass, particularly in individuals who are primary wheelchair users [23]. Additionally, in the presence of a spinal cord lesion, the amount of sympathetic nervous system activation that is stimulated and available for use during exercise varies. In athletes with higher levels of injury (i.e., upper thoracic or cervical SCI), this may result in cardiovascular blunting or a reduction in peak heart rate, blood pressure, and maximal oxygen uptake (VO2max) during exercise, ultimately decreasing energy expenditure [17, 24].
3.1.2 Spina Bifida
No sources were identified that pertained to energy availability and SB in a para athlete population. Therefore, we describe literature found in a non-athlete population. Individuals with SB who are primary wheelchair users likely have considerations regarding reduced basal metabolic rate and daily energy requirements, similar to individuals with paraplegia due to SCI. However, for those with SB who ambulate either with or without an assistive device, energy requirements are proportionally higher than that of the general population due to inefficiency of gait [25, 26]. Additionally, studies have noted that psychosocial and functional factors associated with SB may put young women at increased risk for an eating disorder. One survey reported that 8% of young women with SB met clinical criteria for presence of an eating disorder compared with 0.5–2% of the general female population [27]. Although it is likely that multiple complex factors contribute to this disparity, one report suggested young women with SB may be at an increased risk for disordered eating when weight loss is promoted as a means of increasing daily mobility and easing exertion with functional tasks (e.g., wheelchair transfers) or the care provided by others for activities of daily living [27]. An increased focus on weight control may, in some cases, evolve into disordered eating as a means of compensation for neurological disability [28].
3.1.3 Central Neurologic Injury
While no literature was identified describing energy availability in a para athlete population, the energy needs and expenditures of individuals with a central neurologic injury such as CP or traumatic brain injury (TBI) vary greatly because of the wide range of associated functional impairment related to activities such as ambulation and daily self-care. Inefficiencies in ambulation and the presence of athetosis, spasticity, or ataxia, may all increase energy requirements, while decreased oral motor function may reduce oral intake [29, 30]. This may create a paradigm in which individuals with CP develop low energy availability. Conversely, one study found that total energy expenditure (TEE) for individuals with CP was lower than that of able-bodied individuals, even though TEE for each individual varied widely [31]. Ambulatory status was found to be the only significant predictor of energy expenditure [31]. Finally, individuals with CP may experience low energy availability in circumstances where weight control or weight reduction is desired to make self-care or receiving care from others easier [30].
In individuals with TBI, a combination of reduced energy needs, metabolic changes, and increased food intake may result in weight gain [32, 33]. Hyperphagia and subsequent weight gain can be present in the early stages after the initial injury and may persist for years [32]. For example, one longitudinal study reported that 42% of individuals with TBI gained weight over the initial 38 months post injury, whereas only 28% lost weight [33].
3.1.4 Amputees
No studies were found that examined the prevalence or impact of low energy availability in an amputee para athlete population. However, in the general amputee population, individuals who ambulate with use of a prosthesis may have a higher energy expenditure than the general population due to the inefficiency of movement caused by gait asymmetry, and inefficient ambulation may place amputees at increased risk for low energy availability [34, 35]. In this context, it is important to note that bilateral amputations and more proximal lower extremity amputations are likely to result in higher energy expenditure during ambulation [36, 37]. Other factors that affect nutritional and energy requirements within this population include dermatologic illness involving the residual limb such as rashes, infections, or wounds, most commonly at the site of prosthetic contact. Such conditions may result in a hypermetabolic state, thus increasing systemic energy needs [38].
3.1.5 Short Stature
There is limited research on the unique energy requirements of individuals with short stature (SS), and no research is available in an athlete population. It has been assumed that, compared with the general population, energy needs are likely similar per kilogram of body mass [39]. That said, previous studies have revealed an elevated resting metabolic rate in individuals with achondroplasia, thought to be due to alteration in organ mass or mitochondrial differences [40, 41]. Of note, an earlier study revealed that, although both male and female individuals with achondroplasia had significantly higher resting metabolic rates, the prevalence of obesity in this population was almost twice as high as that of peers of normal stature, likely due to reduced total caloric needs in the setting of a smaller body habitus [40, 41].
3.1.6 Visual Impairment
Although little is reported in the literature, with no sources available from a para athlete population, intuitively, the energy requirements of individuals with visual impairment (VI) should not vary greatly from that of the sighted population. However, some research suggests that, more globally, this population has a higher level of body satisfaction and engages in less dieting than sighted women [42, 43]. This may highlight the influence of sight and visualization of body image on eating behaviors [42, 43]. Conversely, several case reports do cite the occurrence of eating disorders in females with VI [42–47].
3.2 Menstrual Function
Of note, our review characterizes menstrual function in female individuals with a disability more generally, as no literature was available to characterize menstrual function in an athlete population. In addition, the literature review yielded no sources describing menstrual dysfunction in amputee, SS, SB, or VI disability categories.
3.2.1 Spinal Cord Injury
Although experiencing an SCI may affect the hypothalamic–pituitary axis in the acute phase after injury, thus impacting the menstrual cycle, the majority of research supports no significant long-term impact on menstrual function or reproductive health in females with SCI [48]. In one study, young females who sustained an SCI before menarche experienced an age of onset consistent with their non-injured mothers and individuals who sustained an SCI post menarche [49]. Acute SCI may result in transient amenorrhea; however, normal menstruation typically resumes in an average of 5 months following injury [50]. Women with SCI were also found to complete successful pregnancies, although women with adult-onset incomplete paraplegia reported more pregnancies overall than women with complete quadriplegia or women injured at a younger age [50, 51]. Of note, the average age of athletes competing at the 2012 Paralympic games was 30.9 compared with an average age of 26 for the 2012 Olympic games [52, 53]. No studies to date have examined impaired fertility as a consequence of low energy availability in this athlete cohort, which may have heightened consequences given the slightly older para athlete population.
3.2.2 Central Neurologic Injury
Although dependent on severity, almost half of all females experienced menstrual dysfunction including amenorrhea lasting up to 5 years post TBI [54]. For individuals with TBI, severity of the injury was found to be predictive of the duration of amenorrhea. Shorter periods of amenorrhea were significantly associated with higher scores on global outcomes, community participation, and health-related quality of life [54, 55]. Once the menstrual cycle resumed, women with TBI were found to have normal fertility compared with controls [54]. Although little is reported in the literature regarding potential differences in menstrual cycles in individuals with CP, one study reported that 29.4% of adolescents with CP experienced menstrual dysfunction [56].
3.3 Bone Mineral Density
3.3.1 Spinal Cord Injury
One preliminary investigation of the effects of sports activity on BMD in athletes with SCI noted that a timely return to sport following SCI is correlated with higher BMD in the legs, trunk, and total body independent of age and type of sport, and may even help to attenuate bone loss, although further studies are needed [15]. Another study found that athletes participating in wheelchair basketball had increased BMD in the distal radius compared with sedentary individuals with paraplegia [16] (Table 2). No studies to date have directly compared BMD between able-bodied athletes and athletes with SCI. Although the aforementioned studies show the potential positive effect of sports participation on BMD in the upper extremities of athletes with SCI, persistent deficits in the lower extremities are likely in those with reduced weight-bearing status.
Research in the general population of individuals with SCI notes that osteoporosis is seen in virtually all individuals with SCI due to reduced skeletal loading over time [57]. Females with SCI are at a particularly increased risk for osteoporosis as the effect of SCI has been shown to be greater than that of the typical bone health decline associated with estrogen loss in able-bodied women [58]. The combination of these two factors leads to particular vulnerability for compromised bone health in women with SCI, with associated increased risk for low energy fracture [59]. In the majority of individuals with SCI, osteoporotic fractures most commonly affect the distal femur and proximal tibia [59–62]. Although many of these fractures are low impact, they are often associated with a variety of other clinical complications [63].
Evidence suggests that temporal patterns exist for declining bone health in individuals of both sexes with SCI. In adults with complete injuries who remain non-weight bearing, significant loss of BMD in the proximal femur has been identified within 1 year post injury and frequently reaches the fracture threshold within 1–5 years [64]. Although the negative relationship between time since injury and bone health have been clearly demonstrated in the literature, reports of precise temporal relationships vary and depend upon factors such as the bone health of the individual prior to injury and weight-bearing status post injury [64–68]. Given this dramatic, accelerated rate of bone loss post injury, focused early intervention within the first year after SCI may help preserve BMD, at least to some extent [67]. Interventions used may include a combination of pharmacological interventions in addition to physical interventions such as weight bearing (when possible) or the use of standing frames. For example, early participation in intensive loading activities was shown to attenuate bone loss of the tibia in individuals with SCI [69].
3.3.2 Spina Bifida
No studies examining BMD in athletes with SB were available for review. Similar to observations from the SCI population, individuals with SB frequently have significantly lower BMD than their able-bodied counterparts, increasing the risk for fracture [70–72]. BMD is most dramatically reduced in individuals who are wheelchair users for their daily mobility compared with those with limited or full ambulation [70, 71, 73]. Females with SB also show trends toward lower BMD compared with males [70].
3.3.3 Central Neurologic Injury
To date, one study has examined BMD Z-scores and fat-free soft tissue mass among Paralympic track athletes with hemiplegic CP (Table 2). The study showed no difference in BMD on the affected and unaffected sides, despite asymmetry in fat free soft tissue mass in the upper and lower limbs [18]. In a non-athlete population, studies have shown that, because the level of impairment and function varies in individuals with central neurologic injury, the prevalence of reduced BMD can also vary. For example, children with CP display a wide range of BMD, which typically averages one standard deviation below the average for age-matched peers [74]. In several studies, ambulatory status and nutritional status were the most significant predictors of BMD in individuals with CP [74–76]. Grossberg et al. [77] noted a positive correlation between low weight and reduced BMD, further supporting the fact that poor nutritional intake, a common feature of CP, may also lead to alterations in bone health. When classified by ambulatory status, individuals who did not ambulate were found to have lower BMD in the femur than those who ambulated regularly [78].
On an individual basis, the severity and subtype of CP have also been found to be important factors affecting BMD. Adults with spastic CP, associated with muscular hypertonicity and decreased neuromuscular control, had lower BMD Z-scores at the femur than adults with dyskinetic CP [78]. Another recent study of adults with CP found that BMD at the lumbar spine and hip were correlated with Gross Motor Function Classification System (GMFCS) levels, noting that individuals with the lowest mobility showed the lowest associated BMD values [76]. Supporting these findings, one longitudinal study showed that lower BMD correlated with increased severity of CP as defined by difficulty feeding and poor growth and nutrition [79]. In children with moderate to severe CP and resultant reduced BMD, an increased risk of fracture was noted [80, 81]. Finally, additional medical issues observed in individuals with CP, such as seizure activity requiring long-term use of anticonvulsants, have also been found to impact BMD [82–84].
3.3.4 Amputees
No studies examining BMD in an amputee para athlete population were available for review. For non-athletes, one study revealed that cortical and total BMD were significantly lower at the hip on the side affected by lower extremity amputation when compared with the native leg [85]. Supporting this finding, in a cohort of nine below-knee amputees, Royer and Koenig [86] noted that proximal tibia and femoral neck BMD values were significantly lower in the leg affected by limb loss than in the native leg.
3.3.5 Short Stature
No studies examining BMD in the population of para athletes with SS were available for review. Although evidence is limited in the general population of individuals with SS, one study analyzed BMD Z-scores in a cohort of 18 individuals with achondroplasia and four individuals with hypochondroplasia. Researchers found that spinal BMD was below average for both groups, with an average Z score of −1.1 [87]. A recent case series examined dual energy X-ray absorptiometry (DXA) scans of the lumbar region (L1–L4) in individuals with achondroplasia aged 25–53 years and revealed that 5 of 11 patients had low BMD (defined as Z score below −2.0). Of the five individuals with low BMD, four were male and one was female [88]. The mechanism of impaired bone health for individuals with achondroplasia is not well understood; however, a recent case report noted that this may result from bone suppression and remodeling as a result of the achondroplasia in and of itself [89].
3.3.6 Visual Impairment
In a non-athletic population, there is a significant relationship between VI and the incidence of hip fracture due to an increased risk of falls and trauma related to impaired vision [90–92]. These studies additionally noted the risk of hip fracture to be higher in females with VI than in males with VI [90–92]. Little information is available on the relationship between VI and BMD. One study suggested that individuals with VI who lead sedentary lifestyles may be at higher risk for reduced BMD, noting that BMD in the weight-bearing proximal femur of women with VI was 8% lower than in age-matched sighted women, whereas BMD at the distal radius did not vary between the two groups [93].
4 Discussion
Results from our literature review reveal a paucity of research directly investigating the prevalence and impact of low energy availability, menstrual dysfunction, and low BMD on athletes with a disability. As the number of athletes competing in para sports from the grassroots to elite levels continues to expand rapidly, this is an area significantly in need of further research. Although prior work acknowledges the physiological differences between individuals with a disability and their able-bodied counterparts with regard to these three interrelated conditions, how these changes may impact an individual athlete’s risk of injury or illness has not previously been addressed.
4.1 Summary of Key Findings
Several important findings from this literature review warrant specific discussion. Our summative review of the literature identifies the following key findings which, although they are primarily based on literature investigating individuals with disabilities more broadly, are also likely to impact the health and performance of athletes (Table 3).
First, it is very important to note that no data are currently available regarding what constitutes low energy availability or energy deficit in female athletes with varied types of disability or the prevalence of energy deficit within this population. As low energy availability represents the cornerstone of Triad-related illness, with resultant downstream effects on multiple body systems, this constitutes an important gap in knowledge that must be addressed.
Additionally, in able-bodied athletes of both sexes, bone density is typically higher in physically active people than in inactive peers, especially those participating in activities involving high-impact loading [94]. In contrast, sports involving muscle activity without ground reaction forces, such as swimming, do not consistently improve bone health [94]. The absence of impact loading in many adaptive sports may lead to suboptimal benefits of sports participation on skeletal health. Additionally, the disability-specific impacts of reduced weight-bearing status, impaired nutrition (including reduced energy availability or reduced intake of calcium and vitamin D) and changes in menstrual function may all negatively influence skeletal health.
For individuals with altered weight-bearing status, such as SCI and SB, overall energy needs are reduced [17, 21, 23]. This is particularly the case for those with cervical or high thoracic SCI who may also experience cardiovascular blunting [17]. Although these individuals may experience a reduced propensity for low energy availability, they are generally at much higher risk of bone-related injury due to early-onset osteoporosis from reduced weight-bearing status [64–68]. The risks are most profound for those who do not ambulate at all, such as athletes who are reliant on wheelchairs for daily mobility as well as sports participation [64]. Additionally, given that the presence of SCI or SB does not alter the menstrual cycle dramatically, oligomenorrhea or amenorrhea should serve as an important early warning sign of reduced energy availability, as it would for any female athlete.
For individuals with central neurologic injury such as CP or TBI, energy requirements are more challenging to estimate because of the heterogeneity of functional impairment based on the severity of injury. Those with more severe injuries, and thus a greater level of mobility impairment, are likely to have reduced energy needs as well as reduced BMD due to altered weight-bearing over time [31]. An exception exists in individuals with aberrant movement patterns, such as severe dyskinetic CP, for whom dyskinetic movement may lead to higher energy expenditures [29, 30]. Additionally, in females with a central neurologic injury, menstrual dysfunction can exist because of baseline alterations of the hypothalamic–pituitary axis, indicating that the presence of amenorrhea or oligomenorrhea may or may not be a pathologic representation of low energy availability [54–56]. It is notable that, in the study by Burke et al. [56], 29.4% of adolescents with CP experienced menstrual dysfunction. This can be compared with the able-bodied population, for which Hoch et al. [95] reported menstrual dysfunction in 21% of adolescents.
For individuals with primary musculoskeletal disability such as amputees, the prevalence and characteristics of low energy availability, menstrual dysfunction, and impaired bone health may not vary greatly when compared with their able-bodied counterparts, keeping in mind several key points. For example, individuals who utilize a prosthesis are likely to have higher baseline energy needs that place them at risk for low energy availability by increasing estimated energy expenditure, particularly if both lower limbs are affected, such as with double amputees [34–37]. In unilateral amputees, the affected limb may also exhibit reduced BMD, placing it at greater risk for injury [85, 86].
Finally, it is important to note that individuals with disability due to SS or VI may not experience dramatic physiologic alterations that influence energy status, menstruation, or bone health when compared with able-bodied counterparts [39]. However, VI may increase the risk of falls, and therefore, fractures [91–93].
Across disability types, the presence of a more significant functional impairment, with resultant reliance on others for personal care needs, may place an individual at greater risk for disordered eating and thus reduced energy availability [27, 28, 32]. This may be due to altered eating patterns and/or concern for abnormal weight gain that would increase the burden for caregivers, and may lead to an increased risk of injury or illness [32]. This point is germane, given that competitive opportunities for athletes with high support needs are rapidly increasing throughout the Paralympic movement [96].
Our review is limited by the paucity of literature describing energy availability, BMD, and, in female athletes, menstrual function within an athlete population. Although male athletes may also experience reduced bone density and nutritional deficits, alterations of the neuroendocrine axis including the suppression of sex hormones have not been characterized in this population.
4.2 Research Priorities for the Future
Further research is needed to investigate the impact of low energy availability, menstrual dysfunction, and low BMD on athletes with a disability. Based on the findings of this narrative review, the authors recommend that the following research priorities be considered:
-
1.
Assessment of the prevalence of low energy availability (with or without disordered eating), menstrual dysfunction, and low BMD in female athletes from various disability categories. In addition, it is important to assess the combined prevalence of the aforementioned conditions in this athletic population.
-
2.
Assessment of knowledge regarding these three interrelated conditions, optimal energy status for health and performance, and the influence of energy availability on risk of injury and illness among athletes with disabilities and key stakeholders (coaches, athletic trainers, healthcare providers, and other members of the athlete entourage).
-
3.
Characterization of energy needs for athletes of various disability types and within various sport disciplines. For example, although the available literature has described the reduced energy needs of individuals with SCI, little is known regarding how this may vary for athletes based on factors such as level of injury and engagement in sports competition.
-
4.
Characterization of normative BMD values in individuals and athletes with SCI, SB, or central neurologic injury for whom reduced weight bearing over time may lead to an increased risk for fracture from low energy trauma. Given that low BMD is a health consequence of disability, it is important to characterize what DXA measurements should be of particular concern for predicting increased risk of fracture during sports participation.
-
5.
Finally, sex-specific differences in the relationship between energy status, hormonal function and bone health in athletes with disabilities are important to explore and should be used to guide effective management for all athletes who participate in sports, both male and female alike [7].
5 Conclusions
Although energy availability, menstrual function, and BMD have been studied rather extensively in able-bodied female athletes, very few studies have investigated the prevalence, effects, and cumulative impact of the three conditions in athletes with a disability. Our review highlights that female individuals within the major classifications of disability germane to the Paralympic movement have baseline physiological impairments in energy status, menstrual function, and bone health that could be further negatively impacted through sports participation, as seen in able-bodied individuals. Further research is needed to assess the prevalence of the three conditions in female athletes with a disability, beginning with the establishment of baseline energy requirements for both male and female individuals of various impairment types, thus enabling a more detailed understanding of how low energy availability may affect this population. Finally, it is critical to educate athletes with a disability, as well as their coaches, medical providers, and the entire athlete entourage, on the performance and health-related implications of low energy availability, low BMD and, in female athletes, menstrual dysfunction. Only through raising awareness of these conditions can we ultimately implement prevention and treatment strategies appropriately tailored to athletes with a disability.
References
Yeager KK, Agnostini R, Nattiv A, et al. The female athlete triad: disordered eating, amenorrhea, osteoporosis. Med Sci Sports Exerc. 1993;25(7):775–7.
Nattiv A, Loucks AB, Manore MM, et al. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–82.
De Souza MJ, Nattiv A, Joy E, et al. 2014 Female athlete triad coalition consensus statement on treatment and return to play of the female athlete triad: 1st International Conference held in San Francisco, California, May 2012 and 2nd International Conference held in Indianapolis, Indiana, May 2013. Br J Sports Med. 2014;48(4):289
Mountjoy M, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond the Female Athlete Triad-Relative Energy Deficiency in Sport (RED-S). Br J Sports Med. 2014;48(7):491–7.
Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. J Clin Endocrinol Metab. 2003;88(1):297–311.
Ihle R, Louck AB. Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res. 2004;19(8):1231–40.
Tenforde AS, Barrack MT, Nattiv A, et al. Parallels with the female athlete triad in male athletes. Sports Med. 2016;46(2):171–82.
Blauwet CA. The paralympic female athlete. In: Mountjoy M, editor. Handbook of sports medicine and science. West Sussex: John Wiley & Sons, Inc.; 2014. p. 120–8.
Willick S, Webborn N. Medicine. In: Vanlandewijck Y, Thompson W, editors. The paralympic athlete: handbook of sports medicine and science. West Sussex: Wiley Blackwell; 2010. p. 74–88.
London 2012 Facts and Figures. 2013. http://www.olympic.org/Documents/Reference_documents_Factsheets/London_2012_Facts_and_Figures-eng.pdf. Accessed 22 Dec 2015
Gold JR, Gold MM. Access for all: the rise of the Paralympic Games. J R Soc Promot Health. 2007;127(3):133–41.
Webborn N, Van de Vliet P. Paralympic medicine. Lancet. 2012;380(9836):65–71.
Krempien JL, Barr SI. Risk of nutrient inadequacies in elite Canadian athletes with spinal cord injury. Int J Sport Nutr Exerc Metab. 2011;21(5):417–25.
Krempien JL, Barr SI. Eating attitudes and behaviours in elite Canadian athletes with a spinal cord injury. Eat Behav. 2012;13(1):36–41.
Miyahara K, Wang DH, Mori K, et al. Effect of sports activity on bone mineral density in wheelchair athletes. J Bone Miner Metab. 2008;26(1):101–6.
Goktepe AS, Yilmaz B, Alaca R, et al. Bone density loss after spinal cord injury: elite paraplegic basketball players vs. paraplegic sedentary persons. Am J Phys Med Rehabil. 2004;83(4):279–83.
Price M. Energy expenditure and metabolism during exercise in persons with a spinal cord injury. Sports Med. 2010;40(8):681–96.
Runciman P, Tucker R, Ferreira S, et al. Site-specific bone mineral density is unaltered despite differences in fat-free soft tissue mass between affected and nonaffected sides in hemiplegic paralympic athletes with cerebral palsy: preliminary findings. Am J Phys Med Rehabil. 2016;95(10):771–8.
Loucks AB. Low energy availability in the marathon and other endurance sports. Sports Med. 2007;37(4–5):348–52.
2015 ISCD Official Positions-Adult. 2015. http://www.iscd.org/official-positions/2015-iscd-official-positions-adult/. Accessed 4 Feb 2016
Goosey-Tolfrey V, Krempien J, Price M. Spinal Cord Injuries. In: Broad E, editor. Sports Nutrition for Paralympic Athletes. Abingdon: Taylor & Francis Group; 2014. p. 67–90.
Mollinger LA, Spurr GB, el Ghatit AZ, et al. Daily energy expenditure and basal metabolic rates of patients with spinal cord injury. Arch Phys Med Rehabil. 1985;66(7):420–6.
Glaser RM. Physiologic aspects of spinal cord injury and functional neuromuscular stimulation. Cent Nerv Syst Trauma. 1986;3(1):49–62.
Krassioukov A, West C. The role of autonomic function on sport performance in athletes with spinal cord injury. PM R. 2014;6(8 Suppl):S58–65.
Hassler J. The influence of ankle-foot orthoses on gait and energy expenditure in spina bifida. Pediatr Phys Ther. 2001;13(3):146–7.
Evans EP, Tew B. The energy expenditure of spina bifida children during walking and wheelchair ambulation. Z Kinderchir. 1981;34(4):425–7.
Gross SM, Ireys HT, Kinsman SL. Young women with physical disabilities: risk factors for symptoms of eating disorders. J Dev Behav Pediatr. 2000;21(2):87–96.
Silber TJ, Shaer C, Atkins D. Eating disorders in adolescents and young women with spina bifida. Int J Eat Disord. 1999;25(4):457–61.
Jonsson AC, Lindgren I, Norrving B, et al. Weight loss after stroke: a population-based study from the Lund Stroke Register. Stroke. 2008;39(3):918–23.
Crosland J, Boyd C. Cerebral palsy and acquired brain injuries. In: Broad E, editor. Sports nutrition for paralympic athletes. Abingdon: Taylor & Francis Group; 2014. p. 91–105.
Johnson RK, Hildreth HG, Contompasis SH, et al. Total energy expenditure in adults with cerebral palsy as assessed by doubly labeled water. J Am Diet Assoc. 1997;97(9):966–70.
Castano B, Capdevila E. Eating disorders in patients with traumatic brain injury: a report of four cases. NeuroRehabilitation. 2010;27(2):113–6.
Crenn P, Hamchaoui S, Bourget-Massari A, et al. Changes in weight after traumatic brain injury in adult patients: a longitudinal study. Clin Nutr. 2014;33(2):348–53.
Bragaru M, Dekker R, Geertzen JH. Sport prostheses and prosthetic adaptations for the upper and lower limb amputees: an overview of peer reviewed literature. Prosthet Orthot Int. 2012;36(3):290–6.
Goosey-Tolfrey V, Sutton L. Body composition in disease and disability. In: Stewart AD, Sutton L, editors. Body composition in sport, exercise, and health. Abingdon: Routledge; 2012. p. 166–86.
Blumentritt S, Schmalz T, Jarasch R. Significance of static prosthesis alignment for standing and walking of patients with lower limb amputation. Orthopade. 2001;30(3):161–8.
Gonzalez EG, Corcoran PJ, Reyes RL. Energy expenditure in below-knee amputees: correlation with stump length. Arch Phys Med Rehabil. 1974;55(3):111–9.
Meyer N, Edwards S. Amputees. In: Broad E, editor. Sports nutrition for paralympic athletes. Abingdon: Taylor & Francis Group; 2014. p. 107–26.
Broad E. Les Autres. In: Broad E, editor. Sports nutrition for paralympic athletes. Abingdon: Taylor & Francis Group; 2014. p. 127–34.
Weaver DS, Owen GM. Nutrition and short stature. Postgrad Med. 1977;62(6):93–9.
Hunter AG, Hecht JT, Scott CI Jr. Standard weight for height curves in achondroplasia. Am J Med Genet. 1996;62(3):255–61.
Ashikali EM, Dittmar H. Body image and restrained eating in blind and sighted women: a preliminary study. Body Image. 2010;7(2):172–5.
Baker D, Sivyer R, Towell T. Body image dissatisfaction and eating attitudes in visually impaired women. Int J Eat Disord. 1998;24(3):319–22.
Simeunovic Ostojic M, Hansen AM. Sociocultural factors in the development of bulimia nervosa in a blind woman: a case report. Int J Eat Disord. 2013;46(3):284–8.
Kocourkova J, Soltysova M, Mohaplova M, et al. Anorexia nervosa in a blind girl. Neuro Endocrinol Lett. 2011;32(6):748–50.
Fernandez-Aranda F, Crespo JM, Jimenez-Murcia S, et al. Blindness and bulimia nervosa: a description of a case report and its treatment. Int J Eat Disord. 2006;39(3):263–5.
Sharp CW. Anorexia nervosa and depression in a woman blind since the age of nine months. Can J Psychiatry. 1993;38(7):469–71.
Huang TS, Wang YH, Lai JS, et al. The hypothalamus-pituitary-ovary and hypothalamus-pituitary-thyroid axes in spinal cord-injured women. Metabolism. 1996;45(6):718–22.
Anderson CJ, Mulcahey MJ, Vogel LC. Menstruation and pediatric spinal cord injury. J Spinal Cord Med. 1997;20(1):56–9.
Charlifue SW, Gerhart KA, Menter RR, et al. Sexual issues of women with spinal cord injuries. Paraplegia. 1992;30(3):192–9.
Bughi S, Shaw SJ, Mahmood G, et al. Amenorrhea, pregnancy, and pregnancy outcomes in women following spinal cord injury: a retrospective cross-sectional study. Endocr Pract. 2008;14(4):437–41.
Schwellnus M, Derman W, Jordaan E, et al. Factors associated with illness in athletes participating in the London 2012 Paralympic Games: a prospective cohort study involving 49,910 athlete-days. Br J Sports Med. 2013;47(7):433–40.
Could you be an athlete? Olympics 2012 by age, weight and height. https://www.theguardian.com/sport/datablog/2012/aug/07/olympics-2012-athletes-age-weight-height. Accessed 7 Nov 2016.
Colantonio A, Mar W, Escobar M, et al. Women’s health outcomes after traumatic brain injury. J Womens Health (Larchmt). 2010;19(6):1109–16.
Ripley DL, Harrison-Felix C, Sendroy-Terrill M, et al. The impact of female reproductive function on outcomes after traumatic brain injury. Arch Phys Med Rehabil. 2008;89(6):1090–6.
Burke LM, Kalpakjian CZ, Smith YR, et al. Gynecologic issues of adolescents with Down syndrome, autism, and cerebral palsy. J Pediatr Adolesc Gynecol. 2010;23(1):11–5.
Jiang SD, Dai LY, Jiang LS. Osteoporosis after spinal cord injury. Osteoporos Int. 2006;17(2):180–92.
Slade JM, Bickel CS, Dudley GA. The effect of a repeat bout of exercise on muscle injury in persons with spinal cord injury. Eur J Appl Physiol. 2004;92(3):363–6.
Vestergaard P, Krogh K, Rejnmark L, et al. Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord. 1998;36(11):790–6.
Dauty M, Perrouin Verbe B, Maugars Y, et al. Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone. 2000;27(2):305–9.
Frotzler A, Cheikh-Sarraf B, Portehrani M, et al. Long-bone fractures in persons with spinal cord injury. Spinal Cord. 2015;53(9):701–4.
Zehnder Y, Luthi M, Michel D, et al. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int. 2004;15(3):180–9.
Gifre L, Vidal J, Carrasco JL, et al. Risk factors for the development of osteoporosis after spinal cord injury. A 12-month follow-up study. Osteoporos Int. 2015;26(9):2273–80.
Szollar SM, Martin EM, Sartoris DJ, et al. Bone mineral density and indexes of bone metabolism in spinal cord injury. Am J Phys Med Rehabil. 1998;77(1):28–35.
Garland DE, Stewart CA, Adkins RH, et al. Osteoporosis after spinal cord injury. J Orthop Res. 1992;10(3):371–8.
Demirel G, Yilmaz H, Paker N, et al. Osteoporosis after spinal cord injury. Spinal Cord. 1998;36(12):822–5.
Coupaud S, McLean AN, Purcell M, et al. Decreases in bone mineral density at cortical and trabecular sites in the tibia and femur during the first year of spinal cord injury. Bone. 2015;74:69–75.
Frotzler A, Berger M, Knecht H, et al. Bone steady-state is established at reduced bone strength after spinal cord injury: a longitudinal study using peripheral quantitative computed tomography (pQCT). Bone. 2008;43(3):549–55.
Frey-Rindova P, de Bruin ED, Stussi E, et al. Bone mineral density in upper and lower extremities during 12 months after spinal cord injury measured by peripheral quantitative computed tomography. Spinal Cord. 2000;38(1):26–32.
Martinelli V, Dell’Atti C, Ausili E, et al. Risk of fracture prevention in spina bifida patients: correlation between bone mineral density, vitamin D, and electrolyte values. Childs Nerv Syst. 2015;31(8):1361–5.
Marreiros H, Loff C, Calado E. Osteoporosis in paediatric patients with spina bifida. J Spinal Cord Med. 2012;35(1):9–21.
Szalay EA, Cheema A. Children with spina bifida are at risk for low bone density. Clin Orthop Relat Res. 2011;469(5):1253–7.
Marreiros H, Monteiro L, Loff C, et al. Fractures in children and adolescents with spina bifida: the experience of a Portuguese tertiary-care hospital. Dev Med Child Neurol. 2010;52(8):754–9.
Henderson RC, Lin PP, Greene WB. Bone-mineral density in children and adolescents who have spastic cerebral palsy. J Bone Joint Surg Am. 1995;77(11):1671–81.
Finbraten AK, Syversen U, Skranes J, et al. Bone mineral density and vitamin D status in ambulatory and non-ambulatory children with cerebral palsy. Osteoporos Int. 2015;26(1):141–50.
Fowler EG, Rao S, Nattiv A, et al. Bone density in premenopausal women and men under 50 years of age with cerebral palsy. Arch Phys Med Rehabil. 2015;96(7):1304–9.
Grossberg R, Blackford MG, Kecskemethy HH, et al. Longitudinal assessment of bone growth and development in a facility-based population of young adults with cerebral palsy. Dev Med Child Neurol. 2015;57(11):1064–9.
Kim W, Lee SJ, Yoon YK, et al. Adults with spastic cerebral palsy have lower bone mass than those with dyskinetic cerebral palsy. Bone. 2015;71:89–93.
Henderson RC, Kairalla JA, Barrington JW, et al. Longitudinal changes in bone density in children and adolescents with moderate to severe cerebral palsy. J Pediatr. 2005;146(6):769–75.
Henderson RC, Lark RK, Gurka MJ, et al. Bone density and metabolism in children and adolescents with moderate to severe cerebral palsy. Pediatrics. 2002;110(1 Pt 1):e5.
Henderson R. Bone density and size in ambulatory children with cerebral palsy. Dev Med Child Neurol. 2011;53(2):102–3.
Mergler S, Evenhuis HM, Boot AM, et al. Epidemiology of low bone mineral density and fractures in children with severe cerebral palsy: a systematic review. Dev Med Child Neurol. 2009;51(10):773–8.
Presedo A, Dabney KW, Miller F. Fractures in patients with cerebral palsy. J Pediatr Orthop. 2007;27(2):147–53.
Leet AI, Mesfin A, Pichard C, et al. Fractures in children with cerebral palsy. J Pediatr Orthop. 2006;26(5):624–7.
Sherk VD, Bemben MG, Bemben DA. BMD and bone geometry in transtibial and transfemoral amputees. J Bone Miner Res. 2008;23(9):1449–57.
Royer T, Koenig M. Joint loading and bone mineral density in persons with unilateral, trans-tibial amputation. Clin Biomech (Bristol, Avon). 2005;20(10):1119–25.
Matsushita M, Kitoh H, Mishima K, et al. Low bone mineral density in achondroplasia and hypochondroplasia. Pediatr Int. 2016;58(8):705–8.
Arita ES, Pippa MG, Marcucci M, et al. Assessment of osteoporotic alterations in achondroplastic patients: a case series. Clin Rheumatol. 2013;32(3):399–402.
Tasoglu O, Sahin Onat S, Yenigun D, et al. Low bone density in achondroplasia. Clin Rheumatol. 2014;33(5):733–5.
Dargent-Molina P, Favier F, Grandjean H, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348(9021):145–9.
Felson DT, Anderson JJ, Hannan MT, et al. Impaired vision and hip fracture. The Framingham Study. J Am Geriatr Soc. 1989;37(6):495–500.
Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–73.
Uusi-Rasi K, Sievanen H, Rinne M, et al. Bone mineral density of visually handicapped women. Clin Physiol. 2001;21(4):498–503.
Tenforde AS, Fredericson M. Influence of sports participation on bone health in the young athlete: a review of the literature. PM R. 2011;3(9):861–7.
Hoch AZ, Pajewski NM, Moraski L, et al. Prevalence of the female athlete triad in high school athletes and sedentary students. Clin J Sport Med. 2009;19(5):421–8.
Athletes With High Support Needs Committee. 2014. https://www.paralympic.org/the-ipc/committees/athletes-with-high-support-needs. Accessed 27 June 2016.
Acknowledgements
The authors wish to extend their most sincere thanks to Dr. Aurelia Nattiv for her expert review of this manuscript prior to submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Cheri Blauwet, Emily Brook, Adam Tenforde, Elizabeth Broad, Caroline Hu, Eliza Abdu-Glass and Elizabeth Matzkin have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Blauwet, C.A., Brook, E.M., Tenforde, A.S. et al. Low Energy Availability, Menstrual Dysfunction, and Low Bone Mineral Density in Individuals with a Disability: Implications for the Para Athlete Population. Sports Med 47, 1697–1708 (2017). https://doi.org/10.1007/s40279-017-0696-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-017-0696-0