Abstract
Background
Cardiorespiratory fitness (CRF) among people with severe mental illness (SMI) (i.e., schizophrenia, bipolar disorder, and major depressive disorder) is a critical clinical risk factor given its relationship to cardiovascular disease and premature mortality.
Objectives
This study aimed to: (1) investigate the mean CRF in people with SMI versus healthy controls; (2) explore moderators of CRF; and (3) investigate whether CRF improved with exercise interventions and establish if fitness improves more than body mass index following exercise interventions.
Methods
Major electronic databases were searched systematically. A meta-analysis calculating Hedges’ g statistic was undertaken.
Results
Across 23 eligible studies, pooled mean CRF was 28.7 mL/kg/min [95 % confidence interval (CI) 27.3 to 30.0 mL/kg/min, p < 0.001, n = 980]. People with SMI had significantly lower CRF compared with controls (n = 310) (Hedges’ g = −1.01, 95 % CI −1.18 to −0.85, p < 0.001). There were no differences between diagnostic subgroups. In a multivariate regression, first-episode (β = 6.6, 95 % CI 0.6–12.6) and inpatient (β = 5.3, 95 % CI 1.6–9.0) status were significant predictors of higher CRF. Exercise improved CRF (Hedges’ g = 0.33, 95 % CI = 0.21–0.45, p = 0.001), but did not reduce body mass index. Higher CRF improvements were observed following interventions at high intensity, with higher frequency (at least three times per week) and supervised by qualified personnel (i.e., physiotherapists and exercise physiologists).
Conclusion
The multidisciplinary treatment of people with SMI should include a focus on improving fitness to reduce all-cause mortality. Qualified healthcare professionals supporting people with SMI in maintaining an active lifestyle should be included as part of multidisciplinary teams in mental health treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiorespiratory fitness in people with severe mental illness is severely reduced compared with age- and sex-matched controls. |
Exercise improves cardiorespiratory fitness in people with severe mental illness, irrespective of changes in body mass index. |
Early intervention strategies are crucial, while special attention towards outpatient and community settings is needed. |
1 Introduction
People with severe mental illness (SMI) defined as schizophrenia, bipolar disorder, and major depressive disorder (MDD), have a two to three times higher risk for premature death than the general population [1, 2]. This mortality gap translates to a 10- to 20-year shortened life expectancy [3] and appears to be widening [4]. The most important cause for this 10- to 20-year shortened life expectancy is cardiovascular disease (CVD) [5]. Although genetic factors [6] and shared pathophysiological mechanisms [7] contribute, treatment-related factors and unhealthy lifestyle habits play a prominent role [8] in the development of CVD in this population.
In the general population, there is robust evidence demonstrating that low cardiorespiratory fitness (the ability of the circulatory and respiratory systems to supply oxygen to working muscles during sustained physical activity) is a strong and independent predictor for CVD [relative risk (RR) = 1.56; 95 % confidence interval (CI) 1.39–1.75; p < 0.001] and all-cause mortality (RR = 1.70; 95 % CI 1.51–1.92; p < 0.001) [9].
Exercise interventions are effective in improving cardiorespiratory fitness, and are therefore a key component of preventing and treating CVD and reducing associated mortality [10]. Research in the general population has demonstrated that improvements in cardiorespiratory fitness are associated with a lower risk of mortality from CVD independent of age, smoking, and body composition [11].
Investigating cardiorespiratory fitness among people with SMI is of considerable clinical interest given its associations with reduced psychiatric symptoms and cognitive deficits in SMI populations [12] and given the increasing focus on lifestyle interventions as integrated components of standard care for various mental disorders [13–18]. In addition, two recent meta-analyses demonstrated that exercise interventions significantly improve cardiorespiratory fitness in people with schizophrenia [19] and in people with MDD [20]. These data highlight that improved cardiorespiratory fitness should be a key outcome measure for interventions aiming to reduce cardiometabolic risk among people experiencing mental illness.
Despite the clinical significance of cardiorespiratory fitness, data comparing fitness levels across diagnostic SMI subgroups are currently lacking. In the same way, meta-analytic data including all major diagnostic subgroups (i.e., schizophrenia and related psychotic disorders vs. bipolar disorder vs. MDD) are absent in the literature. Moreover, the moderators of cardiorespiratory fitness remain largely unknown in people with SMI. Large-scale pooled analyses exploring differences between diagnostic subgroups in (1) cardiorespiratory fitness, and (2) the effects of exercise on cardiorespiratory fitness across diagnostic subgroups are highly relevant, as they enable (1) risk stratification and (2) investigation of the role of aerobic exercise characteristics (frequency, intensity, duration) across a large number of studies and participants. Pooling data across major diagnostic categories also allows for a more thorough investigation of the effect of demographic variables (age, sex, clinical setting), treatment variables (prescription of antidepressants and antipsychotics), and exercise providers’ characteristics (qualifications) irrespective of the diagnosis. We conducted a meta-analysis with the following aims: (1) investigate the mean cardiorespiratory fitness in people with SMI versus healthy controls, (2) investigate moderators of cardiorespiratory fitness, and (3) investigate if cardiorespiratory fitness improves with exercise interventions, explore moderators of the outcome, and establish if fitness improves more than fatness (body mass index [BMI] and waist circumference reductions) following exercise interventions.
2 Methods
This systematic review adhered to the MOOSE guidelines [21] and the PRISMA statement [22].
2.1 Search Procedure
Three researchers (BS, FS, and DV) searched PubMed, EMBASE, and CINAHL from database inception to December 31, 2015. Key words used were“cardiorespiratory” OR “aerobic fitness” AND “schizophrenia” OR “psychosis” OR “depression” OR “depressive” OR “bipolar” in the title, abstract, or index term fields. Manual searches were also conducted using the reference lists from recovered articles. The eligibility criteria are set out in Sect. 2.2.
2.2 Eligibility Criteria
2.2.1 Participants
Only studies with a confirmed diagnosis of schizophrenia spectrum, MDD, or bipolar disorder according to the Diagnostic and Statistical Manual of Mental Disorders [23, 24] or the International Classification of Diseases [25] were included.
2.2.2 Interventions
Aerobic exercise interventions were defined as physical activity interventions that were planned, structured, repetitive, and purposive, in the sense that improvement or maintenance of physical fitness was an objective [26].
2.2.3 Control Conditions
All non-aerobic interventions (e.g., resistance or strength training), usual-care, or wait-list control conditions were included.
2.2.4 Outcome Measure
The outcome measure was cardiorespiratory fitness (mean ± standard deviation), pre- and, if available, post-exercise intervention, expressed as maximal oxygen uptake (VO2max) or peak oxygen uptake (VO2peak) (mL/kg/min), assessed with a maximal exercise test or estimated with a sub-maximal exercise test. If the standard deviation post-exercise was not available we included the pre-test standard deviation as a proxy measure.
2.2.5 Study Design
We included cross-sectional studies and pre- and post-test studies without a control group and randomized controlled trials or non-randomized clinical controlled trials in which the experimental and control intervention were of similar duration.
2.2.6 Exclusion Criteria
No additional exclusion criteria were applied.
2.3 Study Selection
After the removal of duplicates, two reviewers (DV and BS) screened titles and abstracts of all potentially eligible articles. Both authors applied eligibility criteria, and a list of full-text articles was developed through consensus. Three reviewers (DV, BS, and FS) then applied eligibility criteria and a final list of included articles was reached through consensus. When necessary, the corresponding author was contacted up to two times in a 3-week period to request data that would enable inclusion in the current analyses.
2.4 Data Extraction
Two authors (DV and BS) extracted data using a predetermined data extraction form. The data extracted for exploring moderators of cardiorespiratory fitness were the study setting and patient characteristics (diagnosis, first-episode status or not, age, % Caucasian, % female, % antidepressant use, % antipsychotic use). If age- and sex-matched healthy control data were available, next to the primary outcome also the age and % female of the healthy control groups were collected. For the intervention analyses, data extracted included study design and study setting, participant characteristics in experimental and control conditions (if available) (diagnosis, mean age, % female), duration (<10 vs. ≥10 weeks), frequency (<3 vs. ≥3 times per week) intensity (low/moderate vs. high), and type (aerobic exercise only vs. mixed) of exercise intervention, whether the exercise was supervised or not and qualified versus non-qualified providers. Providers of exercise interventions were considered experts when they had at minimum a bachelor’s degree in physical therapy or exercise physiology, or a similar qualification that included education in exercise prescription and assessment.
2.5 Statistical Analyses
Random-effects meta-analyses were conducted using Comprehensive Meta-Analysis software (Version 3; Biostat, Englewood, NJ, USA). First, we pooled and compared mean cardiorespiratory fitness between people with SMI and healthy controls. Second, we compared baseline cardiorespiratory fitness levels between diagnostic subgroups (i.e., schizophrenia spectrum vs. MDD vs. bipolar disorder vs. studies with mixed diagnoses) and study settings (inpatients vs. outpatients) and conducted meta-regression analyses according to age (year), sex (% female), ethnicity (% Caucasians), and medication use (% antidepressant use, % antipsychotic use). Third, we calculated changes in cardiorespiratory fitness using pre- and post-means and standard deviations of VO2max or VO2peak and, if available, in BMI and waist circumference, of the exercise and control groups, calculating Hedges’ g and the 95 % confidence interval (CI) as estimates of the effect size (ES). If sufficient data were available, exploratory meta-regression analyses were undertaken to investigate the influence on exercise outcomes of mean age (years), sex (% female), baseline BMI, psychotropic medication use (% antidepressants and antipsychotics) in the exercise group, and exercise characteristics (frequency, intensity, duration) and whether exercise interventions were supervised or not by qualified clinicians (exercise physiologists, physical therapists, or similar vs. others). We calculated Hedges’ g statistic, and 95 % CIs for each analysis. Statistical heterogeneity was assessed using the I 2 statistic. Publication bias was assessed with the Begg and Mazumdar test [27].
3 Results
3.1 Search Results and Flow of Studies Through the Review
A total of 1760 records were identified. After screening and the application of the eligibility criteria, 23 studies including 30 CRF values were identified and included in the meta-analysis [28–50]. We requested and received additional data for two studies [30, 44]. Figure 1 presents the flow of studies through the review process.
3.2 Characteristics of Included Studies
Across the 23 studies, the final sample data set included 480 people with schizophrenia (CRF values, n = 15), 424 with MDD (n = 10), and 26 with bipolar disorder (n = 2) and 310 age- and sex-matched healthy controls. There were three CRF values in mixed samples of people with SMI (n = 50). Seven of the included studies were cross-sectional studies and one was longitudinal. There were nine controlled studies (of which eight were randomized controlled trials) whilst the other six were pre- and post-test studies (see Electronic Supplementary Material Table S1). The duration of the interventions ranged from 10 days to 6 months, the frequency from daily to twice a week. Across the interventional studies, 50 participants in the mixed samples, 86 patients with schizophrenia, and 133 patients with MDD underwent exercise interventions while 103 participants with SMI were assigned to a control condition. No studies of exercise interventions investigating cardiorespiratory fitness in people with bipolar disorder were identified.
3.3 Aim 1: Cardiorespiratory Fitness in Patients with SMI Versus Age- and Sex-matched Healthy Controls
Across the 23 studies (including 30 CRF values) (n = 980; mean age at study level = 34.6 years), the pooled mean predicted VO2max or VO2peak was 28.7 mL/kg/min (95 % CI 27.3–30.0 mL/kg/min, p < 0.001). It was possible to pool data from nine CRF values involving 335 participants with SMI and 310 age- and sex-matched healthy controls. Hedges’ g was −1.01 (95 % CI −1.18 to −0.85, p < 0.001) indicating that people with SMI have a large reduction in cardiorespiratory fitness. There was some heterogeneity (I 2 = 47 %), but no publication bias (Kendall tau = 0.11, p = 0.68). People with SMI had a reduced cardiorespiratory fitness of −8.96 mL/kg/min (95 % CI = −12.2 to −5.76 mL/kg/min).
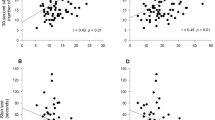
3.4 Aim 2: Moderators of Cardiorespiratory Fitness in Patients with SMI
Full details of the meta-regression analyses of cardiorespiratory fitness are summarized in Table 1. Briefly, no significant differences in cardiorespiratory fitness between diagnostic groups were observed. Older age and a greater proportion of female participants predicted a worse cardiorespiratory fitness level. In contrast, inpatient setting, first episode status, and Caucasian ethnicity (%) predicted a higher cardiorespiratory fitness level. Antidepressant and antipsychotic medication use (%) did not influence the cardiorespiratory fitness level. Details of the subgroup analyses are displayed in Table 1.
When all significant predictors were included in one multivariate regression model only, inpatient status (β = 5.33, 95 % CI 1.60–9.06, p = 0.005) and first-episode illness (β = 6.63, 95 % CI 0.66–12.6, p = 0.03) were significant independent predictors of cardiorespiratory fitness.
3.5 Aims 3: Changes in Cardiorespiratory Fitness Following Exercise Interventions
3.5.1 Meta-analysis of Pre- and Post-test Changes in Cardiorespiratory Fitness in People with SMI
Data from 13 CRF values (n = 255) demonstrated that exercise significantly improved cardiorespiratory fitness across all patients with SMI (Hedges’ g = 0.33, 95 % CI 0.21–0.45, p = 0.001; Fig. 2). There was some heterogeneity (I 2 = 54.4 %) but no evidence of publication bias (Kendall tau = 0.13, p = 0.54). The pooled mean increase in relative predicted VO2max or VO2peak was 2.95 mL/kg/min (95 % CI 2.21–3.69 mL/kg/min, p < 0.001).
3.5.2 Moderators of the Aerobic Exercise Response
High-intensity (vs. low-to-moderate intensity) aerobic exercise and a higher frequency (three or more times per week) of exercise predicted a better outcome. Interventions supervised by qualified personnel (i.e., physiotherapists, exercise physiologists) resulted in higher cardiorespiratory fitness levels. Details of the exercise response subgroup analyses are displayed in Table 2.
3.5.3 Changes in Cardiorespiratory Fitness Versus BMI and Waist Circumference
Seven pre- and post-test exercise intervention studies (n = 113) provided data on changes in fitness (VO2max or VO2peak) and fatness (BMI, although insufficient data on waist circumference changes were available) in the same participants. Our analyses demonstrated that aerobic exercise significantly improved cardiorespiratory fitness (Hedges’ g = 0.37, 95 % CI 0.15–0.59, p < 0.001), whilst no significant changes in BMI were observed (Hedges’ g = −0.04, 95 % CI −0.15 to 0.07, p = 0.46).
3.5.4 Aerobic Exercise Versus Control Conditions
It was possible to pool data from five studies (n = 109) to compare the influence of exercise on predicted VO2max or VO2peak versus control interventions (n = 103). Exercise significantly improved cardiorespiratory fitness compared with the control group (Hedges’ g = 0.43, 95 % CI 0.10–0.76, p = 0.01; n = 109, Fig. 3). There was low heterogeneity (I 2 = 22 %) and no evidence of publication bias (Kendall tau = 0.20, p = 0.62). Compared with controls (n = 103), people with SMI who exercised (n = 109) experienced gains of 2.17 mL/kg/min (95 % CI 0.57–3.77, p = 0.008).
4 Discussion
4.1 General Findings
This is the first quantitative synthesis investigating mean cardiorespiratory fitness in people with SMI versus healthy controls, describing differences between major diagnostic subgroups and exploring the effect of aerobic exercise interventions on cardiorespiratory fitness in the entire SMI population. Our review identified 23 studies and found: (1) cardiorespiratory fitness in people with SMI is, irrespective of the diagnosis, significantly impaired compared with age- and sex-matched healthy controls, (2) first-episode status and inpatient setting were the most important moderators for better fitness levels, and (3) aerobic exercise significantly increased cardiorespiratory fitness, which was significantly better than control conditions. Exercise participation resulted in a pooled mean increase in predicted VO2max or VO2peak of 2.95 mL/kg/min (95 % CI 2.21–3.69 mL/kg/min, p < 0.001). Such improvements in cardiorespiratory fitness are of high clinical relevance. For example, among the general population, every 3.5-mL/kg/min incremental increase in VO2peak is associated with 13 and 15 % decrements in the risk of all-cause mortality and CVD, respectively [9].
Recent debate over the importance of fitness versus fatness in the general population has led to increasing consensus regarding the importance of poor fitness as a better predictor of morbidity and mortality as compared with fatness [11]. This is of particular relevance in people with SMI, given the growing interest in lifestyle interventions aiming to reduce cardiovascular disease risk. Recent clinical trials have demonstrated that achieving weight loss among people experiencing mental illness is possible [14, 51, 52]; however, the optimal way to translate these findings into cost-effective, pragmatic, and scalable interventions is less clear given that reducing weight, waist circumference, and BMI is challenging for people with SMI [15]. Importantly, even in the absence of a reduction in these parameters, improvements in cardiorespiratory fitness following exercise can significantly improve health and reduce mortality [11, 53, 54]. Our meta-analysis, pooling data from seven studies, demonstrated that, although BMI did not reduce with exercise, cardiorespiratory fitness did improve. Because cardiorespiratory fitness improved irrespective of changes in BMI in people with SMI, we advocate that a shift in the focus of exercise interventions away from fatness and towards fitness is justified. Improving cardiorespiratory fitness through exercise seems to be a more feasible, realistic, and clinically meaningful outcome following aerobic exercise interventions in people with SMI. Cardiorespiratory fitness is relatively straightforward to measure in clinical practice using for example (sub-)maximal cycle ergometer tests and clinicians should consider monitoring this as a vital sign, given its significant relationship with all-cause morbidity and mortality. In addition, achieving an increase in cardiorespiratory fitness will provide valuable feedback to patients and clinicians.
Knowledge of demographic variables associated with a lower cardiorespiratory fitness can help identify individuals at greatest need for more intensive monitoring and intervention. As in the general population [55], older age and female sex were associated with lower cardiorespiratory fitness. Potential mechanisms for lower cardiorespiratory fitness levels in studies with a lower percentage of Caucasians have been reported in the general population previously [56]. Because cardiorespiratory fitness levels are determined, in large part, by physical activity levels, an obvious potential mechanism for the observed ethnicity differences could be lower levels of physical activity in ethnic minorities compared with Caucasians. Such a difference was previously reported and is mainly owing to a lack of access to health information, lower participation in health promotion and disease prevention activities, fewer convenient exercise spaces, adequate social support, and access to qualitative healthcare among ethnic minorities [57]. Of particular interest was that first-episode status was, irrespective of age, associated with a better cardiorespiratory fitness indicating that disease-, treatment-, and/or unhealthy lifestyle-related factors contribute to a worsening of cardiorespiratory fitness. This observation points toward the need to adopt a prevention/early intervention approach to reduce worsening of cardiorespiratory fitness and consequent cardio-metabolic risk in people with SMI [58]. One factor accounting for lower cardiorespiratory fitness in outpatients could be that these outpatients often have reduced access to exercise facilities and social support. In addition, there is the burden of having to travel to the treatment facility (including the cost of travel) to participate in the intervention. Previous qualitative research [59] illustrated that people with SMI can feel a sense of anxiety at using community facilities along with the general public. Interventions delivered in inpatient settings may offer more social support and cohesion [60], and therefore increase attendance with physical activity interventions and may consequently result in better cardiorespiratory fitness outcomes. The current findings also echo recent calls [61–63] for more research and clinical attention towards effective physical activity interventions in outpatient and community settings.
4.2 Practical Implications and Future Research
These current meta-analytic data demonstrated that better cardiorespiratory fitness outcomes were obtained following high-intensity exercise interventions and in interventions delivered at higher frequency (at least three times per week). A previous meta-analysis among people who are at increased cardiometabolic risk [64] demonstrated that high-intensity aerobic exercise training significantly increased cardiorespiratory fitness by almost double that achieved by moderate-intensity aerobic exercise training. Our data confirmed that including high-intensity aerobic exercise training leads to greater health-enhancing benefits over a shorter time frame, making high-intensity aerobic exercise a more time efficient and efficacious option when cardiorespiratory fitness improvement is the ultimate goal. Moreover, although more research is needed in people with SMI, and in particular in people with bipolar disorder, short bouts of activity may address another common limiting factor, lack of motivation [65], as it may be a more enticing option than the prospect of continuously exercising for an extended period of time. Short bouts of exercise at higher intensity also resulted in reduced ventilatory response and resultant dyspnea [66], which in people with SMI are limiting factors to continuous exercise [67]. However, of note, the high-intensity aerobic exercise interventions [31, 38] included in this meta-analysis were conducted in young people with SMI. More research therefore is needed to investigate whether such exercise interventions are safe, effective, and efficacious in people with established schizophrenia. Furthermore, the utility of high-intensity interval training as a population-level health promotion strategy has been the focus of considerable debate given concern around adoption and implementation [68], and as such, patients’ preference and motivation must be considered when designing and implementing aerobic exercise interventions. Of interest as well is that long-term interventions (longer than 10 weeks) did not result in more cardiorespiratory fitness improvements than shorter term interventions. Although the limited data available could be a reason for the lack of significance, more research comparing several durations with each other is needed to define the most optimal intervention duration, taking however into account that a sustained active lifestyle should be the ultimate goal.
Of interest for policymakers and budget holders is that better cardiorespiratory fitness outcomes were observed following exercise interventions supervised by qualified healthcare professions such as physiotherapists and exercise physiologists. Our data confirm a recent qualitative review of reviews [17] focusing on non-pharmacological interventions for obesity and related cardiometabolic risk factors proposing that interventions with multiple components, personalized, with more frequent face-to-face contact, and trained treatment providers are associated with better outcomes. Further research is required to determine how to increase adherence to exercise to maximize the potential benefits on cardiorespiratory fitness.
It is important to note that the results of this review highlight the importance of focusing on cardiorespiratory fitness as an outcome following exercise-based interventions. In line with data from lifestyle interventions in the general population [17], we acknowledge the critical importance of dietary-based interventions in achieving weight loss; however, as our results demonstrate, a reduction in cardiometabolic risk can be achieved independent of weight loss through an improvement in cardiorespiratory fitness. As such, focusing on fitness in response to exercise interventions within clinical settings is likely to contribute to closing the premature mortality gap in line with the internationally endorsed Healthy Active Lives (HeAL) goals [69].
5 Conclusion
Our meta-analysis clearly demonstrates that people with SMI should be considered as an important high-risk group for low cardiorespiratory fitness, an important predictor of CVD and premature mortality. However, our analyses also showed that aerobic exercise can improve cardiorespiratory fitness to a clinically relevant degree. Whilst achieving reductions in BMI and weight are important exercise goals that should not be set aside, our results suggest that future exercise interventions should aim to improve cardiorespiratory fitness, with BMI and weight reduction considered as secondary outcomes. Improvements in cardiorespiratory fitness appear to be achievable, and may provide a valid exercise target that could contribute to reductions in premature mortality in people with SMI.
References
Reininghaus U, Dutta R, Dazzan P, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ÆSOP first-episode cohort. Schizophr Bull. 2015;41(3):664–73.
Osborn DP, Levy G, Nazareth I, et al. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Research Database. Arch Gen Psychiatry. 2007;64(2):242–9.
Lawrence D. Excess mortality, mental illness and global burden of disease. Epidemiol Psychiatr Sci. 2015;24(2):141–3.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–31.
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41.
Ellingrod VL, Taylor SF, Dalack G, et al. Risk factors associated with metabolic syndrome in bipolar and schizophrenia subjects treated with antipsychotics: the role of folate pharmacogenetics. J Clin Psychopharmacol. 2012;32(2):261.
Manu P, Correll CU, Wampers M, et al. Markers of inflammation in schizophrenia: association vs. causation. World Psychiatry. 2014;13(2):189–92.
Vancampfort D, Stubbs B, Mitchell AJ, et al. Risk of metabolic syndrome and its components in people with schizophrenia, bipolar and major depressive disorders: a large scale meta-analysis of 198 studies. World Psychiatry. 2015;14(3):339–47.
Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–35.
Barry VW, Baruth M, Beets MW, et al. Fitness vs. fatness on all-cause mortality: a meta-analysis. Progr Cardiovasc Dis. 2014;56(4):382–90.
Lee DC, Artero EG, Sui X, et al. Review: mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24(4 Suppl):27–35.
Kimhy D, Vakhrusheva J, Bartels MN, et al. Aerobic fitness and body mass index in individuals with schizophrenia: implications for neurocognition and daily functioning. Psychiatry Res. 2014;220(3):784–91.
Rosenbaum S, Tiedemann A, Sherrington C, et al. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):964–74.
Bartels SJ, Pratt SI, Aschbrenner KA, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. Am J Psychiatry. 2014;172(4):344–52.
Chwastiak L. Making evidence-based lifestyle modification programs available in community mental health centers: why so slow? J Clin Psychiatry. 2015;76(4):519–20.
Vancampfort D, Rosenbaum S, Probst M, et al. Promotion of cardiorespiratory fitness in schizophrenia: a clinical overview and meta-analysis. Acta Psychiatr Scand. 2015;132(2):131–43.
Ward MC, White DT, Druss BG. A meta-review of lifestyle interventions for cardiovascular risk factors in the general medical population: lessons for individuals with serious mental illness. J Clin Psychiatry. 2015;76(4):477–86.
Firth J, Cotter J, Elliott R, et al. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45(7):1343–61.
Vancampfort D, Rosenbaum S, Ward PB, et al. Exercise improves cardiorespiratory fitness in people with schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2015;169(1–3):453–7.
Stubbs B, Rosenbaum S, Vancampfort D, et al. Exercise improves cardiorespiratory fitness in people with depression: a meta-analysis of randomized control trials. J Affect Disord. 2016;190:249–53.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM 5). Washington, DC: American Psychiatric Association; 2013.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). Washington, DC: American Psychiatric Association; 1994.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Publ Health Rep. 1985;100(2):126.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Knubben K, Reischies FM, Adli M, et al. A randomised, controlled study on the effects of a short-term endurance training programme in patients with major depression. Br J Sports Med. 2007;41(1):29–33.
Krogh J, Saltin B, Gluud C, et al. The DEMO trial: a randomized, parallel-group, observer-blinded clinical trial of strength versus aerobic versus relaxation training for patients with mild to moderate depression. J Clin Psychiatry. 2009;70(6):790–800.
Pajonk FG, Wobrock T, Gruber O, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67(2):133–43.
Heggelund J, Nilsberg GE, Hoff J, et al. Effects of high aerobic intensity training in patients with schizophrenia: a controlled trial. Nord J Psychiatry. 2011;65(4):269–75.
Strassnig M, Brar JS, Ganguli R. Low cardiorespiratory fitness and physical functional capacity in obese patients with schizophrenia. Schizophr Res. 2011;126(1):103–9.
Krogh J, Videbech P, Thomsen C, et al. DEMO-II trial. Aerobic exercise versus stretching exercise in patients with major depression: a randomised clinical trial. PLoS One. 2012;7(10):e48316.
Nilsson BM, Olsson RM, Öman A, et al. Physical capacity, respiratory quotient and energy expenditure during exercise in male patients with schizophrenia compared with healthy controls. Eur Psychiatry. 2012;27(3):206–12.
Scheewe TW, Takken T, Kahn RS, et al. Effects of exercise therapy on cardiorespiratory fitness in patients with schizophrenia. Med Sci Sports Exerc. 2012;44(10):1834–42.
Strassnig MT, Newcomer JW, Harvey PD. Exercise improves physical capacity in obese patients with schizophrenia: pilot study. Schizophr Res. 2012;141(2):284–5.
Ostermann S, Herbsleb M, Schulz S, et al. Exercise reveals the interrelation of physical fitness, inflammatory response, psychopathology, and autonomic function in patients with schizophrenia. Schizophr Bull. 2012;39(5):1139.
Abdel-Baki A, Brazzini-Poisson V, Marois F, et al. Effects of aerobic interval training on metabolic complications and cardiorespiratory fitness in young adults with psychotic disorders: a pilot study. Schizophr Res. 2013;149(1–3):112–5.
Bredin SS, Warburton DE, Lang DJ. The health benefits and challenges of exercise training in persons living with schizophrenia: a pilot study. Brain Sci. 2013;3(2):821–48.
Ozbulut O, Genc A, Bagcioglu E, et al. Evaluation of physical fitness parameters in patients with schizophrenia. Psychiatry Res. 2013;210(3):806–11.
Kimhy D, Vakhrusheva J, Bartels MN, et al. Aerobic fitness and body mass index in individuals with schizophrenia: implications for neurocognition and daily functioning. Psychiatry Res. 2014;220(3):784–91.
Kimhy D, Vakhrusheva J, Bartels MN, et al. The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: a single-blind, randomized clinical trial. Schizophr Bull. 2015;41(4):859–68.
Leone M, Lalande D, Thériault L, et al. Impact of an exercise program on the physiologic, biologic and psychologic profiles in patients with schizophrenia. Schizophr Res. 2015;164(1–3):270.
Nyboe L, Vestergaard CH, Lund H, et al. Metabolic syndrome in first-time hospitalized patients with depression: a 1-year follow-up study. Acta Psychiatr Scand. 2016;133(3):241–8.
Rosenbaum S, Lagopoulos J, Curtis J, et al. Aerobic exercise intervention in young people with schizophrenia spectrum disorders; improved fitness with no change in hippocampal volume. Psychiatry Res Neuroimaging. 2015;232(2):200–1.
Schuch FB, Vasconcelos-Moreno MP, Borowsky C, et al. Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J Psychiatr Res. 2015;61:25–32.
Schuch FB, da Silveira LE, de Zeni TC, et al. Effects of a single bout of maximal aerobic exercise on BDNF in bipolar disorder: a gender-based response. Psychiatry Res. 2015;229(1):57–62.
Vancampfort D, Guelinkcx H, Probst M, et al. Associations between metabolic and aerobic fitness parameters in patients with schizophrenia. J Nerv Ment Dis. 2015;203(1):23–7.
Vancampfort D, Buys R, Sienaert P, et al. Validity of the 6 min walk test in outpatients with bipolar disorder. Psychiatry Res. 2015;230(2):664–7.
Kerling A, Tegtbur U, Gützlaff E, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord. 2015;177:1–6.
Daumit GL, Dickerson FB, Wang NY, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368(17):1594–602.
Green CA, Yarborough BJH, Leo MC, et al. Weight maintenance following the STRIDE lifestyle intervention for individuals taking antipsychotic medications. Obesity. 2015;23(10):1995–2001.
Church TS, LaMonte MJ, Barlow CE, et al. Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med. 2005;165(18):2114–20.
Hainer V, Toplak H, Stich V. Fat or fit: what is more important? Diabetes Care. 2009;32(Suppl 2):S392–7.
Parker BA, Kalasky MJ, Proctor DN. Evidence for sex differences in cardiovascular aging and adaptive responses to physical activity. Eur J Appl Physiol. 2010;110(2):235–46.
Swift DL, Staiano AE, Johannsen NM, et al. Low cardiorespiratory fitness in African Americans: a health disparity risk factor? Sports Med. 2013;43(12):1301–13.
Richardson LD, Norris M. Access to health and health care: how race and ethnicity matter. Mt Sinai J Med. 2010;77(2):166–77.
Curtis J, Watkins A, Rosenbaum S, et al. Evaluating an individualized lifestyle and life skills intervention to prevent antipsychotic-induced weight gain in first-episode psychosis. Early Interv Psychiatry. 2016;10(3):267–76.
Soundy A, Freeman P, Stubbs B, et al. The transcending benefits of physical activity for individuals with schizophrenia: a systematic review and meta-ethnography. Psychiatry Res. 2014;220(1):11–9.
Gross J, Vancampfort D, Stubbs B, et al. A narrative synthesis investigating the use and value of social support to promote physical activity among individuals with schizophrenia. Disabil Rehabil. 2016;38(2):123–50.
Vancampfort D, Rosenbaum S, Probst M, et al. What are the top 10 physical activity research questions in schizophrenia? Disabil Rehabil. 2016;1–9.
Vancampfort D, Stubbs B, Ward P, et al. Integrating physical activity as medicine in the care of people with severe mental illness. Aust N Z J Psychiatry. 2015;49(8):681–2.
Vancampfort D, Stubbs B, Ward PB, et al. Why moving more should be promoted for severe mental illness. Lancet Psychiatry. 2015;2(4):295.
Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–34.
Vancampfort D, Stubbs B, Venigalla SK, et al. Adopting and maintaining physical activity behaviours in people with severe mental illness: the importance of autonomous motivation. Prev Med. 2015;81:216–20.
Beauchamp MK, Nonoyama M, Goldstein RS, et al. Interval versus continuous training in individuals with chronic obstructive pulmonary disease—a systematic review. Thorax. 2010;65(2):157–64.
Vancampfort D, Probst M, Sweers K, et al. Relationships between obesity, functional exercise capacity, physical activity participation and physical self-perception in people with schizophrenia. Acta Psychiatr Scand. 2011;123(6):423–30.
Biddle SJ, Batterham AM. High-intensity interval exercise training for public health: a big HIT or shall we HIT it on the head? Int J Behav Nutr Phys Act. 2015;12(1):95.
Mitchell A, De Hert M. Promotion of physical health in persons with schizophrenia: can we prevent cardiometabolic problems before they begin? Acta Psychiatr Scand. 2015;132(2):83–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Davy Vancampfort has support from the Research Foundation-Flanders (FWOVlaanderen). Brendon Stubbs was supported by the Collaboration for Leadership in Applied Health Research and Care South London for this article. No other sources of funding were used to assist in the preparation of this article.
Conflict of interest
Davy Vancampfort, Simon Rosenbaum, Felipe Schuch, Philip Ward, Justin Richards, James Mugisha, Michel Probst, and Brendon Stubbs declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vancampfort, D., Rosenbaum, S., Schuch, F. et al. Cardiorespiratory Fitness in Severe Mental Illness: A Systematic Review and Meta-analysis. Sports Med 47, 343–352 (2017). https://doi.org/10.1007/s40279-016-0574-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-016-0574-1