Abstract
Non-alcoholic fatty liver disease (NAFLD) is a very common chronic liver disease worldwide, is on the rise following the trend of increasing prevalence of obesity, is the second most common indication for liver transplantation, and is an important cause for hepatocellular carcinoma. Despite the increasing recognition of NAFLD as an important chronic liver disease, little has been published on the economic and health-related quality of life (HR-QOL) impact of NAFLD. We reviewed the current literature related to the economics and HR-QOL of NAFLD and found that increased costs and decreased HR-QOL were associated with NAFLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a paucity of research addressing the health economics and health-related quality of life (HR-QOL) of NAFLD. |
Of the data available, indications are that NAFLD increases costs and resource utilization substantially. |
NAFLD affects HR-QOL, especially in the physical functioning arena. |
Longitudinal studies in patients at risk for NAFLD are warranted. |
1 Introduction
Non-alcoholic fatty liver disease (NAFLD) is a term that encompasses a spectrum of clinico-pathologic changes that range from steatosis to steatohepatitis to cirrhosis. NAFLD is characterized by deposition of hepatic fat with or without other pathologic changes on the liver biopsy. [1, 2] By definition, NAFLD excludes secondary causes of fatty liver including excessive alcohol use, medications, or hereditary disorders such as Wilson’s disease and lipodystrophy [1–3]. NAFLD has been considered the most common cause of liver enzyme elevation and is rapidly becoming one of the most common liver diseases in the Western countries [1–3]. Further, NAFLD is now the second indication for liver transplantation and is associated with hepatocellular carcinoma, a deadly cancer which is currently the fifth leading cause of death in the world [4, 5].
Hepatic steatosis alone (NAFL) is defined as fatty infiltration of the liver without evidence of inflammation, hepatocyte damage or fibrosis [1–4]. Non-alcoholic steatohepatitis (NASH), on the other hand, is characterized by hepatic steatosis with inflammation and hepatocellular ballooning or other evidence of hepatocyte injury or fibrosis [6]. Morphologically, NAFLD is indistinguishable from alcoholic fatty liver disease (AFLD); however, alcohol consumption is the feature that distinguishes NAFLD from AFLD. The amount of alcohol consumed when making this diagnosis is somewhat controversial, though most studies use a cut-off of 70 g/week (females) and 140 g/week (males) [1–4, 6, 7].
NAFLD patients tend to be mostly asymptomatic or have only mild vague symptoms of fatigue or mild right upper quadrant pain [1–4, 6, 7]. Therefore, NAFLD is frequently diagnosed incidentally during follow-up clinical visits for treatment of the components of metabolic syndrome (hypertension, diabetes mellitus, and/or hyperlipidemia) or complications from other disease processes such as polycystic ovary syndrome, obstructive sleep apnea, cardiovascular disease, hypopituitarism, hypogonadism, and hypothyroidism [1–4, 6–14]. Patients with NAFLD may also present with liver enzyme values that could range from normal to five times the upper limit of normal with the ratio of AST to ALT generally <1. Other laboratory abnormalities may include elevated γ-glutamyltransferase (GGT), hyperlipidemia or hyperglycemia [5–8].
The prevalence of NAFLD in the general population is about 20 % but could be as high as 90 % in obese patients undergoing bariatric surgery [15–18]. In contrast, a small proportion of patients with NAFLD are lean and may not have any identifiable metabolic abnormalities [19]. Although there is substantial data available on the prevalence of NAFLD worldwide, little has been reported on the economic and health-related quality-of-life (HR-QOL) burden of this disease. Therefore, the aim of this paper was to present the current evidence related to the economic and HR-QOL issues for patients with NAFLD.
2 Methods
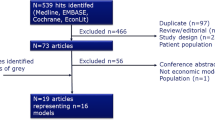
Databases Ovid MEDLINE and PubMed were searched from 1990 to December 2014 using a combination of MeSH, thesaurus terms, and relevant text words: NAFLD, non-alcoholic fatty liver disease, treatment, quality of life, health-related quality of life, resource use, economics, cost effectiveness, and costs. If there were no published full length manuscripts available, presentations from scientific meetings were obtained. Bibliographies from all identified studies were searched for relevant studies. The material used was written in English. Each manuscript was assessed for pertinence to the issue of HR-QOL and economic burden of NAFLD as well as the quality of the study design itself and the quality of the publication. Manuscripts only describing published reviews were not included but were used for background information.
3 Results
Over 600 citations were reviewed; however, after exclusion criteria were applied, a total of 50 potentially relevant articles were identified. Based on a review of these articles, 40 were retrieved for detailed evaluation, and 11 studies met all of the inclusion criteria (6 economic and 5 HR-QOL).
Search results are summarized in Fig. 1. The economic studies represented a total of 293,655 patients with a mean age of 49.86 ± 12.5 years. The majority (63.12 %) of NAFLD patients were male while those with NASH were more commonly female. In addition, the majority of the studies were conducted in the US (n = 3), with one from Germany, one from Iran and one from the UK. The HR-QOL studies represented 2621 patients with an average age of 51.78 ± 11.2 years with 54.6 % of the patients being male. The majority of these studies were also conducted in the US (n = 3), with one from Italy and one from Australia.
3.1 Publications Related to Economic Issues in Patients with Non-Alcoholic Fatty Liver Disease (NAFLD)
There is a remarkable paucity of data addressing economic issues in patients with NAFLD [16, 20–35]. Our search identified six articles related to the economics of NAFLD (four for the general population, one in the ≥65 years old or medically disabled population) (Table 1) [20, 23, 30–33].
In the first study, investigators used Purchasing Power Parity dollars ([PPP$]—an economic technique used to determine the relative values of two different currencies taking into account the impact of exchange rates so one would be able to purchase the same item for the same price in another country) [20, 21]. After following NAFLD patients (n = 528) for 2 years, the investigators calculated healthcare utilization costs based on the price lists approved in 2009–2011 by the Iranian Cabinet for the Public and Private Health Center and then converted the amount to PPP$. The authors reported an annual cost of PPP$1 billion as a result of having NAFLD and its associated comorbidities which was approximately PPP$5043 per individual patient with NAFLD [20].
Another study conducted in the West Suffolk area of the UK attempted to discern the costs of running their hepatology clinics. These investigators found that of the new patients, almost 30 % were being seen for NAFLD, the most frequent reason. They found that the incidence rate for NAFLD was 29 cases per 100,000 people (23.5 non-cirrhotic and 5.5 cirrhotic). These patients were predominantly white (98.4 %) from an area with a low unemployment rate (approximately 2 %) and were seen as new outpatients in the catchment hepatology clinic. Using national indicative tariffs, the total annual hepatology budget for these clinics was £130,000 (£58,000 for resources and £72,000 for clinic attendances). The greatest resource expenditure was on endoscopy (£24,129); however, over 30 % was for ultrasound (£18,291) with an additional 14 % for blood tests (£8090) and 12 % for liver biopsy (£7043) (year 2003/04 values) [33].
A study from the US forecasted the cost of caring for Medicare patients with NAFLD through the year 2050 [23]. This time period was chosen as it potentially includes the years that the baby boomer generation (born 1945–1964) will age into the Medicare system [23–25]. Using data from three major national databases (HealthPartners health plan administrative data; US Census Bureau population projections 2000–2050; and Medical Expenditure Panel Survey [MEPS] 2001 healthcare annual) and calculating per capita costs using the Medical Consumer Price Index of 4.4 % at the claim level to all 2002 services and covering over 60,000 person-years of medical experience for people over age 65 years, the investigators forecasted that the total US per capita costs would increase 18 % (0.3 % annually) with the rate of change steepest from 2000 to 2035 as baby boomers enter retirement. They forecasted costs would level off between 2035 and 2050 as the age structure of the population stabilizes. The projected change in per capita cost due to liver-related conditions was forecasted to increase from 2 % of total per capita costs in 2000 to 11 % by 2050. Further, over 80 % of the increase in the total per capita cost was found to come from only seven Major Practice Categories (MPC: heart and vascular conditions, orthopedic and arthritic conditions, gastric and intestinal conditions, lung conditions, neurologic disorders, endocrine conditions, and urologic conditions), many of which are closely associated with NAFLD. Findings from this study help to forecast costs of treating a disease such as NAFLD, especially since age is strongly associated with more advanced liver disease [23, 26–29].
In a 5-year observational study using data obtained from the Study of Health in Pomerania (SHIP), investigators assessed the relationship of NAFLD to self-reported healthcare utilization and costs. Total costs were calculated as the sum of all outpatient and inpatient costs. All unit costs are reported in year 1999 Euros, and the original costs were inflated using the consumer price indices for healthcare in Germany. After controlling for comorbid conditions, patients with NAFLD experienced a 26 % higher overall increase in their healthcare costs at the 5-year mark. However, the healthcare utilization costs were found to be mediated by the presence of diabetes and cardiovascular disease [30].
Other investigators studied resource utilization for Medicare beneficiaries (n = 29,528) with NAFLD who sought outpatient care. These investigators found that the number of outpatient visits for patients with NAFLD significantly increased over time. In fact, the number of visits almost doubled from 2005 to 2010 (3585 visits in 2005 to 6646 in 2010). Accordingly, so did the patient charges. Patient charges increased 38 % from 2005 to 2010 (US$2624 in 2005 to US$3608 in 2010) while the payments increased only 12 % (US$561 in 2005 to US$629 in 2010) [31].
Using Medicare data from 2005 to 2010 to investigate inpatient and outpatient resource utilization for patients with chronic liver disease (CLD), researchers found that the most common primary diagnosis for inpatient services was hepatic encephalopathy (25.1 %) followed by non-alcoholic cirrhosis (18.01 %), which accounted for 21,576 visits for 14,977 unique patients. Non-alcoholic cirrhosis (14 %) was the most frequent outpatient diagnosis accounting for 515,990 claims for 244,194 unique patients. Inpatient costs increased 5 % over the course of the study (US$11,769 in 2005 to US$12,347 in 2010 after adjustment for inflation). Outpatient costs increased by 10 % over the course of the study (US$366 in 2005 to US$404 in 2010). Predictors of cost common for both inpatients and outpatients were younger age and number of procedures. Although non-alcoholic cirrhosis includes a number of diagnostic categories, some of these patients may have had NAFLD [32].
There are also a few studies assessing the cost effectiveness of bariatric surgery for treating NAFLD [16, 34, 35]. In one systematic review, the researchers found that in addition to patient clinical improvement, there were economic data supporting the cost effectiveness of bariatric surgery as compared with no or conservative treatment for obesity [16]. Another systematic review on the outcomes of bariatric surgery for obese patients with type 2 diabetes conducted in Australia demonstrated similar improvement in clinical outcomes. However, they found that bariatric surgery was much more cost effective for patients with a BMI >35 but <40 than for those with a BMI of >30 but <35 [34].
These few economic studies of NAFLD patients highlight a number of issues. First, there is a lack of robust economic data for patients with NAFLD. Second, the data that is present indicates increasing healthcare resource utilization and costs associated with NAFLD. Furthermore, the data suggest that the costs of NAFLD may be mostly mediated through the presence of metabolic conditions but the impact of NAFLD on liver-related outcomes is expected to grow. Given the increasing prevalence of NAFLD in children, the economic impact must be assessed for both children and adults with NAFLD [36].
3.2 NAFLD and Health-Related Quality of Life
In addition to the economic analysis of NAFLD, studies addressing HR-QOL issues in NAFLD are also quite sparse. Our search identified five studies which measured HR-QOL among patients with NAFLD and one study that measured functional capacity (Table 2).
In a study of 237 patients with CLD who attended a specialty liver clinic, HR-QOL was assessed using the Chronic Liver Disease Questionnaire (CLDQ) for patients with chronic hepatitis B (HBV), chronic hepatitis C (HCV) and NAFLD. Patients with NAFLD (n = 106) were predominantly white, female, and obese with a higher prevalence of diabetes, hypertension, and metabolic syndrome compared with the other groups. The overall HR-QOL scores for NAFLD patients were lower than for patients with HBV or HCV. When the NAFLD HR-QOL scores were compared with those of the HBV patients, NAFLD patients had poorer scores as measured by the overall CLDQ scale score and on five of the six CLDQ subscales (only the Worry domain score did not differ between the two patient groups). Patients with NAFLD also had more impairment in the Systemic and Emotion domains of CLDQ than patients with HCV; however, the overall CLDQ scale and the other four HR-QOL subscales were not different. In the multivariate analysis, NAFLD was found to be an independent predictor for poorer HR-QOL, especially in the three domains of Emotions, Systemic, and Activity. It was concluded that NAFLD patients had poorer HR-QOL than patients with other CLDs, namely HCV or HBV [37].
Another study investigated the effects of CLD on HR-QOL using the generic instrument SF-36. Among 1103 patients with CLD, patient’s age (p < 0.05) was found to be significantly correlated with worsening HR-QOL on every scale of the SF-36. Female patients were found to have more impairments in six (physical functioning, role performance, bodily pain, general health, vitality and mental [p < 0.05]) out of the eight scales of the SF-36. In addition, NAFLD patients (n = 67) showed more impairment of HR-QOL than any other diagnostic group (alcoholic liver disease, autoimmune hepatitis, viral hepatitis, cholestatic liver disease) [38].
In addition to these two studies, another study assessed HR-QOL in adults with NAFLD who were enrolled in the Non-Alcoholic Steatohepatitis Clinical Research Network (NASH-CRN). Again, SF-36 was used as the HR-QOL measurement tool, and the scores were compared with the US population normative scores (norm score = 50). There were a total of 713 subjects with NAFLD with over 62 % of the patients being female (male = 269, female = 444). The mean age of subjects was young at 48.3 years. Over 60 % of the patients had definite NASH, with 28 % having bridging fibrosis or cirrhosis. Almost 30 % of the patients had diabetes. Results indicated that the patients with NAFLD had worse physical component scores (PCS, mean = 45.2) and mental component scores (MCS, mean = 47.6) when compared with the US population norm score or with patients without any chronic illnesses (PCS = 55.8 and MCS = 52.5). Furthermore, patients who had progressed to NASH reported lower PCS scores compared with patients with only NAFLD (44.5 vs 47.1, p = 0.02; respectively). Subjects with cirrhosis had significantly lower PCS results compared with all others (38.4 vs no cirrhosis 47.6, mild cirrhosis 46.2, moderate cirrhosis 44.6, or bridging fibrosis 44.6). MCS did not differ between patients whether they had NASH or by degree of fibrosis when compared with the general healthy US population. MCS score = 52.5) [39].
A study attempted to quantify fatigue (a component closely associated with the vitality domain) in patients with NAFLD. In this two-phase study, NAFLD patients were compared with controls (normal and liver disease) for their level of fatigue using the Fatigue Impact Scale (FIS) as well as exploring the biological associations of fatigue. Patients with NAFLD had significantly more fatigue as indicated by their scores on the FIS (NAFLD 51 ± 38 vs controls 8 ± 12, p < 0.001) as well as their lower level of physical activity as measured by the mean number of steps taken per day for 6 days (NAFLD 7089 ± 2909 vs controls 8676 ± 2894, p = 0.02). There was no evidence of biochemical or histological markers of disease associated with their FIS scores. However, there was a significant association between the level of fatigue measured by the FIS and the amount of daytime sleepiness as measured by the Epworth Sleepiness Scale (r = 0.2, p < 0.001). The authors concluded that the fatigue found in patients with NAFLD is associated with impairment in their physical functioning [40].
In a study conducted in the UK, investigators studied the functional impairment of patients with alcoholic liver disease (ALD) (n = 107) and NAFLD (n = 224) as compared with community controls (n = 100). The researchers then prospectively followed the patients for 3 years to determine if there was any change in their functional ability over time (ALD [n = 69] and NAFLD [n = 162]). Using validated instruments to measure (i) the ability to perform daily activities (Patient-Reported Outcomes Measurement Information System, Health Assessment Questionnaire [PHAQ]), (ii) the presence of cognitive impairment (Cognitive Failures Questionnaire [CFQ]), (iii) the level of fatigue (Fatigue Impact Scale [FIS]), (iv) the presence of vasomotor autonomic dysfunction (Orthostatic Grading Scale [OGS]), and (v) the presence of sleep disturbance (Epworth Sleepiness Scale [ESS]). These investigators found that both groups of patients had a significant level of impairment in all areas as compared with the community controls, but that those suffering from ALD were more impaired than those with NAFLD. Over the long term, they found that functional difficulty persists for patients with ALD and NAFLD. In fact, increased functional difficulty in these patients was significantly associated with death over the 3 years of follow-up. For patients with NAFLD, the significant predictors for worsening functional difficulty were age, fatigue, autonomic dysfunction, and cognitive difficulty [41].
Finally, the impact of NASH treatment on HR-QOL has not been fully described. In a study from Australia, researchers studied a group of 35 patients with CLD and the impact of a 3-month diet and exercise program on clinical outcomes and HR-QOL. The study did show moderate clinical improvement. In terms of HR-QOL, SF-36 was administered at baseline, immediately after the 3-month intervention and then at 15, 12 months after the intervention ended. At baseline, BMI had a strong negative correlation with the HR-QOL physical component score (r = −0.48, p = 0.004), as were four SF-36 health domains: physical functioning (r = −0.54, p = 0.001), general health (r = −0.40, p = 0.02), social functioning (r = −0.40, p = 0.02), and bodily pain (r = −0.40, p = 0.03). The physical and mental composite scores (PCS and MCS, respectively) when compared with the population norms were significantly decreased (p = 0.0003 and p = 0.0007, respectively). In the group of patients who lost weight, PCS and MCS scores after the initial 3-month intervention significantly increased (p = 0.0001 and p = 0.004, respectively) with the majority of the health domains comparable to the population norms. In patients who had maintained their weight loss at 15 months, both the PCS and MCS remained significantly higher than their baseline scores (p = 0.005 and p = 0.003, respectively), while for the patients who regained weight, their PCS and MCS scores decreased and were no different than at baseline [42].
The decrease in HR-QOL may also be affected by the significant and complex interplay between obesity and its associated psychological and psychiatric issues of depression and anxiety [43–45]. To date, most studies of HR-QOL in NAFLD exclude patients with underlying psychiatric issues so the true impact of these co-morbidities on NAFLD patients’ HR-QOL cannot be fully assessed. In the future, it is not only important to perform better designed studies of HR-QOL in NAFLD but also to determine the impact of these co-morbidities on patients’ HR-QOL.
4 Conclusion
The prevalence of NAFLD is rapidly increasing among the general population, and NAFLD is now considered to be one of the most common causes of CLD around the world, mostly due to the increasing prevalence of obesity [46, 47]. NAFLD is a slow, progressive liver disease usually diagnosed incidentally. However, as discussed here, NAFLD is associated with increased healthcare costs and resource utilization [48–50]. Despite significant gaps in robust data, there are predictions that NAFLD-related economic burden will increase, primarily fueled by the epidemic of obesity and metabolic syndrome as well as a high prevalence of NAFLD in children. In addition to its economic burden, patients with NAFLD suffer from significant impairment of HR-QOL. Again, the data on HR-QOL in NAFLD is sparse, but the available data indicates the burden on patients’ HR-QOL is related to fatigue that particularly impacts areas of physical functioning. These gaps in economic and HR-QOL data within the NAFLD population warrant further longitudinal study.
References
Paredes AH, Torres DM, Harrison SA. Nonalcoholic fatty liver disease. Clin Liver Dis. 2012;16:397–419.
Karlas T, Wiegand J, Berg T. Gastrointestinal complications of obesity: non-alcoholic fatty liver disease (NAFLD) and its sequelae. Best Pract Res Clin Endocrinol Metab. 2013;27(2):195–208. doi:10.1016/j.beem.2013.02.002 (Epub 2013 Mar).
Chalasani N, et al. The diagnosis and managements of non-alcoholic fatty liver disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroeneterology, and the American Gastroenterological Association. Hepatology. 2012;55(6):2005–23.
2014 Global cancer facts obtained from the world wide web at: http://www.cancerresearchuk.org/cancer-info/cancerstats/world/incidence/. Accessed 16 Jan 2015.
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, Ahmed A. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547–55 (Epub 2014 Nov 25).
Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA; NASH Clinical Research Network (CRN). Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53(3):810–20. doi:10.1002/hep.24127 (Epub 2011 Feb 11).
Moore JB. Non-alcoholic fatty liver disease: the hepatic consequence of obesity and the metabolic syndrome. Proc Nutr Soc. 2010;69(2):211–20. doi:10.1017/S0029665110000030 (Epub 2010 Feb 17).
Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20(28):9330–7. doi:10.3748/wjg.v20.i28.9330.
Kalaitzakis E. Fatigue in non-alcoholic fatty liver disease: is there a role for hypothyroidism. Gut. 2009;58(1):149–50.
Newton JL, Pairman J, Wilton K, Jones DE, Day C. Fatigue and autonomic dysfunction in non-alcoholic fatty liver disease. Clin Auton Res. 2009;19(6):319–26.
Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–344. [PMID: 23507799]. doi:10.1038/nrgastro.2013.41 (assoc of extra hepatic).
Lonardo A, Sookoian S, Chonchol M, Loria P, Targher G. Disease—atherosclerosis as a major player in the natural course of NAFLD. Curr Pharm Des. 2013;19:5177–5192. [PMID: 23432668]. doi:10.2174/13816128130301 (assoc of extra hepat).
Vanni E, Bugianesi E, Kotronen A, De Minicis S, Yki-JärvinenH, Svegliati-Baroni G. From the metabolic syndrome to NAFLD or vice versa? Dig Liver Dis. 2010;42:320–330. [PMID: 20207596]. doi:10.1016/j.dld.2010.01.016.
Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10(6):646–50. doi:10.1016/j.cgh.2011.12.039 (Epub 2012 Jan 13).
Svane MS. Madsbad S1. Bariatric surgery— effects on obesity and related co-morbidities. Curr Diabetes Rev. 2014;10(3):208–14.
Raghow R. Bariatric surgery-mediated weight loss and its metabolic consequences for type-2 diabetes. World J Diabetes. 2013;4(3):47–50. doi:10.4239/wjd.v4.i3.47.
Mattar SG, Velcu LM, Rabinovitz M, et al. Surgically-induced weight loss significantly improves nonalcoholic fatty liver disease and the metabolic syndrome. Ann Surg. 2005;242:610–7.
Barker KB, Palekar NA, Bowers SP, Goldberg JE, Pulcini JP, Harrison SA. Non-alcoholic steatohepatitis: effect of Roux-en-Y gastric bypass surgery. Am J Gastroenterol. 2006;101:368–73.
Younossi ZM1, Stepanova M, Negro F, Hallaji S, Younossi Y, Lam B, Srishord M. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine (Baltimore). 2012;91(6):319–27. doi:10.1097/MD.0b013e3182779d49.
Chehreh M, Vahedi M, Pourhoseingholi M, Ashtari S, Khedmat H, Amin M, et al. Estimation of diagnosis and treatment costs of non-alcoholic fatty liver disease: a two-year observation. Hepat Mon. 2013;13(5):e7382. doi:10.5812/hepatmon.7382.
Rogoff K. The purchasing power parity puzzle. J Econ Lit. 1996. 34 (2): 647–668. http://www.jstor.org/stable/2729217.
The United States Medicare Program-obtained from the world wide web at http://www.benefits.gov/benefits/benefit-details/598. Accessed 8 Feb 2015.
Martini EM, Garrett N, Lindquist T, Isham GJ. The boomers are coming: a total cost of care model of the impact of population aging on health care costs in the United States by Major Practice Category. Health Serv Res. 2007;42(1 Pt 1):201–18.
Davis GL, Roberts WL. The healthcare burden imposed by liver disease in aging Baby Boomers. Curr Gastroenterol Rep. 2010;12(1):1–6. doi:10.1007/s11894-009-0087-2.
Garrett N, Martini EM. The boomers are coming: a total cost of care model of the impact of population aging on the cost of chronic conditions in the United States. Dis Manag. 2007;10(2):51–60.
Frith J, Day CP, Henderson E, Burt AD, Newton JL. Nonalcoholic fatty liver disease in older people. Gerontology. 2009;55:607–613. [PMID: 19690397]. doi:10.1159/000235677.
Koehler EM, Schouten JN, Hansen BE, van Rooij FJ, Hofman A, Stricker BH, Janssen HL. Prevalence and risk factors of non-alcoholic fatty liver disease in the elderly: results from the Rotterdam study. J Hepatol. 2012;57:1305–1311 [PMID: 22871499]. doi:10.1016/j.jhep.2012.07.028.
Wang Z, Xu M, Peng J, Jiang L, Hu Z, Wang H, Zhou S,Zhou R, Hultström M, Lai EY. Prevalence and associated metabolic factors of fatty liver disease in the elderly. Exp Gerontol. 2013;48:705–709. [PMID: 23721951]. doi:10.1016/j.exger.2013.05.059.
Bertolotti M, Lonardo A, Mussi C, Baldelli E, Pellegrini E, Ballestri S, Romagnoli D, Loria P. Nonalcoholic fatty liver disease and aging: epidemiology to management. World J Gastroenterol. 2014;20(39):14185–204. doi:10.3748/wjg.v20.i39.14185.
Baumeister SE, Volzke H, Marschall P, John U, Schmidt CO, Flessa S, et al. Impact of fatty liver disease on health care utilization and costs in a general population: a 5-year observation. Gastroenterology. 2008;134:85–94.
Younossi ZM1, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2015.
Younossi ZM, Zheng L, Stepanova M, Venkatesan C, Mishra A. Clinical outcomes and resource utilisation in Medicare patients with chronic liver disease: a historical cohort study. BMJ Open. 2014;4(5):e004318.
Whalley S, Puvanachandra P, Desai A, Kennedy H. Hepatology outpatient service provision in secondary care: a study of liver disease incidence and resource costs. Clin Med. 2007;7(2):119–24.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, Clegg AJ. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13(41):1–190, 215–357, iii–iv. doi:10.3310/hta13410.
Loveman E, Frampton GK, Shepherd J, Picot J, Cooper K, Bryant J, Welch K, Clegg A. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol Assess. 2011;15(2):1–182. doi:10.3310/hta15020.
Barshop NJ, Sirlin CB, Schwimmer JB, Lavine JE. Review article: epidemiology, pathogenesis and potential treatments of paediatric non-alcoholic fatty liver disease. liment. Pharmacol Ther. 2008;28(1):13–24. doi:10.1111/j.1365-2036.2008.03703.x (Epub 2008 Apr 4).
Dan AA, Kallman JB, Wheeler A, Younoszai Z, Collantes R, Bondini S, Gerber L, Younossi ZM. Health-related quality of life in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2007;26(6):815–20.
Afendy A, Kallman JB, Stepanova M, Younoszai Z, Aquino RD, Bianchi G, Marchesini G, Younossi ZM. Predictors of health-related quality of life in patients with chronic liver disease. Aliment Pharmacol Ther. 2009;30(5):469–76. doi:10.1111/j.1365-2036.2009.04061.x (Epub 2009 Jun 9).
David K, Kowdley KV, Unalp A, Kanwal F, Brunt EM, Schwimmer JB, NASH CRN Research Group. Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49(6):1904–12. doi:10.1002/hep.22868.
Newton JL, Jones DE, Henderson E, Kane L, Wilton K, Burt AD, Day CP. Fatigue in non-alcoholic fatty liver disease (NAFLD) is significant and associates with inactivity and excessive daytime sleepiness but not with liver disease severity or insulin resistance. Gut. 2008;57(6):807–13. doi:10.1136/gut.2007.139303 (Epub 2008 Feb 12).
Elliott C, Frith J, Day CP, Jones DE, Newton JL. Functional impairment in alcoholic liver disease and non-alcoholic fatty liver disease is significant and persists over 3 years of follow-up. Dig Dis Sci. 2013;58(8):2383–91. doi:10.1007/s10620-013-2657-2 (Epub 2013 Apr 23).
Hickman IJ, Jonsson JR, Prins JB, Ash S, Purdie DM, Clouston AD, Powell EE. Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life. Gut. 2004;53(3):413–9.
Weinstein AA, Kallman Price J, Stepanova M, Poms LW, Fang Y, Moon J, Nader F, Younossi ZM. Depression in patients with nonalcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics. 2011;52(2):127–32. doi:10.1016/j.psym.2010.12.019.
Surdea-Blaga T, Dumitraşcu DL. Depression and anxiety in nonalcoholic steatohepatitis: is there any association? Rom J Intern Med. 2011;49(4):273–80.
Stewart K, Levenson J. Psychological and psychiatric aspects of treatment of obesity and nonalcoholic fatty liver disease. Clin Liver Dis. 2012;16:615–29.
Mavrogiannaki AN, Migdalis IN. Nonalcoholic fatty liver disease, diabetes mellitus and cardiovascular disease: newer data. Int J Endocrinol 2013;2013:450639. [PMID: 23653642]. doi:10.1155/2013/450639.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. [PMID: 21295846]. doi:10.1016/S0140-6736(10)62037-5.
Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–344. [PMID: 23507799]. doi:10.1038/nrgastro.2013.41.
Lonardo A, Sookoian S, Chonchol M, Loria P, Targher G. Cardiovascular and systemic risk in nonalcoholic fatty liver disease—atherosclerosis as a major player in the natural course of NAFLD. Curr Pharm Des. 2013;19:5177–5192. [PMID: 23432668]. doi:10.2174/13816128130301.
Vanni E, Bugianesi E, Kotronen A, De Minicis S, Yki-Järvinen H, Svegliati-Baroni G. From the metabolic syndrome to NAFLD or vice versa? Dig Liver Dis. 2010;42:320–330. [PMID: 20207596]. doi:10.1016/j.dld.2010.01.016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved through our institutional review board and is in full compliance with all ethical standards regarding secondary data research. In addition, no external funding was received for this study; only internal funds were used. Zobair Younossi, MD is a consultant to Abbvie, Gilead, BMS, Intercept and GSK. Linda Henry PhD has any conflicts of interest to report.
Author contributions
Both authors shared responsibility for the development and writing of this manuscript. Dr. Zobair Younossi is the guarantor for the overall content.
Rights and permissions
About this article
Cite this article
Younossi, Z.M., Henry, L. Economic and Quality-of-Life Implications of Non-Alcoholic Fatty Liver Disease. PharmacoEconomics 33, 1245–1253 (2015). https://doi.org/10.1007/s40273-015-0316-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-015-0316-5