Abstract
In Canada, there are two separate review processes for the public reimbursement of drugs: one for cancer drugs (originally called the Joint Oncology Drug Review [JODR] and now called the pan-Canadian Oncology Drug Review [pCODR]) and one for drugs in all other disease areas (called the Common Drug Review). We explore whether a justification that is derived from an economic perspective has been provided, in Canada or elsewhere, for cancer drugs to have a separate reimbursement review process (i.e. to be ‘treated separately’) relative to drugs in all other disease areas. Literature reviews and internet searches were undertaken to identify, collect and analyze relevant documents that would provide information regarding whether an economic rationale has been provided for cancer drugs to be treated separately for resource allocation purposes. Although a number of reasons for cancer drugs to be treated separately were cited both by the JODR and pCODR and in the peer-reviewed literature, a rationale derived from an economic perspective did not appear to be documented. From an economic perspective, separating cancer drugs for resource allocation purposes is likely to impede drug plan decision makers’ ability to allocate resources in a manner that maximizes the total aggregate health benefit for the population from available resources. While we acknowledge the challenges that cancer drugs pose to drug reimbursement decision makers, we suggest that separating the reimbursement review of cancer drugs requires further scrutiny.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Our review of the literature found that a justification derived from an economic perspective has not been provided for cancer drugs to be treated separately from drugs in other disease areas for resource allocation purposes. |
Separating cancer drugs may be inconsistent with an economic perspective and the associated goal of maximizing health benefits for a defined population with available resources. |
We suggest that separating the reimbursement review of cancer drugs from drugs in all other disease areas requires closer scrutiny, both in Canada and by other countries that may be considering a similar approach. |
1 Introduction
Canada is divided into ten provinces and three territories, each of which is responsible for funding and administering its own public drug plan. Individuals covered under these provincial, territorial and federal drug plans (i.e., beneficiaries) receive certain medications for free or at a subsidized cost. However, these publicly funded drug plans typically cannot afford to pay for all possible medications that are needed by beneficiaries. Consequently, drug plan decision makers must make choices regarding which drugs to fund (i.e., reimburse), for whom, at what stage of a disease, and for how long.
In 2003, the Canadian Agency for Drugs and Technologies in Health (CADTH) established the Common Drug Review (CDR) to assist Canada’s various public drug plans with the task described above. The CDR provides formulary listing (i.e., drug funding/reimbursement) recommendations to Canada’s provincial, territorial and federal (i.e., national) drug plans. All provinces except Quebec participate in the CDR process. In 2007, a group known as the Joint Oncology Drug Review (JODR) was established (and funded) by the provincial and territorial Ministries of Health. The JODR’s role was to make recommendations to Canada’s provincial and territorial public drug plans (excluding Quebec) to guide their decisions regarding the funding of new cancer drugs. The JODR review process was considered to be an interim measure (and thus was sometimes referred to as the interim JODR, or iJODR) that would be formally evaluated before a permanent, national process for the reimbursement review of cancer drugs was established. For the iJODR, the province of Ontario’s oncology drug review committee (the Committee to Evaluate Drugs/Cancer Care Ontario [CED/CCO] subcommittee) functioned as the JODR review body. In 2010, the JODR evolved into a permanent process called the pan-Canadian Oncology Drug Review (pCODR), and in 2014, the pCODR process was transferred to sit under CADTH. Thus, CADTH now has two separate processes for making recommendations regarding the reimbursement of drugs on the federal (i.e., national), provincial and territorial drugs plans: the CDR and the pCODR.
This paper seeks to explore whether a rationale derived from an economic perspective has been presented to justify why having two separate drug reimbursement review processes, one for cancer drugs and one for drugs in all other disease areas, is better than having one review process for all drugs for resource allocation purposes (i.e., better able to achieve the commonly cited goal of maximizing benefits for the population with available resources). In doing so we ask the following questions:
-
1.
Was a justification that is derived from an economic perspective provided by the JODR or pCODR for cancer drugs to have a separate reimbursement review process (i.e., to be ‘treated separately’) from drugs in all other disease areas for resource allocation purposes?
-
2.
Does justification that is derived from an economic perspective exist in the peer-reviewed literature for cancer drugs to be treated separately from drugs in other disease areas for resource allocation purposes?
-
3.
Is there another healthcare system in the world where cancer drugs are treated separately from drugs in other disease areas for resource allocation purposes, and was a justification that is derived from an economic perspective provided for this separate treatment?
This paper focuses primarily on the JODR. We expected that a rationale for cancer drugs to be treated separately (even if not derived from an economic perspectiveFootnote 1) would have been provided by the JODR since it was the first incarnation of a national, cancer-specific drug reimbursement review body in Canada. However, given that the JODR ultimately evolved into the pCODR, we also explored (and address in the methods and discussion sections) whether the pCODR provided any such rationale.
The next section describes why we chose an economic perspective for addressing the stated questions. The research method for answering each question is subsequently outlined, followed by a summary and discussion of our findings.
2 Use of an Economic Framework
Economics is a discipline that studies how to allocate scarce resources in order to best achieve the stated goals defined, for example, by decision makers. Economics is based on three fundamental concepts: scarcity (whatever resources are available, they are insufficient to support all possible activities); choices (because resources are scarce, we must choose between different ways of using them) and opportunity cost (by choosing to use resources in one particular way, we forego other opportunities to use the same resources in other ways).
Although economics is just one perspective that could be used to address the questions in this paper, we suggest that it is an appropriate perspective for a number of reasons. First, the very nature of the task with which the JODR/pCODR and provincial drug reimbursement decision makers are involved is one of allocating scarce resources, and economics is a discipline that studies how to allocate scarce resources in order to best achieve decision makers’ goals. Second, the JODR used and the pCODR uses cost-effectiveness analysis (CEA) as a key component of its reimbursement review process. The underlying premise of CEA is that the goal of society or decision makers is to maximize the total aggregate health benefit conferred to a population for a given level of resources [1–4]. The CDR and JODR’s/pCODR’s use of CEA therefore appears to recognize the relevance of applying economics to inform resource allocation decisions. Third, the pCODR states that: “The pCODR process also ensures that scarce health-care resources are used to fund the most effective cancer drugs” [5]. This statement is consistent with the economic perspective, because it recognizes that resources are scarce and that choices need to be made regarding how to allocate resources (i.e., regarding which drugs to fund).
In addressing our research questions, we were searching for arguments describing how having two separate drug reimbursement review processes (one specifically for cancer drugs) is better able to achieve the goal of maximizing health benefits with available resources than having a single reimbursement review process for drugs in all disease areas. Because, as described in detail elsewhere [1, 6–9], efficiency and equity are inextricably linked, we also included any arguments that invoked equity considerations.
3 Methods
For all three questions, the PubMed database was used to identify peer-reviewed publications, with literature searches limited to English-language articles published from January 1, 2000 to October 31, 2014. We also searched the internet for questions #1 and #3 (but not for #2 because it was specific only to the peer-reviewed literature). Relevant published articles were read in full by one reviewer, and references from relevant articles were also scanned to see if they contained information related to the research questions.
3.1 Question #1
(a) Peer-Reviewed Literature Search:
The following search terms and strategy were used:
-
(Joint oncology drug review) OR JODR
Articles were considered relevant for full review if they discussed the establishment of the JODR in any way. Of the 116 abstracts identified using PubMed, none described the establishment of the JODR and, hence, none were deemed relevant for review.
(b) Grey Literature Search:
The terms ‘JODR’ and ‘Joint oncology drug review’ were searched using the Google search engine. To be as broad as possible in this search, materials identified on the internet were deemed relevant if they were written by the JODR and described the JODR in any context. Four documents were deemed relevant for review [10–13]. Although not available on the internet, a presentation given in 2010 at a stakeholder meeting organized by the JODR [14] was also included.
As noted earlier, we subsequently explored whether the pCODR provided a rationale for the separation of cancer drugs for resource allocation purposes. We address this question further in the discussion section.
3.2 Question #2
The following search strategy was used:
-
[(oncology OR cancer) AND (reimbursement OR resource allocation)] OR [(oncology OR cancer) AND (formulary OR funding)] OR [(oncology OR cancer) AND (priority-setting OR priority setting)]
Search terms used in combination with (oncology OR cancer) were limited to abstract/title. Articles were considered to be relevant for full review if they discussed: (1) why cancer should be given special consideration relative to other disease areas or (2) separating cancer from other disease areas for resource allocation purposes. Of the 1,740 abstracts identified, 33 references were deemed relevant for full review.
3.3 Question #3
(a) Peer-reviewed literature search: The same search strategy used for question #2 was used for question #3. Articles were considered to be relevant for full review if they discussed resource allocation systems for cancer drugs in countries outside of Canada. Relevant articles were then reviewed in full to see if any rationales for the separate treatment of cancer were provided. Of the 1,740 abstracts identified, 11 were deemed relevant for full review and another five papers were identified from the reference lists of these articles.
(b) Internet search: using the Google search engine, we searched for any examples of other healthcare systems where cancer drugs are treated separately for resource allocation purposes (using the same search terms as applied for the peer-reviewed literature search). Materials identified through the internet search were again deemed relevant if they discussed resource allocation systems or reimbursement mechanisms for cancer drugs in countries outside of Canada. These materials were reviewed in full to see if cancer had been given a separate review process and, if so, whether a justification for this separate treatment had been provided.
4 Findings
4.1 Question #1
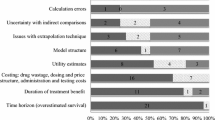
While the JODR cited various reasons for separating cancer drugs from drugs in other disease areas for resource allocation purposes (see Appendix Table 1, electronic supplementary material [ESM]), the focus of our paper was to determine whether any reasons that are derived from an economic perspective (and consistent with the goal of maximizing health benefits with available resources) were provided. Overall, a rationale derived from an economic perspective was not provided by the JODR. We briefly explore some of the rationales provided by the JODR below.
4.1.1 Differences Across Provinces in Structures, Processes and Requirements
The JODR highlighted interprovincial differences in structures, pharmacoeconomic requirements and review processes for cancer drug reimbursement as a rationale for its establishment [11]. However, the JODR did not explain why, from an economic perspective, these differences justify a separation reimbursement review system for cancer drugs.
4.1.2 Different Reimbursement Status and Reimbursement Criteria Across Provinces
The JODR cited “different coverage in each jurisdiction” [10–12] and “variation and inconsistency in coverage criteria across jurisdictions” [13] as reasons for its establishment. The JODR also stated that the (JODR) initiative was a first step towards building a national cancer drug review process that would support “a more consistent standard of therapy” [10–12]. Establishing consistency across provinces in the drugs that are reimbursed and in the reimbursement criteria for these drugs is an equity criterion that, if specified by decision makers, can be incorporated into the resource allocation task as a constraint (assuming the criterion is clearly defined and operationalized). However, the JODR did not provide an explanation that is derived from an economic perspective to explain how this justifies a separate reimbursement review process for cancer drugs.
4.1.3 Budget Impact of Cancer Drugs
Under the theme of budget impact, various reasons for the establishment of the JODR were provided, including the high prevalence of cancer, the rapid emergence of new cancer drugs, the increasing use of cancer drugs, and the high cost of new cancer drugs [10–14]. However, the JODR did not offer an explanation that is derived from an economic perspective for why budget impact justifies a separate reimbursement review body for cancer drugs.
4.2 Question #2
Additional reasons have been provided in the peer-reviewed literature for why cancer drugs should be considered separately from drugs in other disease areas for resource allocation purposes (see Appendix Table 2, ESM). However, these reasons were generally part of broader discussions related to orphan drugs, with cancer drugs being used as examples or case studies. Therefore, these rationales would not necessarily be specific only to cancer drugs. Nonetheless, we briefly address two of these rationales below.
4.2.1 Clinical Evidence Expectations of Reimbursement Review Bodies are Not Appropriate for Cancer Drugs
Some authors have noted that the evidence required by reimbursement review bodies is not available for cancer drugs due to the design of clinical trials for cancer drugs [15, 16]. For example, because cancer can be immediately life-threatening and because there are a lack of treatment options for many types of cancer, early trial results are often used to inform clinical practice. Furthermore, while elements such as surrogate endpoints and cross-over trial designs are often used to ensure that a drug’s benefit (or lack thereof) can be detected early, the validity of these surrogate endpoints as meaningful predictors of clinical benefit is often challenged by reimbursement decision makers. However, an argument derived from an economic perspective for why a discrepancy between the level of evidence generated in clinical trials of cancer drugs and the level of evidence expected by reimbursement decision makers justifies a separate reimbursement review process for cancer drugs is not provided.
4.2.2 Society or the Decision Maker May Place a Higher Value on Health Gains in Cancer Than on Health Gains in Other Disease Areas
It has been posited that society may place a higher value on health gains in cancer than on health gains in other disease areas [17]. If true, special consideration might be warranted to ensure that the benefits derived from cancer drugs are valued properly within the economic analysis framework. However, even if this preference existed, a single reimbursement review system for all disease areas could incorporate the preference into the resource allocation decision-making task by valuing (i.e., weighting) the health gained and foregone by cancer patients differently from the health gained and foregone by patients in other disease areas.
4.3 Question #3
Overall, our literature search did not identify another country where cancer drugs are treated separately for resource allocation purposes and where a rationale that is derived from an economic perspective is provided for such separation. For example, we identified a few countries where a separate budget was set aside for cancer drugs (e.g., Denmark, Belgium, and the UK cancer drugs fund—see Appendix Table 3, ESM). However, an economically derived rationale to justify these separate budgets was not provided. We also identified a few countries where special consideration is incorporated into drug reimbursement decision-making based on specific drug or disease characteristics such as disease severity (Norway, Sweden), [18] prognosis (National Institute for Health and Clinical Excellence [NICE]), [19] need for and cost of drugs (France), [20] or chronicity of illness (Portugal, Greece, Finland, Ireland) [20]. However, while cancer drugs may qualify for special consideration as a result, this special consideration is not specific only to cancer drugs. For example, the UK’s NICE has a separate set of criteria that are applied to end-of-life drugs (including higher incremental cost-effectiveness ratios [ICERs]). However, the criteria are not specific only to cancer drugs and the criteria do not represent an entirely separate reimbursement review process. Rather, they are criteria that are to be used in order to “ensure that the Appraisal Committees fully consider all the benefits which it is appropriate to take into account in appraising treatments designed to extend life” [19] while still reviewing drugs for all disease areas under the same process.
5 Discussion
Reimbursement of cancer drugs is a subject of increasing interest, both in Canada and in other countries around the world. As noted by Mittmann et al. [16], “there has been a great deal of discussion within the health technology assessment community about whether cancer should be treated as a special case, which implies that the agents used to treat cancer need to be evaluated differently from other health care technologies”. To the best of our knowledge, Canada is the first (and appears to be the only) country where a separate reimbursement review process for cancer drugs has been established. However, we did not identify a publicly documented explanation that would justify (from an economic perspective) a separate drug reimbursement review process for cancer drugs.
While not the subject of all our original questions, we also explored whether the pCODR provided any rationale for the separation of cancer drugs for resource allocation purposes. In explaining why “a separate system is needed to review cancer drugs”, the pCODR stated the following:
-
With the increasing use of cancer therapies and the rapid introduction of new, high-cost cancer drugs, provinces and territories require rigorous reviews of the clinical effectiveness and cost-effectiveness of these therapies.
-
The Common Drug Review (CDR) focuses its work primarily on drugs used in a community-based setting. The pCODR process evaluates cancer drugs across the health care spectrum, for both in-hospital treatments and community-based treatments, because this is the nature of cancer care today.
-
The pCODR process is able to capitalize on the existing strengths of the cancer care system, including the strong culture of collaboration and the use of evidence to help guide decision-making [21].
The first rationale above is similar to the budget impact rationale given by the JODR, and, as we discuss in our results section, is not derived from an economic perspective. The latter two rationales are similarly not derived from such a perspective. Furthermore, both of the latter two rationales describe challenges or opportunities that could be addressed by modifying the CDR process: they do not justify the separate treatment of cancer drugs.
From an economic perspective, the establishment of the JODR/pCODR process does not seem to be justifiable. Separating the reimbursement review of cancer drugs from drugs in all other disease areas prevents reimbursement review committees from evaluating cancer drugs within the context of all possible uses of drug budget resources. This interferes with their ability to determine what drugs (from among all possible drug options) will, if reimbursed, confer the maximum aggregate health benefits for the population. Consequently, if provincial drug plan decision makers follow the JODR/pCODR recommendations, they may end up reimbursing drugs that confer fewer health benefits with available resources relative to other (non-cancer) drugs that are competing for the same (scarce) drug budget dollars. Thus, based on an economic perspective, separating the reimbursement review of cancer drugs may do more harm than good because it may ultimately reduce the total aggregate health benefits that are gained for the defined population. Moreover, the increased overhead resulting from operating two separate reimbursement review processes may also reduce the aggregate population health benefits.
Reviewing cancer drugs separately may also disadvantage cancer drugs. For example, assume a situation where some new cancer drugs confer more health benefits for a given level of resources than new drugs in other disease areas. In this case, if cancer drugs are treated separately (and such that they are eligible only for funds allocated separately for cancer drugs), then a non-cancer drug may get reimbursed (from the budget allocated to all other drugs) even though there is a cancer drug that offers more benefits for the same level of resources.
A potential criticism of this paper is that an economic perspective is not an appropriate perspective through which to address the questions raised in this paper. However, we suggest that an economic perspective is an appropriate perspective to use for a number of reasons, which are described in the Introduction. Furthermore, while it might be argued that there are other reasons justifying a separate reimbursement review system for cancer drugs, the JODR/pCODR’s use of economic tools such as CEA to guide its recommendations suggests that the reason for having a separate process should also be derived from (and, at least, not in contradiction to) this approach.
Although we question the justification for the establishment of the JODR and pCODR, we also acknowledge that there are considerable challenges associated with managing the reimbursement of cancer drugs. There has been a rapid emergence of new drugs to treat various forms of cancer, many of these drugs are associated with a high cost, and there is a high prevalence of cancer in Canada and around the world. As such, further consideration regarding how to best manage cancer drugs in an environment of resource scarcity is both warranted and needed.
Finally, the question of how to manage the reimbursement of cancer drugs is increasingly a subject of discussion and debate, both in Canada and internationally. The JODR/pCODR process may therefore set a precedent for cancer drug reimbursement decision-making in other countries. As such, we suggest that the questions addressed in our paper are important and highly relevant not only for Canadians, but also for the international drug reimbursement decision-making community.
6 Conclusion
Our review of the literature found that a justification derived from an economic perspective has not been provided for cancer drugs to be treated separately from drugs in other disease areas for resource allocation purposes. In fact, separating cancer drugs may be inconsistent with an economic perspective and the goal of maximizing health benefits for a defined population with available resources. Based on these findings, we suggest that separating the reimbursement review of cancer drugs from drugs in all other disease areas requires closer scrutiny, both in Canada and by other countries that may be considering a similar approach.
Notes
In this paper we included all rationales given for cancer drugs to be treated separately from drugs in other disease areas for resource allocation purposes and then appraised whether any of these rationales were derived from an economic perspective.
References
Gafni A, Birch S. Incremental cost-effectiveness ratios (ICER): the silence of the lambda. Soc Sci Med. 2006;62:2091–100.
Gold MR, Siegel JE, Russel LB, Weinstein MC (eds) Cost-effectiveness in health and medicine. 1996. New York: Oxford University Press.
National Institute for Clinical Excellence. Guide to the methods of technology appraisal. http://www.nice.org.uk/niceMedia/pdf/TAP_Methods.pdf. Accessed 19 Aug 2013.
Weinstein MC, Stason WB. Foundations of cost effectiveness analysis for health and medical practices. N Engl J Med. 1977;296:716–21.
Pan-Canadian Oncology Drug Review. Frequently Asked Questions about the pCODR. n.d. http://www.pcodr.ca/wcpc/portal/Home/General_PC/FAQs?_afrLoop=25145554173000&_afrWindowMode=0&_adf.ctrl-state=181u3zxy2t_477. Accessed 14 Aug 2013.
Birch S, Gafni A. On being NICE in the UK: guidelines for technology appraisal for the NHS in England and Wales. Health Econ. 2002;11:185–91.
Gafni A, Birch S. Equity considerations in utility-based measures of health outcomes in economic appraisals: an adjustment algorithm. J Health Econ. 1991;10:329–42.
Mooney G. Economics, Medicine and Health Care. Brighton: Wheatsheaf Books; 1986.
Le Grand J. Equity and choice: an essay in economics and applied philosophy. London: Harper Collins; 1991.
Joint Oncology Drug Review. April 2008 JODR Newsletter. 2008. http://www.myelomacanada.ca/docs/jodr%20newsletter%20april%202008.pdf?LanguageID=EN-US. Accessed 21 Aug 2013.
Joint Oncology Drug Review. July 2008 JODR Newsletter. 2008. http://www.myelomacanada.ca/docs/jodr%20newsletter%20july%202008.pdf?LanguageID=EN-US. Accessed 21 Aug 2013.
Joint Oncology Drug Review. Fall 2008 JODR Newsletter. 2008. Private Communication from the Industry Oncology Working Group.
Koester O. P/T Oncology Collaborative Initiative (Joint Oncology Drug Review), Canadian Association for Healthcare Reimbursement Meeting. 2008. http://www.cahrp.ca/resources/WRM-OlafKoester.pdf. Accessed 21 June 2010.
Wilson K, Koester O. Pan-Canadian Oncology Drug Review. Presentation given at pCDOR Stakeholder Sessions meeting on January 21, 2010. 2010. Private communication from Heather McDonald, obtained via attendance at Stakeholder Session meeting.
Drummond M, Evans B, LeLorier J, Karakiewicz P, Martin D, Tugwell P, MacLeod S. Evidence and values: requirements for public reimbursement of drugs for rare diseases: a case study in oncology. Can J Clin Pharmacol. 2009;16(2):e273–81.
Mittmann N, Evans WK, Rocchi A, Longo CJ, Au H-J, Husereau D, Leighl N, Isogai P, Krahn M, Peacock S, Marshall D, Coyle D, Malfair Taylor SC, Jacobs P, Oh PI. Addendum to CADTH’s Guidelines for the Economic Evaluation of Health Technologies: Specific Guidance for Oncology Products. 2009. http://www.cadth.ca/media/pdf/H0405_Guidance_for_Oncology_Prodcuts_gr_e.pdf. Accessed 5 June 2013.
Drummond M, Wilson DA, Kanavos P, Ubel P, Rovira J. Assessing the economic challenges posed by orphan drugs. Int J Technol Assess Health Care. 2007;23(1):36–42.
Mason A, Drummond MF. Public funding of cancer drugs: is NICE getting nastier? Eur J Cancer. 2009;45:1188–92.
National Institute for Health and Clinical Excellence. Appraising life-extending, end of life treatment. July 2009. http://www.nice.org.uk/guidance/gid-tag387/resources/appraising-life-extending-end-of-life-treatments-paper2. Accessed 1 Oct 2014.
Martikainen J, Rajaniemi S. Drug reimbursement systems in EU Member States, Iceland and Norway. 2002. http://helda.helsinki.fi/bitstream/handle/10138/13932/Drug_reimbursement.pdf?sequence=1. Accessed 7 Feb 2011.
Pan-Canadian Oncology Drug Review. Frequently asked questions about the pCODR. n.d. http://www.pcodr.ca/wcpc/portal/Home/General_PC/FAQs?_afrLoop=2334522631803000&_afrWindowMode=0&_adf.ctrl-state=yuukazrq2_4#q4. Accessed 3 Aug 2013.
Acknowledgements
Dr. Heather McDonald was responsible for conception and planning of the work that led to this paper and for preparing the draft and final submitted version of this paper. Drs. Charles, Elit and Gafni were responsible for conception and planning of the work that led to this paper and for critical revision of the manuscript for important intellectual content. No funding was received by any of the authors for the preparation of this paper. Heather McDonald is employed by Bayer Inc., but the work on this paper was part of a PhD dissertation. This paper was not seen by Bayer Inc. personnel, and Bayer Inc. did not have input on the content of this paper.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material [ESM].
Rights and permissions
About this article
Cite this article
McDonald, H., Charles, C., Elit, L. et al. Is There an Economic Rationale for Cancer Drugs to Have a Separate Reimbursement Review Process for Resource Allocation Purposes?. PharmacoEconomics 33, 235–241 (2015). https://doi.org/10.1007/s40273-014-0238-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0238-7