Abstract
Objective
To assess patient preferences for psoriasis treatment features and to investigate the heterogeneity of preferences among patients with different socio-demographic and disease-related characteristics.
Methodology
A discrete choice experiment was conducted on adult patients with moderate to severe plaque-type psoriasis during a routine visit to their physician at 15 centres in Italy. We investigated the preferences of patients with respect to five treatment attributes: (1) mode and frequency of administration; (2) time to improvement; (3) time free of symptoms; (4) unintended life expectancy reduction resulting from treatment; and (5) monthly treatment cost. The heterogeneity of preferences was investigated in a mixed logit model with normally distributed random coefficients.
Results
Overall, patients preferred the subcutaneous or intravenous route of administration (versus oral administration) and treatments that took less time to show improvement, ensured a longer time free of symptoms, involved a lesser reduction in life expectancy and had lower costs. There was significant preference heterogeneity for all attributes. The cost attribute was found to be significantly more important to females and to older patients (above 60 years of age). Older patients placed significantly greater emphasis on reduced life expectancy, whereas the time free of symptoms was significantly less important to them than to patients under 60 years of age. Patients with higher scores on the Dermatology Life Quality Index (DLQI) placed higher value on the time free of symptoms than those with lower DLQI scores. For the overall sample, the marginal willingness to pay (WTP) for a month’s reduction in the time to improvement was €32.4, whereas the WTP for one additional month without symptoms was significantly higher (€68.2).
Conclusion
Patient-centred policies should consider the heterogeneity of patients’ expectations to identify individualized treatments that would aid in optimizing patient satisfaction and wellbeing, as well as overall treatment effectiveness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Investigating the heterogeneity of patients’ preferences is key for defining patient-centred policies
Psoriasis patients give different importance to different treatment characteristics, according to their sex, age and disease-related quality of life
Identifying treatments in line with patient expectations could produce greater wellbeing and improve health outcomes
1 Introduction
For an increasing number of medical conditions, multiple therapeutic options are available, and there are no obvious choices. In such situations, decision making is based on multiple criteria and involves weighting various expected clinical effects, convenience of administration and possibly costs that are often highly uncertain at the individual level. Some of these criteria are genuinely clinical, as they require professional judgment regarding the use of the most recent scientific evidence for each patient. However, the relative importance of other criteria varies across patients, as they depend on individual preferences. Uncovering these preferences is essential for informing patient-centred policies for all diseases but appears to be particularly important for chronic conditions that require patients’ commitment to their management, with important long-term consequences for their personal and social life. Psoriasis may be considered a paradigmatic example in this respect. Several treatment options are now available for psoriasis, including phototherapy, topical therapies, oral medications and biological treatments. However, these treatments vary significantly in terms of efficacy and toxic effects [1], which may explain why patients report high levels of dissatisfaction with therapies [2, 3] and present low levels of adherence [4, 5].
If it is impossible or undesirable to identify optimal strategies for all patients according to their observable clinical characteristics, at least two major issues deserve attention. The first issue concerns patient participation in decision making and the manner in which it can be effectively enhanced [6, 7]. The second issue concerns the methods that are used to investigate patient preferences to support decision making. The present paper focuses on this second issue, as we have employed discrete choice experiment (DCE) methodology to investigate the preferences of a heterogeneous group of patients for different characteristics of a hypothetical but realistic therapeutic regime for psoriasis.
In normal market situations, the preferences of patients are revealed by their choices. In healthcare, however, choices do not reflect patient preferences, because decisions regarding treatments are generally made by doctors, and patient expenses are fully or partially covered by public or private insurers, thus eliminating or limiting the role of price. With the lack of market signals revealing preferences, techniques are employed to elicit preferences through stated decisions—that is, based on hypothetical decisions that can provide information on the intentions of patients. Contingent valuation (CV) and DCE are the most frequently used stated preference techniques in healthcare. These techniques differ in that CV questions directly ask about the willingness of individuals to pay for (or the willingness to accept) treatments (or cessation of treatments), whereas DCE asks individuals to choose between alternative scenarios of treatment characteristics, possibly including price [8]. DCE has the advantage of allowing a breakdown of the characteristics of the treatment and the determination of preferences over each attribute and over the entire treatment [9, 10].
Discrete choice experiment studies in health economics have traditionally employed probit or logit models or their random effects extension to analyse the data [11]. In this traditional framework, heterogeneity of preferences is investigated by expanding the model with interaction terms between the alternative attributes and the socio-demographic characteristics of the respondents. However, traditional models fail to take into account heterogeneity driven by unobservable personal characteristics. In order to investigate heterogeneity of preferences in a more comprehensive way, mixed logit or random parameter models have been proposed [12]. Mixed logit is an extension of the standard logit model, leading to a considerable increase in model fit and improvement in the behavioural realism of the results [13]. The key feature of this model is that it allows parameters associated with DCE attributes to vary between respondents and thus accounts for heterogeneity in preferences driven by observable and non-observable characteristics. The application of mixed logit in DCE health economics studies has increased recently, and a variety of issues have been investigated using this methodological framework [13–17].
The employment of DCE for investigating preferences in psoriasis is not a novel application. Several studies have used this method to elicit the preferences of British dermatologists [18] and British [19], American [20], German [21–23] and Danish [10] psoriasis patients.
In a study with 126 British patients, Ashcroft and colleagues [19] found that risks (liver damage and skin cancer) and benefits (time to improvement and time to relapse) influenced treatment preferences greatly and that most patients would be willing to trade among characteristics of treatments. An American survey used DCE to estimate willingness to pay (WTP) for clinical benefits in terms of reductions in lesion severity and in the body surface area (BSA) covered by lesions, and revealed substantial WTP (about US$200–500 per month) for treatments that eliminated lesions [20]. The German study elicited the preferences of 163 patients and found that they were willing to accept adverse effects to obtain an increased probability and magnitude of therapeutic benefits. More surprisingly, the treatment location and method of delivery were also found to be important [21]. The importance of these process attributes of treatment suggests that personal and professional life may play a major role in determining preferences and that incorporation of preferences into clinical decision making may improve adherence and outcome.
The available empirical literature suggests that DCE is a well-established and accepted method of assessing the preferences of patients with psoriasis and that patients readily make trade-offs between treatment attributes. However, these previous studies have presented important methodological limitations in terms of generalizability of findings [19, 21–23] and the types of patients who were investigated. Given the significant differences in terms of quality-of-life reduction and psychological disability among patients with mild psoriasis compared with those who have moderate to severe forms of the disease, it is important to clearly define the sample population according to severity when investigating preferences. Localized, limited disease can typically be managed satisfactorily with topical agents. Patients with moderate to severe disease often require systemic treatment and are more likely to be candidates for innovative, expensive biological drugs [24]. Thus, investigation of patient values in this category is of particular importance in informing the decision-making process related to new treatment opportunities. Furthermore, only one previous study has used DCE methodology to assess the economic value of different treatment attributes [20]. Finally, all previous DCE studies on preferences for psoriasis treatments have used traditional modelling techniques to analyse the data (standard or random effects logit or probit models).
The current study expands the existing literature on patient preferences for psoriasis treatment and aims to overcome the identified gaps. The primary aims of the study were to assess the feasibility and validity of employing DCE in moderate and severe psoriasis patients and to evaluate the relative importance that patients associate with different treatment attributes and the economic values that they assign to these attributes. The secondary aim of the study was to explore preference heterogeneity for treatment attributes associated with both observable and non-observable patient characteristics.
2 Methods
2.1 Study Design
To reach the aforementioned objectives, a national, multicentre observational study with consecutive enrolment of patients with moderate to severe plaque-type psoriasis was conducted in Italy in late 2011. Patients with moderate to severe plaque-type psoriasis were invited to participate in a health and experimental preference elicitation survey during a routine visit to their physician at 15 centres covering the entire Italian territory (all five macro-areas: Northwestern, Northeastern, Central, Southern and Islands). A total of 300 patients were invited to participate in the survey; this number was based on the projected sample size for the experimental design and analysis plan for the data collected (see the next section). To obtain a geographically representative sample, the number of patients to be enrolled in each macro-area was calculated as a constant proportion of the resident population (using data obtained from the Italian National Institute for Statistics [ISTAT]). All centres belonged to the PSOCARE network, a national psoriasis programme under the supervision of the Italian Drug Agency (AIFA). All participants (1) were at least 18 years of age; (2) had a medical diagnosis of moderate to severe psoriasis; (3) provided informed consent; and (4) were enrolled consecutively during routine physician or hospital visits. The study was approved by the local ethics committee at each of the 15 participating centres.
2.2 Survey Instrument
Patients were asked to express their preferences for hypothetical pharmaceutical treatments for psoriasis described in terms of general attributes (Table 1). The attributes selected for the DCE were initially identified on the basis of theoretical arguments in the literature and subsequently validated during in-depth semi-structured interviews with three psoriasis specialists at a major dermatological centre in Southern Italy. The specialists reviewed the study protocol and the study instruments, including the DCE experiment. Finally, before the main study was conducted, a pilot study was performed with 10 psoriasis patients at the same centre. The main objective of the pilot study was to assess whether the patients fully understood the study design, attributes and associated levels. Furthermore, the patients were asked to express their opinion on the level of difficulty of the task, in order to assess the cognitive burden imposed on the respondents. As a result of this process, the following five attributes were included in the main study: (1) mode and frequency of therapy administration; (2) time to improvement [to obtain at least a 50 % Psoriasis Area and Severity Index (PASI) improvement]; (3) time free of symptoms; (4) reduced life expectancy; and (5) monthly treatment cost not covered by the National Health Service (NHS) (Table 1).
More specifically, the mode and frequency of therapy administration has been used as the attribute in all available DCE studies on psoriasis [10, 18–22]. PASI is a standard measure of the severity of the disease [25].
The time to obtain at least a 50 % PASI improvement was informed by the clinical endpoints commonly used in randomized clinical trials assessing the efficacy of treatments for moderate to severe plaque psoriasis [15, 17, 26–31] and two DCE studies [18, 19], and was subsequently validated by the three specialists. The levels (1, 3 and 6 months) were identified in the same process.
The time free of symptoms, i.e. the time in the remission state after achieving the PASI improvement, was identified to be an important attribute by the three psoriasis specialists, and this was subsequently confirmed by the patients. The previous DCE studies used an analogous attribute: time to relapse, defined as the time taken to lose the improvement in psoriasis obtained from the treatment after the treatment was stopped [18, 19]. In our study, we did not specify that the treatment needed to be stopped after obtaining improvement, to account for a variety of possible treatment strategies currently in use. The levels of this attribute (2, 4 and 6 months) were based on the two DCE studies and subsequent discussion with the three specialists.
The levels of monthly treatment costs (€0, €100 and €500) were first defined on the basis of previous WTP studies conducted in Germany and the USA in the area of dermatology [32–34]. The methods used to estimate WTP varied across studies. Two studies used closed-ended questions inclusive of the three values in our study (€0, €100 and €500) [32, 33]. One study elicited patients’ WTP for dermatology treatment in terms of the percentage of personal monthly income, ranging from 0 to 100 % (with the mean stated value being around 15 %) [34]. Finally, one study adopted open-ended questions, resulting in median WTP values of about €200 [33]. On the basis of these studies, we proposed the three values to the clinicians, who agreed with our choices. The values were further tested in a pilot study with 10 psoriasis patients.
Finally, reduced life expectancy was included as a comprehensive measure of possible negative side effects associated with the treatment. Other DCE studies have used more specific attributes for side effects, such as the 20-year risk of experiencing liver damage or skin cancer [18, 19] or the risk of serious lung infection [20], or have simply introduced the general term ‘side effects’ [21, 22]. We discussed these alternatives thoroughly during in-depth interviews with the three specialists, who expressed serious concerns about introducing probability terms in the study. They all agreed to include reduced life expectancy (in months) as one comprehensive measure of negative side effects that would be more easily understood by the patients. They also defined the three levels to include in the DCE (1, 2 and 3 months).
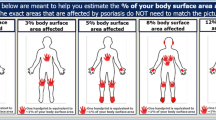
To examine the effects of respondent characteristics on preferences, the questionnaire also collected data on demographics, medical history, current and prior treatments, and disease severity (PASI and BSA covered by lesions). These data were collected directly by the psoriasis specialists involved in the study. In addition, patients were asked to complete a Dermatology Life Quality Index (DLQI) questionnaire.
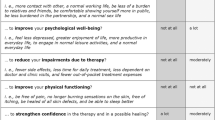
The final part of the questionnaire aimed to further explore patients’ opinion about treatment attributes. Patients were asked to express their opinions on the importance of the five attributes defined above. The levels of importance were measured on an ordinal scale from 1 to 5 (1 = absolutely irrelevant; 2 = not very important; 3 = important; 4 = very important; and 5 = the only important aspect).
2.3 Experimental Design
An experimental (fractional factorial) design is a sample from all possible combinations of attribute levels (full factorial), which is used to construct choice alternatives to be assigned in the choice sets [8]. This method identifies an efficient combination of profiles that can ensure sufficient statistical information regarding respondent preferences for treatment attributes. In our study, the experimental design was generated by SPSS 10.0 software, while considering several features to maximize statistical efficiency: strict orthogonality (independent variation of level across attributes), minimum overlap and level balance [35, 36]. An independent main effects design that was unlabelled and 100 % D efficient resulted in 27 different scenarios that were assembled in choice sets using the cyclical foldover approach. According to this method, each of the alternatives of the fractional factorial design is first allocated to different choice sets. The dimensions of the pairing alternatives are then constructed by cyclically adding alternatives into the choice set based on their attribute level. The foldover approach was used to maintain the statistical properties of the fractional factorial design. We ensured statistical efficiency by design, but we were concerned that 27 choice sets with no overlap (thus forcing respondents to trade on all dimensions at once) would demand an excessive cognitive burden and jeopardize the response efficiency. To account for this challenge, the experimental design was constrained to a maximum of four questions per patient. Twenty-seven different choice questions were randomly allocated into 27 questionnaire versions to ensure that each choice question appeared in four different questionnaire versions. As a result of this process, the projected sample size was 240 patients.
The DCE part of the survey was completed independently by the patients. Prior to completing the survey, the patients were given a thorough explanation of the DCE methodology, as well as the attributes and assigned levels, by their clinicians. All clinicians participating in the study were instructed to provide a standard set of explanations for each of the five attributes and levels, and not to interfere during the survey completion.
2.4 Model Estimation
The analysis of patient preferences is based on responses to DCE choice questions where utility is assumed to depend on the attributes of DCE. If therapy choice j is chosen, it is assumed that j yields the maximum utility between two available options. More specifically, individual i’s utility associated with therapy option j in choice situation s is:
where X ijs is a vector of the relevant attributes of therapy option j (route and administration, time to improvement, time free of symptoms, reduced life expectancy and cost); β is a vector of associated preference parameters; and ε ijs is unobservable to the researcher and treated as a random component. Assuming a specific parametric distribution of the random component allows a probabilistic analysis of individual choice behaviour.
The probability of individual i choosing alternative j in choice set s can be written as the standard logit formula:
The likelihood function is easily computed within the standard logit framework. The key feature of a mixed logit model is that it allows for variation in the coefficient values across individual respondents (while remaining constant over the choice situation for each respondent). Hence, instead of setting the parameters as fixed, the parameters are allowed to vary over individuals in the population with density f(β|θ). Since the researcher does not observe the actual tastes of the individuals, the probability becomes the integral of L is over all possible values of β, weighted by the density chosen (usually, normal or log-normal). The unconditional probability of the observed sequence of choices for a given choice set s is obtained by:
By specifying a distribution for the β parameters, θ can be estimated through a simulated maximum likelihood procedure. In our case, a simulated maximum likelihood estimator was used to estimate the mixed logit model with 500 Halton draws. The output of a mixed logit model includes the means and standard deviations (SDs) of random coefficients, along with their respective confidence intervals (CIs). The mean coefficients represent the relative utility of each attribute conditional on other attributes, while the SDs reflect the degree of heterogeneity among the respondents.
On the basis of this conceptual framework, we specify the utility for individual i associated with therapy option j in choice situation s as:
where Subcutquart and IVmonth are dummy variables with respect to the reference category ‘oral daily’; TTI refers to time to improvement (in months); TFree refers to time free of symptoms (in months); LEred refers to reduced life expectancy (in months); and cost is expressed in Euros. The coefficients β1 to β6 (the mean and SD) are estimated from the model.
To investigate the extent to which heterogeneity of preferences is driven by patient observable characteristics (age, sex, clinical characteristics), we extend Model 1 with a series of interaction terms between the respondents’ characteristics and attribute levels (Model 2). A likelihood ratio test is used to compare goodness of fit and to test the extended model against the restricted model with no interactions.
A pivotal issue in mixed logit models is choosing the coefficients that are allowed to vary and assigning the distributions that they can take. Since our objective was to investigate the heterogeneity of preferences for treatment features defined in the experiment, we allowed all coefficients (β1 to β6) to vary over respondents. The random coefficients are specified to be normally distributed in both models. Assigning normal distribution to coefficients has several advantages: the estimates are more easily interpreted and can be directly compared with coefficients obtained in a standard logit model. However, assigning normal distribution to coefficients for costs and for non-monetary attributes poses a challenge for the calculation of WTP. Since the WTP for an attribute is given by the ratio of the attribute coefficient to the price coefficient, the WTP from a mixed logit model is given by the ratio of two randomly distributed terms and the ratio of two normal distributions does not have defined moments [13, 37]. In addition, normal distribution of cost coefficients can lead to situations in which a proportion of patients result in coefficients with a counterintuitive sign driven by the assumption of normality. Thus, in order to estimate WTP, we estimated a mixed logit model in which the cost coefficient is fixed and we calculated the WTP for nonmonetary attributes as the ratio of the cost coefficient and mean coefficients for the attributes. The WTP for the treatment attributes was calculated in the overall sample and in patient subgroups. Subgroup analyses were performed on the basis of socio-demographic factors (sex and age) and DLQI scores (0–5 = no effect or small effect; 6–9 = moderate effect; or >10 large or extremely large effect).
The treatment choices of the respondents were explored to determine whether they showed evidence of non-trading behaviour among different treatment attributes. Patients who consistently chose an option with the ‘best’ level of the same attribute were labelled as having ‘dominant’ preferences for that attribute. We investigated the differences in patient characteristics between dominant and non-dominant individuals. We also explored differences in opinions expressed in terms of the level of importance of different attributes in the last part of the survey.
The theoretical validity of the model was tested by examining the signs and significance of coefficient estimates in relation to a priori hypotheses. Longer time to improvement, greater reduction in life expectancy and higher cost were all expected to have negative signs. A longer period of time free of symptoms was expected to have a positive sign. We had no a priori expectations of the sign related to the mode and frequency of administration.
3 Results
A total of 244 patients participated in the study by completing the survey during their regular doctor visits at 15 hospital centres. One patient did not provide answers to the DCE part and so was excluded from subsequent analysis. The study population had a mean age of 48.8 years (SD 13.9, range 18–84). The majority of patients (151, 62 %) were male, 189 (78 %) were married and 121 (50 %) were employed. The mean (±SD) age at psoriasis diagnosis was 29.5 ± 15.2 years, with 62 % of patients experiencing psoriasis onset by the age of 30 years. Of the patients, 112 (46 %) had at least one comorbidity, with the majority experiencing hypertension (22 %), followed by psoriatic arthritis (6 %). Furthermore, 85 % of the surveyed sample were using topical treatments at the time of the study, whereas a much smaller proportion (25 %) were using systemic (non-biological) treatment. Finally, 93 patients (38 %) reported that they were receiving biological treatment, while 116 (48 % of the surveyed sample) reported never having used biological therapy in the past. The average DLQI score was 9.2 (SD 7.38), with a majority of patients (68; 27.9 %) reporting that the disease severely affected their quality of life. The mean PASI score was 16.5, and the mean BSA covered by lesions was 21.8 %, reflecting the disease severity experienced by the patients included in our sample (Table 2).
3.1 DCE
The results of the two mixed logit models are presented in Table 3. In the basic model without interactions (Model 1), all attributes had coefficients that were significantly different from zero, indicating that all five attributes had a significant influence on patients’ choice of treatment. The directions of the coefficients were all in accordance with our hypotheses. The negative sign on the coefficient for time to improvement indicates that as the time to obtain at least 50 % PASI improvement increased, the patients’ likelihood of choosing this scenario decreased (β = −0.109, 95 % CI −0.194 to −0.025) Similarly, reduced life expectancy had a negative coefficient (β = −0.237, 95 % CI −0.443 to −0.032), implying that a greater reduction in life expectancy was associated with a lower probability that a treatment would be selected. As expected, the time free of symptoms resulted in a positive mean coefficient (β = 0.258; 95 % CI 0.128 to 0.288). Both the subcutaneous quarterly and intravenous monthly routes of administration were preferred to the oral daily option (both coefficients were positive and significant at the 0.05 level).
In addition to the mean coefficient estimates that reflected overall preferences, Model 1 provides insights on to what extent those preferences varied within our sample. The SDs for all five attributes resulted in statistical significance, suggesting that there was significant heterogeneity in patient preferences for all of the attributes. By looking at the magnitudes of SDs in comparison with the mean coefficients, it can be seen that the extent of this heterogeneity differed across attributes. For example, by applying the approach used by Hole [38], it can be estimated that 37.8 % of patients preferred a longer time to improvement, 32.6 % preferred a greater reduction in life expectancy and 27.4 % preferred a shorter time free of symptoms. In order to explore this heterogeneity further, we expanded Model 1 with interaction terms between attributes and policy-relevant patient characteristics: age, sex and DLQI score. The results of Model 2 suggested that elderly patients (age >60 years) put more weight on reduced life expectancy (β = −0.677; 95 % CI −1.161 to −0.194) and monthly treatment cost than younger patients did (β = −0.229; 95 % CI −0.442 to −0.013). Interestingly, older patients placed significantly less weight on the time free of symptoms than patients below 60 years of age did. The interaction term of the DLQI score with the time free of symptoms was significant and positive, suggesting that patients with a higher DLQI score (i.e. greater effects of psoriasis on the quality of life) placed more value on this attribute (β = 0.016; 95 % CI 0.001 to 0.031). Among sex interactions, only the monthly treatment cost coefficient resulted in significance (β = −0.230; 95 % CI −0.415 to −0.043), suggesting that females were more concerned with this treatment attribute than men were.
It is interesting to note that the mean coefficients and SDs for all treatment attributes remained significant in Model 2. The mean coefficients represented the mean marginal utility of each attribute for respondents in all of the omitted categories, and their significance suggests that all attributes were considered significantly important within these patient groups. The significance of the SD parameter suggests that, after controlling for age, sex and DLQI score, considerable heterogeneity in patient preferences still remained. We made an attempt to expand our model further to include additional interaction terms with other patient characteristics observed in our data (PASI, BSA covered by lesions, treatment type, presence of hypertension), but none of these resulted in significance and there was no improvement in the model fit. On the other hand, the final Model 2 significantly improved the explanatory power in comparison with Model 1 (likelihood ratio test χ2 (df 18) = 47.53, p < 0.001).
From the comparison of the magnitude of coefficients, we can derive some considerations of the relative importance of attributes. More specifically, the ratio between coefficients reveals the trade-offs that patients were willing to make among the dimensions. In particular, setting the coefficient associated with the cost dimension fixed, the WTP for changes in other attributes can be estimated. Table 4 reports mean WTP estimates for changes in other attributes in the overall sample and in groups. The groups were defined by the variables that were significant in Model 2: age, sex and DLQI score. Overall, the marginal WTP for a month’s reduction in the time to improvement was €32.4, whereas the WTP for one additional month without symptoms was significantly higher (€68.2). Reduction in life expectancy by 1 month reduced the value of psoriasis treatment by €60.2. This result shows that the duration of efficacy is the most important dimension for which patients would be willing to pay.
Significant differences in preferences across patient groups also emerged from the WTP estimates. As expected, younger patients attached significantly higher value to time spent free of symptoms (€92.3 and €11.6 for one additional month for younger and older patients, respectively). By contrast, older patients were much more concerned with reduced life expectancy; the WTP for a 1-month lesser reduction was significantly higher in this group (€132.4 versus €25.4). Conversely, younger patients placed higher value on time needed to obtain improvement (€32.4 versus €24.6). Interesting results stemmed from the WTP estimates in the three groups defined by DLQI scores, suggesting that time free of symptoms is considered significantly more important among patients with DLQI scores above 10 (a large or extremely large effect on the quality of life). In this group, the WTP for 1 month without psoriasis symptoms was €134.6 (versus €33.6 and €20.1 in the other two groups). Reduced life expectancy was of concern only in those with a DLQI score signalling a moderate effect (the WTP was €143.5 for a 1-month lesser reduction in life expectancy).
The patients’ opinions about treatment attributes were further investigated by asking them to assign levels of importance to five attributes on a scale from 1 (for an absolutely irrelevant attribute) to 5 (for the only important attribute). The results are displayed in Fig. 1. In the overall sample, time free of symptoms was the attribute with the highest mean score (3.87). This attribute was the only important aspect (with a score of 5) for a significant 17 % of the sample, and it was important or very important (with a score of 3 or 4, respectively) for 79 % of the patients. Time to improvement had the second highest mean score (3.63) for the sample, while the mean score for reduced life expectancy was only slightly lower (3.50), followed by monthly treatment cost (3.27). The patient responses revealed that the cost of therapy was important or very important to 75 % of the sample, but this attribute was the only important aspect to only 5 % of the sample.
The stratification of patients by sex revealed similar patterns in responses from males and females. Although females consistently gave higher scores to each attribute, the difference in scores was significantly different only for the time to improvement attribute. The mean scores varied substantially according to the ages of participants, with scores increasing significantly with patient age. For three of the five attributes, the level of importance significantly differed between age groups, thus substantially confirming the results from the experiment. However, despite significant age-related differences in the mean scores for each attribute, the ranking of the attributes based on these scores did not change with age. Time free of symptoms consistently had the highest score, followed by time to improvement, reduced life expectancy, monthly treatment cost, and the mode and frequency of administration—the same ranking as was observed with the entire sample. The stratification of patients by DLQI scores revealed that patients’ quality of life had a significant influence on their mean scores for almost all attributes (Fig. 1).
The analysis of dominant dimensions shows that 132 patients (54 %) preferred one attribute over the others across the choices. However, interestingly, these dominant preferences were distributed across the attributes as follows: 33 (25 %) preferred a reduced time to symptom improvement, 34 (26 %) preferred more time free of symptoms, 59 (46 %) preferred a lower cost of treatment and 25 (19 %) preferred reduced life expectancy. Some patients simultaneously expressed dominance for two dimensions. We compared the characteristics of dominant versus non-dominant individuals across variables that explained a portion of the preference heterogeneity in the mixed logit model (Table 5). As expected, there were significantly more females among dominant individuals for the cost attribute (44 versus 36 %, p = 0.002). For the dimensions time to improvement and reduced life expectancy, the non-dominant group had a higher prevalence of females, while there was no significant difference in sex composition for the time free of symptoms dimension. Furthermore, the average age of dominant individuals was significantly higher for the time free of symptoms and the cost attribute. Finally, the average DLQI score was significantly higher among dominant individuals for the time free of symptoms attribute.
In addition to patient characteristics, we further explored the expressed level of importance for five attributes among dominant and non-dominant individuals (Table 5). The results of the ranking exercise were largely coherent with the experiment results. More specifically, for all attributes except one, the mean value for the level of importance (obtained on a scale from 1 to 5) was significantly higher among dominant individuals than among non-dominant individuals. Only for time to improvement did the observed difference not reach statistical significance (3.35 versus 3.62, p = 0.107).
4 Discussion
In this study, we employed a DCE to investigate preferences for a set of attributes of treatment for psoriasis patients who were recruited at 15 centres in 10 Italian regions. The key feature of the study model is that we used a mixed logit model that allowed us to account for heterogeneity in preferences driven by observable characteristics and to test the existence of residual significant heterogeneity in non-observable characteristics.
The study findings provide evidence that the questions were understood by the patients and were not answered randomly. All coefficients had the expected signs. In addition, a WTP value of €32.4 for at least a 50 % PASI improvement has some face value, given that Italians are covered by a universal system and do not typically pay significant co-payments. Furthermore, the generally lower WTP of women and older patients appears consistent with their lower personal incomes. In addition, the much higher implied negative WTP for a life expectancy reduction of patients over 60 years is consistent with their shorter time span. Finally, the answers to the direct questions on treatment attributes provided a similar order of importance to those resulting from the DCE questions.
The most important result obtained in this study is that patients have heterogeneous preferences for treatment attributes. In the range of levels presented, more than half of the sample did not appear to use a trade-off between the attributes and stated a dominant preference for one or two of the attributes. Cost was a dominant attribute for nearly half of the sample. While this result may suggest that the chosen values for the cost attribute were too high, it also shows that patients in systems in which care is free or nearly free at the point of use are highly concerned about paying for services and may have lower WTP than patients in systems in which co-payments and full direct payments are common. In addition, approximately one third of the sample stated a dominant preference reduction for each of the following clinical effects: life expectancy; time to improvement; and time free of symptoms. Whether these dominant preferences resulted from level attributes that were not sufficiently large or from lexicographic ordering, they clearly show that patient preferences were heterogeneous, with some patients giving priority to treatments that would avoid an increased risk of mortality and others preferring treatments with long-term effects or prompt responses. Our findings provide additional evidence to that obtained in Britain [19] and Germany [21–23]. In a sample of 126 patients with moderately severe psoriasis (PASI = 11.1), the British study found that approximately one quarter of patients were not willing to trade treatment attributes and that most patients would have traded clinical benefits if the likelihood of severe adverse events were reduced. This study concluded that some patients may not accept a treatment offered to them, no matter how efficacious, if they have serious concerns about adverse effects [19]. The German study, which was based on a sample of 163 patients with rather mild psoriasis (PASI = 5.6) from one setting, presented a different picture. In that study, patients were willing to accept treatment-related adverse effects for therapeutic benefits and even to obtain better process attributes, such as a convenient location for receiving treatment [21]. Our study provides additional evidence because it is based on a larger national sample from a southern European country with patients whose disease was significantly more severe (PASI = 16.5).
There were a number of limitations in the present study, which need to be acknowledged. The first limitation concerns the forced-choice design of our study. It has been argued that forced choice (i.e. not allowing an opt-out option) can lead to biased coefficient estimates, especially when the cost attribute is used in the survey in order to estimate WTP. In fact, we had included an opt-out option in our first version of the survey, but both during the discussion with the three specialists and during the pilot study with 10 patients, we were told that adding this option would be considered by the majority of respondents as a ‘way out’ to avoid the difficult task in front of them—namely, to simultaneously trade-off on five treatment dimensions. Since there is a limit to how much information respondents can meaningfully handle while making a decision, and in order to collect the maximum information possible from the experiment, we opted not to include the third option.
Secondly, the very limited test employed in the present study for detecting dominant preferences may not have been sufficiently powerful to detect violations of the standard axioms. The significant number of dominant individuals (132, 54 %) may have been driven, at least partially, by the small number of questions that each patient answered. Thus, caution is warranted when interpreting the results on individuals resulting in dominance for one or more dimensions in the DCE. However, in our study, we could obtain additional information about the relative importance of the different dimensions. A question asking patients to rank the dimensions was included, allowing the validity of responses in the discrete choice survey to be tested. The results of the ranking exercise largely confirmed those obtained in a discrete choice framework.
The third limitation refers to our choice of empirical model. Although mixed logit models are deemed to be one of the most flexible classes of models within the random utility framework, flexibility comes at a cost. One issue concerns the choice of distribution for random coefficients. In our study, we adopted the most frequently used approach in the literature and assigned normal distributions to all model coefficients. This choice can lead to situations in which a proportion of patients result with coefficients with a counterintuitive sign driven by the assumption of normality, not by preference heterogeneity (for example, patients who prefer to pay more and wait longer for treatment to be effective). On the other hand, assigning log-normal distribution to coefficients raises problems with the WTP estimation. Empirical evidence suggests that models that are log-normally distributed produce WTP with skewed distribution (a long right-tail), and some authors have argued that this property of the distribution can cause unrealistic WTP estimates [39].
Considering our study design, one may argue that the preferences obtained in the DCE reflect differences in the patient–physician communication strategy rather than patients’ preferences for treatment outcomes per se. We attempt to control for this by providing instructions to clinicians administering the survey to give a standard set of explanations to their patients prior to completing the survey, which was done independently by the patients. However, we cannot be fully sure that the information was uniformly distributed in practice. Nevertheless, we argue that the results that were obtained still fully reflect patients’ preferences for different treatment outcomes as they may be observed in real settings. In healthcare, clinician–patient communication is an unavoidable ingredient of patients’ decision making about treatment strategies that cannot be ruled out in any study aimed at eliciting patient preferences.
Despite its limitations, we believe that our study can provide useful input to inform patient-centred policies for psoriasis treatment. Understanding that patients have different preferences is important from a clinical perspective because prescription of treatments that are suitable for individual preferences may improve adherence to treatment [40, 41]. Given the low levels of adherence to therapies, strategies to select the preferred treatment from the patient perspective are worthy of further investigation, possibly with interventional studies involving patient decision making. In addition, from an economic perspective, patients’ wellbeing results from individual tastes that cannot be easily and completely communicated to physicians; thus, a lack of adherence may be the rational response to the characteristics of treatments [42]. Therefore, enhancing the role of patients in decision making may have positive effects, as it may improve their wellbeing through better-matched outcomes and process attributes of treatments according to their individual and subjective expectations. Thus, there may be considerable value in identifying when treatments are cost effective for individual patients, given their preferences or other personal attributes [43].
The heterogeneity of preferences is partially explained by the socio-demographic characteristics of the patients. Those aged under 60 years reported a WTP for time free of symptoms that was eight times higher than that of older patients; however, patients aged over 60 years reported a WTP for reducing life expectancy that was 5 times higher. Clearly, age is a relevant determinant of the preferences expressed by patients with respect to the clinical benefits and adverse effects of treatments. Sex is relevant primarily in terms of overall WTP; for all clinical attributes, women have a lower WTP than men. Whether this finding is observed because women have a lower disposable income (and thus their opportunity cost of paying for treatment is higher), or because of sex-specific characteristics, remains a question worthy of future investigation. The role of the quality of life experienced by patients in treatment preferences is uncertain but for the length of time free of symptoms. Patients experiencing large or extremely large effects in their health-related quality of life have a WTP for time free of symptoms that is six times that of patients with no effects or small effects.
This study also investigated preferences for the mode and frequency of therapy administration. Our findings showed that patients prefer injections (intravenous monthly or subcutaneous quarterly) to oral daily administration. Although it is unclear whether this result stems from the mode of administration (which might be associated with different perceptions of treatment effects) or from the frequency of administration, there is a clear preference in favour of injection regimens, as suggested by the magnitude of WTP values.
5 Conclusion
This study provides evidence that preferences for treatments, modes of administration and costs widely vary among psoriasis patients. Segmenting patients according to socio-demographic characteristics may allow providers to ensure that treatments better match the expectations of patients. In addition, patient wellbeing may be produced by decision-making processes that incorporate their individual perspectives. Given the different risk–benefit profiles of the available treatments, efforts to take into account these preferences in clinical and policy decision making may improve patients’ adherence to therapies and increase patients’ wellbeing.
References
Fairhurst DA, Ashcroft DM, Griffiths CE. Optimal management of severe plaque form of psoriasis. Am J Clin Dermatol. 2005;6(5):283–94.
Renzi C, Picardi A, Abeni D, Agostini E, Baliva G, Pasquini P, et al. Association of dissatisfaction with care and psychiatric morbidity with poor treatment compliance. Arch Dermatol. 2002;138(3):337–42.
Zaghloul SS, Goodfield MJ. Objective assessment of compliance with psoriasis treatment. Arch Dermatol. 2004;140(4):408–14. doi:10.1001/archderm.140.4.408.
Richards HL, Fortune DG, Griffiths CE. Adherence to treatment in patients with psoriasis. J Eur Acad Dermatol Venereol. 2006;20(4):370–9. doi:10.1111/j.1468-3083.2006.01565.x.
van de Kerkhof PC, de Hoop D, de Korte J, Cobelens SA, Kuipers MV. Patient compliance and disease management in the treatment of psoriasis in the Netherlands. Dermatology. 2000;200(4):292–8. doi:18390.
Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2(2):112–21.
Coulter A. Paternalism or partnership? Patients have grown up—and there’s no going back. BMJ. 1999;319(7212):719–20.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Augustovski F, Beratarrechea A, Irazola V, Rubinstein F, Tesolin P, Gonzalez J, et al. Patient preferences for biologic agents in rheumatoid arthritis: a discrete-choice experiment. Value Health. 2013;16(2):385–93. doi:10.1016/j.jval.2012.11.007.
Kjaer T, Bech M, Gyrd-Hansen D, Hart-Hansen K. Ordering effect and price sensitivity in discrete choice experiments: need we worry? Health Econ. 2006;15(11):1217–28. doi:10.1002/hec.1117.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72. doi:10.1002/hec.1697.
McFadden D, Train K. Mixed MNL models for discrete response. J Appl Econometr. 2000;5(5):447–70.
Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ. 2008;27(4):1078–94. doi:10.1016/j.jhealeco.2007.11.006.
Hall J, Fiebig DG, King MT, Hossain I, Louviere JJ. What influences participation in genetic carrier testing? Results from a discrete choice experiment. J Health Econ. 2006;25(3):520–37. doi:10.1016/j.jhealeco.2005.09.002.
King MT, Hall J, Lancsar E, Fiebig D, Hossain I, Louviere J, et al. Patient preferences for managing asthma: results from a discrete choice experiment. Health Econ. 2007;16(7):703–17. doi:10.1002/hec.1193.
Kjaer T, Gyrd-Hansen D. Preference heterogeneity and choice of cardiac rehabilitation program: results from a discrete choice experiment. Health Policy. 2008;85(1):124–32. doi:10.1016/j.healthpol.2007.07.002.
Paterson RW, Boyle KJ, Parmeter CF, Neumann JE, De Civita P. Heterogeneity in preferences for smoking cessation. Health Econ. 2008;17(12):1363–77. doi:10.1002/hec.1336.
Ashcroft DM, Seston E, Griffiths CE. Trade-offs between the benefits and risks of drug treatment for psoriasis: a discrete choice experiment with U.K. dermatologists. Br J Dermatol. 2006;155(6):1236–41. doi:10.1111/j.1365-2133.2006.07535.x.
Seston EM, Ashcroft DM, Griffiths CE. Balancing the benefits and risks of drug treatment: a stated-preference, discrete choice experiment with patients with psoriasis. Arch Dermatol. 2007;143(9):1175–9. doi:10.1001/archderm.143.9.1175.
Hauber AB, Gonzalez JM, Schenkel B, Lofland JH, Martin S. The value to patients of reducing lesion severity in plaque psoriasis. J Dermatol Treat. 2011;22(5):266–75. doi:10.3109/09546634.2011.588193.
Schaarschmidt ML, Schmieder A, Umar N, Terris D, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: process characteristics can outweigh outcome attributes. Arch Dermatol. 2011;147(11):1285–94. doi:10.1001/archdermatol.2011.309.
Schaarschmidt ML, Umar N, Schmieder A, Terris DD, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: impact of treatment experience. J Eur Acad Dermatol Venereol. 2013;27(2):187–98. doi:10.1111/j.1468-3083.2011.04440.x.
Schmieder A, Schaarschmidt ML, Umar N, Terris DD, Goebeler M, Goerdt S, et al. Comorbidities significantly impact patients’ preferences for psoriasis treatments. J Am Acad Dermatol. 2012;67(3):363–72. doi:10.1016/j.jaad.2011.08.023.
Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, et al. British Association of Dermatologists’ guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009;161(5):987–1019. doi:10.1111/j.1365-2133.2009.09505.x.
Gelfand JM, Wan J, CallisDuffin K, Krueger GG, Kalb RE, Weisman JD, et al. Comparative effectiveness of commonly used systemic treatments or phototherapy for moderate to severe plaque psoriasis in the clinical practice setting. Arch Dermatol. 2012;148(4):487–94. doi:10.1001/archdermatol.2012.370.
Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008;371(9625):1665–74. doi:10.1016/S0140-6736(08)60725-4.
Lotti T, Chimenti S, Katsambas A, Ortonne JP, Dubertret L, Licu D, et al. Efficacy and safety of efalizumab in patients with moderate-to-severe plaque psoriasis resistant to previous anti-psoriatic treatment: results of a multicentre, open-label, phase IIIb/IV trial. Arch Drug Inf. 2010;3(1):9–18. doi:10.1111/j.1753-5174.2009.00026.x.
Barker J, Hoffmann M, Wozel G, Ortonne JP, Zheng H, van Hoogstraten H, et al. Efficacy and safety of infliximab vs. methotrexate in patients with moderate-to-severe plaque psoriasis: results of an open-label, active-controlled, randomized trial (RESTORE1). Br J Dermatol. 2011;165(5):1109–17. doi:10.1111/j.1365-2133.2011.10615.x.
Strober BE, Crowley JJ, Yamauchi PS, Olds M, Williams DA. Efficacy and safety results from a phase III, randomized controlled trial comparing the safety and efficacy of briakinumab with etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. Br J Dermatol. 2011;165(3):661–8. doi:10.1111/j.1365-2133.2011.10419.x.
Bissonnette R, Bolduc C, Maari C, Nigen S, Webster JM, Tang L, et al. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: results from a randomized double-blind placebo-controlled, phase II trial. J Eur Acad Dermatol Venereol. 2012;26(12):1516–21. doi:10.1111/j.1468-3083.2011.04332.x.
Strohal R, Puig L, Chouela E, Tsai TF, Melin J, Freundlich B, et al. The efficacy and safety of etanercept when used with as-needed adjunctive topical therapy in a randomised, double-blind study in subjects with moderate-to-severe psoriasis (the PRISTINE trial). J Dermatol Treat. 2013;24(3):169–78. doi:10.3109/09546634.2012.658015.
Cham PM, Chen SC, Grill JP, Jonk YC, Warshaw EM. Reliability of self-reported willingness-to-pay and annual income in patients treated for toenail onychomycosis. Br J Dermatol. 2007;156(5):922–8. doi:10.1111/j.1365-2133.2006.07740.x.
Radtke MA, Schafer I, Gajur A, Langenbruch A, Augustin M. Willingness-to-pay and quality of life in patients with vitiligo. Br J Dermatol. 2009;161(1):134–9. doi:10.1111/j.1365-2133.2009.09091.x.
Schiffner R, Schiffner-Rohe J, Gerstenhauer M, Hofstadter F, Landthaler M, Stolz W. Willingness to pay and time trade-off: sensitive to changes of quality of life in psoriasis patients? Br J Dermatol. 2003;148(6):1153–60.
Carlsson F, Martinsson P. Design techniques for stated preference methods in health economics. Health Econ. 2003;12(4):281–94. doi:10.1002/hec.729.
Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. doi:10.1016/j.jval.2012.08.2223.
Hole AR, Kolstad JR. Mixed logit estimation of willingness to pay distributions: a comparison of models in preference and WTP space using data from a health-related choice experiment. Empir Econ. 2012;42:445–69.
Hole A. Esitmating mixed logit using maximum simulated likelihood. Stata J. 2007;7(3):388–401.
Hensher DA, Greene WH. The mixed logit model: the state of practice. Transportation. 2003;30:133–76.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13. doi:10.1016/j.jval.2010.11.013.
Umar N, Litaker D, Schaarschmidt ML, Peitsch WK, Schmieder A, Terris DD. Outcomes associated with matching patients’ treatment preferences to physicians’ recommendations: study methodology. BMC Health Serv Res. 2012;12:1. doi:10.1186/1472-6963-12-1.
Lamiraud K, Geoffard PY. Therapeutic non-adherence: a rational behavior revealing patient preferences? Health Econ. 2007;16(11):1185–204. doi:10.1002/hec.1214.
Basu A, Meltzer D. Value of information on preference heterogeneity and individualized care. Med Decis Making. 2007;27(2):112–27. doi:10.1177/0272989X06297393.
Acknowledgments
This study was funded by an institutional grant and honoraria from Janssen Italia SpA. A.T. and G.F. received grants from Janssen Italia SpA during the conduct of the study. F.A. served as a consultant to Janssen Italia SpA during the conduct of the study and outside the submitted work.
An independent contract research organization, paid by the funding source, was responsible for the study’s deployment and survey administration in the hospitals. The views expressed in this paper are solely those of the authors, who have no conflicts of interest directly relevant to the content of the paper. The publication of the study results was not contingent on the sponsor’s approval or censorship of the manuscript.
All authors contributed to the conception and design of the study. G.F. and F.A. were in charge of defining the study protocol, while A.T. was involved in the design of the DCE part of the survey and conducted analysis on the experiment data. All authors were involved in drafting the manuscript and revising it critically for important intellectual content. All authors gave final approval of the version to be published. A.T. and G.F. had full access to all of the data in the study, and they both take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Authors are particularly thankful to Stefania Casalini and Antonio Castiglia from Janssen Italia SpA for their support and contribution to the realization of the research project. Finally, authors wish to express their gratitude to all study investigators from 15 hospitals participating in the study: 1) De Simone Clara, D'Agostino Magda (Policlinico Gemelli, Roma), 2) Simonacci Marco, Bettacchi Alberta (Ospedale di Macerata), 3) Papini Manuela, Cicoletti Michela (Azienda Ospedaliera Santa Maria di Terni), 4) Cottoni Francesca, Montesu M. Antonietta (Clinica Dermatologica Università di Sassari), 5) Micali Giuseppe, Musumeci Letizia (Azienda Ospedaliera Universitaria “Policlinico-Vittorio Emanuele”, Presidio Gaspare Rodolico, Catania), 6) La Greca Stefano, Massimino Daniela (Azienda Ospedaliera “Garibaldi-S.L.Currò-Ascoli Tomaselli”, Catania), 7) Patrizi Annalisa, Bardazzi Federico (Policlinico S. Orsola-Malpighi, Bologna), 8) Peserico Andrea, Piaserico Stefano (Azienda Ospedaliera Universitaria di Padova), 9) Girolomoni Giampiero, Del Giglio Micol (Ospedale Civile Maggiore-Università degli Studi di Verona), 10) Parodi Aurora, Cozzani Emanuele (Azienda Ospedaliera San Martino, Genova), 11) Cattaneo Angleo, Carrera Carlo (Ospedale Maggiore Policlinico, Mangiagalli e Regina Elena, Milano), 12) Colombo Enrico, Tiberio Rossana (Ospedale maggiore della Carità, Novara), 13) Valenti Giancarlo, D'Amico Domenico (Azienda Ospedaliera Pugliese Ciaccio, Catanzaro), 14) Balato Nicola (Università degli Studi di Napoli) 15) Griseta Vito, Lerario Andrea (Ospedale Generale Regionale "F. Miulli", Bari).
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Torbica, A., Fattore, G. & Ayala, F. Eliciting Preferences to Inform Patient-Centred Policies: the Case of Psoriasis. PharmacoEconomics 32, 209–223 (2014). https://doi.org/10.1007/s40273-013-0126-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0126-6