Abstract
Background
Idiopathic pulmonary fibrosis (IPF) is a fibrotic disease of the lungs of unknown origin with a poor prognosis. A small trial of co-trimoxazole demonstrated improvements in symptoms and functional parameters over a 3-month period. We therefore conducted a larger trial with a concurrent economic evaluation to investigate this antibiotic further.
Methods
We report an economic evaluation alongside a multi-centre, randomised, placebo-controlled, double-blind trial of 12 months therapy with 960 mg co-trimoxazole daily in 181 patients with fibrotic idiopathic interstitial pneumonia (IIP). Patients were recruited from 28 university and district hospitals in the UK and were aged over 40 years with fibrotic IIP. We report costs to the National Health Service (NHS) and society, change in forced vital capacity (primary endpoint) and quality-adjusted life-years (QALYs) gained, incremental cost effectiveness and cost utility ratios over 12 months.
Results
From the perspective of society, mean cost per patient in the co-trimoxazole arm was approximately £1177 higher than in the placebo arm, but mean QALYs were 0.053 higher yielding an incremental cost-effectiveness ratio of £22,012 per QALY gained with a 54.44 % probability of being below £30,000. The cost of IPF to UK society in 2011 is tentatively estimated at £124 million, of which 13 % is NHS costs, 1 % social services, 2 % patient out-of-pocket costs and 84 % lost productivity.
Conclusions
Given commonly employed thresholds in the UK NHS, on balance co-trimoxazole may be a cost-effective treatment for IPF, although there is substantial decision uncertainty. However, recent guidance on the use of immunosuppressive therapy in IPF patients should be taken into account prior to any policy decision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
• Idiopathic pulmonary fibrosis (IPF) is a lung disease with dismal prognosis.
• A small randomised controlled trial showed promise that the antibiotic co-trimoxazole might have some impact on disease progression.
• The TIPAC study found no evidence for a disease-modifying effect but some survival benefit in those adhering to treatment [1].
• Because of its low cost, co-trimoxazole may be a cost-effective treatment in IPF patients.
• Recent changes in treatment guidelines, especially regarding immunosuppressive treatment should be taken into account when generalising these results to other settings.
1 Introduction
Idiopathic interstitial pneumonia (IIP) consists of a number of conditions of unknown aetiology that result in fibrosis of the lung parenchyma; the most common of which is idiopathic pulmonary fibrosis (IPF). Approximately 5,000 patients are diagnosed with IPF in the UK each year, typically aged 50–70 years, with the incidence rising over time [2]. The prognosis for patients is poor, with a 5-year survival of between 20 and 40 % [3] and no treatments shown to be effective at reducing mortality. International guidelines recognise the urgent need for new treatments [4] but most studies to date have failed to provide convincing evidence of effectiveness [5]. Furthermore, there are no data on the costs or cost effectiveness of interventions in IPF.
A small, pilot, randomised controlled trial of the antibiotic co-trimoxazole in 20 patients with IIP demonstrated improvements in forced vital capacity (FVC) and shuttle walk distance over 3 months [6]. We therefore conducted a larger clinical trial to compare the efficacy, safety and cost effectiveness of the addition of 12 months of oral co-trimoxazole to standard treatment for IPF [1]. Here, we report the results of an economic evaluation conducted alongside the clinical trial, estimating the incremental cost per point improvement in FVC and per quality-adjusted life-year (QALY) gained from co-trimoxazole versus placebo from the perspectives of the UK National Health Service (NHS) and society over a time horizon of 12 months. We also calculate a tentative estimate of the cost of IPF to UK society based on placebo group resource use data.
2 Method
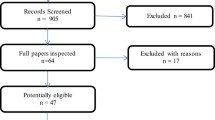
Reporting of this economic evaluation is compliant with the CHEERS statement [7]. Full details of the trial are reported elsewhere [1]. Briefly, this was a double-blind, multi- (28) centre, randomised, parallel, placebo-controlled trial of 12 months therapy with co-trimoxazole in 181 patients aged over 40 years with fibrotic IIP. The study was set in the community in the UK. Patients were excluded if a secondary cause for pulmonary fibrosis was identified, if they were receiving immunosuppressant medication other than prednisolone, azathioprine or mycophenolate mofetil, had co-trimoxazole allergy or intolerance, untreated folate or B12 deficiency, a respiratory tract infection within 2 months prior to randomisation or if they had a significant concomitant disease that could affect subject safety or influence the study outcome. The study was conducted in accordance with Good Clinical Practice and all participants gave written informed consent. Full ethical approval was granted for the study.
Patients were randomised to receive either co-trimoxazole (Essential Generics, Egham, Surrey, UK) 960 mg (as two tablets of 480 mg each) twice daily or an identical placebo (manufactured from the pharmacy at Guy’s and St Thomas’s Hospital, London, UK) two tablets twice daily in addition to their usual care. Each patient received folic acid (non-proprietary) 5 mg once daily. The use of additional antibiotics was permitted for intercurrent infections. Randomisation was performed centrally using a computer-generated code with stratification for the site and the use of azathioprine/mycophenolate mofetil.
The primary outcome of the study was change in FVC at 12 months. In addition, change in overall health-related quality of life (via the EuroQol EQ-5D-3L) [8] and resource use were assessed at baseline, 6 weeks and 6, 9, and 12 months following randomisation. For the duration of the study an assessment of secondary endpoints including all-cause mortality, hospitalisations, the requirement for escalation of therapy and adverse events was made. The clinical trial did not detect a statistically significant difference in change in FVC at 12 months (mean difference +15.5 mL, 95 % confidence interval [CI] −93.6 to 124.6). Other outcome measures and details of safety monitoring are reported elsewhere [1].
Responses to the EQ-5D-3L at each time point were converted to utilities using standard UK health state valuations [9], and thence to QALYs gained by calculating the area under the curve over the 12-month time horizon.
Resource use data were collected by means of a self-administered questionnaire. Data collected at baseline pertained to the 3 months prior to randomisation, which were then used as a predictor of future cost in an adjusted analysis. Resource data were divided into four categories: NHS, social services, patient out-of-pocket expenditure and lost productivity. Within each category a number of sub-categories were defined (Table 1) with individual resource items assigned to a sub-category. Cost per patient was calculated by multiplying unit costs identified from standard reference sources (Table 2) by resource quantities (Table 3). The price year of the analysis is 2011/2012. Discounting of costs (and outcomes) was not appropriate as the time horizon of the study was only 12 months.
Results are reported as details of resource use, mean cost and outcome (change in FVC and QALYs) per patient, increments and point estimate incremental cost-effectiveness ratio (ICER) from the perspectives of the NHS and society. 95 % CIs are calculated around increments by means of a non-parametric bootstrap of 5,000 iterations using the percentile method, the results of which are used to show uncertainty in cost effectiveness as cost-effectiveness acceptability curves. Analyses are based on an intention-to-treat (ITT) and per-protocol (PP) basis. The PP analysis excludes non-adherent patients and those withdrawing prior to death. Complete case analysis results are reported as well as increments adjusted for baseline utility and cost, with missing values imputed using multiple imputation (see “Appendix” for full details) [10]. Finally, the placebo arm of the study was used to estimate the cost of IPF to the NHS and UK society in 2011 (see below). Analysis was performed in a blinded fashion.
2.1 Cost-of-Illness Study
During data collection, patients were asked to attribute contacts with the health service due to either their IPF or other causes. This presented an opportunity to estimate the cost of IPF to society based on the cost of resource use reported by patients as attributable to IPF in the placebo arm of the study.
Patients were not asked to attribute over-the-counter (OTC) medications, prescribed drugs or informal care received for IPF. Therefore, OTC and prescribed drugs were attributed based on discussion between two authors (EW and AW). As these were all IPF patients, all informal care received was assumed attributable to IPF.
Data on primary, secondary and tertiary resource use were available on 72 patients. OTC and prescription data were available on all 85 patients in the placebo arm. Data on travel costs and lost productivity were available on 69 and 67 patients, respectively. Summary totals in the analysis are based on observations for which complete data are available, thus the reported sum may not equal the sum of the individual components (e.g. in the case of cost of out-of-pocket, indirect, overall NHS and societal costs).
Per patient costs were multiplied by the prevalence of IPF in the UK in 2011 to provide an estimate of the cost to the NHS and society of IPF. We were not able to identify any UK-specific data on the prevalence of IPF. However, a recent study estimated the overall incidence at 7.44 per 100,000 person-years [2]. A study on both the incidence and prevalence of IPF in the USA used both a broad and narrow definition of IPF [11]. The narrow definition generated an overall incidence of 6.8 per 100,000 person-years with an associated prevalence of 14.0 per 100,000 person-years. Given the similarity in the estimates of the incidence between the US and UK studies, it was assumed that the ‘narrow definition’ of IPF was the most consistent with that used in the UK and thus prevalence would also be similar (this is contingent on an assumption of similar prognosis for IPF patients in both the US and UK). Thus, a prevalence of 14.0 per 100,000 was applied to the 2011 UK population of 63.2 million [12] to estimate the prevalence in 2011 of 8,800.
3 Results
Patients were generally well matched at baseline although patients in the co-trimoxazole group may have had shorter disease duration prior to study entry [1]. Complete data were available for 79 patients (active, placebo: 41, 38) for the PP cost-utility analysis from the societal perspective and for 125 patients (61, 64) for the ITT cost-utility analysis from the NHS perspective. These numbers vary because of the pattern of missing data, for example, a patient with full resource use and FVC data would be included in the cost-effectiveness complete case analysis, but if utility data were missing (even just for one time point) the patient was excluded from the cost utility analysis. Imputed analyses comprised 180 patients (95, 85) [one patient was not imputable because of missing covariates].
3.1 Resource Use and Cost
Point estimate analyses of resource use (Table 3) show very little difference in primary, secondary or other healthcare resource use between the groups. From the perspective of the NHS, co-trimoxazole is associated with an additional cost of £100 per patient per year (SE £495). However, from a societal perspective, co-trimoxazole is associated with a saving of £484 per patient per year (SE £4,203; Table 4).
3.2 Outcomes
Co-trimoxazole was observed with increases in mean QALYs gained compared with placebo, but as with resource use, there is a great deal of uncertainty and 95 % CIss did not exclude zero.
3.3 Cost Effectiveness
In all analyses, 95 % CIs did not exclude zero. Point estimate results, adjusted for baseline and with missing data imputed, showed a higher cost and very little difference in incremental FVC for the treatment group compared with placebo (Table 5). Overall health gain was on average higher in the treatment group (Table 6). The ICER varied between co-trimoxazole being dominant to £22,012 per QALY gained, depending on perspective and ITT/PP population (Table 6). There is between 54.4 and 91.9 % probability that the ICER is below £30,000, depending on perspective and analysis (Fig. 1).
Cost-effectiveness acceptability curves. The cost-effectiveness acceptability curve is the probability that the incremental cost-effectiveness ratio (ICER) is below a given willingness to pay for a quality-adjusted life-year (i.e. the probability that co-trimoxazole is cost effective given a threshold of X). There is between 54.44 and 91.86 % probability that the ICER is below £30,000, depending on analytic perspective. ITT intention-to-treat analysis, NHS National Health Service, PP per-protocol analysis, QALY quality-adjusted life-year
3.4 Cost of Illness
Based on analysis of the placebo arm enrolled in the trial, the cost to UK society of IPF in 2011 is estimated at £124 million (SE £25.3 million), of which approximately £14 million (12 %) is attributable to the NHS, £0.6 million (1 %) to social services, £1.6 million (2 %) to out-of-pocket costs to patients and the remainder (85 %) attributable to morbidity associated with lost productivity (Table 7).
4 Discussion
4.1 Interpretation of Results
The results present a number of separate analyses. When analysing cost alone, mean cost to the NHS per patient in the co-trimoxazole arm is approximately £100 higher than in the placebo arm. When overall societal costs are included, mean cost per patient in the co-trimoxazole arm is approximately £400 less than in the placebo arm (Table 4). However, when cost data are combined with outcomes, point estimate incremental costs vary somewhat between analyses (Tables 5, 6). This is simply because of the exclusion of data in the complete case analyses and high uncertainty in incremental cost (and outcomes): the high standard errors mean that, for example, none of the 95 % CIs around the increments exclude zero.
One conclusion would be that as we have failed to demonstrate a statistically significant effect on cost, outcomes or cost effectiveness, we can make no policy recommendation from these data. However, as the study was powered on the primary outcome (change in FVC at 12 months) and not cost, QALYs or cost effectiveness, such a conclusion may be a type one error. Alternatively, a decision theoretic approach would argue that a decision has to be made whether to adopt co-trimoxazole as part of routine therapy in these patients or not, and that the decision has to be made on the evidence available irrespective of the uncertainty: a decision to delay pending further information is still a decision to withhold a treatment for the current cohort of patients. This implies that decisions should be based on mean values alone (and uncertainty used to determine the value of gathering further information) [13, 14]. The latter (decision theoretic) approach risks being “fooled by randomness”, whilst the former (inferential approach) is inconsistent with the principles of decision theory, and will not lead to maximising expected outcomes subject to the resources available.
Following decision theoretic reasoning, the point estimate of the ICER should be used to determine whether co-trimoxazole represents good value for money. However, in Tables 5 and 6 we present numerous ICERs from separate analyses representing different analytic perspectives (NHS and society), different outcomes (change in FVC and QALYs gained) and statistical techniques to handle missing data. It is argued that the most appropriate analytic perspective for an economic evaluation is that of society as any lesser perspective may lead to misleading conclusions owing to simple cost shifting between budgets rather than genuine changes in resource consumption [15]. Similarly, the QALY may be seen as a preferable outcome measure to a change in FVC as the QALY is a measure of overall quality-adjusted life expectancy, rather than focusing on one particular symptom or functional aspect. Finally, the ITT analytic approach is the least subject to bias [16], the imputed analysis avoids discarding informative data [10] and adjustment for baseline values takes into account any differences in patient characteristics at baseline [17].
On this basis, the most appropriate analysis is the adjusted, imputed ITT cost-utility analysis conducted from the societal perspective (Table 6, row 2). Point estimates suggest co-trimoxazole increases the mean cost per patient by £1177, for a gain of 0.053 QALYs in these patients. The incremental cost per incremental QALY gained is therefore £22,012. This is below the upper limit considered ‘acceptable’ by the National Institute for Health and Care Excellence (NICE) [NICE argues that a threshold of £20,000–£30,000 per QALY is an appropriate willingness to pay] [18], and therefore co-trimoxazole may be considered a cost-effective treatment. Analysis of uncertainty suggests a 54.44 % probability that the ICER is below £30,000.
4.2 Clinical Implications
Despite the cost-effectiveness results, analysis of the study primary and some secondary clinical endpoints suggests that co-trimoxazole has no effects on the traditional surrogate measures of disease progression [1]. This brings into question the usefulness of these markers. Although the majority of patients die of sub-acute respiratory failure, up to 30 % die of an acute exacerbation of their disease [19]. These exacerbations cannot be predicted based upon the severity of lung function impairment [20]. The annual incidence of exacerbations, per patient, is between 5 and 19 % [21] and they have an associated 3-month mortality of up to 80 % [20]. Indeed, hospitalisation along with age and lung function, are independent predictors of survival in IPF [22].
Our results suggest that either infection has an important role in IPF pathogenesis or co-trimoxazole has clinically relevant non-antimicrobial effects. Recent data published following the completion of the study have led to a change in the medical management of IPF, with a reduction in the use of immunosuppressive therapy [23]. The drug history of patients at randomisation reflected UK prescribing practices at the time [24], with half of the patients receiving prednisolone. However, as mentioned, UK guidelines no longer recommend the routine use of immunosuppressive therapy. Therefore, the typical patient seen in practice may differ from those enrolled in the study; specifically, patients are less likely to be immunosuppressed. If the capacity to benefit in non-immunosuppressed patients is lower (they are less at risk of opportunistic infections), the ICER is likely to be higher (i.e. co-trimoxazole may be less cost effective than our results suggest). Whether it crosses the £20,000–£30,000 threshold is an empirical question for which further research is required.
4.3 Comparison with Other Studies
There are very few data on the costs of interstitial lung disease or the cost effectiveness of treatments. Although researchers have investigated the economics of diagnostic assessments for IPF [25, 26], the only data relating to IPF treatment are in abstract form and show rising healthcare costs using a database of medical and pharmacy claims from private health plans in USA; the researchers found that 70 % of mean annual total healthcare costs were due to hospitalisation and that costs increased with age and were significantly higher in those who died at the end of the annual follow-up [27]. At the time of writing, we are not aware of any published estimates of the costs of the illness to society or cost effectiveness of other IPF treatments with which to compare our results.
The cost of IPF to society in 2011 was estimated at £124 million. By way of comparison, a longitudinal cost-of-illness study of the cost of occupational asthma estimated a lifetime societal cost (rather than a cross-sectional annual cost) for the 2003 cohort of new cases at £95–£135 m (£2004) [28]. Total expenditure on bronchodilators, respiratory corticosteroids and leukotriene receptor antagonists in England in 2011 was £971 million [29], and UK gross domestic product was £1.516 trillion [30]. IPF therefore likely represents a small component of total expenditure on lung disease. Possible explanations for this include the relative rarity of the disease, the poor prognosis and lack of effective interventions.
4.4 Strengths and Weaknesses
To our knowledge, this is the first cost-effectiveness analysis of a potential treatment for IPF. It is also the first study to estimate the cost of IPF to UK society and the NHS. It is non-commercially funded and based on a well-conducted, double-blind, randomised controlled trial using prospective data collection over 12 months via detailed questionnaires and should therefore be of high internal validity.
A 12-month time horizon was chosen for several reasons. First, the horizon was constrained by budgetary requirements. Second, the disease is associated with a poor prognosis and therefore 12 months may allow any changes in mortality between groups to be apparent. Third, the study was powered on the primary outcome (change in FVC at 12 months), and such a time horizon was considered to be a clinically relevant endpoint.
The major weakness of the study is the relatively low proportion of the data included in the complete case analysis. However, this is due to the strict definition of a ‘complete case’, requiring complete data on primary, secondary and other NHS care, drug costs, out-of-pocket costs and lost productivity as well as FVC and EQ5D measures at every follow-up. If any one of these items were missing then the observation was excluded from the complete case analysis, leading to exclusion of the data that were present. However, the imputed analysis (using the multiple imputation technique [10]) includes these data, repeatedly replacing the missing data with plausible values sampled from the distribution around the conditional mean. This therefore makes best use of the data available whilst allowing for uncertainty in the missing values.
We are not aware of any estimates of the cost of IPF to the UK economy. The placebo arm of this trial therefore provided an opportunity to estimate this cost. Because of this somewhat opportunistic approach, the estimates must be interpreted with appropriate caution. The danger with using placebo arms of studies to estimate the cost of illness is that cost items common to both arms of a trial are typically excluded from analysis (as they cancel each other out in the incremental analysis), and thus the cost per arm may not accurately reflect all cost items. Second, trials may involve activity and contacts with the health service that would not be seen in routine care (protocol-driven costs). Third (and possibly most importantly), inclusion and exclusion criteria may select a sample of patients enrolled in a study that is not representative of the ‘typical’ patient population. Additionally in this study, OTC, prescription drug costs and informal care costs were attributed to IPF based on the clinical and economics experience of two of the authors (AW and EW, respectively). Where patients have co-morbidities, we may have overestimated the indirect cost attributable to IPF. In response to these limitations, owing to the nature of the data collection in this trial, we are confident that no major cost items were excluded and that the placebo arm of this study represents a reasonable picture of routine practice for IPF patients. Comparison of the sub-group used in the cost-of-illness study with the rest of the trial population shows no substantial differences except for a longer time since diagnosis (data not shown), and we believe the trial population to be representative of the patient population at the time of randomisation (but we refer readers to comments above regarding current policy for immunosuppressive therapy).
5 Conclusion
On average, co-trimoxazole for patients with IPF for 1 year leads to increases in both mean cost and QALYs gained. The point estimate ICER is £22,012 from the perspective of society (£6,818 from the NHS perspective). Analysis of uncertainty suggests a 54.44 % probability that the ICER is below £30,000 per QALY from the perspective of society (86.98 % from the NHS perspective). Point estimate ICERs are below the maximum willingness to pay for a QALY in the UK (considered to be around £20,000–£30,000) [18], and therefore the addition of co-trimoxazole to standard treatment may be considered a cost-effective treatment. However, changes in UK management practice, particularly with regard to immunosuppressive therapy means that current patient populations may differ from the one enrolled into this study. Assessment of the comparability of the patient population with that enrolled in the study should precede any policy decision based on this analysis.
References
Shulgina L, Cahn AP, Chilvers ER, et al. Treating idiopathic pulmonary fibrosis with the addition of co-trimoxazole: a randomised controlled trial. Thorax. 2013;68(2):155–62.
Navaratnam V, Fleming KM, West J, et al. The rising incidence of idiopathic pulmonary fibrosis in the U.K. Thorax. 2011;66(6):462–7.
Nicholson AG, Colby TV, du Bois RM, et al. The prognostic significance of the histologic pattern of interstitial pneumonia in patients presenting with the clinical entity of cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med. 2000;162(6):2213–7.
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824.
Spagnolo P, Del Giovane C, Luppi F, et al. Non-steroid agents for idiopathic pulmonary fibrosis. Cochrane Database Syst Rev. 2010;(9):CD003134. doi:10.1002/14651858.CD003134.pub2.
Varney VA, Parnell HM, Salisbury DT, et al. A double blind randomised placebo controlled pilot study of oral co-trimoxazole in advanced fibrotic lung disease. Pulm Pharmacol Ther. 2008;21(1):178–87.
Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Pharmacoeconomics. 2013;31(5):361–7. doi:10.1007/s40273-013-0032-y.
The EuroQol Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–108.
Rubin DB. Multiple imputation for nonresponse in surveys. Hoboken: Wiley; 2004.
Raghu G, Weycker D, Edelsberg J, et al. Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006;174(7):810–6. doi:10.1164/rccm.200602-163OC.
Office for National Statistics. Statistical bulletin: 2011 census: population estimates for the United Kingdom. 2011. http://www.ons.gov.uk/ons/rel/census/2011-census/population-and-household-estimates-for-the-united-kingdom/stb-2011-census-population-estimates-for-the-united-kingdom.html. Accessed 24 July 2013.
Pratt J, Raiffa H, Schlaifer R. Introduction to statistical decision theory. Cambridge: Massachusetts Institute of Technology; 1995.
Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ. 1999;18(3):341–64. doi:10.1016/S0167-6296(98)00039-3.
Byford S, Raftery J. Perspectives in economic evaluation. BMJ. 1998;316(7143):1529–30.
Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319(7211):670–4.
Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14(5):487–96. doi:10.1002/hec.944.
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. Accessed http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf.
Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183(4):431–40. doi:10.1164/rccm.201006-0894CI.
Kim DS, Park JH, Park BK, et al. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J. 2006;27(1):143–50. doi:10.1183/09031936.06.00114004.
Song JW, Hong SB, Lim CM, et al. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J. 2011;37(2):356–63. doi:10.1183/09031936.00159709.
du Bois RM, Weycker D, Albera C, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(4):459–66. doi:10.1164/rccm.201011-1790OC.
Raghu G, Anstrom KJ, King TE Jr, et al. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366(21):1968–77. doi:10.1056/NEJMoa1113354.
Dempsey OJ, Welham S, Hirani N. P84 BTS National Interstitial Lung Diseases (ILD) Survey 2010–2011. Thorax. 2011;66(Suppl 4):A102. doi:10.1136/thoraxjnl-2011-201054c.84.
Hagaman JT, Kinder BW, Eckman MH. Thiopurine S-methyltransferase [corrected] testing in idiopathic pulmonary fibrosis: a pharmacogenetic cost-effectiveness analysis. Lung. 2010;188(2):125–32. doi:10.1007/s00408-009-9217-8.
Molin LJ, Steinberg JB, Lanza LA. VATS increases costs in patients undergoing lung biopsy for interstitial lung disease. Ann Thorac Surg. 1994;58(6):1595–8. doi:10.1016/0003-4975(94)91638-1.
Weycker D, Oster G, Edelsberg J, et al. Economic costs of idiopathic pulmonary fibrosis: annual meeting of the American College of Chest Physicians. Chest. 2002:150s.
Ayres JG, Boyd R, Cowie H, et al. Costs of occupational asthma in the UK. Thorax. 2011;66(2):128–33. doi:10.1136/thx.2010.136762.
NHS Health and Social Care Information Centre. Prescription cost analysis. 2011. http://www.ic.nhs.uk/pubs/prescostanalysis2011. Accessed 22 March 2013.
Office for National Statistics. United Kingdom National Accounts—The Blue Book 2012 Edition; 2012. http://www.ons.gov.uk/ons/rel/naa1-rd/united-kingdom-national-accounts/the-blue-book--2012-edition/index.html
Department of Health: National Schedule of Reference Costs 2011–12 for NHS Trusts and NHS Foundation Trusts. Appendix NSRC01. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/127114/Nationalschedules.zip.zip
Curtis L. Unit costs of health and social care 2012. Canterbury: University of Kent at Canterbury; 2013.
Office for National Statistics. Annual survey of hours and earnings, 2012 provisional results. 2012. http://www.ons.gov.uk/ons/dcp171778_286243.pdf
British National Formulary 62. 62 ed. London: British Medical Journal Group & Royal Pharmaceutical Society of Great Britain; 2011. http://www.bnf.org
Acknowledgments
The authors would like to thank the local principal investigators (detailed below), the research nursing staff, Dr Veronica Varney, Dr Julie Anderson, Mrs Sue Steel, Mr Tony Dyer, NIHR Cambridge Biomedical Research Centre, Papworth Research and Development Department, and the patients who made this study possible. Local Principal Investigators: R. Allcock (Queen Elizabeth Hospital, Gateshead), M. Azher (Bedford Hospital, Bedford), D. Boldy (Pilgrim Hospital, Boston), T. Cotter (James Paget University Hospital, Gt. Yarmouth), M. Darmalingam (Whipps Cross University Hospital, London), J. Douse (Ipswich Hospital), D. Ellis (James Paget University Hospital, Gt. Yarmouth), I. Forrest (Royal Victoria Infirmary, Newcastle), K. Harrison (Morriston Hospital, Swansea), P. Hawkins (Colchester Hospital), T. Howes (Colchester Hospital), S. Iles (Royal Cornwall Hospital, Truro), N. Innes (Ipswich Hospital), O. Khair (Birmingham City Hospital), C. Leonard (Wythenshawe Hospital, Manchester), J. Mann (New Cross Hospital, Wolverhampton), R. O’Driscoll (Salford Royal University Hospital), A. Pawlowicz (Queen Elizabeth Hospital, Kings Lynn), P. Pillai (Luton Hospital), A. Promnitz (Ipswich Hospital), J. Ramsay (Luton Hospital), L. Spencer (Aintree University Hospital, Liverpool), M. Spiteri (North Staffordshire University Hospital), D. Stock (South Tyneside Hospital, South Shields), E. Thomas (Bedford Hospital), C. Warburton (Aintree University Hospital, Liverpool), J. White (West Suffolk Hospital), M. Whyte (University of Sheffield), J. Wiggins (Heatherwood and Wexham Park Hospitals, Slough), B. Yung (Basildon Hospital), H. Yussef (Chorley and South Ribble Hospital). This paper presents independent research commissioned by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0906-11116). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding
East Anglia Thoracic Society, National Institute for Health Research for Patient Benefit (RfPB) Programme, NIHR Cambridge BRC, Boehringer Ingelheim non-commercial educational grant. ISRCTN22201583.
Author contributions
EW undertook the economic evaluation. AMW was the chief investigator and LS was the study co-ordinator. All authors participated in study conception and design. Study research sites and LS were responsible for data collection. LS and AMW were responsible for data validation. LS, APC, EC, HP, OT, AMW and ABC participated in data analysis, ABC undertook the statistical analysis. All authors participated in data interpretation, writing and revision of the report, and approval of the final version.
Conflict of interest
EW’s salary is funded by the NIHR (the funder of this research) through the Research Design Service for the East of England. APC is an employee of, and holds stock and stock options in, GlaxoSmithKline. AW has received funding from Intermune (manufacturer of pirfenidone) to attend a respiratory conference. LS, EC, HP, AC and OT have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 Details of Imputation
Missing data were imputed in STATA using the ‘ice’ command at the level of total NHS and societal costs, QALYs and change in FVC at 12 months. Explanatory variables were baseline NHS and societal cost, utility and FVC, whether the patient was prescribed prednisolone, age left education, marital status, employment status and intervention arm. Five datasets were generated, each based on 1000 markov chain monte carlo (MCMC) iterations. The code is provided below:

1.2 Details of Adjustment to Baseline Values
The imputed, adjusted increments were calculated as follows:
-
The imputed datasets resulting from the ‘ice’ command above were resampled with replacement (thus five ‘new’ datasets were generated).
-
OLS regressions were used to estimate NHS cost, societal cost, QALYs and change in FVC for each of the ‘new’ datasets, using treatment group and baseline NHS or societal cost, utility or FVC as explanatory variables respectively.
-
The coefficients on treatment group were recorded as the adjusted incremental cost or outcome respectively.
-
Steps 1-3 were repeated 1000 times, thus generating 5000 sets of adjusted incremental cost and outcomes (1000 from each imputed dataset).
-
The percentile method was used to calculate 95 % confidence intervals around point estimate increments.
Rights and permissions
About this article
Cite this article
Wilson, E.C.F., Shulgina, L., Cahn, A.P. et al. Treating Idiopathic Pulmonary Fibrosis with the Addition of Co-Trimoxazole: An Economic Evaluation Alongside a Randomised Controlled Trial. PharmacoEconomics 32, 87–99 (2014). https://doi.org/10.1007/s40273-013-0112-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0112-z