Abstract
Background
Self-care in people with chronic obstructive pulmonary disease (COPD) can improve health-related quality of life, reduce hospital admissions and decrease dyspnoea.
Objective
This review aimed to systematically identify, evaluate and synthesise the qualitative literature on the self-care behaviours and strategies used by people with COPD.
Methods
The Joanna Briggs Institute (JBI) meta-aggregative method was followed. An electronic search of six relevant databases was conducted. The search was limited to articles published from January 1996 to January 2016. Reference lists of all identified articles were searched to find additional literature. Two independent reviewers analysed the studies against the inclusion criteria, extracted the data and assessed the methodological quality of the 14 identified papers using the JBI qualitative assessment and review critical appraisal instrument. Findings were synthesised using a meta-aggregation process.
Results
Four synthesised findings emerged from the aggregation of 114 findings: self-care is directed towards the prevention, control and management of the physical consequences of COPD; self-care focuses on the management of the psychological effects of COPD; self-care is aimed at reducing the impact of COPD on social life; and self-care is influenced by contact with healthcare services and requires the acquisition of knowledge and skills.
Conclusions
This meta-synthesis provides evidence on the self-care behaviours and strategies that people with COPD perform to prevent, control and manage the physical, psychological and social consequences of the disease. The findings of this meta-synthesis could help healthcare professionals to tailor self-care educational programmes to the experiences, preferences and priorities of people with COPD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
People with chronic obstructive pulmonary disease (COPD) implement self-care activities and strategies directed towards the prevention, control and management of the physical consequences of the disease, including respiratory and sleep problems, limitations in daily activities and exacerbations. |
The emotional wellbeing of people affected by COPD is compromised by the disease, which causes depression, anxiety, embarrassment and frustration. Therefore, self-care focuses on managing the emotional disturbances caused by COPD. |
COPD influences the social and family lives of people affected by the disease, requiring the use of various self-care strategies to reduce its effects on their social lives. |
To perform self-care behaviours, people with COPD must acquire the necessary knowledge and skills to maintain the disease’s stability and to control and manage symptoms. |
Qualitative evidence of the self-care that people with COPD perform to prevent, control and manage its physical, psychological and social consequences should be used to inform individualised self-care educational programmes. |
1 Introduction
Chronic obstructive pulmonary disease (COPD) is a non-reversible disease characterised by a persistent and progressive airflow limitation associated with frequent exacerbations and comorbidities [1]. It is a major cause of chronic morbidity and mortality worldwide. Globally, the prevalence of COPD is 11.4% in people aged 30 years or older. In particular, the prevalence is 12.0% in Europe, 14.1% in North America and 10% in Asia, where it is expected to increase in the next few years [2]. Moreover, COPD is the fourth leading cause of deaths worldwide and is estimated to become the third cause of death by 2030 [3]. Self-care in people with COPD is particularly important as it can improve health-related quality of life, reduce hospital admissions and decrease dyspnoea [4]. According to the middle-range theory of self-care in chronic diseases proposed by Riegel et al., self-care in COPD can comprise three distinct but related dimensions: self-care maintenance, self-care monitoring and self-care management [5]. Self-care maintenance includes the behaviours that people with COPD perform to maintain physical and emotional stability, including medication adherence, smoking cessation, physical activity and respiratory exercises. Self-care monitoring embraces the behaviours aimed at monitoring the disease’s signs and symptoms, including sputum’s increased production or changes in its colour. Self-care management consists of the behaviours performed to manage the disease’s symptoms or the treatments’ side effects when they occur, including breathlessness, insomnia and panic attacks [5, 6].
Self-care behaviours performed by people with COPD encompasses the recommendations of healthcare professionals as well as self-determined behaviours based on individual knowledge, beliefs, cultural traditions, experiences, habits and the recommendations of family and friends [7].
Despite the information and self-management programmes provided by healthcare professionals, based on the clinical guidelines produced by international organisations, such as those of the Global Initiative for Chronic Obstructive Lung Disease [1], individuals with COPD seldom comply with the recommended self-care behaviours, and little is known about what these individuals truly do to take care of themselves in their daily lives [8, 9]. Social factors, the feeling of being disabled and physical barriers may prevent people with COPD from engaging in suggested self-care practices, such as respiratory or physical exercises [10]. In addition, people with acute exacerbation may be unwilling or unable to comply with health professionals’ advice; for example, dyspnoea, anxiety and fear of death can prevent patients from paying attention to the information provided, or the presence of hypoxaemia can compromise their attention and other cognitive functions [11]. During advanced stages of the disease, individuals may struggle with the changes imposed by their condition and may find following self-care practices particularly challenging [12]. People may decide to perform different behaviours to deal with the disease, since self-care is considered a naturalistic decision-making process that reflects the automatic, impulsive and contextual decisions that people with chronic diseases make in a complex real world [5]. In fact, in the real world, decisions are made in a variety of situations, many of which involve uncertainty and time constraints [6].
In general, the literature is focused primarily on self-care management education provided by healthcare professionals, particularly nurses and physiotherapists, and is aimed at increasing levels of function, improving adherence to medical regimens and avoiding exacerbations. These educational interventions are delivered in hospitals and community care settings (pulmonary clinics and rehabilitation centres) and are offered individually or in small patient groups [4, 11]. By contrast, self-care experiences from the point of view of people with COPD are rarely investigated [4, 7]. Understanding people’s experiences of self-care is essential to enable healthcare professionals to tailor self-care programmes to the specific needs of people affected by COPD, integrating their experiences, beliefs and habits with the best evidence-based practices.
To our knowledge, no systematic syntheses of qualitative studies exploring experiences of self-care in people with COPD have yet been carried out. Qualitative syntheses may enhance quantitative findings by helping to capture people’s perspectives and understand what is important from the point of view of the people who live with the disease. The generation of such knowledge will help to reveal the complexity of natural settings and, thus, support health professionals in developing more effective, cost-effective and tailored self-care interventions that are responsive to real people’s needs [13]. Therefore, the aim of this meta-synthesis was to systematically identify, appraise and synthesise the qualitative literature on the self-care experiences of people affected by COPD. In particular, the experiences explored comprised self-care behaviours and strategies related to the disease.
2 Methods
The Joanna Briggs Institute (JBI) meta-aggregative approach was followed to conduct a synthesis of the existing qualitative literature [14]. Meta-aggregation is a well-consolidated and rigorous method that enables accurate and reliable data to be obtained with no reviewer re-interpretation, and the qualitative evidence derived through this approach is useful for practical decision making. Qualitative evidence differs from quantitative evidence, as it analyses human experiences and cultural and social phenomena instead of producing numerical data and seeking to establish relations between variables. Meta-aggregation is a method of systematic review that reflects the process of a quantitative review; however, it maintains the traditions and requirements of qualitative research. Meta-aggregation combines study findings into a whole that is more than the sum of the studies’ individual findings, making it similar to the meta-analysis process [14]. Therefore, JBI meta-aggregations can include different methodological studies that can be used to understand the whole phenomenon of interest rather than one single aspect of it. The rationale is that the methodology of a particular study is incorporated within the findings rather than distinct to them; consequently, when a finding is extracted from a study, the perspective or context that the researcher intended for that finding is incorporated in the extraction [14].
The JBI process of meta-aggregation involves three phases. In the first phase, the findings of the original studies are extracted, as are illustrations representing the studies’ findings; regardless of their designs, all qualitative studies produce results as categories, themes or metaphors, which are supported by direct or indirect quotes (illustrations) from the research participants. In the second phase, the extracted findings are categorised based on similarities in meanings; the commonality in the themes, categories and metaphors across all original papers are determined, which is similar to the procedure used in qualitative research through constant comparative and thematic analysis. In the third phase, a further aggregation of these categories is performed to generate a comprehensive set of synthesised findings, which are considered the outcomes of the evidence synthesis, providing the lines of action for clinical practice [15].
The Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI) software was used to guide the review process.
2.1 Search Strategy
According to JBI guidelines, a three-step search strategy was utilised [14]. An initial limited search of the PubMed and CINAHL databases was undertaken with the terms “self-care”, “experience”, and “COPD”. This was followed by an analysis of the text words contained in the titles and abstracts of the identified articles, as well as of the index terms used to describe the articles. A second comprehensive search was then carried out across the PubMed, CINAHL, PsycINFO, ISI Web of Knowledge, Embase and Scopus databases. The main search terms used were as follows: self-care OR self-management OR self-monitoring OR self-maintenance OR self-regulation AND chronic obstructive pulmonary disease AND experience. Thirdly, the reference lists of all identified articles were searched to find additional literature. The search was limited to articles in English, French, Italian, Spanish and Portuguese published in the period January 1996–January 2016. The time period was set to include the last 2 decades because the therapeutic approaches to COPD have changed in recent years, influencing the management of the disease. The specific search strategy for PubMed is included as electronic supplementary material in Table S1 (see online resource 1). Two reviewers (MC and MM) independently screened the eligibility of the article titles and abstracts. Papers that were considered relevant were then read in full to determine their consistency with the study’s aim and inclusion criteria. Any disagreement between reviewers was solved by discussion.
2.2 Inclusion and Exclusion Criteria
Participants People aged 18 years and over with a diagnosis of COPD, at any stage of the disease, were included. Participants affected by other lung diseases, such as lung cancer, asthma and sarcoidosis, were excluded. For those studies in which the participants were not only people affected by COPD (e.g. included caregivers or healthcare personnel or people affected by other lung diseases), only data from COPD participants were extracted.
Phenomenon of interest Experiences of self-care behaviours and strategies of individuals with COPD were considered. Self-care strategies included the actions planned by individuals with COPD to manage the disease or improve their health status. Experiences of healthcare services (e.g. pulmonary rehabilitation) or of specific self-care education programmes were not included in the review.
Type of studies Primary qualitative studies, including, but not limited to, phenomenology, grounded theory, ethnography, action research, qualitative descriptive designs and qualitative strands of mixed method studies, were included. Quantitative studies, dissertations and papers that were not peer reviewed were excluded.
Setting Studies carried out in all kinds of settings (e.g. primary care settings, hospitals, rehabilitation centres) were considered for the review.
2.3 Assessment of Methodological Quality
The methodological quality of the selected papers was assessed by two independent reviewers using the JBI-QARI critical appraisal tool. This tool considers ten quality criteria: the congruity between (1) the philosophical perspective and the research methodology, (2) the research methodology and the questions, (3) the research methodology and the data collection methods, (4) the research methodology and the data analysis, and (5) the research methodology and the interpretation of the results; (6) the description of the culture or the theoretical grounding of the researchers; (7) the influence of the researchers on the research; (8) the representativeness of the participants’ voices; (9) the proof of ethical approval of the study; and (10) the relationship between the findings and the conclusions. We scored each criterion as “yes” (fulfilled), “no” (not fulfilled) or “unclear” and assigned a score of 1 when the criterion was fulfilled. Therefore, the maximum score was 10. The JBI-QARI does not recommend a specific cut-off score for study inclusion; instead, it leaves this decision to the reviewers based on what they consider acceptable levels of quality for their specific reviews. We decided to include all studies that obtained a total score of at least 6 out of 10. Any disagreement among the reviewers was resolved through discussion or by consulting a third independent reviewer. The results of the study’s critical appraisal are presented as supplementary material in Table S2.
2.4 Data Extraction
Data from the papers included in the review were extracted using the JBI-QARI standardised data extraction tool. The extracted data included: study methodologies; data collection methods; phenomena of interest; settings; information about the populations’ geographical and cultural contexts; the characteristics of the participants; data analyses; study conclusions; and reviewers’ conclusions.
The findings reported in the original qualitative studies and the more representative illustrations (verbatim, direct observations, or other data supporting the study findings) were extracted independently by two reviewers, after several readings of the papers, with the support of the QARI software. The findings were included, as suggested by QARI, only if they were supported by original data beyond any reasonable doubt (classified as unequivocal) or if the findings were plausible or could be logically inferred from the data (classified as credible). All the findings for which no relationship was found between the data and the findings (unsupported) were excluded.
2.5 Data Synthesis
According to the JBI-QARI approach, the findings extracted from the original articles were aggregated or synthesised in categories based on similarities in meaning. To produce a category, a minimum of two findings was required. Afterward, two reviewers created a meta-aggregation of the categories to produce a single comprehensive set of synthesised findings that can be used to inform the clinical practice [14].
3 Results
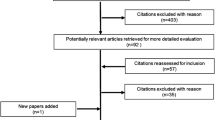
The systematic literature search retrieved 1049 papers, of which 398 were duplicates. The titles and abstracts of 651 studies were screened, and 27 appeared to fulfil the inclusion criteria. After reading these 27 articles in full, 12 articles were excluded (see supplementary material, Table S3). Thus, a total of 15 full-text articles were evaluated for inclusion. One article was then excluded following the critical appraisal because it obtained a score lower than six for the quality of the methodology [16]. Therefore, finally, 14 articles were included in the review (Fig. 1) [17–30].
The included studies were published between 2000 and 2015. Of the studies, ten used a qualitative descriptive approach [17–21, 25, 26, 28–30], three used a phenomenological design [23, 24, 27] and one was a grounded theory study [22]. Furthermore, 12 studies used individual interviews to collect data [17, 18, 20–27, 29, 30], while two used focus-group interviews [19, 28]. The total number of participants was 262 (164 men and 98 women), with ages ranging from 49 to 86 years. Most people with COPD included in the review were white, lived with a spouse/partner or family and were retired from work. The advanced stages of the disease (severe and very severe) were the most studied. Five studies were conducted in North America (four in the USA and one in Canada) [19, 21, 27, 28, 30], five were conducted in Europe (two in the UK and one each in Ireland, Sweden and Finland) [17, 18, 20, 22, 26], one was conducted in Australia [23], two were conducted in Eastern Asia (Taiwan) [25, 29], and one was conducted in Western Asia (Turkey). The majority of the participants were recruited in community care settings. A more detailed description of the included studies is presented in Table 1.
3.1 Meta-Synthesis
Four synthesised findings were identified: (1) self-care of people with COPD is directed towards the prevention, control and management of the physical consequences of COPD; (2) self-care focuses on the management of the psychological effects of COPD; (3) self-care is aimed at reducing the impact of COPD on social life; and (4) self-care is influenced by contact with healthcare services and requires the acquisition of knowledge and skills. These four synthesised findings emerged from ten categories, which were obtained from the aggregation of 114 study findings (Table 2). Each finding was identified with an alphanumeric code, with letters representing the article and numbers representing the progressive findings retrieved (Table 2). One finding extracted from Sossai et al.’s article and four findings extracted from Nield’s study were excluded [23, 30], as they were considered to not be supported by the data.
3.1.1 Self-Care of People with COPD is Directed Towards the Prevention, Control and Management of the Physical Consequences of the Disease
People with COPD engage in self-care activities and implement strategies directed towards the prevention, control and management of the physical consequences of the disease. COPD causes respiratory and sleep problems, limits physical and daily life activities and involves frequent exacerbations. The severity of the physical consequences depends on the stage of the disease.
Self-care to prevent, control and manage the effects of the COPD on respiratory symptoms The most common respiratory symptoms of COPD include dyspnoea, coughing and phlegm [22, 23, 29]. Dyspnoea is the disease manifestation that causes the most worry for patients, with episodes ranging from shortness of breath (SOB) to severe respiratory impairment [27]. Dyspnoea considerably influences the lives of people with COPD, changing their priorities and causing anxiety and panic, which may worsen their symptoms [21, 23], and fear of death. As one patient underscored: “When I am out of breath, I think I will die…” [24].
The included studies identify several factors that provoke the dyspnoea attacks, including environmental conditions, such as pollution, dust, smoke, humidity and extreme external temperatures [22, 23, 25]; moderate or heavy physical activities, such as climbing stairs and carrying weights [27]; and emotions, such as anxiety and anger [21, 24, 29]. In addition, the incorrect use of drugs or breathing techniques has been recognised as a possible cause of SOB [24].
While dyspnoea is the symptom found to subjectively frighten patients the most, coughing and sputum have been found to be the COPD manifestations that cause the most embarrassment [22]. Knowing the triggers of dyspnoea allows sick people to engage in prevention activities, such as avoiding bending down to the floor while doing housework [24]; stopping or slowing physical activities [21, 30]; avoiding heavy work or other activities that have caused SOB in the past [18, 21]; remaining near their homes to allow them to return in the event of worsened conditions [25, 29]; and trying to relax [29]. People with COPD recognise the need to protect themselves from illness by avoiding people suffering from colds or flu and by dressing properly in the winter. One participant acknowledged the weather as a risk factor as follows: “The disease has something to do with the weather” [29].
People with COPD receive several types of advice for maintaining stable lung function from healthcare professionals. Advice aimed at stabilising the symptoms of COPD that was least likely to be followed included flu immunisations and exercises to promote lung expansion and strengthen chest muscles. Instead of performing their daily, prescribed exercises, many patients prefer alternative methods of exercise, such as Kung Fu, and sedentary activities [25, 28].
Tobacco smoking, pollution and chemical hazards have been recognised as possible causes of COPD [17, 22, 23, 29]. Although smoking cessation is considered important for decreasing symptoms, people with COPD do not always manage to stop smoking [23, 25].
People in oxygen therapy regulate their oxygen levels while performing physical activities to prevent SOB [27]. They also monitor their breathing using pulse oximeters [21].
When a dyspnoea attack occurs, individuals affected by COPD perform activities derived from their own experiences or learned from healthcare personnel. One frequent practice used to manage dyspnoea attacks is the use of inhalers or nebulisers [24, 27]. Many patients also learn to bring their medications with them at all times. As one patient described: “Like my American Express Card; I never leave home without it” [27].
Individuals with COPD recognise that, to be effective, inhalers must be used with the appropriate technique, which requires time to learn [18, 24] and can be difficult to implement during a dyspnoea episode: “When I’m panicking … it [inhalers] doesn’t do me any good, because I can’t breathe in and hold my breath long enough for it to be effective…” [27].
The controlled breathing technique, which may involve pursed lips or diaphragmatic breathing, is another method used to manage dyspnoea [25, 27]. Individuals with COPD know this technique well, even though it takes time to learn [30]. These individuals use specific positions to improve their lung expansion, such as sitting, leaning forward and elevating the shoulders [27]. Chinese patients reported using isometric and alternative physical exercises to improve their breathing, such as Shang Tung Kung Fu or Tai Chi [25, 29]. Moreover, when a dyspnoea episode occurs, people with COPD may stop their activities and rest as long as needed to resolve the episode [30].
Self-care to prevent and manage limitations in daily activities COPD forces people to modify their daily living and physical activities. As the disease progresses, people must adapt their daily tasks to reduced activity tolerance to keep their condition stable and avoid worsening their respiratory symptoms [17]. Affected daily tasks may include showering and bathing, house cleaning, yard maintenance and shopping. Some patients impute this reduced ability to the aging process instead of their COPD [18, 29]: “At the back of my mind also is the fact that I am 79 years old, in all probability the body isn’t so responsive at that age than it would be for a younger person” [18].
Many people engage in strategic planning for their day-to-day activities. As one man stated: “Planning and thinking ahead of time is the key. Knowing my limit is essential and being smart about the activities I do. Otherwise I would end up un well” [23].
Strategising about all daily tasks is a common approach to managing the symptoms of COPD. People often see modifying their daily routines as an effective method to reduce the burden of the disease [21–23, 26]. Furthermore, the use of assistive mobility devices improves patients’ ability to overcome physical limitations [21, 23]. These devices can vary from basic tools, such as wheel chairs or canes, to more complex tools, such as motorised shopping carts or a computer battery pack to power car nebulisers while travelling [21, 23].
Additional strategies may be used to compensate for losses in physical function. For example, people may reduce their activities or shift to more sedentary activities [24–26, 28, 29]. They may also integrate prescribed physical exercises into their daily living activities: “I’ve got to do my vacuuming, so I pick up the vacuum cleaner and use it to do my exercises, and when I’m cooking I do the arms out, [and with] reading, I sit right down or squat down [and] I do quarter squats” [28].
Continuing to work outside the home is also seen as a way to keep the body active [17, 25]: “Work is social and keeps you active … sometimes it’s difficult but you have to struggle … if you had been at home you would have been inactive” [17].
The severity of COPD influences the impact of the disease on daily activities [22]. However, even in the disease’s advanced stages, performing limited daily activities independently gives people with COPD pleasure [27, 29]. At the end of their COPD, when people are unable to perform daily self-care activities, their life standards decrease and they must depend on others: “Even taking bath alone at home becomes difficult. I am having difficulty when I raise my hands up to wash my hair […] Sometimes my daughter washes me” [24].
Asking for and accepting help from others forces people to reconsider the ways in which they perform their daily activities. Support from family and friends allows people affected by COPD to maximise their residual abilities, gain control and accept help when offered [24, 26, 27].
Self-care to manage sleeping problems Another symptom reported by people with COPD involves sleep disturbances. Individuals may have difficulty falling or staying asleep and experience sleepiness during the day [19, 23]. As one person reported:
“Yeah, I wake up like three or four times at night and it’s hard for me to get to sleep – same as she said. And once you get to sleep, it’s hard to stay asleep, and then I pay for it the next day ‘cause I be sleep […] drowsy and tired, you know? And I fall asleep on buses” [19].
Besides dyspnoea, humidity and stagnant air can also cause sleep disturbances [19, 23]. Sleeping difficulties can result in distressing thoughts. In particular, people with COPD report that staying awake leads to episodes of exacerbation and feelings of panic: “I’m willing to try anything because like I said, I’m scared. You know, I’m scared. I panic. When I can’t get that […] like I can push air out, but I can’t get it coming in and I panic” [19].
People with COPD develop different strategies to address their sleeping problems. For example, they may perform physical activities during the day to grow more tired, even if these activities are challenging given their condition [19]. They may also use fans or air conditioning year round to enhance the room climate or try to stay calm and control their thoughts by using meditation or doing breathing exercises [19].
Self-care to control and manage exacerbations of the disease During stable periods of the disease, people with COPD use ordinary self-care practices. However, during periods of exacerbation, they must engage in additional self-care practices and strategies to monitor and manage the disease [20]. During periods of exacerbation, patients evaluate their symptoms, such as sputum production and fever, by comparing them with their normal conditions [20, 21]. People with COPD learn to identify exacerbations by assessing symptoms, such as chest soreness, breathlessness and sensations of tightness or heaviness in their chest, that occur before the onset of more evident disease manifestations [20]. These subtle symptoms are perceived as the specific ways in which individuals’ bodies tell them that an exacerbation is developing [20].
When they identify an acute exacerbation, people use a variety of self-management behaviours. One of these involves using medications, such as oral steroids, antibiotics or over-the-counter medications: “Usually I go by the sputum. If it changes colour, I go on antibiotics and steroids” [20].
However, due to the possible occurrence of side effects, which can represent a barrier to medication adherence, the use of medications is not always perceived as positive. Moreover, some patients prefer postponing the use of medications in the hopes that their bodies can overcome the exacerbations without help: “I don’t really want to take too many things if you can get better without it” [20].
An adequate level of knowledge is necessary for patients to feel confident in using medication: “I just presumed I did right … but then again, would it got so bad if I’d gone earlier?” [18].
When self-management attempts fail, people use different strategies, such as promptly seeking professional healthcare help [20, 21, 25], procrastinating in contacting healthcare providers [21] or delaying the decision until someone else (e.g. a family member) makes it for them [21, 28].
3.1.2 Self-Care Focuses on the Management of the Psychological Effects of COPD
The emotional wellbeing of people affected by COPD is compromised by the disease, which causes depression, anxiety, embarrassment and frustration over the loss of independence. Therefore, self-care must also focus on managing the emotional disturbances caused by COPD.
Impact on emotional wellbeing People in the initial stages of COPD often try to hide their condition from others, and even themselves, in their attempt to continue with their normal lives [18, 22]. These individuals may present with depression and anxiety both at the time of diagnosis and over the whole course of the disease. Furthermore, their progressive loss of independence decreases their emotional wellbeing, and their negative feelings may influence their activity levels [22, 23], preventing them from engaging in meaningful activities: “It [COPD] interferes with every aspect of my life. Even when I go out, I know people are looking at me thinking that poor sickly bastard, it makes me feel embarrassed” [23].
During advanced stages of the disease, people with COPD are no longer able to hide their symptoms. At this point, many cut out all social activities, resulting in a social isolation that worsens their mood and quality of life [24, 27]. A person with very severe COPD defined his/her quality of life as follows: “The only word I can say is poor” [27].
Self-care to manage emotional discomfort To handle negative emotions, people with COPD apply different strategies, such as finding a balance between acceptance and capitulation [17]; replacing activities with new, more significant activities, such as taking part in social events and socialising with family and friends [17]; and accepting the limitations imposed by the disease [17, 25]. One person expressed his feelings in this way: “First thing is for a person, if diagnosed with this disease [is] to accept it. To accept your problem is half the battle. If you don’t well, you’ll become a basket case” [28].
People with COPD can get used to their symptoms and turn their negative feelings into positive ones [17, 25, 28, 30]. Laughing can help people deal with the disease more positively: “Laughter is very important, I think about the best exercise there is for people with lung problems” [28].
Other important strategies include self-talk activities [28, 30], imagination and spirituality [30]. At the end stages of the disease, patients’ families are often their only reasons for continuing to live, and self-care activities may be performed solely in order to remain alive for the sake of family [28].
3.1.3 Self-care is aimed at reducing the impact of COPD on social life
Self-care may also be aimed at reducing the impact of COPD on social activities. COPD influences the social and family lives of those it affects, forcing them to renegotiate their family and social activities. These limitations require the use of personal and external resources to reduce the burden of the disease.
Impact of COPD on social life The manifestations of COPD often interfere with people’s social activities outside the home, and they can decide to limit or cancel them [26]. The expectations of family members and friends to continue a normal social life often lead to feelings of frustration, embarrassment and exclusion. In addition, people with COPD may decide to retire from social life following their diagnosis. As one man reported:
“Since I got this, I don’t socialize at all. You don’t want to sit around having people looking at you and only seeing your sickness and what you might not be able to get involved in because of it. The way I see it, you’re better off not going anywhere at all” [23].
Self-care to manage social life modifications People adopt different self-care strategies to reduce the effects of the disease on their social lives. The need to limit or avoid certain activities forces them to renegotiate their social or family roles. People with COPD may transfer their activities or roles to their partners or other family members, which may affect family relationships [18, 23]. This is especially true for male participants, since it is not always easy to transfer typical masculine activities from husband to wife [18, 23].
People with COPD consider it an invisible disease. At first, they try consciously to hide the disease; however, in so doing, they often make it difficult for others to believe the severity of their symptoms: “Because I don’t look as though I’m ill, the upsetting thing is that people don’t believe you, they think you’re putting it on, sometimes even friends and family” [18].
People who attend rehabilitation courses or join peer support groups find their involvement very effective in improving their self-care. In fact, their participation improves their motivation and information and enhances their capacity to solve problems from an insider point of view [26, 28]. As one person pointed out: “You get an incentive to try and help yourself more when you see what other people have done, you say okay, maybe I should try this, maybe I should try that…” [28].
3.1.4 Self-Care is Influenced by Contact with Healthcare Services and Requires the Acquisition of Knowledge and Skills
Self-care is a lifelong learning process influenced by personal experiences and contact with healthcare services and providers. To perform self-care behaviours to maintain the stability of the disease and manage the symptoms, people must acquire new knowledge and skills during each of the disease’s different stages.
Contact with healthcare services Contact with healthcare services and continuity of care are considered important by people with COPD [17]. Patients report that the accessibility, responsiveness and flexibility of healthcare services are essential for increasing their self-care abilities [22]. Healthcare providers are seen as the individuals responsible for not only their physical health, but also their psychological wellbeing [26, 28]. The information provided by healthcare services and alliances with healthcare providers is important because it improves self-decision making in the management of COPD. As one patient noted:
“As you work with your doctor, he said you know let’s work together and we’ll try to eliminate some of your medication. Well [now] I’m down on my medication [dosage] so you have to work with your doctor” [28].
Acquisition of new knowledge and skills for self-care A lack of knowledge about how to monitor symptoms and what to do in the event of exacerbations negatively influences engagement in self-care behaviours [18]. When people feel that the information provided by healthcare professionals is insufficient, they use alternative sources of information [21, 23], such as the Internet: “So I did my own research on the Internet just to make sense of what they were all saying was happening to my body and to see what other things were available that could help me get better” [23].
Even if healthcare providers offer appropriate education, people with COPD tend to use their own experiences to strengthen their self-care skills. They report that some activities and strategies are performed without formal instruction from healthcare professionals. Examples may include adapting activities to accommodate breathlessness and distracting oneself from symptoms when they occur [18]. These strategies are learnt on a ‘trial and error’ basis; only those strategies that work become effective self-care activities [18, 21]. Some mediating factors, such as COPD severity and the presence of comorbidities, may influence self-care behaviours, and high levels of knowledge and skills enhance self-care behaviours [22].
To give a complete overview of the behaviours and strategies performed by people with COPD investigated in our review, we extracted the activities and the strategies from the study findings and synthesised them for each category identified by the reviewers. These synthesised findings are presented in Table 3.
4 Discussion
This meta-synthesis has identified the self-care behaviours and strategies performed by people affected by COPD.
People living with COPD have primary responsibility for their own care. These individuals use personal self-care behaviours combined with the recommendations of their healthcare professionals. The main self-care activities of people with COPD, especially during advanced stages of the disease, are performed to prevent, control and manage the physical effects of the disease, including, particularly, the respiratory problems [32]. Dyspnoea is the most worrisome symptom for most people with COPD. It causes panic, distress and desperation and limits daily activities and social life [33]. People use several strategies to prevent dyspnoea episodes, including pacing and planning activities, controlling air quality and avoiding exposure to extreme weather conditions. Strategies focused on limiting the physical effects of COPD are essential for preventing deconditioning and worsening symptoms [34, 35]. Like other studies, our review shows that efforts to understand the main triggers of dyspnoea and avoid its occurrence represent the most challenging self-care behaviours [36]. One of the most challenging self-care skills that people with COPD must acquire is the ability to recognise the onset of disease exacerbations. However, while individuals use several strategies to prevent the onset of dyspnoea, they use only a few strategies to monitor their disease [32]. The self-ability to identify exacerbations is fundamental to disease control, since the successful identification of an acute episode can reduce hospitalisations and the deterioration of health status [37].
Maintaining physical activity and exercising are fundamental for minimising the impact of COPD on people’s lives. Despite this, physical inactivity is common, which contributes to worsening patients’ outcomes [38]. In our review, different physical activities were reported by participants from Western and Eastern countries. Usually, in Western countries, aerobic exercises, such as running, walking or cycling, are performed, while, in Asian countries, isometric traditional exercises, such as Shang Tung Kung Fu or Tai Chi, are used. The isometric practices seem to be more effective in improving physical performance quality and other outcomes in people with COPD, as shown in recent meta-analyses [39, 40].
Identifying and managing symptoms are not sufficient for effective self-care. As with other chronic conditions, self-care behaviours must focus on improving everyday life, rather than solely managing possible crises [41]. For this reason, self-care in day-to-day activities is important, as self-care is focused on promoting and maintaining health, such as smoking cessation and regular physical activity [42, 43].
To address the psychological effects of the disease, people affected by COPD use different strategies. Coping strategies used with chronic diseases can be either emotion focused or problem focused [44]. Emotion-focused coping strategies are used when the disease is considered to fall outside the control of the sick person; such strategies focus on disease stressors and aim to reduce negative emotional responses. Emotion-focused coping strategies may include, as reported in our review, suppressing negative thoughts or emotions and distracting oneself with social activities. By contrast, problem-focused strategies aim to reduce the causes of stressful situations. The most commonly used problem-focused strategy in our review was using social support to cope with the disease. Emotion-focused strategies are often less effective than problem-focused strategies in relation to health outcomes, especially in cases of chronic diseases [45–47]. As identified in our review and confirmed in the literature [1], people affected by COPD often suffer from depression and anxiety, both at the time of diagnosis and throughout the course of the disease. This might be the cause of frequent use of emotion-focused strategies, as reported by Nes and Segerstrom [48]. For these reasons, knowledge on successful coping strategies, as provided by an insider perspective, could be useful in helping healthcare professionals promote personalised and adaptive coping strategies [49].
To overcome the social impact of COPD, individuals often adapt their social lives to the disease’s different manifestations and stages of the disease. People with COPD must often renegotiate their roles inside their families. Despite their difficulties performing normal activities, people do not want to be seen as needy and often reluctantly seek the help of others [50]. Therefore, their self-care behaviours are aimed at continuing to live independently; in this way, self-care is a key motivator for people with COPD [12]. Understanding the personal behaviours of people with COPD could help to identify broader aspects of self-care to better define which kinds of self-care support are needed [51].
In line with the results of Jordan et al.’s review [52], our review showed that the support of healthcare professionals and the availability of healthcare services are directly linked to self-care skills and behaviours. Healthcare providers contribute to enhancing the self-care decision making of people with COPD and are responsible for both their physical and their psychological wellbeing. Self-care is a complex, multicomponent process in which continuous professional support from healthcare professionals is necessary to maintain behavioural changes and improve health outcomes. Moreover, the more the disease progresses, the more complex the decision-making process becomes. This results in different self-care approaches during different disease stages, ranging from autonomously initiated self-care behaviours during early stages to completely dependent care provided by caregivers during the last stages [53].
The research has shown that educational interventions are effective in improving health-related quality of life and reducing hospital readmissions and dyspnoea [4, 54]. However, educational programmes are heterogeneous in content and methods, making it difficult to identify which self-care behaviours are responsible for effective outcomes [52]. Furthermore, in most existing educational programmes, a variety of healthcare professionals are responsible for providing self-care education and assessing programme effectiveness [4]. Future research should be conducted to understand how to tailor education interventions in the different stages of the disease to motivate people towards self-care behaviours. Furthermore, since self-care is a complex process, further efforts are needed to identify self-care behaviours that are effective in different population groups with COPD, for example, people with different ages, genders, social conditions and educational levels, and how they can be incorporated into clinical guidelines. The results of our qualitative review could be integrated with the results of quantitative research to develop more comprehensive clinical guidelines that consider the knowledge progression in the disease treatment, as well as the individual’s preferences and priorities.
4.1 Implications for Clinical Practice
Since self-care is essential for managing chronic conditions and for maintaining independence, understanding how people care for themselves can improve self-care education programmes. Healthcare professionals should recognise and understand people’s orientations and expectations that are highlighted in the qualitative evidence to create individualised self-care education plans. For example, healthcare providers should not only focus on training patients regarding the correct utilisation of inhalators or assistive devices and technology, teaching respiratory exercises, providing an action plan in case of exacerbation and informing them on the importance of smoking cessation. The treatment of the chronic disease and the prevention of its physical effects is not the most important aim for people with COPD, as it is for the healthcare providers. COPD patients mainly want to continue living full and satisfying lives for as long as possible, despite the effects of the disease. In fact, people affected by COPD want help in dealing with the disease’s emotional impact and the social and familial changes it imposes as it progresses. They need to be motivated to make changes in many aspects of their lives and to discover effective coping strategies. For example, healthcare professionals can negotiate with people with COPD regarding the social activities that can be conducted in or outside their home and can find new ways for the individuals with COPD to maintain a meaningful social and family life. It is also possible to consider the preferences and needs of the specific patients involved in a group educational programme and then tailor the educational interventions accordingly. A preliminary evaluation of the requests and the preferences of the people with COPD should be carried out to shape the interventions to their real needs, without providing pre-built educational programmes. At different stages of the disease, people need to acquire more complex knowledge and skills, depending on the treatment requirements or effects of the disease; consequently, different self-care behaviours and strategies are required. The availability of this evidence and the improvement in the disease treatment does not ensure the implementation of the recommended practices by healthcare professionals. Internal factors, such as attitudes, perceptions and knowledge, as well as external factors, including guidelines’ format and usability, resources and organisational culture, can influence the use of clinical guidelines in practice [55]. The integration of qualitative evidence into clinical guidelines could facilitate their use, as the perception of not providing individualised care could be overcome.
4.2 Limitations
Our review has a few limitations. Although a number of databases and languages were searched, studies indexed in other databases and written in other languages may have been overlooked. Moreover, self-care is a broad concept with different theorisations, and even if this review encompassed the most common terms to indicate self-care, it is possible that papers using other terms and different theoretical approaches have been excluded. Furthermore, our results mainly reflect the self-care of selected populations of Western countries, and self-care behaviours performed in other countries are only partially represented. This makes it difficult to transfer our results to populations from other geographical areas. As self-care is affected by social and cultural factors, self-care practices derived from different cultural habits and beliefs might not be represented in our review [56, 57]. Since no study has explicitly analysed self-care in people with COPD with different genders, education levels and social or marital statuses, it was not possible to stratify the findings for such factors or to determine related differences in self-care practices. Despite these limitations, our paper is the first meta-synthesis describing the experiences of self-care of people with COPD.
5 Conclusions
This meta-synthesis provides qualitative evidence on the self-care behaviours that individuals affected by COPD perform to face the physical, psychological and social effects of the disease. The self-care strategies used by people with COPD are developed through a continuous learning process that can be facilitated by the support of the healthcare providers. Moreover, the deep understanding of the self-care experiences of individuals with COPD provided by this review could help healthcare professionals to improve educational programmes, integrating people’s preferences and expectations with clinical recommendations.
References
Global Initiative For Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2016. http://www.goldcopd.org. Accessed 15 Oct 2016.
Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Global Health. 2015;5(2):020415. doi:10.7189/jogh.05-020415.
World Health Organization. Global health estimates: projection of deaths by cause, age and sex, by world bank income group and WHO region. 2013. http://www.who.int/healthinfo/global_burden_disease/en/. Accessed 15 Oct 2016.
Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014(3):CD002990. doi:10.1002/14651858.CD002990.pub3.
Riegel B, Jaarsma T, Stromberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012;35(3):194–204. doi:10.1097/ANS.0b013e318261b1ba.
Riegel B, Dickson VV, Faulkner KM. The situation-specific theory of heart failure self-care: revised and updated. J Cardiovasc Nurs. 2016;31(3):226–35. doi:10.1097/JCN.0000000000000244.
Effing TW, Bourbeau J, Vercoulen J, Apter AJ, Coultas D, Meek P, et al. Self-management programmes for COPD: moving forward. Chronic Respir Dis. 2012;9(1):27–35. doi:10.1177/1479972311433574.
Lomundal BK, Steinsbekk A. Five-year follow-up of a one-year self-management program for patients with COPD. Int J Chronic Obstr Pulm Dis. 2012;7:87–93. doi:10.2147/COPD.S27352.
Monninkhof E, van der Aa M, van der Valk P, van der Palen J, Zielhuis G, Koning K, et al. A qualitative evaluation of a comprehensive self-management programme for COPD patients: effectiveness from the patients’ perspective. Patient Educ Couns. 2004;55(2):177–84. doi:10.1016/j.pec.2003.09.001.
Sohanpal R, Steed L, Mars T, Taylor SJ. Understanding patient participation behaviour in studies of COPD support programmes such as pulmonary rehabilitation and self-management: a qualitative synthesis with application of theory. NPJ Primary Care Respir Med. 2015;25:15054. doi:10.1038/npjpcrm.2015.54.
Harrison SL, Janaudis-Ferreira T, Brooks D, Desveaux L, Goldstein RS. Self-management following an acute exacerbation of COPD: a systematic review. Chest. 2015;147(3):646–61. doi:10.1378/chest.14-1658.
Pinnock H, Steed L, Jordan R. Supported self-management for COPD: making progress, but there are still challenges. Eur Respir J. 2016;48(1):6–9. doi:10.1183/13993003.00576-2016.
Rycroft-Malone J, Burton CR. The synthesis of qualitative data. In: Richards DA, Hallberg IR, editors. Complex interventions in health: an overview of research methods. London: Routledge Taylor & Francis Group; 2015. p. 80–7.
Joanna Briggs Institute. Reviewers’ manual. 2014. http://joannabriggs.org/assets/docs/sumari/ReviewersManual-2014.pdf. Accessed 15 Oct 2016.
Hannes K, Lockwood C. Synthesizing qualitative research: choosing the right approach. Chichester: BMJ Books-Wiley-Blackwell; 2012.
Thomas LA. Effective dyspnea management strategies identified by elders with end-stage chronic obstructive pulmonary disease. Appl Nurs Res ANR. 2009;22(2):79–85. doi:10.1016/j.apnr.2007.04.010.
Stridsman C, Zingmark K, Lindberg A, Skar L. Creating a balance between breathing and viability: experiences of well-being when living with chronic obstructive pulmonary disease. Primary Health Care Res Dev. 2015;16(1):42–52. doi:10.1017/S1463423614000048.
Apps LD, Harrison SL, Williams JE, Hudson N, Steiner M, Morgan MD, et al. How do informal self-care strategies evolve among patients with chronic obstructive pulmonary disease managed in primary care? A qualitative study. Int J Chronic Obstr Pulm Dis. 2014;9:257–63. doi:10.2147/COPD.S52691.
Kauffman KS, Doede M, Diaz-Abad M, Scharf SM, Bell-Farrell W, Rogers VE, et al. Experience of insomnia, symptom attribution and treatment preferences in individuals with moderate to severe COPD: a qualitative study. Patient Prefer Adher. 2014;8:1699–704. doi:10.2147/PPA.S71666.
Williams V, Hardinge M, Ryan S, Farmer A. Patients’ experience of identifying and managing exacerbations in COPD: a qualitative study. NPJ Primary Care Respir Med. 2014;24:14062. doi:10.1038/npjpcrm.2014.62.
Brandt CL. Study of older adults’ use of self-regulation for COPD self-management informs an evidence-based patient teaching plan. Rehabil Nurs Off J Assoc Rehabil Nurses. 2013;38(1):11–23. doi:10.1002/rnj.56.
Cooney A, Mee L, Casey D, Murphy K, Kirwan C, Burke E, et al. Life with chronic obstructive pulmonary disease: striving for ‘controlled co-existence’. J Clin Nurs. 2013;22(7–8):986–95. doi:10.1111/j.1365-2702.2012.04285.x.
Sossai K, Gray M, Tanner B. Living with chronic obstructive pulmonary disease: experiences in northern regional Australia. Int J Ther Rehabil. 2011;18(11):631–42.
Avsar G, Kasikci M. Living with chronic obstructive pulmonary disease: a qualitative study. Aust J Adv Nurs. 2010;28(2):46–52.
Chen KH, Chen ML, Lee S, Cho HY, Weng LC. Self-management behaviours for patients with chronic obstructive pulmonary disease: a qualitative study. J Adv Nurs. 2008;64(6):595–604. doi:10.1111/j.1365-2648.2008.04821.x.
Karnevisto M, Kaistila T, Paavilainen E. Severe chronic obstructive pulmonary disease in a family’s everyday life in Finland: perceptions of people with chronic obstructive pulmonary disease and their spouses. Nurs Health Sci. 2007;9(1):40–7.
Fraser DD, Kee CC, Minick P. Living with chronic obstructive pulmonary disease: insiders’ perspectives. J Adv Nurs. 2006;55(5):550–8. doi:10.1111/j.1365-2648.2006.03946.x.
Cicutto L, Brooks D, Henderson K. Self-care issues from the perspective of individuals with chronic obstructive pulmonary disease. Patient Educ Couns. 2004;55(2):168–76. doi:10.1016/j.pec.2003.08.012.
Jeng C, Tsao LI, Ho CH, Chang PC. Experiences of daily activities within two weeks after hospital discharge among Taiwanese elderly patients with chronic obstructive pulmonary disease. J Nurs Res JNR. 2002;10(3):168–76.
Nield M. Dyspnea self-management in African Americans with chronic lung disease. Heart Lung J Crit Care. 2000;29(1):50–5.
Patton M. Qualitative evaluation and research methods. 3rd ed. Newbury Park, CA: Sage publications; 2002.
Kaptein AA, Fischer MJ, Scharloo M. Self-management in patients with COPD: theoretical context, content, outcomes, and integration into clinical care. Int J Chronic Obstr Pulm Dis. 2014;9:907–17. doi:10.2147/COPD.S49622.
Braido F, Baiardini I, Menoni S, Bagnasco AM, Balbi F, Bocchibianchi S, et al. Disability in COPD and its relationship to clinical and patient-reported outcomes. Curr Med Res Opin. 2011;27(5):981–6. doi:10.1185/03007995.2011.563285.
Jorgensen LB, Dahl R, Pedersen PU, Lomborg K. Evaluation of a multi-modal grounded theory approach to explore patients’ daily coping with breathlessness due to chronic obstructive pulmonary disease. J Res Nurs. 2013;18(5):423–40.
Pooler C. Living with chronic lower pulmonary disease: disruptions of the embodied phenomenological self. Global Qual Nurs Res. 2014;1:1–11.
Christenbery TL. Dyspnea self-management strategies: use and effectiveness as reported by patients with chronic obstructive pulmonary disease. Heart Lung J Crit Care. 2005;34(6):406–14. doi:10.1016/j.hrtlng.2005.07.005.
Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060. doi:10.1136/bmj.e1060.
McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015(2):CD003793. doi:10.1002/14651858.CD003793.pub3.
Guo JB, Chen BL, Lu YM, Zhang WY, Zhu ZJ, Yang YJ, et al. Tai Chi for improving cardiopulmonary function and quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clin Rehabil. 2016;30(8):750–64. doi:10.1177/0269215515604903.
Luo X, Zhang J, Castelberg R, Wu T, Yu P, He C, et al. The effects of traditional Chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. PLoS One. 2016;11(9):e0161564. doi:10.1371/journal.pone.0161564.
Parke HL, Epiphaniou E, Pearce G, Taylor SJ, Sheikh A, Griffiths CJ, et al. Self-management support interventions for stroke survivors: a systematic meta-review. PLoS One. 2015;10(7):e0131448. doi:10.1371/journal.pone.0131448.
Garcia-Aymerich J, Pitta F. Promoting regular physical activity in pulmonary rehabilitation. Clin Chest Med. 2014;35(2):363–8. doi:10.1016/j.ccm.2014.02.011.
Tonnesen P. Smoking cessation and COPD. Eur Respir Rev Off J Eur Respir Soc. 2013;22(127):37–43. doi:10.1183/09059180.00007212.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychol Bull. 2009;135(1):121–41. doi:10.1037/a0014210.
Duangdao KM, Roesch SC. Coping with diabetes in adulthood: a meta-analysis. J Behav Med. 2008;31(4):291–300. doi:10.1007/s10865-008-9155-6.
Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: a meta-analytic review. J Behav Med. 2002;25(6):551–603.
Nes LS, Segerstrom SC. Dispositional optimism and coping: a meta-analytic review. Pers Soc Psychol Rev Off J Soc Pers Soc Psychol Inc. 2006;10(3):235–51. doi:10.1207/s15327957pspr1003_3.
Ersek M, Turner JA, Kemp CA. Use of the chronic pain coping inventory to assess older adults’ pain coping strategies. J Pain Off J Am Pain Soc. 2006;7(11):833–42. doi:10.1016/j.jpain.2006.04.002.
Kendall M, Buckingham S, Ferguson S, MacNee W, Sheikh A, White P et al. Exploring the concept of need in people with very severe chronic obstructive pulmonary disease: a qualitative study. BMJ Support Palliat Care. 2015. doi:10.1136/bmjspcare-2015-000904.
Bourbeau J, Lavoie KL, Sedeno M. Comprehensive self-management strategies. Semin Respir Crit Care Med. 2015;36(4):630–8. doi:10.1055/s-0035-1556059.
Jordan RE, Majothi S, Heneghan NR, Blissett DB, Riley RD, Sitch AJ, et al. Supported self-management for patients with moderate to severe chronic obstructive pulmonary disease (COPD): an evidence synthesis and economic analysis. Health Technol Assess. 2015;19(36):1–516. doi:10.3310/hta19360.
Rijken M, Jones M, Heijmans M, Dixon A. Supporting self-management. In: Nolte E, McKee M, editors. Caring for people with chronic conditions: a health system perspective. Berkshire: Open University Press; 2008. p. 116–42.
Jonkman NH, Westland H, Trappenburg JC, Groenwold RH, Bischoff EW, Bourbeau J, et al. Characteristics of effective self-management interventions in patients with COPD: individual patient data meta-analysis. Eur Respir J. 2016;48(1):55–68. doi:10.1183/13993003.01860-2015.
Jun J, Kovner CT, Witkoski Stimpfel A. Barriers and facilitators of nurses’ use of clinical practice guidelines: an integrative review. Int J Nurs Stud. 2016;60:54–68. doi:10.1016/j.ijnurstu.2016.03.006.
Riegel B, Vaughan Dickson V, Goldberg LR, Deatrick JA. Factors associated with the development of expertise in heart failure self-care. Nurs Res. 2007;56(4):235–43. doi:10.1097/01.NNR.0000280615.75447.f7.
Tseng J, Halperin L, Ritholz MD, Hsu WC. Perceptions and management of psychosocial factors affecting type 2 diabetes mellitus in Chinese Americans. J Diabetes Complicat. 2013;27(4):383–90. doi:10.1016/j.jdiacomp.2013.01.001.
Author contributions
MC and MM were responsible for the conception and design of the study, the acquisition, analysis and interpretation of data, and drafted the manuscript. DI contributed to data acquisition and analysis. MGM critically reviewed the manuscript for important intellectual content. All the authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
M. Clari, M. Matarese, D. Ivziku and M. G. De Marinis declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Clari, M., Matarese, M., Ivziku, D. et al. Self-Care of People with Chronic Obstructive Pulmonary Disease: A Meta-Synthesis. Patient 10, 407–427 (2017). https://doi.org/10.1007/s40271-017-0218-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-017-0218-z