Abstract
Background
Hypogonadism, or low testosterone, is a common disorder. There are currently no patient-reported outcome (PRO) instruments designed to comprehensively evaluate the symptoms of hypogonadism and to detect changes in these symptoms in response to treatment.
Objective
The purpose of this study was to develop a PRO instrument, the Hypogonadism Impact of Symptoms Questionnaire (HIS-Q) and to assess its content validity.
Methods
A literature review, expert clinician input, and qualitative concept elicitation with 39 male hypogonadism patients (four focus groups: n = 25; individual interviews: n = 14; mean age 52.3 ± 14.3 years) from the USA were used to develop the draft HIS-Q. Subsequent cognitive interviews (n = 29; mean age 51.5 ± 15.4 years) were used to evaluate content validity.
Results
Emergent discussion with participants yielded symptoms within the sexual, physical, energy, sleep, cognition, and mood domains. Low libido and tiredness were most commonly reported. The initial version of the HIS-Q includes 53 items that were consistently understood by the participants, who found the instrument to be relevant to their experiences with hypogonadism and comprehensive in the content coverage of symptoms.
Conclusion
The HIS-Q is a comprehensive PRO measure of hypogonadism symptom severity in males. Its design elements, including the response options and recall period, were suitable, and content validity was confirmed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A patient-reported outcome measure to evaluate the symptoms of hypogonadism has been developed on the basis of direct input from patients and in accordance with regulatory guidelines. |
The draft Hypogonadism Impact of Symptoms Questionnaire (HIS-Q) is intended to evaluate changes in hypogonadism symptoms in response to treatment in clinical or clinical trial settings. |
The draft measure is content valid and includes sexual, physical, energy, sleep, cognition, and mood domains. |
1 Introduction and Aims
Hypogonadism, or low testosterone, in males is often associated with low libido, erectile dysfunction (ED), irritability, psychological problems, and other symptoms. Hypogonadism occurs frequently in the general population; approximately 5.6 % of men between 30 and 79 years of age are symptomatic, with marked increases in prevalence among older men [1]. Clinically, hypogonadism is diagnosed through patients’ reports of their symptoms and laboratory testing, including a blood sample for serum testosterone determination [2]. Hypogonadism often results in decrements in quality of life and sexual dysfunction [3].
Patient-reported symptoms of hypogonadism often comprise a variety of physical and psychological complaints. Many symptoms of hypogonadism are known best to patients (e.g., sexual functioning, mood, sleep); therefore, symptom severity and changes after treatment may be most accurately assessed through the patients’ self-reports. There are several existing instruments that have been used to evaluate men with low testosterone, including sexual functioning questionnaires [4, 5], a 7-day diary to assess psychosexual functioning [6], several self-report measures that were designed primarily for screening for hypogonadism [7–11], and a general assessment of the symptoms associated with aging [12, 13]. None of these instruments was specifically designed to comprehensively evaluate the symptoms of hypogonadism and to detect changes in these symptoms in response to treatment. From conception, the development of the Hypogonadism Impact of Symptoms Questionnaire (HIS-Q) was conducted according to published US Food and Drug Administration (FDA) guidelines and International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Guidelines for development of patient-reported outcome (PRO) measures to be used as clinical trial endpoints [14–16].
The objective of this study was to design a PRO instrument that could be used to evaluate treatments for hypogonadism in clinical studies of men with low testosterone. Such a measure may also eventually prove useful in screening for, and assessing, the severity of hypogonadism in clinical and research settings.
2 Methods
2.1 Design and Study Sample
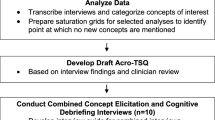
The instrument development included a literature review, input from expert clinicians, and qualitative interviews/focus groups with 65 male participants from the USA (Fig. 1). The inclusion and exclusion criteria were similar to those used for clinical trials. The inclusion criteria included male sex; age ≥18 years; clinical diagnosis of hypogonadism; serum total testosterone level <300 ng/dL; and ability to read, speak, and understand English. Participants in the first two phases of qualitative work either were androgen-therapy naïve, were not currently on androgen therapy, or had been on androgen therapy for <6 months. Participants in all phases were excluded if they had an abnormal finding on digital rectal examination; had a prostate-specific antigen (PSA) level of >2.5 ng/mL; had undergone radical prostatectomy; had a degenerative central nervous system disease or spinal cord injury; had any clinically significant neurological, hematological, autoimmune, endocrine, cardiovascular, liver, renal, gastrointestinal, pulmonary, psychiatric (including anxiety, major depressive disorder, drug or alcohol abuse) or infectious disease; or had a history of sleep apnea. Participants were recruited through eight geographically diverse clinical sites.
The first phase included focus groups and individual telephone interviews for the purposes of concept elicitation (n = 30) and subsequent cognitive interviewing (n = 21) on the draft instrument. Cognitive interviews are qualitative interviews with the objective of assessing patients’ overall understanding and the acceptability of a draft instrument, including the instructions, recall period, draft items, response options, and content coverage. On the basis of feedback from regulatory agencies, additional in-person concept elicitation interviews (n = 6) were conducted in the second phase with a younger sample of male patients (aged <55 years), who had lower testosterone levels (<250 ng/dL on at least two occasions, or <225 ng/dL on at least one occasion); these men were not on testosterone therapy or ED medications, and they had a body mass index (BMI) of ≤30. The third and final phase of work included additional cognitive interviews (n = 8), including three participants with congenital hypogonadism who completed the concept elicitation and cognitive components of the interview (Fig. 1).
2.2 Procedures
Figure 1 shows a flow chart of the steps in the HIS-Q instrument development process. Concept elicitation was achieved through focus groups and interviews using semi-structured interview guides aimed at spontaneous elicitation of symptoms related to hypogonadism. Subsequent probes were also included to explore symptoms within the sexual, mood, cognitive, and physical domains. Participants who had been on treatment for low testosterone were asked about changes in their symptomatology they had experienced during treatment (see the Electronic Supplementary Material, available online).
The four focus groups each comprised 5–8 male patients (n = 25) and were conducted by the same experienced moderator (MKV) and trained assistant (KDS). Eleven individual concept elicitation interviews were conducted either over the telephone (n = 5) or in person (n = 6). Three additional qualitative interviews were conducted with congenital hypogonadism participants, yielding a total combined concept elicitation sample of 39 subjects. Data were collected and analyzed until saturation was reached, defined as the point at which no substantially new themes, descriptions of a concept, or terms were introduced as additional focus groups or interviews were conducted [17]. Draft questions and response options were developed on the basis of the results of the initial open-ended concept elicitation phases of work.
Cognitive interviews to evaluate the content validity of the draft instrument were conducted in three iterative rounds. The first cognitive interviews included completion of the paper-and-pencil instrument (n = 9) or an electronic version of the instrument on tablet computers (n = 12). These interviews were used to reduce the item pool through evaluation of the item relevance and redundancy, and were aimed at evaluating the content validity of the instructions and items, including assessment of item comprehension, content coverage, appropriateness of the recall period and response options (see the Electronic Supplementary Material, available online). An additional round of interviews was conducted (n = 8), aimed at confirming the concept coverage, evaluating minor changes to the instrument, and gathering additional data on the content validity of the instrument among specific subsamples. Specifically, younger men and patients with congenital hypogonadism were interviewed to determine whether the concepts and items that had been identified were relevant and consistent among these subgroups of patients who experienced testosterone deficiencies from a young age into adulthood and were underrepresented in the original sample. These additional eight participants increased the sample size and were helpful in further testing the content validity of the instrument.
2.3 Measures
Participants were scored on the Aging Males Symptoms Scale (AMS) [12, 18]. The AMS yields scores for psychological, somatic, and sexual subscales, and a total score; higher scores indicate a greater degree of symptom severity and can be categorized on the basis of reference scores [19]. The AMS has been used previously to characterize the symptoms experienced by men with hypogonadism and to evaluate responses to treatment in clinical studies, although it was not explicitly designed for this purpose [13, 20–23]. Participants also completed a sociodemographic and clinical questionnaire. For each patient enrolled in the cognitive interview phase of the work, the site staff completed a clinical form, which gathered information on the hypogonadism diagnosis, etiology, and prior treatment of the participants.
2.4 Analyses
Qualitative data were analyzed using qualitative analysis software (ATLAS.ti; version 5.0) [24]. Data from the interviews were analyzed using thematic analysis. A coding dictionary was created and continually updated with codes emerging during the analysis process. A saturation grid was developed to document the concepts endorsed by each participant or focus group. The saturation grid was used to confirm the point at which saturation was reached and no new concepts were identified with additional focus groups or interviews.
Descriptive statistics were calculated for the sociodemographic and clinical questionnaire, the AMS, and the clinical items, using SAS version 9.1.3 software.
3 Results
3.1 Participant Characteristics
3.1.1 Concept Elicitation Participants
The mean age of the concept elicitation participants was 52.3 ± 14.3 years [range 25.0–84.0], and the men were of diverse race (Table 1). The mean of the patients’ lowest recorded testosterone levels was 192.9 ± 48.5 ng/dL, and the patients had been diagnosed with hypogonadism for 2.7 ± 2.6 years [range 0.0–11.8] (Table 2). Additional demographic and clinical information is presented in Tables 1 and 2. The demographic and clinical characteristics of the men were similar to those of men participating in prior clinical trials of testosterone replacement therapy [25]. The mean total AMS score for the concept elicitation participants was 39.9 ± 10.2; their subscale scores were 10.1 (moderate) for the psychological subscale, 16.4 (moderate) for the somatic subscale, and 12.9 (severe) for the sexual subscale.
3.1.2 Cognitive Interview Participants
The mean age of the cognitive interview participants was 51.5 ± 15.4 years [range 25.0–86.0], and they included men of diverse race (Table 1). The mean AMS score for the cognitive interview participants was 35.0 ± 11.4 (little impairment); subscale scores were 9.1 (moderate) for the psychological subscale, 14.3 (moderate) for the somatic subscale, and 11.2 (severe) for the sexual subscale.
3.2 Concept Elicitation Results
To start each focus group discussion, participants were asked to describe symptoms they experienced related to their hypogonadism. Sexual symptoms were the most frequently noted symptoms; they were mentioned first in all four focus groups and in five of the 11 individual interviews (Fig. 2). The results from the primary concept elicitation phase among 36 participants yielded six symptom domains: sexual, physical, energy, sleep, cognition, and mood symptoms (Fig. 3). The sexual symptoms fitted into three broad categories: sexual desire, sexual functioning, and sexual pleasure. The most commonly reported sexual symptom was low sexual desire, which was identified by 23 of the 36 participants (64 %). Difficulty achieving erections and difficulty maintaining erections were each discussed by 18 participants (50 %). Other symptoms reported by participants included less sensation/pleasure (n = 7; 19 %), difficulty achieving orgasm (n = 4; 11 %), premature ejaculation (n = 5; 13.9 %), and no morning erection (n = 3; 8 %).
Summary of concept elicitation results. Symptoms reported by 5 or fewer participants included difficulty achieving orgasm (n = 4); premature ejaculation (n = 5); no morning erection (n = 3); difficulty going back to sleep (n = 4); easily tired, winded (n = 4); body shape changes (n = 4); loss of body hair (n = 2); mellow (n = 2); introverted/alone (n = 5); frustrated (n = 5); fear of rejection (n = 1); anxiety (n = 4); moody, emotional, sensitive (n = 3); focus (n = 3); concentration (n = 4); indecisive (n = 1); less drive/ambition (n = 3); and short attention span (n = 3)
The majority of the participants reported a range of symptoms that fitted within the general domain of tiredness (n = 23; 64 %), exhaustion (n = 7; 19 %), physical tiredness (n = 6; 17 %), or no energy/low energy (n = 17; 47 %). These symptoms had profound and interrelated impacts on participants’ lives. Feelings of tiredness led to naps, which interfered with ability to stay asleep at night, which affected sleep quality, which led to feelings of physical tiredness or weakness in the subsequent days.
01-103: “… mostly, I was just tired. I just didn’t have any energy. I just couldn’t—you know—what I used to do … I woke up in the morning, I felt like I was more tired than when I went to bed … you just find yourself exhausted. And then on top of it now, I don’t have that energy I used to have.”
The sleep disturbances the participants described were varied; the participants reported that they regularly woke up at night (n = 10; 28 %), had difficulty going back to sleep (n = 4; 11 %), or had poor quality sleep (n = 8; 22 %); nine of the men (25 %) reported increased napping.
The physical symptoms the participants described were related to weight gain (n = 9; 25 %), muscle loss (n = 6; 17 %), body shape changes (n = 4; 11 %), and hair loss (n = 2; 6 %). They also reported several mood symptoms, including depression/sadness/feeling low (n = 16; 44 %), frustration (n = 5; 14 %), anger (n = 7; 19 %), intolerance or impatience (n = 8; 22 %), and irritability or crankiness (n = 14; 39 %). Participants frequently associated mood symptoms with problems they experienced with sexual functioning. Many of the men reported having less confidence or lower self-esteem (n = 10; 28 %). A few men also reported symptoms such as feeling mellow, introversion, feeling alone, fear of rejection, anxiety, and being moody, emotional, or sensitive. Finally, within the cognitive domain, participants reported issues with motivation (n = 16; 44 %), loss of interest (n = 11; 31 %), problems with memory/forgetfulness (n = 11; 31 %), problems with focus/concentration (n = 6; 17 %), less drive/ambition (n = 3; 8 %), short attention span (n = 3; 8 %), and indecisiveness (n = 1; 3 %).
The results from concept elicitation interviews with men (n = 6) who were recruited on the basis of more stringent recruitment criteria—yielding a sample that was younger (aged 18–55 years), was not taking ED medications, and had lower serum testosterone levels (<250 ng/dL)—did not differ from those observed in the rest of the sample. In addition, when stratified according to age group (<55 years versus ≥55 years), by testosterone treatment status, and by ED treatment status, there were no notable differences in the nature or frequency of the symptom concepts across the groups. Interviews with the congenital participants (n = 3) yielded some additional physical signs and symptoms, including decreased testicle size, gynecomastia, height, and kneecap appearance. However, these concepts were not added to the HIS-Q, as they are identifiable by physical examination and may not be best assessed through self-report by patients.
Patients were asked to report on changes in symptomatology they had experienced during treatment. This information was used to determine which symptoms may be impacted by treatment, and also to clarify the language that participants used when discussing changes in their symptoms. The participants most frequently noted improvements in sexual symptoms, libido, and energy levels:
02-104: “… the erections were better, sex was better, ejaculations were better; I started noticing a good difference, high energy; I was keeping the weight down.”
01-108: “I have more desire than I did for a long time.”
01-109: “My energy level’s up; my libido’s up.”
03-104: “Well, you have a drive again. I have interest in my wife, so it does make a difference.”
To a lesser extent, the men who had been on treatment also reported improvements in their erectile functioning and memory, and increased muscle mass.
3.3 Instrument Development
The qualitative results were used to generate a draft HIS-Q instrument. Participants reported that their symptoms varied, in some cases daily, but most felt they would be best recalled over a 1- to 2-week period. The decision to use a recall period of 2 weeks for the sexual and physical symptoms was prompted by concerns regarding the frequency of sexual activity for many men with hypogonadism and reports that accurate recall would be difficult for a period longer than 2 weeks. A recall period of 1 week was used for the energy, sleep, cognitive, and mood symptoms. A Likert-type five-point ordinal scale was chosen, with response options on the final draft version that ranged from “not at all” to “extremely” and from “never” to “always” for severity and frequency items, respectively.
Once developed, the initial item pool was reviewed by the co-authors who are expert clinicians in the field of hypogonadism (SEA, LRD, ADS, and AD). In addition, a cultural and linguistic translation expert reviewed the draft of the instrument to improve the clarity and translatability. The initial draft HIS-Q included a total of 62 questions within the sexual (22), physical (3), energy (8), sleep (7), cognition (5), and mood (17) domains.
3.4 Cognitive Interview Results
The draft HIS-Q was further evaluated through one-on-one cognitive interviews with 29 patients. The results of these interviews suggested that most of the items were consistently understood by participants, the instrument was relevant and comprehensive in terms of the content coverage, and the recall periods and response options were appropriate. Nine of the original draft items were removed on the basis of the three rounds of cognitive debriefing because they were inconsistently interpreted, difficult to answer, redundant/overlapped with other items, and/or were not relevant. On the basis of the participant feedback, the current draft HIS-Q includes a total of 53 questions—sexual (17), physical (4), energy (4), sleep (6), cognition (5), and mood symptoms (17)—and includes recall periods of either 14 days (sexual and physical domains) or 7 days (energy, sleep, cognition, and mood domains). The preliminary conceptual framework for the instrument is shown in Fig. 3.
4 Discussion
The HIS-Q is a PRO instrument aimed at measuring the frequency and severity of symptoms of hypogonadism, and is designed to be used to evaluate changes in symptomatology in response to treatment. The instrument is being developed according to current FDA guidelines [14] and is intended to capture important changes in hypogonadal symptomatology. The current draft instrument includes 53 questions across the sexual, physical, energy, sleep, cognition, and mood domains.
The HIS-Q domains and symptoms are similar—but not identical—to those reported in the recently developed New England Research Institutes (NERI) Hypogonadism Screener (NERI-HG) [7]. It is interesting to note that the 53 draft items that currently constitute the HIS-Q cover a much broader range of symptoms than those represented by the NERI-HG, an 18-item screening instrument [10]. The current draft HIS-Q includes many of the same concepts as the NERI-HG but includes substantially more symptoms, many of which appear to represent disparate concepts, particularly within the sexual, mood, and cognitive domains. Future plans for the HIS-Q include item reduction and psychometric evaluation. Given the different intended uses of each PRO, with the NERI-HG primarily intended as a screener and the HIS-Q intended as a measure of severity and changes in symptomatology, it would not be surprising to find that the HIS-Q ultimately includes a larger number of items, which together constitute a more detailed evaluation of a broader range of symptoms.
Overall, the men participating in the focus groups most commonly reported symptoms of sexual dysfunction and tiredness. While these are commonly experienced by men with low testosterone, it is important to consider that recruitment through clinical sites may have increased the chances of identifying symptoms associated with treatment seeking. Future studies may include control subjects to determine the extent to which those symptoms that are included in the HIS-Q discriminate between men with and those without hypogonadism.
A unique aspect of the current study was that those participants who had been treated for their hypogonadism were specifically asked to report on the changes they had experienced as a consequence of treatment. Asking this question is likely to highlight symptoms that are most noticeable and relevant to participants, are highly bothersome, and potentially may be most sensitive to changes in serum total testosterone levels. The majority of the participants noticed changes in their energy level and an increased libido after starting testosterone replacement therapy. In future studies, HIS-Q items and scale scores will be correlated with serum total testosterone levels, both at a single point in time and with respect to changes over time.
5 Conclusion
The draft HIS-Q is a comprehensive PRO measure, which was designed to assess symptom frequency and severity among men with hypogonadism. The content validity of the draft HIS-Q, including the items, response options, and recall period, are suitable and have been confirmed through focus groups and cognitive interviews. A prospective psychometric evaluation study of the HIS-Q has recently been completed [26]. This subsequent study was conducted for the purposes of item reduction to generate the final HIS-Q instrument and to evaluate the reliability, validity, and responsiveness of the measure. The results from the current study, which provide evidence for the content validity of the draft HIS-Q, may be used in conjunction with information from the psychometric evaluation study to support the use of the final version of the HIS-Q to assess the symptoms associated with low testosterone in adult males.
References
Araujo AB, Esche GR, Kupelian V, O’Donnell AB, Travison TG, Williams RE, et al. Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab. 2007;92(11):4241–7.
Seftel A. Male hypogonadism. Part II: etiology, pathophysiology, and diagnosis. Int J Impot Res. 2006;18(3):223–8.
Fleishman SB, Khan H, Homel P, Suhail MF, Strebel-Amrhein R, Mohammad F, et al. Testosterone levels and quality of life in diverse male patients with cancers unrelated to androgens. J Clin Oncol. 2010;28(34):5054–60.
O’Connor DB, Corona G, Forti G, Tajar A, Lee DM, Finn JD, et al. Assessment of sexual health in aging men in Europe: development and validation of the European Male Ageing Study Sexual Function Questionnaire. J Sex Med. 2008;5(6):1374–85.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
Lee KK, Berman N, Alexander GM, Hull L, Swerdloff RS, Wang C. A simple self-report diary for assessing psychosexual function in hypogonadal men. J Androl. 2003;24(5):688–98.
Rosen RC, Araujo AB, Connor MK, Elstad EA, McGraw SA, Guay AT, et al. Assessing symptoms of hypogonadism by self-administered questionnaire: qualitative findings in patients and controls. Aging Male. 2009;12(2–3):77–85.
Morley JE, Charlton E, Patrick P, Kaiser FE, Cadeau P, McCready D, et al. Validation of a screening questionnaire for androgen deficiency in aging males. Metabolism. 2000;49(9):1239–42.
Smith KW, Feldman HA, McKinlay JB. Construction and field validation of a self-administered screener for testosterone deficiency (hypogonadism) in ageing men. Clin Endocrinol (Oxf). 2000;53(6):703–11.
Rosen RC, Araujo AB, Connor MK, Gerstenberger EP, Morgentaler A, Seftel AD, et al. The NERI Hypogonadism Screener: psychometric validation in male patients and controls. Clin Endocrinol (Oxf). 2011;74(2):248–56.
Wiltink J, Beutel ME, Brahler E, Weidner W. Hypogonadism related symptoms: development and evaluation of an empirically derived self-rating instrument (HRS ‘Hypogonadism Related Symptom Scale’). Andrologia. 2009;41(5):297–304.
Heinemann LA, Saad F, Zimmermann T, Novak A, Myon E, Badia X, et al. The Aging Males’ Symptoms (AMS) Scale: update and compilation of international versions. Health Qual Life Outcomes. 2003;1:15.
Heinemann LA, Moore C, Dinger JC, Stoehr D. Sensitivity as outcome measure of androgen replacement: the AMS Scale. Health Qual Life Outcomes. 2006;4:23.
US Food and Drug Administration. Guidance for industry on patient-reported outcome measures: use in medical product development to support labeling claims. Federal Regist. 2009;74(235):65132–3.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity-establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–77.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity-establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2—assessing respondent understanding. Value Health. 2011;14(8):978–88.
Leidy NK, Vernon M. Perspectives on patient-reported outcomes: content validity and qualitative research in a changing clinical trial environment. Pharmacoeconomics. 2008;26(5):363–70.
Heinemann LA, Zimmermann T, Vermeulen A, Thiel C, Hummel W. A new, aging males’ symptoms’ rating scale. Aging Male. 1999;2:105–14.
Berlin Center for Epidemiology and Health Research. Norm values. [Cited 2011 May 26]. Available from: http://www.aging-males-symptoms-scale.info/documents/norm.pdf.
Giltay EJ, Tishova YA, Mskhalaya GJ, Gooren LJ, Saad F, Kalinchenko SY. Effects of testosterone supplementation on depressive symptoms and sexual dysfunction in hypogonadal men with the metabolic syndrome. J Sex Med. 2010;7(7):2572–82.
Moore C, Huebler D, Zimmermann T, Heinemann LA, Saad F, Thai DM. The Aging Males’ Symptoms Scale (AMS) as outcome measure for treatment of androgen deficiency. Eur Urol. 2004;46(1):80–7.
Behre HM, Tammela TL, Arver S, Tolra JR, Bonifacio V, Lamche M, et al. A randomized, double-blind, placebo-controlled trial of testosterone gel on body composition and health-related quality-of-life in men with hypogonadal to low-normal levels of serum testosterone and symptoms of androgen deficiency over 6 months with 12 months open-label follow-up. Aging Male. 2012;15(4):198–207.
Srinivas-Shankar U, Roberts SA, Connolly MJ, O’Connell MD, Adams JE, Oldham JA, et al. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2010;95(2):639–50.
Muhr T. User’s manual for ATLAS.ti 5.0. 2nd edition. Berlin: Scientific Software Development GmbH; 2004. [Cited 2015 Aug 20]. Available from: http://www.ugr.es/~textinfor/documentos/atlman.pdf.
Dobs AS, McGettigan J, Norwood P, Howell J, Waldie E, Chen Y. A novel testosterone 2 % gel for the treatment of hypogonadal males. J Androl. 2012;33(4):601–7.
Gelhorn HL, Dashiell-Aje E, Miller MG, Brod M, DeRogatis LR, Dobs A, et al. Evaluation of the psychometric properties of the Hypogonadism Impact of Symptoms Questionnaire (HIS-Q). 2015 (In preparation).
Acknowledgments
AbbVie participated in the review and approval of the manuscript. The authors would like to thank Fritz Hamme for assistance in the preparation of this manuscript for publication.
Authorship
All persons designated as authors qualify for authorship. Specific contributions are as follows: Heather L. Gelhorn and Margaret K. Vernon participated in all aspects of the work, including the conception and design of the study, analysis and interpretation of data, drafting the manuscript, and revision and final approval of the version of the manuscript to be published. Katie D. Stewart, Dennis A. Revicki, Meryl Brod, and Michael G. Miller participated in the conception and design of the study, analysis and interpretation of data, and revision and final approval of the version of the manuscript to be published. Stanley E. Althof, Leonard R. DeRogatis, Adrian Dobs, and Allen D. Seftel participated in the conception and design of the study, interpretation of data, revision of the manuscript for critically important content, and final approval of the version of the manuscript to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this manuscript was provided by AbbVie.
Conflict of interest
Heather L. Gelhorn, Dennis A. Revicki, Margaret K. Vernon, and Katie D. Stewart are employees of Evidera; Evidera received research study support from AbbVie. Meryl Brod was a paid consultant to AbbVie on this project. Michael G. Miller is an employee of AbbVie and a stockholder of AbbVie. Stanley E. Althof serves as an unpaid consultant to Eli Lilly. Adrian Dobs, Allen D. Seftel, and Leonard R. DeRogatis have no conflicts of interest to declare.
Ethical approval
This study was approved by an institutional review board (Ethical Review Committee study no. 491-09-09, approved on September 16, 2009; Ethical Review Committee study no. 512-01-10, approved on January 29, 2010; Ethical & Independent Review Services study no. 11216-01, approved on September 12, 2011), and all participants provided informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gelhorn, H.L., Vernon, M.K., Stewart, K.D. et al. Content Validity of the Hypogonadism Impact of Symptoms Questionnaire (HIS-Q): A Patient-Reported Outcome Measure to Evaluate Symptoms of Hypogonadism. Patient 9, 181–190 (2016). https://doi.org/10.1007/s40271-015-0138-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-015-0138-8