Abstract
The term Lewy body dementia refers to either of two related diagnoses: dementia with Lewy bodies (DLB) and Parkinson's disease dementia (PDD). Clinical management of Lewy body dementia is challenging. The current treatment options focus on relieving symptoms; no disease-modifying therapies are available. There are currently no US Food and Drug Administration (FDA) approved drugs for the treatment of DLB, and there are only a few for PDD. Cholinesterase inhibitors are shown to be beneficial in improving cognitive symptoms in Lewy body dementia. Rivastigmine was approved by the FDA to treat PDD. Donepezil was approved in Japan as a treatment for DLB. Levodopa may provide modest benefit in treating motor symptoms and zonisamide in adjunct to low-dose levodopa helps with parkinsonism. Treatment of autonomic symptoms are based on symptomatic treatment with off-label agents. Our main objective in this article is to present an overview of the current pharmacological options available to treat the clinical features of DLB and PDD. When evaluating the existing management options for Lewy body dementia, it is difficult to fully separate PDD from DLB. However, we have attempted to identify whether the cited studies include patients with PDD and/or DLB. Moreover, we have provided an overview of the current drug pipeline in Lewy body dementia. All currently active trials are in phase I or II and most are focused on disease modification rather than symptomatic treatment. Phase II trial results for neflamapimod show promising results. Due to heterogeneity of symptoms and underlying pathophysiology, there is a need for new biomarker strategies and improved definitions of outcome measures for Lewy body dementia drug trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most of the commonly prescribed drugs for Lewy body dementia are derived from clinical trials in Alzheimer’s or Parkinson’s diseases. |
A major focus of the management of neurobehavioral symptoms of Lewy body dementia is the discontinuation of medications with the greatest anticholinergic effect without worsening motor symptoms. |
Various therapies are being developed to address the heterogeneity of the Lewy body dementia pathology, but there are inconsistent outcome measures between these studies. |
1 Introduction
Lewy body dementia (LBD) is an umbrella term describing a range of clinical symptoms that are characterized pathologically by Lewy-related pathology (LRP), including both Lewy bodies and Lewy neurites. The clinical diagnoses associated with LRP include Parkinson’s disease dementia (PDD) and dementia with Lewy bodies (DLB), as well as multiple system atrophy (MSA).
In terms of clinical phenotypes, PDD and DLB may represent different points along a Lewy body disease continuum but have similar pathological aspects. While PDD and DLB each have separate diagnostic criteria, there is considerable overlap between the two in symptomatology and treatment. The two diseases are clinically distinguished by the arbitrary 1-year rule based on the temporal onset of motor symptoms relative to cognitive symptoms. In PDD, the motor symptoms appear at least a year before the onset of dementia.
The diagnosis and clinical management of LBD can be challenging for physicians. As will be discussed later, patients with LBD present with varying degrees and combinations of dementia pathology, motor changes, and neuropsychiatric disturbances. DIAMOND-Lewy is a collaborative research program between Cambridge and Newcastle University that has developed a checklist to assist physicians in diagnosing and managing DLB and PDD patients based on 2017 consensus criteria [1, 2]. The checklist improved diagnostic rates of DLB, but not PDD, at two geographical regions in England [3]. A primary analysis found some benefits for patients and caregivers based on global outcome measures and caregiver burden, when the toolkit was used in comparison with standard therapy [4].
Management options are currently directed towards alleviation of symptoms; a disease-modifying therapy does not currently exist. However, appropriate use of available treatments can significantly reduce symptom burden and improve quality of life.
The primary focus of this article is to review the current pharmacological options available to treat the clinical features of DLB and PDD. Lewy body dementia describes a spectrum of conditions; it is difficult to fully separate PDD and DLB when reviewing the existing management options. However, we have attempted to identify if the cited studies involve patients with PDD and/or DLB. We also provide an overview of the current investigational drug pipeline in LBD.
2 Dementia with Lewy Bodies
DLB is a relatively common cause of dementia. In a 2014 meta-analysis by Vann Jones and O’Brien, DLB accounted for 4.2% of all community-based diagnoses of dementia, and increased to 7.5% of diagnoses in a secondary care setting [5]. It is commonly accepted that DLB is the third most common cause of dementia behind only Alzheimer’s disease (AD) and vascular dementia.
Pathologically, DLB is characterized by the presence of Lewy bodies, which are scattered throughout the limbic system, neocortex, brainstem, and peripheral autonomic nervous system [1]. Lewy bodies are round, eosinophilic intraneuronal cytoplasmic inclusions consisting primarily of α-synuclein (SCNA). In addition, Lewy neurites are also present, typically in the transentorhinal cortex, amygdala, the CA2 and CA3 regions of the hippocampus, the nucleus basalis of Meynert, and additional brainstem nuclei [6]. In addition to LRP, up to 80% of patients with DLB will have concomitant Alzheimer’s disease pathological changes and many meet the pathological criteria for AD [7].
From a biochemical perspective, DLB is associated with marked dopaminergic and cholinergic deficiencies. Particularly, there is a loss of cholinergic neurons in the nucleus basalis of Meynert and reductions in markers of cholinergic activity in the parietal and temporal cortices [8]. Additionally, the reduction in post-synaptic D2 receptor density in the striatum is more pronounced in DLB than in healthy controls [9].
It should be mentioned that there is considerable convergence of the neuropathologic features of DLB and PDD. The distinguishing features that may separate DLB and PDD from a neuropathological perspective are variable and somewhat unreliable, making it difficult to separate them into two separate pathologic entities. Because of this, a single Lewy body disorder research model has been proposed and accepted, with abnormal SCNA aggregation being the defining process common to both [10].
In 2017, revised clinical diagnostic criteria for DLB were published by the DLB consortium. Required for the diagnosis is the establishment of cognitive changes significant enough that they impact an individual’s level of function, or, in other words, the presence of dementia. Additional core criteria include fluctuations in cognition, recurrent visual hallucinations, rapid eye movement sleep behavior disorder (RBD), and spontaneous motor features of Parkinsonism (one or more cardinal features of bradykinesia, rest tremor, and/or rigidity). There are several features that are supportive of a diagnosis of DLB, including (i) severe antipsychotic sensitivity, (ii) postural instability, (iii) repeated falls, (iv) hypersomnia, (v) hyposmia, (vi) syncope or transient episodes of unresponsiveness, (vii) non-visual hallucinations, (viii) systematized delusions, and (ix) apathy, anxiety, and depression [1].
In addition to these clinical features, the updated diagnostic criteria outline various indicative and supportive biomarkers [1]. There are currently no blood or cerebrospinal fluid biomarkers that can reliably diagnose DLB. Multiple previous studies have reported low β-amyloid 40–42 in DLB compared with those in PDD and controls, but they have not been validated to be able to reliably differentiate DLB from other neurodegenerative conditions [11, 12]. Along with there being no blood or spinal fluid biomarkers, direct imaging of α-synuclein pathological changes is also not available.
Using ligands specific for dopamine transporters, both positron emission tomography (PET) and single photon emission computed tomography (SPECT) demonstrate decreased dopaminergic activity in the basal ganglia in patients with parkinsonian disorders. This finding cannot be used to distinguish between other parkinsonian conditions. Therefore, its utility is most relevant when attempting to differentiate between DLB and other neurodegenerative conditions that typically lack parkinsonism such as AD. A 2007 study involving 326 patients with dementia reported a sensitivity of 78% and specificity of 90% in using DAT SPECT imaging to diagnose DLB [13]. This imaging finding of reduced dopaminergic activity in the striatum is considered to be an indicative biomarker of DLB [1].
A second indicative biomarker, which is discussed in more depth later in the treatment section of our discussion, is the presence of REM sleep without atonia or RBD on polysomnography [1]. Polysomnography-confirmed RBD has a specificity of 98% for Lewy body disease [14].
Lewy body disease is associated with cardiac autonomic denervation which can be quantified using metaiodobenzylguanidine (MIBG) myocardial scintigraphy [1]. A third indicative biomarker for DLB is the finding of reduced sympathetic innervation on MIBG myocardial scintigraphy, with previous studies demonstrating a sensitivity of 69% and specificity of 89% [15].
In addition to indicative biomarkers, supportive biomarkers have also been identified. In structural magnetic resonance imaging (MRI), the medial temporal structures and hippocampi are typically well preserved without significant atrophy. Additionally, a quantitative electroencephalogram (EEG) showing prominent posterior slow-wave activity with periodic fluctuations in the pre-alpha and theta range is currently categorized as an indicative biomarker. Finally, fludeoxyglucose PET imaging demonstrating either occipital hypometabolism and/or the presence of the cingulate island sign are also supportive findings [1].
Based on the 2017 revised clinical criteria for DLB, the presence of two or more core clinical features or one core clinical feature and at least one indicative biomarker is sufficient for a diagnosis of probable dementia with Lewy bodies. Possible dementia with Lewy bodies is diagnosed in the context of one core clinical feature with no indicative biomarker or the presence of one or more indicative biomarkers but no core clinical features [1].
3 Parkinson’s Disease Dementia
PDD is defined as the presence of dementia which occurs in the setting of an established diagnosis of Parkinson’s disease (PD). From a historical perspective, the chief feature that previously separated PD and DLB was the timing of onset of cognitive symptoms relative to the appearance of motor changes. The ‘1-year rule’ refers to the well accepted idea that the presence of dementia within the first year of onset of parkinsonism was exclusionary for PD and more suggestive of underlying DLB. DLB Consortium has remained supportive of the 1-year rule distinguishing DLB from PDD in 2017 consensus criteria, as it continues to be useful in clinical practice [1]. The International Parkinson and Movements Disorder Society deleted the 1-year rule with the release of new clinical diagnostic criteria for PD in 2015 [16]. With their new criteria, individuals may be diagnosed with PD regardless of their cognitive impairment. Those with significant cognitive impairment are assigned the label of PD, dementia with Lewy bodies subtype [16].
Dementia is a common feature of PD, with the prevalence estimated to be around 25–30% of patients with PD [17]. Older age and the duration of disease are both risk factors for PDD. In a study published in 2005 by Hely et al., at 15 years of disease duration, 48% of their cohort of PD patients met criteria for a diagnosis of dementia, and 36% fulfilled criteria for PD mild cognitive impairment [18].
Consensus criteria for the diagnosis of PDD were developed in 2007. The core features of these criteria include the requirement of a diagnosis of PD according to the Queen Square Brain Bank criteria, along with the presence of dementia with impairment in more than one cognitive domain (attention, memory, executive function, visuospatial function) [19].
4 Treatment of Cognitive Impairment and Cognitive Fluctuations
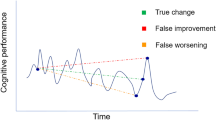
One of the primary features of both DLB and PDD is a progressive decline of cognitive function resulting in a loss of the ability to function independently. The cognitive deficits seen in DLB and PDD are similar, both with notable deficiencies in executive function, attention, and visuospatial function with relatively milder deficits in memory retrieval. Additionally, patients with DLB often have pronounced fluctuations in alertness and attention. Caregivers will describe drastic changes ranging from seemingly normal cognitive performance followed by periods of severe confusion and impairment that may raise concern for seizures or strokes. Bradshaw et al. demonstrated that the cognitive fluctuations in DLB differ qualitatively from the normal variations seen in other types of neurodegenerative disease [20]. Additionally, a study done in 2000 involving attention and vigilance tasks showed that the fluctuating cognition in DLB occurs on a second-to-second basis [21].
When it comes to the management of the cognitive symptoms of DLB, cholinesterase inhibitors are the mainstay of treatment. Similarly to those with Alzheimer’s disease, profound degeneration of cholinergic neurons of the basal forebrain is seen in both DLB and PDD [22]. Cholinesterase inhibitors exert their effect by blocking the enzymatic breakdown and increasing the availability of the central nervous system acetylcholine. It should be noted that no head-to-head comparison trials of the different cholinesterase inhibitors have ever been performed. In regards to the specific cholinesterase inhibitors, donepezil and rivastigmine appear to be equally efficacious. Rivastigmine is the only cholinesterase inhibitor that is US Food and Drug Administration (FDA) approved for use in PDD.
In a placebo-controlled, double-blinded multicenter study involving 120 patients with LBD, participants were randomized to either 6–12 mg/day of rivastigmine or placebo for 20 weeks. Patients who received the rivastigmine demonstrated a significant improvement on a computerized cognitive assessment, particularly on tasks related to attention. Patients on rivastigmine also demonstrated reduced apathy and anxiety, along with experiencing a reduction in delusions and hallucinations [23].
In another randomized study involving 140 DLB patients, 12 weeks of treatment with either 5 or 10 mg of donepezil were significantly superior to placebo on Mini Mental Status Examination (MMSE) scores (5 mg: mean difference 3.8; 95% confidence interval [CI] 2.3–5.3; p < 0.001; 10 mg: mean difference 2.4; 95% CI 0.9–3.9; p = 0.001) and CIBIC-plus. Improvements were also noted in behavioral measures and caregiver burden [24]. A second, double-blind, randomized controlled trial in 2015 showed a statistically significant improvement in MMSE scores only with the 10-mg dose compared with placebo. The change in the 5-mg group was not significant [25].
Evidence for galantamine is limited only to open-label studies. In one such study by Edwards et al. in 2007 involving oral galantamine, there were statistically significant changes noted in the Neuropsychiatric Inventory (NPI-12) which improved by 8.24 points from baseline. Additionally, scores on the Clinician’s Global Impression of Change improved by 0.5 points from baseline [26].
The most common side effects of cholinesterase inhibitors are primarily gastrointestinal in nature. Additionally, because they enhance vagal tone, they may lead to cardiac issues such as bradycardia, syncope, or heart block. For those unable to tolerate oral formulations, it is reasonable to switch to the patch formulation of rivastigmine to see if it is better tolerated.
The benefits of memantine are much less clear compared with the benefits of cholinesterase inhibitors. Memantine is an N-methyl d-aspartate (NMDA) receptor antagonist that limits the neurotoxicity of glutamate. Previous animal model studies of parkinsonism have suggested evidence for glutamatergic overactivity, which explains the theoretical rationale for use of memantine in DLB [27]. However, the actual data for the efficacy of memantine in treating the cognitive symptoms of DLB is mixed and further studies are required.
A 24-week, randomized, placebo-controlled study of memantine 20 mg per day involving 72 patients with PDD or DLB showed that the memantine group performed better on the AD Cooperative Study—Clinical Global Impression of Change scale (ADCS-CGIC) compared with those receiving placebo (mean difference 0.7, 95% CI 0.04–1.39; p = 0.03). No significant differences were noted in secondary outcome measures [28]. Another larger study involving 199 patients with either DLB or PDD who were treated with memantine 20 mg per day again demonstrated a significant improvement in ADCS-CGIC scores in patients with DLB but not those with PDD [29]. The studies were somewhat limited by small sample sizes.
A phase II randomized controlled trial of neflamapimod, a p38αkinase inhibitor, in patients with DLB showed a statistically significant improvement on a custom battery of six cognitive tests over 16 weeks compared with placebo (AscenD-LB; ClinicalTrials.gov identifier: NCT04001517). The sponsor reported, in a press release, an improvement in gait as captured by timed up-and-go test [30]. The researchers attributed the result of the study as an indication of positive effect on basal forebrain cholinergic dysfunction [31].
5 Treatment of Motor Symptoms/Parkinsonism
The cardinal parkinsonian symptoms, including bradykinesia, resting tremor, rigidity, and postural instability, are observed in approximately 70% of patients with DLB [32]. The frequency and distribution of motor symptoms differ from those seen in idiopathic PD. Patients with DLB often experience fairly symmetric rigidity and bradykinesia, though a tremor is less common and less severe than in idiopathic PD [33, 34]. The reason for this difference has not been fully elucidated, though it has been postulated to be secondary to differences in the degree and distribution of Lewy body-related pathology [10].
While not necessarily supported by extensive or rigorous clinical trials, levodopa’s benefit on motor symptoms in patients with DLB is generally considered modest and less robust than the response in patients with idiopathic PD. In one study of levodopa treatment for extrapyramidal symptoms in DLB, a significant motor response was noted in only about one third of patients. Four out of 14 patients withdrew due to side effects, with two dropping out because of gastrointestinal symptoms and the other two due to worsening confusion [35]. In another study published in 2008, motor benefit defined as > 10% improvement over baseline UPDRS III scores was achieved in only one-third of study subjects with DLB without exacerbation of psychotic symptoms [36]. A suggested approach would be to start with a low dose of one-half tablet of carbidopa-levodopa 25–100 mg three times daily, with slow increases according to the motor response and tolerance of side effects. Alternatively, while dopamine agonists such as a pramipexole and ropinirole are good options for younger patients with mild parkinsonism secondary to PD, they are generally avoided in patients with DLB because of their propensity to cause somnolence and worsen hallucinations.
Various therapies are available to treat Parkinsonism in people with Parkinson's disease. DLB patients are less likely to be treated with these drugs than those with Parkinson’s disease.
Zonisamide, an anticonvulsant medication that inhibits sodium and T-type calcium channels, has been approved in Japan for the treatment of PD [37]. The dosage typically studied in PD is 25–50 mg/day, much lower than the doses used to treat seizures. The exact mechanism through which it exerts its effect is unclear, though several theories have been proposed. In 2016, Murata et al. explored the efficacy and safety of zonisamide 25–50 mg/day taken once daily as compared with placebo. Both zonisamide 25 mg/day and 50 mg/day demonstrated a statistically significant reduction in UPDRS III scores [38]. More recently, Murata et al. published their results of a phase III randomized trial assessing the benefit of zonisamide for parkinsonism in patients with DLB [39]. Patients with parkinsonism who were diagnosed with probable DLB were randomized to receive oral zonisamide (25 or 50 mg/day) or placebo for a 12-week period, followed by a 40-week open-label extension. At week 12, the group difference (least squares mean ± SEM) for changes from baseline versus placebo in UPDRS III total score was − 2.7 ± 0.9 (95% CI − 4.4 to − 0.9; p = 0.005) in the zonisamide 25 mg/day group and − 2.6 ± 0.9 (95% CI − 4.4 to − 0.8; p = 0.005) in the zonisamide 50 mg/day group [39]. Following these trials, Japanese regulators approved zonisamide for the indication of parkinsonism in DLB in 2018 [40].
Zonisamide had a moderate effect on parkinsonism, but was still achieved with a relatively low dose of levodopa (254 mg/day), which is an alternative to increasing levodopa dosage. In DLB patients, the adverse effect of mental slowing, which can occur with epilepsy patients, may also occur if they are at a more advanced stage or taking higher doses [41]. The side effect of loss of appetite is relatively common, and it may put a burden on patients and their families [39].
Zonisamide 25–50 mg once a day may be a safe and effective adjunct to levodopa for the management of parkinsonism in PD and DLB. DLB patients who cannot tolerate an increase in the dose of levodopa because of gastrointestinal side effects or the development of hallucinations might benefit from zonisamide [42].
It has a mild therapeutic benefit, but its effects on cognition may limit its maximum dosage.
In addition to the pharmacological measures discussed above, it is also important to consider the importance of non-pharmacological interventions to help with motor symptoms. There are multiple studies demonstrating that regular aerobic exercise has a positive impact in patients with PD [43, 44]. A meta-analysis published in 2017 by Song et al. found that tai chi was associated with improvements in motor outcomes, including in the Timed Up and Go testing, the Unified Parkinson’s Disease Rating Scale III score, balance, fall frequency, and 6-min walk [45].
6 Treatment of Neuropsychiatric Symptoms
Neuropsychiatric symptoms such as delusions, hallucinations, apathy, and anxiety are common in DLB and PDD. While relatively rare for other types of neurodegenerative disease such as Alzheimer’s disease, recurrent visual hallucinations are one of the core clinical features for DLB. When compared with Alzheimer’s disease, hallucinations, depression, and delusions occurred earlier and were more frequent in patients with DLB [46]. It is more common to see neuropsychiatric symptoms early on in LBD than in AD. The symptoms of hallucinations, delusions, sleep disorders, and irritability tend to remain more frequent over time in LBD, contributing significantly to personal strain [47]. Generally, neuropsychiatric symptoms play a similar role in other dementias, such as AD. However, in cases of LBD where the prevalence of these symptoms may be high, they may be especially important, requiring changes in treatment based on caregiver’s report. DLB caregivers’ subjective burden scores were higher than those typically reported by caregivers of AD or mixed diagnoses. Falling is a significant problem for patients with LBD, but it was not a significant predictor of any burden dimension [47].
Visual hallucinations are comparatively less common in PDD, and often are more prevalent later in the disease course [48].The visual hallucinations in DLB are typically detailed and well formed. Most are benign and not distressing to the patient. Descriptions are often centered on well-formed images of animals or people, or alternatively as the visualization of non-specific shapes or flashes of color. Visual illusions, misperceptions, illusions of presence, or the observation of the movement of shadows in the peripheral vision are also common. Auditory hallucinations are less specific and less frequent for DLB and PDD, and often go underreported.
Delusions are also common in DLB. These delusions are typically complex and bizarre, often involving entrenched thoughts related to visual hallucinations that a patient has experienced [49]. The delusions in DLB are contrasted with those experienced in AD, which are more frequently related to misidentification or their own memory impairment. Of note, a study done in 2010 showed that the frequency of somatoform disorder was higher in DLB and PD than in other types of neurodegenerative diseases. These somatoform disorders consisted of non-physiological sensory or motor symptoms frequently accompanied by delusional thought content [50].
Depression and anxiety are common in both DLB and PDD. In a 2007 study by Borroni et al., 61.9% of their cohort of DLB patients had depression, 67.4% experienced significant anxiety, and 57.6% had apathy [51]. An additional study in 2017 demonstrated that co-morbid depression was more common in patients with DLB versus those with Alzheimer’s disease [52].
It bears mention that antipsychotic sensitivity is considered to be clinical feature supportive of DLB, and also occurs in patients with PDD. Previous studies have shown that approximately 50% of patients with DLB will have severe sensitivity to antipsychotic medications [53]. The mechanism of this phenomenon is thought to be mediated by dopamine-2 receptor blockade. Adverse reactions occur more commonly with older, first-generation antipsychotics, though reactions to newer agents are also frequently encountered.
In patients with LBD, treatment of hallucinations and psychotic symptoms is challenging since dopaminergic medications are the main option for treating motor impairments. To achieve optimal outcomes, it is helpful to follow a stepwise approach. The initial step should focus on identifying systemic disorders that may aggravate neuropsychiatric symptoms based on the history and physical examination, such as urinary tract infection, followed by discontinuing anticholinergics. In the next step, relatively low-potency antiparkinsonian medications can be stopped first, including monoamine oxidase B inhibitors or amantadine, which may worsen neurobehavioral symptoms. Next, dopamine agonists should be reduced or discontinued. In one randomized controlled trial of patients with LBD, rivastigmine 6–12 mg daily significantly and clinically improved apathy and anxiety, with fewer delusions and hallucinations compared with the control group [23]. Because of the significant safety concerns and the aforementioned antipsychotic sensitivity, antipsychotics are typically a last resort for more severe behavioral symptoms after other measures have been attempted. Additionally, dopaminergic blockade may result in worsening of pre-existing motor symptoms, so it should be used with caution in patients with more pronounced parkinsonism.
In clinical trials of antipsychotics for patients with DLB or PDD, there has been no strong evidence of efficacy. Typical antipsychotics such as haloperidol should be avoided. In a small case series published in 2003, Takahashi et al. demonstrated that five out of nine DLB patients who received quetiapine 25–75 mg/day had a decline of > 50% in the sum of scores measuring agitation, hallucinations, and delusions on the Neuropsychiatric Inventory scale [54]. However, in a multicenter, randomized, double-blind, placebo-controlled study in 2007 involving 23 patients with DLB and nine with PDD, quetiapine did not show a benefit for treating agitation or psychosis when compared with placebo [55].
In another study done in 2002, patients receiving olanzapine 5 mg showed significant reductions in delusions and hallucinations without worsening of motor symptoms [56]. There is supportive evidence for the use of clozapine for patients with psychotic symptoms in the setting of PD. In a 4-week, randomized, double-blind, placebo-controlled study, patients receiving clozapine demonstrated improved psychotic symptom assessment scores, with no change in motor and cognitive function compared with those receiving placebo [57]. The use of clozapine is limited by its potential to cause serious hematological side effects such as granulocytopenia, and the need for close laboratory monitoring. There are relatively few randomized clinical trials of high quality regarding LBD treatment, as most pharmacological studies focus on uncontrolled clinical trials. Consequently, there are no direct comparisons of pharmacotherapies for LBD randomized clinical trials. Network meta-analysis (NMA) is a technique for comparing multiple treatments simultaneously in a single analysis by incorporating direct and indirect evidence within a network of randomized controlled trials. NMA can generate estimates with precision and accuracy [58, 59]. A recent NMA of nine randomized controlled trials found that none of the treatments (olanzapine, quetiapine, memantine, rivastigmine, donepezil, or zonisamide) had statistical significance for managing neuropsychiatric symptoms (k = 6, n = 653). According to a second network meta-analysis of randomized clinical trials and single-arm studies, aripiprazole, olanzapine, and yokukansan (an eastern Asian herbal supplement) were associated with improvements in symptoms based on NPI-10 scores (k = 27, n = 1073) [59].
Pimavanserin, a selective serotonin 5-HT2A receptor inverse agonist, has been approved by the US FDA for use in patients with PD psychosis. Due to its lack of effects on both dopaminergic and histaminergic receptors, there are less of the problematic side effects seen with other antipsychotics. In a 6-week, randomized, double-blind, placebo-controlled study of pimavanserin published in 2013, a subgroup of patients with cognitive impairment had an improvement in a psychosis score that was better than the change observed in patients who had normal cognition [60].
The HARMONY trial was a relapse-prevention study evaluating the efficacy and safety of pimavanserin for treating hallucinations and delusions associated with dementia-related psychosis. The study showed efficacy when a prespecified interim analysis revealed > 2.8-fold reduction in risk of relapse with pimavanserin (hazard ratio 0.353; 95% CI 0.172–0.727; 1-sided p = 0.0023). Patients with dementia-related psychosis who had a response to pimavanserin had a lower risk of relapse with continuation of the drug (13%) than with discontinuation (28%) [61]. The FDA has rejected the manufacturer’s request that pimavanserin be the first approved treatment of hallucinations and delusions associated with dementia-related psychosis due to the absence of statistically significant changes in some of the dementia subgroups, and low numbers of patients with less common dementia subtypes [62]. The efficacy of pimavanserin in DLB has not been fully established.
The results of a meta-analysis of four randomized clinical trials, including 680 patients with PDD, showed that pimavanserin significantly reduced delusions and hallucinations [63]. A retrospective cohort study compared patients with PD or DLB who started on quetiapine or pimavanserin for psychosis and assessed time to discontinuation of the medication using a Kaplan-Meier study [64]. Analyzing time to discontinuation accounted for efficacy, safety, and tolerability. The pimavanserin group had a lower discontinuation rate at early stage compared with the quetiapine group but a higher discontinuation rate at late stage. Lower early discontinuation rates in the pimavanserin cohort may indicate better results when it comes to promptly treating psychosis. In fact, more patients remain on quetiapine long term because of its delayed effects, possibly as a result of improvement in secondary indications such as agitation or insomnia [64].
Pimavanserin does not have negative impacts on cognitive function in patients with neurodegenerative diseases compared with those on placebo and is thought to be well tolerated without worsening parkinsonian symptoms. Pimavanserin may be clinically useful for promptly managing psychosis in LBD patients, but it is not recommended for patients with preexisting QT prolongation.
No specific treatment or guideline has been defined for treating depression and anxiety in patients with DLB and PDD. To address the gaps in the treatment of LBD, an expert opinion consensus has been developed [65]. However, further trials are needed. The International Parkinson and Movement Disorder Society Evidence-Based Medicine Committee recommended venlafaxine as clinically useful treatment for depressive symptoms in PD [66]. Despite conflicting studies on paroxetine, citalopram, and sertraline for treatment of depression in PD, the committee considered these SSRIs as possibly useful due to established efficacy outside of PD [66]. However, these drugs should be used with caution in those with rapid eye movement (REM) sleep behavior disorder due to the risk of exacerbation. In a 2010 study, 71% of patients with DLB treated with citalopram discontinued therapy because of intolerable side effects [67]. Tricyclic antidepressants are widely known to be anticholinergic and, therefore, should be avoided.
7 Treatment of Rapid Eye Movement Sleep Behavior Disorder
RBD is a common symptom in all synucleinopathies and is one of the core clinical criteria of DLB [1]. In normal REM sleep, the skeletal musculature is atonic, leading to absence of motor activity. This absence of motor function is thought to be mediated by a network of inhibitory projections originating in the brainstem which then terminate in the motor neurons of the spinal cord [68].
In RBD, the normal atonia during REM sleep is lost, resulting in recurrent episodes of complex motor behavior and/or vocalizations during sleep, often accompanied by vivid dreams of being attacked or chased [69]. These episodes most typically occur in the second half of sleep when REM sleep is most prevalent. This differs in relation to other parasomnias such as sleep walking, confusional arousals, and sleep terrors which typically occur in earlier sleep periods. The movements of RBD are described as purposeful, ranging in severity from violent punching of the limbs to more subtle, benign gesturing of the hands. Patients with RBD are at a high risk of injury due to falling or jumping out of the bed.
RBD has been shown to be associated with an increased risk of development of an α-synucleinopathy. The estimated 10-year risk for developing a neurodegenerative disease in patients with idiopathic RBD is 40.6% [70]. In another series, 81% of patients diagnosed with idiopathic RBD eventually developed a parkinsonian or dementia syndrome, with the mean interval being 14 years from the onset of RBD [71].
The evaluation of RBD often involves corroboration from a partner or informant but definitive diagnosis of RBD requires a video polysomnography which will demonstrate REM sleep without atonia (RSWA) measured using surface electromyography [72].
In regards to the treatment of RBD, the first and most essential priority should be ensuring a safe sleep environment. Dangerous items such as knives and firearms should be made inaccessible. The immediate sleeping environment should be modified with removal of all items that may be easily broken. In extreme cases, more restrictive measures such as bed alarms and padded railings may be utilized.
Pharmacologically, melatonin is often considered to be the first-line therapy. Melatonin is an endogenous hormone secreted by the pineal gland which helps regulate circadian rhythms. Melatonin production is reduced in PD with a reported association between slow-wave sleep and melatonin area under curve in PD patients [73]. The exact mechanism through which melatonin improves RBD symptoms is unknown. However, multiple studies have demonstrated that melatonin decreases the severity and frequency of RBD. In a 2013 study by McCarter et al., 12% of patients using melatonin 6 mg had complete resolution of their RBD. Approximately 48% reported moderate or greater subjective improvement in their episodes. Additionally, melatonin treatment was also associated with decreased reported severity of injuries [74]. McGrane et al. reviewed multiple prospective and retrospective studies involving the use of melatonin in the range of 3–9 mg [75]. The authors found that each of the studies demonstrated that melatonin again reduced both the severity and frequency of RBD. As mentioned, melatonin is often an ideal first-line treatment due to its favorable safety and tolerability profile when compared with other medications used to treat RBD. It tends to be well tolerated, with most side effects (GI upset, headaches, fatigue, and dizziness) usually being fairly mild [75]. The dose of melatonin required to suppress RBD often varies, with a typical starting dose of 3 mg prior to bedtime that may be increased periodically in similar increments until the symptoms have improved or ceased.
Clonazepam is a long-acting benzodiazepine that has been shown to be efficacious in treating RBD. Much like melatonin, the exact mechanism through which clonazepam affects RBD is unknown. Clonazepam is often effective in doses as small as 0.25 mg/night, though doses above 1 mg/night may be necessary in certain cases [76]. The main limitations of clonazepam are related to its problematic side effect profile, particularly as it pertains to elderly patients with dementia. These side effects may include increased confusion, drowsiness, and dizziness. Clonazepam should also be used with caution in those with pre-existing sleep apnea and gait disorders.
There have been multiple case series which have demonstrated the effectiveness of clonazepam on RBD. A study by Olson et al. demonstrated that clonazepam treatment was completely or partially successful in approximately 87% of patients who were given the medication [77]. Similarly, a study done in 1996 by Schenck and Mahowald followed 170 patients with RBD for a 12-year period who were treated with nightly clonazepam. In that cohort, complete or substantial control of RBD was achieved in 86% of patients [78].
Melatonin and clonazepam can be used together in cases where either one alone is not sufficient to treat RBD. In addition to melatonin and clonazepam, other treatments for RBD have also been investigated. A small crossover study done in 2012 showed a benefit in reducing the frequency of RBD episodes with the use of a rivastigmine patch at a dose of 4.6 mg/24 h [79]. Similarly, a case series involving three patients with RBD demonstrated some improvement with the use of donepezil [80].
Of note, there are several classes of medications that have been shown to induce or potentially exacerbate the symptoms of RBD and should be avoided if possible. These include tricyclic antidepressants, monoamine oxidase inhibitors, noradrenergic antagonists, and SSRIs [81].
8 Treatment of Autonomic Symptoms
As previously discussed, there are several associated features often encountered in patients with underlying Lewy body disease, including autonomic dysfunction, which may manifest as orthostatic hypotension, urinary issues, erectile dysfunction, and/or constipation. Dysautonomia occurs commonly in α-synucleinopathies, occurring in up to 60% of patients [82]. The distribution of Lewy body pathology is not strictly confined to the central nervous system, being found also in the peripheral sympathetic autonomic ganglia and the myenteric plexus of the gastrointestinal tract [83]. I-123 metaiodobenzylguanidine (MIBG) scans will demonstrate reduction of uptake in the peripheral sympathetic nervous system in both patients with DLB and PD regardless of whether they are experiencing symptoms of dysautonomia or not [84].
Orthostatic hypotension is defined as a reduction of 20 mmHg or more in systolic blood pressure and/or a reduction of 10 mmHg or more in diastolic blood pressure within 2–5 min of standing. In DLB, the orthostatic hypotension is often delayed, and may occur outside of the 5-min requirement [85]. Approximately 68% of patients with DLB experience orthostatic hypotension, and roughly 28% experience an episode of syncope [86, 87]. When orthostatic hypotension is verified in DLB, a thorough screening should be undertaken for possible medications that could be exacerbating the symptoms. These include diuretics, medications that induce vasodilation such as sildenafil, α-blockers, and tricyclic antidepressants. Levodopa and dopamine agonists may also worsen orthostatic hypotension. Non-pharmacological, supportive measures such as raising the head of the bed, increasing fluid and salt intake, and the use of support stockings or an abdominal binder should be initiated. If conservative measures fail, pharmacological agents such as fludrocortisone, midodrine, or droxidopa may be utilized. Fludrocortisone works to expand intravascular volume, while midodrine and droxidopa increase peripheral vascular resistance [88].
In addition to orthostatic hypotension, urinary issues are common in both PDD and DLB. In a Japanese study published in 2015 involving 32 patients with DLB, 91% had urinary symptoms [89]. Commonly encountered issues include urinary urgency, frequency, and incontinence. Antimuscarinic medications such as oxybutynin and trospium are generally avoided due to their potential for worsening cognitive deficits. In one case series involving 50 patients with PD using mirabegron (a β-3 adrenoceptor agonist) 50 mg daily, 50% reported improvement in their urinary symptoms, including 11.4% who had complete resolution [90].
Patients with α-synucleinopathies have widespread gastrointestinal disturbances at all levels. Dysphagia and drooling are common, occurring in 50–60% of patients with PD [91]. Patients with sialorrhea/drooling may benefit from multiple treatment options. Oral glycopyrrolate 1 mg twice daily has been shown to be beneficial. In a 4-week, randomized, double-blind, placebo-controlled crossover trial with oral glycopyrrolate in 23 patients with PD, the mean sialorrhea score improved from 4.6 with the placebo to 3.8 with glycopyrrolate (p = 0.011) [92]. Additionally, botulinum toxic injections into the salivary glands have been shown to be beneficial in reducing sialorrhea in PD [93].
Along with the aforementioned dysphagia and drooling, previous studies have also shown that up to 90% of patients with PD may have constipation [94]. In patients with DLB, similar studies have shown a frequency of approximately 30% [95]. When patients with Lewy body disease experience constipation, aggravating medications such as opiates should be discontinued if possible. Although not formally studied in clinical trials, dietary modifications such as increasing fiber and ensuring adequate hydration are usually recommended. Oral bulking agents such as psyllium may be beneficial. A previous study published in 1997 showed the psyllium increased stool frequency in PD patients with constipation [96]. Finally, another study involving the osmotic laxative polyethylene glycol showed efficacy in increasing bowel movement frequency in a placebo-controlled study involving patients with PD [97]. According to the evidence-based medicine committee of the Movement Disorder Society, lubiprostone and macrogol are possibly useful in treating constipation in PD [57]. In a high quality randomized clinical trial of PD patients with constipation, consumption of fermented milk containing probiotics and prebiotic fiber was superior to placebo in increasing bowel movements [98]. Linaclotide (guanylate cyclase C agonist) and prucalopride (selective 5-HT4 receptor agonist) are both FDA approved for treatment of chronic idiopathic constipation. In a retrospective study of patients with neurodegenerative parkinsonism and constipation who failed to respond to initial treatment for constipation, linaclotide (145 or 290 μg/day) or prucalopride (1–4mg/day) significantly increased the number of bowel movements [99]. A higher proportion of patients reported subjective satisfaction in controlling their constipation symptoms with the use of linaclotide as compared with prucalopride [99].
9 Lewy Body Dementia Drug Pipeline in 2022
There is an insufficient number of medications approved for the treatment of LBD. Rivastigmine is the only prescription drug approved by the US FDA in 2000 to treat mild to moderate dementia in people with PD. Japanese regulators have approved donepezil and zonisamide for treating cognition-related and motor symptoms in DLB, respectively [37, 100]. The failed phase IIb clinical study of intepirdine in 2016 was the first multi-continental trial involving patients with DLB [101]. There is currently no disease-modifying treatment for LBD. There has been a significant increase in interest in conducting clinical trials for patients with LBD over the past decade.
The ClinicalTrials.gov site was examined in March 2022. Dementia with Lewy bodies was the disease specified, as was Lewy body disease and Lewy body dementia. The review includes only drug-related interventional trials. There were four types of recruitment status included: not yet recruiting, recruiting, enrolling by invitation, and active but not recruiting. Trials not included were completed, terminated, suspended, or withdrawn, or the subjects did not have dementia. In total, 10 drug trials were identified. The trials of all of the agents presented were listed as phase I (N = 1) or phase II (N = 9) in the database and there were multiple key topics entered: agent, condition, beginning date, projected end date, number of subjects planned to enroll, number of arms of the study, whether a biomarker was described, mechanism of action, primary outcome, sponsorship by biopharma companies or NIH or academic medical center, ClinicalTrials.gov identifier (NCT number), and phase of the study (Table 1). Another topic entered was the mechanism of action (MOA); all but one of the current trials were disease-modifying treatments (DMTs). DMTs were arranged by mechanisms of action. We also included one agent (irsenontrine, E2027) after discussion as the trial was recently completed, and therefore would not have fallen under our defined search criteria for 2022.
9.1 Tyrosine Kinase Inhibitors
Currently, three of the medications under investigation for DLB are tyrosine kinase inhibitors. These trials are being conducted on a single trial site.
9.1.1 Nilotinib
Nilotinib is approved for treating certain types of leukemia by the FDA. Studies were conducted to determine if this compound can break down abnormal α-synuclein proteins found in DLB or decrease phosphorylated tau levels in the brain as reported in animal models [102, 103].
Nilotinib appeared to promote the clearance of α-synuclein by autophagy in animal models [104]. Phase II trials in PD and PDD failed to demonstrate benefits. Georgetown University’s first trial showed that the group that received 300 mg daily had a decline in activities of daily living from baseline to 12 months. A multicenter trial found no effect of the drug on dopamine biomarkers [105].
Another trial of nilotinib in AD failed to report any benefit, and participants taking 300 mg daily experienced significantly worse behavioral symptoms [106].
Previous phase II trials of nilotinib in PD, PDD, and AD did not show any benefit. Nilotinib is currently being tested in a phase II trial at Georgetown University in patients with DLB (NCT04002674).
9.1.2 Bosutinib
Bosutinib is an oral inhibitor of Abl and Src tyrosine kinases approved by the FDA for the treatment of chronic myeloid leukemia. Bosutinib reduced levels of α-synuclein in mouse models expressing human synucleinopathy.
Bosutinib enhanced dopaminergic neuron survival, modulated the immune response to α-synuclein, and helped with α-amyloid and tau clearance and cognitive improvement [103, 107].
One open-label study of bosutinib in patients with AD or PD found that after 1 year of treatment, bosutinib resulted in less decline in both Clinical Dementia Rating (CDR) scores and Repeatable Battery Assessment of Neuropsychological Status (RBANS) performance than predicted population-based decline [108].
A single-site, phase II study is underway to assess safety tolerability, biomarkers, and clinical outcomes of bosutinib in DLB (NCT03888222).
9.1.3 K0706
K0706 is under development for treatment of chronic myeloid leukemia (CML) and Philadelphia positive acute lymphoblastic leukemia that is resistant or intolerant to prior tyrosine kinase inhibitor therapy. Tyrosine kinase inhibitors induce autophagy, which degrades neurotoxic proteins such as α-synuclein, β-amyloid, and tau in PD and AD models. The current study will serve as a proof of concept for future trials in DLB and PD (NCT03996460).
9.2 Irsenontrine (E2027)
E2027 is a highly selective and potent inhibitor of phosphodiesterase 9 (PDE9) [109]. PDE9 breaks down cyclic guanosine monophosphate (cGMP), which serves as a second messenger in synaptic function and cognitive function. PDE9 inhibition by E2027 increases cGMP levels which may protect against α-synuclein toxicity in DLB [109, 110]. In 2018, a phase II/III trial enrolled 206 participants with DLB for 12 weeks of treatment with E2027 50 mg daily, or placebo. The results have not been published yet. The sponsor has followed with an open-label trial of E2027 in four groups of participants with DLB or PDD with or without amyloid co-pathology. The results are expected to be released in 2022.
9.3 Terazosin
Terazosin is an α-blocker, approved for management of benign prostate hypertrophy symptoms by relaxing the muscles of the bladder and prostate. It is proposed that terazosin also enhances the activity of phosphoglycerate kinase 1 (PGK1), stimulating glycolysis and increases cellular brain ATP levels and slowed neuron loss in mouse and rat models of PD. Dopamine level was also increased with partial restoration of mobility [111].
A cohort database study from Denmark and the United States showed that men taking terazosin were between 12% and 37% less likely to develop PD during the follow-up period than men taking tamsulosin, another α1-adrenergic receptor antagonist which does not activate phosphoglycerate kinase [112].
Lack of ATP production is a common feature of Parkinson’s and other neurodegenerative conditions. The above studies are encouraging, and suggest that terazosin can be a good candidate to repurpose in clinical trials across the PD spectrum. The current randomized clinical trial in DLB explores tolerability and changes in cognition, mobility, and behavior. The secondary outcome also explore changes in fluorodeoxyglucose (FDG)-PET, a surrogate for glucose metabolism, serum ATP, and terazosin level (NCT04760860).
A carrier for a pathological mutation in β-glucocerebrosidase gene (GBA1) has a strong genetic risk factors for PD, PDD, and LBD [113]. Animal models have shown that raising the levels of glucocerebrosidase can decrease levels of α-synuclein. Ambroxol is able to raise the levels glucocerebrosidase and is proposed as a disease-modifying treatment for PDD [114]. A phase II, single-center, double-blind, randomized placebo-controlled trial involving 75 individuals with mild to moderate PDD was designed (NCT02914366). Primary outcome measures were the Alzheimer’s Disease Assessment Scale—cognitive subscale (ADAS-Cog) and the ADCS-CGIC. Secondary measures included different cognitive and mobility scales. Markers of neurodegeneration will include MRI and CSF measures [114]. The results are not published yet. The current phase II trial investigates the effects of ambroxol on cognition, functional decline, and on neuropsychiatric symptoms of the glucocerebrosidase-enhancing chaperone ambroxol in 172 participants diagnosed with prodromal and early DLB (NCT04588285). Another clinical trial is underway for 15 participants with LBD (NCT04405596). The participants will be randomized to placebo or ambroxol 450 mg/day with titration to a maximum of 1350 mg/day.
9.4 CT1812
CT1812 is a small molecule receptor antagonist designed to inhibit synaptic binding and signaling by soluble Aβ oligomers [115]. CT1812 does not appear to interact directly with β-amyloid protein. Instead, CT1812 binds to the σ-2 receptor complex, which is a key oligomer binding site regulator, displacing Aβ oligomers from their receptor targets at the synapses in preclinical AD models, which facilitates oligomer clearance into the CSF [116]. A small study in patients with mild AD showed the CT1812-treated group had significantly lower levels of neurogranin, a marker of synaptic damage [116].
A randomized clinical trial (NCT05225415) is underway for DLB patients at doses of 300 and 100 mg over a 24-week period based on the hypothesis that σ-2 receptors regulate autophagy, which is impaired in synucleinopathy [117]. Additionally, DLB patients often have both amyloid pathology and synucleinopathy in the brain. It has been hypothesized that σ-2 receptor modulators may inhibit α-synuclein oligomer and Aβ oligomer-induced toxicity to neurons, thereby restoring normal neuronal function.
9.5 NYX-458
NYX-458 is an NMDA receptor modulator. In primate models of PD, NYX-458 improved attention, working memory, and executive function rapidly and continuously [118].
The current trial is being conducted on subjects with MCI or mild dementia associated with PD or DLB (NCT04148391).
9.6 CST-103 (Clenbuterol)
Clenbuterol (CST-103) is a β2-agonist that was reported to increase cerebral blood flow in patients with MCI or PD [119].
The reduction of noradrenergic signaling from neurons in the locus coeruleus may result in reduced activity of neurons in the prefrontal cortex, thalamus, hippocampus, and amygdala. In neurodegenerative disorders, activation of excitatory receptors of the ascending noradrenergic system by β2-adrenergic receptors could serve as an attractive therapeutic target. Long-term exposure to β2-agonists may cause undesirable peripheral effects, such as tachycardia, hyperglycemia, and hypokalemia. To counter the adverse effects of chronic therapy on cardiovascular and metabolic systems, co-administration of a peripherally restricted β-blocker, nadolol, was studied [120].
A small study with seven patients with MCI and one with PD was conducted. The patients received a first dose of clenbuterol 80 g at the beginning of the study and a second dose following a 7-day washout. In the second visit, half of the patients were pre-treated with nadolol 1 mg 2.5 h before receiving clenbuterol. Following clenbuterol administration, the hippocampus, the thalamus, and the amygdala showed significant increases in cerebral blood flow. Nadolol administered before clenbuterol did not alter the central effect of clenbuterol on cerebral blood flow [120].
The current trial is a two-period, two-way crossover trial to evaluate clenbuterol in four subject populations of PD patients with RBD and depression, MCI with depression, DLB with cognitive fluctuations, and PDD with cognitive fluctuations. Clenbuterol will be co-administered with nadolol for a 14-day period (NCT04739423) [121].
9.7 ATH-1017 (Fosgonimeton)
Fosgonimeton (ATH-1017, formerly known as NDX-1017), is a small molecule designed to affect neurodegeneration by activating hepatocyte growth factor (HGF) signaling and its tyrosine kinase receptor, MET. Activation of the HGF/MET system promotes survival and regeneration [122].
A phase I (NCT03298672) safety study of single subcutaneous daily injections of fosgonimeton in healthy people and AD patients raised no safety issues, with dose-proportional pharmacokinetics in all groups [123]. Quantitative electroencephalography (qEEG) and event-related potential (ERP) measured neurophysiological signals as indicative of brain penetration and target engagement. People with AD have prolonged P300 latency. P300 refers to the spike in activity following the presentation of a stimulus as measured during EEG. In the trial, fosgonimeton improved p300 latency in the AD group. The fast-onset normalization of ERP P300 latency in AD subjects was hypothesized to enhance synaptic function and potential cognitive effects [123]. In addition to two ongoing phase II trials for participants with mild to moderate AD, a current trial intends to enroll 75 patients with LBD to receive fosgonimeton or placebo over the course of 26 weeks (NCT04831281).
10 Conclusions
DLB and PDD are complex disorders with heterogeneous and often overlapping clinical and pathological findings. The treatment of these disorders is primarily symptomatic, as disease-modifying therapies do not currently exist. There is some evidence to support the benefit of cholinesterase inhibitors for treating cognitive and neuropsychiatric symptoms in LBD. Additionally, rivastigmine is FDA-approved for use in PDD. The benefits of memantine for treating the cognitive symptoms of LBD are not as well established and further studies are required. The motor symptoms of DLB are often less responsive to levodopa when compared with patients with PD. More recently, a phase III clinical trial demonstrated the benefit of zonisamide in improving the motor symptoms of DLB. In patients with significant neuropsychiatric symptoms, typical antipsychotics should be avoided. There is some data to suggest possible efficacy of atypical antipsychotics, quetiapine, clozapine, and olanzapine. For PD psychosis, pimavanserin has been shown to be beneficial, though its efficacy in DLB patients has not been fully established. Both melatonin and clonazepam are effective in decreasing the frequency and severity of RBD. Symptoms of dysautonomia are common in DLB and PDD, and include orthostatic hypotension, constipation, and urinary symptoms. Medications such as fludrocortisone, midodrine, or droxidopa may be utilized for orthostatic hypotension if conservative measures are insufficient. For urinary issues, mirabegron may be beneficial in decreasing symptoms. And finally, psyllium and polyethylene glycol, lubiprostone, linaclotide, or prucalopride have demonstrated efficacy when constipation is present.
LBD drug development has improved noticeably over the past few years. Neflamapimod may be the first new drug to advance toward a phase III trial for LBD in the near future. With nine agents currently in clinical trials looking to find a disease-modifying treatment, the landscape of LBD drug development is moving more towards disease-modifying therapies. Given the heterogeneous nature of Lewy body dementia, new biomarker strategies and better definition of outcome measures are necessary to improve drug trial designs.
References
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88–100.
Thomas AJ, Taylor JP, McKeith I, Bamford C, Burn D, Allan L, et al. Development of assessment toolkits for improving the diagnosis of the Lewy body dementias: feasibility study within the DIAMOND Lewy study. Int J Geriatr Psychiatry. 2017;32(12):1280–1304.
O’Brien JT, Taylor J-P, Thomas A, Bamford C, Vale L, Hill S, et al. Improving the diagnosis and management of Lewy body dementia: the DIAMOND-Lewy research programme including pilot cluster RCT. Program Grants Appl Res. 2021;9(7):1–120.
Taylor J-P, Pillai M. Current management strategies: the DIAMOND-Lewy toolkit. Alzheimer’s Dement [Internet]. 2021;17(Suppl.6):e052531. https://doi.org/10.1002/alz.052531.
Vann Jones SA, O’Brien JT. The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Psychol Med [Internet]. 2014;44(4):673–83. https://pubmed.ncbi.nlm.nih.gov/23521899/. [cited 2021 Nov 14].
Irizarry MC, Growdon W, Gomez-Isla T, Newell K, George JM, Clayton DF, et al. Nigral and cortical Lewy bodies and dystrophic nigral neurites in Parkinson’s disease and cortical Lewy body disease contain alpha-synuclein immunoreactivity. J Neuropathol Exp Neurol [Internet]. 1998;57(4):334–7. https://pubmed.ncbi.nlm.nih.gov/9600226/. [cited 2021 Nov 14].
Jellinger KA, Attems J. Prevalence and impact of vascular and Alzheimer pathologies in Lewy body disease. Acta Neuropathol [Internet]. 2008;115(4):427–36. https://pubmed.ncbi.nlm.nih.gov/18273624/. [cited 2021 Nov 14].
Perry EK, Haroutunian V, Davis KL, Levy R, Lantos P, Eagger S, et al. Neocortical cholinergic activities differentiate Lewy body dementia from classical Alzheimer’s disease. Neuroreport [Internet]. 1994;5(7):747–9. https://pubmed.ncbi.nlm.nih.gov/8018843/. [cited 2021 Nov 14].
Piggott MA, Marshall EF, Thomas N, Lloyd S, Court JA, Jaros E, et al. Striatal dopaminergic markers in dementia with Lewy bodies, Alzheimer’s and Parkinson’s diseases: rostrocaudal distribution. Brain [Internet]. 1999;122 (Pt 8)(8):1449–68. https://pubmed.ncbi.nlm.nih.gov/10430831/. [cited 2021 Nov 14].
Lippa CF, Duda JE, Grossman M, Hurtig HI, Aarsland D, Boeve BF, et al. DLB and PDD boundary issues: diagnosis, treatment, molecular pathology, and biomarkers. Neurology [Internet]. 2007;68(11):812–9. https://pubmed.ncbi.nlm.nih.gov/17353469/. [cited 2021 Nov 14].
Mollenhauer B, Esselmann H, Trenkwalder C, Schulz-Schaeffer W, Kretzschmar H, Otto M, et al. CSF amyloid-β peptides in neuropathologically diagnosed dementia with Lewy bodies and Alzheimer’s disease. J Alzheimers Dis [Internet]. 2011;24(2):383–91. https://pubmed.ncbi.nlm.nih.gov/21297274/. [cited 2021 Nov 14].
Parnetti L, Tiraboschi P, Lanari A, Peducci M, Padiglioni C, D’Amore C, et al. Cerebrospinal fluid biomarkers in Parkinson’s disease with dementia and dementia with Lewy bodies. Biol Psychiatry [Internet]. 2008;64(10):850–5. https://pubmed.ncbi.nlm.nih.gov/18395699/. [cited 2021 Nov 14].
McKeith I, O’Brien J, Walker Z, Tatsch K, Booij J, Darcourt J, et al. Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with Lewy bodies: a phase III, multicentre study. Lancet Neurol [Internet]. 2007;6(4):305–13. https://pubmed.ncbi.nlm.nih.gov/17362834/. [cited 2021 Nov 14].
Boeve BF, Silber MH, Ferman TJ, Lin SC, Benarroch EE, Schmeichel AM, et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med [Internet]. 2013;14(8):754–62. https://pubmed.ncbi.nlm.nih.gov/23474058/. [cited 2021 Nov 14].
Yoshita M, Arai H, Arai H, Arai T, Asada T, Fujishiro H, et al. Diagnostic accuracy of 123I-meta-iodobenzylguanidine myocardial scintigraphy in dementia with Lewy bodies: a multicenter study. PLoS One [Internet]. 2015;10(3). https://pubmed.ncbi.nlm.nih.gov/25793585/. [cited 2021 Nov 14].
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord [Internet]. 2015;30(12):1591–601. https://pubmed.ncbi.nlm.nih.gov/26474316/. [cited 2021 Nov 14].
Aarsland D, Creese B, Politis M, Chaudhuri KR, Ffytche DH, Weintraub D, et al. Cognitive decline in Parkinson disease. Nat Rev Neurol [Internet]. 2017;13(4):217–31. https://pubmed.ncbi.nlm.nih.gov/28257128/. [cited 2021 Nov 14].
Hely MA, Morris JGL, Reid WGJ, Trafficante R. Sydney multicenter study of Parkinson’s disease: non-l-dopa-responsive problems dominate at 15 years. Mov Disord [Internet]. 2005;20(2):190–9. https://pubmed.ncbi.nlm.nih.gov/15551331/. [cited 2021 Nov 14].
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord [Internet]. 2007;22(12):1689–707. https://pubmed.ncbi.nlm.nih.gov/17542011/. [cited 2021 Nov 14].
Bradshaw J, Saling M, Hopwood M, Anderson V, Brodtmann A. Fluctuating cognition in dementia with Lewy bodies and Alzheimer’s disease is qualitatively distinct. J Neurol Neurosurg Psychiatry [Internet]. 2004;75(3):382–7. https://pubmed.ncbi.nlm.nih.gov/14966152/. [cited 2021 Nov 14].
Walker MP, Ayre GA, Cummings JL, Wesnes K, McKeith IG, O’Brien JT, et al. Quantifying fluctuation in dementia with Lewy bodies, Alzheimer’s disease, and vascular dementia. Neurology [Internet]. 2000;54(8):1616–24. https://pubmed.ncbi.nlm.nih.gov/10762503/. [cited 2021 Nov 14].
Grothe MJ, Schuster C, Bauer F, Prudlo J, Teipel SJ, Heinsen H. Atrophy of the cholinergic basal forebrain in dementia with Lewy bodies and Alzheimer’s disease dementia. J Neurol [Internet]. 2014;261(10):1939–48. https://pubmed.ncbi.nlm.nih.gov/25059393/. [cited 2021 Nov 14].
McKeith I, Del Ser T, Spano P, Emre M, Wesnes K, Anand R, et al. Efficacy of rivastigmine in dementia with Lewy bodies: a randomised, double-blind, placebo-controlled international study. Lancet. 2000;356(9247):2031–6.
Mori E, Ikeda M, Kosaka K. Donepezil for dementia with Lewy bodies: a randomized, placebo-controlled trial. Ann Neurol [Internet]. 2012;72(1):41–52. https://pubmed.ncbi.nlm.nih.gov/22829268/. [cited 2021 Nov 14].
Ikeda M, Mori E, Matsuo K, Nakagawa M, Kosaka K. Donepezil for dementia with Lewy bodies: a randomized, placebo-controlled, confirmatory phase III trial. Alzheimers Res Ther. 2015;7(1):4-014-0083–0 (eCollection 2015).
Edwards K, Royall D, Hershey L, Lichter D, Hake A, Farlow M, et al. Efficacy and safety of galantamine in patients with dementia with Lewy bodies: a 24-week open-label study. Dement Geriatr Cogn Disord [Internet]. 2007;23(6):401–5. https://pubmed.ncbi.nlm.nih.gov/17409748/. [cited 2021 Nov 14].
Warre R, Thiele S, Talwar S, Kamal M, Johnston TH, Wang S, et al. Altered function of glutamatergic cortico-striatal synapses causes output pathway abnormalities in a chronic model of parkinsonism. Neurobiol Dis [Internet]. 2011;41(3):591–604. https://pubmed.ncbi.nlm.nih.gov/20971190/. [cited 2021 Nov 14].
Aarsland D, Ballard C, Walker Z, Bostrom F, Alves G, Kossakowski K, et al. Memantine in patients with Parkinson’s disease dementia or dementia with Lewy bodies: a double-blind, placebo-controlled, multicentre trial. Lancet Neurol [Internet]. 2009;8(7):613–8. https://pubmed.ncbi.nlm.nih.gov/19520613/. [cited 2021 Nov 14].
Emre M, Tsolaki M, Bonuccelli U, Destee A, Tolosa E, Kutzelnigg A, et al. Memantine for patients with Parkinson’s disease dementia or dementia with Lewy bodies: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(10):969–77.
EIP. EIP Pharma Announces Presentation of Positive Clinical Trial Results with Neflamapimod at the 13th Clinical Trials in Alzheimer’s Disease (CTAD) Meeting [Internet accessed 2021 Nov 14]. 2020. https://www.eippharma.com/news/eip-pharma-announces-presentation-of-positive-clinical-trial-results-with-neflamapimod-at-the-13th-clinical-trials-in-alzheimers-disease-ctad-meeting/.
Alam J, EIP Pharma Boston M. Clinical results with Novel Approaches that Reverses BFCN Dysfunction. J Prev Alzhiemer’s Dis. 2021;8(4):S9.
Aarsland D, Ballard C, McKeith I, Perry RH, Larsen JP. Comparison of extrapyramidal signs in dementia with Lewy bodies and Parkinson’s disease. J Neuropsychiatry Clin Neurosci [Internet]. 2001;13(3):374–9. https://pubmed.ncbi.nlm.nih.gov/11514644/. [cited 2021 Nov 14].
Burns A, O’Brien J, Group BAPDC, Auriacombe S, Ballard C, Broich K, et al. Clinical practice with anti-dementia drugs: a consensus statement from British Association for Psychopharmacology. J Psychopharmacol. 2006;20(6):732–55.
Burn DJ, Rowan EN, Minett T, Sanders J, Myint P, Richardson J, et al. Extrapyramidal features in Parkinson’s disease with and without dementia and dementia with Lewy bodies: a cross-sectional comparative study. Mov Disord [Internet]. 2003;18(8):884–9. https://pubmed.ncbi.nlm.nih.gov/12889077/. [cited 2021 Nov 14].
Molloy S, McKeith IG, O’Brien JT, Burn DJ. The role of levodopa in the management of dementia with Lewy bodies. J Neurol Neurosurg Psychiatry [Internet]. 2005;76(9):1200–3. https://pubmed.ncbi.nlm.nih.gov/16107351/. [cited 2021 Nov 14].
Goldman JG, Goetz CG, Brandabur M, Sanfilippo M, Stebbins GT. Effects of dopaminergic medications on psychosis and motor function in dementia with Lewy bodies. Mov Disord. 2008;23(15):2248–50.
Sumitomo Dainippon Pharma Co. Sumitomo Dainippon Pharma Obtains Approval in Japan for TRERIEF, a therapeutic agent for Parkinson’s disease, for an Additional Indication of Parkinsonism in Dementia with Lewy Bodies [Internet]. 2018. https://www.ds-pharma.com/ir/news/2018/20180702.html. Accessed 4 Dec 2021.
Murata M, Hasegawa K, Kanazawa I, Shirakura K, Kochi K, Shimazu R. Randomized placebo-controlled trial of zonisamide in patients with Parkinson’s disease. Neurol Clin Neurosci. 2016;4(1):10–15.
Murata M, Odawara T, Hasegawa K, Kajiwara R, Takeuchi H, Tagawa M, et al. Effect of zonisamide on parkinsonism in patients with dementia with Lewy bodies: a phase 3 randomized clinical trial. Park Relat Disord. 2020;76:91–97.
Dainippon Sumitomo Pharma Co. Parkinson’s disease drug “TRERIEF” obtained manufacturing and marketing approval [Internet]. 2009. https://www.ds-pharma.com/ir/news/2009/20090121.html.
Seino M. Review of zonisamide development in Japan. Seizure. 2004.
Tousi B, Leverenz JB. The application of zonisamide to patients suffering from dementia with Lewy bodies: emerging clinical data. Drug Des Devel Ther. 2021;15:1811–17.
Shulman LM, Katzel LI, Ivey FM, Sorkin JD, Favors K, Anderson KE, et al. Randomized clinical trial of 3 types of physical exercise for patients with Parkinson disease. JAMA Neurol [Internet]. 2013;70(2):183–90. https://pubmed.ncbi.nlm.nih.gov/23128427/. [cited 2021 Nov 14].
Uc EY, Doerschug KC, Magnotta V, Dawson JD, Thomsen TR, Kline JN, et al. Phase I/II randomized trial of aerobic exercise in Parkinson disease in a community setting. Neurology [Internet]. 2014;83(5):413–25. https://pubmed.ncbi.nlm.nih.gov/24991037/. [cited 2021 Nov 14].
Song R, Grabowska W, Park M, Osypiuk K, Vergara-Diaz GP, Bonato P, et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord [Internet]. 2017;41:3–13. https://pubmed.ncbi.nlm.nih.gov/28602515/. [cited 2021 Nov 14].
Ballard C, Holmes C, McKeith I, Neill D, O’Brien J, Cairns N, et al. Psychiatric morbidity in dementia with Lewy bodies: a prospective clinical and neuropathological comparative study with Alzheimer’s disease. Am J Psychiatry [Internet]. 1999;156(7):1039–45. https://pubmed.ncbi.nlm.nih.gov/10401449/. [cited 2021 Nov 14].
Leggett AN, Zarit S, Taylor A, Galvin JE. Stress and burden among caregivers of patients with Lewy body dementia. Gerontologist. 2011;51(1):76–85.
Jellinger KA. Dementia with Lewy bodies and Parkinson’s disease-dementia: current concepts and controversies. J Neural Transm [Internet]. 2018;125(4):615–50. https://pubmed.ncbi.nlm.nih.gov/29222591/. [cited 2021 Nov 14].
Ballard CG, O’Brien JT, Swann AG, Thompson P, Neill D, McKeith IG. The natural history of psychosis and depression in dementia with Lewy bodies and Alzheimer’s disease: persistence and new cases over 1 year of follow-up. J Clin Psychiatry [Internet]. 2001;62(1):46–9. https://pubmed.ncbi.nlm.nih.gov/11235928/. [cited 2021 Nov 14].
Bonanni L, Thomas A, Tiraboschi P, Perfetti B, Varanese S, Onofrj M. EEG comparisons in early Alzheimer’s disease, dementia with Lewy bodies and Parkinson’s disease with dementia patients with a 2-year follow-up. Brain. 2008;131(Pt 3):690–705.
Borroni B, Agosti C, Padovani A. Behavioral and psychological symptoms in dementia with Lewy-bodies (DLB): frequency and relationship with disease severity and motor impairment. Arch Gerontol Geriatr. 2008;46(1):101–6.
Chiu PY, Wang CW, Tsai CT, Li SH, Lin CL, Lai TJ. Depression in dementia with Lewy bodies: A comparison with Alzheimer’s disease. PLoS One [Internet]. 2017;12(6). https://pubmed.ncbi.nlm.nih.gov/28617831/. [cited 2021 Nov 14].
Aarsland D, Perry R, Larsen JP, McKeith IG, O’Brien JT, Perry EK, et al. Neuroleptic sensitivity in Parkinson’s disease and parkinsonian dementias. J Clin Psychiatry [Internet]. 2005;66(5):633–7. https://pubmed.ncbi.nlm.nih.gov/15889951/. [cited 2021 Nov 14].
Takahashi H, Yoshida K, Sugita T, Higuchi H, Shimizu T. Quetiapine treatment of psychotic symptoms and aggressive behavior in patients with dementia with Lewy bodies: a case series. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(3):549–53.
Kurlan R, Cummings J, Raman R, Thal L, Group ADCS. Quetiapine for agitation or psychosis in patients with dementia and parkinsonism. Neurology. 2007;68(17):1356–63.
Cummings JL, Street J, Masterman D, Clark WS. Efficacy of olanzapine in the treatment of psychosis in dementia with lewy bodies. Dement Geriatr Cogn Disord [Internet]. 2002];13(2):67–73. https://pubmed.ncbi.nlm.nih.gov/11844887/. [cited 2021 Nov 14.
Pollak P, Tison F, Rascol O, Destée A, Péré JJ, Senard JM, et al. Clozapine in drug induced psychosis in Parkinson’s disease: a randomised, placebo controlled study with open follow up. J Neurol Neurosurg Psychiatry [Internet]. 2004;75(5):689–95. https://pubmed.ncbi.nlm.nih.gov/15090561/. [cited 2021 Nov 14].
Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. 2017;12(1):103–11.
Chu CS, Yang FC, Tseng PT, Stubbs B, Dag A, Carvalho AF, et al. Treatment efficacy and acceptabilityof pharmacotherapies for dementia with Lewy bodies: a systematic review and network meta-analysis. Arch Gerontol Geriatr [Internet]. 2021;96. https://pubmed.ncbi.nlm.nih.gov/34256210/. [cited 2021 Nov 14].
Cummings J, Isaacson S, Mills R, Williams H, Chi-Burris K, Corbett A, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet (London, England). 2014;383(9916):533–40.
Tariot PN, Cummings JL, Soto-Martin ME, Ballard C, Erten-Lyons D, Sultzer DL, et al. Trial of pimavanserin in dementia-related psychosis. N Engl J Med [Internet]. 2021];385(4):309–19. https://pubmed.ncbi.nlm.nih.gov/34289275/. [cited 2021 Nov 14.
Acadia Pharmaceuticals Receives Complete Response Letter from US FDA for Supplemental New Drug Application for Pimavanserin for the Treatment of Hallucinations and Delusions Associated with Dementia-Related Psychosis | Acadia Pharmaceuticals Inc. [Internet]. [Accessed 2021 Nov 14]. https://ir.acadia-pharm.com/news-releases/news-release-details/acadia-pharmaceuticals-receives-complete-response-letter-us-fda.
Yasue I, Matsunaga S, Kishi T, Fujita K, Iwata N. Serotonin 2A receptor inverse agonist as a treatment for Parkinson’s disease psychosis: a systematic review and meta-analysis of serotonin 2A receptor negative modulators. J Alzheimer’s Dis. 2016;50(3):733–40.
Horn S, Richardson H, Xie SX, Weintraub D, Dahodwala N. Pimavanserin versus quetiapine for the treatment of psychosis in Parkinson’s disease and dementia with Lewy bodies. Park Relat Disord. 2019;69:119–24.
Taylor JP, McKeith IG, Burn DJ, Boeve BF, Weintraub D, Bamford C, et al. New evidence on the management of Lewy body dementia. Lancet Neurol. 2020;19:157–69.
Seppi K, Ray Chaudhuri K, Coelho M, Fox SH, Katzenschlager R, Perez Lloret S, et al. Update on treatments for nonmotor symptoms of Parkinson’s disease—an evidence-based medicine review. Mov Disord. 2019;34:180–98.
Culo S, Mulsant BH, Rosen J, Mazumdar S, Blakesley RE, Houck PR, et al. Treating neuropsychiatric symptoms in dementia with Lewy bodies: a randomized controlled-trial. Alzheimer Dis Assoc Disord [Internet]. 2010;24(4):360–4. https://pubmed.ncbi.nlm.nih.gov/20625270/. [cited 2021 Nov 14].
Arrigoni E, Chen MC, Fuller PM. The anatomical, cellular and synaptic basis of motor atonia during rapid eye movement sleep. J Physiol. 2016;594:5391–414.
Boxer AL, Gold M, Huey E, Hu WT, Rosen H, Kramer J, et al. The advantages of frontotemporal degeneration drug development (part 2 of frontotemporal degeneration: the next therapeutic frontier). Alzheimers Dement. 2013;9(2):189–98.
Postuma RB, Gagnon JF, Vendette M, Fantini ML, Massicotte-Marquez J, Montplaisir J. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology [Internet]. 2009;72(15):1296–300. https://pubmed.ncbi.nlm.nih.gov/19109537/. [cited 2021 Nov 14].
Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med [Internet]. 2013;14(8):744–8. https://pubmed.ncbi.nlm.nih.gov/23347909/. [cited 2021 Nov 14].
Neikrug AB, Ancoli-Israel S. Diagnostic tools for REM sleep behavior disorder. Sleep Med Rev [Internet]. 2012;16(5):415–29. https://pubmed.ncbi.nlm.nih.gov/22169258/. [cited 2021 Nov 14].
Breen DP, Vuono R, Nawarathna U, Fisher K, Shneerson JM, Reddy AB, et al. Sleep and circadian rhythm regulation in early parkinson disease. JAMA Neurol. 2014;71(5):589–95.
McCarter SJ, Boswell CL, St. Louis EK, Dueffert LG, Slocumb N, Boeve BF, et al. Treatment outcomes in REM sleep behavior disorder. Sleep Med [Internet]. 2013;14(3):237–42. https://pubmed.ncbi.nlm.nih.gov/23352028/. [cited 2021 Nov 14].
McGrane IR, Leung JG, St Louis EK, Boeve BF. Melatonin therapy for REM sleep behavior disorder: a critical review of evidence. Sleep Med. 2015;16(1):19–26.
Schenck CH, Mahowald MW. Polysomnographie, neurologic, psychiatric, and clinical outcome report on 70 consecutive cases with REM sleep behavior disorder (RBD): sustained clonazepam efficacy in 89.5% of 57 treated patients. Cleve Clin J Med [Internet]. 1990;57(1 suppl 1):S-9. https://www.ccjm.org/content/57/1_suppl_1/S-9. [cited 2021 Nov 14].
Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain [Internet]. 2000;123 (Pt 2)(2):331–9. https://pubmed.ncbi.nlm.nih.gov/10648440/. [cited 2021 Nov 14].
Schenck CH, Mahowald MW. Long-term, nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med [Internet]. 1996;100(3):333–7. https://pubmed.ncbi.nlm.nih.gov/8629680/. [cited 2021 Nov 14].
Di Giacopo R, Fasano A, Quaranta D, Marca G Della, Bove F, Bentivoglio AR. Rivastigmine as alternative treatment for refractory REM behavior disorder in Parkinson’s disease. Mov Disord [Internet]. 2012;27(4):559–61. https://pubmed.ncbi.nlm.nih.gov/22290743/. [cited 2021 Nov 14].
Ringman JM, Simmons JH. Treatment of REM sleep behavior disorder with donepezil: a report of three cases. Neurology [Internet]. 2000;55(6):870–1. https://pubmed.ncbi.nlm.nih.gov/10994012/. [cited 2021 Nov 14].
Gagnon JF, Postuma RB, Montplaisir J. Update on the pharmacology of REM sleep behavior disorder. Neurology [Internet]. 2006;67(5):742–7. https://pubmed.ncbi.nlm.nih.gov/16966533/. [cited 2021 Nov 14].
Mendoza-Velásquez JJ, Flores-Vázquez JF, Barrón-Velázquez E, Sosa-Ortiz AL, Illigens BMW, Siepmann T. Autonomic Dysfunction in α-Synucleinopathies. Front Neurol [Internet]. 2019;10(APR). https://pubmed.ncbi.nlm.nih.gov/31031694/. [cited 2021 Nov 14].
Goedert M, Spillantini MG, Del Tredici K, Braak H. 100 years of Lewy pathology. Nat Rev Neurol [Internet]. 2013;9(1):13–24. https://pubmed.ncbi.nlm.nih.gov/23183883/. [cited 2021 Nov 14].
Yoshita M, Taki J, Yamada M. A clinical role for [(123)I]MIBG myocardial scintigraphy in the distinction between dementia of the Alzheimer’s-type and dementia with Lewy bodies. J Neurol Neurosurg Psychiatry [Internet]. 2001;71(5):583–8. https://pubmed.ncbi.nlm.nih.gov/11606666/. [cited 2021 Nov 14].
Joseph A, Wanono R, Flamant M, Vidal-Petiot E. Orthostatic hypotension: a review. Nephrol Ther [Internet]. 2017;13 Suppl 1:S55–67. https://pubmed.ncbi.nlm.nih.gov/28577744/. [cited 2021 Nov 14].
Horimoto Y, Matsumoto M, Akatsu H, Ikari H, Kojima K, Yamamoto T, et al. Autonomic dysfunctions in dementia with Lewy bodies. J Neurol [Internet]. 2003;250(5):530–3. https://pubmed.ncbi.nlm.nih.gov/12736730/. [cited 2021 Nov 14].
Bengtsson-Lindberg M, Larsson V, Minthon L, Wattmo C, Londos E. Lack of orthostatic symptoms in dementia patients with orthostatic hypotension. Clin Auton Res [Internet]. 2015;25(2):87–94. https://pubmed.ncbi.nlm.nih.gov/24743866/. [cited 2021 Nov 14].
Palma JA, Kaufmann H. Treatment of autonomic dysfunction in Parkinson disease and other synucleinopathies. Mov Disord [Internet]. 2018;33(3):372–90. https://pubmed.ncbi.nlm.nih.gov/29508455/. [cited 2021 Nov 14].
Tateno F, Sakakibara R, Ogata T, Kishi M, Tsuyusaki Y, Takahashi O, et al. Lower urinary tract function in dementia with Lewy bodies (DLB). Mov Disord [Internet]. 2015;30(3):411–5. https://pubmed.ncbi.nlm.nih.gov/25356960/. [cited 2021 Nov 14].
Peyronnet B, Vurture G, Palma JA, Malacarne DR, Feigin A, Sussman RD, et al. Mirabegron in patients with Parkinson disease and overactive bladder symptoms: a retrospective cohort. Parkinsonism Relat Disord [Internet]. 2018;57:22–6. https://pubmed.ncbi.nlm.nih.gov/30037689/. [cited 2021 Nov 14].
Kalf JG, De Swart BJM, Borm GF, Bloem BR, Munneke M. Prevalence and definition of drooling in Parkinson’s disease: a systematic review. J Neurol [Internet]. 2009;256(9):1391–6. https://pubmed.ncbi.nlm.nih.gov/19288042/. [cited 2021 Nov 14].
Arbouw MEL, Movig KLL, Koopmann M, Poels PJE, Guchelaar HJ, Egberts TCG, et al. Glycopyrrolate for sialorrhea in Parkinson disease: a randomized, double-blind, crossover trial. Neurology [Internet]. 2010;74(15):1203–7. https://pubmed.ncbi.nlm.nih.gov/20385892/. [cited 2021 Nov 14].
Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, et al. The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord [Internet]. 2011;26 Suppl 3(0 3). https://pubmed.ncbi.nlm.nih.gov/22021174/. [cited 2021 Nov 14].
Martinez-Martin P, Chaudhuri KR, Rojo-Abuin JM, Rodriguez-Blazquez C, Alvarez-Sanchez M, Arakaki T, et al. Assessing the non-motor symptoms of Parkinson’s disease: MDS-UPDRS and NMS Scale. Eur J Neurol [Internet]. 2015;22(1):37–43. https://pubmed.ncbi.nlm.nih.gov/23607783/. [cited 2021 Nov 14].
Stubendorff K, Aarsland D, Minthon L, Londos E. The impact of autonomic dysfunction on survival in patients with dementia with Lewy bodies and Parkinson’s disease with dementia. PLoS One [Internet]. 2012;7(10). https://pubmed.ncbi.nlm.nih.gov/23049679/. [cited 2021 Nov 14].
Ashraf W, Pfeiffer RF, Park F, Lof J, Quigley EMM. Constipation in Parkinson’s disease: objective assessment and response to psyllium. Mov Disord [Internet]. 1997;12(6):946–51. https://pubmed.ncbi.nlm.nih.gov/9399219/. [cited 2021 Nov 14].
Zangaglia R, Martignoni E, Glorioso M, Ossola M, Riboldazzi G, Calandrella D, et al. Macrogol for the treatment of constipation in Parkinson’s disease. A randomized placebo-controlled study. Mov Disord [Internet]. 2007;22(9):1239–44. https://pubmed.ncbi.nlm.nih.gov/17566120/. [cited 2021 Nov 14].
Barichella M, Pacchetti C, Bolliri C, Cassani E, Iorio L, Pusani C, et al. Probiotics and prebiotic fiber for constipation associated with Parkinson disease. Neurology. 2016;87(12):1274–80.
Freitas ME, Alqaraawi A, Lang AE, Liu LWC. Linaclotide and prucalopride for management of constipation in patients with parkinsonism. Mov Disord Clin Pract. 2018;5(2):218–20.
Eisai. ARICEPT® approved in japan as treatment for dementia with Lewy bodies [Internet]. 2014. https://www.eisai.com/news/news201452.html. [cited 2022 Mar 30].
Lang FM, Kwon DY, Aarsland D, Boeve B, Tousi B, Harnett M, et al. An international, randomized, placebo-controlled, phase 2b clinical trial of intepirdine for dementia with Lewy bodies (HEADWAY-DLB). Alzheimers Dement (N Y). 2021;7(1):e12171.
Hebron M, Moussa CEH. Two sides of the same coin: tyrosine kinase inhibition in cancer and neurodegeneration. Neural Regener Res. 2015;10:1767–9.
Hebron ML, Lonskaya I, Moussa CEH. Nilotinib reverses loss of dopamine neurons and improves motor behavior via autophagic degradation of α-synuclein in Parkinson’s disease models. Hum Mol Genet. 2013;22(16):3315–28.
Mahul-Mellier AL, Fauvet B, Gysbers A, Dikiy I, Oueslati A, Georgeon S, et al. C-Abl phosphorylates α-synuclein and regulates its degradation: Implication for α-synuclein clearance and contribution to the pathogenesis of Parkinson’s disease. Hum Mol Genet. 2014;23(11):2858–79.
Merchant K, Simuni T, Fiske B, Coffey C, Matthews H, Wyse R, et al. Pharmacokinetics and biomarker changes in NILO-PD, a phase 2A study of nilotinib in patients with moderate to advance Parkinson’s disease (4418). Neurology. 2020;94(15 Supplement).
Turner RS, Hebron ML, Lawler A, Mundel EE, Yusuf N, Starr JN, et al. Nilotinib effects on safety, tolerability, and biomarkers in Alzheimer’s disease. Ann Neurol. 2020;88(1):183–94.
Lonskaya I, Hebron ML, Selby ST, Turner RS, Moussa CEH. Nilotinib and bosutinib modulate pre-plaque alterations of blood immune markers and neuro-inflammation in Alzheimer’s disease models. Neuroscience. 2015;304:316–27.
Mahdavi K, Jordan S, Barrows H, Pravdic M, Habelhah B, Evans N, et al. Treatment of dementia with bosutinib: an open-label study of a tyrosine kinase inhibitor. Neurol Clin Pract. 2021;11(3):e294–e302.
Ando M, Ishikawa Y, Horie K, Mochizuki T, Yamamoto M, Watanabe N, et al. P3‐062: effect of repeated administration of E2027, a novel phosphodiesterase‐9 inhibitor, on cyclic GMP levels in rat cerebrospinal fluid. Alzheimer’s Dement. 2018;14(7S_Part_20).
Höllerhage M, Moebius C, Melms J, Chiu WH, Goebel JN, Chakroun T, et al. Protective efficacy of phosphodiesterase-1 inhibition against alpha-synuclein toxicity revealed by compound screening in LUHMES cells. Sci Rep. 2017;7(1):11469.
Cai R, Zhang Y, Simmering JE, Schultz JL, Li Y, Fernandez-Carasa I, et al. Enhancing glycolysis attenuates Parkinson’s disease progression in models and clinical databases. J Clin Investig. 2019;129(10):4539–4549.
Simmering JE, Welsh MJ, Liu L, Narayanan NS, Pottegård A. Association of glycolysis-enhancing α-1 blockers with risk of developing Parkinson disease. JAMA Neurol. 2021;78(4):407–413.
Sidransky E, Lopez G. The link between the GBA gene and parkinsonism. Lancet Neurol. 2012;11(11):986–98.
Silveira CRA, MacKinley J, Coleman K, Li Z, Finger E, Bartha R, et al. Ambroxol as a novel disease-modifying treatment for Parkinson’s disease dementia: Protocol for a single-centre, randomized, double-blind, placebo-controlled trial. BMC Neurol. 2019;19(1):20.
Grundman M, Morgan R, Lickliter JD, Schneider LS, DeKosky S, Izzo NJ, et al. A phase 1 clinical trial of the sigma-2 receptor complex allosteric antagonist CT1812, a novel therapeutic candidate for Alzheimer’s disease. Alzheimer’s Dement Transl Res Clin Interv. 2019;5:20–26.
Izzo NJ, Yuede CM, LaBarbera KM, Limegrover CS, Rehak C, Yurko R, et al. Preclinical and clinical biomarker studies of CT1812: A novel approach to Alzheimer’s disease modification. Alzheimer’s Dement. 2021;17(8)1365–1382.
Arotcarena M-L, Teil M, Dehay B. Autophagy in synucleinopathy: the overwhelmed and defective machinery. Cells. 2019;8(6):565.
Barth AL, Schneider JS, Johnston TH, Hill MP, Brotchie JM, Moskal JR, et al. NYX-458 improves cognitive performance in a primate Parkinson’s disease model. Mov Disord. 2020;35(4):640–9.
CuraSen. Safety, Tolerability and cerebral blood flow after single doses of the Β2-agonist, Clebbuterol, in patients with mild cognitive impairment or Parkinson’s disease. [Internet]. 2021 [cited 2022 Mar 30]. https://www.curasen.com/curasen-therapeutics-presents-phase-1b-clinical-data-with-cst-103-demonstrating-significant-increases-in-cerebral-blood-flow-in-patients-with-mild-cognitive-impairment-or-parkinsons-disease/.
Lodeweyckx T, De hoon J, Van Laere K, Koole M, Vandenberghe W, Bishop C, et al. Abstract: Posters: 14th Clinical Trials on Alzheimer’s Disease (CTAD) November 9-12, 2021. J Prev Alzheimer’s Dis [Internet]. 2021;8(S1):S73–170. Available from: https://pubmed.ncbi.nlm.nih.gov/34773456
ClinicalTrials.gov[Internet]. Bethesda (MD): National Library of Medicine, (US). A Study of CST-103 Co-administered With CST-107 in Subjects With Neurodegenerative Disorders (CLIN-011) [Internet]. NCT04739423. 2021 [Accessed 2022 Dec 3]. https://clinicaltrials.gov/ct2/show/NCT04739423?term=cst-103&cond=Lewy+Body+Disease&draw=2&rank=1.
Takeuchi D, Sato N, Shimamura M, Kurinami H, Takeda S, Shinohara M, et al. Alleviation of Aβ-induced cognitive impairment by ultrasound-mediated gene transfer of HGF in a mouse model. Gene Ther. 2008;15(8):561–71.
Moebius H, Hua X, Church K, Walker W, L’hostis P, Danjou P, et al. Phase 1 study of NDX-1017: safety, pharmacokinetics, and pharmacodynamics in healthy volunteers and dementia patients. J Prev Alzheimer’s Dis. 2019;6, S22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There was no funding for this review.
Conflicts of interest
Babak Tousi has received consultancy and speaker fees and been a consultant for Eisai, Biogen, and Lilly. He has received honorarium for the Scientific Advisory Board from Biogen, Eisai, and Lilly. Steve MacDonald and Ayushi Shah have no conflicts of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
BT and SM had the idea for the article, drafted and critically revised the work. BT, AS, and SM performed the literature search and data analysis. All authors have read and approved the final submitted manuscript, and agree to be accountable for the work.
Rights and permissions
About this article
Cite this article
MacDonald, S., Shah, A.S. & Tousi, B. Current Therapies and Drug Development Pipeline in Lewy Body Dementia: An Update. Drugs Aging 39, 505–522 (2022). https://doi.org/10.1007/s40266-022-00939-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00939-w