Abstract
Introduction
Previous studies of antihypertensive treatment of older patients have focused on blood pressure control, cardiovascular risk or adherence, whereas data on inappropriate antihypertensive prescriptions to older patients are scarce.
Objectives
The aim of the study was to assess inappropriate antihypertensive prescriptions to older patients.
Methods
An observational, prospective multicentric study was conducted to assess potentially inappropriate prescription of antihypertensive drugs, in patients aged 75 years and older with arterial hypertension (HTN), in the month prior to hospital admission, using four instruments: Beers, Screening Tool of Older Person’s Prescriptions (STOPP), Screening Tool to Alert Doctors to the Right Treatment (START) and Assessing Care of Vulnerable Elders 3 (ACOVE-3). Primary care and hospital electronic records were reviewed for HTN diagnoses, antihypertensive treatment and blood pressure readings.
Results
Of 672 patients, 532 (median age 85 years, 56% female) had HTN. 21.6% received antihypertensive monotherapy, 4.7% received no hypertensive treatment, and the remainder received a combination of antihypertensive therapies. The most frequently prescribed antihypertensive drugs were diuretics (53.5%), angiotensin-converting enzyme inhibitors (ACEIs) (41%), calcium antagonists (32.2%), angiotensin receptor blockers (29.7%) and beta-blockers (29.7%). Potentially inappropriate prescription was observed in 51.3% of patients (27.8% overprescription and 35% underprescription). The most frequent inappropriately prescribed drugs were calcium antagonists (overprescribed), ACEIs and beta-blockers (underprescribed). ACEI and beta-blocker underprescriptions were independently associated with heart failure admissions [beta-blockers odds ratio (OR) 0.53, 95% confidence interval (CI) 0.39–0.71, p < 0.001; ACEIs OR 0.50, 95% CI 0.36–0.70, p < 0.001].
Conclusion
Potentially inappropriate prescription was detected in more than half of patients receiving antihypertensive treatment. Underprescription was more frequent than overprescription. ACEIs and beta-blockers were frequently underprescribed and were associated with heart failure admissions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Potentially inappropriate prescription of antihypertensive medication affects over half of elderly patients: overprescription 27.8% and underprescription 35%. |
Underprescription of angiotensin-converting enzyme inhibitors (ACEIs) and beta-blockers is associated with heart failure admissions in elderly patients with arterial hypertension. |
Physicians should carefully select and monitor response to antihypertensive treatment in elderly patients, bearing in mind adverse effects such as postural hypotension and constipation, and should take special care to avoid underprescription of ACEIs and beta-blockers in patients with heart failure. |
1 Introduction
High blood pressure [arterial hypertension (HTN)] is a major risk factor for cardiovascular disease. The prevalence of HTN in the general population in Spain is estimated to be around 30–35% [1] and to be as high as 71% in the population aged over 80 years [2]. By the year 2060, given a forecasted European population of around 30% of persons aged over 65 years and 14% aged over 80 years [3], HTN and associated morbidity and mortality will acquire progressively greater epidemiological relevance as the population ages.
The Hypertension in the Very Elderly Trial (HYVET) [4] demonstrated that antihypertensive treatment of even very elderly patients is clinically beneficial. In patients with a mean age of 83 years, cerebrovascular accidents fell by 30%, the overall death rate by 21% and death from cardiovascular causes by 23%. The benefits of treatment become apparent within the first year [4]. Recent US [5] and European [6] clinical practice guidelines for HTN recommend (as a class A recommendation with level I scientific evidence) medicating elderly patients with HTN and systolic blood pressure (SBP) of >160 mmHg, provided the treatment is well tolerated [1]. The recently published Systolic Blood Pressure Intervention Trial (SPRINT) [7] shows that, even for the cohort of non-diabetic patients over 75 years old, a target of SBP <120 mmHg results in both lower major cardiovascular event rates (both fatal and non-fatal) and deaths from any cause. Nonetheless, significantly higher rates of certain adverse effects were observed, including hypotension, syncope, electrolyte abnormalities and acute kidney injury or failure.
Numerous clinical trials to evaluate HTN medication have focused especially on the benefits of controlling blood pressure and preventing cardiovascular disease [4, 8, 9]. However, other crucial geriatric care factors, such as cost effectiveness, tolerability and safety, also need to be taken into account in choosing antihypertensive treatments [1, 10].
Criteria [11–16] have been devised to assist in identifying inappropriate prescriptions in the elderly. Inappropriate prescription, defined as a situation in which pharmacotherapy does not follow accepted medical standards, includes overprescribing, misprescribing and underprescribing [13]. Overprescribing [14, 17], defined as the use of one or more unnecessary drugs, is strongly linked to polypharmacy and adverse drug events, drug interactions, non-adherence, reduced quality of life and increased health expenditure. Misprescribing, defined as the use of drugs without evidence-based medical indications or of drugs lacking cost effectiveness, is also potentially related to adverse effects. Underprescribing is omission or underdosage of (or non-adherence to) a drug with a favourable benefit/risk ratio for the treatment or prevention of a condition or disease. Inappropriate prescription rates of between 25 and 75% in the elderly have been reported in the literature [15]. The application of criteria aimed at reducing potentially inappropriate prescriptions has been shown to reduce falls, delirium episodes, hospital stays, care visits (primary and emergency) and medication costs, although no evidence has been reported regarding quality-of-life or mortality improvements [18].
Numerous studies have been conducted in patients with HTN aged over 65 years [19–22] regarding antihypertensive treatment adherence and antihypertensive drugs associated with cardiovascular conditions [Study on Cognition and Prognosis in the Elderly (SCOPE), Systolic Hypertension in China (SysTChina), the Coope and Warrender study, Systolic Hypertension in the Elderly Program (SHEP)] [1]. However, little data are available for patients aged 75 years and older regarding key geriatric aspects of fragility (delirium, falls, constipation, etc.) or the appropriateness of prescribed antihypertensive drugs. Geriatric syndromes in these often vulnerable and polymedicated patients frequently develop in the context of an adverse reaction to drugs, associated in turn with an increased risk of hospital admission and functional decline [15].
The aim of our study was to analyse antihypertensive drug use and evaluate potentially inappropriate medication in patients aged 75 years and older in the month prior to admission to internal medicine departments.
2 Methods
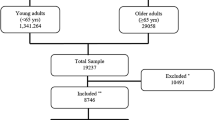
Described below is a sub-study of the Potentially Inappropriate Prescribing in Older Patients in Spain (PIPOPS) study [15] that uses the previously described methodology [15, 23]. The PIPOPS research project was a multicentre prospective observational study that tracked 672 patients aged 75 years and older, hospitalized for an acute event or exacerbation of a chronic condition in the internal medicine departments of seven Spanish hospitals between April 2011 and March 2012 (52 weeks). The objectives of the PIPOPS study were to analyse use and misuse of drugs in the month prior to hospitalization, compare inappropriate prescription assessment tools and explore factors associated with drug misuse. Our sub-study focuses on antihypertensive prescriptions. Excluded from the PIPOPS study were patients admitted on a scheduled basis, patients admitted for under 24 h, patients treated as outpatients by one of the study investigators, patients for whom primary care medical information was not available and patients who did not give their informed consent. The PIPOPS study design was based on two distinct age groups: patients aged 75–84 years and patients aged 85 years and older. From the total of 1563 patients admitted, each hospital included two patients per week (one in each age group) who complied with the inclusion criteria. Patients were randomly selected from hospitalization lists each week on consecutive days [15].
Demographic and clinical data for the included patients were obtained from hospital and primary care electronic medical records and from a structured questionnaire completed in interviews with the patients (or their caregiver, in the case of cognitively impaired patients). Variables recorded were sex and age; reason for admission and whether admission was due to an adverse drug event; functional status (Barthel index [22]) on admission and a month before admission (self-reported or proxy-reported); cognitive status (Reisberg Global Deterioration Scale [24] and Pfeiffer test [25]); detailed chronic medical history (specifically HTN); and Charlson Comorbidity Index scores [15, 26]. Patients were defined as hypertensive if, at baseline, they had a previous HTN diagnosis. HTN was defined and blood pressure was measured according to standard European guidelines for HTN and cardiovascular risk [1, 27]. Information on blood pressure control was obtained by reviewing blood pressure readings noted in hospital or primary care electronic medical records. Pharmacological anamnesis (Appendix 1) consisted of an open question to patients (or their caregiver) about drug use in the month before admission, followed by administration of a structured questionnaire about drug use for common and frequently medicated symptoms and conditions [15]. Data were completed with information obtained from primary care electronic medical records. In the event of information conflicts, the information reported by the patient (or caregiver) was used. Antihypertensive drugs were classified in one of five pharmacological groups as follows: angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs); diuretics; beta-blockers; alpha-blockers; and calcium antagonists.
The study was conducted in accordance with international ethical recommendations and national directives in relation to post-authorization studies and was also approved by the clinical research ethics committees of each participating hospital.
2.1 Measurements
Inappropriate antihypertensive treatment was assessed using the following widely used instruments:
-
Beers criteria [11]: a list of 48 drugs or drug classes to be avoided in the elderly regardless of diagnosis and another list of 20 diseases or conditions and the corresponding medications to be avoided in treating those conditions.
-
Screening Tool of Older Person’s Prescriptions (STOPP) [12]: a list of 65 clinically significant criteria, organized by physiological system, to identify administered drugs that should be avoided.
-
Screening Tool to Alert Doctors to the Right Treatment (START) [12, 28]: a list of 22 evidence-based prescribing indicators for commonly encountered diseases in older people, organized by physiological system.
-
Assessing Care of Vulnerable Elders Version 3 (ACOVE-3) [23]: care quality indicators for 26 key clinical conditions in elderly and vulnerable patients, defined as older adults at high risk of a serious decline in health and functions. Note that, in the PIPOPS study [15], 37 underprescription indicators were analysed for 11 key conditions (the methodology is described elsewhere [23]).
Each patient was evaluated using all four instruments. The corresponding antihypertensive treatment criteria are listed in Appendices 2–5. All the interviewers were consultants or nurses trained in geriatric assessment and in the use of inappropriate prescribing criteria, with full access to any hospital and primary care record information necessary to apply the instruments. Good inter-rater reliability has been reported for the Beers, STOPP and START criteria [21, 28], and similar results were obtained for observers from our seven-hospital study for the STOPP, START and ACOVE-3 criteria [22].
2.2 Statistical Analysis
Quantitative variables were expressed in terms of medians and interquartile ranges (IQRs) with their 95% confidence intervals (CI); categorical variables were expressed as percentages. The chi-square test or Fisher’s exact test were used to compare categorical variables, and the non-parametric Mann–Whitney U test was used to compare quantitative variables. Multiple logistic regression with stepwise selection was used to determine predictor variables for admission due to heart failure. The variables analysed in the multiple logistic regression were sex, age, Charlson index and Barthel index scores, the total number of prescribed antihypertensive drugs and the analysed underprescription criteria. All variables with statistical significance in the bivariate analysis were included in the multivariate analysis. The entry threshold for the multivariate model was p ≤ 0.05. The regression analyses included an examination of collinearity [29] using a variance inflation factor. Statistical significance was determined at the 5% level. The statistical software package SPSS version 22 was used for the analyses.
3 Results
Of the 672 patients included in the PIPOPS study, all 532 patients (79.2%) with HTN were included in this sub-study (median age 85 years, 56.6% women). Distribution in the two age groups was as follows: 60% (n = 319) aged 75–84 years [median 81 (IQR 6) years (95% CI 80–81)] and 40% (n = 213) aged 85 years and older [median 88 (IQR 4) years (95% CI 88–89)]. The characteristics of PIPOPS study patients with and without HTN are summarized in Table 1. Patients with HTN had more comorbidities (p = 0.001), ingested more prescribed drugs (median 11.5 vs. 11; p = 0.03) and had twice the incidence of diabetes, dyslipidaemia, heart failure and chronic kidney disease (p < 0.001). No other statistically significant differences were observed in baseline characteristics for the two age groups. Regarding reasons for admission (Table 2), it is noteworthy that 297 (55.83%) of patients with HTN were admitted for cardiovascular problems.
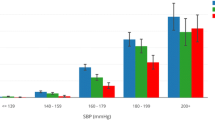
Antihypertensive treatment received by the two age groups is summarized in Table 3. 4.7% of patients with HTN were not receiving antihypertensive treatment (with no differences between the two age groups). Furthermore, 1.6% were not receiving antihypertensive medication despite SBP of >160 mmHg in two consecutive visits, mostly patients in the older age group (3.3 vs. 0.6%; p = 0.02). The number of antihypertensive drugs prescribed per patient was as follows: one drug to 115 patients (21.6%); two drugs to 175 patients (32.9%); three drugs to 141 patients (26.5%); and four or more drugs to 75 patients (14.2%). The main antihypertensive drug families prescribed were diuretics (53.5%), ACEIs (41%), calcium antagonists (32.2%), ARBs (29.7%) and beta-blockers (29.7%). No differences were observed in antihypertensive treatment by age group, except that ACEIs were more frequently prescribed to patients in the older age group (44 vs. 35%; p = 0.04).
A total of 273 patients (51.3%) with HTN met at least one of the potentially inappropriate prescription criteria, summarized in Table 4 (overprescription) and Table 5 (underprescription) by age group. Table 4 shows that 148 patients (27.8%) met at least one overprescription criterion: 109 patients (20.5%) according to STOPP and 85 patients (15.9%) according to Beers. Most frequently overprescribed were calcium antagonists, prescribed to patients with chronic constipation (8%). Table 5 shows that 186 patients (35%) met at least one underprescription criterion: 120 patients (22.6%) according to START and 166 patients (31.2%) according to ACOVE-3. ACEIs and beta-blockers were the most frequently underprescribed drugs (but not to a statistically significant degree). Potentially inappropriate prescription was higher (although not to a statistically significant degree) in patients aged 85 years and older (54.9 vs. 48.9%; p = 0.17): overprescription (31.9 vs. 25.1%; p = 0.08) (Table 4) and underprescription (36.2 vs. 34.2%; p = 0.6) (Table 5).
Of the 672 patients included in the PIPOPS study, 42 admissions (6.2%) were due to an adverse drug effect and, of these, eight (1.1%) were due to the adverse effects of an antihypertensive drug, namely calcium antagonists (n = 2), beta-blockers (n = 3) and diuretics (n = 3), whereas overprescription was a reason for admission for only two patients (receiving calcium antagonists). In our study, underprescription was found to have a far greater impact: of 39 patients admitted for HTN, one patient (2.6%) was not receiving any antihypertensive treatment; of 23 patients admitted for ischaemic heart disease, two (8.7%) and five patients (2.2%) were not receiving ACEIs or beta-blockers, respectively; and of 149 patients admitted for congestive heart failure, 43 (28.8%) and 44 patients (29.5%) were not receiving ACEIs or beta-blockers, respectively. Admission due to congestive heart failure was associated with ACEI and beta-blocker underprescription in both the bivariate (p < 0.001) and multivariate analyses (beta-blockers odds ratio (OR) 0.527; 95% CI 0.39–0.71 vs. ACEIs OR 0.50; 95% CI 0.36–0.70; p < 0.001) (Table 6).
4 Discussion
More than half of the elderly patients in our study had been inappropriately prescribed antihypertensive drugs. Underprescription (35%) was more frequent than overprescription (27.8%). Particularly noteworthy was the association between beta-blocker undermedication and admissions for congestive heart failure.
Elderly patients with HTN in our study were prescribed a mean of 12.6 drugs, a significantly higher number than prescribed to patients without HTN, although similar to previous values reported for patients with diabetes [30]. Most patients with HTN were receiving antihypertensive treatment (95.3%), corroborating results reported for recent population studies in Spain (>90.5% of patients aged 70 years and older) [31]. Only 1.6% of elderly patients with SBP of >160 mmHg recorded in two consecutive visits were not receiving antihypertensive treatment. In contrast, 6.6% of patients with HTN were receiving vasodilator treatment despite having persistent postural hypotension. Diuretics were the most frequently prescribed drugs (corroborating a recent US study [32]), followed by ACEIs and then (with similar percentages) by calcium antagonists, beta-blockers and ARBs. The relatively greater use of ACEIs in comparison with other series is probably explained by greater comorbidity rates in our patients and the lower cost of ACEIs compared to ARBs in Spain.
At least one potentially inappropriate medication prescription criterion for antihypertensive treatment was met in more than half of our patients with HTN. Overprescription was detected in nearly a third (27.8%) of those patients, with the STOPP criteria more sensitive than the Beers criteria as has been reported elsewhere for the full instruments [33]. Nevertheless, the overall impact on hospital admissions of adverse drug effects due to overprescription was very low. The drugs most overprescribed were calcium antagonists and diuretics. Underprescription was, as well as more frequent (35%), also more clinically significant, as it affected more than a third of patients admitted for cardiovascular reasons. ACOVE-3 was more sensitive in detecting underprescription than START, corroborating the PIPOPS findings for the full instruments [15]. The main underprescribed drugs were ACEIs, ARBs and beta-blockers. No significant differences were observed between the two age groups, although the tendency to overprescribe was greater among patients aged 85 years and older.
Although more than half of our patients were treated with diuretics, the association with potentially inappropriate prescription was minimal, as only 4 and 1% of patients received loop diuretics as monotherapy for HTN and thiazide diuretics as treatment for gout, respectively. Note, however, that our analysis did not consider the appropriateness of diuretics in relation to electrolyte disturbances, impaired renal function or urinary incontinence, all of which are taken into account in newer versions of the STOPP [34] and Beers [35] instruments published after our analysis was conducted.
Calcium antagonists, prescribed to around a third of patients with HTN, were the drugs most likely to be overprescribed, especially for chronic constipation (8% of patients with HTN). In accordance with guidelines [1], calcium antagonists and diuretics are recommended antihypertensive treatments for the elderly. In the latest versions of the STOPP [36] and Beers [37] criteria, however, less importance is attached to this criterion, which continues to feature only in STOPP in relation to verapamil. Fortunately, other more serious criteria were infrequently present; for instance, patients with New York Heart Association (NYHA) functional class III or IV heart failure being prescribed short-acting nifedipine, verapamil plus beta-blocker or diltiazem/verapamil.
Beta-blockers, prescribed to a third of our patients with HTN, were rarely associated with overprescription but very much so with underprescription; significant proportions of elderly patients with ischaemic heart disease (10.1%) and low ejection fractions (8.3%) did not receive these drugs. While these percentages are lower than reported in other cardiovascular disease series [38], underprescription of beta-blockers for these recognized indications was associated with hospitalization in our study. Indeed, the fact that underprescription of beta-blockers was a risk factor for congestive heart failure admission is a crucial factor from the clinical practice perspective.
A prominent role in underprescribing was played by ACEIs and ARBs, prescribed to 41 and 30% of the patients in our study, respectively. Some 20% of elderly patients with HTN were not receiving these treatments (with no clear justification), despite having comorbidities that advised their use (congestive heart failure, left ventricular hypertrophy, ischaemic heart disease, chronic renal failure, cerebrovascular disease and diabetes mellitus with proteinuria). The impact of underprescribing ACEIs was particularly evident in admissions for congestive heart failure.
Our study has limitations. As a post hoc study, it was initially designed to assess inappropriate prescription in hospitalized patients and so did not include detailed blood pressure control data. However, detailed records on drugs, comorbidities and especially HTN enabled us to conduct this sub-study without departing from the objectives set in the PIPOPS study. Furthermore, because of the multimorbidity of the included patients, it was challenging to assign specific drugs to specific disease states. For example, a significant number of antihypertensive treatments could also be prescribed for other indications, e.g. heart failure, diabetic nephropathy, secondary prevention, etc. Nevertheless, based on the fact that, in clinical trials, no antihypertensive drug has proven to be consistently superior in terms of all important outcomes, guideline recommendations on antihypertensive selection were based on comorbidities and individual patient characteristics [33]. Our study did not analyse whether the antihypertensive treatment was optimal for each elderly patient; this was because the objective was to analyse potentially inappropriate antihypertensive treatments according to standardized geriatric criteria regarding over- and underprescription. Moreover, our results may not be applicable to patients from other regions or countries, since our study population is representative of patients aged 75 years and older admitted to the internal medicine departments of seven Spanish hospitals. Finally, in the 4 years since data collection, new HTN management guidelines and new Beers and STOPP/START criteria have been released, so it would be advisable to reconsider our results as reported above against the most recently published versions of these instruments.
A strength of the study is the detailed information yielded on the appropriateness of antihypertensive treatment in relation to cardiovascular events and adverse drug effects in elderly patients in a routine clinical practice context [33]. Another strength is our analysis of the potential impact of drugs on reasons for admission. Although previous studies have analysed potentially inappropriate prescription to elderly populations, whether community-dwelling [39], hospitalized [40] or with cardiovascular problems [34], as far as we are aware ours is the first detailed analysis of elderly patients with HTN.
5 Conclusions
We detected inappropriate antihypertensive treatment in more than half of the elderly patients with HTN in our study; more specifically, nearly one third of our subjects were overmedicated and an even higher proportion was undermedicated. Our results highlight the importance of routine checks not only for blood pressure and cardiovascular risk in the elderly, but also of the risk of triggering, via antihypertensive treatment, postural hypotension or a worsening of constipation. The underprescription of ACEIs and beta-blockers needs to be avoided in the antihypertensive management of elderly patients, but most especially in patients with congestive heart failure, as this very prevalent condition in the elderly has a great impact on quality of life and hospital admissions.
References
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. Hipertensión. Hipertens riesgo vasc. 2013;30:1–94. http://www.seh-lelha.org/pdf/Guia2013.pdf.
Gómez-Huelgas R, Martínez-Sellés M, Formiga F, Alemán Sánchez JJ, Camafort M, Galve E, et al. Management of vascular risk factors in patients older than 80. Med clínica. Elsevier; 2014 [cited 2015 Dec 17];143:134.e1–11. http://www.elsevier.es/es-revista-medicina-clinica-2-articulo-tratamiento-los-factores-riesgo-vascular-90334864.
Kaiser EA, Lotze U, Schäfer HH. Increasing complexity: which drug class to choose for treatment of hypertension in the elderly? Clin Interv Aging. 2014 [cited 2016 Jan 10];9:459–75. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3969251&tool=pmcentrez&rendertype=abstract.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008 [cited 2016 Jan 10];358:1887–98. http://www.ncbi.nlm.nih.gov/pubmed/18378519.
Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly. J Am Soc Hypertens. 2011 [cited 2016 Jan 6];5:259–352. http://www.ncbi.nlm.nih.gov/pubmed/21771565.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by re. Eur Heart J. 2012 [cited 2014 Jul 10];33:1635–701. http://eurheartj.oxfordjournals.org/content/33/13/1635.
Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015 [cited 2015 Nov 10];373:2103–16. http://www.ncbi.nlm.nih.gov/pubmed/26551272.
Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010 [cited 2015 Dec 17];56:196–202. http://hyper.ahajournals.org/content/56/2/196.short.
O’rourke MF, Namasivayam M, Adji A. Treatment of hypertension in patients 80 years of age or older. Minerva Med. 2009 [cited 2016 Jan 10];100:25–38. http://www.ncbi.nlm.nih.gov/pubmed/19277002.
De Villar JHP, Miranda MG, Perez-Monteoliva NR, Gregori JA, Musso CG, Núñez JM. La hipertensión arterial en los pacientes octogenarios. Reflexiones sobre los objetivos, el tratamiento y sus consecuencias. Nefro Plus. 2011;4:18–28. http://www.revistanefrologia.com/es-publicacion-nefroplus-imprimir-articulo-la-hipertension-arterial-los-pacientes-octogenarios-reflexiones-sobre-los-objetivos-X1888970011001133.
Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. American Medical Association; 2003 [cited 2015 Aug 21];163:2716–24. http://archinte.jamanetwork.com/article.aspx?articleid=757456.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008 [cited 2016 Jan 10];46:72–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18218287.
Barry PJ, Gallagher P, Ryan C, O’mahony D. START (Screening Tool to Alert doctors to the Right Treatment)–an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing. 2007 [cited 2016 Jan 10];36:632–8. http://ageing.oxfordjournals.org/cgi/content/long/36/6/632.
Welsh TJ, Gladman JR, Gordon AL. The treatment of hypertension in people with dementia: a systematic review of observational studies. BMC Geriatr. 2014 [cited 2016 Jan 10];14:19. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3923425&tool=pmcentrez&rendertype=abstract.
San-José A, Agustí A, Vidal X, Formiga F, López-Soto A, Fernández-Moyano A, et al. Inappropriate prescribing to older patients admitted to hospital: a comparison of different tools of misprescribing and underprescribing. Eur J Intern Med. 2014 [cited 2016 Jan 10];25:710–6. http://www.ncbi.nlm.nih.gov/pubmed/25179678.
Higashi T. The quality of pharmacologic care for vulnerable older patients. Ann Intern Med. American College of Physicians; 2004 [cited 2016 Jan 10];140:714. http://annals.org/article.aspx?articleid=717420.
Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. [cited 2015 Aug 21];163:2716–24. http://www.ncbi.nlm.nih.gov/pubmed/14662625.
Hill-Taylor B, Walsh KA, Stewart S, Hayden J, Byrne S, Sketris IS. Effectiveness of the STOPP/START (Screening Tool of Older Persons’ potentially inappropriate Prescriptions/Screening Tool to Alert doctors to the Right Treatment) criteria: systematic review and meta-analysis of randomized controlled studies. J Clin Pharm Ther. 2016;41:158–69.
Levi Marpillat N, Macquin-Mavier I, Tropeano A-I, Bachoud-Levi A-C, Maison P. Antihypertensive classes, cognitive decline and incidence of dementia. J Hypertens. 2013 [cited 2016 Jan 10];31:1073–82. http://www.ncbi.nlm.nih.gov/pubmed/23552124.
Schubert I, Küpper-Nybelen J, Ihle P, Thürmann P. Prescribing potentially inappropriate medication (PIM) in Germany’s elderly as indicated by the PRISCUS list. An analysis based on regional claims data. Pharmacoepidemiol Drug Saf. 2013 [cited 2015 Dec 30];22:719–27. http://www.ncbi.nlm.nih.gov/pubmed/23585247.
Jones SA, Bhandari S. The prevalence of potentially inappropriate medication prescribing in elderly patients with chronic kidney disease. Postgrad Med J. 2013 [cited 2016 Jan 10];89:247–50. http://pmj.bmj.com/content/89/1051/247.long.
Clínica G, Galega S, Interna DM, De E, Medicina S De, Complexo I, et al. Escalas de valoración funcional en el anciano. Galicia Clin. 2011;72:11–6. http://www.galiciaclinica.info/PDF/11/225.pdf.
San-José A, Agustí A, Vidal X, Barbé J, Torres OH, Ramírez-Duque N, et al. An inter-rater reliability study of the prescribing indicated medications quality indicators of the Assessing Care Of Vulnerable Elders (ACOVE) 3 criteria as a potentially inappropriate prescribing tool. Arch Gerontol Geriatr. [cited 2016 Jan 10];58:460–4. http://www.ncbi.nlm.nih.gov/pubmed/24438879.
Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–9.
Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975 [cited 2015 May 20];23:433–41. http://www.ncbi.nlm.nih.gov/pubmed/1159263.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987 [cited 2014 Jul 10];40:373–83. http://www.ncbi.nlm.nih.gov/pubmed/3558716.
Coca A, Aranda P, Bertomeu V, Bonet A, Esmatjes E, Guillén F, et al. Estrategias para un control eficaz de la hipertensión arterial en España. Documento de consenso. Rev Clínica Española. 2006;206:510–4.
Delgado Silveira E, Muñoz García M, Montero Errasquin B, Sánchez Castellano C, Gallagher PF, Cruz-Jentoft AJ. [Inappropriate prescription in older patients: the STOPP/START criteria]. Rev Esp Geriatr Gerontol. 2009 [cited 2015 Nov 11];44:273–9. http://www.sciencedirect.com/science/article/pii/S0211139X09001310.
Kleinbaum DG, Kupper LL, Muller KE. Applied regression analysis and other multivariable methods. Boston: PWS-Kent Pub. Co; 1988.
Formiga F, Vidal X, Agustí A, Chivite D, Rosón B, Barbé J, et al. Inappropriate prescribing in elderly people with diabetes admitted to hospital. Diabet Med. 2015 [cited 2015 Dec 4]. http://www.ncbi.nlm.nih.gov/pubmed/26333026.
Banegas JR, Navarro-Vidal B, Ruilope LM, de la Cruz JJ, Lopez-Garcia E, Rodriguez-Artalejo F, et al. Trends in hypertension control among the older population of spain from 2000 to 2001 to 2008 to 2010: role of frequency and intensity of drug treatment. Circ Cardiovasc Qual Outcomes. 2015 [cited 2016 Jan 10];8:67–76. http://circoutcomes.ahajournals.org/content/8/1/67.long.
Gu A, Yue Y, Argulian E. Age differences in treatment and control of hypertension in US physician offices, 2003–2010: a serial cross-sectional study. Am J Med. 2016 [cited 2016 Jan 10];129:50–58.e4. http://www.ncbi.nlm.nih.gov/pubmed/26299315.
Butt DA, Harvey PJ. Benefits and risks of antihypertensive medications in the elderly. J Intern Med. 2015 [cited 2015 Nov 26];278:599–626. http://onlinelibrary.wiley.com/doi/10.1111/joim.12446/full.
Coupet M, Renvoize D, Rousseau C, Fresil M, Lozachmeur P, Somme D. [Validity of cardiovascular prescriptions to the guidelines in the elderly according to the STOPP and START method]. Gériatrie Psychol. Neuropsychiatr du Vieil. 2013 [cited 2016 Jan 10];11:237–43. http://www.ncbi.nlm.nih.gov/pubmed/24026128.
Campanelli CM, Fick DM, Semla T, Beizer J. Potentially inappropriate medication use in older adults: the American Geriatrics Society 2012 Beers Criteria. J Am Geriatr Soc. 2012;60:616–31.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2014 [cited 2014 Oct 17];44:213–8. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4339726&tool=pmcentrez&rendertype=abstract.
American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015 [cited 2015 Oct 9];63:n/a–n/a. http://www.ncbi.nlm.nih.gov/pubmed/26446832.
Moubarak G, Ernande L, Godin M, Cazeau S, Vicaut E, Hanon O, et al. Impact of comorbidity on medication use in elderly patients with cardiovascular diseases: the OCTOCARDIO study. Eur J Prev Cardiol. 2012 [cited 2016 Jan 10];20:524–30. http://cpr.sagepub.com/content/20/4/524.short.
Galvin R, Moriarty F, Cousins G, Cahir C, Motterlini N, Bradley M, et al. Prevalence of potentially inappropriate prescribing and prescribing omissions in older Irish adults: findings from The Irish LongituDinal Study on Ageing study (TILDA). Eur J Clin Pharmacol. 2014 [cited 2016 Jan 10];70:599–606. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3978378&tool=pmcentrez&rendertype=abstract.
Gallagher P, Lang PO, Cherubini A, Topinková E, Cruz-Jentoft A, Montero Errasquín B, et al. Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol. 2011 [cited 2016 Jan 10];67:1175–88. http://www.ncbi.nlm.nih.gov/pubmed/21584788.
Assessing Care of Vulnerable Elders-3 Quality Indicators. J Am Geriatr Soc. 2007;55(Suppl 2):S464–87. doi:10.1111/j.1532-5415.2007.01329.x.
Acknowledgements
We would like to thank the Spanish Ministry of Health, Social Affairs and Equality for its financial support and Ailish Maher for revising the English in this manuscript.
Contributors:
PIPOPS Investigators Coordinating group: Antonio San-José (principal investigator), Antonia Agustí, Xavier Vidal, Cristina Aguilera, Elena Balların, Eulalia Pérez. Hospital Universitari Vall d’Hebron (Barcelona): José Barbe, Carmen Pérez Bocanegra, Ainhoa Toscano, Carme Pal, Teresa Teixidor. Hospital San Juan de Dios de Aljarafe (Seville): Antonio Fernández-Moyano, Mercedes Gómez Hernández, Rafael de la Rosa Morales, María Nicolas Benticuaga Martínez. Hospital Clínic (Barcelona): Alfonso López-Soto, Xavier Bosch, María José Palau, Joana Rovira, Margarita Navarro. Hospital Universitari de Bellvitge (Hospitalet de Llobregat, Barcelona): Francesc Formiga, David Chivite, Beatriz Roson, Antonio Vallano, Carme Cabot. Hospital Juan Ramón Jiménez (Huelva): Juana García, Isabel Ballesteros. Hospital Santa Creu i Sant Pau (Barcelona): Olga H. Torres, Domingo Ruiz, Miquel Turbau, Paola Ponte Márquez, Gabriel Ortiz. Hospital Universitario Virgen Del Rocío (Sevilla): Nieves Ramírez-Duque, Paula-Carlota Rivas Cobas, Paloma Gil.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The project was financed by Grant EC10-077 obtained in a request for aid for the promotion of independent clinical research (SAS/2370/2010 Order of 27 September from the Spanish Ministry of Health, Social Affairs and Equality).
Conflict of interest
P. Ponte Márquez, O. Torres, A. San-José, X. Vidal, A. Agustí, F. Formiga, A. López-Soto, N. Ramirez-Duque, A. Fernández-Moyano and J. García-Moreno, J. A Arroyo and D Ruiz declare that they have no conflict of interest that might be relevant to the contents of this manuscript.
Appendices
Appendix 1: Pharmacological Anamnesis
See Fig. 1 for the questionnaire used for pharmacological anamnesis.
Appendix 2: Beers Criteria for Potentially Inappropriate Medication Use in Older Adults
For the Beers criteria for potentially inappropriate medication use in older adults, see Tables 7 and 8.
Appendix 3: Screening Tool of Older People’s Potentially Inappropriate Prescriptions (STOPP)
The following drug prescriptions are potentially inappropriate in persons aged >65 years of age (see reference [12] for individual references below):
A. Cardiovascular system
Item 3. Loop diuretic as first-line monotherapy for hypertension (safer, more effective alternatives available) [Williams et al. 2004]
Item 4. Thiazide diuretic with a history of gout (may exacerbate gout) [Dougall and McLay 1996].
Item 5. Non-cardioselective beta-blocker with chronic obstructive pulmonary disease (risk of increased bronchospasm) [van der Woulde et al. 2005, Salpeter et al. 2005]
Item 6. Beta-blocker in combination with verapamil (risk of symptomatic heart block) [BNF 2006]
Item 7. Use of diltiazem or verapamil with NYHA class III or IV heart failure (may worsen heart failure) [BNF 2006]
Item 8. Calcium channel blockers with chronic constipation (may exacerbate constipation) [Dougall and McLay 1996]
G. Endocrine system
Item 2. Beta-blockers in those with diabetes mellitus and frequent hypoglycaemia
H. Drugs that adversely affect fallers
Item 4. Vasodilator drugs with persistent postural hypotension, i.e. recurrent >20 mmHg drop in systolic blood pressure (risk of syncope, falls) [Leipzig et al. 1999]
Appendix 4 Screening Tool to Alert Doctors to Right Treatments (START)
These medications should be considered as appropriate and indicated for people >65 years of age with the following conditions, where no contraindication to prescription exists (see reference [12] for individual references below):
A. Cardiovascular system
Item 4. Antihypertensive therapy where systolic blood pressure consistently >160 mmHg [Williams et al. 2004, Papademetriou et al. 2004, Skoog et al. 2004, Thenkwalder et al. 2005]
Item 6. ACE inhibitor with chronic heart failure [Hunt et al. 2005]
Item 7. ACE inhibitor following acute myocardial infarction [ACE Inhibitor Myocardial infarction Collaborative Group 1998, Antman et al. 2004]
Item 8. Beta-blocker with chronic stable angina [Gibbons et al. 2003]
F. Endocrine system
Item 2. ACE inhibitor or ARB in diabetes with nephropathy, i.e. overt urinalysis proteinuria or microalbuminuria (>30 mg/24 h) ± serum biochemical renal impairment* [Sigal et al. 2005]
*Serum creatinine >150 µmol/l, or estimated glomerular filtration rate <50 ml/min [BNF 2006].
Appendix 5: Assessing Care of Vulnerable Elders-3 (ACOVE-3) Quality Indicators [41]
Abbreviations ACE angiotensin-converting enzyme, ARB angiotensin receptor blocker, BP blood pressure, HF heart failure, HTN hypertension/elevated BP, IHD ischaemic heart disease, LVEF left ventricular ejection fraction, MI myocardial infarction, NSTEMI non-ST elevation myocardial infarction, STEMI ST-segment elevation myocardial infarction, VE vulnerable elder.
5.1 Hypertension
5.1.1 Intervening for Persistent HTN
Item 9. IF a VE with HTN has persistent (on two consecutive visits) systolic BP above goal*, THEN an intervention (e.g. pharmacological, lifestyle, compliance) should occur, or there should be documentation of reversible cause or other justification for the elevation.
*Goal systolic BP (mmHg): diabetes mellitus or chronic renal disease 130 mmHg; home ambulatory monitoring 135 mmHg; all other patients 140 mmHg of other specified goal.
5.1.2 Beta-Blocker for HTN and IHD
Item 13. IF a VE with HTN has IHD, THEN treatment with a beta-blocker should be recommended or there should be documentation of why it should not be provided.
5.1.3 ACE Inhibitor for Comorbid Vascular Disease
Item 14. IF a VE with HTN has a history of HF, left ventricular hypertrophy, IHD, chronic kidney disease or cardiovascular accident, THEN he or she should be treated with an ACE inhibitor or ARB or there should be documentation of why it should not be provided.
5.2 Heart Failure
5.2.1 ACE Inhibitor
Item 1. IF a VE has LVEF less than 40%, THEN he or she should receive an ACE inhibitor (or ARB if ACE inhibitor intolerant).
5.2.2 Selective Beta-Blocker
Item 7. IF a VE has HF and LVEF less than 40%, THEN he or she should be treated with a beta-blocker known to prolong survival (carvedilol, metoprolol, or bisoprolol).
5.3 Ischaemic Heart Disease
5.3.1 Early ACE Inhibitor Therapy for MI and HF
Item 5. IF a VE has an MI (STEMI or NSTEMI) complicated by HF or LVEF less than 40%, THEN he or she should be given an ACE inhibitor or ARB within 36 h of presentation and advised to continue this treatment for 4 weeks or longer.
5.3.2 Beta-Blocker Therapy
Item 14. IF a VE has had an MI (STEMI or NSTEMI), THEN he or she should be offered a beta-blocker and advised to continue treatment for 2 years or longer after infarction.
5.3.3 ACE Inhibitor Therapy
Item 15. IF a VE has IHD, THEN he or she should be offered ACE inhibitor or ARB therapy and advised to continue the treatment indefinitely.
5.4 Diabetes Mellitus
5.4.1 Proteinuria
Item 4. IF a VE with diabetes mellitus has proteinuria, THEN an ACE inhibitor or ARB should be prescribed.
Rights and permissions
About this article
Cite this article
Márquez, P.H.P., Torres, O.H., San-José, A. et al. Potentially Inappropriate Antihypertensive Prescriptions to Elderly Patients: Results of a Prospective, Observational Study. Drugs Aging 34, 453–466 (2017). https://doi.org/10.1007/s40266-017-0452-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0452-z