Abstract
Introduction
Dopaminergic agonists (DAs) are widely used to treat motor symptoms in Parkinson’s disease (PD). The differential effect of DAs on neuropsychiatric symptoms of PD has not been accurately studied.
Materials and methods
We performed a prospective cross-sectional study of 515 non-demented PD patients receiving treatment with pramipexole [n = 250, monotherapy or with levodopa (l-dopa)], ropinirole (n = 150, monotherapy or with l-dopa), or l-dopa (n = 115, monotherapy); all formulations were immediate release. Neuropsychiatric disturbances were assessed through the Neuropsychiatric Inventory (NPI). Groups were matched in terms of age, education, sex, disease severity (Hoehn and Yahr), disease duration, executive function, total l-dopa daily equivalent dose, and concomitant psychotropic medications (antidepressants, anxiolytics and antipsychotic agents).
Results
Patients on pramipexole showed significantly lower total NPI scores than patients on ropinirole (17.2 ± 11 vs. 20.9 ± 13, p = 0.015). Regarding the spectrum of neuropsychiatric symptoms, pramipexole was associated with significantly lower apathy scores than the l-dopa group (1.01 ± 1.7 vs. 1.87 ± 2.93, p = 0.02). The frequency of patients with clinically meaningful symptoms of apathy (NPI apathy scores ≥4) was significantly lower in the pramipexole group (11.2 %) than in the ropinirole (20.3 %) and l-dopa (23.8 %) groups (χ 2 12.49, p = 0.002). No other significant differences were found in NPI subscores between groups.
Conclusions
This is the first head-to-head comparative study of the effect of DAs on neuropsychiatric disturbances in PD that has controlled the sample for the most important confounding factors. In comparable groups of patients, the use of pramipexole seems to be associated with a lower frequency and severity of apathetic symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neuropsychiatric symptoms are frequent in Parkinson’s disease. Using the Neuropsychiatric Inventory (NPI), we compared the neuropsychiatric profile of 515 non-demented patients treated with different dopaminergic agonists or levodopa (l-dopa) in monotherapy matched for l-dopa daily equivalent dose, and we found differences only in apathy score. |
Patients on pramipexole showed significantly lower total apathy scores. Moreover, clinically meaningful symptoms of apathy were significantly lower in the pramipexole group (11.2 %) than in the ropinirole (20.3 %) and l-dopa (23.8 %) groups (p = 0.002). |
1 Introduction
Dopaminergic agonists (DAs) were introduced as alternative dopaminergic drugs capable of improving motor symptoms with a lower risk of developing motor fluctuations and dyskinesias [1]. Beyond their clear effect on parkinsonian motor symptoms, less evidence is available about the effects that DAs can exert over neuropsychiatric symptoms.
Neuropsychiatric disturbances are highly disabling symptoms currently recognized as integral to Parkinson’s disease (PD) phenomenology. While some of these symptoms have a clear relationship with the use of DAs (i.e., psychosis [2], impulse control disorders [3]), the effect of DAs on affective symptoms (depression, anxiety, and apathy) has not been well established.
In observational and open-label studies in which pramipexole has been used as add-on therapy to levodopa (l-dopa), significant improvements have consistently been shown in depressive scales [4–6] and associated anhedonia [12]. In addition, in a double-blind, placebo-controlled study, pramipexole improved depressive symptoms through a direct antidepressant effect, independent of motor symptom alleviation [7]. In a comparative study of pramipexole versus sertraline, both drugs achieved significant improvements in depressive symptoms, but the proportion of patients with remission from depression was significantly higher in the pramipexole group [8, 9]. Two studies have examined the antidepressant properties of ropinirole, showing improvement in depression scores and functional scales in PD patients with motor complications [9, 10]. Pergolide, however, in a head-to-head comparative study with pramipexole, showed inconsistent results in several depressive scales [5]. In the randomized evaluation of the 24 hours coverage: efficace of rotigotine (RECOVER) study, onset of treatment with rotigotine significantly improved Beck Depression Inventory scores, but no analysis indicated whether this change could be explained by parallel improvement in motor function [11].
Due to the lack of use of specific scales, the effects of DAs on apathy (defined by Marin as a lack of motivation [13]) are still inconclusive. Motivational items in the unified Parkinson’s disease rating scale-1 (UPDRS-1) and the Non-Motor Symptoms Scale clearly improved with the use of pramipexole [4] and rotigotine [14]. And recently, piribedil, a non-ergoline D2 and D3 receptor selective dopamine agonist, showed significant improvements on Apathy Inventory scores in patients who developed apathy after subthalamic nucleus deep brain stimulation [15]. Nevertheless, focused studies are still needed to clarify and disentangle the antidepressant and motivational effects of DAs on representative samples of PD.
In the present study, we aimed to compare the differential effects that pramipexole, ropinirole, and levodopa in monotherapy may exert on neuropsychiatric symptoms in PD, as assessed by the Neuropsychiatric Inventory (NPI), in a large and representative sample of patients matched for the most important variables that may influence the presence and severity of neuropsychiatric disturbances, such as age, sex, education, disease severity, disease duration, executive functions, total levodopa equivalent dose, and concomitant psychotropic medications (antidepressants, anxiolytics, and antipsychotic agents).
2 Materials and Methods
2.1 Subjects
A sample of 515 outpatients was prospectively recruited from January to December 2007, from 55 centers in Spain with hospital-based or hospital-associated neurologists experienced in movement disorders [17]. This is a sample that included non-demented patients at different stages of the disease, with well-controlled motor symptoms after the introduction of appropriate dopaminergic drugs according to daily clinical practice and clinical guidelines. The TRAPECIO study was designed to evaluate the prevalence of neuropsychiatric symptoms in non-demented patients [19]. Eligibility criteria were as follows: clinical diagnosis of idiopathic PD based on standard criteria [16]; at least one follow-up visit by a neurologist experienced in movement disorders; absence of global cognitive decline accomplishing criteria for dementia associated with PD according to diagnostic and statistical manual of mental disorders (DSM-IV) [18]; and being on stable medication the 4 weeks prior to inclusion.
Dementia was evaluated using the semi-structured interview of the Clinical Dementia Rating Scale (CDR). In order to rule out dementia properly, all raters in the study were trained in the administration of the CDR and DSM-IV criteria for dementia in PD [18], and those individuals who accomplished criteria for dementia were ruled out.
Patients on treatment with a DA or levodopa in monotherapy were carefully matched for variables that could influence the presence and severity of neuropsychiatric disturbances. Patient groups were matched for age, sex, education, disease severity, disease duration, executive function, total l-dopa equivalent daily dose (LEDD), DA-LEDD, and concomitant psychotropic medications [patients were allowed to be on psychotropic medications (antidepressants, anxiolytics, and antipsychotic agents) if they were controlled in terms of overall clinical management in the 4 weeks before inclusion in the study]. Disease severity was assessed using the Hoehn and Yahr scale [20]. Current medications and doses were calculated for l-dopa daily dose, DA daily equivalent dose, and total LEDD [21]. Phonemic, semantic and alternating verbal fluencies were used to assess executive function. Patients on treatment with pramipexole or ropinirole were using the DAs either as monotherapy or in combination with l-dopa, and there were no patients on treatment with both DAs simultaneously. When the initial sample was recruited in Spain, rotigotine had been on the market for only 18 months, and only a small minority of recruited patients was on this drug. These patients were therefore excluded in the present study.
Informed consent to participate in the study was obtained from all participants, according to the Declaration of Helsinki. The study was approved by the local ethics committee.
2.2 Neuropsychiatric Assessment
The 10-item Spanish version of the NPI [22] was used to assess the frequency and severity of a wide range of neuropsychiatric symptoms, including delusions, hallucinations, dysphoria, anxiety, agitation, euphoria, disinhibition, irritability, apathy, and aberrant motor behavior. The NPI is a validated informant-rated scale that assesses the listed behavioral disturbances. Domains are rated on the basis of frequency and severity, with 12 being the maximum score per domain. A specific domain is considered clinically relevant when frequency × severity results in a score ≥4. The NPI has been extensively used in PD and has been shown to be valid to rate the frequency and severity of neuropsychiatric symptoms in PD patients with and without dementia [23–25].
Neuropsychiatric and cognitive assessment was performed by a rater with expertise in cognition and movement disorders specifically trained to achieve this goal. The NPI was performed with the patient and caregiver (defined as a person that lives with the patient or has contact with the patient at least three times per week).
2.3 Statistical Analysis
Data are expressed as mean ± standard deviation (SD) for the continuous variables, as percentages for the categorical variables, and as mean and range for the ordinal variables. Clinical and socio-demographic characteristics of the three groups were compared with one-way ANOVA (analysis of variance) for continuous variables with Tukey post hoc analysis and Chi square (χ 2) test for categorical variables. The matching procedure performed, so as to match patients in the three groups for confounding variables on the NPI, was based on the generation of random samples of patients, choosing ‘random sample of cases’ in the SPSS program, and entering a seed number that was automatically chosen by the same program (SPSS). Statistical significance was set at p < 0.05. Data analysis was performed with SPSS v20.
3 Results
A sample of 515 PD carefully matched patients, with ages ranging from 40 to 80 years, was included in the study (Table 1). Patients were classified as belonging to the pramipexole group (n = 250), ropinirole group (n = 150), or levodopa monotherapy group (n = 115). Patients in the pramipexole group received a mean daily dose of 1.59 ± 0.7 mg/day, and those on ropinirole were taking 8.17 ± 5.3 mg/day.
Table 2 summarizes NPI total scores and item subscores for the whole sample and medication group. Up to 89.3 % exhibited at least one neuropsychiatric symptom. The total composite NPI score for the whole sample was 18.7 ± 12.7. Depression and anxiety were the most common symptoms, with a frequency of 71.5 % for each symptom. Irritability (51.5 %) and apathy (49.1 %) were also very common, while agitation (24.3 %), hallucinations (18.4 %), aberrant motor behavior (15.3 %), euphoria (15 %), and disinhibition (11.1 %) were less frequent. When frequencies were calculated by means of clinically meaningful symptoms (score ≥4), depression (31.9 %) and anxiety (31.8 %) also appeared as the most frequent clinically relevant symptoms, followed by apathy (15.5 %), irritability (13.8 %), hallucinations (6.3 %), agitation (5.6 %), aberrant motor behavior (4.5 %), euphoria (2.8 %), and disinhibition (2.5 %).
3.1 Comparison of Neuropsychiatric Symptoms Between Medication Groups
One-way ANOVA comparison between medication groups showed significant differences for the NPI total score (F = 3.972; p = 0.019) and the apathy NPI subscore (F = 6.46; p = 0.002). No other NPI subscores differed between groups. Tukey post hoc analysis showed NPI total scores to be significantly lower in the pramipexole versus ropinirole group (17.24 ± 11 vs. 20.89 ± 13; p = 0.015), but they did not differ between pramipexole and l-dopa (p = 0.41), or between ropinirole and l-dopa (p = 0.46).
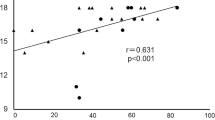
Tukey post hoc analysis of the NPI apathy subscore showed scores in the pramipexole group were significantly lower than in the l-dopa group (1.01 ± 1.7 vs. 1.87 ± 2.93; p = 0.02), and lower scores in the pramipexole group almost reached significance when compared with ropinirole (1.01 ± 1.7 vs. 1.54 ± 2.3; p = 0.06). Apathy scores did not differ between ropinirole and l-dopa groups (p = 0.45). When the frequency of patients with clinically meaningful symptoms of apathy (NPI apathy scores ≥4) was considered, differences in the apathy subscore could be better distinguished between the three groups. Patients in the pramipexole group showed a significantly lower frequency of clinically meaningful apathy (11.2 %) than patients in the ropinirole (20.3 %) and levodopa (23.8 %) groups (χ 2 12.49, p = 0.002) (Fig. 1). Moreover, patients on treatment with pramipexole had an odds ratio (OR) of 2.76 [95 % confidence interval (CI) 1.52–5.01; p = 0.001] for being less apathetic than the group treated with levodopa in monotherapy, and an OR of 2.06 (95 % CI 1.15–3.69; p = 0.015) compared with the ropinirole group. No differences in OR were seen comparing ropinirole and levodopa in monotherapy. When we analyzed the subgroup of subjects with clinically meaningful apathy (n = 22) without clinical meaningful symptoms of depression (apathy without depression) we found that patients in the pramipexole group presented a significantly lower frequency of clinically meaningful apathy (3.4 %) than patients in the ropinirole (8.5 %) and levodopa (9.9 %) groups (χ 2 5.1; p = 0.03).
No other significant differences were found in NPI subscores between medication groups. Specifically, NPI subscores for depression (pramipexole = 2.41 ± 2.7; ropinirole = 2.69 ± 2.7; l-dopa = 2.37 ± 2.8; p = 0.48), anxiety (pramipexole = 2.18 ± 2.5; ropinirole = 2.4 ± 2.4; l-dopa = 2.45 ± 2.7; p = 0.41), or psychosis (pramipexole = 0.46 ± 1.5; ropinirole = 0.64 ± 1.5; l-dopa = 0.61 ± 1.8; p = 0.41) did not differ, irrespective of the drug used.
4 Discussion
This is the first head-to-head comparative study of the effect of DAs on neuropsychiatric disturbances in PD that has controlled the sample for the most important confounding factors. The main findings of the present study show that (1) mood disorders (depression, anxiety, apathy, irritability) are predominant in non-demented PD patients; (2) despite depression and anxiety appearing as the most prevalent and severe neuropsychiatric features in this sample, no differences in frequency or severity emerged between medication groups; and (3) patients treated with pramipexole are less likely to manifest apathy when compared with patients treated with ropinirole or levodopa in monotherapy.
Our data reproduce previously reported frequencies of neuropsychiatric symptoms in non-demented PD populations [26, 27]. Mood disorders are predominant in recently diagnosed PD patients [17, 25]. In the last decade, an effort has been made to describe mood disorders in more detail, trying to separate better the presence and severity of apathy, depression, and anxiety [28, 29]. Apathy, when considered as an independent nosological entity, has emerged as one of the most common and frequently misdiagnosed symptoms in PD, it being difficult to differentiate from depression if appropriate scales are not used [28–30]. The Movement Disorders Society has suggested several scales (including the NPI) to screen for apathy [31]. Although apathy has been mainly related to executive dysfunction and global cognitive deterioration, it has also been clearly identified in early to mid-PD stages when it has been carefully assessed [32, 33], and is probably related to decreased dopaminergic innervation of mesolimbic circuits. In the present sample of non-demented patients, the semistructured interview of the NPI allowed us to obtain different frequencies and severity scores for apathy and depression. Up to 49.1 % of patients exhibited some degree of apathy, with clinically meaningful scores in 15.5 %. Given that patients on pramipexole had less apathy on the NPI than patients on ropinirole or levodopa, but no significant differences were found on depression scores, we suggest that pramipexole may be more efficacious for this specific symptom. Given the cross-sectional nature of the study, it cannot be concluded that ropinirole or levodopa do not improve apathy in PD, or that pramipexole or ropinirole did not produce a benefit on depressive symptoms in this sample. We conclude that the present data indicate that pramipexole may exert an additional and more specific effect on motivational symptoms than ropinirole and levodopa. Furthermore, since there was no difference between pramipexole and ropinirole in patients with mild to moderate apathy, the present results suggest that dopamine agonists as a group have a tendency to be less associated with apathy than levodopa.
In addition, since medication groups were matched in terms of executive dysfunction, the lower frequency of apathy observed in the pramipexole group suggests that motivational changes are linked to a more specific activation of dopamine receptors within the limbic system and ventral striatum. A higher affinity of pramipexole over ropinirole for D3 dopamine receptors, found in high density in limbic and paralimbic structures, may explain the differences observed in our study [34–38]. Likewise, specific activations of piribedil on D2/D3 receptors along the mesolimbic pathway are linked to the beneficial effects observed in apathetic symptoms in PD patients after deep brain stimulation [15].
None of the previous studies that analyzed the antidepressant effect of DAs used scales to measure depression and apathy separately [5, 7]. It is therefore difficult to determine whether DAs improved depression by the specific relief of sadness and negativity, or by alleviation of loss of interest and blunted affect [29, 39].
Non-significant differences observed in the frequency and severity of hallucinations in patients treated with DAs or l-dopa can be understood by the characteristics of the sample. On one hand, only non-demented PD patients were included, explaining the low frequency of psychosis found in this sample compared with other series. On the other hand, patients were allowed to be on psychotropic medications if they were controlled in terms of overall clinical management in the 4 weeks before inclusion in the study. It is thus likely that only patients with hallucinations that were well-controlled in clinical practice and through drug management were finally selected.
This study has some limitations. First, we used the NPI, a scale designed for screening neuropsychiatric symptoms. Although it has been claimed that this scale is also appropriate for measuring the severity of these symptoms [22], future studies aiming to determine the possible differential effect of DAs on depression and apathy should use more specific scales for each psychiatric domain. Second, this is a non-randomized, cross-sectional study, and we cannot guarantee that patients were selected to certain DA or levodopa in monotherapy depending of their neuropsychiatric profile. However, currently there are no guidelines to treat apathy in PD, so it is unlikely that physicians selected their therapy on the basis of the presence or absence of apathy. Third, we could not include a group of patients on treatment with rotigotine, and doses of other drugs, such as amantadine or catechol-O-methyl transferase (COMT) inhibitors, were not systematically collected, so we cannot know whether these were well-balanced between groups. And finally, the development of impulse control disorders was not systematically addressed, so we have not been able to analyze their presence in each medication group.
5 Conclusions
Overall, after having controlled medication groups for potentially confounding variables, this study suggests that pramipexole has beneficial effects on apathy that may be added to the previously reported improvements on depression.
References
Olanow CW, Stern MB, Sethi K. The scientific and clinical basis for the treatment of Parkinson disease. Neurology. 2009;72(21 Suppl 4):S1–136.
Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: a retrospective autopsy study. Lancet Neurol. 2005;4(10):605–10.
Evans AH, Strafella AP, Weintraub D, Stacy M. Impulsive and compulsive behaviors in Parkinson’s disease. Mov Disord: Off J Mov Disord Soc. 2009;24(11):1561–70.
Leentjens AF, Koester J, Fruh B, Shephard DT, Barone P, Houben JJ. The effect of pramipexole on mood and motivational symptoms in Parkinson’s disease: a meta-analysis of placebo-controlled studies. Clin Ther. 2009;31(1):89–98.
Rektorova I, Rektor I, Bares M, Dostal V, Ehler E, Fanfrdlova Z, et al. Pramipexole and pergolide in the treatment of depression in Parkinson’s disease: a national multicentre prospective randomized study. Eur J Neurol: Off J Eur Fed Neurol Soc. 2003;10(4):399–406.
Kano O, Ikeda K, Kiyozuka T, Iwamoto K, Ito H, Kawase Y, et al. Beneficial effect of pramipexole for motor function and depression in Parkinson’s disease. Neuropsychiatr Dis Treat. 2008;4(4):707–10.
Barone P, Poewe W, Albrecht S, Debieuvre C, Massey D, Rascol O, et al. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(6):573–80.
Barone P, Scarzella L, Marconi R, Antonini A, Morgante L, Bracco F, et al. Pramipexole versus sertraline in the treatment of depression in Parkinson’s disease: a national multicenter parallel-group randomized study. J Neurol. 2006;253(5):601–7.
Rektorova I, Balaz M, Svatova J, Zarubova K, Honig I, Dostal V, et al. Effects of ropinirole on nonmotor symptoms of Parkinson disease: a prospective multicenter study. Clin Neuropharmacol. 2008;31(5):261–6.
Pahwa R, Stacy MA, Factor SA, Lyons KE, Stocchi F, Hersh BP, et al. Ropinirole 24-hour prolonged release: randomized, controlled study in advanced Parkinson disease. Neurology. 2007;68(14):1108–15.
Trenkwalder C, Kies B, Rudzinska M, Fine J, Nikl J, Honczarenko K, et al. Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord: Off J Mov Disord Soc. 2011;26(1):90–9.
Lemke MR, Brecht HM, Koester J, Reichmann H. Effects of the dopamine agonist pramipexole on depression, anhedonia and motor functioning in Parkinson’s disease. J Neurol Sci. 2006;248(1–2):266–70.
Marin RS. Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci. 1991;3(3):243–54 (summer).
Ray Chaudhuri K, Martinez-Martin P, Antonini A, Brown RG, Friedman JH, Onofrj M, et al. Rotigotine and specific non-motor symptoms of Parkinson’s disease: post hoc analysis of RECOVER. Parkinsonism Relat Disord. 2013;19(7):660–5.
Thobois S, Lhommee E, Klinger H, Ardouin C, Schmitt E, Bichon A, et al. Parkinsonian apathy responds to dopaminergic stimulation of D2/D3 receptors with piribedil. Brain: J Neurol. 2013;136(Pt 5):1568–77.
Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55(3):181–4.
Estorch M, Camacho V, Paredes P, Rivera E, Rodriguez-Revuelto A, Flotats A, et al. Cardiac (123)I-metaiodobenzylguanidine imaging allows early identification of dementia with Lewy bodies during life. Eur J Nucl Med Mol Imaging. 2008;35(9):1636–41.
Dubois B, Burn D, Goetz C, Aarsland D, Brown RG, Broe GA, et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov Disord: Off J Mov Disord Soc. 2007;22(16):2314–24.
Kulisevsky J, Pagonabarraga J, Pascual-Sedano B, Garcia-Sanchez C, Gironell A, Trapecio Group S. Prevalence and correlates of neuropsychiatric symptoms in Parkinson’s disease without dementia. Mov Disord: Off J Mov Disord Soc. 2008;23(13):1889–96.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–42.
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord: Off J Mov Disord Soc. 2010;25(15):2649–53.
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–14.
Aarsland D, Bronnick K, Ehrt U, De Deyn PP, Tekin S, Emre M, et al. Neuropsychiatric symptoms in patients with Parkinson’s disease and dementia: frequency, profile and associated care giver stress. J Neurol Neurosurg Psychiatry. 2007;78(1):36–42.
Aarsland D, Cummings JL, Larsen JP. Neuropsychiatric differences between Parkinson’s disease with dementia and Alzheimer’s disease. Int J Geriatr Psychiatry. 2001;16(2):184–91.
Aarsland D, Bronnick K, Alves G, Tysnes OB, Pedersen KF, Ehrt U, et al. The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2009;80(8):928–30.
Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, et al. The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord: Off J Mov Disord Soc. 2009;24(11):1641–9.
Aarsland D, Marsh L, Schrag A. Neuropsychiatric symptoms in Parkinson’s disease. Mov Disord: Off J Mov Disord Soc. 2009;24(15):2175–86.
Zahodne LB, Marsiske M, Okun MS, Bowers D. Components of depression in Parkinson disease. J Geriatr Psychiatry Neurol. 2012;25(3):131–7.
Kirsch-Darrow L, Marsiske M, Okun MS, Bauer R, Bowers D. Apathy and depression: separate factors in Parkinson’s disease. J Int Neuropsychol Soc: JINS. 2011;17(6):1058–66.
Starkstein SE. Apathy in Parkinson’s disease: diagnostic and etiological dilemmas. Mov Disord: Off J Mov Disord Soc. 2012;27(2):174–8.
Leentjens AF, Dujardin K, Marsh L, Martinez-Martin P, Richard IH, Starkstein SE, et al. Apathy and anhedonia rating scales in Parkinson’s disease: critique and recommendations. Mov Disord: Off J Mov Disord Soc. 2008;23(14):2004–14.
Martinez-Horta S, Pagonabarraga J, Fernandez de Bobadilla R, Garcia-Sanchez C, Kulisevsky J. Apathy in Parkinson’s disease: more than just executive dysfunction. J Int Neuropsychol Soc JINS. 2013;19(5):571–82.
Pedersen KF, Alves G, Bronnick K, Aarsland D, Tysnes OB, Larsen JP. Apathy in drug-naive patients with incident Parkinson’s disease: the Norwegian ParkWest study. J Neurol. 2010;257(2):217–23.
Mierau J, Schingnitz G. Biochemical and pharmacological studies on pramipexole, a potent and selective dopamine D2 receptor agonist. Eur J Pharmacol. 1992;215(2–3):161–70.
Mierau J, Schneider FJ, Ensinger HA, Chio CL, Lajiness ME, Huff RM. Pramipexole binding and activation of cloned and expressed dopamine D2, D3 and D4 receptors. Eur J Pharmacol. 1995;290(1):29–36.
Piercey MF, Hoffmann WE, Smith MW, Hyslop DK. Inhibition of dopamine neuron firing by pramipexole, a dopamine D3 receptor-preferring agonist: comparison to other dopamine receptor agonists. Eur J Pharmacol. 1996;312(1):35–44.
Eden RJ, Costall B, Domeney AM, Gerrard PA, Harvey CA, Kelly ME, et al. Preclinical pharmacology of ropinirole (SK&F 101468-A) a novel dopamine D2 agonist. Pharmacol Biochem Behav. 1991;38(1):147–54.
Coldwell MC, Boyfield I, Brown T, Hagan JJ, Middlemiss DN. Comparison of the functional potencies of ropinirole and other dopamine receptor agonists at human D2(long), D3 and D4.4 receptors expressed in Chinese hamster ovary cells. Br J Pharmacol. 1999;127(7):1696–702.
Mayberg HS. Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci. 1997;9(3):471–81 (summer).
Acknowledgments
The authors thank Ignasi Gich (Epidemiology Department, Sant Pau Hospital) for expert statistical advice and Carolyn Newey (language support, Sant Pau Hospital) for English correction. Funding: The present research was partially funded by CIBERNED (Fundación CIEN, Instituto de Salud Carlos III, Spain).
Compliance with ethical standards
All procedures performed in this study were in accordance with the ethical standards of the local ethics committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Full Financial Disclosures: Jesús Pérez-Pérez: none. Javier Pagonabarraga has received honoraria for lecturing or consultation from Boheringer Ingelheim, UCB, Allergan, Ipsen, and Lundbeck. Saul Martinez-Horta: None. Ramón Fernández de Bobadilla: None. Salvador Sierra: None. Berta Pascual-Sedano received honoraria as a speaker from Medtronic and Novartis. Alexandre Gironell: None. Jaime Kulisevsky has received honoraria for lecturing or consultation from the Michael J. Fox Foundation, Merch serono, AbbVie, Boheringer Ingelheim, UCB, Zambon, MSD, Italfarmaco, General Electric, and Lundbeck.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-Pérez, J., Pagonabarraga, J., Martínez-Horta, S. et al. Head-to-Head Comparison of the Neuropsychiatric Effect of Dopamine Agonists in Parkinson’s Disease: A Prospective, Cross-Sectional Study in Non-demented Patients. Drugs Aging 32, 401–407 (2015). https://doi.org/10.1007/s40266-015-0264-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-015-0264-y