Abstract
Background
Medication use is a potentially modifiable risk factor for falling; psychotropic and cardiovascular drugs have been indicated as main drug groups that increase fall risk. However, evidence is mainly based on studies that recorded falls retrospectively and/or did not determine medication use at the time of the fall. Therefore, we investigated the associations indicated in the literature between medication use and falls, using prospectively recorded falls and medication use determined at the time of the fall.
Methods
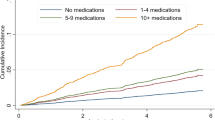
Data from the B-PROOF (B-vitamins for the prevention of osteoporotic fractures) study were used, concerning community-dwelling elderly aged ≥65 years. We included 2,407 participants with pharmacy dispensing records. During the 2- to 3-year follow-up, participants recorded falls using a fall calendar. Cox proportional hazard models were applied, adjusting for potential confounders including age, sex, health status variables and concomitant medication use.
Results
During follow-up, 1,147 participants experienced at least one fall. Users of anti-arrhythmic medication had an increased fall risk (hazard ratio [HR] 1.61; 95 % confidence interval [CI] 1.12–2.32) compared with non-users. Similarly, non-selective beta-blocker use was associated with an increased fall risk (HR 1.41 [95 % CI 1.12–1.78]), while statin use was associated with a lower risk (HR 0.81 [95 % CI 0.71–0.94]). Benzodiazepine use (HR 1.32 [95 % CI 1.02–1.71]), and antidepressant use (HR 1.40 [95 % CI 1.07–1.82]) were associated with an increased fall risk. Use of other cardiovascular and psychotropic medication was not associated with fall risk.
Conclusion
Our results strengthen the evidence for an increased fall risk in community-dwelling elderly during the use of anti-arrhythmics, non-selective beta-blockers, benzodiazepines, and antidepressant medication. Clinicians should prescribe these drugs cautiously and if possible choose safer alternatives for older patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In a prospective setting, including a community-dwelling population aged ≥65 years, the use of anti-arrhythmic medication, non-selective beta-blockers, benzodiazepines, and antidepressant medication was associated with an increased fall risk |
Statin use was associated with a decreased fall risk |
Clinicians should prescribe the fall risk-increasing drugs with caution and if possible choose safer alternatives for older patients |
1 Introduction
Fall incidents are a major problem in older individuals, as one in every three experiences at least one fall per year [1]. Of all falls, 5–12 % [2, 3] result in serious injuries or fractures requiring medical attention, which leads to reduced quality of life and substantial healthcare costs [4, 5]. A potentially modifiable risk factor for falls is medication use [6, 7]. Over the last decade, medication-related falls have received more and more attention. Psychotropic [8–10] and cardiovascular [8, 9, 11] medications have been indicated as the main drug groups contributing to an increased fall risk. However, evidence for these associations is mainly based on observational studies, which have applied varying methods for recording fall incidents and medication use. The most recent meta-analysis showed that only 6 of 22 studies included recorded falls prospectively and ascertained medication use at the time of the fall [8]. In addition, current evidence is based on studies in community-dwelling older individuals as well as in those living in long-term care facilities, while these populations clearly differ in clinical characteristics. Therefore, the question arises whether these results can be validly combined. Although overall results point in a similar direction, only psychotropic drug use is consistently associated with an increased fall risk [8, 9, 12–14]. Therefore, our objective is to investigate associations previously indicated in literature between medication use and fall incidents, using prospectively recorded fall incidents and pharmacy dispensing records to determine medication use at the time of the fall. The study setting concerns a large population of community-dwelling older individuals, with a follow-up period of 2–3 years.
2 Methods
2.1 Study Population and Setting
Data from the B-PROOF study were used. B-PROOF is an acronym for ‘B-vitamins for the prevention of osteoporotic fractures’, a study whose design has been described elsewhere in more detail [15]. Briefly, it is a multi-centre, randomized, placebo-controlled, double-blind trial investigating the efficacy of vitamin B12 and folic acid supplementation on the prevention of fracture incidence in individuals aged ≥65 years. In total, 2,919 participants were included from the area of three Dutch cities: Wageningen, Rotterdam and Amsterdam. All participants had mildly elevated homocysteine levels (12–50 μmol/L), sufficient renal function (creatinine ≤150 μmol/L), and did not report malignancies in the past 5 years. Participants were randomly selected to receive daily the intervention tablet containing 500 μg vitamin B12, 400 μg folic acid and 600 IU vitamin D, or the placebo tablet containing only 600 IU of vitamin D. In total, the intervention period comprised 2–3 years. The Medical Ethics Committee of Wageningen University approved the study protocol, and the Medical Ethics Committees of Erasmus Medical Centre and VU University Medical Centre gave approval for local feasibility. Before entering the study, all participants gave written informed consent.
Previous results indicated that the intervention had no effect on the time to the first or second fall, and the number of falls experienced during the study [unpublished data]. Therefore, in the current study, we treated the study population as a cohort, and, to rule out potential residual confounding that might relate to the intervention, we adjusted for the intervention status. The intervention status indicated whether a participant received the intervention or the placebo tablet during follow-up.
2.2 Outcome
Fall incidents were prospectively recorded during the study period. Participants reported fall incidents each week on a fall and fracture calendar, which was returned to the research team every 3 months. When a calendar was incomplete or unclear, the participant was contacted by telephone. A fall incident was defined as an unintentional change in position resulting in coming to a rest at a lower level or on the ground [16]. Participants were followed until their first fall incident. The Thursday in that particular week was defined as the index date. Participants who experienced more than one fall during the follow-up period were censored after their first fall incident. Drop-outs (of the intervention study) without further calendar information after drop-out were censored at their drop-out date. Participants who kept filling out the calendar after their drop-out were followed until their last calendar. Therefore, a participant’s follow-up time ended at the date of their first fall incident, their drop-out date or the date of their last calendar, date of death, or the end of the study, whichever came first.
2.3 Medication Use
Medication use was determined on the basis of pharmacy dispensing records. These records contain information regarding the product name, the anatomical therapeutic chemical code [17], the administration route, the dispensing date, the total amount of drug units per prescription and the prescribed daily number of units. Electronic pharmacy dispensing records were obtained from the Dutch Foundation for Pharmaceutical Statistics (SFK). This foundation gathers data of all the pharmacies in their panel, which is approximately 95 % of all Dutch community pharmacies [18]. Dispensing records were only obtained for participants who gave written informed consent for gathering these data. Additionally, the pharmacists approved the use of the data. The pharmacy dispensing data of a participant were defined as complete when all participant pharmacies were in the SFK panel and data could be obtained. Data were available for the participants throughout their follow-up period.
Medication usage periods were calculated from the dispensing date, the number of tablets prescribed, and the prescribed daily number of tablets. A participant was considered a current user of a medication group when the time of the fall (index date) fell within a prescription episode. The average prescribed daily dose was expressed in standardized defined daily doses (DDDs) [17].
The medication groups from Table 1, covering previously suggested fall risk-increasing drugs (FRID) [8–11, 19, 20], were used as potential exposure determinants. Medication groups with <1 % users at baseline were not included in the analyses.
2.4 Covariates
Baseline demographic characteristics were ascertained using a questionnaire that gathered data on age, sex, use of a walking aid, history of falls and fractures, and health status variables (which included smoking habits, alcohol consumption, prevalent cardiovascular disease parameters, diabetes and hypercholesterolemia). A history of cardiovascular disease was defined as having a history of at least one of the following disorders: myocardial infarction, angina pectoris, heart failure, percutaneous coronary intervention, intermittent claudication, transient ischaemic attack, stroke, thrombosis or embolism. During the baseline study visit, various characteristics were measured, including weight, height, blood pressure, physical performance, handgrip strength, depressive symptoms and cognitive status. Weight was measured with a calibrated scale, and height was measured using a stadiometer. From this, the body mass index (BMI, kg/m2) was calculated. Blood pressure was measured twice, using an Omron M1 plus device (Omron Healthcare Europe, Hoofddorp, The Netherlands), and the lowest diastolic and corresponding systolic blood pressure reading were included in the analyses. Hypertension was defined as systolic blood pressure >140 mmHg and/or diastolic blood pressure >90 mmHg [21]. A physical performance score was calculated from the results of three physical function tests: walking test, chair stand test, and the tandem stand test [22]. For every test, a maximum score of 4 could be obtained, resulting in a physical performance score ranging from 0 to 12 (low physical performance–high physical performance) [23]. Handgrip strength (kg) was assessed by performing two maximum trials per hand using a dynamometer (Takei TKK 5401, Takei Scientific Instrument CO. Ltd., Tokyo, Japan). The highest result of the four trials was used as the maximum handgrip strength. Depressive symptoms were measured using the 15-item version of the Geriatric Depression Scale (GDS) [24], and cognitive status was measured by using the Mini-Mental State Examination (MMSE) [25].
Blood was drawn when the participants had fasted or had consumed a light restricted breakfast. Plasma homocysteine levels were assessed from blood collected in a tube containing EDTA (ethylenediaminetetraacetic acid), which was stored on ice after blood collection and processed within 4 h. To determine homocysteine, Wageningen University used high-performance liquid chromatography (intra assay coefficient of variation [CV] 3.1 %, inter assay CV 5.9 %), Erasmus Medical Centre used liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS) (intra assay CV 5.5 %, inter assay CV 1.3 %), and VU Medical Centre used the Architect i2000 RS analyser (intra assay CV 2 %, inter assay CV 4 %). Cross calibration of the assays indicated no significant difference between the outcomes.
Serum creatinine was measured using the enzymatic colorimetric Roche CREA plus assay (CV 2 %). It was used to calculate an age- and sex-adjusted estimate of the glomerular filtration rate (GFR) according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [26]. For men, it was calculated when their creatinine was ≤80 μmol/L using the formula 141 × [serum creatinine (μmol/L)/80]−0.411 × [0.993age (years)], and if their creatinine was >80 μmol/L using the formula 141 × [serum creatinine (μmol/L)/80]−1.209 × [0.993age (years)] in ml/min/1.73 m2. For women, it was calculated when their creatinine levels were ≤62 μmol/L using the formula 144 × [serum creatinine (μmol/L)/62]−0.329 × [0.993age (years)], and if their creatinine was >62 μmol/L using the formula 144 × [serum creatinine (μmol/L)/62]−1.209 × [0.993age (years)] in ml/min/1.73 m2.
Serum 25-hydroxy vitamin D [25(OH)D], was used as marker for vitamin D status and determined by isotope dilution—online solid phase extraction liquid chromatography—tandem mass spectrometry (ID-XLS-MS/MS), which is described elsewhere in detail [27].
2.5 Statistical Analyses
Baseline characteristics were determined for the overall group and for fallers and non-fallers separately. These characteristics were also assessed for the whole B-PROOF population, including those without electronic pharmacy dispensing records. Differences between groups were tested using a t test for continuous variables and a Chi-squared test for categorical variables. If a variable was non-normally distributed, a Mann–Whitney U test was used.
Cox proportional hazards models were used to calculate hazard ratios (HR). The model compares the prevalence of exposure to the medication group in the incident fall cases on the index date with the exposure prevalence in all other participants in the cohort on that date [28]. The models were adjusted for age, sex and intervention status. The variables that differed at baseline between fallers and non-fallers (p < 0.2) were added to the model using the forward selection methods (model 2). Medication groups that resulted in significant HRs were added to the other significant medication groups, thereby adjusting for concomitant medication use (model 3). The effect of handgrip strength and physical performance was investigated separately by adding them separately as well as combined to the model. Physical function parameters are known fall risk factors, but they might also be affected by medication use itself, and thereby might act as an intermediate. In addition, the effect of fall history was examined by adding it to the model. When the HR was changed >5 %, the parameter was regarded to influence the association. Interaction with CKD-EPI was tested for medication groups with renal clearance, since associations may be different in those with reduced renal function. When the p value of the interaction term was <0.1, the results were stratified.
To further investigate the robustness of our findings, we investigated the dose–response relationship for the medication groups that were significantly associated with fall risk. The categories for dose were created based on the median number of prescribed DDDs. Furthermore, additional analyses were conducted for non-selective β-blockers, diuretics, statins and antidepressants. Non-selective β-blocker use was subdivided in timolol use—administered as eye drops with potential systemic effects—and other non-selective β-blocker use, to investigate whether the association was driven by timolol use. For thiazide and loop diuretics, duration periods were investigated, since previous research indicated an increased fall risk on initiation of treatment [29–31]. The duration periods were defined as the first 21 days of use, 22–45 days, and longer than 45 days of use, taking non-users as the reference [29–31]. In addition, the association between past use of statins and antidepressants with fall incidents was assessed. The reason for this was that the association between statins and antidepressants might have been confounded by the indications for their use. Past use was defined as use prior to the index date. All statistical analyses were carried out using the statistical software package SPSS version 21.0 (IBM, Armonk, NY, USA), and p values <0.05 were considered to be statistically significant.
3 Results
3.1 Study Population Characteristics
The study population with pharmacy dispensing records consisted of 2,407 participants. Their baseline characteristics, also subdivided into those who did and did not experience a fall during follow-up, are presented in Table 2. Participants who experienced a fall during follow-up were slightly older, more likely to be women and to have a positive fall history. Furthermore, fallers were more likely to use a walking aid, have lower handgrip strength and lower physical performance score, while their MMSE and GDS score was slightly higher than those who did not fall during the follow-up.
Characteristics of the subgroup with pharmacy dispensing data were very similar to the overall B-PROOF population (n = 2,919, data not shown). The only significant difference was a slightly lower percentage of women (49.1 vs. 50.0, p = 0.026) and participants using a walking aid (13.6 vs. 14.6, p = 0.001) in the pharmacy dispensing data group. Furthermore, the representation of study centres was slightly altered and the physical performance score was slightly higher in those with pharmacy dispensing data than the whole B-PROOF study population, although the difference in physical performance score did not result in different median and interquartile range (IQR) values: 9 (6–11) vs. 9 (6–11), p = 0.017.
3.2 Fall Risk-Increasing Drugs (FRID)
Of the cardiovascular drugs, the use of anti-arrhythmic medication was associated with an increased risk for falls compared with non-users (HR 1.61; 95 % confidence interval [CI] 1.12–2.32; p = 0.010) (Table 3, model 3). Similarly, use of non-selective beta-blockers was associated with an increased fall risk (HR 1.41 [95 % CI 1.12–1.78] p = 0.004), while statin use was associated with a lower fall risk (HR 0.81 [95 % CI 0.71–0.94] p = 0.004) (Table 3, model 3). Use of antihypertensive medication overall or any of the other cardiovascular medication groups was not significantly associated with fall incidents (Table 3, model 2). In addition, the use of ‘other’ analgesics was associated with an increased fall risk (HR 1.45 [95 % CI 1.00–2.11] p = 0.049) (Table 3, model 3). This ‘other’ analgesics group included the non-opioid analgesics, covering the Anatomical Therapeutic Chemical (ATC) codes N02B and N02C. With regard to psychotropic drugs, the use of benzodiazepines was associated with an increased risk (HR 1.32 [95 % CI 1.02–1.71] p = 0.034) (Table 3, model 3). Likewise, antidepressant use was associated with an increased risk (HR 1.31 [95 % CI 1.00–1.70] p = 0.046) (Table 3, model 3). No other significant associations were observed between the use of psychotropic mediation or any of the other medication groups and fall incidents (Table 3, model 2 and 3).
3.3 The Role of Physical Performance, Fall History and Renal Function Parameters
Adding handgrip strength, physical performance, or both parameters to the model did not change most of the HRs substantially; only the association with non-opioid analgesics and antidepressants was affected. After adding the physical performance score to the model, the association with non-opioid analgesics lost significance (HR 1.39 [95 % CI 0.95–2.05] p = 0.093). Conversely, when physical performance was added to the antidepressant model, the association became stronger (HR 1.40 [95 % CI 1.07–1.82] p = 0.013), indicating a potentially protective effect of physical performance.
Adding fall history to the model did not substantially change the HR of any of the medication groups that were significantly associated with fall risk (Table S1 in the Electronic Supplementary Material [ESM]).
The interaction term for renal function with a medication group did not suggest effect modification for any of the medication groups (data not shown).
3.4 Additional Analyses
No clear dose–response association was observed for any of the medication groups that were significantly associated with fall risk (Table S2 in the ESM).
The use of non-selective β-blockers—excluding timolol—was associated with an increased fall risk (HR 1.41 [95 % CI 1.03–1.95] p = 0.034), while timolol use was borderline significantly associated (HR 1.37 [95 % CI 0.99–1.90] p = 0.060). Both associations were adjusted for age, sex, intervention status, study centre, MMSE and GDS score, and the other medication groups that were significantly associated with fall risk (data not shown).
The first 21 days of thiazide use (HR 0.89 [95 % CI 0.59–1.35] p = 0.588) and loop diuretic use (HR 1.36 [95 % CI 0.74–2.48] p = 0.321) were not associated with an increased fall risk; both associations were adjusted for age, sex, intervention, study centre, and MMSE and GDS score.
Past use of statins was not associated with fall risk (HR 1.07 [95 % CI 0.78–1.46] p = 0.690). Likewise, past use of antidepressants was not associated with fall risk (HR 1.37 [95 % CI 0.88–2.14] p = 0.161). Both associations were adjusted for age, sex, intervention status, study centre, MMSE and GDS score, and the other medication groups that were significantly associated with fall risk (data not shown).
4 Discussion
Our results indicate an increased fall risk in community-dwelling older adults during the use of anti-arrhythmic medication, non-selective beta-blockers, benzodiazepines and antidepressant medication. Additionally, a decreased fall risk was observed for statin use, whereas no significant association was observed for other antihypertensive medication, including diuretics, and for non-steroidal anti-inflammatory drugs (NSAIDs).
In concordance with our results, the meta-analysis by Leipzig et al. [11] indicated an increased fall risk from anti-arrhythmic class IA drug use. However, our exposure category was slightly different because we combined all classes of anti-arrhythmic medication. Potential adverse effects of anti-arrhythmics that may contribute to fall risk are bradycardia, hypotension or torsade de pointes [32].
The meta-analysis by Woolcott et al. [8] did not indicate an increased fall risk for beta-blocker use, whereas two recent self-controlled case series studies did observe an increased risk [29, 30]. Our results indicated an increased risk for use of non-selective beta-blockers. Previous studies did not distinguish between different types of beta-blockers, and it is unclear whether eye drops such as timolol were included. Timolol is a non-selective beta-blocker known to be able to cause systemic adverse effects [33, 34]. Its use has been associated with syncope [35]. Timolol is regularly used in the elderly population, including our population, mainly for glaucoma or ocular hypertension [33, 34]. Although timolol by itself was borderline significantly associated with an increased fall risk, the HR was similar to that for non-selective beta-blocker use, excluding timolol. Furthermore, the combination of non-selective beta-blocker use and timolol has a higher level of significance than when separated. An increased fall risk by beta-blockers may be a result of bradycardia and hypotension. However, non-selective beta-blocker use might have additional adverse effects by which they may increase the fall risk. For example, sotalol also exhibits class III anti-arrhythmic properties, which is associated with torsade de pointes [32], and propranolol use may result in central nervous system adverse effects, such as dizziness and insomnia, due to its lipophilic properties [36].
The use of antihypertensive medication overall has been indicated to increase fall risk [8, 29]. Similarly, diuretic use overall has been associated with increased fall risk [11], but not consistently [8]. Recent results indicated that initiation of antihypertensives [29] and especially thiazide diuretics [29–31] increased fall risk, which is potentially attributed to an initially induced hypotensive effect that stabilizes over time [29, 31]. Nevertheless, according to our additional analyses, initiation of thiazides or loop diuretics was not associated with fall risk. This discrepancy in findings might be due to our low number of users who initiated thiazides or loop diuretics.
Remarkably, our results indicated a decreased fall risk during statin use, while previously an increased risk has been proposed due to potential negative effects on muscle strength and balance. Nevertheless, no significant associations were observed [37]. A beneficial effect on fall risk might be due to the cardioprotective effects of statin use [37–39]. An opposite explanation might be confounding by indication. It is possible that more frail older individuals may not have received a statin prescription, and therefore the non-statin users had an increased fall risk. However, this is speculative, and our additional analyses investigating the association with past use of statins did not support this speculation. Because our finding is new and potential mechanisms are lacking, more research is required before firm conclusions can be drawn.
Analyses with use of ‘other’ analgesics, covering the non-opioids, indicated a significant association with fall risk in the first analysis, but lost significance after including physical performance. For this particular drug group, a confounding effect is more likely than a mediating effect. Use of non-opioid analgesics may reflect an impaired overall health status, including physical performance state, and may thereby be related to fall risk. Previously, Leipzig et al. [11] also did not observe an association between use of non-opioid analgesics and fall risk.
The use of sedatives and hypnotics, and especially benzodiazepines, has been consistently shown to increase fall risk [8, 9, 12–14]. Benzodiazepine use could influence fall risk in several ways, by negatively affecting balance, gait and cognition [9]. In addition, it may induce hyponatremia [40], which is also associated with falls [41, 42].
In line with previous findings [8, 9, 31, 43], we observed an increased fall risk for antidepressant medication use overall, while no significant association with its subgroups were seen. This may be due to low numbers of users in the subgroups. Antidepressant use has been proposed to affect fall risk in several ways, including by inducing sedation, impaired sleep and balance, slower gait speed and reaction time, and orthostatic hypotension [43–45]. Nevertheless, it is difficult to separate the effect from depression itself, as that could result in falls via similar mechanisms [43–45]. However, our additional analyses did not indicate an increased fall risk for past users of antidepressants. In addition, two self-controlled case-series studies also reported an increased risk, and this method is less subject to confounding by indication [45, 46]. Furthermore, a cohort study investigating the association with both depression and antidepressants concluded that both aspects contributed to fall risk [43]. Thus, our result strengthens the evidence for an increased fall risk during antidepressant use.
This study has several limitations. First, the studied population included participants with slightly elevated homocysteine levels at baseline. Therefore, our results cannot be extrapolated to the general ambulant older population. Nevertheless, it is questionable whether the observed association would be different in populations that also included participants with lower homocysteine levels, as there is, to our knowledge, no association between homocysteine levels and medication-related falls. Second, half of the participants received folic acid and vitamin B12, and all participants received vitamin D supplementation during their follow-up. However, no differences were observed between the intervention and placebo groups regarding the time to the first fall or second fall and the number of falls experienced during follow-up [unpublished data]. With respect to the vitamin D supplementation, this has been suggested to reduce fall risk, though evidence is inconsistent [47]. Because all participants received supplementation, and we do not expect interference with medication-related falls, we do not think this affected our results. Third, falls were self-reported in a weekly fashion, thereby the fall week was known instead of the exact fall date. However, we do not think that this minimal random misclassification in timeframe has altered the results. Fourth, confounding by indication or contra-indication could not be investigated thoroughly in our study and could have affected our results. Finally, based on the number of medication groups investigated, a chance finding could have occurred. Although there are limitations, our study has major strengths. It investigated a large community-dwelling population in which a wide range of health status determinants were assessed. Furthermore, falls were recorded prospectively, and medication use was determined using pharmacy dispensing records, making it possible to determine medication use at time of the fall. Thereby, we could more closely approach the true association between medication use and fall incidents compared with cross-sectional studies.
5 Conclusion and Perspective
Overall, our results strengthen the evidence for an increased fall risk in community-dwelling older individuals during the use of anti-arrhythmic medication, non-selective beta-blockers, benzodiazepines and antidepressant medication. Although medication use is a potentially modifiable fall risk factor, single interventions targeting reductions in the number or doses of medications are limited, though more studies focused on fall prevention using medication reviews to modify prescription. Fall rate could be reduced by such interventions, but results regarding fall risk reduction are modest [47, 48], which is partly attributed to the complexity of dose reduction or stopping medication and the possible reintroduction of medication use after stopping [48]. Nevertheless, clinicians should be aware of drugs associated with fall risk during prescription, and consider the risk–benefit balance. If available, safer alternatives should be recommended.
References
Cumming RG. Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging. 1998;12(1):43–53.
Tinetti ME, Doucette J, Claus E, et al. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(11):1214–21.
Stel VS, Smit JH, Pluijm SMF, et al. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. 2004;33(1):58–65.
Hartholt KA, Polinder S, Van der Cammen TJ, et al. Costs of falls in an ageing population: a nationwide study from the Netherlands (2007–2009). Injury. 2012;43(7):1199–203.
Roudsari BS, Ebel BE, Corso PS, et al. The acute medical care costs of fall-related injuries among the U.S. older adults. Injury. 2005;36(11):1316–22. doi:10.1016/j.injury.2005.05.024.
Karlsson MK, Vonschewelov T, Karlsson C, et al. Prevention of falls in the elderly: a review. Scand J Public Health. 2013;41(5):442–54.
Panel on Prevention of Falls in Older Persons American Geriatrics Society. British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57.
Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–60.
Hartikainen S, Lönnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62(10):1172–81.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30–9.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47(1):40–50.
van Strien AM, Koek HL, van Marum RJ, et al. Psychotropic medications, including short acting benzodiazepines, strongly increase the frequency of falls in elderly. Maturitas. 2013;74(4):357–62.
Hill K, Wee R. Psychotropic drug-induced falls in older people. Drugs Aging. 2012;29(1):15–30. doi:10.2165/11598420-000000000-00000.
Moden B, Merlo J, Ohlsson H, et al. Psychotropic drugs and falling accidents among the elderly: a nested case control study in the whole population of Scania, Sweden. J Epidemiol Community Health. 2010;64(5):440–6.
van Wijngaarden JP, Dhonukshe-Rutten RA, van Schoor NM, et al. Rationale and design of the B-PROOF study, a randomized controlled trial on the effect of supplemental intake of vitamin B12 and folic acid on fracture incidence. BMC Geriatr. 2011;11:80.
The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34(Suppl 4):1–24.
ATC and DDD Index. WHO Collaborating Centre for Drug Statistics Methodology, Oslo. http://www.whocc.no/atc_ddd_index/.
Pincus T, Summey JA, Soraci SA Jr, et al. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum. 1983;26(11):1346–53.
Sjoberg C, Wallerstedt SM. Effects of medication reviews performed by a physician on treatment with fracture-preventing and fall-risk-increasing drugs in older adults with hip fracture-a randomized controlled study. J Am Geriatr Soc. 2013;61(9):1464–72.
Hartholt KA, Boye ND, Van der Velde N, et al. [Cost] effectiveness of withdrawal of fall-risk increasing drugs versus conservative treatment in older fallers: design of a multicenter randomized controlled trial (IMPROveFALL-study). BMC Geriatr. 2011;11:48.
Whitworth JA, World Health Organization ISoHWG. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11):1983–92.
Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94.
Swart KMA, Enneman AW, van Wijngaarden JP, et al. Homocysteine and the methylenetetrahydrofolate reductase 677C[srarr]T polymorphism in relation to muscle mass and strength, physical performance and postural sway. Eur J Clin Nutr. 2013;67(7):743–8. doi:10.1038/ejcn.2013.97.
Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Heijboer AC, Blankenstein MA, Kema IP, et al. Accuracy of 6 routine 25-hydroxyvitamin D assays: influence of vitamin D binding protein concentration. Clin Chem. 2012;58(3):543–8.
Stricker BH, Stijnen T. Analysis of individual drug use as a time-varying determinant of exposure in prospective population-based cohort studies. Eur J Epidemiol. 2010;25(4):245–51.
Butt DA, Mamdani M, Austin PC, et al. The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int. 2013;24(10):2649–57.
Gribbin J, Hubbard R, Gladman J, et al. Risk of falls associated with antihypertensive medication: self-controlled case series. Pharmacoepidemiol Drug Saf. 2011;20(8):879–84.
Gribbin J, Hubbard R, Gladman JR, et al. Risk of falls associated with antihypertensive medication: population-based case-control study. Age Ageing. 2010;39(5):592–7.
Lee HC, Ti Huang K, Shen WK. Use of antiarrhythmic drugs in elderly patients. J Geriatr Cardiol. 2011;8(3):184–94.
Volotinen M, Hakkola J, Pelkonen O, et al. Metabolism of ophthalmic timolol: new aspects of an old drug. Basic Clin Pharmacol Toxicol. 2011;108(5):297–303.
Nieminen T, Lehtimaki T, Maenpaa J, et al. Ophthalmic timolol: plasma concentration and systemic cardiopulmonary effects. Scand J Clin Lab Invest. 2007;67(2):237–45.
Muller ME, van der Velde N, Krulder JW, et al. Syncope and falls due to timolol eye drops. BMJ. 2006;332(7547):960–1.
Reiter MJ. Cardiovascular drug class specificity: β-blockers. Prog Cardiovasc Dis. 2004;47(1):11–33. doi:10.1016/j.pcad.2004.04.004.
Haerer W, Delbaere K, Bartlett H, et al. Relationships between HMG-CoA reductase inhibitors (statin) use and strength, balance and falls in older people. Intern Med J. 2012;42(12):1329–34.
Macedo AF, Taylor FC, Casas JP, et al. Unintended effects of statins from observational studies in the general population: systematic review and meta-analysis. BMC Med. 2014;12(1):51.
Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):CD004816.
Liamis G, Rodenburg EM, Hofman A, et al. Electrolyte disorders in community subjects: prevalence and risk factors. Am J Med. 2013;126(3):256–63.
Cumming K, Hoyle GE, Hutchison JD, et al. Prevalence, incidence and etiology of hyponatremia in elderly patients with fragility fractures. PLoS One. 2014;9(2):e88272.
Gunathilake R, Oldmeadow C, McEvoy M, et al. Mild hyponatremia is associated with impaired cognition and falls in community-dwelling older persons. J Am Geriatr Soc. 2013;61(10):1838–9.
Quach L, Yang FM, Berry SD, et al. Depression, antidepressants, and falls among community-dwelling elderly people: the MOBILIZE Boston study. J Gerontol A Biol Sci Med Sci. 2013;68(12):1575–81.
Kvelde T, McVeigh C, Toson B, et al. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(5):694–706.
Coupland CA, Dhiman P, Barton G, et al. A study of the safety and harms of antidepressant drugs for older people: a cohort study using a large primary care database. Health Technol Assess. 2011;15(28):1–202 (iii-iv).
Gribbin J, Hubbard R, Gladman J, et al. Serotonin-norepinephrine reuptake inhibitor antidepressants and the risk of falls in older people: case-control and case-series analysis of a large UK primary care database. Drugs Aging. 2011;28(11):895–902.
Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9):CD007146.
Boyle N, Naganathan V, Cumming RG. Medication and falls: risk and optimization. Clin Geriatr Med. 2010;26(4):583–605.
Acknowledgments
The authors gratefully thank all study participants and all dedicated co-workers who helped in the success of the B-PROOF trial, especially S. Smits, R.N.; P.H. in ‘t Veld, MSc; M. Hillen-Tijdink; A. Nicolaas-Merkus; and N. Pliester. In addition, we thank SFK for their cooperation and for providing the pharmacy dispensing records, especially J. Lukaart, MSc.
B-PROOF is supported and funded by The Netherlands Organization for Health Research and Development (ZonMw, Grant 6130.0031 and 11-31010-06), the Hague; unrestricted grant from NZO (Dutch Dairy Association), Zoetermeer; NCHA (Netherlands Consortium for Healthy Ageing) Leiden/ Rotterdam; Ministry of Economic Affairs, Agriculture and Innovation (project KB-15-004-003), the Hague; Wageningen University, Wageningen; VU University Medical Centre, Amsterdam; Erasmus Medical Center, Rotterdam. All organisations are based in the Netherlands. The sponsors do not have any role in the design or implementation of the study, data collection, data management, data analysis, data interpretation, or in the preparation, review, or approval of the manuscript.
The authors have no potential conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ham, A.C., Swart, K.M.A., Enneman, A.W. et al. Medication-Related Fall Incidents in an Older, Ambulant Population: The B-PROOF Study. Drugs Aging 31, 917–927 (2014). https://doi.org/10.1007/s40266-014-0225-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0225-x