Abstract
Background
Drug-related problems (DRPs) are common in aged care facilities and few studies have been conducted to determine the impact of the pharmacist-conducted medication review services. Studies determining the prevalence of chronic kidney disease (CKD) and data regarding inappropriate prescribing of renally cleared medications in aged care facilities in Australia are also lacking.
Objectives
To investigate the number and nature of DRPs identified and recommendations made by pharmacists in residents of aged care facilities. To determine the prevalence of CKD and estimate the magnitude of inappropriate prescribing of renally cleared medications in residents of aged care facilities.
Methods
DRPs identified and recommendations made by pharmacists were classified using the adapted version of the DOCUMENT classification system. The modification of diet in renal disease formula was used to estimate the prevalence of CKD, and the Cockcroft–Gault formula was used to estimate the magnitude of inappropriate prescribing of renally cleared medications.
Results
Over 98 % of residents of aged care facilities had at least one DRP. Most (83.8 %) recommendations made by accredited pharmacists to resolve DRPs were accepted by general practitioners. CKD was prevalent in 48 % of residents, and inappropriate prescribing of renally cleared medications was identified in 28 (16 %) residents with CKD.
Conclusions
DRPs are common in aged care facilities and the impact of medication review services appears to be high. CKD is also common among residents of aged care facilities, and inappropriate prescribing of renally cleared medications was also prevalent, warranting attention to regular renal function monitoring and appropriate drug and dose selection in residents of aged care facilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The collaborative Residential Medication Management Review service can significantly reduce drug-related problems encountered in residents of the Australian aged care facilities. |
Chronic kidney disease and prescribing of renally cleared medications in residents of the aged care facilities in Australia is prevalent and residents should be routinely monitored for decline in kidney function. |
1 Introduction
Older people with multiple chronic conditions take multiple medications and are therefore at an increased risk of experiencing a drug-related problem (DRP) and an adverse drug event (ADE) [1]. A DRP is an event or circumstance which occurs when a drug treatment actually or potentially interferes with the patient experiencing an optimum outcome of medical care; high dose, drug interaction, and ADE are some examples of DRPs [2].
Prescribing in older people is often guided by consensus statements or guidelines informed by clinical trials performed in ‘younger’ people without significant co-morbidities [3, 4]. Therefore, prescribing in older people remains challenging. Prescribing in residents of aged care facilities is even more challenging as they are often the frailest old and take up to four times more medications than their age-matched community-dwelling counterparts [5]. In addition, residents generally have age-related changes in pharmacokinetics and pharmacodynamics, which increase their risk of developing ADEs [6, 7]. This risk is further increased when drugs are prescribed inappropriately.
Inappropriate prescribing is defined as a situation where risk from the adverse effects of a prescribed medication outweighs the desired clinical benefits of treating a particular condition [3]. Previous studies have reported prescribing in aged care residents as being relatively poor in quality, particularly with respect to overuse of inappropriate drugs and underuse of beneficial therapies [8–11]. Inappropriate prescribing is often implicated as the cause of DRPs and increased risk of hospitalisation and death in this population [12, 13].
There is also evidence that aged care residents are not ideally managed with respect to chronic conditions, especially chronic kidney disease (CKD) [14, 15]. CKD occurs when the glomerular filtration rate (GFR) falls below 60 ml/min/1.73 m2 [14, 16] and the prevalence of CKD increases disproportionately in older people because of the age-related decline in GFR of approximately 8 ml/min/1.73 m2 with each decade of life after the age of 40 years [17]. Furthermore, age-related decline in kidney function in older people may not be associated with obvious complications of CKD but impaired kidney function that could markedly affect the clearance of drugs by the kidney [14, 18].
Despite the high prevalence of CKD [19, 20] and its association with mortality, it is often under-recognised in older people, which could lead to inappropriate prescribing [21]. Two studies conducted in the US have shown that renal dosing guidelines are often overlooked in residents of aged care facilities, and this is a major contributor to overall inappropriate prescribing and DRPs in aged care facilities [15, 22]. It is therefore important to identify residents with impaired renal function in aged care facilities and accordingly adjust the dosage of renally cleared medications.
In Australia, the Residential Medication Management Review (RMMR) is a nationally remunerated clinical service available to all permanent residents of Australian Government-funded aged care facilities [23]. The RMMR is a comprehensive medication review conducted by accredited pharmacists and aims to optimise the benefits of medicine use, improve therapeutic outcomes, and ensure the appropriate, safe and effective use of medicines in aged care facility residents [24, 25]. The RMMR service may be conducted either by an accredited pharmacist alone [pharmacist RMMR] or in collaboration with a general practitioner (GP) [collaborative RMMR] [25]. The collaborative RMMR process comprises (i) GP referral of the resident to an approved RMMR service provider; (ii) pharmacist written report documenting RMMR findings and recommendations sent to the GP; (iii) discussion by the GP and pharmacist to develop a medication management plan based on the findings and recommendations; and (iv) consultation with the resident to obtain agreement to the medication management plan [25]. A recent retrospective study reported that over 96 % of aged care facility residents had potential DRPs identified by accredited pharmacists [26]. Other studies have shown that pharmacist-conducted medication reviews can improve medication use by reducing DRPs in aged care facility residents [11, 27, 28]. However, there is limited research on the impact of the collaborative RMMR service on DRPs in general and on therapeutic outcomes for residents with renal impairment. The main objectives of this study were:
-
To investigate the number and nature of DRPs identified by accredited pharmacists.
-
To investigate the number and nature of recommendations made by accredited pharmacists to resolve DRPs.
-
To investigate the GP acceptance of accredited pharmacists’ recommendations.
-
To estimate the prevalence of CKD in residents of aged care facilities.
-
To determine the extent of inappropriate prescribing (defined as the use of contraindicated medication or use of higher-than-recommended dosage based on renal function) of renally cleared medications in residents with CKD.
2 Methods
2.1 Ethics and Study Population
The Human Research Ethics Committee (Tasmania) Network exempted this study from ethical review as the study was identified as being of negligible risk.
This retrospective study involved the collection of de-identified RMMR reports pertaining to 911 residents of aged care facilities from a single Sydney-based RMMR service provider (Meditrax Pty Ltd). The RMMR service was conducted by accredited pharmacists in collaboration with GPs between August 2011 and December 2012. All pharmacists were accredited either by the Australian Association of Consultant Pharmacy (AACP) or the Society of Hospital Pharmacists of Australia (SHPA) [25].
2.2 Exclusion Criteria
RMMR reports were excluded from the study if they met any of the following criteria: (i) age and sex in the RMMR report did not match the same on the pathology report; (ii) duplicate RMMR report; (iii) medication chart was missing from the RMMR report; (iv) pharmacists’ recommendations were missing in the RMMR report; and (v) the identification number of the resident on the RMMR report did not match the same on the pathology report.
2.3 Data Extraction and Coding
One study investigator (PAG) performed a thorough review of the 911 RMMR reports, and performed data extraction and coding. Drugs taken by the residents of aged care facilities were coded according to the Anatomical Therapeutic Chemical (ATC) classification system, an international standard for drug utilisation studies identified by the World Health Organization [29]. Medical diagnoses were categorised according to the International Classification of Diseases, 10th revision (ICD-10) disease categories [30].
Each RMMR report written by the accredited pharmacist was divided into two parts: (i) DRPs identified, and (ii) recommendations made to resolve those DRPs. These DRPs and recommendations were then classified using the adapted version of the DOCUMENT classification system [2]. One new category of DRP and six new subcategories of recommendation were appended to the original categories of DRPs and recommendations of the DOCUMENT classification system, which are as follows: U4—condition resolved, R3a—add drug to therapy, R3b—cease/withdraw therapy, R9a—start drug/supplement, R9b—review prescribed medications, R9c—change drug to a combination formulation, and R20—information for nursing staff. An explanation and example of each category of DRPs and recommendations are described in electronic supplementary material (ESM) Tables S1 and S2.
The prevalence of CKD was estimated by calculating the estimated GFR (eGFR) using the modification of diet in renal disease (MDRD) formula [17, 31], and residents with CKD were then categorised into five stages of CKD based on their eGFR [16]. These five stages are: stage 1—kidney damage with normal or increase in GFR (≥90 ml/min/1.73 m2); stage 2—kidney damage with mild decrease in GFR (60–89 ml/min/1.73 m2); stage 3—moderate decrease in GFR (30–59 ml/min/1.73 m2); stage 4—severe decrease in GFR (15–29 ml/min/1.73 m2); and stage 5—kidney failure (<15 ml/min/1.73 m2 or on dialysis). Stage 3 is subdivided into 3A (GFR 45–59 ml/min/1.73 m2) and 3B (GFR 30–44 ml/min/1.73 m2) [16].
The Australian Medicines Handbook (AMH) [32] has specific guidelines for dosage adjustments of renally cleared medications based on the creatinine clearance (CLCR) value and, therefore, it was used as a reference to determine the inappropriate prescribing of renally cleared medications in residents with CKD in whom the estimated CLCR (eCLCR) value could be calculated using the Cockroft–Gault (CG) formula [33]. Recommended dosing guidelines for renally cleared medications inappropriately prescribed in the study are described in ESM Table S3. The eGFR value based on the MDRD formula was used to assess the appropriateness of prescribing if weight was not recorded [31]. Also, DRPs identified and recommendations made by the accredited pharmacists for inappropriately prescribed renally cleared medications, and GP acceptance of these, were recorded.
2.4 Statistical Analysis
Data analysis was carried out using Microsoft Excel and Microsoft Access (Microsoft Corporation, Redmond, WA, USA). Descriptive statistics are presented as means. The inter-rater reliability of the DRP and recommendation coding was tested for 40 randomly selected cases by two study investigators (PAG. and RLC). The inter-rater reliability was assessed with Cohens’ Kappa using R 3.0 [34].
3 Results
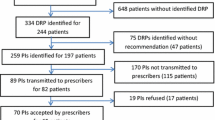
A total of 911 RMMR reports were provided by the medication review service provider. Sixty-four reports were excluded from the final analysis using the exclusion criteria shown in Fig. 1. Table 1 shows the characteristics of the study population at baseline. The mean (±SD) age of residents was 84.9 (8.8) years, and 31 % of residents were male. The mean (±SD) number of medical diagnoses identified per resident was 7.3 (2.9), and the mean (±SD) number of medications prescribed per resident was 11.2 (4.8).
3.1 Drug-Related Problems
Table 2 shows the various types of DRPs identified by the accredited pharmacists, classified according to the adapted version of the DOCUMENT system of classification. A total of 2,712 DRPs were identified by the pharmacists in 98 % of residents. The mean (±SD) number of DRPs identified per resident was 3.2 (1.7). Recommendations made by the pharmacists to resolve these DRPs were classified using the adapted version of the DOCUMENT system of classification, as shown in Table 3. Of 3,054 recommendations made, 2,560 (83.8 %) were accepted by the GP. The mean (±SD) number of recommendations made per resident by the pharmacist was 3.6 (1.9) and mean (±SD) number of recommendations accepted by the GP per resident was 3.0 (1.9). The inter-rater reliability assessed was high, with a Cohen’s Kappa statistic of k = 0.88 for DRP and k = 0.94 for recommendation.
3.2 Prevalence of Chronic Kidney Disease and Inappropriate Prescribing of Renally Cleared Medications
The prevalence of CKD was determined for residents with reported serum creatinine value using the MDRD formula. Overall, 154 (48 %) of 323 residents with reported serum creatinine value had CKD (eGFR below 60 ml/min/1.73 m2). RMMR reports of 18 residents did not have a serum creatinine value recorded; however, the eGFR value was recorded in the RMMR report, which confirmed that these residents had CKD. Therefore, a total of 172 residents of the aged care facilities were identified with CKD. Residents with CKD were then categorised into five stages based on the eGFR; of these, 76 (44 %) had stage 3A, 68 (39.5 %) had stage 3B, and 28 (16.3 %) had stage 4/5 CKD.
A serum creatinine value was not available for 524 (61.9 %) residents and, of these, 321 (61.2 %) residents were prescribed at least one renally cleared medication. Recommendations were made by the pharmacists in 94 (29.2 %) of these residents to monitor renal function, and 87 (92.5 %) of these recommendations were accepted by the GP. Twenty-eight residents who had CKD were inappropriately prescribed renally cleared medications. DRPs identified with respect to renally cleared medications and recommendations made by the pharmacists to resolve these are shown in Table 4. Twenty of 28 (71.4 %) recommendations were accepted by the GP.
4 Discussion
Inappropriate prescribing, which potentially leads to DRPs, is responsible for a significant burden on the healthcare system and is associated with risks of hospitalisation and death [8, 9, 11–13]. Over 98 % residents in this study were identified to have at least one DRP; similar to the 96 % identified by Nishtala et al. [26] and Finkers et al. [35]. The mean number of DRPs per resident (3.2) was also similar to Finkers et al.’s [35] value (3.5) of mean DRPs identified per resident. Most of the DRPs identified in this study were associated with the alimentary tract and metabolism, nervous system and cardiovascular system categories of the ATC classification system, and this finding is consistent with that of the previous studies [26, 36, 37].
This study used an adaptation of the DOCUMENT classification system to classify the DRPs and recommendations. Most of the problems identified by pharmacists were grouped as not classifiable (N0). This category of classification was used frequently when the reviewing pharmacist gave detailed information on a drug to the GP for consideration of further monitoring and review. The second most common category associated with DRPs was toxicity or adverse reaction (T1), and is defined as a situation when the patient is showing signs and symptoms of drug-associated adverse effects or toxicity. The most common nature of DRP identified in this study is different from the study by Nishtala et al. [26], which identified risk of ADR as the most frequent DRPs identified by reviewing pharmacists. Previous studies performed have specifically looked into inappropriate prescribing and associated ADE in aged care facility [36–38]; however, this study covers a broader range of DRPs encountered in aged care facilities.
Also, a high proportion (84 %) of recommendations made by accredited pharmacists in this study was accepted by GPs. The acceptance rate of pharmacists’ recommendations in this study was higher than the 74 % acceptance rate in the study by Nishtala et al. [26]. This finding was also higher compared with previous studies conducted in nursing homes in Australia and the US, which showed acceptance rates of 38 % [27] and 66 % [39], respectively. Most frequent recommendations made by the pharmacists in this study were R18 (monitoring: laboratory tests) followed by R9c (review prescribed medication), and the GP acceptance rate of these recommendations was also high. However, GPs seemed more reluctant to accept recommendations such as change the drug, decrease the dose of the drug and add drug to therapy; similar to the findings from the study by Nishtala et al. [26]. Although the exact reasons regarding the uptake of pharmacists’ recommendations are unclear, previous studies have highlighted several plausible explanations as to why GPs may be reluctant to accept pharmacists’ recommendations. These include suboptimal communication between specialists and GPs and inadequate models of shared care, which may result in GPs being reluctant to make changes to regimens initiated by specialists [40, 41]; the reluctance of GPs to change medications in residents who are stable and compliant [42]; and GPs balancing the risks of therapy against the clinical need for the drug [42].
This study showed that actual or potential DRPs are common among residents of Australian aged care facilities. Moreover, findings of this study suggest that accredited pharmacists can efficiently identify DRPs in residents of aged care facilities, and GPs acknowledge the majority of these recommendations. Thus, the pharmacist-conducted collaborative RMMR service with the GP can significantly reduce the number of actual or potential DRPs and has a high impact in improving the medication regimen for residents of aged care facilities in Australia.
This study estimated that 48 % of residents with a reported serum creatinine value had CKD, based on the MDRD formula. This finding is consistent with the 50 % identified by McClellan et al. [43] who also used the MDRD equation to determine the prevalence of CKD in aged care facility residents. The majority of residents (44 %) with CKD in this study were stage 3A, which was consistent with the findings of McClellan et al. [43] where 47.6 % of the study population with CKD had stage 3A.
This study found that serum creatinine values were not routinely recorded in the clinical notes for more than half of the residents of aged care facilities. Furthermore, a high proportion (61 %) of these residents was prescribed at least one renally cleared medication. It is possible that the resident would have previously had a serum creatinine test and the GP would have a record of this. However, this data was not available to the accredited pharmacists and requires careful attention as pharmacists would require relevant clinical chemistry data to assess the appropriate use of not only renally cleared medications but also other medications, such as for diabetes, heart disease, etc., in residents of aged care facilities. In addition, the residents’ height and weight was not recorded on a regular basis. Current guidelines recommend using the CG formula to guide dosing of renally cleared medications [31, 33]. For example, ‘number 3 metformin’ in Table 4 has an eCLCR value of 79 ml/min and an eGFR value of 116 ml/min/1.73 m2, and recommendation was made by the accredited pharmacist to reduce the dose of the prescribed drug based on the eCLCR value. Hence, it is important to record the weight in order to calculate the eCLCR so that dosage adjustment of renally cleared medications could be done accurately.
It is also important to note that recent studies have highlighted that there is inconsistency among drug information sources with regards to dosage adjustment in renal impairment [44–46]. Moreover, a recent study evaluating the product information of brands of the same drug highlighted the lack of consistency in the product information to guide prescribing in renal impairment [47]. This lack of consistency could create uncertainty and ambiguity among prescribers [44]. More recently, consensus guidelines have been published to aid prescribers to guide prescribing in renal impairment [48, 49].
Overall, the study found that pharmacists made recommendations to monitor kidney function in 29 % of residents who did not have a serum creatinine value recorded and were prescribed renally cleared medications. These 29 % of residents were considered high-risk for receiving a renally cleared medication based on their risk factors for CKD, such as diabetes, hypertension, etc., and therefore warrant a kidney function test. Almost 93 % of the recommendations to monitor kidney function were accepted by the GP. These findings reveal that kidney function of the aged care facility residents should be routinely monitored, and, if it is, then relevant pathology values should be routinely recorded in the clinical notes of aged care facility residents as this will allow the pharmacist to conduct the medication review services more efficiently and determine the appropriate use of renally cleared medications.
A total of 145 of 172 residents with CKD were prescribed at least one renally cleared medication. Of these, 28 (16 %) residents were inappropriately prescribed a renally cleared medication. This finding is lower than the 17.9 % identified by Hanlon et al. [14], and significantly lower than the 42 % and 46 % identified by Papaioannou et al. [22] and Rahimi et al. [15], respectively. There are many possible reasons for this, with the most likely being that the RMMR service is provided annually and, from the data collected for this study, it could not be determined whether an RMMR for a particular resident in previous years had been conducted. Our study and previous studies [24, 26] have shown that positive impact of the RMMR service is high; therefore, if any DRPs pertaining to renal impairment were identified by accredited pharmacists and implemented by the GP in previous years, it could not be recognised. Hence, research investigating the previous RMMR reports for inappropriate prescribing of renally cleared medications in aged care facilities would be of importance.
The most common inappropriately prescribed renally cleared medications identified in this study were metformin and perindopril. Metformin was also one of the common inappropriately prescribed renally cleared medications in the study by Papaioannou et al. [22]. These findings are very different from the American study conducted by Hanlon et al. [14], which found ranitidine, sulfamethoxazole/trimethoprim, ciprofloxacin and gabapentin as the most common inappropriately prescribed renally cleared medications.
4.1 Limitations
This was a retrospective study and the data collected for this study could not be validated for accuracy. The RMMR data collected from a single RMMR service provider was performed by approximately ten accredited pharmacists who received additional training by the RMMR service provider and, therefore, the DRPs identified and recommendations made by them could not be generalised for those identified by other accredited pharmacists nationally. Also, from the data provided for the purpose of this study, it could not be inferred whether the DRPs encountered in the residents were actual or potential; hence, all DRPs were classified using the adapted version of the DOCUMENT classification, which categorises DRPs irrespective of their actual or potential nature.
The RMMR data provided for this study were conducted between August 2011 and December 2012. However, this data did not contain information on whether the residents had previously received the RMMR service and if any changes had been made to their medication regimen based on a previous review. Therefore, this study may have under- or over-estimated the number of DRPs identified by accredited pharmacists, and also the number of residents identified with inappropriate prescribing of renally cleared medications. GPs’ acceptance of recommendations was investigated; however, actual implementation of these recommendations could not be estimated from the data collected for this study. Also, serum creatinine value, weight and height were not always recorded in the RMMR report for each resident, and information on the renal dosing guidelines or any explicit criterion used by the accredited pharmacists to guide dosage adjustments of renally cleared medications was not available; hence, this could not be investigated further for accuracy.
5 Conclusions
DRPs identified by accredited pharmacists in residents of aged care facilities are common, and the impact of the collaborative RMMR service is high. Also, CKD is common among residents of aged care facilities, and inappropriate prescribing of renally cleared medications is prevalent in this elderly group of people. However, serum creatinine values are not routinely recorded in the clinical notes of these residents even though renally cleared medications are commonly prescribed. Residents of aged care facilities should be regularly monitored for a decline in kidney function, and serum creatinine value should be routinely recorded.
References
Hamilton HJ, Gallagher PF, O’Mahony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatr. 2009;9:5. doi:10.1186/1471-2318-9-5.
Williams M, Peterson GM, Tenni PC, et al. DOCUMENT: a system for classifying drug-related problems in community pharmacy. Int J Clin Pharm. 2012;34(1):43–52. doi:10.1007/s11096-011-9583-1.
Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24. doi:10.1001/archinte.163.22.2716.
Beyth RJ, Shorr RI. Principles of drug therapy in older patients: rational drug prescribing. Clin Geriatr Med. 2002;18(3):577–92.
Walley T, Scott AK. Prescribing in the elderly. Postgrad Med J. 1995;71(838):466–71.
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14.
ElDesoky ES. Pharmacokinetic-pharmacodynamic crisis in the elderly. Am J Ther. 2007;14(5):488–98. doi:10.1097/01.mjt.0000183719.84390.4d.
Stafford AC, Alswayan MS, Tenni PC. Inappropriate prescribing in older residents of Australian care homes. J Clin Pharm Ther. 2011;36(1):33–44. doi:10.1111/j.1365-2710.2009.01151.x.
Castelino RL, Bajorek BV, Chen TF. Targeting suboptimal prescribing in the elderly: a review of the impact of pharmacy services. Ann Pharmacother. 2009;43(6):1096–106. doi:10.1345/aph.1L700.
Beers MH, Ouslander JG, Fingold SF, et al. Inappropriate medication prescribing in skilled-nursing facilities. Ann Intern Med. 1992;117(8):684–9.
Gill SS, Misiaszek BC, Brymer C. Improving prescribing in the elderly: a study in the long term care setting. Can J Clin Pharmacol. 2001;8(2):78–83.
O’Connor MN, Gallagher P, O’Mahony D. Inappropriate prescribing: criteria, detection and prevention. Drugs Aging. 2012;29(6):437–52. doi:10.2165/11632610-000000000-00000.
Ruggiero C, Dell’Aquila G, Gasperini B, et al. Potentially inappropriate drug prescriptions and risk of hospitalization among older, Italian, nursing home residents: the ULISSE project. Drugs Aging. 2010;27(9):747–58. doi:10.2165/11538240-000000000-00000.
Hanlon JT, Wang X, Handler SM, et al. Potentially inappropriate prescribing of primarily renally cleared medications for older veterans affairs nursing home patients. J Am Med Dir Assoc. 2011;12(5):377–83. doi:10.1016/j.jamda.2010.04.008.
Rahimi AR, Kennedy K, Thomason M, et al. Improper renal dosing in long-term care facilities. South Med J. 2008;101(8):802–5. doi:10.1097/SMJ.0b013e31817f1f71.
Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Stevens LA, Coresh J, Greene T, et al. Assessing kidney function: measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83. doi:10.1056/NEJMra054415.
Olyaei AJ, Steffl JL. A quantitative approach to drug dosing in chronic kidney disease. Blood Purif. 2011;31(1–3):138–45. doi:10.1159/000321857.
Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47. doi:10.1001/jama.298.17.2038.
Jose MD, Otahal P, Kirkland G, et al. Chronic kidney disease in Tasmania. Nephrology (Carlton). 2009;14(8):743–9. doi:10.1111/j.1440-1797.2009.01198.x.
Rothberg MB, Kehoe ED, Courtemanche AL, et al. Recognition and management of chronic kidney disease in an elderly ambulatory population. J Gen Intern Med. 2008;23(8):1125–30. doi:10.1007/s11606-008-0607-z.
Papaioannou A, Clarke JA, Campbell G, et al. Assessment of adherence to renal dosing guidelines in long-term care facilities. J Am Geriatr Soc. 2000;48(11):1470–3.
Department of Health. Medication Management Reviews/Residential Medication Management Review. 2013. http://www.health.gov.au/internet/main/publishing.nsf/Content/medication_management_reviews.htm. Accessed 30 Sep 2013.
Nishtala PS, Hilmer SN, McLachlan AJ, et al. Impact of residential medication management reviews on drug burden index in aged-care homes: a retrospective analysis. Drugs Aging. 2009;26(8):677–86. doi:10.2165/11316440-000000000-00000.
Pharmaceutical Society of Australia. Guidelines for pharmacists providing Residential Medication Management Review (RMMR) and Quality Use of Medicines (QUM). 2011. http://www.psa.org.au/aprc-residential-medication-review/unserstand-service-information. Accessed 30 Sep 2013.
Nishtala PS, McLachlan AJ, Bell JS, et al. A retrospective study of drug-related problems in Australian aged care homes: medication reviews involving pharmacists and general practitioners. J Eval Clin Pract. 2011;17(1):97–103. doi:10.1111/j.1365-2753.2010.01374.x.
Roberts MS, Stokes JA, King MA, et al. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. Br J Clin Pharmacol. 2001;51(3):257–65.
Zermansky AG, Alldred DP, Petty DR, et al. Clinical medication review by a pharmacist of elderly people living in care homes: randomised controlled trial. Age Ageing. 2006;35(6):586–91. doi:10.1093/ageing/afl075.
WHO Collaborating Centre for Drug Statistics Mthodology. Anatomical Therapeutic Chemical (ATC) Classification System. Norweigan Institute of Public Health. http://www.whocc.no/atc_ddd_publications/atc_ddd_index/. Accessed 25 Sep 2013.
WHO. International Classification of Diseases (ICD)-10, version 2010. http://www.who.int/classifications/icd/en/. Accessed 25 Sep 2013.
Stevens LA, Nolin TD, Richardson MM, et al. Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis. 2009;54(1):33–42. doi:10.1053/j.ajkd.2009.03.008.
Australian Medicines Handbook (AMH). Evidence-based independent medicines reference. 2014. https://shop.amh.net.au/. Accessed 21 July2014.
Faull R, Lee L. Prescribing in renal disease. Australian Prescriber. 2007. http://www.australianprescriber.com/magazine/30/1/17/20. Accessed 25 Sep 2013.
R Core Team (2013) R: A language for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.r-project.org/. Accessed 3 Oct 2013.
Finkers F, Maring JG, Boersma F, et al. A study of medication reviews to identify drug-related problems of polypharmacy patients in the Dutch nursing home setting. J Clin Pharm Ther. 2007;32(5):469–76. doi:10.1111/j.1365-2710.2007.00849.x.
Gurwitz JH, Field TS, Avorn J, et al. Incidence and preventability of adverse drug events in nursing homes. Am J Med. 2000;109(2):87–94.
Nguyen JK, Fouts MM, Kotabe SE, et al. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing home residents. Am J Geriatr Pharmacother. 2006;4(1):36–41. doi:10.1016/j.amjopharm.2006.03.002.
Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005;118(3):251–8. doi:10.1016/j.amjmed.2004.09.018.
Vlasses PH, Lucarotti RL, Miller DA, et al. Drug therapy review in a skilled nursing facility: an innovative approach. J Am Pharm Assoc. 1977;17(2):92–4.
Mandryk JA, Wai A, Mackson JM, et al. Evaluating the impact of educational interventions on use of antithrombotics in Australia. Pharmacoepidemiol Drug Saf. 2008;17(2):160–71. doi:10.1002/pds.1536.
Schoen C, Osborn R, Huynh PT, et al. Taking the pulse of health care systems: experiences of patients with health problems in six countries. Health Aff (Millwood). 2005;Suppl Web Exclusives:W5-509-25. doi:10.1377/hlthaff.w5.509.
Harding G, Wilcock M. Community pharmacists’ perceptions of medicines use reviews and quality assurance by peer review. Pharm World Sci. 2010;32(3):381–5. doi:10.1007/s11096-010-9381-1.
McClellan WM, Resnick B, Lei L, et al. Prevalence and severity of chronic kidney disease and anemia in the nursing home population. J Am Med Dir Assoc. 2010;11(1):33–41. doi:10.1016/j.jamda.2009.07.003.
Khanal A, Castelino RL, Peterson GM, et al. Dose adjustment guidelines for medications in patients with renal impairment: how consistent are drug information sources? Intern Med J. 2014;44(1):77–85. doi:10.1111/imj.12291.
Sweileh WM, Janem SA, Sawalha AF, et al. Medication dosing errors in hospitalized patients with renal impairment: a study in Palestine. Pharmacoepidemiol Drug Saf. 2007;16(8):908–12. doi:10.1002/pds.1412.
Decloedt E, Leisegang R, Blockman M, et al. Dosage adjustment in medical patients with renal impairment at Groote Schuur Hospital. S Afr Med J. 2010;100(5):304–6.
Khanal A, Peterson GM, Castelino RL, et al. Renal drug dosing recommendations: evaluation of product information for brands of the same drug. Intern Med J. 2014;44(6):591–6. doi:10.1111/imj.12446.
Hanlon JT, Aspinall SL, Semla TP, et al. Consensus guidelines for oral dosing of primarily renally cleared medications in older adults. J Am Geriatr Soc. 2009;57(2):335–40. doi:10.1111/j.1532-5415.2008.02098.x.
Desrochers JF, Lemieux JP, Morin-Belanger C, et al. Development and validation of the PAIR (Pharmacotherapy Assessment in Chronic Renal Disease) criteria to assess medication safety and use issues in patients with CKD. Am J Kidney Dis. 2011;58(4):527–35. doi:10.1053/j.ajkd.2011.04.020.
Acknowledgments
Pankti Gheewala, Gregory Peterson, Colin Curtain, Prasad Nishtala, Paul Hannan and Ronald Castelino have no potential conflicts of interests that are directly relevant to the content of this study. No sources of funding were used to assist in this study. Paul J. Hannan is a consultant for Meditrax Pty Ltd. The authors acknowledge Meditrax Pty Ltd and staff for providing de-identified medication reviews used in this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gheewala, P.A., Peterson, G.M., Curtain, C.M. et al. Impact of the Pharmacist Medication Review Services on Drug-Related Problems and Potentially Inappropriate Prescribing of Renally Cleared Medications in Residents of Aged Care Facilities. Drugs Aging 31, 825–835 (2014). https://doi.org/10.1007/s40266-014-0208-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0208-y