Abstract
Background
Polypharmacy, and specifically the use of multiple fall-risk-increasing drugs (FRID), have been associated with increased risk of falling in older age. However, it is not yet clear whether the known set of FRIDs can be extrapolated to recurrent fallers, since they form a distinct group of more vulnerable older persons with different characteristics.
Objectives
We aim to investigate which classes of medications are associated with recurrent falls in elderly patients visiting the Emergency Department (ED) after a fall.
Methods
This study had a cross-sectional design and was conducted in the ED of an academic medical center. Patients who sustained a fall, 65 years or older, and who visited the ED between 2004 and 2010 were invited to fill in a validated fall questionnaire designed to assess patient and fall characteristics (CAREFALL Triage Instrument [CTI]). We translated self-reported medications to anatomical therapeutic chemical (ATC) codes (at the second level). Univariate logistic regression analysis was performed to explore the association between medication classes and the outcome parameter (recurrent fall). Multivariate logistic regression was used to assess the associations after adjustment to potential confounders.
Results
In total 2,258 patients participated in our study, of whom 39 % (873) had sustained two or more falls within the previous year. After adjustment for the potential confounders, drugs for acid-related disorders (adjusted odds ratio [aOR] 1.29; 95 % CI 1.03–1.60), analgesics (aOR 1.22; 95 % CI 1.06–1.41), anti-Parkinson drugs (aOR 1.59; 95 % CI 1.02–2.46), nasal preparations (aOR 1.49; 95 % CI 1.07–2.08), ophthalmologicals (aOR 1.51; 95 % CI 1.10–2.09); antipsychotics (aOR 2.21; 95 % CI 1.08–4.52), and antidepressants (aOR 1.64; 95 % CI 1.13–2.37) remained statistically significantly associated with an ED visit due to a recurrent fall.
Conclusions
Known FRIDs, such as psychotropic drugs, also increase the risk of recurrent falls. However, we found four relatively new classes that showed significant association with recurrent falls. In part, these classes may act as markers of frailty and comorbidity, or they may reflect differences in the risk factors affecting the older, frailer population that tends to sustain recurrent falls. Further investigation is needed to elucidate causes and ways to prevent recurrent falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
About 30 % of people aged 65 years or older living in the community fall at least once annually, and up to 20 % fall twice or more [1–6]. Although not all falls lead to injury, approximately 20 % require medical attention and around 5 % result in (serious) injuries, such as fractures, dislocation of joints or other serious injuries [2, 4, 5, 7, 8]. Falls have been shown to lead to substantial loss of quality of life, mobility problems, loss of independence, and even mortality in the elderly population [4, 9–11]. In The Netherlands, between 2003 and 2007 annual healthcare costs due to falls were estimated at €474.4 million, which represents 21 % of total healthcare expenses due to injuries [4]. Falls therefore form a major health concern.
Falling in older age is often multifactorial [2, 12, 13]. Besides a history of previous falls, major risk factors include age, mobility and balance problems, and use of certain drugs. A recent meta-analysis again confirmed a significant association between falls and the use of sedatives and hypnotics, especially benzodiazepines, and also antidepressants in older individuals [14]. Furthermore, fall risk has been shown to be dependent on both number of fall-risk-increasing drugs (FRIDs) [16] and dose [15]. In patients with recurrent falls, a stronger association between medication use and falls may be hypothesized [16]. Although having history of falls is an important risk factor for recurrent falling [17], a first fall is often accidental. Nevertheless, only a minority of studies focused on a possible association between use of certain medications and recurrent falls [16–18]. This is of interest, since the underlying mechanisms may differ between single and multiple falls. First, some drugs may only increase initial fall risk, for example, medications that cause a transient orthostasis [19] that subsides after prolonged use. Furthermore, recurrent fallers are often older and frailer due to comorbidity and/or other risk factors, and therefore have a higher risk of sustaining further falls and fall-related injuries [20, 21]. Finally, in recurrent fallers, additive effects and interactions with other fall-risk factors like comorbidity and mobility may change the effect of individual drugs on fall risk. Since recurrent fallers are less likely to have sustained an accidental fall [22], they can benefit from targeted treatment and are in need of more stringent follow-up. This has important implications for fall-prevention programs/assessment. In the case of FRIDs, for example, potential beneficial effects have to be carefully weighed against expected adverse drug reactions, e.g. recurrent falls. Our aim in this study was therefore to investigate potential associations of medication and recurrent falls based on the anatomical therapeutic chemical (ATC) classes of medications.
2 Methods
2.1 Study Design and Patient Population
For the current study, we conducted a cross-sectional analysis of data from an observational cohort study among patients who were 65 years or older and presented after a fall to the Emergency Department (ED) of the academic medical center (AMC) in Amsterdam, The Netherlands, a 1,024-bed Tertiary University-Teaching Hospital. All patients gave informed consent for the use of the data for research purposes and the study was approved by the medical ethics committee of the AMC.
2.2 Source of Data
For this study, we used data that were gathered using the combined Amsterdam and Rotterdam evaluation of falls (CAREFALL) triage instrument (CTI) in our ED from July 2004 until July 2010. The CTI was developed on behalf of the Dutch National Fall Prevention Collaboration and consists of 44 questions to determine patient characteristics, the characteristics and possible cause(s) of the fall, and (modifiable) risk factors for falling (including self-reported medication use) [13]. The CTI was designed to identify risk factors for falls in the older population and has been shown to be an adequately valid and reliable instrument for assessing (modifiable) risk factors in older patients presenting to the ED after a fall. The validation of the CTI has been described elsewhere [23].
All charts of patients aged 65 years or over presenting to the ED were reviewed on a daily basis for fall incidents. Patients sustaining a fall received a letter with the CTI questionnaire (including an explanation) within 1 week. Patients not responding within 2 weeks were reminded by telephone to fill in the questionnaire.
2.3 Definition of (Recurrent) Falls
Fall incidents were defined as coming to rest unintentionally on the ground or a lower level with or without losing consciousness. Fall recurrence was defined as experiencing two or more falls within the past 12 months. This means having a fall incident(s) in the year preceding the injurious fall that led to the ED visit. Patients with falls due to acute medical factors such as myocardial infarction or cerebrovascular accident and those with dementia were excluded from this study.
2.4 Covariates
Covariates in our study included use of medications as well as fall risk factors as defined in the CTI (age, sex, vision problems, urinary incontinence, mood problems, mobility and balance problems, orthostatic hypotension symptoms, drinking alcohol, and weight less than 60 kg). Orthostatic hypotension and vasovagal collapse symptoms were scored as positive if the patient reported one or more instances of falling with symptoms consistent with these conditions. Impaired vision was scored as positive if the patient could not read a newspaper, or had significantly poor vision the last 6 months, or used reading glasses. Mood problems were scored as positive if the patient experienced less pleasure or interest in doing things, or felt gloomy. Mobility and balance problems were scored as positive if the patient had difficulty with walking, used a walking aid, had balance problems, experienced pain in his or her legs or felt stiffness, or had less feeling in his or her feet. Urinary incontinence was scored as positive if the patient was not able to hold urine or had to get up more than two times during the night to urinate.
2.5 Data Classification of Medication Use
Medication use in the CTI questionnaire was self-reported and recorded in free text, which we structured using the ATC classification system as described below. The ATC coding system structures medications on their therapeutic chemical components.
We manually looked up the generic name of the drug (trade) names, which were reported as free text, and subsequently linked these generic names with the ATC code using a computer program. This linking was obtained primarily based on the second level of the ATC classification, due to a lack of detailed information at higher levels (such as ATC level five). In cases where more specific information was present (ATC level three or four), this was coded as such. Besides analyzing the ATC second-level groups separately, we also grouped them clinically as ‘antihypertensives’, ‘sedatives and hypnotics’, ‘antidepressants’, and ‘benzodiazepines’ using the classification system presented in the meta-analysis of medications related to falls [14].
2.6 Statistical Analysis
Differences in variables between the single and recurrent fallers were tested using the χ 2 test, Student’s t-test or the Mann–Whitney test based on the variable’s distribution.
Univariate regression analyses for recurrent falls were performed to identify potential FRID classes. Each medication class with a p-value <0.2 was retained for further analysis. For each such medication, we identified the non-medication candidate covariates that changed the odds ratio (OR) of the medication by at least 10 % when entered into a multivariate logistic regression model containing the medication, age, and sex. These non-medication covariates are considered either candidate confounders, to be incorporated in the final model, or intermediates [24]. An intermediate was defined as any risk factor that represents a step in the causal chain between the exposure and outcome. To identify intermediates we checked whether a covariate was associated with the medication with a p-value ≤0.01, and asked our expert panel (consisting of two experienced geriatricians and one pharmacologist) to decide whether these covariates could reasonably be considered intermediates. All covariates not considered intermediates were considered as confounders. To reduce the number of covariates in the model we used stepwise variable selection based on Akaike’s information criterion [25]. All statistical analyses were carried out using the R statistical software environment version 2.11.1 (R Foundation for Statistical Computing, Vienna, Austria) and GraphPad Instat (GraphPad Software, Inc., CA, USA).
3 Results
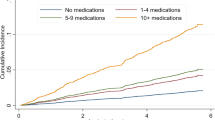
Our cohort consisted of 2,258 patients with an average age of 77.7 years (standard deviation [SD] 7.8 years); 873 patients had sustained two or more falls within 1 year (39 %). Table 1 shows the patient characteristics.
There were 46 ATC groups classified in the second level entered in the univariate analysis. This analysis showed a potential association with recurrent falls in 20 groups. Table 2 shows potential classes that were considered in the multivariate analysis (p < 0.2). In total, six ATC second-level groups of medication classes remained significant in the final multivariate regression analysis: drugs for acid-related disorders (A02), analgesics (N02), anti-Parkinson drugs (N04), psychoanaleptics (N06), nasal preparations for respiratory system (R01), and ophthalmologicals (S01). From the medication classes classified in the third-level ATC, antipsychotics (N05A), anxiolytics (N05B), hypnotics and sedatives (N05C), and antidepressants (N06A) were considered in our multivariate analysis (p < 0.2) (see Table 3). Antipsychotics (N05A) and antidepressants (N06A) showed significant association with recurrent falls in our population among the above-mentioned groups (see Table 3). An extended version of Table 2 is available as Electronic Supplementary Material, Table S1.
4 Discussion
In addition to reaffirming well known FRIDs such as antipsychotics, antidepressants, analgesics, and anti-Parkinson drugs, our results also showed that drugs for acid-related disorders, nasal preparations, and ophthalmologicals were associated with recurrent falls in a population consisting of patients who visited the ED due to a recurrent fall.
The identified association between antidepressants and recurrent falling is in line with previous studies [16, 17]. Furthermore, the association of anti-Parkinson drugs (N04) with recurrent falls is concordant with the study of Nevitt et al. [18]. They suggested that this was probably due to the problems in postural control associated with Parkinson’s disease [18]. The association we found could be at least partly due to the medications acting as a proxy for the disease itself, which is a risk factor for recurrent falls. Anti-Parkinson medications have side effects that could themselves be associated with falling, such as hypotension and orthostasis [19, 26]. Therefore, it is possible that the drugs themselves as well as the disease increase risk of falling, a relationship that merits further research. Adjusting for orthostatic hypotension symptoms reduced the OR for having the medication from 2.16 (95 % CI 1.41–3.32) to 1.85 (95 % CI 1.21–2.84). If the medication itself is the reason for increased fall risk, then therapy can better be started under the supervision of clinicians.
Analgesics showed an association, albeit small, with recurrent falling. The known adverse effects of opioid analgesics include a deterioration in mobility, diminished concentration, prolonged reaction time, impaired balance, and orthostatic hypotension [27]. In addition, it has been shown that withdrawal of opioid analgesics may be effective as an intervention for reducing risk of falls [27]. An additional analysis in our sample did show a significant association between non-opioid analgesics with recurrent falling (adjusted OR [aOR] 1.63; 95 % CI 1.28–2.08). Most opioid and non-opioid analgesics in our sample were tramadol and paracetamol, respectively.
Furthermore, we also showed a significant association with ophthalmologicals, which include anti-glaucoma medications. Aside from being a proxy for the fall-risk factor ‘poor vision,’ anti-glaucoma drugs could increase fall risk through systemic adverse effects. For example, anti-glaucoma drugs have a beta-blocking effect and can cause hypotension and bradycardia [28]. Eye drops may cause severe systemic adverse effects. The majority of the administered drop drains through the nasolacrimal duct, where it is absorbed by the nasal mucosa. Therefore, due to systemic spreading, and as there is no hepatic first-pass effect, the absorbed dose behaves like an intravenous drug dose. No significant association was found in a small cross-sectional observational study assessing the effect of long-term use of beta-blocker eye drops and falls, dizziness, or orthostatic hypotension in older ophthalmic outpatients, compared with long-term use of prostaglandin eye drops [29]. Potentially this was caused by a subsidence of the initial orthostatic effect, but this is not a common effect of chronic beta-blocker use. It is more likely that this finding was due to, among other things, bias by contraindication, e.g. patients with higher fall risk and orthostatic hypotension were more likely to be prescribed prostaglandin eye drops or switched when a side effect occurred. However, beta-blocking eye drops can potentially cause orthostasis, hypotension, and bradycardia, and caution has been advised when using them in elderly patients [28].
The finding that drugs for acid-related disorders increased the risk of recurrent falling is relatively new. The potential underlying causal relationship could be due to electrolyte disorders, muscle weakness, or dizziness caused by the use of these medications. Some classes of medications for acid-related disorders, such as proton pump inhibitors (PPIs), are among the most prescribed medications and are much more commonly used among individuals with indicators of frailty, including polypharmacy and higher levels of overall comorbidity [30, 31]. PPIs have been associated with fracture and decreased bone density [30, 32]. Through this mechanism, serious falls (e.g. those leading to fracture) could also be associated with use of this medication.
To our surprise, we found no association between the anxiolytics and hypnotics and sedatives with recurrent falls. This is perhaps because self-reported use of sedatives is under-reported, partly because patients may not consider their sleeping medication as a drug, or because they may not use it on a daily basis.
Finally, another unexpected finding was the association with nasal preparations (e.g. treatment of asthma or allergic rhinitis). The sedative effects of these (antihistaminic) drugs most likely underlie the associated fall risk. Moreover, patients who use these medications could have poorer pulmonary function, which is connected with overall vulnerability, sarcopenia, and disability. In a study by Koski et al. [33], poor pulmonary function was found to be a possible risk factor for injurious falling. Although all mentioned potential mechanisms could clarify the association between these medications and recurrent falling, more research is needed to gain stronger evidence of such an association.
For vitamins, anti-anemic preparations, and antibacterials for systemic use, we considered mobility and balance problems as a confounder because we do not think that they act as an intermediate in the causal pathway corresponding to these medications. Without adjusting for mobility and balance problems in the final models, these medications have significant association with recurrent falling, but it is probable that the medications act as proxies for illness and hence adjustment seems justified. More research is needed to determine whether or not these groups are truly associated with recurrent falling.
Our study is the largest study exclusively focusing on the association between medications and recurrent falls in elderly patients. In addition, the self-reported drug use is likely to better represent actual, not only prescribed, use. Nevertheless, our study also has some limitations. First, we did not know for which specific medical reasons the reported medications were prescribed, which could affect the ATC coding and hinder adjusting for these specific reasons. However, the (side) effect of the medication will not change due to a different ATC coding. In addition, we were not able to consider the period of exposure to a certain drug due to a lack of this information. However, these are the medications the patient was taking at the time the fall occurred, and it is likely that most medications had been used for some time before the fall occurred. Second, our study had a cross-sectional observational design; therefore, establishing a causal relation is not possible. Some of these correlations may reflect the frailty of the patients rather than a direct relationship with recurrent falls. Third, our evidence was based solely on medication names reported by the patients without information on dosage or therapy duration. Fourth, although the CTI has been validated for recurrent falls, the risk of recall bias is still present [23]. The registration of recurrent falls may therefore be susceptible to misclassification. Finally, this study cannot rule out confounding by indication, nevertheless we were partly able to correct for this by including covariates addressing geriatric conditions such as poor mobility and vision.
5 Conclusion
Although the benefit of a FRID will sometimes outweigh the risk, clinicians should be aware of potential risks of recurrent falls due to the use of drugs from certain medication classes. It appears that some FRIDs increase not only the initial risk of falls but also carry lasting increased fall risk even compared with the risk of single falls. In this study, we showed four relatively new FRID classes associated with recurrent falls. In part, these classes may act as markers of frailty and comorbidity, or they may reflect differences in the risk factors affecting the older, frailer population that tends to sustain recurrent falls. Further investigation, preferably in prospective cohorts, is needed to elucidate causes and ways to prevent recurrent falls, including FRID withdrawal.
References
Tromp AM, Smit JH, Deeg DJ, Bouter LM, Lips P. Predictors for falls and fractures in the longitudinal aging study Amsterdam. J Bone Miner Res. 1998;13(12):1932–9.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7.
Blake AJ, Morgan K, Bendall MJ, Dallosso H, Ebrahim SB, Arie TH, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17(6):365–72.
Hartholt KA, van Beeck EF, Polinder S, van der velde N, van Lieshout EM, Panneman MJ, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma. 2011;71(3):748–53.
Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med. 1989;320(16):1055–9.
Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55(11):1088–94.
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–93.
Stalenhoef PA, Crebolder H, Knottnerus JA, van der Horst FGEM. Incidence, risk factors and consequences of falls among elderly subjects living in the community. A criteria-based analysis. Eur J Public Health 1997;7(3):328–34.
Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Jarvinen M, et al. Fall-induced injuries and deaths among older adults. JAMA. 1999;281(20):1895–9.
Tidermark J, Zethraeus N, Svensson O, Tornkvist H, Ponzer S. Quality of life related to fracture displacement among elderly patients with femoral neck fractures treated with internal fixation. 2002. J Orthop Trauma. 2003; 17(8 Suppl):S17–21.
Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. 2004;33(1):58–65.
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006; 35 Suppl 2:ii37–41.
van Nieuwenhuizen RC, van der Velde N, van Breda FG, Scheffer AC, Korevaar JC, van der Cammen TJ, et al. Assessing the prevalence of modifiable risk factors in older patients visiting an ED due to a fall using the CAREFALL triage instrument. Am J Emerg Med. 2010;28(9):994–1001.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–60.
Sterke CS, van Beeck EF, van der Velde N, Ziere G, Petrovic M, Looman CW, et al. New insights: dose-response relationship between psychotropic drugs and falls: a study in nursing home residents with dementia. J Clin Pharmacol. 2012;52(6):947–55.
Cumming RG, Miller JP, Kelsey JL, Davis P, Arfken CL, Birge SJ, et al. Medications and multiple falls in elderly people: the St. Louis OASIS study. Age Ageing. 1991;20(6):455–61.
Luukinen H, Koski K, Laippala P, Kivela SL. Predictors for recurrent falls among the home-dwelling elderly. Scand J Prim Health Care. 1995;13(4):294–9.
Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. JAMA. 1989;261(18):2663–8.
Kujawa K, Leurgans S, Raman R, Blasucci L, Goetz CG. Acute orthostatic hypotension when starting dopamine agonists in Parkinson’s disease. Arch Neurol. 2000;57(10):1461–3.
Fang X, Shi J, Song X, Mitnitski A, Tang Z, Wang C, et al. Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing longitudinal study of aging. J Nutr Health Aging. 2012;16(10):903–7.
Tom SE, Adachi JD, Anderson FA Jr, Boonen S, Chapurlat RD, Compston JE, et al. Frailty and fracture, disability, and falls: a multiple country study from the global longitudinal study of osteoporosis in women. J Am Geriatr Soc. 2013;61(3):327–34.
Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57(3):492–8.
Boele van Hensbroek P, van Dijk N, van Breda GF, Scheffer AC, van der Cammen TJ, Lips P et al. The CAREFALL triage instrument identifying risk factors for recurrent falls in elderly patients. Am J Emerg Med 2009; 27(1):23–36.
Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–9.
Burnham KP, Anderson DR. Model selection and multimodel inference: a practical-theoretic approach. 2nd ed. Berlin: Springer; 2012.
Jenner P. Pharmacology of dopamine agonists in the treatment of Parkinson’s disease. Neurology. 2002;58(4 Suppl 1):S1–8.
Van der Velde N, Stricker BH, Pols HA, van der Cammen TJ. Withdrawal of fall-risk-increasing drugs in older persons: effect on mobility test outcomes. Drugs Aging. 2007;24(8):691–9.
Muller ME, van der velde N, Krulder JW, van der Cammen TJ. Syncope and falls due to timolol eye drops. BMJ. 2006;332(7547):960–1.
Ramdas WD, van der velde N, van der Cammen TJ, Wolfs RC. Evaluation of risk of falls and orthostatic hypotension in older, long-term topical beta-blocker users. Graefes Arch Clin Exp Ophthalmol. 2009;247(9):1235–41.
Targownik LE, Leslie WD, Davison KS, Goltzman D, Jamal SA, Kreiger N, et al. The relationship between proton pump inhibitor use and longitudinal change in bone mineral density: a population-based from the Canadian Multicentre Osteoporosis Study (CaMos). Am J Gastroenterol. 2012;107(9):1361–9.
Teramura-Gronblad M, Hosia-Randell H, Muurinen S, Pitkala K. Use of proton-pump inhibitors and their associated risks among frail elderly nursing home residents. Scand J Prim Health Care. 2010;28(3):154–9.
Kwok CS, Yeong JK, Loke YK. Meta-analysis: risk of fractures with acid-suppressing medication. Bone. 2011;48(4):768–76.
Koski K, Luukinen H, Laippala P, Kivela SL. Physiological factors and medications as predictors of injurious falls by elderly people: a prospective population-based study. Age Ageing. 1996;25(1):29–38.
Acknowledgments
MA, SE, and NVV conceived the study and study design. AS collected the data. AA and SR coordinated the study. MA carried out the data analysis under supervision of AA, NVV, and SE. MA drafted the manuscript. All authors participated in the design, interpreted the data, steered the analysis, and critically read and revised the manuscript. All authors read and approved the final manuscript. The authors thank Karlijn van Stralen (epidemiologist) for her methodological advice.
Conflict of interest
The authors declare that they have no conflicts of interest. No information reported in this manuscript has been previously presented. This research was partly funded by ZonMw (The Netherlands Organization for Health Research and Development) by Grants for the PROFIT (#300020010) and ICOVE (#311020302) projects.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Askari, M., Eslami, S., Scheffer, A.C. et al. Different Risk-Increasing Drugs in Recurrent versus Single Fallers: Are Recurrent Fallers a Distinct Population?. Drugs Aging 30, 845–851 (2013). https://doi.org/10.1007/s40266-013-0110-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-013-0110-z