Abstract
Background
The number of elderly and the prevalence of dementia have grown considerably in recent years. Little is known about how aging and dementia affect care patterns after discharge for acute coronary syndrome (ACS).
Objective
This study was designed to assess the impact of dementia on care patterns after admission for patients with ACS across different age groups.
Methods
Of 87,321 patients hospitalized for ACS between 1 January 2006 and 31 December 2007, 1,835 patients with dementia and 3,670 matched patients without dementia (1:2 ratio, matched by age, sex and hospital level) were identified from Taiwan’s National Health Insurance Research Database. Use of interventional therapies at hospitalization and guideline-recommended medications post-discharge were compared between patients with and without dementia across different age groups (≤65, 66–75, 76–85, ≥86 years). Multivariate logistic regression models were performed to examine the impact of dementia on care patterns.
Results
Overall, dementia was associated with a 27 % lower likelihood of receipt of interventional therapies [adjusted odds ratio (OR) = 0.73; 95 % CI 0.63, 0.83] and a 22 % lower likelihood of guideline-recommended medications (adjusted OR = 0.78; 95 % CI 0.68, 0.89) in ACS patients. The use of interventional therapies and guideline-recommended medications decreased with age, and interactions between age and dementia were found. The proportions of patients receiving interventional therapies were 39.4 % (without dementia) versus 21.8 % (with dementia) in the youngest age group and 18.6 % (without dementia) versus 14.5 % (with dementia) in the oldest age group. Patients with dementia (age ≤65 years 73.6 %; age 66–75 years 82.3 %; age 76–85 years 71.8 %; age ≥86 years 55.6 %) were less likely to receive guideline-recommended medications as compared with those without dementia (age ≤65 years 85.6 %; age 66–75 years 87.5 %; age 76–85 years 81.2 %; age ≥86 years 62.0 %).
Conclusion
Dementia and aging were associated with decreased use of interventional therapies and guideline-recommended medications in ACS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Clinical guidelines have supported the beneficial effects of interventional (such as percutaneous coronary interventions) and medical therapies [such as aspirin, β-blockers (β-adrenoceptor antagonists), angiotensin-converting enzyme inhibitors (ACEIs), statins (HMG-CoA reductase inhibitors) and clopidogrel] for reducing the risks of morbidity and mortality in acute coronary syndrome (ACS) patients [1–5]. Increasing evidence, including the 1999/2000 American College of Cardiology (ACC) and American Heart Association (AHA) guidelines, has further suggested that older patients might benefit more from these guideline-recommended therapies than younger patients would [6–8]. However, studies have consistently revealed the decreased use of these therapies in ACS patients [9, 10], especially in the elderly population [11–16].
Studies have reported that the decreased use of these therapies in ACS patients may be attributed to patient demographic variables or comorbidities [12, 13, 17–20]. Because of the increasing prevalence of dementia in the elderly population [21, 22], significant concerns have been raised about its impact on care patterns in this group. However, most available data lack generalizability either because of the very small sample size of dementia patients (n = 22 and 62) [23, 24] or because the studies evaluated ACS patients enrolled in the early 1990s before the release of the updated ACC/AHA guidelines [25, 26]. In addition, most randomized controlled trials that have been conducted since the release of the current ACC/AHA guidelines have not included older adults or people with dementia. Therefore, quantification of the impacts of dementia on care patterns in patients after their ACS events would be relevant to both clinical practice and policy making in the provision of better care in the elderly population.
Using the 2005–2008 Taiwan National Health Insurance Research Database (NHIRD), the objective of this study was to assess the differences between care patterns for ACS patients with and without dementia. In addition, this study examined the interactions of age and dementia on the care patterns of ACS patients.
2 Methods
We conducted a nationwide, retrospective, population-based cohort study of patients hospitalized for ACS between 1 January 2006 and 31 December 2007. Our data were obtained from the 2005–2008 Taiwan NHIRD. The NHIRD includes all claims data of outpatient and inpatient visits from the National Health Insurance (NHI) programme in Taiwan, which covers over 99 % of the entire Taiwanese population (23.7 million people). Because the NHIRD is converted to a de-identified dataset before its release to the public for research purposes, the study was exempt from full review by the National Taiwan University Hospital institutional review board.
2.1 Study Population
We identified patients who had their first hospitalization for ACS between 1 January 2006 and 31 December 2007 (N = 111,347) from the NHIRD. Patients with ACS were defined as those who had primary discharge diagnosis codes of 410.xx, 411.xx or 414.xx based on the International Classification of Diseases, Ninth Revision—Clinical Modification (ICD-9-CM) codes [27]. Patients who were previously admitted to hospitals because of ACS in 2005, were less than 18 years old or had an unknown discharge date for the first ACS event were excluded from our study. The persons who met the inclusion criteria were further categorized into those with dementia (n = 1,835) and those without dementia (n = 85,323).
Patients with dementia were defined as those who had at least three ambulatory claim records or one inpatient record with dementia-related diagnosis codes [ICD-9-CM codes: 290.0 (senile dementia, uncomplicated), 290.1x (presenile dementia), 290.2x (senile dementia with delusional or depressive features), 290.3 (senile dementia with delirium), 290.4x (arteriosclerotic dementia), 294.1 (dementia in conditions classified elsewhere), 331.0 (Alzheimer’s disease), 331.1 (Pick’s disease) and 331.2 (senile degeneration of the brain)] before their first ACS event. This definition was adopted from a previous study on dementia using the NHIRD in Taiwan [28]. Medications used for dementia within 365 days prior to the first ACS event, including memantine, donepezil, rivastigmine and galantamine, were also recorded to characterize the treatments of dementia patients.
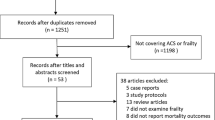
To account for potential confounders between patients with and without dementia, a matched cohort from those without dementia was selected for every patient with dementia. We took into consideration age, sex and provider sites (medical centre, regional hospital, local hospital and others) in creating the matched cohort. The final study cohort included 1,835 ACS patients with dementia and 3,670 ACS patients without dementia at a 1:2 ratio (Fig. 1).
2.2 Outcome Measurements
Interventional therapies, including percutaneous transluminal coronary angioplasty (PTCA) with/without a stent (defined by ICD-9-CM procedure codes 3601, 3605 or 3606) and coronary artery bypass graft (CABG) (ICD-9-CM procedure codes 3611–3616) during the first ACS event, were our primary outcome of interest. Secondary outcomes included use of guideline-recommended medications, such as aspirin, β-blockers, ACEIs or angiotensin receptor blockers (ARBs), statins and clopidogrel, for at least 30 days or for at least 180 days within 365 days after the first ACS event.
2.3 Statistical Analysis
Differences in baseline characteristics between patients with and without dementia were compared using Chi-squared tests and t-tests. Multivariate logistic regression models were constructed to examine the relationships between the diagnosis of dementia in ACS patients and the use of interventional therapies and guideline-recommended medications. Multivariate logistic regression models were adjusted for patient demographics, prior medical histories (hypertension, hyperlipidaemia, diabetes mellitus, cerebrovascular disease, renal disease, heart failure, peripheral vascular disease, ischaemic heart disease, peptic ulcer and gastrointestinal bleeding), procedures (PTCA, PTCA with stent, and CABG) performed at the index ACS event, and medications [aspirin, β-blockers, ACEIs, ARBs, statins, nonsteroidal anti-inflammatory drugs (NSAIDs) and cyclo-oxygenase (COX)-2 inhibitors] received when patients were discharged after the index event. Four separate logistic regression models were used to analyse the effect of age (≤65, 66–75, 76–85 and ≥86 years) on the association between dementia and interventional therapies and guideline-recommended medications. All tests were two-sided, and an alpha level of 0.05 was considered statistically significant. All analyses were performed using SPSS software, version 17.0 (SPSS Inc., Chicago, IL, USA) or SAS software version 9.1 (SAS Institute, Cary, NC, USA).
3 Results
In the original cohort, there were 1,835 ACS patients with dementia and 85,323 ACS patients without dementia. The prevalence rate of dementia was 2.1 % in ACS patients in this study. In the original cohort, those with dementia were older and had a higher prevalence rate of cerebrovascular disease, heart failure and peptic ulcer but were less likely to have a history of hypertension, hyperlipidaemia, diabetes, ischaemic heart disease and liver disease than those without dementia (Table 1). The two groups were balanced in the matched cohort in terms of age [79.1 ± 8.8 (mean ± SD) years in the dementia group vs. 78.8 ± 9.3 (mean ± SD) years in the group without dementia] and distributions of sex, provider sites and most of the baseline characteristics (Table 1). However, a slightly higher proportion of patients without dementia had comorbidities of hypertension, hyperlipidaemia and ischaemic heart diseases. Similar results were found after dividing these patients into four different age groups (Table 2).
Compared with the ACS patients without dementia, interventional therapies during hospitalization and guideline-recommended medications post-discharge were less likely to be used in those with dementia (Table 3). Overall, the proportions of patients receiving interventional therapies were 11.5 % in patients without dementia and 6.4 % in patients with dementia. Multivariable logistic regression analysis revealed that dementia was associated with a 27 % lower likelihood of receipt of interventional therapies [adjusted odds ratio (OR) = 0.73; 95 % CI 0.63, 0.83] in ACS patients. The majority of our study cohort was prescribed one of the listed guideline-recommended medications, but the proportion of patients with dementia (70.8 %) receiving these medications was lower than the proportion of those without dementia who received these drugs (78.7 %) (adjusted OR = 0.78; 95 % CI 0.68, 0.89). Among all guideline-recommended medications, aspirin had the highest use (60.8 % patients without dementia vs. 50.0 % with dementia), and statins had the lowest use (29.8 % patients without dementia vs. 18.0 % with dementia). Except for the use of clopidogrel, dementia was statistically associated with decreased uses of aspirin (adjusted OR = 0.84; 95 % CI 0.74, 0.94), β-blockers (adjusted OR = 0.78; 95 % CI = 0.69, 0.89), ACEIs or ARBs (adjusted OR = 0.79; 95 % CI 0.70, 0.89) and statins (adjusted OR = 0.68; 95 % CI 0.58, 0.79).
The proportion of ACS patients receiving interventional therapies and guideline-recommended medications also decreased with age (Table 3). The proportions of patients receiving interventional therapies were 39.4 % (without dementia) versus 21.8 % (with dementia) in the youngest age group and 18.6 % (without dementia) versus 14.5 % (with dementia) in the oldest age group. The impact of dementia on receiving interventional therapies in ACS patients was the most pronounced in patients less than 65 years old (adjusted OR = 0.43; 95 % CI 0.25, 0.75) but was not statistically significant in patients aged 86 years and older (adjusted OR = 0.83; 95 % CI 0.59, 1.19). Over 80 % of ACS patients without dementia received guideline-recommended medications (age ≤65 years 85.6 %; age 66–75 years 87.5 %; age 76–85 years 81.2 %), although the proportion decreased to 60 % in patients aged 86 years and older. Again, patients with dementia were less likely to receive guideline-recommended medications (age ≤65 years 73.6 %; age 66–75 years 82.3 %; age 76–85 years 71.8 %; age ≥86 years 55.6 %).
In the sensitivity analyses, in which the use of guideline-recommended medications was redefined as at least 180 days’ use within 365 days after the first ACS event, the proportion of patients receiving these medications decreased from 78.7 to 48.4 % in patients without dementia and from 70.8 to 41.3 % in patients with dementia. Similar results were observed across all age groups. Based on this definition of drug use, the proportions of our study cohorts who received guideline-recommended medications decreased dramatically. For example, only 11.1 % of patients without dementia and 6.9 % of patients with dementia received statins (Table 4).
4 Discussion
From our results, after ACS events, older patients were less likely to receive interventional therapies and guideline-recommended medications. Patients who were aged 86 years and older were least likely to receive those treatments. In addition, the care pattern of ACS patients with dementia differed from the care pattern of patients without dementia. Dementia was associated with decreased use of interventional therapies and guideline-recommended medications in the ACS population.
Previous studies have reported an inverse association between age and use of interventional therapies and guideline-recommended medications in the ACS population [6, 7, 11, 12, 15]. Furthermore, our study adds to the literature by showing the care patterns across different age groups in older ACS patients. While the universal coverage of the NHI programme in Taiwan guaranteed a greater than 80 % use of guideline-recommended medications in ACS patients between the ages of 65 and 85 years (without dementia), only 60 % of those who were aged 86 years and older received these medications. These results may thus support some explanations from previous studies that attitudes of providers and patients might in fact lead to lower service use [11].
In addition to age, dementia affects the use of invasive procedures, such as PTCA or CABG, and the use of aspirin, β-blockers, ACEIs and ARBs, and statins. Our study found that dementia was associated with a decreased likelihood of undergoing invasive procedures (adjusted OR = 0.73; 95 % CI 0.63, 0.83) or receiving guideline-recommended medications (adjusted OR = 0.78; 95 % CI 0.68, 0.89), which was consistent with results reported in one study performed in a US Medicare population [coronary angioplasty: relative risk (RR) = 0.58; 95 % CI 0.51, 0.66; cardiac bypass surgery: RR = 0.41; 95 % CI 0.33, 0.50; and receipt of an ACEI: RR = 0.90; 95 % CI 0.86, 0.95] [17, 26]. Moreover, our study revealed that dementia might have different impacts on the use of these interventions in different age groups of ACS patients. The impacts of dementia on the care patterns of ACS patients, especially on the receipt of invasive procedures, was more pronounced in the younger population than in the older population [age ≤65 years OR = 0.43 (95 % CI 0.25, 0.75) vs. age ≥86 years OR = 0.83 (95 % CI = 0.59, 1.19)]. This raises the question of what the appropriate treatments for dementia patients after their ACS events are, while considering both costs and benefits to these patients.
Although our study found that dementia and aging were associated with decreased use of interventional therapies and guideline-recommended medications in ACS patients, these did not simply imply ‘suboptimal’ care or ‘underutilization’ for several reasons. First, existing guidelines are mostly based on randomized controlled trials, from which elderly or dementia patients are usually excluded. Second, some ACS patients with dementia may be approaching the end of life, and the priority of their care would be quality of life, not mortality or morbidity. Furthermore, these patients may be vulnerable to the adverse effects of the guideline-recommended medications, and the risks of the medications might outweigh the benefit of them. In addition, disease-specific guidelines often do not take into account multiple comorbid conditions and geriatric syndromes that occur frequently in the elderly [8]. Suggestions from different guidelines might be conflicting and result in drug–drug or drug–diseases interactions. Therefore, treatments for the elderly should be holistic and take into account heterogeneous health statuses with variable life expectancies, multiple comorbidities, patient preferences, goals of care and quality of life [29].
Results from our sensitivity analyses indicated that these patients might not only be less likely to receive guideline-recommended medications but might also have the potential to discontinue these therapies if the ‘definition’ of use was based on at least 180 days’ use within 365 days after the ACS hospitalization. Because persistence in the use of these medical therapies is necessary to achieve expected decreases in cardiovascular morbidity and mortality in ACS patients [1–5], more studies are warranted to determine the potential reasons for discontinuation. This will be particularly important for patients with dementia, as functional status is believed to be one of the key factors associated with the discontinuation of treatments [30].
Our findings should be interpreted in the context of the following limitations. First, identification of diagnoses of ACS, dementia or any other comorbid medical condition was dependent on the ICD-9-CM codes. This is a limitation of studies using claims data compared with studies using a standardized diagnostic approach. However, the Bureau of National Health Insurance in Taiwan interviews patients and reviews charts from random samples for a certain percentage of medical claims from every hospital each year to verify the validity of disease diagnoses. Second, the definitions of dementia cases were based on ICD-9-CM codes. Dementia severity was therefore not available in our study. In addition, measures of patients’ activities of daily living were not available in the claim-based NHIRD. However, the prevalence rate of dementia is 2.1 % in ACS patients in our study, which was comparable with the rates reported in studies conducted in the USA [4.5 % in acute myocardial infarction (AMI) patients] and Japan (2.1–3.4 % dementia in AMI patients) [23, 24, 26]. Third, social history (such as smoking) and clinical presentation of ACS were not included in the claim-based NHIRD. Despite these limitations, our empirical findings found that dementia was associated with decreased utilization of interventional therapies and guideline-recommended medications in the ACS population. In addition, the impact of dementia may be more pronounced in the younger population than in the elderly population.
5 Conclusion
Dementia and aging were associated with decreased use of interventional therapies and guideline-recommended medications in ACS patients. With the increasing prevalence of dementia, more effort should be invested in formulating optimal care procedures for ACS in this population to avoid cardiovascular morbidity, mortality and negative effects on quality of life.
References
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494–502.
Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318(7200):1730–7.
ACE Inhibitor Myocardial Infarction Collaborative Group. Indications for ACE inhibitors in the early treatment of acute myocardial infarction: systematic overview of individual data from 100,000 patients in randomized trials. Circulation. 1998;97(22):2202–12.
Dagenais GR, Pogue J, Fox K, Simoons ML, Yusuf S. Angiotensin-converting-enzyme inhibitors in stable vascular disease without left ventricular systolic dysfunction or heart failure: a combined analysis of three trials. Lancet. 2006;368(9535):581–8.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78.
Soiza RL, Leslie SJ, Harrild K, Peden NR, Hargreaves AD. Age-dependent differences in presentation, risk factor profile, and outcome of suspected acute coronary syndrome. J Am Geriatr Soc. 2005;53(11):1961–5.
Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005;149(1):67–73.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–24.
Margulis AV, Choudhry NK, Dormuth CR, Schneeweiss S. Variation in initiating secondary prevention after myocardial infarction by hospitals and physicians, 1997 through 2004. Pharmacoepidemiol Drug Saf. 2011;20(10):1088–97.
Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–43.
Schoenenberger AW, Radovanovic D, Stauffer JC, Windecker S, Urban P, Eberli FR, et al. Age-related differences in the use of guideline-recommended medical and interventional therapies for acute coronary syndromes: a cohort study. J Am Geriatr Soc. 2008;56(3):510–6.
Yan RT, Yan AT, Tan M, Chow CM, Fitchett DH, Ervin FL, et al. Age-related differences in the management and outcome of patients with acute coronary syndromes. Am Heart J. 2006;151(2):352–9.
Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27(7):789–95.
Barchielli A, Buiatti E, Balzi D, Santoro GM, Carrabba N, Fabiani P, et al. Age-related changes in treatment strategies for acute myocardial infarction: a population-based study. J Am Geriatr Soc. 2004;52(8):1355–60.
Rathore SS, Mehta RH, Wang Y, Radford MJ, Krumholz HM. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am J Med. 2003;114(4):307–15.
Mehta RH, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38(3):736–41.
Brogan GX Jr, Peterson ED, Mulgund J, Bhatt DL, Ohman EM, Gibler WB, et al. Treatment disparities in the care of patients with and without diabetes presenting with non-ST-segment elevation acute coronary syndromes. Diabetes Care. 2006;29(1):9–14.
Bugiardini R, Yan AT, Yan RT, Fitchett D, Langer A, Manfrini O, et al. Factors influencing underutilization of evidence-based therapies in women. Eur Heart J. 2011;32(11):1337–44.
Hasdai D, Haim M, Behar S, Boyko V, Battler A. Acute coronary syndromes in patients with prior cerebrovascular events: lessons from the Euro-Heart Survey of Acute Coronary Syndromes. Am Heart J. 2003;146(5):832–8.
Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003;42(2):201–8.
World Alzheimer Report: the global economic impact of dementia. London: Alzheimer’s Disease International (ADI). 2010.
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–7.
Kimata T, Hirakawa Y, Uemura K, Kuzuya M. Absence of outcome difference in elderly patients with and without dementia after acute myocardial infarction. Int Heart J. 2008;49(5):533–43.
Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Uemura K. Differences in cardiac management and in-hospital mortality between elderly patients with and without dementia after acute myocardial infarction: findings from TAMIS data. Nippon Ronen Igakkai Zasshi. 2007;44(5):606–10.
Cordero A, Morillas P, Bertomeu-González V, Quiles J, Soria F, Guindo J, et al. Pathological ankle-brachial index is equivalent of advanced age in acute coronary syndromes. Eur J Clin Invest. 2011;41(12):1268–74.
Sloan FA, Trogdon JG, Curtis LH, Schulman KA. The effect of dementia on outcomes and process of care for Medicare beneficiaries admitted with acute myocardial infarction. J Am Geriatr Soc. 2004;52(2):173–81.
International classification of diseases, ninth revision (ICD-9). Geneva: World Health Organization; 2011.
Wu CS, Ting TT, Wang SC, Chang IS, Lin KM. Effect of benzodiazepine discontinuation on dementia risk. Am J Geriatr Psychiatry. 2011;19(2):151–9.
Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003; (5 Suppl Guidelines):S265–80.
Parsons C, Hughes CM, Passmore AP, Lapane KL. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging. 2010;27(6):435–49.
Acknowledgments
This work was supported by grants (DOH099-FDA-41005 and DOH101-TD-B-111-001) from the Bureau of Food and Drug Administration, Department of Health, Taiwan. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
F.-Y. Hsiao, L.-J. Shen contributed equally to the study.
Rights and permissions
About this article
Cite this article
Lin, CF., Wu, FL.L., Lin, SW. et al. Age, Dementia and Care Patterns after Admission for Acute Coronary Syndrome. Drugs Aging 29, 819–828 (2012). https://doi.org/10.1007/s40266-012-0011-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-012-0011-6