Abstract
Pulmonary hypertension, defined as an increase in mean arterial pressure > 20 mmHg, is a chronic and progressive condition with high mortality and morbidity. Drug therapy of patients with pulmonary hypertension is based on the distinctive pathophysiologic aspect that characterizes the different groups. However, recently, levosimendan, a calcium-sensitizing agent with inotropic, pulmonary vasodilator, and cardioprotective properties, has been shown to be an effective and safe therapeutic strategy for patients with pulmonary arterial hypertension (in addition to specific drugs) and pulmonary hypertension associated with left heart disease (as possible treatment). This review provides a comprehensive overview of the current evidence on the use of levosimendan in patients with pulmonary hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Levosimendan is an inodilator drug that, for its many pleiotropic effects, has been hypothesized to be beneficial in pulmonary arterial hypertension and in pulmonary hypertension due to left heart disease. |
In patients with pulmonary arterial hypertension, the inhibition of pulmonary artery smooth muscle cell proliferation, and the positive hemodynamic effects on pulmonary circulation could account for the use of levosimendan in addition to guideline-directed medical therapy. |
In patients with pulmonary hypertension associated with left heart disease, the reduction in left ventricular filling pressures, the improvement of endothelial function and of right ventricular systolic function, as well as the improvement of right ventricular pulmonary artery coupling, make levosimendan a possible treatment of this disease. |
1 Introduction
Pulmonary hypertension (PH) is a chronic progressive disease characterized by increased pulmonary arterial pressures and pulmonary vascular resistance leading to right heart failure and death from cardiovascular causes [1]. According to the European Society of Cardiology/European Respiratory Society guidelines, PH is defined as a mean pulmonary artery pressure > 20 mm Hg in the resting position [2]. The management of patients with PH is based on the distinctive pathophysiological aspect that characterizes the different groups [3] (Table 1).
In pulmonary arterial hypertension (PAH, group 1), therapy targets one of the three main pathways involved in disease progression: nitric oxide, endothelin-1, and prostacyclin [4]. Treatment of PH induced by chronic increased left atrial pressures (pulmonary venous hypertension, group 2) consists primarily of treating the underlying left-sided heart disease with drugs, interventional therapy, or cardiac surgery [5]. Treatment of PH due to chronic lung disease (group 3) is based on correcting the hypoxia and respiratory disease responsible for PH [6]; in chronic thromboembolic PH (group 4), the disease is predominantly located in the central pulmonary arteries, and treatment consists mainly of relieving the vascular obstruction by a surgical or interventional approach [7]. Finally, group 5 PH (miscellaneous forms) treatment is based on the underlying pathology [8].
Levosimendan is an established therapeutic option for acute heart failure and for advanced heart failure [9, 10] and is currently under development as a treatment for PH in the presence of heart failure with preserved ejection fraction [11]. For its many pleiotropic effects [12], levosimendan has been proposed as a therapeutic strategy in patients with PAH and in other forms of PH due to left heart disease (e.g., PH in presence of heart failure with reduced ejection fraction) [13]. In this review, we summarize and discuss existing evidence on the clinical use of levosimendan in the various form of PH, as well as the future perspective on the use of this drug in this challenging clinical setting.
2 Clinical Pharmacology of Levosimendan
The mechanism of action of levosimendan is complex and involves at least three main pharmacological effects, including positive inotropism, vasodilation, and cardioprotection [14]. The inotropic action is due to the sensitization of myocardial troponin C to calcium [15]. This unique mechanism means that, unlike other inotropes, levosimendan does not result in an increase in intracellular calcium and, therefore, there is no increase in oxygen demand by the myocardium [16]. In addition, levosimendan has a positive lusitropic effect [17] because the calcium sensitization effect is dependent on intracellular calcium levels, which decrease during diastole.
Levosimendan induces vasodilation through the opening of K+ adenosine triphosphate (ATP) dependent channels of vascular smooth muscle cells [18]. Because vasodilation occurs in both arterial and venous smooth muscle cells, levosimendan results in a simultaneous reduction in both ventricular preload and afterload [19]. A further vasodilatory action also occurs via activation of voltage-gated K+ channels and large conductance Ca2+-activated K+ channels; activation of these channels appears particularly important for vasodilation of pulmonary circulation [20].
Moreover, levosimendan also attenuated the vascular remodeling process in a rat model of PH, suggesting long-term anti-proliferative and anti-inflammatory effects mediated via effects on K(ATP) channel activation/opening [21]. Finally, protective properties on the myocardial tissue and other organs seem to be related to the opening of mitochondrial ATP-dependent K+ channels, which protect against apoptosis and oxidative stress [12].
Levosimendan has a short elimination half-life of about 1 h, while the active metabolite OR-1896 has an elimination half-life of 70–80 h [22]; this allows the hemodynamic effects to persist for at least 10 days after a 24-h infusion of levosimendan [23]. In patients with severe renal dysfunction or moderate hepatic dysfunction, the pharmacokinetic profile of levosimendan remains unchanged [24, 25], although the elimination time of active metabolites may be prolonged.
The current recommended dose for achieving hemodynamic benefit in patients with heart failure with reduced ejection fraction is a continuous infusion of 0.1 mg/kg/min for 24 h, which can be reduced to 0.05 mg/kg/min or increased to 0.2 mg/kg/min based on blood pressure [26].
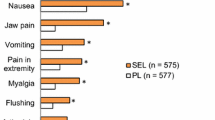
The main side effects of levosimendan include hypotension related to vasodilatation with a consequent reduction in peripheral vascular resistance [27], and hypokalemia, the mechanism for which is not established [28]. Levosimendan has a lower risk of ventricular arrhythmias compared with other inotropes (as it does not increase the intracellular calcium level) [29] though a slight increase in the incidence of atrial fibrillation has been reported [30].
3 Levosimendan in PAH
As shown in Fig. 1, levosimendan exerts several effects in experimental models of PAH; these effects provide a solid pathophysiological basis for the efficacy of levosimendan in this clinical condition. In an experimental model of rat PAH (monocrotaline), treatment with levosimendan for 3 weeks attenuated the development of PAH by inhibiting the proliferation of pulmonary artery smooth muscle cells [21]. These anti-proliferative actions occurred via three mechanisms:
-
1.
direct inhibition of pulmonary artery smooth muscle cell proliferation;
-
2.
increased formation of nitric oxide;
-
3.
reduction in inflammation.
In a subsequent study in a model of rats’ isolated perfused lungs, levosimendan reduced the adverse hemodynamic effects of endothelin 1 (increased pulmonary arterial pressure and pulmonary vascular resistance); this effect, together with levosimendan-induced arterial and venous vasodilatation through activation of potassium channels (K+ATP, BKCa2+, and Kv) explains the positive results observed in PAH [31]. These antiproliferative and hemodynamic effects, coupled with positive effects on the right ventricle remodeling and systolic function, may delay and attenuate the development of PAH [32,33,34] (see Fig. 2).
In humans, there are small studies with promising results. A pilot randomized trial enrolled 18 patients with PH of different etiologies, including seven with PAH, and assessed the short- and long-term effects of repeated levosimendan infusions. The acute response was evaluated after a loading dose of 12 μg/kg infused over 10 min, followed by a continuous infusion of 0.1 μg/kg/min for 50 min; then, the dose was increased to 0.2 μg/kg/min and maintained for 23 h. In addition, the long-term effect was evaluated at 8 weeks, during which levosimendan was administered at fixed intervals every 2 weeks at a dose of 0.2 μg/kg/min for 6 h. In patients with PAH, levosimendan decreased pulmonary vascular resistance (Δ at 24 h, 12 ± 36 vs 25 ± 33; p = 0.009) and mean pulmonary arterial pressure (Δ at 24 h, 14 ± 15 vs 2.0 ± 8.9; p = 0.05) at 24 h; these positive hemodynamic effects were maintained throughout the duration of treatment [35].
Similar positive hemodynamic effects were documented in an open-label non-randomized trial of 45 patients with PAH and severe acute right heart failure [36]. An infusion of 12.5 mg of levosimendan at a rate of 0.1–0.2 μg/kg/min was associated with an improvement at 7 days in World Health Organization functional class (p = 0.008), 6-min walk distance (< 50 vs 260.8 ± 112.9 m; p < 0.001), and NT-proBNP (2420.0 [1831.0–3882.0] pg/mL vs 1631.5 [962.3–2625.5] pg/mL; p < 0.001).
In a retrospective study of 87 patients with PAH due to connective tissue disease complicated by acute right heart failure, infusion of levosimendan for 24 h at a dose of 0.1 μg/kg/min was associated with a modest improvement in mixed venous oxygen saturation (65.28 ± 6.28 vs 69.26 ± 3.76 %; p < 0.001), tricuspid annular systolic plane excursion (increase during follow-up of 3.36 ± 0.71 mm vs 3.81 ± 0.72 mm; p = 0.01), and NT-proBNP (1130.31 ± 534.06 vs 430.79 ± 188.66 pg/mL; p < 0.001) compared with patients treated with enoximone 0.5 μg/kg/min [37]. It is not clear whether these small differences are clinically relevant; the study noted that there were no significant differences in the survival rate at the 6-month follow-up between the levosimendan and enoximone groups.
Overall, evidence from small studies with a limited follow-up is promising. Levosimendan appears to have a positive hemodynamic effect in patients with PAH. However, randomized clinical trials enrolling patients with clear hemodynamic phenotyping and long-term clinically relevant endpoints are needed to confirm the efficacy and safety of levosimendan in PAH.
4 Levosimendan in PH Associated with Left Heart Disease
Left heart disease-associated PH represents the most frequent form of PH, 65–80% of all PH cases [38]. As shown in Table 2, levosimendan exerts favorable effects on the various pathophysiological mechanisms involved in this genesis of Group 2 PH; because of this, several trials of levosimendan have been conducted on patients with PH and heart failure reduced ejection fraction (HFrEF), and heart failure preserved ejection fraction.
The first study aimed to assess the hemodynamic effects of levosimendan on pulmonary circulation was published in 2000 [39]. This randomized placebo-controlled study enrolled 146 patients with advanced HFrEF. Patients treated with levosimendan showed a statistically significant improvement at 6 h in both mean pulmonary arterial pressure (reduction of 6 ± 1 mmHg at 6 h vs an increase of 1 ± 1 mmHg in the placebo group; p < 0.001) and pulmonary vascular resistance values (reduction of 80 ± 13 dyne/s/cm5 vs a rise of 33 ± 19 dyne/s/cm5 in the placebo group; p < 0.001).
A subsequent, randomized, placebo-controlled clinical trial in 54 patients with advanced HFrEF confirmed the positive hemodynamic effects of levosimendan and extended the observations to demonstrate a sustained improvement. After a 24-h infusion of levosimendan, there was a reduction in systolic pulmonary arterial pressure (54 ± 11 vs 43 ± 11 mmHg, p < 0.01) as well as an improvement in echocardiographic parameters of right ventricular function [40].
In a study of 62 patients with acute heart failure randomized to levosimendan or dobutamine [41], patients in the levosimendan group had a greater increase in right ventricular systolic function (s wave velocity change 1.9 ± 0.7 cm/sec in the levosimendan group vs change of 0.2 ± 0.05 cm/sec in the dobutamine group; p = 0.001) and a smaller increase in pulmonary arterial pressure (change 7.3 ± 5.0 mmHg in the levosimendan group vs change of 3.7 ± 3.0 mmHg; p = 0.002).
The impact of ambulatory infusions of levosimendan in patients with advanced HFrEF has also been assessed [42]. In 30 patients with advanced HFrEF, infusion of levosimendan (0.2 mcg/kg/min for 6–8 h according to the patient’s weight) reduced pulmonary artery mean pressure compared with baseline at 48 h (27.69 ± 4.64 vs 23.24 ± 5.32 mmHg; p < 0.01).
A meta-analysis analyzed the effects of levosimendan on right ventricular function in patients with left ventricular systolic dysfunction. In an analysis of the eight studies with a total of 390 patients [43], levosimendan was associated with a significant reduction in both systolic pulmonary arterial pressure (− 5.57, 95% confidence interval − 7.60, − 3.54, p < 0.00001) and mean pulmonary arterial pressure (− 1.01, 95% confidence interval − 1.64, − 0.37, p = 0.002).
The effects of levosimendan on PH due to heart failure preserved ejection fraction were recently evaluated in the HELP (Levosimendan Improves Hemodynamics and Exercise Tolerance in PH-HFpEF) study [11]. After a run-in period, which required hemodynamic improvements after 24 h of levosimendan, the study randomized 37 patients (84%) with heart failure preserved ejection fraction PH (mean pulmonary artery pressure ≥ 35 mmHg) to levosimendan versus placebo. The study failed to meet its primary endpoint of change in exercise pulmonary artery wedge pressure at 25 watts of exercise at 6 weeks. However, levosimendan reduced pulmonary artery wedge pressure across all stages of exercise (− 3.9 ± 2.0 mm Hg; p = 0.047) compared with placebo as well as central venous pressure. There was also a 29.3-m difference in the 6-min walk distance (p = 0.033) between levosimendan and placebo groups.
Despite its potential inotropic and vasodilatory effects, the hemodynamic benefits of levosimendan appear to be mediated via a reduction in stressed blood volume, suggesting venodilation as the prominent mechanism of action. A phase III study is needed to confirm these results.
5 Levosimendan in PH Associated with Lung Disease
Pulmonary hypertension due to lung disease or conditions causing hypoxemia is the second leading cause of PH (14% of the overall form of PH in patients aged < 65 years) [44]. The pathogenesis of this form of PH is complex and still not fully elucidated. However, experimental data suggest that levosimendan may counteract some of the mechanisms involved in group 3 PH.
Levosimendan vasodilating-related effects could theoretically prevent the hypoxic pulmonary vasoconstriction that represents the principal mechanism for the development of PH associated with lung disease. Additionally, levosimendan enhances force generation of respiratory in patients with chronic obstructive pulmonary disease [45] with a theoretical positive effect on ventilation and hypoxia. Finally, levosimendan enhances nitric oxide production, which is impaired in group 3 PH [46].
Despite the theoretical beneficial impact on the pathophysiology of Group 3 PH, only one study has evaluated the role of levosimendan in PH associated with pulmonary disease. This pilot study enrolled 35 patients with PH due to acute respiratory distress syndrome and septic shock [47]. In those patients, 24-h infusion of levosimendan reduced mean pulmonary arterial pressure (29 ± 3 vs 25 ± 3 mmHg; p < 0.05) and pulmonary vascular resistance (290 ± 77 vs 213 ± 50 dynes/s/cm5/m2; p < 0.05).
It is worth noting that levosimendan may also incur a theoretical risk in patients with PH from pulmonary disease as levosimendan-related vasodilation could worsen the dead-space effect (increased perfusion in non-ventilated areas of the lung) [48], resulting in reduced saturation and clinical deterioration. On the basis of these limited data, the role of levosimendan in patients with PH from pulmonary disease is not established.
The unique mechanism of action of levosimendan (inodilation), as well as current experience in the literature, suggest that levosimendan may have a role in the treatment of various forms of PH, either as possible treatment (as in the case of PH associated with left heart disease) or as an addition to specific therapy (as in the case of PAH). The currently available results summarized in this review should be confirmed in a robustly designed, prospective, comparative trial of levosimendan in selected patients with PH.
The availability of a formulation for an oral administration of levosimendan (currently under development) will facilitate the conduct of randomized clinical trials with adequate statistical power to confirm the preliminary positive results of levosimendan in these two forms of PH, specifically with regard to sustained benefit with longer term use on clinically relevant endpoints. More laboratory and clinical research is needed to evaluate if levosimendan will have a role in the treatment of the other forms of PH.
References
Mandras SA, Mehta HS, Vaidya A. Pulmonary hypertension: a brief guide for clinicians. Mayo Clin Proc. 2020;95:1978–88.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS, Escribano-Subias P, Ferrari P, Ferreira DS, Ghofrani HA, Giannakoulas G, Kiely DG, Mayer E, Meszaros G, Nagavci B, Olsson KM, Pepke-Zaba J, Quint JK, Rådegran G, Simonneau G, Sitbon O, Tonia T, Toshner M, Vachiery JL, Vonk Noordegraaf A, Delcroix M, Rosenkranz S. ESC/ERS Scientific Document Group. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–3731. https://doi.org/10.1093/eurheartj/ehac237. PMID: 36017548.
Hajra A, Safiriyu I, Balasubramanian P, Gupta R, Chowdhury S, Prasad AJ, et al. Recent advances and future prospects of treatment of pulmonary hypertension. Curr Probl Cardiol. 2022;29: 101236.
Ruopp NF, Cockrill BA. Diagnosis and treatment of pulmonary arterial hypertension: a review. JAMA. 2022;327:1379–91.
Kennedy JLW, Mihalek AD. Update in approaches to pulmonary hypertension because of left heart disease. Curr Opin Pulm Med. 2022;28:337–42.
Seeger W, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension in chronic lung diseases. J Am Coll Cardiol. 2013;62:109–16.
Ruaro B, Baratella E, Caforio G, Confalonieri P, Wade B, Marrocchio C, et al. Chronic thromboembolic pulmonary hypertension: an update. Diagnostics (Basel). 2022;12:235–46.
Hsu CH, Huang WC, Chang WT. Future perspectives of pulmonary hypertension treatment. Acta Cardiol Sin. 2022;38:435–42.
Masarone D, Melillo E, Gravino R, Errigo V, Martucci ML, Caiazzo A, et al. Inotropes in patients with advanced heart failure: not only palliative care. Heart Fail Clin. 2021;17:587–98.
Agostoni P, Farmakis DT, García-Pinilla JM, Harjola VP, Karason K, von Lewinski D, et al. Haemodynamic balance in acute and advanced heart failure: an expert perspective on the role of levosimendan. Card Fail Rev. 2019;5:155–61.
Burkhoff D, Borlaug BA, Shah SJ, et al. Levosimendan improves hemodynamics and exercise tolerance in PH-HFpEF: results of the randomized placebo-controlled HELP Trial. JACC Heart Fail. 2021;9:360–70.
Farmakis D, Alvarez J, Gal TB, et al. Levosimendan beyond inotropy and acute heart failure: evidence of pleiotropic effects on the heart and other organs: an expert panel position paper. Int J Cardiol. 2016;222:303–12.
Hansen MS, Andersen A, Nielsen-Kudsk JE. Levosimendan in pulmonary hypertension and right heart failure. Pulm Circ. 2018;8:1–7.
Papp Z, Agostoni P, Alvarez J, Bettex D, Bouchez S, Brito D, et al. Levosimendan efficacy and safety: 20 years of SIMDAX in clinical use. Card Fail Rev. 2020;6:19–26.
Cleland JGF, Nikitin N, James M. Levosimendan: first in a new class of inodilator for acute and chronic severe heart failure. Cardiovasc Ther. 2004;2:9–19.
Nieminen MS, Pollesello P, Vajda G, Papp Z. Effects of levosimendan on the energy balance: preclinical and clinical evidence. J Cardiovasc Pharmacol. 2009;53:302–10.
Fredholm M, Jörgensen K, Houltz E, Ricksten SE. Inotropic and lusitropic effects of levosimendan and milrinone assessed by strain echocardiography: a randomised trial. Acta Anaesthesiol Scand. 2018;62:1246–54.
Yildiz O. Vasodilating mechanisms of levosimendan: involvement of K+ channels. J Pharmacol Sci. 2007;104:1–5.
Pathak A, Lebrin M, Vaccaro A, Senard JM, Despas F. Pharmacology of levosimendan: inotropic, vasodilatory and cardioprotective effects. J Clin Pharm Ther. 2013;38:341–9.
Burkhoff D, Rich S, Pollesello P, Papp Z. Levosimendan-induced venodilation is mediated by opening of potassium channels. 365 ESC Heart Fail. 2021;8:4454–64.
Revermann M, Schloss M, Mieth A, Babelova A, Schröder K, Neofitidou S, et al. Levosimendan attenuates pulmonary vascular remodeling. Intensive Care Med. 2011;37:1368–77.
Puttonen J, Laine T, Ramela M, et al. Pharmacokinetics and excretion balance of OR-1896, a pharmacologically active metabolite of levosimendan, in healthy men. Eur J Pharm Sci. 2007;32:271–7.
Lilleberg J, Laine M, Palkama T, Kivikko M, Pohjanjousi P, Kupari M. Duration of the haemodynamic action of a 24-h infusion of levosimendan in patients with congestive heart failure. Eur J Heart Fail. 2007;9:75–82.
Puttonen J, Kantele S, Kivikko M, et al. Effect of severe renal failure and haemodialysis on the pharmacokinetics of levosimendan and its metabolites. Clin Pharmacokinet. 2007;46:235–46.
Puttonen J, Kantele S, Ruck A, et al. Pharmacokinetics of intravenous levosimendan and its metabolites in subjects with hepatic impairment. J Clin Pharmacol. 2008;48:445–54.
Bouchez S, Fedele F, Giannakoulas G, Gustafsson F, Harjola VP, Karason K, et al. Levosimendan in acute and advanced heart failure: an expert perspective on posology and therapeutic application. Cardiovasc Drugs Ther. 2018;32:617–24.
Lehtonen L, Mills-Owens P, Akkila J. Safety of levosimendan and other calcium sensitizers. J Cardiovasc Pharmacol. 1995;26:70–6.
Moreno N, Tavares-Silva M, Lourenço AP, Oliveira-Pinto J, Henriques-Coelho T, Leite-Moreira AF. Levosimendan: the current situation and new prospects. Rev Port Cardiol. 2014;33:795–800.
Silva-Cardoso J, Ferreira J, Oliveira-Soares A, Martins-de-Campos J, Fonseca C, Lousada N, PORTLAND Investigators, et al. Effectiveness and safety of levosimendan in clinical practice. Rev Port Cardiol. 2009;28:143–54.
Mebazaa A, Nieminen MS, Packer M, et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. JAMA. 2007;297:1883–91.
Rieg AD, Suleiman S, Bünting NA, Verjans E, Spillner J, Schnöring H, et al. Levosimendan reduces segmental pulmonary vascular resistance in isolated perfused rat lungs and relaxes human pulmonary vessels. PLoS ONE. 2020;15: e0233176.
Vildbrad MD, Andersen A, Holmboe S, Ringgaard S, Nielsen JM, Nielsen-Kudsk JE. Acute effects of levosimendan in experimental models of right ventricular hypertrophy and failure. Pulm Circ. 2014;4:511–9.
Hansen MS, Andersen A, Holmboe S, Schultz JG, Ringgaard S, Simonsen U, et al. Levosimendan prevents and reverts right ventricular failure in experimental pulmonary arterial hypertension. J Cardiovasc Pharmacol. 2017;70:232–8.
Hansen MS, Andersen A, Tolbod LP, Hansson NH, Nielsen R, Vonk-Noordegraaf A, et al. Levosimendan improves cardiac function and myocardial efficiency in rats with right ventricular failure. Pulm Circ. 2018;8:1–12.
Kleber FX, Bollmann T, Borst MM, et al. Repetitive dosing of intravenous levosimendan improves pulmonary hemodynamics in patients with pulmonary hypertension: results of a pilot study. J Clin Pharmacol. 2009;49:109–15.
Jiang R, Zhao QH, Wu WH, et al. Efficacy and safety of a calcium sensitizer, levosimendan, in patients with right heart failure due to pulmonary hypertension. Clin Respir J. 2018;12:1518–25.
Qu C, Feng W, Zhao Q, et al. Effect of levosimendan on acute decompensated right heart failure in patients with connective tissue disease-associated pulmonary arterial hypertension. Front Med (Lausanne). 2022;9:778620–9.
Vachiéry JL, Tedford RJ, Rosenkranz S, Palazzini M, Lang I, Guazzi M, et al. Pulmonary hypertension due to left heart disease. Eur Respir J. 2019;53:1801897.
Slawsky MT, Colucci WS, Gottlieb SS, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure Study Investigators. Circulation. 2000;102:2222–7.
Parissis JT, Paraskevaidis I, Bistola V, et al. Effects of levosimendan on right ventricular function in patients with advanced heart failure. Am J Cardiol. 2006;98(11):1489–92.
Duygu H, Ozerkan F, Zoghi M, et al. Effect of levosimendan on right ventricular systolic and diastolic functions in patients with ischaemic heart failure. Int J Clin Pract. 2008;62:228–33.
Masarone D, Melillo E, Errigo V, Martucci ML, Pacileo R, Pollesello P, et al. Hemodynamic effects of levosimendan in outpatients with advanced heart failure: an echocardiographic pilot study. J Cardiovasc Pharmacol. 2022;79:36–40.
Hu Y, Wei Z, Zhang C, Lu C, Zeng Z. The effect of levosimendan on right ventricular function in patients with heart dysfunction: a systematic review and meta-analysis. Sci Rep. 2021;16(11):24097–105.
Pugh ME, Sivarajan L, Wang L, Robbins IM, Newman JH, Hemnes AR. Causes of pulmonary hypertension in the elderly. Chest. 2014;146:159–66.
Van Hees HW, Dekhuijzen PN, Heunks LM. Levosimendan enhances force generation of diaphragm muscle from patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179:41–7.
Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008;7:156–67.
Morelli A, Teboul JL, Maggiore SM, et al. Effects of levosimendan on right ventricular afterload in patients with acute respiratory distress syndrome: a pilot study. Crit Care Med. 2006;34:2287–93.
Robertson HT. Dead space: the physiology of wasted ventilation. Eur Respir J. 2015;45:1704–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of the article.
Conflicts of Interest/Competing Interests
Ryan J. Tedford was a funded site principal investigator for the HELP study. Piero Polesello is a full-time employee of Orion Pharma, where levosimendan was discovered and developed. Daniele Masarone, Michelle Kittleson, and Giuseppe Pacileo have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code Availability
Not applicable.
Authors’ Contributions
DM and GP: Conceptualization. DM and GP: Writing - Original Draft. MK, RT and PP: Writing - Review & Editing.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masarone, D., Kittleson, M., Pollesello, P. et al. Use of Levosimendan in Patients with Pulmonary Hypertension: What is the Current Evidence?. Drugs 83, 195–201 (2023). https://doi.org/10.1007/s40265-022-01833-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01833-w