Abstract
Parkinson’s disease (PD) is a chronic, progressive condition affecting around 1% of the population older than 60 years. Upon long-term treatment with levodopa, the mainstay of treatment in PD, most patients, especially younger ones exposed to higher doses, will experience symptoms related to end-of-dose deterioration, peak-dose dyskinesias, and other motor fluctuations. Therapeutic strategies are grounded on modification of oral levodopa pharmacokinetics to extend levodopa benefit and development of new routes of drug delivery (e.g., levodopa/carbidopa intestinal gel infusion) or long-acting formulations of existing dopaminergic drugs to prolong the duration of striatal dopamine receptors stimulation. As our understanding of the pathophysiology of motor complications evolves, our therapeutic armamentarium is actively expanding and the focus of research is now actively pointing to the new non-dopaminergic agents acting both within the basal ganglia and in other brain regions (e.g., drugs acting on glutamate, GABA, serotonin, and calcium channels). Despite the fact that trials comparing the different therapeutic strategies are lacking, we aimed at devising practical evidence- and experience-guided suggestions for the clinical management of motor complications, emphasizing that this should always be an individualized endeavor. This review summarizes the pharmacological management of motor complications in PD, including new formulations and routes of delivery, and the newer released drugs such as istradefylline, opicapone, safinamide, and zonisamide. Advanced therapeutic strategies for selected cases such as treatment with apomorphine and surgical techniques (deep brain stimulation) are also discussed. A comprehensive knowledge of the available options and evidence is fundamental for the successful management of these challenging complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Parkinson’s disease (PD) is a chronic, progressive condition affecting around 1% of the population older than 60 years, second only to Alzheimer’s disease [1]. The cardinal clinical motor features are bradykinesia, rigidity, postural instability, and tremor at rest [2]. Non-motor symptoms are also important due to their negative impact on the quality of life (QOL) of these patients [2, 3]. Two major neuropathological findings changed the paradigm of PD diagnosis, therapeutics, and research, since it was first described 200 years ago, namely the loss of dopaminergic neurons in the substantia nigra pars compacta [4] and the identification of α-synuclein protein as the main component of Lewy bodies and Lewy neurites [5]. Levodopa has been prescribed for decades in PD with the aim of restoring the nigrostriatal dopaminergic deficiency, and it remains the mainstay of treatment in PD, due to its proven efficacy and safety [6, 7]. However, upon long-term treatment, most PD patients experience symptoms and disability due to wearing-off (end-of-dose deterioration), peak-dose dyskinesias, and other motor complications, which may present even at early disease stages [2, 4, 8,9,10,11]. Ultimately, motor complications may cause extreme fluctuations of the motor state of patients, causing important loss of QOL and impairment. Motor complications in PD and their definition are summarized in Table 1.
The development and course of motor complications in PD is characterized by an important amount of unpredictability. Disease duration and stage, exposure to levodopa and cumulative dose, delayed or erratic gastric emptying, female gender, and low body weight all seem to play a role [12,13,14]. Moreover, patients with young disease onset (including carriers of genetic mutations such as parkin, PINK1, and DJ-1) seem especially predisposed to develop motor complications earlier in the disease course or after a shorter exposure to levodopa [15]. In an era where genetics has a prominent role in medical research and clinical medicine, PD is not an exception, and some pharmacogenetic studies have suggested an association between some genetic variations and the risk of developing dyskinesias [15]. Despite increasing knowledge, the pathophysiological underpinnings of motor complications are not fully understood. Intermittent oral delivery of levodopa, as opposed to continuous physiological dopaminergic stimulation, along with the relentless loss of nigrostriatal nerve terminals and reduced endogenous dopamine storage/release capacity, contribute decisively to the appearance of motor complications, with symptomatic benefit becoming progressively dependent on oral levodopa intake and plasma bioavailability [16].
In this article we discuss the pharmacological options and clinical management of motor complications in PD, a major challenge for both physicians and patients.
2 Treating Motor Fluctuations in PD
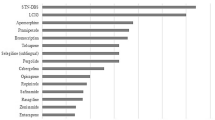
Table 2 summarizes the drugs currently used to treat motor fluctuations and dyskinesias in PD. Figure 1 provides practical suggestions for daily clinical practice in this regard.
Suggested therapeutic strategies to tackle the most common motor complications in Parkinson’s disease. MAO-B monoamine oxidase B, COMT cathecol-O-methyl-transferase, DA dopamine agonist, STN subthalamic nucleus, GPi globus pallidus interna. *These strategies increase the risk of peak-dose dyskinesias and psychosis; **these strategies increase the risk of “off” symptoms
2.1 Levodopa
Parkinsonian symptoms are highly responsive to levodopa administration, especially at earlier disease stages [17], and every patient will eventually receive levodopa in order to achieve optimal control of their motor symptoms [18]. The potential long-term effects of levodopa on Parkinson’s disease beyond its immediate benefit remain uncertain as a previous randomized control trial suggested that it might slow the progression of Parkinson’s disease or have an effect on the motor symptoms of the disease when compared to placebo (ELLDOPA trial), an effect that was somewhat contradicted by neuroimaging study data suggesting a possible detrimental acceleration of nigrostriatal dopamine nerve terminal neurodegeneration/dopamine transporter modification in those patients exposed to levodopa [17]. One of the reasons determining delay in levodopa initiation is the concern about the development of motor complications. In fact, doses higher than 600 mg per day or 5–6 mg/kg body weight are associated with an increased risk of both wearing-off and dyskinesia [17], with patient’s age being the next most important predictor.
These data influenced PD treatment practices, and for many years levodopa remained in the background with many physicians using it in a restricted manner and mostly as second-line strategy. To clarify this important topic, a unique of its kind randomized, double-blind, placebo-controlled, delayed-start trial was conducted in early PD patients (up to 2 years since diagnosis, treatment-naïve) and aimed to distinguish between a beneficial disease-modifying effect and a symptomatic effect of an intermediate dose of levodopa (LEAP trial). To attain this clinically meaningful effect, authors analyzed a primary outcome—change from baseline to the end of the trial period (80 weeks) in the UPDRS III motor score between those treated for all 80 weeks (early-start group) versus those treated with levodopa–carbidopa for the second 40 weeks (delayed-start group). Importantly, there was no difference in the primary outcome, which was further supported by a non-inferiority analysis of disease progression between the groups in the second phase of the trial, rates of dyskinesia and levodopa-related motor fluctuations between both group patients. This study is the first providing level 1 evidence that levodopa does not have a disease-modifying effect in PD [19].
So the practical question remains: when exactly should levodopa be started in PD patients? Although there are no robust data to support objective advice on this subject, we feel that clinicians should not withhold levodopa if the patient’s QOL is at stake, especially in elderly patients, where there is a higher risk of cognitive deterioration, multi-morbidity, and a higher number of concomitant medications, and also in all patients with significant disability derived from PD motor symptoms, regardless of their age, including those who do not get enough clinical benefit with other antiparkinsonian drugs.
Regarding strategies to ameliorate motor complications, over the years an alternative strategy has been to improve oral levodopa pharmacokinetics (adjusting the timing interval of levodopa preparations and/or improving absorption). In 1994, Nutt et al. studied whether meals affected levodopa absorption and if they contributed to the discrepancy that had been observed between drug ingestion and levodopa plasma peak concentrations. This study was a milestone because one of its major conclusions was that high-protein meals or large oral intake of neutral amino acids neutralize levodopa’s therapeutic effect, an interaction that had been suggested by previous studies [20]. This interaction seems to be determined by blood–brain barrier competition effects and by the composition and chemical properties of a protein meal in gastric emptying, delaying levodopa’s absorption [21]. These conclusions must not be interpreted as a justification for protein-restricted diets, which also carry side effects, namely dyskinesia, weight loss, malnutrition [22], and long-term insufficient adherence [23], but they underscore why patients taking levodopa are advised to take it on an empty stomach (ideally at least 30 min before meals).
A widespread strategy is to combine levodopa with a dopa-decarboxylase inhibitor (carbidopa, benserazide) to improve absorption and reduce levodopa peripheral metabolism. However, immediate-release (IR) combined formulations of levodopa have a short half-life and require frequent dosing, leading to marked fluctuations in levodopa plasma concentrations, which may play a role in motor complications. Controlled-release formulations of levodopa–carbidopa have been developed, but they have been associated with erratic absorption and variable plasma concentrations and treatment effects. A new extended-release (ER) levodopa–carbidopa (IPX066/Rytary/Numient) is available in North America in a capsule formulation in a 1:4 ratio of carbidopa:levodopa in four distinct dosages, providing a characteristic and unique levodopa plasma profile [24, 25]. After oral administration, there is rapid absorption of levodopa, the concentration of which reaches its peak (Cmax) by approximately 1 h, comparable to the IR carbidopa–levodopa formulation, followed by a sustained release of levodopa, the concentration of which remains stable for approximately 4–5 h before declining again, thus avoiding pulsatile stimulation of dopamine receptors and resulting motor complications [24]. Given this profile, unlike some other formulations, IPX066 cannot be chewed, divided, or split. It was shown to reduce “off” time as a percentage of waking hours in comparison with the IR levodopa–carbidopa formulation and levodopa–carbidopa–entacapone preparations in a large pool of early and advanced PD patients with motor complications [26, 27], which had not been achieved with the previously available prolonged-release levodopa–carbidopa formulations [28,29,30]. It was thus approved by the US Food and Drug Administration (FDA) in 2015.
Another way to prolong striatal dopamine receptors stimulation is by using new drug delivery methods, as we discuss later [31]. A dry powder aerosol containing levodopa was developed to treat intermittent and predictable motor and refractory “off” periods, and has just received FDA approval for treating “off” episodes in PD. Due to the large surface area, pulmonary absorption of levodopa is quicker because it avoids the variability related to gastrointestinal absorption and it provides a more predictable response and greater bioavailability than standard oral l-dopa. In a placebo-controlled 4-week study, approximately 25% of patients reported mild coughing and none experienced serious pulmonary problems, but further studies on long-term safety are necessary [32, 33].
2.2 Dopamine Agonists
In PD patients not optimally controlled with levodopa, it may be desirable to add levodopa-sparing agents instead of increasing levodopa, in order to address motor fluctuations. Pramipexole [34, 35] and ropinirole [36] significantly reduced “off” time compared with placebo [37]. Similarly, two studies evaluated the change in UPDRS III during “on” time between rotigotine, a non-ergot dopamine agonist with activity across D1–D5 receptors, and other dopamine agonists (DAs) (pramipexole and ropinirole) in PD patients with motor fluctuations. Rotigotine proved to be non-inferior to these DAs [38, 39], with a higher rate of application-site reactions, although mostly insignificant, and a similar incidence of impulse control disorders (ICDs) [38]. Additional evidence for rotigotine came from 24-h transdermal delivery of rotigotine (2–16 mg/24 h) that resulted in significant benefit in a primary endpoint combining early-morning motor dysfunction (evaluated by Unified Parkinson’s Disease Ratings Scale (UPDRS) III) and nocturnal sleep disturbances, compared to placebo in a double-blind trial (RECOVER) [40, 41]. Newer extended-release formulations DAs promote more stable plasma levels and a comfortable number of intakes. Ropinirole ER was compared with ropinirole IR and the former was found to be more efficacious in maintaining reduction in “off” time equal or superior to 20% [42]. A study with 518 patients with advanced PD and an “off” time per day higher than 2 h compared the efficacy of pramipexole ER to pramipexole IR and placebo. Once-daily pramipexole ER versus three times daily pramipexole IR resulted in a decrease in “off” time from baseline means by an adjusted mean of − 2.1 h/day for pramipexole ER and − 2.5 h/day for pramipexole IR compared to − 1.4 h/day in the placebo group over 18 weeks, and this treatment effect was retained over an extended period of 33 weeks, without any particular adverse effects [43, 44]. Thus, the choice may depend on the duration of action, local availability, cost, and individual tolerability [37].
Nonetheless, the major concern with DAs is related to their adverse effects, mainly peripheral edema, excessive daytime sleepiness, constipation, hallucinations, nausea, postural hypotension, and neuropsychiatric issues, in particular ICDs (e.g., hypersexuality, pathological gambling, compulsive shopping) punding, and dopamine dysregulation syndrome, which may appear at all disease stages [45]. There is a paucity of evidence on how to address this issue. Usually, the first action is dose reduction/withdrawal. However, while this may solve ICDs, a worsening of motor function and the so-called dopamine agonist withdrawal syndrome (DAWS) may emerge. DAWS is a severe condition that may affect up to one-third of patients who attempt to reduce dopamine agonists [46,47,48,49]. Its symptoms mirror those related to the withdrawal of other psychostimulants and range from anxiety, panic, agoraphobia, fatigue, dysphoria, nausea, vomiting, diaphoresis, and even suicidal ideation, among others. Currently, there is no known effective treatment for ICDs or DAWS, and it does not seem to be ameliorated by using levodopa as a replacement for the dopamine agonist [46, 47]. Furthermore, the most serious side effect of ergot DAs specifically (cabergoline, bromocriptine, pergolide, lisuride)—fibrotic reactions (heart valves, pleuropulmonary, retroperitoneal)—led to the discontinuation of these drugs in many countries around the globe [50].
There is general concern that some of these side effects may preclude using DAs in elderly patients, even in those who have mild symptoms early in the course of the disease. Few older (i.e. at least 75 years old) PD patients are enrolled in clinical trials [51], but it is expected that they are more prone to adverse effects related to altered drug metabolism, co-morbid conditions, including neuropsychiatric manifestations, and drug interactions [52]. For these reasons, DAs have traditionally been avoided in this population. However, accumulating evidence suggests that these drugs may be well tolerated in appropriately selected elderly PD patients, as other characteristics besides chronological age should be considered [53,54,55]. Of note, a 1-year open-label extension study of the RECOVER trial, in which patients received rotigotine (2–16 mg/24 h) for a 10-month maintenance period (79% completion rate) and another open-label extension study for the newly developed long-term-acting ropinirole, in which patients who completed one of the three prior studies evaluating this drug were enrolled and followed for up to 73 months while taking long-acting ropinirole (up to 24 mg/day) and levodopa or another non-dopamine agonist PD medication both pointed to lower rates of ICDs, regardless of age [40, 56].
For a long time, dopamine agonists have been considered clinically valuable to prevent or delay the onset of motor fluctuations, contributing to the clinical dogma that levodopa should be used only late in the course of the disease, and at the lowest dose possible to avoid motor complications. Nonetheless, according to the most recent evidence derived from follow-up studies, there is no long-term clinically relevant difference on motor complications or mortality between levodopa or dopamine agonists [45, 57,58,59], supporting the notion that motor complications will eventually emerge in most patients regardless of how dopaminergic therapy is initiated. Yet, the same is not valid regarding clinical symptomatic benefit in PD. The pragmatic PD-MED trial randomized early or newly diagnosed PD patients to either levodopa or levodopa-sparing agents and confirmed that levodopa was superior with respect to improvement in motor scores and quality of life, as previously mentioned, with most patients requiring levodopa for symptomatic control and significantly higher rates of treatment discontinuation due to greater non-motor side effects in the dopamine-agonist and monoamine oxidase B inhibitor groups versus levodopa [18].
2.3 Catechol-O-Methyltransferase (COMT) Inhibitors
After oral administration, levodopa is metabolized in the gut and liver by catechol-O-methyl transferase (COMT). Drugs inhibiting COMT act by increasing the elimination half-life of levodopa. When given as adjunctive therapies, levodopa bioavailability increases and “off” time decreases, possibly decreasing the required daily levodopa dose. It has been postulated that the administration of COMT inhibitors could provide more stable plasma levodopa levels and, consequently, sustained brain dopaminergic stimulation, a mechanism thought to reduce the risk of motor complications.
Entacapone is a selective, reversible inhibitor of COMT, primarily acting to block gut metabolism and improve levodopa absorption. Repeated administration of entacapone in the recommended dose of 200 mg administered with each dose of levodopa/carbidopa increases the levodopa plasma concentration by approximately 30% [60]. Three double-blind placebo-controlled randomized trials evaluated the effect of entacapone as an adjunct to levodopa in PD patients with suboptimal levodopa response and wearing-off motor fluctuations, demonstrating the superiority of this strategy with regard to the improvement of patient-reported “off” times and the UPDRS motor scores [61,62,63], an effect that is independent of the type of dopa decarboxylase inhibitor used [40]. Later, a prospective, randomized, double-blind study comparing perampanel, placebo, or entacapone in a large sample size of 723 moderately severe PD patients with motor fluctuations on levodopa confirmed the validity of the initial findings. This study was terminated early due to the lack of efficacy of perampanel, but a significant reduction in mean total daily “off” time was observed with entacapone versus placebo [64]. However, patients randomized to entacapone in a triple regimen of levodopa/carbidopa/entacapone (STRIDE-PD study) involving pulsatile administration, actually developed a higher rate of dyskinesias as compared to levodopa/carbidopa alone [65, 66]. Also, during a pre-approval randomized clinical trial for entacapone, an increased incidence of prostate cancer was observed among patients in the treatment arm, though posterior studies ruled out this association [67, 68]. These results, along with potentially fatal toxic liver effects due to tolcapone decreased the popularity of these agents [37].
Recently, opicapone, a new COMT inhibitor with a longer half-life than entacapone, received approval in Europe for the treatment of end-of-dose fluctuations in patients on levodopa [69]. Compared with both entacapone and tolcapone, opicapone shows a much higher degree of COMT inhibition in erythrocytes [70]. It is administered once daily at a dose of 50 mg in the evening since this dose was found to be superior to placebo and non-inferior to entacapone in reducing the daily “off” time during the 15-week study period [69, 71]. The data further revealed that opicapone 50 mg was associated with significant improvement in the proportion of both “off” and “on” times (minimum 1 h improvement) compared to placebo. Moreover, this was further addressed in another study that concluded that opicapone led to further improvement, comparative to entacapone, in both Patient Global Impression of Change and Clinical Global Impression of Change. Finally, the incidence of treatment-emergent adverse events in those patients taking opicapone was slightly reduced [72]. To date, opicapone has not been evaluated in nonfluctuating PD patients, but it remains an area of future research. Of note, the main side effects with this drug class are diarrhea and urine discoloration [73], which can sometimes be very concerning to the patient. Notably, with opicapone the most common adverse effects were dyskinesia, constipation, and dry mouth, and no change in liver function or severe diarrhea were reported [69].
2.4 Monoamine Oxidase B (MAO-B) Inhibitors
Rasagiline mesylate and selegiline act by selectively and irreversibly blocking MAO-B, the main enzyme responsible for degrading dopamine in the synaptic cleft, and so increase concentrations of dopamine in the brain. Clinical trials have demonstrated the efficacy and safety of these drugs as adjunctive therapy to levodopa [37, 74]. In the PRESTO trial, a randomized, double-blind study, 472 patients experiencing motor fluctuations received either rasagiline 0.5 mg or 1 mg/day; rasagiline was beneficial in reducing the mean total daily “off” time as compared to placebo at 26 weeks of treatment [75]. Analysis of secondary outcomes also revealed an increase in time without troublesome dyskinesias in patients who were administered rasagiline. The LARGO trial found that the efficacy and safety of rasagiline were comparable to entacapone in reducing “off” time and increasing daily “on” time without dyskinesias in levodopa-treated patients with PD and motor fluctuations [76]. Regarding selegiline, the recommendations are solely based on lower quality studies that demonstrated only a modest reduction in daily “off” time with this drug. The drug undergoes extensive first-pass metabolism, which results in only 10% bioavailability, high concentrations of its metabolites, and a variable pharmacokinetic profile. Therefore, selegiline orally disintegrating tablets were developed to allow direct absorption into the systemic circulation due to the highly vascularized nature of the oral mucosa, thus bypassing the gastrointestinal system and the first-pass metabolism in the liver. Preclinical studies have been performed to explore the neuroprotective potential of MAO-B inhibitors, but there is not enough evidence to recommend rasagiline or selegiline for this purpose, either as initial monotherapy or as adjunctive therapy [37].
The main adverse events with this drug class include confusion, hallucinations, and hypertensive crises. It is important to keep in mind that they might be involved in drug-drug interactions if administered simultaneously with tricyclic antidepressants, selective serotonin reuptake inhibitors, or serotonin–norepinephrine reuptake inhibitors, with a possible risk of serotonin syndrome [9], although this seems notably uncommon for therapeutic doses of 10 mg daily and 1 mg daily, respectively, for selegiline and rasagiline. However, at higher doses, they lose selectivity and inhibit both MAO-B and MAO-A, which may result in serotonin syndrome, even when used alone. Currently, concomitant use of rasagiline/selegiline and selective serotonin reuptake inhibitors (SSRIs) is not recommended/contraindicated according to product monographs/labels, interaction checkers (MicroMedex database, Medscape Drug Interaction Checker, Stockley’s Drug Interactions), UpToDate, and supporting literature. Nonetheless, to date, the only report to estimate the incidence of serotonin syndrome with the coadministration of an MAO-B inhibitor and an SSRI is the Parkinson Study Group survey [77], which found an incidence of 0.24%, which was not confirmed in a large posterior retrospective phase IV study with 1504 patients (471 of whom took rasagiline plus antidepressants (74.5% were SSRIs)) that used a formal definition of serotonin syndrome (Sternbach criteria) and did not identify any cases of serotonin syndrome [78]. As such, a potential interaction between the two is largely based on case reports. This may lead to a cautious recommendation that selegiline or rasagiline can be prescribed with an SSRI, given the recognized benefits of these agents in treating depression in PD, provided that their doses are kept in the lower range for therapeutic benefit. Interactions of MAO-B inhibitors with tyramine, found in various foods such as cheese, are also described [79].
Safinamide is a new highly selective and reversible MAO-B inhibitor that presents additional mechanisms of action such as blocking of voltage-dependent sodium and calcium channel and reduction of neuronal glutamate release. Safinamide given orally (50–100 mg/day) was tested against placebo in PD patients with motor fluctuations, and a significant effect of treatment was verified with respect to change in “on” time with no or non-troublesome dyskinesia, an effect that was prolonged for 18 months, and therefore it is now approved for the treatment of PD patients experiencing motor fluctuations [37, 80,81,82].
Zonisamide (25–50 mg/day) has multiple modes of action, with its main mechanisms being the activation of dopamine synthesis in the striatum at the level of mRNA of tyrosine hydroxylase with a resultant increase in dopamine content and moderate inhibition of MAO-B. It also inhibits T-type calcium channels and glutamate release, exerts inhibition on an indirect pathway in the basal ganglia through the δ opioid receptor, and regulates oxidative stress, which points to further neuroprotective effects. It has no effects on dopamine receptors, dopamine transporter, dopamine release, adenosine receptors, or serotonergic system. A placebo-controlled randomized trial in PD patients with wearing-off symptoms on other PD medications revealed a benefit of zonisamide 50 mg in reducing “off” time, without increasing dyskinesias, over a period of 1 year [83]. It is now approved for the treatment of PD in Japan, where it was originally synthetized. It remains unclear if there is a relative benefit of either safinamide or zonisamide when compared to other adjunctive therapies.
2.5 Adenosine A2 Antagonists
Recent evidence implicates the adenosine system in basal ganglia function, and several adenosine A2A receptor antagonists have since been developed. Istradefylline is an adenosine A2A antagonist now approved as adjunctive therapy in Japan. Several studies have assessed the efficacy of this agent in the treatment of motor fluctuations, with somewhat conflicting outcomes, which may relate to differences regarding therapeutic schemes and dosage and patient selection, but overall available evidence, including an unblinded 1-year follow-up extension, supports its use in clinical practice [84]. No particular safety concerns were associated with this drug apart from a slight increase in dyskinesias.
3 Dyskinesias
Dyskinesias appear as a result of supratherapeutic stimulation of dopamine receptors, causing hyperkinetic involuntary movements typically affecting the upper and lower limbs, trunk, and/or facial muscles. Initially, they may manifest as low-amplitude choreic movements, but as the disease progresses, they evolve into jerky, irregular movements, often becoming very disabling and impairing the QOL of patients. Sometimes patients present with dystonic postures, which may be present in both the “on” and “off” phases, and this combination of dystonic and choreic patterns varies from patient to patient [85]. Appearance of dyskinesias poses a significant problem related to drug management, requiring a delicate therapeutic balance to account for this trade-off between control of “on” time with dyskinesias at the possible expense of increased “off” time duration and severity. Estimates vary, but the median frequency of dyskinesias is around 40% after 4–6 years of levodopa therapy [11].
The so-called “peak-dose dyskinesias,’ in relation to plasma peak concentrations of levodopa, are temporally related to levodopa administration and correlate with the levodopa dose, with higher doses (e.g., 600 mg/day) associated with higher risk when compared to lower doses (e.g., 150 mg/day) [17, 86]. Although the exact neural mechanisms involved in dyskinesias are still undefined, progressive nigrostriatal degeneration, cortical dysfunction (particularly at the supplementary motor area), and abnormal plasticity of corticostriatal synapses may all play a role [87, 88]. Different animal models of PD and levodopa-induced dyskinesias have associated a decrease in dendritic spine density of striatal spiny projection neurons and an enlargement in spine head size in different brain regions with dopaminergic denervation and chronic levodopa treatment. These morphological changes are consistent with the lack of depotentiation, which is the electrophysiological hallmark of dyskinesias, suggesting spine enlargement as a possible structural basis for levodopa-induced dyskinesias. The mechanisms for this synaptic plasticity may be connected with modulation of receptors and ion channels that are abundantly present over the neuronal dendrites such as the N-methyl-d-aspartate (NMDA) and AMPA receptors and L-type Ca2+ channels, which explains why drugs blocking these structures might have a possible benefit for the treatment of dyskinesias, through a potential mechanism of spine loss and spine head enlargement prevention [88]. As a result, non-dopaminergic pathways such as glutamatergic, serotoninergic, GABAergic, and noradrenergic may all be involved in the development of dyskinesias. This opened up new avenues for different therapeutic approaches thought to counteract the postsynaptic changes, as we discuss further on [85]. Since patient factors are not modifiable, and until now no neuroprotective drugs have been proven to exist the traditional strategies that have been proposed to manage dyskinesias mainly focus on lowering or fractionating the levodopa dose, dropping the dose of adjunctive dopaminergic agents, adding a longer-acting dopamine agonist, and providing continuous dopaminergic delivery [37].
3.1 Prevention of Dyskinesias
Administering DAs (e.g., pramipexole, ropinirole) as a strategy to delay the introduction of levodopa in order to reduce the risk of dyskinesia in early PD, compared to levodopa as initial treatment, has been supported by high-quality studies over the years [12, 13, 72, 89,90,91,92]. The longer half-life of dopamine agonists and the ability to rapidly cross the blood–brain barrier has been suggested as a reasonable explanation for these results. Surprisingly, however, prolonged-release formulations of ropinirole and pramipexole did not change the risk of developing dyskinesias [93, 94], nor does this seem dependent on the affinity for dopamine D3 receptors, unlike previous studies suggested [95, 96]. This is because pramipexole is a D3-preferring dopamine agonist and ropinirole is a dopamine receptor agonist with highest affinity for D2 receptors, with both yielding similar results. Two open-label 6-year extensions of the randomized studies evaluating rotigotine (titrated to an optimal dose of ≤ 16 mg/24 h) in monotherapy in early PD were conducted to assess the long-term incidence and severity of dyskinesia in these patients. A post hoc analysis concluded that only 19% of the 596 patients reported dyskinesias, mainly after levodopa initiation, with more than half the patients with dyskinesias considering it to be “non-disabling” [97]. It should be kept in mind that no randomized trial has been specifically designed to address this outcome. Besides dopamine agonists, there is not enough evidence to recommend other oral strategies such as adjunctive COMT or MAO-B inhibitors for the purpose of preventing dyskinesias [37].
Contradicting this customary clinical practice, evidence now points to an equal risk of dyskinesias in patients on dopamine agonists after the introduction of levodopa to the risk observed in those who had received levodopa from the beginning, and attention is now turning to the disease duration and treatment dosage as the main determinant factors for the development of dyskinesias, rather than early initiation of levodopa [98,99,100]. Interestingly, patients with PD also seem to be more concerned with wearing-off than with dyskinesias [101]. Despite this, many PD patients continue to be undertreated for fear of inducing dyskinesia (so-called “levodopa-phobia”). There is a need to investigate if additional therapies developed to assure a more stable dopaminergic delivery, such as the new levodopa extended-release formulation (IPX 066/Rytary), have a potential role in preventing or delaying dyskinesias. In fact, levodopa administered continuously via intestinal infusion was shown to increase “on” time without troublesome dyskinesias compared to IR oral levodopa–carbidopa, which suggests that dyskinesias might be related to the pulsatile dopaminergic stimulation as a result of oral levodopa treatment. Delaying levodopa with the intent of preventing dyskinesias is thus not evidence-supported in the long run, and it may actually prove to be counter-productive with regard to efficient symptomatic control.
3.2 Treatment of Dyskinesias
While the prevention of dyskinesias still remains an unmet need, symptomatic management of this phenomenon is also challenging, as there are only a few clinically available specific interventions for dyskinesias, and no drug therapy with this aim had been approved until recently.
Amantadine is a noncompetitive NMDA receptor antagonist, selectively blocking activated open-channel NMDA receptors, an important target when addressing dyskinesias, as previously discussed, and it has direct and indirect effects on glutamatergic and dopaminergic signaling. Amantadine IR was originally approved for the treatment of influenza virus, and only 30 years later did it receive the additional indication for the treatment of PD. A daily dose up to 200 mg/day (higher doses are associated with an increased frequency of adverse events related to anticholinergic and NMDA receptor antagonist activity such as dry mouth, urinary retention, constipation, and hallucinations) has been shown to lower dyskinesia rating scales and UPDRS dyskinesia subscore items addressing duration and severity [102,103,104]. Moreover, withdrawing amantadine significantly aggravated levodopa-induced dyskinesias within a median time of 7 days, underlining its clinical value [102]. However, well-designed randomized long-term trials addressing the efficacy and safety of this drug are still needed, and so guideline recommendations are widely variable, which has limited its clinical use [105]. A novel formulation of higher-dosing ER amantadine with a distinct pharmacokinetic profile exhibits a slow initial rise in amantadine levels during the night and peak high levels in the morning that remain sustained throughout the day (prolonged Tmax), when dyskinesias become more uncomfortable for the patients, without any new safety concerns [106]. It has a once-daily bed-time dosing scheme (a direct switch from amantadine IR to amantadine ER can be done and consists of administering 137 mg for 1 week, increasing to a target dose of 274 mg thereafter [107]), which was shown to induce a significant primary reduction in the Unified Dyskinesia Rating Scale score, and a secondary increase in “on” time without troublesome dyskinesias when compared to placebo according to the results from the EASED and EASE LID 3 trials [106, 108]. Both effects were sustained for up to 64 weeks [109]. Like amantadine IR, it is generally well tolerated, but precautions are necessary and patients should be especially monitored for the development of depression and suicidal ideation or behavior; an open-label long-term safety study is currently ongoing. Of note, no direct comparison with amantadine IR exists, which would be necessary to sustain the relative efficacy and safety of this new formulation of ER amantadine.
Different experimental oral drugs with potential anti-dyskinetic effects have been evaluated in randomized placebo-controlled trials, but results fell short of expectations derived from experimental studies with some agents being discontinued for conflicting results, lack of efficacy, troublesome side effects, or worsening of motor symptoms [85]. An anti-dyskinetic effect of safinamide has been suggested, but so far not demonstrated, and its formal indication is adjunctive therapy to levodopa in order to decrease “off” time [37]. A study evaluated pramipexole as add-on therapy or a switch from ergot dopamine agonists in patients with PD and peak-dose dyskinesias on levodopa and an ergot dopamine agonist; the conclusions from this study were limited due to the lack of precise reporting of the outcome parameters, so the use of pramipexole to treat dyskinesias merits further research [110]. Two placebo-controlled trials have evaluated the use of levetiracetam, an antiepileptic agent targeting synaptic vesicle glycoprotein 2A channels, in PD patients with dyskinesias. However, different dosage schemes, small sample sizes, and a large range of dyskinesia scores at baseline as well as conflicting outcomes have impacted the validity of these studies [37]. Mavoglurant (AFQ056) is a noncompetitive antagonist at the metabotropic glutamate receptor-5 binding site. Initial results regarding the efficacy of mavoglurant in reducing dyskinesias seemed promising but further research proved disappointing [111]. As discussed, the serotonin system has emerged as a possible relevant player in the pathogenesis of dyskinesias. In fact, serotonin neurons can convert exogenous levodopa to dopamine, which is stored in synaptic vesicles and then released in an activity-dependent manner. However, serotonin neurons lack autoregulatory feedback mechanisms (e.g., dopamine transporter), and the release of dopamine as a false neurotransmitter from serotonin neurons leads to the consequent pulsatile stimulation of dopamine receptors; in advanced PD there might be an excessive stimulation of hypersensitive striatal dopamine receptors. Thus, drugs acting on serotonin 1A/1B autoreceptors (5-HT1A/B receptors) are likely to “silence” these serotonin neurons. Additional evidence suggests that simultaneous activation of 5-HT1A/B receptors has a synergistic effect on the suppression of dyskinesia. Eltoprazine is a mixed 5-HT1A/B agonist with a safe toxicological profile that lacks antagonistic affinity for the dopamine receptors. This drug, combined with levodopa, appears promising in animal models and in a clinical study, with no major adverse effects [112]. It is possible that eltoprazine and amantadine may have complementary efficacy against dyskinesias [113]. Clozapine is another drug targeting 5-HT receptors, and it is somewhat efficacious regarding dyskinesias, but there are important safety concerns with this drug (e.g., agranulocytosis, myocarditis), requiring strict blood count monitoring [37]. Intensive inpatient physical therapy may also prove useful as it seems to improve dyskinesia and reduce levodopa equivalents dose in comparison to general home exercises in at least one study [114].
In conclusion, there is an unmet need regarding safe therapies addressing dyskinesias without compromising PD symptomatic control.
4 Advanced Therapies
4.1 Deep Brain Stimulation
Available evidence and accumulating experience support deep brain stimulation (DBS) of the subthalamic nucleus (STN) or globus pallidus internus (GPi) in PD in those patients whose parkinsonian symptoms improve under levodopa, but who fail to achieve satisfactory control of their motor fluctuations under optimized medical therapy. DBS was the second major landmark in PD therapy, after the introduction of levodopa. A study conducted in patients with PD and at least 6 h per day of “off” time or moderate to severe dyskinesias assessed the effects of bilateral STN DBS by comparing patients exposed to stimulation within 7 days of implantation or implantation without activation. Results showed that stimulation improved QOL and time free of dyskinesias [115]. Several studies have suggested that targeting either the STN or the GPi bring largely similar results in this regard [116,117,118,119]. Recently, a follow-up study was conducted to compare motor symptoms, cognition, mood, and behavior 3 years after GPi and STN DBS in advanced PD; this study provided class II evidence that STN DBS provides better motor improvement, with a similar risk for non-motor complications (namely, cognition, mood, and behavior) [120]. Documented adverse effects to date are mostly related to the surgical procedure, the implanted hardware, or the stimulation itself, ranging from infection, intracerebral bleeding, stroke, seizures, weight gain, infection, to increased suicide risk, among others [121]. The incidence of permanent severe morbidity or death may be as high as 4% [121, 122]. Given that this is not a risk-free procedure, a clear balance between risks and benefits, and a comprehensive discussion with the patient are essential. Moreover, this therapy is restricted to highly specialized centers, and there are some restrictions to its use, such as age, cognitive impairment, and severe psychiatric disorders, thus limiting patient eligibility.
4.2 Levodopa/Carbidopa Intestinal Gel
The rationale behind levodopa–carbidopa intestinal gel delivered continuously through an intrajejunal percutaneous tube and portable infusion pump involves the ability to reduce the dose of oral levodopa and to continuously stimulate dopamine receptors, rather than the intermittent, non-physiological, pulsatile dopaminergic stimulation derived from oral levodopa therapy. It provides continuous exposure to levodopa during waking hours and was specifically tested in advanced PD patients with worrisome motor complications including dyskinesias. It was observed that besides a significant reduction in “off” time, the infusion of levodopa promoted a relevant increase in mean “on” time without dyskinesias compared to oral levodopa–carbidopa plus placebo intestinal gel infusion, and both effects were prolonged for at least 12 months, although it may take several months until real benefits are noted [123, 124]. Recently, results from a larger sample of patients in an open-label study confirmed these results, with a benefit that was sustained throughout a period of 54 weeks [125]. Taken together, these data support the use of levodopa–carbidopa intestinal gel as a viable alternative to surgery, and possibly as an option for those unsuitable for surgery. Nonetheless, it is an invasive procedure and the implications of wearing an infusion system, including possible device malfunctioning, are not minor. In the aforementioned study, two (3%) of 71 patients discontinued due to complications of surgery and 63 (89%) had device-related complications, including tube dislocations, percutaneous gastrojejunostomy insertion complications, stoma insertion complications, pump malfunctions, and pneumoperitoneum. The potential development of polyneuropathy has been suggested in some case reports [126,127,128,129]. Further safety studies will clarify these issues.
4.3 Apomorphine
Apomorphine is a short-acting D1/D2 dopamine agonist administered by subcutaneous continuous infusion. Additionally, apomorphine portable pens are currently available and can be considered as an on-demand treatment for patients with severe and unpredictable “off” periods (80–90% of patients experience an “on” response within 30 min of treatment). The reason why it is administered parenterally is its rapid sulfonation if swallowed; however, new formulations are being investigated, as discussed below. Apomorphine was licensed in 1993 and has been established in clinical practice for a long time, but evidence regarding its efficacy relied solely on open-label and observational studies. It is also highly effective for reducing dyskinesias and the levodopa dose in patients with severe motor complications, despite optimized oral or transdermal therapy.
Only recently, with the completion of the first randomized double-blind trial to investigate its efficacy, safety, and tolerability (TOLEDO study) over a 12-week period, which was conducted in PD patients with > 3 years disease duration plus motor fluctuations not controlled by medical treatment, was this evidence confirmed [130]. This study, in which 106 patients were assigned to apomorphine (3–8 mg/h) or placebo saline infusion (14–18 h per day) was a significant contribution, because it bridges the evidence gap around apomorphine utilization and opens an avenue towards its inclusion in future guidelines, which may facilitate its introduction in countries where it is not currently approved. Difficulties related to the injection system (i.e., technical aspects of the pump), the complexity of the initial titration schedule, the difficulty of tailing off levodopa and other oral dopamine agonists, the short duration of benefit, and the risk of skin nodules and ulceration, a consequence of the low pH necessary to maintain drug stability, may account for its limited acceptance and explain why it is not used so widely. Because it is a dopamine agonist, the side effects attributed to this drug class—of which some of the most serious were sedation, hypotension, and cardiac rhythm disturbances—may also manifest and contribute to the high dropout rate documented, which reached 25% in patients previously assigned to apomorphine and 34.1% in those who had been previously randomized to placebo, among patients who entered the TOLEDO open label phase [131].
Interestingly, a small retrospective study conducted in the UK analyzed 28 advanced PD patients receiving treatment with subcutaneous apomorphine (12 of whom had experienced impulsive compulsive behaviors before starting apomorphine) and found that in six of them there was a complete resolution with oral dopamine agonist dose reduction before apomorphine initiation and in the other six there was an improvement/stabilization under this therapy, while only one of the 16 with no previous history of impulsive compulsive behaviors developed this adverse event [132]. As previously mentioned, there is no effective treatment for impulsive compulsive behaviors and they may lead to serious complications, so a potential benefit of this drug may lead to its consideration in this specific patient population.
5 Future Directions
Besides the evidence-based therapies we have discussed here, there are a number of other therapies in development. A phase III study to determine whether a gastric-retentive accordion pill of levodopa/carbidopa is more effective than the carbidopa/levodopa IR in reducing motor fluctuations is currently ongoing. Besides the subcutaneous route for apomorphine administration, which has been associated with injection-site reactions and lower acceptance rates, a new sublingual apomorphine film strip (APL-130277) is now under development and has been designed to be taken up to five times a day, with a minimum 2-h dose interval. Like the pulmonary surface, the oral cavity mucosa allows for rapid absorption, and is thus attractive when exploring new drug formulations with the purpose of prompt on-demand delivery, which is necessary for both predictable (e.g., upon waking up in the morning) and unpredictable “off” episodes, without the former inconvenience associated with subcutaneous drug delivery. A 12-week, double-blind, placebo-controlled phase III trial has been conducted, and even though the initial results are promising (with benefits starting 15 min post-dose and sustained for 90 min, with mild to moderate and reversible side effects), further studies are needed and a 24-week open-label extension study (NCT02542696) is currently ongoing [103].
Recently, the FDA released a complete letter response stating that current evidence is insufficient to approve the apomorphine sublingual film NDA in its present form, requesting additional information and analyses, but no additional clinical trials were requested [133].
6 Conclusions
Nigrostriatal degeneration and resulting dopaminergic deficits underlie the classical motor symptoms of PD, thus the dopamine precursor levodopa became the mainstay of PD therapy. Levodopa has demonstrated robust efficacy; however, the emergence of motor complications is common with this drug, affecting most patients after 10 years [11]. Due to its potential dramatic impact on the QOL of patients, the development of motor complications represents a clinically meaningful disease milestone. Current therapeutic approaches for motor complications are grounded on modification of levodopa pharmacokinetics, new formulations that promote more constant blood levels, therapies sparing levodopa or blocking non-dopaminergic targets known to have an interplay in the pathogenesis of motor complications (such as NMDA receptors).
Interestingly, even after 50 years since its introduction, levodopa remains an evolving drug. Levodopa ER is now an alternative for patients with motor complications. Regarding levodopa-sparing therapy, the most commonly used drugs in clinical practice include dopamine agonists, MAO-B inhibitors, and COMT inhibitors. All these drugs display variable degrees of success and must be adapted to individual circumstances, tolerability, cost, and local availability. Studies on direct comparisons within drug classes are rare; however, some differences have emerged. Opicapone is a new COMT inhibitor with a higher COMT inhibition potency [70] and a longer half-life than entacapone, thus relaunching COMT inhibitors to the frontline of therapies addressing motor fluctuations. Safinamide and zonisamide provide mixed MAO-B inhibitor activity combined with dopaminergic and nondopaminergic actions, and are exclusively approved for patients with motor complications. Amantadine ER was recently approved and it is the first oral treatment with a proven benefit for both levodopa-induced dyskinesias and “off” time reduction.
For suitable PD patients with motor complications despite optimized medical therapy, invasive therapies such as DBS, intrajejunal levodopa, and subcutaneous apomorphine are valid alternatives to control motor fluctuations and dyskinesias, but they remain available only in specialized centers. There are no randomized studies comparing apomorphine infusion, levodopa infusion, and DBS—although evidence is more robust for the latter. The management of motor complications in patients with PD remains challenging, requiring a thorough knowledge of available evidence and an important amount of clinical experience.
References
Mayeux R, Marder K, Cote LJ, Denaro J, Hemenegildo N, Mejia H, et al. The frequency of idiopathic Parkinson’s disease by age, ethnic group, and sex in northern Manhattan, 1988–1993. Am J Epidemiol. 1995;142(8):820–7.
Lees AJ, Hardy J, Revesz T. Parkinson’s disease. Lancet. 2009;373(9680):2055–66. https://doi.org/10.1016/S0140-6736(09)60492-X.
Poewe W. Non-motor symptoms in Parkinson’s disease. Eur J Neurol. 2008;15(Suppl 1):14–20. https://doi.org/10.1111/j.1468-1331.2008.02056.x.
Schapira AHV, Emre M, Jenner P, Poewe W. Levodopa in the treatment of Parkinson’s disease. Eur J Neurol. 2009;16:982–9. https://doi.org/10.1111/j.1468-1331.2009.02697.x.
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M. Alpha-synuclein in Lewy bodies. Nature. 1997;388(6645):839–40. https://doi.org/10.1038/42166.
Yahr M, Duvoisin R, Schear M, Barrett R, Hoehn M. Treatment of parkinsonism with levodopa. Arch Neurol. 1969;21(4):343–54.
Cotzias GC, Papavasiliou PS, Gellene R. Modification of Parkinsonism—chronic treatment with l-dopa. N Engl J Med. 1969;280(7):337–45. https://doi.org/10.1056/NEJM196902132800701.
Jankovic J. Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79(4):368–76. https://doi.org/10.1136/jnnp.2007.131045.
Jankovic J, Stacy M. Medical management of levodopa-associated motor complications in patients with Parkinson’s disease. CNS Drugs. 2007;21(8):677–92. https://doi.org/10.2165/00023210-200721080-00005.
Stocchi F, Jenner P, Obeso JA. When do levodopa motor fluctuations first appear in Parkinson’s disease? Eur Neurol. 2010;63(5):257–66. https://doi.org/10.1159/000300647.
Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001;16(3):448–58. https://doi.org/10.1002/mds.1090.
Sharma JC, Ross IN, Rascol O, Brooks D. Relationship between weight, levodopa and dyskinesia: the significance of levodopa dose per kilogram body weight. Eur J Neurol. 2008;15(5):493–6. https://doi.org/10.1111/j.1468-1331.2008.02106.x.
Warren Olanow C, Kieburtz K, Rascol O, Poewe W, Schapira AH, Emre M, et al. Factors predictive of the development of Levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Mov Disord. 2013;28(8):1064–71. https://doi.org/10.1002/mds.25364.
Doi H, Sakakibara R, Sato M, Masaka T, Kishi M, Tateno A, et al. Plasma levodopa peak delay and impaired gastric emptying in Parkinson’s disease. J Neurol Sci. 2012;319(1–2):86–8. https://doi.org/10.1016/j.jns.2012.05.010.
Aquino CC, Fox SH. Clinical spectrum of levodopa-induced complications. Mov Disord. 2015;30(1):80–9. https://doi.org/10.1002/mds.26125.
Antonini A, Moro E, Godeiro C, Reichmann H. Medical and surgical management of advanced Parkinson’s disease. Mov Disord. 2018;33(6):900–8. https://doi.org/10.1002/mds.27340.
Fahn S, Oakes D, Shoulson I, Kieburtz K, Rudolph A, Lang A, et al. Levodopa and the progression of Parkinson’s disease. N Engl J Med. 2004;351(24):2498–508. https://doi.org/10.1056/NEJMoa033447.
PD Med Collaborative Group, Gray R, Ives N, Rick C, Patel S, Gray A, Jenkinson C, McIntosh E, Wheatley K, Williams A, Clarke CE. Long-term effectiveness of dopamine agonists and monoamine oxidase B inhibitors compared with levodopa as initial treatment for Parkinson’s disease (PD MED): a large, open-label, pragmatic randomised trial. Lancet. 2014;384(9949):1196–205. https://doi.org/10.1016/s0140-6736(14)60683-8.
Verschuur CVM, Suwijn SR, Boel JA, Post B, Bloem BR, van Hilten JJ, et al. Randomized delayed-start trial of levodopa in Parkinson’s disease. N Engl J Med. 2019;380(4):315–24. https://doi.org/10.1056/NEJMoa1809983.
Carter J, Nutt J, Woodward W, Hatcher L, Trotman T. Amount and distribution of dietary protein affects clinical response to levodopa in Parkinson’s disease. Neurology. 1989;39(4):552–6.
Nutt J, Woodward W, Hammerstad J, Carter J, Anderson J. The, “on–off” phenomenon in Parkinson’s disease. Relation to levodopa absorption and transport. N Engl J Med. 1984;310(8):483–8.
Wang L, Xiong N, Huang J, Guo S, Liu L, Han C, et al. Protein-restricted diets for ameliorating motor fluctuations in Parkinson’s disease. Front Aging Neurosci. 2017;9(206):1663–4365. https://doi.org/10.3389/fnagi.2017.00206.
Cereda E, Barichella M, Pedrolli C, Pezzoli G. Low-protein and protein-redistribution diets for Parkinson’s disease patients with motor fluctuations: a systematic review. Mov Disord. 2010;25(13):2021–34. https://doi.org/10.1002/mds.23226.
Mittur A, Gupta S, Modi NB. Pharmacokinetics of Rytary((R)), an extended-release capsule formulation of carbidopa–levodopa. Clin Pharmacokinet. 2017;56(9):999–1014. https://doi.org/10.1007/s40262-017-0511-y.
Yao HM, Hsu A, Gupta S, Modi NB. Clinical pharmacokinetics of IPX066: evaluation of dose proportionality and effect of food in healthy volunteers. Clin Neuropharmacol. 2016;39(1):10–7. https://doi.org/10.1097/WNF.0000000000000126.
Morgan JC, Dhall R, Rubens R, Khanna S, Gupta S. Dosing patterns during conversion to IPX066, extended-release carbidopa–levodopa (ER CD-LD), in Parkinson’s disease with motor fluctuations. Parkinsons Dis. 2018;2018:9763057. https://doi.org/10.1155/2018/9763057.
Pahwa R, Lyons KE, Hauser RA, Fahn S, Jankovic J, Pourcher E, et al. Randomized trial of IPX066, carbidopa/levodopa extended release, in early Parkinson’s disease. Parkinsonism Relat Disord. 2014;20(2):142–8. https://doi.org/10.1016/j.parkreldis.2013.08.017.
Hauser RA, Hsu A, Kell S, Espay AJ, Sethi K, Stacy M, et al. Extended-release carbidopa–levodopa (IPX066) compared with immediate-release carbidopa–levodopa in patients with Parkinson’s disease and motor fluctuations: a phase 3 randomised, double-blind trial. Lancet Neurol. 2013;12(4):346–56. https://doi.org/10.1016/S1474-4422(13)70025-5.
Stocchi F, Hsu A, Khanna S, Ellenbogen A, Mahler A, Liang G, et al. Comparison of IPX066 with carbidopa–levodopa plus entacapone in advanced PD patients. Parkinsonism Relat Disord. 2014;20(12):1335–40. https://doi.org/10.1016/j.parkreldis.2014.08.004.
Dhall R, Kreitzman DL. Advances in levodopa therapy for Parkinson disease: review of RYTARY (carbidopa and levodopa) clinical efficacy and safety. Neurology. 2016;86(14 Suppl 1):S13–24. https://doi.org/10.1212/WNL.0000000000002510.
Rascol O, Perez-Lloret S, Ferreira JJ. New treatments for levodopa-induced motor complications. Mov Disord. 2015;30(11):1451–60. https://doi.org/10.1002/mds.26362.
LeWitt PA, Hauser RA, Grosset DG, Stocchi F, Saint-Hilaire MH, Ellenbogen A, et al. A randomized trial of inhaled levodopa (CVT-301) for motor fluctuations in Parkinson’s disease. Mov Disord. 2016;31(9):1356–65. https://doi.org/10.1002/mds.26611.
LeWitt PA, Hauser RA, Pahwa R, Isaacson SH, Fernandez HH, Lew M, et al. Safety and efficacy of CVT-301 (levodopa inhalation powder) on motor function during off periods in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Neurol. 2019;18(2):145–54. https://doi.org/10.1016/S1474-4422(18)30405-8.
Mizuno Y, Yanagisawa N, Kuno S, Yamamoto M, Hasegawa K, Origasa H, et al. Randomized, double-blind study of pramipexole with placebo and bromocriptine in advanced Parkinson’s disease. Mov Disord. 2003;18(10):1149–56. https://doi.org/10.1002/mds.10508.
Moller JC, Oertel WH, Koster J, Pezzoli G, Provinciali L. Long-term efficacy and safety of pramipexole in advanced Parkinson’s disease: results from a European multicenter trial. Mov Disord. 2005;20(5):602–10. https://doi.org/10.1002/mds.20397.
Lieberman A, Olanow CW, Sethi K, Swanson P, Waters CH, Fahn S, et al. A multicenter trial of ropinirole as adjunct treatment for Parkinson’s disease. Ropinirole Study Group. Neurology. 1998;51(4):1057–62.
Fox SH, Katzenschlager R, Lim SY, Barton B, de Bie RMA, Seppi K, et al. International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018;33(8):1248–66. https://doi.org/10.1002/mds.27372.
Mizuno Y, Nomoto M, Hasegawa K, Hattori N, Kondo T, Murata M, et al. Rotigotine vs ropinirole in advanced stage Parkinson’s disease: a double-blind study. Parkinsonism Relat Disord. 2014;20(12):1388–93. https://doi.org/10.1016/j.parkreldis.2014.10.005.
Poewe WH, Rascol O, Quinn N, Tolosa E, Oertel WH, Martignoni E, et al. Efficacy of pramipexole and transdermal rotigotine in advanced Parkinson’s disease: a double-blind, double-dummy, randomised controlled trial. Lancet Neurol. 2007;6(6):513–20. https://doi.org/10.1016/S1474-4422(07)70108-4.
Trenkwalder C, Kies B, Dioszeghy P, Hill D, Surmann E, Boroojerdi B, et al. Rotigotine transdermal system for the management of motor function and sleep disturbances in Parkinson’s disease: results from a 1-year, open-label extension of the RECOVER study. Basal Ganglia. 2012;2(2):79–85. https://doi.org/10.1016/j.baga.2012.05.009.
Trenkwalder C, Kies B, Rudzinska M, Fine J, Nikl J, Honczarenko K, et al. Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord. 2011;26(1):90–9. https://doi.org/10.1002/mds.23441.
Stocchi F, Giorgi L, Hunter B, Schapira AH. PREPARED: comparison of prolonged and immediate release ropinirole in advanced Parkinson’s disease. Mov Disord. 2011;26(7):1259–65. https://doi.org/10.1002/mds.23498.
Poewe W, Rascol O, Barone P, Hauser RA, Mizuno Y, Haaksma M, et al. Extended-release pramipexole in early Parkinson disease: a 33-week randomized controlled trial. Neurology. 2011;77(8):759–66. https://doi.org/10.1212/WNL.0b013e31822affb0.
Frampton JE. Pramipexole extended-release: a review of its use in patients with Parkinson’s disease. Drugs. 2014;74(18):2175–90. https://doi.org/10.1007/s40265-014-0322-5.
Hauser RA, Rascol O, Korczyn AD, Jon Stoessl A, Watts RL, Poewe W, et al. Ten-year follow-up of Parkinson’s disease patients randomized to initial therapy with ropinirole or levodopa. Mov Disord. 2007;22(16):2409–17. https://doi.org/10.1002/mds.21743.
Chaudhuri KR, Todorova A, Nirenberg MJ, Parry M, Martin A, Martinez-Martin P, et al. A pilot prospective, multicenter observational study of dopamine agonist withdrawal syndrome in Parkinson’s disease. Mov Disord Clin Pract. 2015;2(2):170–4. https://doi.org/10.1002/mdc3.12141.
Nirenberg MJ. Dopamine agonist withdrawal syndrome: implications for patient care. Drugs Aging. 2013;30(8):587–92. https://doi.org/10.1007/s40266-013-0090-z.
Patel S, Garcia X, Mohammad ME, Yu XX, Vlastaris K, O’Donnell K, et al. Dopamine agonist withdrawal syndrome (DAWS) in a tertiary Parkinson disease treatment center. J Neurol Sci. 2017;379:308–11. https://doi.org/10.1016/j.jns.2017.06.022.
Rabinak CA, Nirenberg MJ. Dopamine agonist withdrawal syndrome in Parkinson disease. Arch Neurol. 2010;67(1):58–63. https://doi.org/10.1001/archneurol.2009.294.
Zanettini R, Antonini A, Gatto G, Gentile R, Tesei S, Pezzoli G. Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med. 2007;356(1):39–46. https://doi.org/10.1056/NEJMoa054830.
Fitzsimmons PR, Blayney S, Mina-Corkill S, Scott GO. Older participants are frequently excluded from Parkinson’s disease research. Parkinsonism Relat Disord. 2012;18(5):585–9. https://doi.org/10.1016/j.parkreldis.2012.03.003.
Stowe RL, Ives NJ, Clarke C, van Hilten J, Ferreira J, Hawker RJ, et al. Dopamine agonist therapy in early Parkinson’s disease. Cochrane Database Syst Rev. 2008;2:CD006564. https://doi.org/10.1002/14651858.cd006564.pub2.
Silver D. Impact of functional age on the use of dopamine agonists in patients with Parkinson disease. Neurologist. 2006;12(4):214–23.
Castro ES, Santos-Garcia D, de Deus Fonticoba T, Exposito Ruiz I, Tunas Gesto C, Arribi MM. Causes and factors related to dopamine agonist withdrawal in Parkinson’s disease. Brain Behav. 2016;6(7):e00453. https://doi.org/10.1002/brb3.453.
Shulman L, Minagar A, Rabinstein A, Weiner W. The use of dopamine agonists in very elderly patients with Parkinson’s disease. Mov Disord. 2000;15(4):664–8.
Makumi CW, Asgharian A, Ellis J, Shaikh S, Jimenez T, VanMeter S. Long-term, open-label, safety study of once-daily ropinirole extended/prolonged release in early and advanced Parkinson’s disease. Int J Neurosci. 2016;126(1):30–8. https://doi.org/10.3109/00207454.2014.991924.
Katzenschlager R, Head J, Schrag A, Ben-Shlomo Y, Evans A, Lees AJ, et al. Fourteen-year final report of the randomized PDRG-UK trial comparing three initial treatments in PD. Neurology. 2008;71(7):474–80. https://doi.org/10.1212/01.wnl.0000310812.43352.66.
Hely MA, Morris JG, Reid WG, Trafficante R. Sydney Multicenter Study of Parkinson’s disease: non-l-dopa-responsive problems dominate at 15 years. Mov Disord. 2005;20(2):190–9. https://doi.org/10.1002/mds.20324.
Constantinescu R, Romer M, McDermott MP, Kamp C, Kieburtz K, Group C-PIotPS. Impact of pramipexole on the onset of levodopa-related dyskinesias. Mov Disord. 2007;22(9):1317–9. https://doi.org/10.1002/mds.21292.
Kuoppamaki M, Leinonen M, Poewe W. Efficacy and safety of entacapone in levodopa/carbidopa versus levodopa/benserazide treated Parkinson’s disease patients with wearing-off. J Neural Transm (Vienna). 2015;122(12):1709–14. https://doi.org/10.1007/s00702-015-1449-6.
Rinne UK, Larsen JP, Siden A, Worm-Petersen J. Entacapone enhances the response to levodopa in parkinsonian patients with motor fluctuations. Nomecomt Study Group. Neurology. 1998;51(5):1309–14. https://doi.org/10.1212/WNL.51.5.1309.
Poewe WH, Deuschl G, Gordin A, Kultalahti ER, Leinonen M, Celomen Study Group. Efficacy and safety of entacapone in Parkinson’s disease patients with suboptimal levodopa response: a 6-month randomized placebo-controlled double-blind study in Germany and Austria (Celomen study). Acta Neurol Scand. 2002;105(4):245–55. https://doi.org/10.1034/j.1600-0404.2002.1o174.x.
Brooks DJ. Entacapone is beneficial in both fluctuating and non-fluctuating patients with Parkinson’s disease: a randomised, placebo controlled, double blind, six month study. J Neurol Neurosurg Psychiatry. 2003;74(8):1071–9. https://doi.org/10.1136/jnnp.74.8.1071.
Rascol O, Barone P, Behari M, Emre M, Giladi N, Olanow CW, et al. Perampanel in Parkinson disease fluctuations: a double-blind randomized trial with placebo and entacapone. Clin Neuropharmacol. 2012;35(1):15–20. https://doi.org/10.1097/WNF.0b013e318241520b.
Stocchi F, Rascol O, Kieburtz K, Poewe W, Jankovic J, Tolosa E, et al. Initiating levodopa/carbidopa therapy with and without entacapone in early Parkinson disease: the STRIDE-PD study. Ann Neurol. 2010;68(1):18–27. https://doi.org/10.1002/ana.22060.
Tolosa E, Hernandez B, Linazasoro G, Lopez-Lozano JJ, Mir P, Marey J, et al. Efficacy of levodopa/carbidopa/entacapone versus levodopa/carbidopa in patients with early Parkinson’s disease experiencing mild wearing-off: a randomised, double-blind trial. J Neural Transm (Vienna). 2014;121(4):357–66. https://doi.org/10.1007/s00702-013-1114-x.
Korhonen P, Kuoppamaki M, Prami T, Hoti F, Christopher S, Ellmen J, et al. Entacapone and prostate cancer risk in patients with Parkinson’s disease. Mov Disord. 2015;30(5):724–8. https://doi.org/10.1002/mds.26140.
Major JM, Dong D, Cunningham F, By K, Hur K, Shih DC, et al. Entacapone and prostate cancer in Parkinson’s disease patients: a large Veterans Affairs healthcare system study. Parkinsonism Relat Disord. 2018;53:46–52.
Ferreira JJ, Lees A, Rocha J-F, Poewe W, Rascol O, Soares-da-Silva P. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, double-blind, controlled trial. Lancet Neurol. 2016;15(2):154–65. https://doi.org/10.1016/s1474-4422(15)00336-1.
Ferreira JJ, Rocha JF, Falcao A, Santos A, Pinto R, Nunes T, et al. Effect of opicapone on levodopa pharmacokinetics, catechol-O-methyltransferase activity and motor fluctuations in patients with Parkinson’s disease. Eur J Neurol. 2015;22(5):815–825, e56. https://doi.org/10.1111/ene.12666.
Lees AJ, Ferreira J, Rascol O, Poewe W, Rocha JF, McCrory M, et al. Opicapone as adjunct to levodopa therapy in patients with Parkinson disease and motor fluctuations: a randomized clinical trial. JAMA Neurol. 2017;74(2):197–206. https://doi.org/10.1001/jamaneurol.2016.4703.
Ferreira J, Poewe W, Rascol O, Costa R, Arbe E, Rocha J, et al. Relationship between patient global impression of change and other efficacy endpoints in Parkinson’s disease: a post-hoc analysis from combined BIPARK-I and II [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/relationship-between-patient-global-impression-of-change-and-other-efficacy-endpoints-in-parkinsons-disease-a-post-hoc-analysis-from-combined-bipark-i-and-ii/. Accessed March 8, 2019.
Larsen JP, Worm-Petersen J, Siden A, Gordin A, Reinikainen K, Leinonen M, et al. The tolerability and efficacy of entacapone over 3 years in patients with Parkinson’s disease. Eur J Neurol. 2003;10(2):137–46. https://doi.org/10.1046/j.1468-1331.2003.00559.x.
Elmer LW. Rasagiline adjunct therapy in patients with Parkinson’s disease: post hoc analyses of the PRESTO and LARGO trials. Parkinsonism Relat Disord. 2013;19(11):930–6. https://doi.org/10.1016/j.parkreldis.2013.06.001.
Parkinson Study Group. A randomized placebo-controlled trial of rasagiline in levodopa-treated patients with Parkinson disease and motor fluctuations: the PRESTO study. Arch Neurol. 2005;62(2):241–8. https://doi.org/10.1001/archneur.62.2.241.
Rascol O, Brooks DJ, Melamed E, Oertel W, Poewe W, Stocchi F, et al. Rasagiline as an adjunct to levodopa in patients with Parkinson’s disease and motor fluctuations (LARGO, Lasting effect in Adjunct therapy with Rasagiline Given Once daily, study): a randomised, double-blind, parallel-group trial. Lancet. 2005;365(9463):947–54. https://doi.org/10.1016/s0140-6736(05)71083-7.
Richard IH, Kurlan R, Tanner C, Factor S, Hubble J, Suchowersky O, et al. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson’s disease. Parkinson Study Group. Neurology. 1997;48(4):1070–7.
Panisset M, Chen JJ, Rhyee SH, Conner J, Mathena J, STACCATO study investigators. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014;34(12):1250–8. https://doi.org/10.1002/phar.1500.
Finberg JP, Gillman K. Selective inhibitors of monoamine oxidase type B and the “cheese effect”. Int Rev Neurobiol. 2011;100:169–90. https://doi.org/10.1016/B978-0-12-386467-3.00009-1.
Borgohain R, Szasz J, Stanzione P, Meshram C, Bhatt M, Chirilineau D, et al. Randomized trial of safinamide add-on to levodopa in Parkinson’s disease with motor fluctuations. Mov Disord. 2014;29(2):229–37. https://doi.org/10.1002/mds.25751.
Stocchi F, Borgohain R, Onofrj M, Schapira AH, Bhatt M, Lucini V, et al. A randomized, double-blind, placebo-controlled trial of safinamide as add-on therapy in early Parkinson’s disease patients. Mov Disord. 2012;27(1):106–12. https://doi.org/10.1002/mds.23954.
Schapira AH, Fox SH, Hauser RA, Jankovic J, Jost WH, Kenney C, et al. Assessment of safety and efficacy of safinamide as a levodopa adjunct in patients with Parkinson disease and motor fluctuations: a randomized clinical trial. JAMA Neurol. 2017;74(2):216–24. https://doi.org/10.1001/jamaneurol.2016.4467.
Murata M, Hasegawa K, Kanazawa I, Fukasaka J, Kochi K, Shimazu R, et al. Zonisamide improves wearing-off in Parkinson’s disease: a randomized, double-blind study. Mov Disord. 2015;30(10):1343–50. https://doi.org/10.1002/mds.26286.
Kondo T, Mizuno Y, Japanese Istradefylline Study Group. A long-term study of istradefylline safety and efficacy in patients with Parkinson disease. Clin Neuropharmacol. 2015;38(2):41–6. https://doi.org/10.1097/wnf.0000000000000073.
Pilleri M, Antonini A. Therapeutic strategies to prevent and manage dyskinesias in Parkinson’s disease. Expert Opin Drug Saf. 2015;14(2):281–94. https://doi.org/10.1517/14740338.2015.988137.
Fahn S, Parkinson Study Group. Does levodopa slow or hasten the rate of progression of Parkinson’s disease? J Neurol. 2005;252(Suppl 4):IV37–42.
Calabresi P, Di Filippo M, Ghiglieri V, Picconi B. Molecular mechanisms underlying levodopa-induced dyskinesia. Mov Disord. 2008;23(Suppl 3):S570–9. https://doi.org/10.1002/mds.22019.
Nishijima H, Ueno T, Funamizu Y, Ueno S, Tomiyama M. Levodopa treatment and dendritic spine pathology. Mov Disord. 2018;33(6):877–88. https://doi.org/10.1002/mds.27172.
Parkinson Study Group. A randomized controlled trial comparing pramipexole with levodopa in early Parkinson’s disease: design and methods of the CALM-PD Study. Parkinson Study Group. Clin Neuropharmacol. 2000;23(1):34–44.
Whone AL, Watts RL, Stoessl AJ, Davis M, Reske S, Nahmias C, et al. Slower progression of Parkinson’s disease with ropinirole versus levodopa: the REAL-PET study. Ann Neurol. 2003;54(1):93–101. https://doi.org/10.1002/ana.10609.
Rascol O, Brooks DJ, Korczyn AD, De Deyn PP, Clarke CE, Lang AE. A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. N Engl J Med. 2000;342(20):1484–91. https://doi.org/10.1056/NEJM200005183422004.
Holloway RG. Pramipexole vs levodopa as initial treatment for Parkinson disease. Arch Neurol. 2004;61(7):1044–53. https://doi.org/10.1001/archneur.61.7.1044.
Zhou CQ, Lou JH, Zhang YP, Zhong L, Chen YL, Lu FJ, et al. Long-acting versus standard non-ergot dopamine agonists in Parkinson’s disease: a meta-analysis of randomized controlled trials. CNS Neurosci Ther. 2014;20(4):368–76. https://doi.org/10.1111/cns.12239.
Shen Z, Kong D. Meta-analysis of the adverse events associated with extended-release versus standard immediate-release pramipexole in Parkinson disease. Medicine (Baltimore). 2018;97(34):e11316. https://doi.org/10.1097/MD.0000000000011316.
Payer DE, Guttman M, Kish SJ, Tong J, Adams JR, Rusjan P, et al. D3 dopamine receptor-preferring [11C]PHNO PET imaging in Parkinson patients with dyskinesia. Neurology. 2016;86(3):224–30. https://doi.org/10.1212/WNL.0000000000002285.
Berthet A, Bezard E. Dopamine receptors and l-dopa-induced dyskinesia. Parkinsonism Relat Disord. 2009;15(Suppl 4):S8–12. https://doi.org/10.1016/S1353-8020(09)70827-2.
Giladi N, Ghys L, Surmann E, Boroojerdi B, Jankovic J. Effects of long-term treatment with rotigotine transdermal system on dyskinesia in patients with early-stage Parkinson’s disease. Parkinsonism Relat Disord. 2014;20(12):1345–51. https://doi.org/10.1016/j.parkreldis.2014.09.016.
Schrag A, Quinn N. Dyskinesias and motor fluctuations in Parkinson’s disease. A community-based study. Brain. 2000;123(Pt 11):2297–305. https://doi.org/10.1093/brain/123.11.2297.
Fox SH, Lang AE. ‘Don’t delay, start today’: delaying levodopa does not delay motor complications. Brain. 2014;137(Pt 10):2628–30. https://doi.org/10.1093/brain/awu212.
Cilia R, Akpalu A, Sarfo FS, Cham M, Amboni M, Cereda E, et al. The modern pre-levodopa era of Parkinson’s disease: insights into motor complications from sub-Saharan Africa. Brain. 2014;137(Pt 10):2731–42. https://doi.org/10.1093/brain/awu195.
Hattori N, Fujimoto K, Kondo T, Murata M, Stacy M. Patient perspectives on Parkinson’s disease therapy in Japan and the United States: results of two patient surveys. Patient Relat Outcome Meas. 2012;3:31–8. https://doi.org/10.2147/PROM.S29443.
Ory-Magne F, Corvol JC, Azulay JP, Bonnet AM, Brefel-Courbon C, Damier P, et al. Withdrawing amantadine in dyskinetic patients with Parkinson disease: the AMANDYSK trial. Neurology. 2014;82(4):300–7. https://doi.org/10.1212/WNL.0000000000000050.
Goetz CG, Stebbins GT, Chung KA, Hauser RA, Miyasaki JM, Nicholas AP, et al. Which dyskinesia scale best detects treatment response? Mov Disord. 2013;28(3):341–6. https://doi.org/10.1002/mds.25321.
Sawada H, Oeda T, Kuno S, Nomoto M, Yamamoto K, Yamamoto M, et al. Amantadine for dyskinesias in Parkinson’s disease: a randomized controlled trial. PLoS One. 2010;5(12):e15298. https://doi.org/10.1371/journal.pone.0015298.
Hubsher G, Haider M, Okun MS. Amantadine: the journey from fighting flu to treating Parkinson disease. Neurology. 2012;78(14):1096–9. https://doi.org/10.1212/WNL.0b013e31824e8f0d.
Oertel W, Eggert K, Pahwa R, Tanner CM, Hauser RA, Trenkwalder C, et al. Randomized, placebo-controlled trial of ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 3). Mov Disord. 2017;32(12):1701–9. https://doi.org/10.1002/mds.27131.
Isaacson SH, Fahn S, Pahwa R, Tanner CM, Espay AJ, Trenkwalder C, et al. Parkinson’s patients with dyskinesia switched from immediate release amantadine to open-label ADS-5102. Mov Disord Clin Pract. 2018;5(2):183–90. https://doi.org/10.1002/mdc3.12595.
Pahwa R, Tanner CM, Hauser RA, Sethi K, Isaacson S, Truong D, et al. Amantadine extended release for levodopa-induced dyskinesia in Parkinson’s disease (EASED Study). Mov Disord. 2015;30(6):788–95. https://doi.org/10.1002/mds.26159.
Hauser RA, Pahwa R, Tanner CM, Oertel W, Isaacson SH, Johnson R, et al. ADS-5102 (Amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 2 Study): interim results of an open-label safety study. J Parkinsons Dis. 2017;7(3):511–22. https://doi.org/10.3233/JPD-171134.
Utsumi H, Okuma Y, Kano O, Suzuki Y, Iijima M, Tomimitsu H, et al. Evaluation of the efficacy of pramipexole for treating levodopa-induced dyskinesia in patients with Parkinson’s disease. Intern Med. 2013;52(3):325–32. https://doi.org/10.2169/internalmedicine.52.8333.
Trenkwalder C, Stocchi F, Poewe W, Dronamraju N, Kenney C, Shah A, et al. Mavoglurant in Parkinson’s patients with l-Dopa-induced dyskinesias: two randomized phase 2 studies. Mov Disord. 2016;31(7):1054–8. https://doi.org/10.1002/mds.26585.
Svenningsson P, Rosenblad C, Af Edholm Arvidsson K, Wictorin K, Keywood C, Shankar B, et al. Eltoprazine counteracts l-DOPA-induced dyskinesias in Parkinson’s disease: a dose-finding study. Brain. 2015;138(Pt 4):963–73. https://doi.org/10.1093/brain/awu409.
Bezard E, Tronci E, Pioli EY, Li Q, Porras G, Bjorklund A, et al. Study of the antidyskinetic effect of eltoprazine in animal models of levodopa-induced dyskinesia. Mov Disord. 2013;28(8):1088–96. https://doi.org/10.1002/mds.25366.
Frazzitta G, Bertotti G, Riboldazzi G, Turla M, Uccellini D, Boveri N, et al. Effectiveness of intensive inpatient rehabilitation treatment on disease progression in parkinsonian patients: a randomized controlled trial with 1-year follow-up. Neurorehabil Neural Repair. 2012;26(2):144–50. https://doi.org/10.1177/1545968311416990.
Okun MS, Gallo BV, Mandybur G, Jagid J, Foote KD, Revilla FJ, et al. Subthalamic deep brain stimulation with a constant-current device in Parkinson’s disease: an open-label randomised controlled trial. Lancet Neurol. 2012;11(2):140–9. https://doi.org/10.1016/S1474-4422(11)70308-8.
Follett KA, Weaver FM, Stern M, Hur K, Harris CL, Luo P, et al. Pallidal versus subthalamic deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2010;362(22):2077–91. https://doi.org/10.1056/NEJMoa0907083.
Weaver FM, Follett KA, Stern M, Luo P, Harris CL, Hur K, et al. Randomized trial of deep brain stimulation for Parkinson disease: thirty-six-month outcomes. Neurology. 2012;79(1):55–65. https://doi.org/10.1212/WNL.0b013e31825dcdc1.
Schuepbach WM, Rau J, Knudsen K, Volkmann J, Krack P, Timmermann L, et al. Neurostimulation for Parkinson’s disease with early motor complications. N Engl J Med. 2013;368(7):610–22. https://doi.org/10.1056/NEJMoa1205158.
Odekerken VJ, van Laar T, Staal MJ, Mosch A, Hoffmann CF, Nijssen PC, et al. Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced Parkinson’s disease (NSTAPS study): a randomised controlled trial. Lancet Neurol. 2013;12(1):37–44. https://doi.org/10.1016/S1474-4422(12)70264-8.
Odekerken VJ, Boel JA, Schmand BA, de Haan RJ, Figee M, van den Munckhof P, et al. GPi vs STN deep brain stimulation for Parkinson disease: three-year follow-up. Neurology. 2016;86(8):755–61. https://doi.org/10.1212/WNL.0000000000002401.
Ferreira JJ, Katzenschlager R, Bloem BR, Bonuccelli U, Burn D, Deuschl G, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur J Neurol. 2013;20(1):5–15. https://doi.org/10.1111/j.1468-1331.2012.03866.x.
Kleiner-Fisman G, Herzog J, Fisman DN, Tamma F, Lyons KE, Pahwa R, et al. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord. 2006;21(Suppl 14):S290–304.
Olanow CW, Kieburtz K, Odin P, Espay AJ, Standaert DG, Fernandez HH, et al. Continuous intrajejunal infusion of levodopa–carbidopa intestinal gel for patients with advanced Parkinson’s disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014;13(2):141–9. https://doi.org/10.1016/S1474-4422(13)70293-X.
Fernandez HH, Standaert DG, Hauser RA, Lang AE, Fung VS, Klostermann F, et al. Levodopa–carbidopa intestinal gel in advanced Parkinson’s disease: final 12-month, open-label results. Mov Disord. 2015;30(4):500–9. https://doi.org/10.1002/mds.26123.
Antonini A, Fung VS, Boyd JT, Slevin JT, Hall C, Chatamra K, et al. Effect of levodopa–carbidopa intestinal gel on dyskinesia in advanced Parkinson’s disease patients. Mov Disord. 2016;31(4):530–7. https://doi.org/10.1002/mds.26528.
Sensi M, Cossu G, Mancini F, Pilleri M, Zibetti M, Modugno N, et al. Which patients discontinue? Issues on Levodopa/carbidopa intestinal gel treatment: Italian multicentre survey of 905 patients with long-term follow-up. Parkinsonism Relat Disord. 2017;38:90–2. https://doi.org/10.1016/j.parkreldis.2017.02.020.
Merola A, Romagnolo A, Zibetti M, Bernardini A, Cocito D, Lopiano L. Peripheral neuropathy associated with levodopa–carbidopa intestinal infusion: a long-term prospective assessment. Eur J Neurol. 2016;23(3):501–9. https://doi.org/10.1111/ene.12846.
Rispoli V, Simioni V, Capone JG, Golfre Andreasi N, Preda F, Sette E, et al. Peripheral neuropathy in 30 duodopa patients with vitamins B supplementation. Acta Neurol Scand. 2017;136(6):660–7. https://doi.org/10.1111/ane.12783.
Devigili G, Rinaldo S, Lettieri C, Eleopra R. Levodopa/carbidopa intestinal gel therapy for advanced Parkinson disease: AN early toxic effect for small nerve fibers? Muscle Nerve. 2016;54(5):970–2. https://doi.org/10.1002/mus.25377.
Katzenschlager R, Poewe W, Rascol O, Trenkwalder C, Deuschl G, Chaudhuri KR, et al. Apomorphine subcutaneous infusion in patients with Parkinson’s disease with persistent motor fluctuations (TOLEDO): a multicentre, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2018;17(9):749–59. https://doi.org/10.1016/S1474-4422(18)30239-4.
Dietrichs E, Odin P. Algorithms for the treatment of motor problems in Parkinson’s disease. Acta Neurol Scand. 2017;136(5):378–85. https://doi.org/10.1111/ane.12733.
Barbosa P, Lees AJ, Magee C, Djamshidian A, Warner TT. A retrospective evaluation of the frequency of impulsive compulsive behaviors in Parkinson’s disease patients treated with continuous waking day apomorphine pumps. Mov Disord Clin Pract. 2017;4(3):323–8. https://doi.org/10.1002/mdc3.12416.
Sunovion Receives Complete Response Letter from FDA for Apomorphine Sublingual Film (APL-130277) [press release]. Marlborough: Sunovion Pharmaceuticals; 2019. http://businesswire.com/news/home/20190130005919/en/Sunovion-Receives-Complete-Response-Letter-FDA-Apomorphine. Accessed Feb 26, 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors received no funding for this article from any entity in the public or private domains.
Conflict of interest
Verónica Cabreira has received financial support to attend scientific meetings from Roche. João Massano received advisor honoraria from Bial, Merck Sharp and Dohme, and Zambon; he received financial support to speak at or attend meetings from Bial, Boston Scientific, GE Healthcare, Grunenthal, Medtronic, and Novartis. Patrício Soares-da-Silva is employed by Bial—Portela & Cª, S.A.
Rights and permissions
About this article
Cite this article
Cabreira, V., Soares-da-Silva, P. & Massano, J. Contemporary Options for the Management of Motor Complications in Parkinson’s Disease: Updated Clinical Review. Drugs 79, 593–608 (2019). https://doi.org/10.1007/s40265-019-01098-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01098-w