Abstract
Larotrectinib (VITRAKVI®) is an orally administered, small molecule, highly-selective, tropomyosin receptor kinase (TRK) inhibitor that was developed by Loxo Oncology in collaboration with Bayer AG as a treatment for adult and paediatric patients whose cancers harbour neurotrophic receptor tyrosine kinase (NTRK) gene fusions. In November 2018 larotrectinib received its first global approval in the USA for the treatment of adult and paediatric patients with solid tumours that have a NTRK gene fusion without a known acquired resistance mutation, are metastatic or where surgical resection is likely to result in severe morbidity, and have no satisfactory alternative treatments or that have progressed following treatment. A registration application for the use of larotrectinib in paediatric and adult patients with locally advanced or metastatic solid tumours with NTRK gene fusion proteins has been submitted in the EU. This article summarizes the milestones in the development of larotrectinib leading to its first approval for the treatment of adult and paediatric patients with solid tumours that have NTRK gene fusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Oncogenic gene fusions involving the neurotrophic receptor tyrosine kinase (NTRK) genes encoding tropomyosin receptor kinases (TRK) A, TRKB and TRKC (i.e. NTRK1, NTRK2 and NTRK3, respectively) result in constitutively activated, ligand-independent downstream signalling of TRKs in a diverse spectrum of solid tumours in paediatric and adult patients [1,2,3]. TRKs are involved in growth, differentiation and survival of neurons, with TRK expression primarily limited to the nervous system after embryogenesis. NTRK gene fusions involve recurrent chromosomal rearrangements between an expressed 5′ partner (over 60 identified to date) and a 3′ partner encoding a tyrosine kinase, with these oncogenic fusions implicated in up to 1% of all solid tumours. However, this frequency is markedly higher (range 5 to ≥ 75%) in some rare paediatric (e.g. infantile fibrosarcoma, congenital mesoblastic nephroma, papillary thyroid cancer and spitzoid neoplasms) and paediatric/adult cancers (e.g. mammary analogue secretory carcinoma of the salivary gland, secretory carcinoma of the breast), with the presence of NTRK gene fusions highly characteristic of some cancers such as infantile fibrosarcoma. Hence, NTRK gene fusions represent a novel oncogenic driver for targeted antineoplastic therapy via inhibition of TRKs [1,2,3].

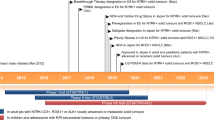
Key milestones in the development of larotrectinib for the treatment of advanced solid tumours harbouring a neurotrophic receptor tyrosine kinase (NTRK) gene fusion. BT breakthrough therapy, Est estimated, MAA Marketing Authorization Application, NDA New Drug Application, OD orphan drug
Larotrectinib (VITRAKVI®) is a small molecule, highly-selective, TRK inhibitor that was developed by Loxo Oncology in collaboration with Bayer AG as a treatment for adult and paediatric patients whose cancers have a specific genetic biomarker, namely NTRK gene fusions [4]. Based on pooled results from three open-label, single-arm, multicentre phase 1 and 2 trials (LOXO-TRK-14001, SCOUT and NAVIGATE trials), on 26 November 2018 larotrectinib received its first global approval (under accelerated approval) in the USA for the treatment of adult and paediatric patients with solid tumours that have a NTRK gene fusion without a known acquired resistance mutation, are metastatic or where surgical resection is likely to result in severe morbidity, and have no satisfactory alternative treatments or that have progressed following treatment [4, 5]. Select patients for treatment with larotrectinib based on the presence of an NTRK gene fusion in tumour specimens; an FDA-approved test for the detection of NTRK gene fusion is not currently available [4]. The recommended dosage of oral larotrectinib in adult and paediatric patients with a body surface area (BSA) of ≥ 1 m2 is 100 mg twice daily and in paediatric patients with a BSA of < 1 m2 is 100 mg/m2 twice daily (drug taken with or without food). Larotrectinib treatment should continue until disease progression or unacceptable toxicity occurs [4]. Prescribing information should be consulted regarding dosage modifications which may be required for adverse reactions and in special patient populations such as patients with hepatic impairment. In the EU, a Marketing Authorization Application has been submitted to the EMA for the use of larotrectinib in paediatric and adult patients with locally advanced or metastatic solid tumours with NTRK gene fusion [6]; larotrectinib has orphan drug designation for the treatment of soft tissue sarcomas [7] and salivary gland cancers [8] with NTRK-fusion mutations.
1.1 Company Agreements
In July 2013, Array BioPharma and Loxo Oncology entered into a multi-year license and drug discovery collaboration agreement, whereby Array BioPharma agreed to design, conduct and perform research and preclinical testing for certain compounds, including larotrectinib [9]. In November 2017, Loxo Oncology entered into an exclusive global development and commercialization agreement with Bayer AG for larotrectinib [10].

Chemical structure of larotrectinib
2 Scientific Summary
2.1 Pharmacodynamics
Larotrectinib is a highly selective, potent inhibitor of TRKA, TRKB and TRKC (in vitro 50% inhibitory constant 5–11 nmol/L), with minimal or no activity against other kinase and non-kinase targets [1, 2, 4, 11]. Inhibition of TRKs prevents TRK activation, resulting in both the induction of cellular apoptosis and the inhibition of cell growth in tumours that overexpress TRKs.
In vivo and in vitro, larotrectinib exhibited antitumour activity in cells with constitutive activation of TRK proteins resulting from gene fusions or deletion of a protein regulatory domain, or cells overexpressing TRK protein [1, 4, 11].
In vitro, larotrectinib exhibited minimal activity in cell lines with point mutations in the TRKA kinase domain, including the clinically identified acquired resistance mutation G595R [4, 12]. Clinically identified acquired resistance to larotrectinib associated with point mutations in the TRKC kinase domain included G632R, G696A and FD617L [4, 12].
At supratherapeutic doses (9 × recommended adult dose), larotrectinib does not prolong the QTc interval to any clinically relevant extent [4].
2.2 Pharmacokinetics
Oral larotrectinib exhibits dose proportional pharmacokinetics across a dose range of 100–400 mg (i.e. 1–4 × recommended adult dose) [4]. In adult patients receiving larotrectinib 100 mg twice daily, maximum plasma concentrations were attained in ≈ 1 h, with steady state plasma levels reached within 3 days. In healthy volunteers, the mean absolute bioavailability of oral larotrectinib was 34% and, after an intravenous dose, the mean volume of distribution was 48 L. Food had no clinically relevant effect on the pharmacokinetics of larotrectinib after an oral dose. In vitro, larotrectinib is 70% bound to plasma proteins, with binding independent of drug concentration [4].
The rate and extent of absorption of larotrectinib was similar in paediatric patients receiving oral larotrectinib 100 mg/m2 twice daily (maximum 100 mg twice daily) to that in adult patients receiving 100 mg twice daily [13]. There were also no apparent differences in the pharmacokinetics of larotrectinib between the capsule and tablet formulations or between different paediatric age groups [13].
Larotrectinib is primarily metabolized by CYP3A4 [4]. After oral administration of a radiolabeled 100 mg dose in healthy volunteers, unchanged larotrectinib and an O-linked glucuronide accounted for 19 and 26% of the major circulating radioactive drug components in plasma. Of this 100 mg dose, 58 and 39% was recovered in the faeces and urine, 5 and 20% of which was unchanged drug. After an oral dose in healthy volunteers, the mean clearance of larotrectinib was 98 L/h and the half-life was 2.9 h [4].
Larotrectinib pharmacokinetics are not affected to any clinically relevant extent by age (age range 28 days–82 years), gender, bodyweight or renal impairment [4]. Relative to patients with normal hepatic function, exposure to larotrectinib was increased by 1.3-, 2- and 3.2-fold in patients with mild (Child–Pugh class A), moderate (Child-Pugh class B) or severe (Child–Pugh class C) hepatic impairment, respectively; the starting dosage of larotrectinib should be reduced by 50% in patients with moderate to severe hepatic impairment [4].
Clinically relevant drug interactions may occur when larotrectinib is coadministered with strong CYP3A4 inhibitors (e.g. itraconazole) or inducers (e.g. rifampicin); coadministration of these agents with larotrectinib should be avoided [4]. If coadministration cannot be avoided, the dose of larotrectinib should be reduced by 50% when it’s coadministered with a strong CYP3A4 inhibitor and the dose of larotrectinib should be doubled when the drug is given concomitantly with a strong CYP3A4 inducer [4]; see prescribing information for further details.
Features and properties of larotrectinib
Alternative names | ARRY-470; LOXO-101; VITRAKVI® |
Class | Amides, antineoplastics, pyrazoles, pyrimidines, pyrrolidines, small molecules |
Mechanism of Action | TRKA receptor antagonists; TRKB receptor antagonists; TRKC receptor antagonists |
Route of Administration | Oral |
Pharmacodynamics | Binds to and inhibits TRKA, TRKB and TRKC, thereby preventing TRK activation, resulting in both the induction of cellular apoptosis and the inhibition of cell growth in tumours that overexpress TRK |
Pharmacokinetics | Linear pharmacokinetics across doe range of 100–400 mg (i.e. 1–4 × recommended adult dose); tmax ≈ 1 h; bioavailability 34%; volume of distribution 48 L (intravenous dose); metabolized primarily by CYP3A4; 58 and 39% of a dose recovered in faeces and urine; mean clearance 98 L/h; half-life 2.9 h |
Adverse reactions | |
Most frequent (≥ 20% of pts) | Fatigue, nausea, dizziness, vomiting, anaemia, increased transaminase levels, cough, constipation, diarrhoea |
ATC codes | |
WHO ATC code | L01X-E53 (larotrectinib) |
EphMRA ATC code | L1 (antineoplastic) |
Chemical name | (3S)-N-(5-((2R)-2-(2,5-Difluorophenyl)pyrrolidin-1-yl)pyrazolo(1,5-a)pyrimidin-3-yl)-3-hydroxypyrrolidine- 1-carboxamide |
2.3 Therapeutic Trials
2.3.1 SCOUT Trial
Oral larotrectinib was associated with a high objective response rate (93% of patients; 14/15 patients) at data cut-off (July 2017; median follow-up 5.6 months) in patients with solid tumours harbouring NTRK gene fusions in the prospective, open-label, dose-escalation phase (phase 1) [13]. The other patient with a TRK fusion-positive tumour had a partial response that became stable disease; this patient subsequently developed an NTRK3 mutation known to confer resistance to larotrectinib and experienced disease progression. All seven patients without documented NTRK gene fusion treated with larotrectinib experienced disease progression [13].
In this three-cohort, multicentre, phase 1/2 trial (the phase 1 expansion and phase 2 part are ongoing) eligible patients were aged 1 month–21 years, had a locally advanced or metastatic solid tumour or a primary CNS tumour that had relapsed, progressed or had an inadequate response to available therapies and for which no standard or systemic curative therapy existed [13]. Testing for NTRK gene fusion was only an eligibility criteria in infants aged 1 month to a year, although local NTRK gene fusion testing pre-enrolment meant that investigators enriched the study population with patients with TRK fusion cancer. After a protocol amendment in 2016, eligibility criteria were extended to include patients with locally advance infantile fibrosarcoma who would require disfiguring surgery to achieve complete resection of the tumour. In phase 1, the first cohort received doses ranging from 17 to 96% of the BSA-adjusted recommended adult phase 2 dose of oral larotrectinib 100 mg twice daily; the second cohort received doses ranging from 30 to 208% of the same BSA-adjusted adult dose; and the final cohort received 100 mg/m2 (maximum dose 100 mg) irrespective of age (equated to 173% of recommended adult phase 2 dose). Dose modifications and/or interruptions were permitted based on efficacy and toxicity, with treatment continued until disease progression or unacceptable toxicity occurred [13].
At data cut-off, tumour burden was reduced in all 15 evaluable patients with TRK fusion-positive tumours, irrespective of the specific NTRK gene fusion or whether patients had infantile fibrosarcoma or other soft tissue sarcomas [13]. Presurgical treatment with larotrectinib was a viable option in children (median age 2 years) who had locally advanced infantile fibrosarcoma (n = 3) or soft tissue sarcomas (n = 2) [14]. Of these five patients, three had a complete or near complete (> 98% treatment effect) pathologic response and were continuing in follow-up (minimum of 7–15 months post-surgery) without larotrectinib treatment, with the other two patients who had viable tumour at the time of resection continuing larotrectinib [14].
Key clinical trials of larotrectinib
Indication | Treatment | Phase | Status | Location(s) | Identifier | Sponsor |
|---|---|---|---|---|---|---|
Adult pts with advanced solid tumours harbouring NTRK gene fusion | LAR | 1 | Recruiting + ongoing | USA | NCT02122913; LOXO-TRK-14001 | Loxo Oncology Inc. |
Paediatric and adult pts (aged 1 day to 21 years) with advanced solid or primary CNS tumours | LAR | 1/2 | Recruiting + ongoing | Australia, Canada, Europe, Ireland, UK, USA | NCT02637687; LOXO-TRK-15003; SCOUT | Loxo Oncology Inc. |
Adult pts with advanced solid tumours (e.g. NSCLC, thyroid, salivary gland, colorectal, biliary, primary CNS) harbouring NTRK gene fusion | LAR | 2 (Basket) | Recruiting + ongoing | Asia, Europe, Ireland, UK, USA | NCT02576431; LOXO-TRK-15002; NAVIGATE | Loxo Oncology Inc. |
Targeted therapy directed by genetic testing in paediatric and adult pts (aged 12 months to 21 years) with advanced solid tumours, non-Hodgkin lymphoma or histiocytic disorders | Various including LAR | 2 | Recruiting + ongoing | USA, Puerto Rico | NCT03155620; NCI-2017-01251; APEC1621SC; Paediatric MATCH screening | National Cancer Institute |
Paediatric and adult pts (aged 12 months–21 years) with advanced solid tumours, non-Hodgkin lymphoma or histiocytic disorders harbouring NTRK gene fusion | LAR | 2 | Recruiting + ongoing | USA, Puerto Rico | NCT03213704; NCI-2017-01264; APEC1621A; Paediatric MATCH treatment | National Cancer Institute |
Targeted therapy directed by genetic testing in adult pts with advanced solid tumours, lymphomas or multiple myeloma | Various including LAR | 2 | Recruiting + ongoing | USA, Puerto Rico | NCT02465060; NCI-2015-00054; EAY131; MATCH screening | National Cancer Institute |
2.3.2 Combined Analyses for the Clinical Trial Program
In intent-to-treat analyses (n = 55) at primary data cut-off (July 2017), the centrally-assessed overall response rate (ORR; based on RECIST 1.1 criteria) was 75% (95% CI 61, 85) [primary endpoint for combined analysis], with the investigator-assessed ORR consistent with this (80%; 95% CI 67, 90) [12]. Responses occurred irrespective of TRK fusion characteristics, the patient’s age or the tumour type. By central assessment, complete responses, partial responses, stable disease and disease progression were achieved by 13, 62, 13 and 9% of patients, respectively; two patients included in the analysis withdrew early because of clinical deterioration. The median time to response was 1.8 months. The median duration of response and median progression-free survival had not been reached at a median follow-up of 8.3 and 9.9 months, respectively. At 1 year, responses were maintained in 71% of patients and 55% of patients remained progression free, with the response sustained after 27 months of larotrectinib therapy in the first enrolled patient with a TRK fusion-positive tumour. The majority of patients (86%) with a response at data cut-off continued to receive larotrectinib or had undergone surgery that was intended to be curative [12].
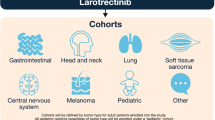
This primary dataset included the first 55 consecutive paediatric or adult patients with prospectively identified TRK fusion cancers that were enrolled (from March 2015 to February 2017) in phase 1 of the phase 1/2 SCOUT trial (phase 2 part in children had not yet started), and in the dose-escalation, phase 1 LOXO-TRK-14001 trial and phase 2 NAVIGATE (basket) trial [12]. Evaluated patients had 17 unique cancers, including mammary analogue secretory carcinoma of the salivary gland (12 patients), infantile fibrosarcoma (7), melanoma (4), and thyroid (5), colon (4), lung (4) or gastrointestinal (4) tumours. In NAVIGATE, adolescents and adults with a BSA of ≥ 1 m2 received the recommended dose of larotrectinib 100 mg twice daily and children with a BSA of < 1 m2 received 100 mg/m2, with treatment continued until disease progression or unacceptable toxicity occurred. In NAVIGATE, but not in the phase 1 studies, all patients had to have a documented NTRK gene fusion (TRKA, TRKB and TRKC in 45, 2 and 53% of patients, respectively), as determined by next-generation sequencing or fluorescence in situ hybridization [12].
At a data cut-off of July 2018, the ORR was 81% (95% CI 72, 88), with complete and partial responses occurring in 17 and 63% of patients, in an updated analysis of 109 evaluable paediatric and adult patients with TRK fusions across 24 unique cancer types. After a median follow-up of 17.6 months in the primary dataset comprising 55 patients, the median duration of response had not been reached [15].
2.3.3 Adverse Events
Oral larotrectinib had a manageable safety and tolerability profile in patients with various unresectable or metastatic solid tumours (60% harbouring NTRK gene fusions) and no satisfactory alternative treatment options or disease progression following treatment, based on a pooled analysis of three trials [dose-finding LOXO-TRK-14001 (n = 70), SCOUT (n = 43) [13] and NAVIGATE (n = 63) [12]] [4]. In this pooled analysis [4], 40% of patients had > 6 months’ exposure to larotrectinib and 20% had > 1 year of exposure. The median age of patients was 51 years (25% were aged ≤ 18 years) and 52% of patients were male. The most common tumours were soft tissue sarcoma (16%), salivary gland (11%), lung (10%), thyroid (9%), colon (8%), infantile fibrosarcoma (8%), primary CNS (7%) and melanoma (5%). Most adults (80%) received larotrectinib 100 mg twice daily (dosage range 50–200 mg twice daily); 68% of paediatric patients (aged ≤ 18 years) received larotrectinib 100 mg/m2 twice daily (maximum dose 100 mg twice daily) [dosage range 9.6–120 mg/m2 twice daily] [4].
The most common (frequency ≥ 20%) adverse reactions of any grade occurring in larotrectinib recipients were increased AST level (45%), increased ALT level (45%), anaemia (42%), fatigue (37%), nausea (29%), dizziness (28%), vomiting (26%), cough (26%), constipation (23%) and diarrhoea (22%) [4]. The most common adverse reactions leading to treatment discontinuation (1–2% of patients for each) were brain edema, intestinal perforation, pericardial effusion, pleural effusion, small intestinal obstruction, dehydration, fatigue, increased ALT or AST level, enterocutaneous fistula, increased amylase, muscular weakness, abdominal pain, asthenia, decreased appetite, dyspnea, hyponatraemia, jaundice, syncope, vomiting acute myeloid leukaemia and nausea. Adverse reactions leading to dose interruptions or reductions that occurred in ≥ 3% of larotrectinib recipients were increased ALT level (6%), increased AST level (6%) and dizziness (3%), most of which occurred during the first 3 months of exposure [4].
Grades 3 or 4 adverse reactions occurred in 51% of larotrectinib recipients and resulted in dose interruption or reductions in 37% of patients, with 13% of patients permanently discontinuing larotrectinib because of these reactions [4]. The most common serious adverse reactions (frequency ≥ 2%) were pyrexia, diarrhoea, sepsis, abdominal pain, dehydration, cellulitis and vomiting.
Adverse reactions with warnings and precautions include neurotoxicity, hepatotoxicity and embryo-foetal toxicity; the latter was based on literature reports in humans with congenital mutations leading to changes in TRK signaling, data from animal studies and the mechanism of action of larotrectinib [4]. In the pooled analysis, neurologic adverse events of any grade, grade 3 and grade 4 occurred in 53, 6 and 0.6% of patients (the latter was a single case of grade 4 encephalopathy), respectively, with most events (65%) occurring during the initial 3 months of larotrectinib treatment. Increased transaminase levels of any grade, increased transaminase levels of grade 3 and increased AST of grade 4 (single patient) occurred in 45, 6 and 0.6% of patients, respectively, with a median time to onset of increased AST or ALT of 2 months. Increased AST and ALT levels resulted in dose modifications in 4 and 6% of larotrectinib recipients, with 2% of patients permanently discontinuing treatment because of these increases. Patients should be advised of the potential risks of neurological adverse reactions, hepatoxicity adverse reactions and embryo-fetal toxicity (females should use effective contraception); monitor liver tests (e.g. ALT and AST) every 2 weeks during the first month, then monthly and as clinically indicated [4].
2.4 Companion Diagnostic
An FDA-approved test for the detection of NTRK gene fusion is not currently available [4]. A larotrectinib companion diagnostic is being developed by Illumina in collaboration with Loxo Oncology to identify patients with cancer who will best respond to treatment with larotrectinib; TruSight™ Tumour 170 is a comprehensive, next-generation sequencing-based test that identifies point mutations, fusions, amplifications and splice variants in 170 genes associated with common solid tumours [16].
2.5 Ongoing Clinical Trials
Clinical trials are ongoing, including LOXO-TRK-14001 (NCT02122913), SCOUT (NCT02637687) and NAVIGATE (NCT02576431). The paediatric MATCH treatment trial (NCT03213704) will evaluate larotrectinib treatment in patients with solid tumours, non-Hodgkin lymphoma or histiocytic disorders harbouring NTRK gene fusions that have spread to other places in the body and have come back or do not respond to treatment. Larotrectinib will also be evaluated in the MATCH screening trial (NCT02465060) in adults and the paediatric MATCH screening trial (NCT0315560) in patients aged 12 months–21 years, which are both designed to evaluate targeted therapy directed by genetic testing in treating various advance refractory cancers.
3 Current Status
Larotrectinib received its first global approval on 26 November 2018 in the USA for the treatment of adult and paediatric patients with solid tumours that have a NTRK gene fusion without a known acquired resistance mutation, are metastatic or where surgical resection is likely to result in severe morbidity, and have no satisfactory alternative treatments or that have progressed following treatment.
References
Berger S, Martens UM, Bochum S. Larotrectinib (LOXO-101). Recent Results Cancer Res. 2018;211:141–51.
Vaishnavi A, Le A, Doebele RC. TRKing down an old oncogene in a new era of targeted therapy. Cancer Discov. 2015;5(1):25–34.
Kummar S, Lassen UN. TRK inhibition: a new tumor-agnostic treatment strategy. Target Oncol. 2018;13(5):545–56.
Loxo Oncology. Vitrakvi® (Larotrectinib): US prescribing information. 2018. https://www.fda.gov/. Accessed 04 Dec 2018.
FDA. FDA approves an oncology drug that targets a key genetic driver of cancer, rather than a specific type of tumor [media release]. 2018. https://www.fda.gov/. Accessed 2018.
Loxo Oncology. Loxo oncology announces submission of European Marketing Authorization Application for larotrectinib [media release]. 2018. http://www.loxooncology.com. Accessed 06 Dec 2018.
Loxo Oncology. Loxo Oncology announces EMA Orphan Drug Designation granted to LOXO-101 for treatment of soft tissue sarcoma [media release]. 2016. http://www.loxooncology.com. Accessed 06 Dec 2018.
Agency EM. Larotrectinib: orphan designation EU/3/18/1995. 2018. http://www.ema.europa.eu/. Accessed 06 Dec 2018.
Array BioPharma Inc. Loxo Oncology and Array BioPharma announce license and collaboration agreement [media release]. 2013. http:http://www.arraybiopharma.com. Accessed 03 Dec 2018.
Bayer. Bayer and Loxo Oncology to develop and commercialize two therapies that selectively target genetic drivers of cancer [media release]. 2017. http://www.bayer.com. Accessed 03 Dec 2018.
Doebele RC, Davis LE, Vaishnavi A, et al. An oncogenic NTRK fusion in a patient with soft-tissue sarcoma with response to the tropomyosin-related kinase inhibitor LOXO-101. Cancer Discov. 2015;5(10):1049–57.
Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. New Engl J Med. 2018;378(8):731–9.
Laetsch TW, DuBois SG, Mascarenhas L, et al. Larotrectinib for paediatric solid tumours harbouring NTRK gene fusions: phase 1 results from a multicentre, open-label, phase 1/2 study. Lancet Oncol. 2018;19(5):705–14.
DuBois SG, Laetsch TW, Federman N, et al. The use of neoadjuvant larotrectinib in the management of children with locally advanced TRK fusion sarcomas. Cancer. 2018;124(21):4241–7.
Lassen UN, Albert CM, Kummar S, et al. Larotrectinib efficacy and safety in TRK fusion cancer: an expanded clinical dataset showing consistency in an age and tumor agnostic approach [abstract no. 409O plus oral presentation]. Ann Oncol. 2018;29(Suppl 8):133–48.
Loxo Oncology. Loxo Oncology and illumina to partner on developing next-generation sequencing-based pan-cancer companion diagnostics [media release]. 2018. http://ir.loxooncology.com. Accessed 03 Dec 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the author on the basis of scientific completeness and accuracy. Lesley Scott is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Scott, L.J. Larotrectinib: First Global Approval. Drugs 79, 201–206 (2019). https://doi.org/10.1007/s40265-018-1044-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-1044-x