Abstract
Lidocaine is an amide local anaesthetic initially used intravenously as an antiarrhythmic agent. At some point it was proposed that intravenous lidocaine (IVL) had an analgesic effect that could be potentially beneficial in perioperative settings. Since these preliminary reports, a large body of evidence confirmed that IVL had anti-inflammatory and opiate-sparing effects, a combination of characteristics leading to an array of effects such as a decrease in postoperative pain and opiate consumption, and a reduction in the duration of digestive ileus. Additional studies demonstrated IVL to possess antithrombotic, antimicrobial and antitumoral effects. Beneficial effects of IVL have been characterized in abdominal surgery but remain controversial in other types of surgeries. Because the quality of evidence was limited, due to inconsistency, imprecision and study quality, recent conclusions from meta-analysis pooling together all types of surgery stated the uncertainty about IVL benefits. Additional indications such as the prevention of propofol-induced injection pain, prevention of hyperalgesia, protection against bronchial reactivity by bronchotracheal relaxation during surgery, and the increase in depth of general anaesthesia have since emerged. IVL is rapidly distributed in the body and metabolized by the liver. With the commonly recommended doses, lidocaine’s therapeutic index remains very high and the plasma concentrations stay largely below the cardiotoxic and neurotoxic threshold levels, a notion that may be used by clinicians to draw conclusions on the benefit-risk profile of IVL in comparison to other analgesic strategies. The purpose of this review is to address the pharmacokinetic and pharmacodynamic properties of lidocaine in healthy and pathological conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intravenous lidocaine (IVL) has many properties that can be beneficial when used in a perioperative setting. |
The clinical efficacy of IVL seems especially clear in abdominal surgery where it may reduce pain intensity and accelerate postoperative recovery. Benefits in other types of surgeries are uncertain. |
Knowledge of the pharmacokinetic properties of IVL will lead to its safer use within the perioperative period and help clinicians draw conclusions on its benefit-risk profile in comparison with other analgesic strategies. |
1 Introduction
Lidocaine is an amide local anaesthetic and a Class 1b antiarrhythmic agent, first synthesized in 1942, and after approval for human use was launched in 1948 in Sweden [1]. The first observations of postoperative analgesic effects of perioperative intravenous lidocaine (IVL) were initially proposed in 1951 [2]; subsequently many more enthusiastic reports followed. Postoperative formal clinical evaluations in the perioperative setting were conducted in the late 1950s where IVL was demonstrated to have a postoperative analgesic effect without posing the risk of respiratory depression, reducing the occurrence of postoperative nausea and vomiting (PONV), and helping patients into a rapid course of post-surgical recovery [3]. IVL also potentiated the depth of anaesthesia and led to a better tolerance of endotracheal intubation in women who underwent intraperitoneal pelvic procedures under thiopental/nitrous-oxide/succinylcholine anaesthesia [4]. Since these preliminary reports, more than 2000 papers have been published on the topic, contributing enormously to our understanding of lidocaine. Meanwhile, the development of new intravenous and volatile anaesthetic agents, with improved pharmacological practicality and patient tolerance profiles, has pushed aside the use of lidocaine in the general perioperative setting. With a rise in the concept of ‘day-surgery’ and high expectations from Enhanced Recovery After Surgery programs (ERAS), IVL can play a pivotal role [5]. For example, studies with a moderate quality of evidence show that patients undergoing abdominal surgery and receiving IVL infusion may have lower relative pain scores, less postoperative analgesic requirements, lower incidence of nausea and faster recovery of bowel function [6]. Concomitantly, due to its analgesic properties, IVL can be expected to lead to a reduction in opiate-related side effects that may hamper the post-surgical recovery process [7, 8]. Finally, lidocaine infusion is a technique that can assist in further development of ‘opiate-free anaesthesia’, although its relative contribution remains to be investigated [9, 10].
Despite accumulating data from clinical trials and recommendations by expert consensus groups, IVL remains underutilized. A recent survey with French university hospital abdominal surgery departments indicated that only 64% were using IVL to improve postoperative pain and recovery [11]. This value is probably even lower in other European neighbouring countries. Insufficient knowledge on the basic pharmacology and properties of IVL are among the principal factors that restrain a greater adoption of IVL into common surgical practice. Furthermore, several authors have reiterated the rather off-label use of IVL in the perioperative setting [11, 12], suggesting a need for further analysis of the obstacles that hinder its use in common practice.
The purpose of this review is to provide a practical guide on lidocaine’s pharmacokinetic and pharmacodynamic properties relevant to clinical settings, to ultimately highlight indications for proper use of IVL within the perioperative period.
2 Pharmacokinetics
Chemically, lidocaine is a 2-diethylaminoaceto-2′, 6′-xylidide, with the empirical molecular formula of C14H22N2O and a molecular mass of 234.3 g/mole (Fig. 1).
2.1 Overview
Pharmacokinetic properties are historically derived from studies using IVL as an antiarrhythmic agent [1, 13]. In this setting, lidocaine plasma concentrations between 1.4 µg/ml and 6.0 µg/ml are considered safe and effective. In healthy volunteers, the average dose associated with the occurrence of neurological symptoms (such as the risk of convulsions) is about 8 mg/kg [14, 15], corresponding to a plasmatic value of about 15 µg/ml [16]. First signs of cardiotoxicity were observed at plasma concentrations above 21 µg/ml [1].
Plasma concentrations of lidocaine decline biexponentially after its intravenous administration, suggesting a multicompartment model of lidocaine disposition into different organs [1, 17]. With a distribution half-life (t1/2α) of 5–8 min, the distribution starts from the vascular compartment into the peripheral tissues, passing first through highly perfused areas (heart, lung, liver, spleen), to the less perfused areas (muscles and adipose tissue). Post-mortem studies have subsequently demonstrated a three times higher blood concentration of lidocaine in the brain and the heart a few minutes post intravenous injection, relative to other organs [18, 19]. Autoradiography with labelled lidocaine in rats indicates that approximately one-third of lidocaine accumulates in the liver 15 min post-injection [20]. The elimination half-life (t1/2β) is between 80 and 110 min in healthy adults, predominantly via the hepatic route. After intravenous injection in mammalians, lidocaine accumulates in endocrine cells such as the pancreatic islets, the pituitary gland, the thyroid and the adrenal medulla [21].
Lidocaine has a high hepatic extraction ratio (approximately 70%), explaining a metabolic rate more dependent on liver blood flow than on liver metabolic capacity, and therefore an adequate liver blood flow is pivotal for its efficient metabolism. Approximately 90% of lidocaine is metabolized in the liver by oxidative deethylation (dealkylation) to monoethylglycinexylidide (MEGX), which is further de-ethylated to glycinexylidide (GX). The latter is hydrolyzed to xylidine and then oxidized to 4-hydroxy-xylidine, the main metabolic by-product found in urine. The cytochrome P450 system is involved in this transformation (mainly CYP3A4, and CYP1A2 to a lesser extent) [22]. Hence, inhibiting the CYP3A4 enzyme with erythromycin, for example, leads to a 20% reduction in lidocaine clearance, with a concomitant elevation of MEGX concentration [23]. MEGX concentration analysis post-lidocaine administration is, thus, a method used to evaluate liver function [24]. In healthy young adults, the MEGX concentration at the end of a steady-state long duration continuous infusion of lidocaine is between 15 and 35% of that of lidocaine [15, 18].
MEGX exhibits pharmacological properties comparable to those of lidocaine but with a less potency (about 80–90% of its antiarrhythmic and anticonvulsant potencies) [25]. The clearance rate of MEGX is slightly lower than that of lidocaine’s and its distribution volume is slightly higher, resulting in a longer total clearance (t1/2β ≈ 2.3–2.8 h) [25]. Lidocaine and its metabolites are finally excreted predominantly by the kidneys. GX has a lower clinical significance than the other metabolites and is rapidly eliminated in the urine. Less than 10% of lidocaine is excreted unchanged in the urine. The involvement of other organs in the metabolism of lidocaine cannot be completely ruled out. Some studies have suggested that the CYP3A4 enzyme in the lung could also be involved in lidocaine metabolism [26].
The concentration of protein-bound lidocaine in the plasma is inversely proportional to the drug concentration, being 40% at a drug concentration of 10 µg/ml, and 90% at a drug concentration of 3 µg/ml [1, 27]. For a given lidocaine concentration, the binding fraction is linearly dependent on the plasma levels of the postoperative acute phase reactant alpha-1-acid–glycoprotein (AAG) [1, 13, 15, 27]. In a virtual situation without AAG, binding is approximately 20%, mostly related to serum albumin. Because the unbound fraction of lidocaine represents the toxic form, prediction regarding the toxicity threshold becomes difficult [15]. Other factors can influence the toxicity threshold of lidocaine, for example, in a clinical setting; haemodilution increases the relative free unbound fraction due to a lower serum protein concentration, decreasing the toxicity threshold. Lidocaine is also bound to red blood cells to a certain extent, but anaemia by itself does not change the binding of lidocaine [28].
When used as an antiarrhythmic drug, lidocaine’s efficacy depends on maintenance of the therapeutic plasma concentration [13]. Therefore, the administration of a single loading dose of lidocaine can result in transient arrhythmia suppression, which dissipates rapidly as plasma concentrations fall below the therapeutic levels. Institution of a continuous intravenous infusion immediately after the bolus dose replaces the drug removed by hepatic metabolism, allowing for a steady plasma concentration. In the absence of a loading dose, achievement of a therapeutic steady-state plasma concentration takes more than 60 min [29].
The duration of infusion can decrease the clearance rate of lidocaine due to enzymatic saturation and competitive binding with other lidocaine’s active metabolites (MGEX), leading to a slower lidocaine clearance rate relative to time. The clearance rate seems to be mostly affected after 24 h of continuous infusion, a phenomenon confirmed by clinical trials [30]. Therefore, lidocaine infusions should be dosed per total body weight and decreased after 24 h to avoid overdosage and toxicity.
To maintain a steady-state plasma concentration, the following recommended dose is suggested: a loading intravenous bolus of 1.0–1.5 mg/kg of lidocaine followed by a continuous infusion of 50 μg/kg/min (3.0 mg/kg) for the first hour, 25 μg/kg/min (1.5 mg/kg) for the second hour, 12 μg/kg/min (0.7 mg/kg) for the next 22 h, and finally 10 μg/kg/min (0.6 mg/kg) from 24 to 48 h [13, 30]. Although continuous infusion might theoretically lead to toxicity over time, lidocaine blood concentrations reported in clinical studies remained below toxic levels (≈ 5 µg/ml), except for cardiac surgery trials in which higher doses were used for a longer duration (Table 1). Interestingly, concentrations of serum lidocaine remained quite similar or slightly lower than those reported during its prolonged epidural administration [42, 43].
2.2 Specific Populations
Lidocaine’s elimination half-life is prolonged in patients with cardiac failure, mainly due to a reduction in liver blood flow [18], an important point to be taken into consideration, especially in prolonged infusions.
No dose adjustment is necessary in patients with moderate liver cirrhosis; however, the dose is recommended to be halved in patients with severe cirrhosis (Child score C), again mainly due to decreased hepatic blood flow [23].
Lidocaine clearance is linearly altered with kidney impairment [44]. As expected, in severe renal insufficiency, a reduction in lidocaine clearance was observed, leading to a double elimination half-life in comparison with healthy subjects. MEGX levels were independent of renal function, and GX levels were more than twice those of controlled healthy subjects. No such alterations were observed in patients undergoing haemodialysis.
A significant increase in apparent distribution volume was observed in the elderly population. Elderly patients have a significantly longer elimination half-life compared to younger patients (2.7 vs. 1.6 h). However, despite a reduction in liver blood flow in the elderly population, no changes in plasma metabolic clearance were observed [45]. For the elderly population, the initial loading dose should be the same dose as for younger patients, but the continuous infusion rate is recommended to be decreased by approximately 35%.
In obese patients, clearance was markedly prolonged as compared to non-obese patients [46]. This was primarily due to an increase in the absolute volume of distribution, corresponding to a higher body weight. Lidocaine loading dose in the obese population should be calculated based on the total body weight, but the continuous infusion rate should be based on the ideal body weight.
Due to differences in body water distribution, blood volume, body composition and drug binding affinities, children absorb, distribute and eliminate medicinal products differently to adults. In this case, the AAG fraction is lower in neonates and infants, explaining a higher unbound fraction of lidocaine than in adolescents and adults [47]. However, lidocaine distributes in a relatively larger volume in neonates and infants than in adults, and as a result, an initial high serum drug concentration is not observed after a single injection [48]. Data on the pharmacokinetics of IVL in children are limited. Early studies suggested a quicker elimination rate than in adults [49]. However, in a study with 10 children (aged 0.5–3 years) and eight adults to determine lidocaine pharmacokinetics during anaesthesia with halothane, nitrous oxide and oxygen, no significant differences were reported between children and adults for all parameters analysed when standardized for body weight, suggesting that children older than 6 months of age distribute and eliminate IVL in the same manner as adults [50].
Finally, it should be noted that lidocaine crosses the placenta and the blood–brain barrier by simple passive diffusion. Lidocaine is also excreted in breast milk and the clearance rate should be taken into consideration for breast-feeding mothers to avoid toxicity in the breast-fed infant.
3 Properties
The main clinical properties of IVL are illustrated in Fig. 2. Lidocaine acts mainly as a blocker of voltage-gated open and inactivated sodium channels [51]. However, lidocaine has additional molecular properties. It can block inward potassium rectifier channels in cardiomyocytes and also interact with acetylcholine and 5-hydroxytryptamine (5HT-3) receptors [52]. The molecular effect depends on the concentration. Low‐dose lidocaine inhibits the glycinergic system, some potassium channels and the Gαq‐coupled protein receptors. Higher lidocaine concentrations block potassium and calcium channels, as well as the N-methyl-d-aspartate (NMDA) receptor [53].
3.1 Analgesic and Antihyperalgesic Properties
An analgesic effect is observed by systemic lidocaine affecting both the peripheral [54] and the central nervous system [55]. In healthy volunteers, pain intensity induced by interdigital pinch stimulations is significantly reduced by intravenous lidocaine [56]. However, this effect is of moderate magnitude. The most important effect was the control of pain after repeated stimulations, indicating a prevention of hypersensitization and major anti-hyperalgesic effect of IVL. Kawamata et al. showed that treatment with lidocaine prior to a surgical incision reduced the excessive inputs from the injured peripheral nerves, consequently suppressing flare formation and secondary hyperalgesia through a combination of peripheral and central mechanisms [57, 58]. It has also been shown that IVL inhibits the pain sensitization induced by remifentanil infusion [59]. In an elegant experimental model allowing differentiation between central and peripheral components, it was shown that most of the lidocaine effect was ascribed to central mechanisms [60]. The peripheral action, although of lesser magnitude than the central component, has been characterized by use of the lidocaine analogue QX-134, which does not cross the blood–brain barrier [61].
The mechanism of action of systemic lidocaine for the prevention of acute pain in the perioperative setting is still not fully understood and is unlikely to be solely based on the well-known sodium channel blockade effect [53, 62]. As mentioned above, lidocaine inhibits the glycinergic system, some potassium and calcium channels, Gαq‐coupled protein receptors and NMDA receptors. Serotonin receptors are also involved because the 5-HT3 antagonist ondansetron inhibits the sensory block induced by intrathecal lidocaine [63]. Additionally, IVL may even act directly through opiate receptor stimulation [64, 65]. Consistent with its local anaesthetic effect, parenteral lidocaine was demonstrated to be able to directly decrease excitability and conduction of unmyelinated C fibres after various painful stimulations [54, 66, 67]. In addition, IVL is able to suppress polysynaptic reflexes in the spinal dorsal horn [68]. Central anti-nociceptive effects produced by systemically administered lidocaine are mediated through an action on muscarinic and nicotinic receptors, which consequently increase the intraspinal release of acetylcholine, previously known to reinforce the inhibitory descending pain pathway [69]. Additionally, inhibition of the NMDA receptor appears to be a major trigger for antihyperalgesic effects [70,71,72]. A reduction of direct or synaptically driven NMDA and neurokinin receptor-mediated post-synaptic depolarizations have been well demonstrated [70,71,72]. Finally, lidocaine infusion may also have analgesic effects at the cerebral level. Indeed, IVL has the ability to depress the electrical potential elicited by sciatic nerve stimulation in the mid-brain reticular formation [73].
3.2 Anti-Inflammatory Effects
The anti-inflammatory properties of lidocaine have been well characterized [74, 75]. Lidocaine, as well as other amide local anaesthetics, inhibits leukocyte activation and adhesion to the site of injury in both in vitro and in vivo models. Lidocaine protects cells from inflammation by blocking the priming of neutrophils and therefore inhibiting the release of superoxide anions [76, 77] and interleukin-1B [78]. In animal studies, the injection of 1.5 mg/kg of lidocaine reduced granulocyte adhesion in the exudate of a sterile injured peritoneum by approximately 98%, compared to 40% in methylprednisolone-treated animals [79]. After cutaneous injection of live staphylococci, the skin showed moderate oedema with virtually no granulocyte infiltration in the lidocaine-treated animals, whereas a major oedema with pronounced granulocytes adhesion was observed in the control group [79]. In an animal model of endotoxemia, lidocaine pre-treatment significantly reduced leucocyte-endothelial cell adhesion and endothelial fluid leakage [80]. Neutrophil adhesion and endothelial hyperpermeability was also reduced by lidocaine, due to its inhibitory effect on the TNFα signalling pathway, thereby reducing Src cascade phosphorylation (a non-receptor tyrosine kinase protein that regulates angiogenic factors and vascular permeability) [81].
Besides lidocaine’s effect on adhesion, lidocaine also reduces activated leucocyte migration [77]. In human surgical wounds, lidocaine was demonstrated to significantly decrease the leucocyte count up to 72 h post-surgery, compared to the control group [82].
Lidocaine is involved in numerous anti-inflammatory mechanisms, including through white blood cells such as neutrophils and macrophages. The absence of voltage-gated sodium channels on neutrophils and macrophages suggests that IVL acts on these cells through a different mechanism to sodium channels. So far, a Gprot-q-coupled signalling pathway has been suggested as a mechanism of superoxide anion production by activated neutrophils [83, 84]. Furthermore, protection of the endothelial cells during endotoxemia is linked to a decrease in mitochondrial calcium overload through activation of mitochondrial potassium-ATP channels [85].
From a clinical point of view, the anti-inflammatory effect of lidocaine has been emphasized in several situations. Topical lidocaine is able to decrease the inflammatory extravasation of blue Evans coloration from a hydrochloric acid-induced peritonitis [86]. In a murine model of septic peritonitis, lidocaine (mean plasma level of 2.25 µM/l) prevents kidney and liver dysfunction and improves survival [87]. In this experiment, pro-inflammatory markers such as TNF-α remained at low levels in the IVL group, not different from those in control aseptic animals. In this study, the intracellular adhesion molecule (ICAM-1) and the monocyte chemoattractant protein (MCP-1) were also significantly reduced in the lidocaine group [87]. Finally, the anti-inflammatory properties of lidocaine were demonstrated in a mechanically ventilated murine model, where IVL increased the level of the anti-inflammatory cytokine IL-10, thereby potentially reducing the ventilatory-induced lung injury [88].
Although human studies documenting anti-inflammatory effects of lidocaine are scarce, several clinical studies showed that perioperative administration of lidocaine was significantly associated with attenuation of surgery-induced release of pro-inflammatory cytokines, e.g. IL-6 and IL-8, and/or decreased C-reactive protein levels [32, 89,90,91,92,93,94].
3.3 Effects on the Respiratory System
Lidocaine is a very weak respiratory depressant. In propofol-anaesthetized patients breathing spontaneously, the injection of a 1.5 mg/kg lidocaine bolus decreased the tidal volume and respiratory rate, and prolonged the expiratory duration [95]. The peak effect occurred 2.5–3 min after the injection of bolus lidocaine and was of moderate magnitude.
In in vitro studies on isolated tracheal smooth muscle cells, lidocaine at clinical concentrations exhibits a relaxant effect [96]. Furthermore, lidocaine reverses muscular contraction induced by acetylcholine, carbamylcholine or histamine, partly mediated by muscarinic M1 receptors antagonism [97]. Studies demonstrate that during anaphylaxis, lidocaine has a dual direct inhibitory effect on mast-cell release of pro-inflammatory mediators and subsequent bronchial muscle contractions [98]. IVL inhibits the bronchial hypersensitivity induced by mechanical irritation, thermal stimuli and irritants, such as particles, gases and blood. In conscious volunteers with bronchial hyper-reactivity, IVL attenuates the response to histamine inhalation to a similar extent to salbutamol aerosol [99]. In anaesthetized patients, a bolus of 1.5 mg/kg of lidocaine (corresponding to a plasma concentration above 2 µg/ml) abolishes the expiration reflex, cough reflex and spasmodic panting (but not the apnoeic reflex) elicited by water instillation in the trachea [100]. The same observation has been made in children under sevoflurane anaesthesia [101].
Finally, IVL 1–2 mg/kg is effective in laryngospasm prevention during general anaesthesia [101,102,103], and can markedly suppress fentanyl-induced cough during induction of general anaesthesia; this effect is also observed with a dose as low as 0.5 mg/kg [104].
3.4 Cardiovascular Effects
IVL was initially successfully used as an antiarrhythmic agent [1, 29]. Lidocaine has very moderate effects on cardiac function at doses used for analgesic purposes in clinical practice [105]. A slight negative chronotropic effect on the heart rate has been observed. However, under conditions of increased vagal activity, an anti-vagal effect capable of increasing the rate of the sinus rhythm was demonstrated using IVL. Effects on intracardiac conduction and myocardial inotropic depression are negligible and were only observed at supra-clinical concentrations.
Lidocaine has a biphasic action on smooth muscle of peripheral blood vessels, with vasoconstriction at low concentrations and vasodilation at higher concentrations [106]. When low concentrations of lidocaine are injected directly into the radial artery, it induces vasoconstriction [107]. At larger concentrations, lidocaine displays a dose-dependent vasodilatory effect, especially on precontracted vessels. In intact isolated rat aortic rings precontracted by norepinephrine, lidocaine produced a concentration-dependent relaxation [108]. Removal of the endothelium significantly increased the aortic ring responsiveness. The relaxing factor(s) responsible for enhancing the aortic ring relaxation did not seem to be nitric oxide- or prostacyclin-dependent, as NG-nitro-l-Arginine Methyl Ester (L-NAME) and indomethacin had little or no effect on intact ring relaxation. By contrast, lidocaine relaxation was completely abolished by voltage-dependent potassium channel inhibition (4-aminopyridine) and significantly reduced by the antagonism of vascular smooth muscle cells adenosine A2 receptors [108].
3.5 Effects on the Digestive Tract
IVL is well known to accelerate the resolution of post-operative ileus [109, 110]. The pathophysiology of post-operative ileus is complex and multifactorial. It is a combination of activation of inhibitory sympathetic reflexes, release of local and systemic inflammatory mediators as well as inhibitory gastrointestinal peptides. Factors such as opioid-induced inhibition of gastrointestinal motility and increased permeability of the intestinal mucosa may also contribute to postoperative ileus [111], which can be potentially ameliorated by IVL. Recent advances have identified handling and manoeuvring of intestines during surgery to be a major risk factor for intestinal inflammation. This local inflammatory process activates inhibitory neural pathways and hence compromises the contractile activity of the manipulated intestine [112], potentially increasing the risk of ileus. Macrophages residing in the muscularis externa and mast cells residing in the peritoneum are the key players in this inflammatory cascade.
The exact mechanism of action of IVL with regard to intestinal motility seems multifactorial and is not yet fully understood. IVL may indirectly be involved in restoring postoperative bowel function through the reduction of pain intensity and opiate consumption. However, other pharmacological mechanisms should be considered. Most of the understanding of these mechanisms comes from animal studies involving observations of lidocaine’s direct contractility effect on circular and longitudinal intestinal smooth muscles [113]. This effect does not seem to be mediated by the enteric nervous system [114]. Although the presence of voltage-gated sodium channels on human intestinal smooth muscle cells has been well documented, IVL seems to act through different pathways in non-human systems [114]. Although IVL’s direct role on postoperative ileus has not been well established, the indirect anti-inflammatory effect of lidocaine on epithelial intestinal cells, through the established inhibition of interleukin production, is plausible [115]. Accordingly, IVL reduces lipopolysaccharide permeability in ischaemic-injured horse jejunum and accelerates the recovery of the mucosal barrier [116]. Besides these direct effects, it has been assumed that IVL would be able to decrease the excitability and conduction in nerve fibres of the enteric nervous system, supporting the hypothesis that lidocaine depresses the activity of primary afferent neurons involved in reflex inhibition of gut motility [109]. In rats, lidocaine infusion inhibits the visceromotor reflex of neurons excited by ‘colorectal distension’ in a dose-dependent manner, emphasizing IVL’s potential ability to alleviate visceral pain in humans [117].
3.6 Effects on Non-Gastrointestinal Smooth Muscle Cells
Lidocaine and its active by-product MEGX depress smooth muscles of the uterus [118]. Lidocaine also has inhibitory effects on the smooth muscles of the human bladder through the combination of a direct effect and the suppression of neural-mediated contractions [119].
3.7 Antithrombotic Effects
Local anaesthetics in general significantly inhibit platelet aggregation. Among different local anaesthetics, lidocaine was the most effective platelet anti-aggregating compound, and had a longer contact time and concentration corresponding to a stronger effect [120, 121]. This effect seems clinically significant only for very high plasma concentrations, explaining some of the negative results [122]. As implicated by thromboelastographic studies (a method of testing the efficiency of blood coagulation), lidocaine produces a significant hypocoagulable change relative to the control [123]. Furthermore, the application of lidocaine-inhibited thrombus formation restored microcirculation after laser-induced microvascular injury [124].
In a 1977 study with a small sample size, a 6-day postoperative IVL infusion reduced the incidence of thromboembolism from 78 to 14% after hip arthroplasty [125]. This finding is consistent with the observation that a neuraxial block using local anaesthetics is able to reduce the incidence of venous thrombosis by almost 50% [126]. If the magnitude of a local anaesthetic’s antithrombotic effects remains unknown, it may have at least partly contributed to this observation.
3.8 Antimicrobial Properties
The antimicrobial effects of lidocaine have been demonstrated in in vitro settings [127]. Lidocaine has been shown to inhibit the growth of Gram-positive, Gram-negative mycobacterium and various fungi [128]. Consistently, the topical application of lidocaine in the respiratory tract during diagnostic pulmonary fibroscopy is able to modify the bacterial flora because of its powerful bactericidal effects on Haemophilus influenza and anaerobic microorganisms [129]. It is also noteworthy that the addition of lidocaine in a solution of propofol may prevent against syringe contamination by Echerichia coli [130]. Finally, lidocaine also has a direct antiviral effect against herpes simplex virus type 1 [131].
3.9 Antitumoral Properties
The direct and indirect antitumoral effects of lidocaine have been demonstrated in in vitro settings [132]. Lidocaine increased the expression of killer cell lectin-like receptor D (NKG2D) receptors and stimulated the function of natural killer (NK) cells against ovarian and pancreatic cancer cell lines. It also increased the cytolytic activity of NK cells from patients who underwent oncological surgery [133]. At clinically relevant concentrations, lidocaine has been shown to demethylate DNA in breast cancer cells lines, making them more sensitive to tumour suppressor genes and therefore inhibiting in vitro tumour growth [134]. Additional mechanisms involve the inhibition of phosphorylation of thyrosin kinase Src and ICAM-1, with clinically relevant concentrations (Src-dependent inflammatory signalling events), contributing to the inhibition of adhesion, migration and endothelial permeability, thereby preventing the development of metastasis at clinically relevant concentrations [81, 135]. This effect seems to be independent of voltage-gated sodium channel inhibition. In hepatocellular carcinoma, lidocaine was shown to increase Bax protein and activate caspase-3, which inhibit the growth of tumour cells by blocking replication and inducing eventual apoptosis in a time- and dose-dependent manner [136]. Furthermore, mRNA levels of key tumour cell regulators are profoundly decreased by lidocaine, leading to direct cytostatic effects and apoptosis in hepatocellular carcinoma cells [137]. The clinical relevance of such observations is currently difficult to appraise. However, the use of local anaesthetic agents is always referenced as being able to influence cancer evolution through anaesthetic management and could contribute to future cancer research [138]. In in vivo experiments, lidocaine was shown to suppress tumour development [136, 139]. At clinically relevant concentrations, intraperitoneal lidocaine improved survival of mice with peritoneal carcinomatosis. In addition, the antitumoral properties of lidocaine seem to be able to markedly potentiate the effects of cytotoxic agents such as cisplatin [136].
4 Clinical Applications
4.1 Preventing Propofol Injection Pain
Propofol is used for induction of anaesthesia in millions of patients every year. However, one of the disadvantages of propofol is distressing pain during injection [140]. Without preventive measures, the overall percentage of patients experiencing pain and percentage of patients experiencing high-intensity pain following propofol injection was found to be 63.7 and 37.9%, respectively, in adults [141], and 66.8 and 15.6%, respectively, in children [142]. Some patients recall the induction of anaesthesia as the most painful part of the perioperative period [140].
The underlying mechanisms of propofol-induced injection pain are still not fully understood [141]. Pain immediately after injection of propofol may be caused either by direct stimulation of nociceptors and free nerve endings in the venous wall or indirectly by the release of mediators, such as bradykinin and prostaglandin E2, which stimulate afferent nerve endings, leading to a delayed onset of pain [141]. Several studies in adults and children have explored various strategies to reduce the rate and severity of propofol-induced injection pain. A meta-analysis indicated that IVL alone, or IVL combined with other interventions, seems to be the most promising strategy to reduce propofol-induced injection pain [141,142,143,144]. In these studies, lidocaine was administered with propofol (lidocaine-propofol admixture) or as an intravenous pre-treatment (with or without venous occlusion), i.e. prior to the propofol injection. Venous drainage was occluded at mid-forearm, or just above the elbow, by a tourniquet or a blood pressure cuff (50–70 mmHg), often after elevation of the arm for 15–30 s for gravity drainage of venous blood. Venous occlusion was then maintained for 30–120 s (usually 60 s). Venous occlusion was then released and induction with propofol was started.
Both lidocaine admixture and pre-treatment were effective in reducing high-intensity pain on propofol injection. There was no significant difference between a -ow dose (≤ 20 mg or ≤ 0.2 mg/kg) and a high-dose (> 20 mg or > 0.2 mg/kg) lidocaine admixture. The low-dose lidocaine pre-treatment without venous occlusion seemed to be the least effective method [141].
As stated earlier, the mechanisms of action of lidocaine in preventing pain on propofol injection remain unclear [141]. A preceding injection of lidocaine prevents pain probably because of a direct effect on vessels. A recent study from Xing J et al. suggests that low-dose lidocaine acts preferentially by a peripheral local anaesthetic effect because the same dose administered in the contralateral arm did not alleviate propofol injection pain [145]. An exclusion of a central effect cannot be made; however, if it exists it would most likely be observed in doses above 1.5 mg/kg. The decrease in pain on injection observed by mixing a small amount of lidocaine to propofol might be due to the fact that lidocaine hydrochloride is a weak free-base cation solution, which would lower the pH of the admixture after mixing it with propofol.
4.2 Improving Post-Operative Recovery
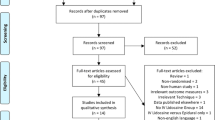
The overall impact of IVL on pain, opiate consumption, return of bowel function, length of hospital stay and safety profile was appraised in an initial review by a Cochrane group [146, 147]. Forty-five trials performed between 1966 and 2014, gathering data from various types of surgeries (12 open abdominal, 13 laparoscopic abdominal and 20 other non-abdominal surgeries) were analysed. Despite the quality of the evidence from the included studies being rated as low, results supported the benefit of IVL on pain during the first 24 h after surgery across studies, with the strongest effect observed with abdominal surgeries. Post-operative ileus occurred in 4.8% of the subjects in the treatment group and in 13.9% of subjects in the control group (risk ratio = 0.38; 95% CI 0.15–0.99; I2 = 0%). Furthermore, evidence of positive secondary outcomes such as a reduction in average length of hospital stay, postoperative nausea at early and > 24-h time points, as well as intraoperative and postoperative opioid requirements were shown with IVL use.
This particular review was recently updated by the same group [148], adding 23 trials, reaching a total of 68 trials (22 open abdominal surgery, 20 laparoscopic surgery and 26 other non-abdominal surgery), comprising 2254 subjects in the treatment group versus 2271 subjects in the control group. The conclusions were modified according to these new incorporations. The quality of evidence to conclude on the benefit of IVL was limited due to inconsistency, imprecision, study quality and a high uncertainty on the favourable effects of lidocaine with regard to the reported outcomes. Evidence of very low quality suggests IVL may lead to a reduction of pain intensity during the first 4 h after surgery. A clinically relevant reduction in pain with lidocaine at intermediate (24 h) and at late time points (48 h) was ruled out via moderate-quality evidence. Similarly, intraoperative and postoperative opiate consumption was reduced in a statistically significant manner, but by small amounts in a clinical sense. The incidence of postoperative ileus was reduced (RR = 0.37, 95% CI 0.15–0.87), as did the time to first defaecation/bowel movement. Incidence of nausea (but not vomiting) was also reduced (RR = 0.72, 95% CI 0.53–0.98). A subgroup difference for different types of surgeries could no longer be confirmed in this meta-analysis due to the nature of the newly included studies [148].
In spite of these results, which have to be analysed after taking into consideration the very low quality of evidence for the benefit of IVL, it may still be worthwhile in shedding light more precisely on different kinds of surgical procedures. A recent review has underlined the perioperative benefit of IVL for improving postoperative recovery given the type of surgery [6].
4.2.1 Abdominal Surgery
The significant clinical benefits of perioperative IVL in reducing pain intensity, nausea, duration of ileus, postoperative opioid requirements and average length of hospital stay after abdominal surgery have been demonstrated in many randomized controlled trials and reported in all meta-analyses focusing on abdominal surgery released over the last decade [6, 149,150,151,152,153,154].
In the meta-analysis by Marret et al. based on eight randomized controlled trials including abdominal surgery, postoperative pain intensity 24 h after surgery, rated on a VAS, was reduced by 5.9 mm (95% CI 2.2–9.6, p < 0.01), duration of ileus was reduced by 8.3 h [95% CI 3–13, p < 0.01), incidence of PONV was reduced (ODDS = 0.39, 95% CI 0.2–0.76) and length of hospital stay was reduced by 0.84 day (95% CI 0.3–1.38, p < 0.01) in subjects who had received IVL [149].
Another meta-analysis including 14 randomized controlled trials that consisted of data from 742 patients compared IVL versus placebo/routine treatment for postoperative analgesia following laparoscopic surgery [153]. IVL was associated with a clinically small but significant reduction in opiate requirement at 24 h compared with placebo/routine care (WMD − 7.62 mg; CI − 12.37, − 2.86; p = 0.002). IVL was associated with reduced cumulative opiate requirements (WMD 5.93 mg; CI − 11.07, − 0.79; p = 0.02), reduced pain scores at rest, at 2, 12 and 24 h (but not at 48 h), reduced nausea and vomiting, and a shorter time until resumption of feeding. The length of stay did not differ between groups. There was a low incidence of IV lidocaine-associated toxicity.
In obese patients undergoing laparoscopic bariatric surgery, IVL was associated with a reduction in postoperative opiate consumption and an improved quality of recovery 24 h after the surgery [155]. It is also noteworthy that IVL could have beneficial effects in the ambulatory setting for short-duration procedures [156,157,158]. Relative to a control group, 1.5 mg/kg bolus followed by 2 mg/kg/h of IVL given to patients undergoing gynaecological outpatient laparoscopic procedures led to a quicker hospital discharge and a better recovery score at 24 h post surgery. This was probably related to a reduction in total post-surgical opiate requirements [157]. Two recent meta-analysis of randomized controlled trials (RCTs) on laparoscopic cholecystectomy showed that IVL was associated with a reduction in pain intensity (at 12, 24 and 48 h postoperatively), opiate consumption and opiate-related side-effects (PONV, ileus and pruritus) compared to a placebo group [158, 159]. In this indication, intraoperative IVL seems more efficacious than intraperitoneal instillation [160].
The benefit of IVL in non-bowel abdominal surgery is more controversial [6]. However, it should be noted that this is not a recommendation against the use of lidocaine in certain types of surgeries, but rather an indication of a lack of literature and reliable evidence.
A significant beneficial effect on pain intensity, post-surgical opiate requirement and average length of hospital stay has been demonstrated after intra-abdominal prostatectomy, justifying its use in this indication [161,162,163,164]. Results after nephrectomy are in general less positive [165]. However, a recent study has reported an improvement in pain intensity and functional capacity, a reduction in post-surgical opiate consumption and average length of stay after 1.5 mg/kg of IVL administration at the induction of anaesthesia followed by infusion of 1 mg/kg/h intraoperatively and for 24 h postoperatively on patients who underwent open nephrectomy [166]. Similarly, several results on abdominal hysterectomy have failed to show a benefit [35, 167], although more recent studies show moderate benefits [168], and additional positive effects when IVL was associated with dexmedetomidine [169].
4.2.2 Non-Abdominal Surgery
One meta-analysis of four RCTs including 167 subjects undergoing breast surgery [170] showed that IVL infusion did not provide benefits in terms of acute post-operative pain from 2 h to 3 days. However, in the first 72 h, the treatment group reported fewer analgesic consumption compared with the placebo/no treatment group. Moreover, patients in the treatment group had a significantly lower risk of developing chronic pain 3–6 months after surgery (RR = 0.332; 95% CI 0.141–0.781, p = 0.012). These conclusions were further reinforced by the results of another recent randomized trial [171]. However, the impact of IVL on chronic postoperative pain remains to be further investigated before a definite conclusion is drawn.
Regarding spine surgery, an RCT had previously shown a reduction in pain intensity and postoperative fentanyl consumption [172], and perhaps an improvement in quality of recovery [173]; however, a recent RCT concluded on the absence of benefit of IVL for spine surgery, even on residual postoperative pain [174]. Furthermore, the use of IVL during hip arthroplasty does not seem to provide significant clinical benefits either [175].
Patients undergoing thyroid surgery may benefit from IVL administration (better pain relief and reduction in postoperative opiate consumption, as well as lower C-reactive protein). However, it should be noted that the benefit was limited to the first 4 h after the surgery [93, 176]. It has also been suggested that IVL can reduce chronic post-surgical incisional pain [176].
Despite the reduction in the incidence of PONV in the IVL group [177], IVL seems to have no effect in pain management after tonsillectomy [178].
There is not enough evidence to support the benefits of using IVL during cardiac surgery [41, 43, 179], although a protective effect against postoperative cognitive dysfunction has been suggested [43], but not found in another more recent study [179]. Conversely, IVL was shown to provide significant benefits on pain intensity and postoperative opiate consumption after thoracic surgery [180].
After neurosurgery (supratentorial tumour resection), IVL provides a slight improvement in pain intensity with limited duration [181, 182]. Neurosurgical patients given IVL (1.5 mg/kg) were able to control the increase in blood pressure and the intracranial pressure in a similar magnitude to a bolus injection of 1.5 mg/kg of esmolol [183].
Finally, IVL is safe and effective in attenuating the maternal stress response to surgery for caesarean delivery [35].
4.2.3 Recommended IVL Dosing to Improve Post-Operative Recovery
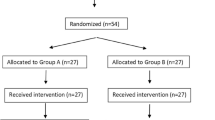
There are many unresolved questions regarding optimal modalities of IVL administration. According to the published literature [148], systemic lidocaine administration was generally initiated up to 30 min before induction, at induction or after induction of anaesthesia, at the latest 30 min before skin incision. In 69% of studies, IVL administration was initiated with a bolus dose of 1–3 mg/kg of body weight, 1.5 mg/kg being the most common dose. Lidocaine infusion dose varied between studies from 1 mg/kg/h to 5 mg/kg/h. Continuous lidocaine infusion was terminated either at the end of the surgical procedure or with skin closure, 30 min after arrival at the post-anaesthesia care unit (PACU), 1 h after the end of surgery/skin closure, 1–2 h after arrival in the PACU, or at discharge from the PACU. In some studies, IVL infusion was continued up to 4 or 8 h postoperatively, after a total of 12 h, after a total of 24 h, 24 h postoperatively, 48 h postoperatively or on the day of return of bowel function, or on the fifth postoperative day at the latest. One meta-analysis of seven RCTs including 362 subjects [154] aimed to estimate an appropriate end-time for intraoperative IVL infusion in bowel surgery. The meta-analysis showed that there was no additional benefit of extending IVL infusion beyond 1 h after surgery. During laparoscopic colon surgery, it should be noted that the analgesic effect of IVL was not observed if the administration was limited to the postoperative period [184].
4.3 Other Clinical Benefits
IVL has several other intraoperative pharmacodynamics effects. Among the most remarkable effects, lidocaine is effective in blunting cerebral haemodynamic responses to airway manipulation [185]. As mentioned above, IVL can control the tracheobronchial reflex induced by local stimulation [100]. Furthermore, administration of IVL at 1.5–2 mg/kg, 2–3 min before laryngoscopy, may blunt a rise in heart rate, systolic blood pressure, mean arterial pressure and catecholamine levels associated with intubation and extubation [186]. During the anaesthetic period, IVL also reduces hypnotic medication requirements by up to one-third in adult patients, to a similar extent to sevoflurane [163, 187] rather than to propofol [188]. Intraoperative opiate requirements are also significantly reduced by up to 50% in a report by Lauwick et al. [180, 189]. Consistently, IVL decreases the bispectral index (increase the depth of anaesthesia) in a dose-dependent manner [190].
5 Safety
Local anaesthetics, through their actions on sodium and potassium channels, have the potential to induce systemic toxicity (corresponding to the so-called LAST: Local Anesthetic Systemic toxicity) [191]. LAST is mainly the consequence of the blockade of impulse propagation on the central nervous system and myocardial conduction tissue. Early symptoms are dysgeusia (metal taste), perioral numbness, tongue paraesthesia, dizziness, tinnitus and blurred vision. Severe intoxication is followed by excitatory signs (agitation) that may progress to seizures, cardiac arrest (atrioventricular heart block and arrhythmias) and even death. Even if lidocaine is commonly considered to have a greater margin of safety than other local anaesthetics, direct intravenous administration raises the question about its tolerance. As outlined above, the average dose associated with the occurrence of neurological symptoms in healthy volunteers is about 8 mg/kg [14, 15], corresponding to a plasma value of about 15 µg/ml [16]. First signs of cardiotoxicity were observed at plasma concentrations above 21 µg/ml [1]. These toxic thresholds are far above the plasma concentration commonly observed after usual administration in the perioperative period (see Table 1). However, other conditions should be taken into account for LAST prevention, such as the concomitant administration of other local anaesthetics for locoregional analgesia (toxicity is additive), co-morbidities and extremes of age [191]. Treatment of LAST is currently clearly codified, combining symptomatic measures (oxygen, benzodiazepines) and lipid emulsion injection [191].
The effect of IV lidocaine on adverse effects compared to placebo is uncertain, as only a small number of studies systematically analysed the occurrence of adverse effects (very low-quality evidence). However, analysis of the available data, using commonly recommended protocols of administration, reveals that there was no evidence that IVL was associated with an increased risk of adverse effects. Some neuropsychological disturbances have been reported, including light-headedness, dizziness, visual disturbances, drowsiness and sedation, but with the same or even higher frequencies in the control population [148]. Accordingly, one study reported a detailed summary table with numerous monitored adverse events, but no significant differences were reported in their occurrence between the treatment and control groups [192]. In conclusion, with respect to common protocols of administration, no major adverse events due to systemic lidocaine administration in the perioperative period could be detected.
Post-marketing safety monitoring revealed several interactions of lidocaine with other antiarrhythmic drugs. Due to the increased risk of cardiac adverse effects, combination with antiarrhythmic drugs of the same class is not recommended and should be considered only in exceptional cases. Furthermore, combination with antiarrhythmic drugs of other classes (e.g. amiodarone, disopyramide, quinidine, sotalol) is contraindicated. Amiodarone is known to reduce hepatic metabolism of lidocaine leading to increased lidocaine plasma concentrations, which may result in adverse neurological and cardiac effects. The same is applicable for combined use of lidocaine with fluvoxamine or cimetidine at cimetidine dosages ≥ 800 mg/day. In all of these cases, patients have to be closely monitored and lidocaine dosage should be adapted as required. The combined use of lidocaine with beta-blockers in heart failure may have a negative inotropic effect with risk of cardiac decompensation. Furthermore, the combination with drugs with inotropic negative bradycardic properties and/or slowing atrioventricular conduction is difficult and requires clinical monitoring and ECG monitoring.
Lidocaine does not have local venous toxicity. A study observed thrombophlebitis in four of 85 subjects who were treated with 10 mg of lidocaine, compared to eight of 85 subjects in the control group [193]. An in vitro study by Masaki et al. reported coalescence of oil droplets (diameter ≥ 5 µm) 30 min after the addition of 40 mg lidocaine to propofol (time- and dose-dependent reaction), which was theorized to potentially cause pulmonary embolism [194]. Despite the coalescence formation, no adverse events (including pulmonary embolism) were reported in vivo.
Finally, lidocaine could be associated with allergic reactions. Immunologically mediated Type 1 hypersensitivity reactions with a positive skin prick test have been described in the past, but are extremely rare [195]. Other ingredients in local anaesthetic preparations must be considered as elicitors, e.g. preservatives such as benzoates or sulphites, or latex contaminants in injection bottles. During a 2-year study period conducted in France, true lidocaine anaphylaxis was encountered in only one case [196]. It should be noted that skin cross-reactivity between different amide type local anaesthetics was not observed in every case [197]. A positive history of anaphylaxis should be followed up with extensive testing for the amide family of drugs.
6 Conclusion
Since its introduction in clinical practice, IVL has been the subject of many assessments. Meta-analysis focusing on abdominal surgery demonstrated beneficial effects on pain management, opiate consumption, postoperative ileus, incidence of PONV and hospital length of stay. Results are more controversial for non-abdominal surgeries. Another recent meta-analysis combining data from studies with different kinds of surgeries showed a general uncertainty with IVL use, but also showed IVL to have a beneficial impact on pain scores in the early postoperative phase, and on gastrointestinal recovery, postoperative nausea and opioid consumption. The quality of evidence in this meta-analysis was limited due to inconsistency, imprecision and quality of the included studies. Besides its well-known analgesic and anti-inflammatory properties, IVL may have additional beneficial effects on bronchial reactivity, incidence of venous thrombosis and recovery from post-surgical ileus. Considering the safety profile of IVL at the common dose, the benefits may outweigh the risks compared to other analgesic strategies. In-depth knowledge of its pharmacokinetic and pharmacodynamics properties may help physicians to better understand the effects of IVL and to use it in the most appropriate manner.
References
Weinberg L, Peake B, Tan C, Nikfarjam M. Pharmacokinetics and pharmacodynamics of lignocaine: a review. World J Anesthesiol. 2015;4:17–29.
Gilbert CR, Hanson IR, Brown AB, Hingson RA. Intravenous use of xylocaine. Curr Res Anesth Analg. 1951;30:301–13.
De Clive-Lowe SG, Desmond J, North J. Intravenous lignocaine anaesthesia. Anaesthesia. 1958;13(2):138–46.
Philipps OC, Lyons WB, Harris LC, Nelson AT, Graff TD, Frazier TM. Intravenous lidocaine as an adjunct to general anesthesia: a clinical evaluation. Anesth Analg. 1960;39:317–22.
Helander EM, Webb MP, Bias M, Whang EE, Kaye AD, Urman RD. A comparison of multimodal analgesic approaches in institutional enhanced recovery after surgery protocols for colorectal surgery: pharmacological agents. J Laparoendosc Adv Surg Tech A. 2017;27:903–8.
Dunn LK, Durieux ME. Perioperative use of intravenous lidocaine. Anesthesiology. 2017;126:729–37.
Apfelbaum JL, Gan TJ, Zhao S, Hanna DB, Chen C. Reliability and validity of the perioperative opioid-related symptom distress scale. Anesth Analg. 2004;99:699–709.
Oderda GM, Said Q, Evans RS, Stoddard GJ, Lloyd J, Jackson K, Rublee D, Samore MH. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41:400–6.
Bakan M, Umutoglu T, Topuz U, Uysal H, Bayram M, Kadioglu H, Salihoglu Z. Opioid-free total intravenous anesthesia with propofol, dexmedetomidine and lidocaine infusions for laparoscopic cholecystectomy: a prospective, randomized, double-blinded study. Braz J Anesthesiol. 2015;65:191–9.
Kim DJ, Bengali R, Anderson TA. Opioid-free anesthesia using continuous dexmedetomidine and lidocaine infusions in spine surgery. Korean J Anesthesiol. 2017;70:652–3.
Mure-Zamparini M, Fiant AL, Filipov T, Flais F, Fobe F, Hanouz JL. Intravenous lidocaine: an increasing but unauthorized prescription. Ann Fr Anesth Reanim. 2014;33:550–1.
Grassi P, Bregant GM, Crisman M. Systemic intravenous lidocaine for perioperative pain management: a call for changing indications in the package sheet. Heart Lung Vessel. 2014;6:137–8.
Sampson KJ, Kass RS. Anti-arrhythmic drugs. Lidocaine. In: Brunton L, Chabner B, Knollman B (eds) Goodman and Gilman. The pharmacological basis of therapeutics, 12th edn. McGraw-Hill, New York, pp 841–842.
Usubiaga JE, Wikinski J, Ferrero R, Usubiaga LE, Wikinski R. Local anesthetic-induced convulsions in man—an electroencephalographic study. Anesth Analg. 1966;45:611–20.
Drayer DE, Lorenzo B, Werns S, Reidenberg MM. Plasma levels, protein binding, and elimination data of lidocaine and active metabolites in cardiac patients of various ages. Clin Pharmacol Ther. 1983;34:14–22.
DeToledo JC. Lidocaine and seizures. Ther Drug Monit. 2000;22:320–2.
Boyes RN, Scott DB, Jebson PJ, Godman MJ, Julian DG. Pharmacokinetics of lidocaine in man. Clin Pharmacol Ther. 1971;12:105–16.
Nation RL, Triggs EJ, Selig M. Lignocaine kinetics in cardiac patients and aged subjects. Br J Clin Pharmacol. 1977;4:439–48.
Oertel R, Arenz N, Zeitz SG, Pietsch J. Investigations into distribution of lidocaine in human autopsy material. Biomed Chromatogr. 2015;29:1290–6.
Katz J, Gershwin ME, Hood NL. The distribution of 14C-labelled lidocaine in the rat using whole-body autoradiography. Arch Int Pharmacodyn Ther. 1968;175:339–46.
Hammarström L, Slanina P, Tjälve H, Ullberg S. Distribution of local anesthetics: accumulation in some endocrine polypeptide-hormone producing cell systems. Br J Pharmacol. 1974;52:367–74.
Bargetzi MJ, Aoyama T, Gonzalez FJ, Meyer UA. Lidocaine metabolism in human liver microsomes by cytochrome P450IIIA4. Clin Pharmacol Ther. 1989;46:521–7.
Orlando R, Piccoli P, De Martin S, Padrini R, Palatini P. Effect of the CYP3A4 inhibitor erythromycin on the pharmacokinetics of lignocaine and its pharmacologically active metabolites in subjects with normal and impaired liver function. Br J Clin Pharmacol. 2003;55:86–93.
Oellerich M, Burdelski M, Ringe B, Lamesch P, Gubernatis G, Bunzendahl H, Pichlmayr R, Herrmann H. Lignocaine metabolite formation as a measure of pre-transplant liver function. Lancet. 1989;1(8639):640–2.
Thomson AH, Elliott HL, Kelman AW, Meredith PA, Whiting B. The pharmacokinetics and pharmacodynamics of lignocaine and MEGX in healthy subjects. J Pharmacokinet Biopharm. 1987;15:101–15.
Aoki M, Okudaira K, Haga M, Nishigaki R, Hayashi M. Contribution of rat pulmonary metabolism to the elimination of lidocaine, midazolam, and nifedipine. Drug Metab Dispos. 2010;38:1183–8.
Routledge PA, Barchowsky A, Bjornsson TD, Kitchell BB, Shand DG. Lidocaine plasma protein binding. Clin Pharmacol Ther. 1980;27:347–51.
Lönnqvist PA, Herngren L. Effects of pronounced haemodilution on the plasma protein binding of lidocaine. Perfusion. 1995;10:17–20.
Gianelly R, von der Groeben JO, Spivack AP, Harrison DC. Effect of lidocaine on ventricular arrhythmias in patients with coronary heart disease. N Engl J Med. 1967;277:1215–9.
Hsu YW, Somma J, Newman MF, Mathew JP. Population pharmacokinetics of lidocaine administered during and after cardiac surgery. J Cardiothorac Vasc Anesth. 2011;25:931–6.
Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, Hering W. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004;98(4):1050–5.
Herroeder S, Pecher S, Schönherr ME, Kaulitz G, Hahnenkamp K, Friess H, Böttiger BW, Bauer H, Dijkgraaf MG, Durieux ME, Hollmann MW. Systemic lidocaine shortens length of hospital stay after colorectal surgery: a double-blinded, randomized, placebo-controlled trial. Ann Surg. 2007;246:192–200.
Bryson GL, Charapov I, Krolczyk G, Taljaard M, Reid D. Intravenous lidocaine does not reduce length of hospital stay following abdominal hysterectomy. Can J Anaesth. 2010;57:759–66.
Oliveira CM, Sakata RK, Slullitel A, Salomão R, Lanchote VL, Issy AM. Effect of intraoperative intravenous lidocaine on pain and plasma interleukin-6 in patients undergoing hysterectomy. Rev Bras Anestesiol. 2015;65:92–8.
El-Tahan MR, Warda OM, Diab DG, Ramzy EA, Matter MK. A randomized study of the effects of perioperative i.v. lidocaine on hemodynamic and hormonal responses for cesarean section. J Anesth. 2009;23(2):215–21.
Cassuto J, Wallin G, Högström S, Faxén A, Rimbäck G. Inhibition of postoperative pain by continuous low-dose intravenous infusion of lidocaine. Anesth Analg. 1985;64:971–4.
Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012;28:567–72.
Kasten GW, Owens E. Evaluation of lidocaine as an adjunct to fentanyl anesthesia for coronary artery bypass graft surgery. Anesth Analg. 1986;65:511–5.
Insler SR, O’Connor M, Samonte AF, Bazaral MG. Lidocaine and the inhibition of postoperative pain in coronary artery bypass patients. J Cardiothorac Vasc Anesth. 1995;9:541–6.
Mitchell SJ, Pellett O, Gorman DF. Cerebral protection by lidocaine during cardiac operations. Ann Thorac Surg. 1999;67:1117–24.
Wang D, Wu X, Li J, Xiao F, Liu X, Meng M. The effect of lidocaine on early postoperative cognitive dysfunction after coronary artery bypass surgery. Anesth Analg. 2002;95:1134–41.
Inoue R, Suganuma T, Echizen H, Ishizaki T, Kushida K, Tomono Y. Plasma concentrations of lidocaine and its principal metabolites during intermittent epidural anesthesia. Anesthesiology. 1985;63:304–10.
Shono A, Sakura S, Saito Y, Doi K, Nakatani T. Comparison of 1% and 2% lidocaine epidural anaesthesia combined with sevoflurane general anaesthesia utilizing a constant bispectral index. Br J Anaesth. 2003;91:825–9.
De Martin S, Orlando R, Bertoli M, Pegoraro P, Palatini P. Differential effect of chronic renal failure on the pharmacokinetics of lidocaine in patients receiving and not receiving hemodialysis. Clin Pharmacol Ther. 2006;80:597–606.
Abernethy DR, Greenblatt DJ. Impairment of lidocaine clearance in elderly male subjects. J Cardiovasc Pharmacol. 1983;5:1093–6.
Abernethy DR, Greenblatt DJ. Lidocaine disposition in obesity. Am J Cardiol. 1984;53:1183–6.
Lerman J, Strong HA, LeDez KM, Swartz J, Rieder MJ, Burrows FA. Effects of age on the serum concentration of alpha 1-acid glycoprotein and the binding of lidocaine in pediatric patients. Clin Pharmacol Ther. 1989;46:219–25.
Burrows FA, Lerman J, LeDez KM, Strong HA. Pharmacokinetics of lidocaine in children with congenital heart disease. Can J Anaesth. 1991;38:196–200.
Tucker GT. Pharmacokinetics of local anaesthetics. Br J Anaesth. 1986;58:717–31.
Finholt DA, Stirt JA, DiFazio CA, Moscicki JC. Lidocaine pharmacokinetics in children during general anesthesia. Anesth Analg. 1986;65:279–82.
Butterworth JF 4th, Strichartz GR. Molecular mechanisms of local anesthesia: a review. Anesthesiology. 1990;72:711–34.
Arias HR. Role of local anesthetics on both cholinergic and serotonergic ionotropic receptors. Neurosci Biobehav Rev. 1999;23:817–43.
van der Wal SE, van den Heuvel SA, Radema SA, van Berkum BF, Vaneker M, Steegers MA, Scheffer GJ, Vissers KC. The in vitro mechanisms and in vivo efficacy of intravenous lidocaine on the neuroinflammatory response in acute and chronic pain. Eur J Pain. 2016;20:655–74.
Devor M, Wall PD, Catalan N. Systemic lidocaine silences ectopic neuroma and DRG discharge without blocking nerve conduction. Pain. 1992;48:261–8.
Jaffe RA, Rowe MA. Subanesthetic concentrations of lidocaine selectively inhibit a nociceptive response in the isolated rat spinal cord. Pain. 1995;60:167–74.
Koppert W, Zeck S, Sittl R, Likar R, Knoll R, Schmelz M. Low-dose lidocaine suppresses experimentally induced hyperalgesia in humans. Anesthesiology. 1998;89:1345–53.
Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E, Watanabe H, Namiki A. Experimental incision-induced pain in human skin: effects of systemic lidocaine on flare formation and hyperalgesia. Pain. 2002;100:77–89.
Kawamata M, Watanabe H, Nishikawa K, Takahashi T, Kozuka Y, Kawamata T, Omote K, Namiki A. Different mechanisms of development and maintenance of experimental incision-induced hyperalgesia in human skin. Anesthesiology. 2002;97:550–9.
Cui W, Li Y, Li S, Yang W, Jiang J, Han S, Li J. Systemic lidocaine inhibits remifentanil-induced hyperalgesia via the inhibition of cPKCgamma membrane translocation in spinal dorsal horn of rats. J Neurosurg Anesthesiol. 2009;21:318–25.
Koppert W, Ostermeier N, Sittl R, Weidner C, Schmelz M. Low-dose lidocaine reduces secondary hyperalgesia by a central mode of action. Pain. 2000;85:217–24.
Kawamata M, Sugino S, Narimatsu E, Yamauchi M, Kiya T, Furuse S, Namiki A. Effects of systemic administration of lidocaine and QX-314 on hyperexcitability of spinal dorsal horn neurons after incision in the rat. Pain. 2006;122:68–80.
Lauretti GR. Mechanisms of analgesia of intravenous lidocaine. Rev Bras Anestesiol. 2008;58:280–6.
Fassoulaki A, Melemeni A, Zotou M, Sarantopoulos C. Systemic ondansetron antagonizes the sensory block produced by intrathecal lidocaine. Anesth Analg. 2005;100:1817–21.
Hirota K, Okawa H, Appadu BL, Grandy DK, Lambert DG. Interaction of local anaesthetics with recombinant mu, kappa, and delta-opioid receptors expressed in Chinese hamster ovary cells. Br J Anaesth. 2000;85(5):740–6.
Cohen SP, Mao J. Is the analgesic effect of systemic lidocaine mediated through opioid receptors? Acta Anaesthesiol Scand. 2003;47:910–1.
Wagers PW, Smith CM. Responses in dental nerves of dogs to tooth stimulation and the effects of systemically administered procaine, lidocaine and morphine. J Pharmacol Exp Ther. 1960;130:89–105.
De Jong RH, Nace RA. Nerve impulse conduction during intravenous lidocaine injection. Anesthesiology. 1968;29:22–8.
Woolf CJ, Wiesenfeld-Hallin Z. The systemic administration of local anaesthetics produces a selective depression of C-afferent fibre evoked activity in the spinal cord. Pain. 1985;23:361–74.
Abelson KS, Höglund AU. Intravenously administered lidocaine in therapeutic doses increases the intraspinal release of acetylcholine in rats. Neurosci Lett. 2002;317:93–6.
Nagy I, Woolf CJ. Lignocaine selectively reduces C fibre-evoked neuronal activity in rat spinal cord in vitro by decreasing N-methyl-d-aspartate and neurokinin receptor-mediated post-synaptic depolarizations; implications for the development of novel centrally acting analgesics. Pain. 1996;64:59–70.
Muth-Selbach U, Hermanns H, Stegmann JU, Kollosche K, Freynhagen R, Bauer I, Lipfert P. Antinociceptive effects of systemic lidocaine: involvement of the spinal glycinergic system. Eur J Pharmacol. 2009;613:68–73.
Sugimoto M, Uchida I, Mashimo T. Local anaesthetics have different mechanisms and sites of action at the recombinant N-methyl-d-aspartate (NMDA) receptors. Br J Pharmacol. 2003;138:876–82.
Wagman IH, De Jong RH, Prince DA. Effects of lidocaine on the central nervous system. Anesthesiology. 1967;28:155–72.
Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology. 2000;93:858–75.
Caracas HC, Maciel JV, Martins PM, de Souza MM, Maia LC. The use of lidocaine as an anti-inflammatory substance: a systematic review. J Dent. 2009;37:93–7.
Peck SL, Johnston RB Jr, Horwitz LD. Reduced neutrophil superoxide anion release after prolonged infusions of lidocaine. J Pharmacol Exp Ther. 1985;235(2):418–22.
Fischer LG, Bremer M, Coleman EJ, Conrad B, Krumm B, Gross A, Hollmann MW, Mandell G, Durieux ME. Local anesthetics attenuate lysophosphatidic acid-induced priming in human neutrophils. Anesth Analg. 2001;92:1041–7.
Sinclair R, Eriksson AS, Gretzer C, Cassuto J, Thomsen P. Inhibitory effects of amide local anaesthetics on stimulus-induced human leukocyte metabolic activation, LTB4 release and IL-1 secretion in vitro. Acta Anaesthesiol Scand. 1993;37:159–65.
MacGregor RR, Thorner RE, Wright DM. Lidocaine inhibits granulocyte adherence and prevents granulocyte delivery to inflammatory sites. Blood. 1980;56:203–9.
Schmidt W, Schmidt H, Bauer H, Gebhard MM, Martin E. Influence of lidocaine on endotoxin-induced leukocyte-endothelial cell adhesion and macromolecular leakage in vivo. Anesthesiology. 1997;87:617–24.
Piegeler T, Votta-Velis EG, Bakhshi FR, Mao M, Carnegie G, Bonini MG, Schwartz DE, Borgeat A, Beck-Schimmer B, Minshall RD. Endothelial barrier protection by local anesthetics: ropivacaine and lidocaine block tumor necrosis factor-α-induced endothelial cell Src activation. Anesthesiology. 2014;120:1414–28.
Eriksson AS, Sinclair R, Cassuto J, Thomsen P. Influence of lidocaine on leukocyte function in the surgical wound. Anesthesiology. 1992;77:74–8.
Hollmann MW, Gross A, Jelacin N, Durieux ME. Local anesthetic effects on priming and activation of human neutrophils. Anesthesiology. 2001;95:113–22.
Hollmann MW, Herroeder S, Kurz KS, Hoenemann CW, Struemper D, Hahnenkamp K, Durieux ME. Time-dependent inhibition of G protein-coupled receptor signaling by local anesthetics. Anesthesiology. 2004;100:852–60.
de Klaver MJ, Weingart GS, Obrig TG, Rich GF. Local anesthetic-induced protection against lipopoly saccharide-induced injury in endothelial cells: The role of mitochondrial adenosine triphosphate-sensitive potassium channels. Anesth Analg. 2006;102:1108–13.
Rimbäck G, Cassuto J, Wallin G, Westlander G. Inhibition of peritonitis by amide local anesthetics. Anesthesiology. 1988;69:881–6.
Gallos G, Jones DR, Nasr SH, Emala CW, Lee HT. Local anesthetics reduce mortality and protect against renal and hepatic dysfunction in murine septic peritonitis. Anesthesiology. 2004;101:902–11.
Van Der Wal S, Vaneker M, Steegers M, Van Berkum B, Kox M, Van Der Laak J, Van Der Hoeven J, Vissers K, Scheffer GJ. Lidocaine increases the anti-inflammatory cytokine IL-10 following mechanical ventilation in healthy mice. Acta Anaesthesiol Scand. 2015;59:47–55.
Kuo CP, Jao SW, Chen KM, Wong CS, Yeh CC, Sheen MJ, Wu CT. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006;97:640–6.
Yardeni IZ, Beilin B, Mayburd E, Levinson Y, Bessler H. The effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesth Analg. 2009;109:1464–9.
Yon JH, Choi GJ, Kang H, Park JM, Yang HS. Intraoperative systemic lidocaine for pre-emptive analgesics in subtotal gastrectomy: a prospective, randomized, double-blind, placebo-controlled study. Can J Surg. 2014;57:175–82.
Sridhar P, Sistla SC, Ali SM, Karthikeyan VS, Badhe AS, Ananthanarayanan PH. Effect of intravenous lignocaine on perioperative stress response and post-surgical ileus in elective open abdominal surgeries: a double-blind randomized controlled trial. ANZ J Surg. 2015;85:425–9.
Choi GJ, Kang H, Ahn EJ, Oh JI, Baek CW, Jung YH, Kim JY. Clinical efficacy of intravenous lidocaine for thyroidectomy: a prospective, randomized, double-Blind, placebo-controlled trial. World J Surg. 2016;40:2941–7.
Song X, Sun Y, Zhang X, Li T, Yang B. Effect of perioperative intravenous lidocaine infusion on postoperative recovery following laparoscopic cholecystectomy—a randomized controlled trial. Int J Surg. 2017;45:8–13.
Goodman NW, Stratford N. Effect of i.v. lignocaine on the breathing of patients anaesthetized with propofol. Br J Anaesth. 1995;75:573–7.
Downes H, Loehning RW. Local anesthetic contracture and relaxation of airway smooth muscle. Anesthesiology. 1977;47:430–6.
Hollmann MW, Fischer LG, Byford AM, Durieux ME. Local anesthetic inhibition of m1 muscarinic acetylcholine signaling. Anesthesiology. 2000;93:497–509.
Weiss EB, Hargraves WA, Viswanath SG. The inhibitory action of lidocaine in anaphylaxis. Am Rev Respir Dis. 1978;117:859–69.
Groeben H, Silvanus MT, Beste M, Peters J. Combined intravenous lidocaine and inhaled salbutamol protect against bronchial hyperreactivity more effectively than lidocaine or salbutamol alone. Anesthesiology. 1998;89:862–8.
Nishino T, Hiraga K, Sugimori K. Effects of i.v. lignocaine on airway reflexes elicited by irritation of the tracheal mucosa in humans anaesthetized with enflurane. Br J Anaesth. 1990;64:682–7.
Erb TO, von Ungern-Sternberg BS, Keller K, Frei FJ. The effect of intravenous lidocaine on laryngeal and respiratory reflex responses in anaesthetised children. Anaesthesia. 2013;68:13–20.
Mihara T, Uchimoto K, Morita S, Goto T. The efficacy of lidocaine to prevent laryngospasm in children: a systematic review and meta-analysis. Anaesthesia. 2014;69:1388–96.
Qi X, Lai Z, Li S, Liu X, Wang Z, Tan W. The efficacy of lidocaine in laryngospasm prevention in pediatric surgery: a network meta-analysis. Sci Rep. 2016;6:32308.
Gecaj-Gashi A, Nikolova-Todorova Z, Ismaili-Jaha V, Gashi M. Intravenous lidocaine suppresses fentanyl-induced cough in children. Cough. 2013;9:20.
Lieberman NA, Harris RS, Katz RI, Lipschutz HM, Dolgin M, Fisher VJ. The effects of lidocaine on the electrical and mechanical activity of the heart. Am J Cardiol. 1968;22:375–80.
Johns RA, DiFazio CA, Longnecker DE. Lidocaine constricts or dilates rat arterioles in a dose-dependent manner. Anesthesiology. 1985;62:141–4.
Abe S, Meguro T, Endoh N, Terashima M, Mitsuoka M, Akatsu M, Kikuchi Y, Takizawa K. Response of the radial artery to three vasodilatory agents. Catheter Cardiovasc Interv. 2000;49:253–6.
Arsyad A, Dobson GP. Lidocaine relaxation in isolated rat aortic rings is enhanced by endothelial removal: possible role of Kv, KATP channels and A2a receptor crosstalk. BMC Anesthesiol. 2016;16:121.
Rimbäck G, Cassuto J, Tollesson PO. Treatment of postoperative paralytic ileus by intravenous lidocaine infusion. Anesth Analg. 1990;70:414–9.
Harvey KP, Adair JD, Isho M, Robinson R. Can intravenous lidocaine decrease postsurgical ileus and shorten hospital stay in elective bowel surgery? A pilot study and literature review. Am J Surg. 2009;198:231–6.
Holte K, Kehlet H. Postoperative ileus: progress towards effective management. Drugs. 2002;62:2603–15.
Boeckxstaens GE, de Jonge WJ. Neuroimmune mechanisms in postoperative ileus. Gut. 2009;58:1300–11.
Tappenbeck K, Hoppe S, Reichert C, Feige K, Huber K. In vitro effects of lidocaine on contractility of circular and longitudinal equine intestinal smooth muscle. Vet J. 2013;198:170–5.
Tappenbeck K, Hoppe S, Geburek F, Feige K, Huber K. Impact of tetrodotoxin application and lidocaine supplementation on equine jejunal smooth muscle contractility and activity of the enteric nervous system in vitro. Vet J. 2014;201:423–6.
Lang A, Ben Horin S, Picard O, Fudim E, Amariglio N, Chowers Y. Lidocaine inhibits epithelial chemokine secretion via inhibition of nuclear factor kappa B activation. Immunobiology. 2010;215:304–13.
Cook VL, Jones Shults J, McDowell M, Campbell NB, Davis JL, Blikslager AT. Attenuation of ischaemic injury in the equine jejunum by administration of systemic lidocaine. Equine Vet J. 2008;40:353–7.
Ness TJ. Intravenous lidocaine inhibits visceral nociceptive reflexes and spinal neurons in the rat. Anesthesiology. 2000;92:1685–91.
Munson ES, Embro WJ. Lidocaine, monoethylglycinexylidide, and isolated human uterine muscle. Anesthesiology. 1978;48:183–6.
Oh SJ, Paick SH, Lim DJ, Lee E, Lee SE. Effects of local anesthetics on human bladder contractility. Neurourol Urodyn. 2005;24:288–94.
Borg T, Modig J. Potential anti-thrombotic effects of local anaesthetics due to their inhibition of platelet aggregation. Acta Anaesthesiol Scand. 1985;29:739–42.
Gotta AW, Sullivan CA. Platelet aggregation and the pharmacology of local anaesthetics. Drugs Exp Clin Res. 1986;12:853–6.
Berntsen RF, Simonsen T, Sager G, Olsen H. Therapeutic lidocaine concentrations have no effect on blood platelet function and plasma catecholamine levels. Eur J Clin Pharmacol. 1992;43:109–11.
Tobias MD, Henry C, Augostides YG. Lidocaine and bupivacaine exert differential effects on whole blood coagulation. J Clin Anesth. 1999;11:52–5.
Luostarinen V, Evers H, Lyytikäinen MT. Scheinin, Wahlén A. Antithrombotic effects of lidocaine and related compounds on laser-induced microvascular injury. Acta Anaesthesiol Scand. 1981;25:9–11.
Cooke ED, Bowcock SA, Lloyd MJ, Pilcher MF. Intravenous lignocaine in prevention of deep venous thrombosis after elective hip surgery. Lancet. 1977;2:797–9.
Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321:1–12.
Johnson SM, Saint John BE, Dine AP. Local anesthetics as antimicrobial agents: a review. Surg Infect. 2008;9:205–13.
Schmidt RM, Rosenkranz HS. Antimicrobial activity of local anesthetics: lidocaine and procaine. J Infect Dis. 1970;121:597–607.
Ravin CE, Latimer JM, Matsen JM. In vitro effects of lidocaine on anaerobic respiratory pathogens and strains of Hemophilus influenzae. Chest. 1977;72:439–41.
Sakuragi T, Yanagisawa K, Shirai Y, Dan K. Growth of Escherichia coli in propofol, lidocaine, and mixtures of propofol and lidocaine. Acta Anaesthesiol Scand. 1999;43:476–9.
De Amici D, Ramaioli F, Ceriana P, Percivalle E. Antiviral activity of local anaesthetic agents. J Antimicrob Chemother. 1996;37:635.
Chamaraux-Tran TN, Piegeler T. The Amide local anesthetic lidocaine in cancer surgery-potential antimetastatic effects and preservation of immune cell function? A narrative review. Front Med. 2017;20(4):235.
Cata JP, Ramirez MF, Velasquez JF, Di AI, Popat KU, Gottumukkala V, Black DM, Lewis VO, Vauthey JN. Lidocaine stimulates the function of natural killer cells in different experimental settings. Anticancer Res. 2017;37:4727–32.
Lirk P, Hollmann MW, Fleischer M, Weber NC, Fiegl H. Lidocaine and ropivacaine, but not bupivacaine, demethylate deoxyribonucleic acid in breast cancer cells in vitro. Br J Anaesth. 2014;113(Suppl 1):i32–8.
Piegeler T, Votta-Velis EG, Liu G, Place AT, Schwartz DE, Beck-Schimmer B, Minshall RD, Borgeat A. Antimetastatic potential of amide-linked local anesthetics: inhibition of lung adenocarcinoma cell migration and inflammatory Src signaling independent of sodium channel blockade. Anesthesiology. 2012;117:548–59.
Xing W, Chen DT, Pan JH, Chen YH, Yan Y, Li Q, Xue RF, Yuan YF, Zeng WA. Lidocaine induces apoptosis and suppresses tumor growth in human hepatocellular carcinoma cells in vitro and in a xenograft model in vivo. Anesthesiology. 2017;126:868–81.
Le Gac G, Angenard G, Clément B, Laviolle B, Coulouarn C, Beloeil H. Local anesthetics inhibit the growth of human hepatocellular carcinoma cells. Anesth Analg. 2017;125:1600–9.
Cassinello F, Prieto I, del Olmo M, Rivas S, Strichartz GR. Cancer surgery: how may anesthesia influence outcome? J Clin Anesth. 2015;27:262–72.
Chamaraux-Tran TN, Mathelin C, Aprahamian M, Joshi GP, Tomasetto C, Diemunsch P, Akladios C. Antitumor effects of lidocaine on human breast cancer cells: an in vitro and in vivo experimental trial. Anticancer Res. 2018;38:95–105.
Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid? The perspective of a panel of expert anesthesiologists. Anesth Analg. 1999;88:1085–91.
Euasobhon P, Dej-Arkom S, Siriussawakul A, Muangman S, Sriraj W, Pattanittum P, Lumbiganon P. Lidocaine for reducing propofol-induced pain on induction of anaesthesia in adults. Cochrane Database Syst Rev. 2016;2:CD007874.
Lang BC, Yang CS, Zhang LL, Zhang WS, Fu YZ. Efficacy of lidocaine on preventing incidence and severity of pain associated with propofol using in pediatric patients: a PRISMA-compliant meta-analysis of randomized controlled trials. Medicine (Baltimore). 2017;96:e6320.
Picard P, Tramèr MR. Prevention of pain on injection with propofol: a quantitative systematic review. Anesth Analg. 2000;90:963–9.
Jalota L, Kalira V, George E, Shi YY, Hornuss C, Radke O, Pace NL, Apfel CC, Perioperative clinical research core. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ. 2011;342:d1110.
Xing J, Liang L, Zhou S, Luo C, Cai J, Hei Z. Intravenous lidocaine alleviates the pain of propofol injection by local anesthetic and central analgesic effects. Pain Med. 2018;19:598–607.
Kranke P, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Weibel S. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015;16:CD009642.
Weibel S, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Afshari A, Kranke P. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016;116:770–83.
Weibel S, Jelting Y, Pace NL, Helf A, Eberhart LH, Hahnenkamp K, Hollmann MW, Poepping DM, Schnabel A, Kranke P. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst Rev. 2018;6:CD009642.
Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95:1331–8.
McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010;70:1149–63.
Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, McIntyre LA, Nicole PC, Fergusson DA. Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth. 2011;58:22–37.
Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2012;55:1183–94.
Ventham NT, Kennedy ED, Brady RR, Paterson HM, Speake D, Foo I, Fearon KC. Efficacy of intravenous lidocaine for postoperative analgesia following laparoscopic surgery: a meta-analysis. World J Surg. 2015;39:2220–34.
Khan JS, Yousuf M, Victor JC, Sharma A, Siddiqui N. An estimation for an appropriate end time for an intraoperative intravenous lidocaine infusion in bowel surgery: a comparative meta-analysis. J Clin Anesth. 2016;28:95–104.
De Oliveira GS, Duncan K, Fitzgerald P, Nader A, Gould RW, McCarthy RJ. Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: a randomized double-blinded placebo-controlled trial. Obes Surg. 2014;24:212–8.
McKay A, Gottschalk A, Ploppa A, Durieux ME, Groves DS. Systemic lidocaine decreased the perioperative opioid analgesic requirements but failed to reduce discharge time after ambulatory surgery. Anesth Analg. 2009;109:1805–8.
De Oliveira GS, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012;115(2):262–7.
Li J, Wang G, Xu W, Ding M, Yu W. Efficacy of intravenous lidocaine on pain relief in patients undergoing laparoscopic cholecystectomy: a meta-analysis from randomized controlled trials. Int J Surg. 2018;50:137–45.
Zhao JB, Li YL, Wang YM, Teng JL, Xia DY, Zhao JS, Li FL. Intravenous lidocaine infusion for pain control after laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97(5):e9771.
Ram D, Sistla SC, Karthikeyan VS, Ali SM, Badhe AS, Mahalakshmy T. Comparison of intravenous and intraperitoneal lignocaine for pain relief following laparoscopic cholecystectomy: a double-blind, randomized, clinical trial. Surg Endosc. 2014;28:1291–7.
Groudine SB, Fisher HA, Kaufman RP Jr, Patel MK, Wilkins LJ, Mehta SA, Lumb PD. Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg. 1998;86:235–9.
Lauwick S, Kim DJ, Mistraletti G, Carli F. Functional walking capacity as an outcome measure of laparoscopic prostatectomy: the effect of lidocaine infusion. Br J Anaesth. 2009;103:213–9.
Weinberg L, Rachbuch C, Ting S, Howard W, Yeomans M, Gordon I, McNicol L, James K, Story D, Christophi C. A randomised controlled trial of peri-operative lidocaine infusions for open radical prostatectomy. Anaesthesia. 2016;71(4):405–10.
Weinberg L, Jang J, Rachbuch C, Tan C, Hu R, McNicol L. The effects of intravenous lignocaine on depth of anaesthesia and intraoperative haemodynamics during open radical prostatectomy. BMC Res Notes. 2017;10:248.
Wuethrich PY, Romero J, Burkhard FC, Curatolo M. No benefit from perioperative intravenous lidocaine in laparoscopic renal surgery: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2012;29(11):537–43.
Jendoubi A, Naceur IB, Bouzouita A, Trifa M, Ghedira S, Chebil M, Houissa M. A comparison between intravenous lidocaine and ketamine on acute and chronic pain after open nephrectomy: a prospective, double-blind, randomized, placebo-controlled study. Saudi J Anaesth. 2017;11:177–84.
Grady MV, Mascha E, Sessler DI, Kurz A. The effect of perioperative intravenous lidocaine and ketamine on recovery after abdominal hysterectomy. Anesth Analg. 2012;115:1078–84.
Samimi S, Taheri A, Davari Tanha F. Comparison between intraperitoneal and intravenous lidocaine for postoperative analgesia after elective abdominal hysterectomy, a double-blind placebo controlled study. J Family Reprod Health. 2015;9:193–8.
Xu SQ, Li YH, Wang SB, Hu SH, Ju X, Xiao JB. Effects of intravenous lidocaine, dexmedetomidine and their combination on postoperative pain and bowel function recovery after abdominal hysterectomy. Minerva Anestesiol. 2017;83:685–94.
Chang YC, Liu CL, Liu TP, Yang PS, Chen MJ, Cheng SP. Effect of perioperative intravenous lidocaine infusion on acute and chronic pain after breast surgery: a meta-analysis of randomized controlled trials. Pain Pract. 2017;17:336–43.
Kendall MC, McCarthy RJ, Panaro S, Goodwin E, Bialek JM, Nader A, De Oliveira GS Jr. The effect of intraoperative systemic lidocaine on postoperative persistent pain using initiative on methods, measurement, and pain assessment in clinical trials criteria assessment following breast cancer surgery: a randomized, double-blind, placebo-controlled trial. Pain Pract. 2018;18:350–9.
Kim KT, Cho DC, Sung JK, Kim YB, Kang H, Song KS, Choi GJ. Intraoperative systemic infusion of lidocaine reduces postoperative pain after lumbar surgery: a double-blinded, randomized, placebo-controlled clinical trial. Spine J. 2014;14:1559–66.
Farag E, Ghobrial M, Sessler DI, Dalton JE, Liu J, Lee JH, Zaky S, Benzel E, Bingaman W, Kurz A. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology. 2013;119:932–40.
Dewinter G, Moens P, Fieuws S, Vanaudenaerde B, Van de Velde M, Rex S. Systemic lidocaine fails to improve postoperative morphine consumption, postoperative recovery and quality of life in patients undergoing posterior spinal arthrodesis. A double-blind, randomized, placebo-controlled trial. Br J Anaesth. 2017;118:576–85.
Martin F, Cherif K, Gentili ME, Enel D, Abe E, Alvarez JC, Mazoit JX, Chauvin M, Bouhassira D, Fletcher D. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology. 2008;109:118–23.
Choi KW, Nam KH, Lee JR, Chung WY, Kang SW, Joe YE, Lee JH. The effects of intravenous lidocaine infusions on the quality of recovery and chronic pain after robotic thyroidectomy: a randomized, double-blinded, controlled study. World J Surg. 2017;41:1305–12.
Striebel HW, Klettke U. Is intravenous lidocaine infusion suitable for postoperative pain management? Schmerz. 1992;6:245–50.
Echevarría GC, Altermatt FR, Paredes S, Puga V, Auad H, Veloso AM, Elgueta MF. Intra-operative lidocaine in the prevention of vomiting after elective tonsillectomy in children: a randomised controlled trial. Eur J Anaesthesiol. 2018;35:343–8.
Mathew JP, Mackensen GB, Phillips-Bute B, Grocott HP, Glower DD, Laskowitz DT, Blumenthal JA, Newman MF, Neurologic Outcome Research Group (NORG) of the Duke Heart Center. Randomized, double-blinded, placebo controlled study of neuroprotection with lidocaine in cardiac surgery. Stroke. 2009;40:880–7.
Cui W, Li Y, Li S, Wang R, Li J. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil-based anaesthesia. Eur J Anaesthesiol. 2010;27:41–6.
Peng Y, Zhang W, Kass IS, Han R. Lidocaine reduces acute postoperative pain after supratentorial tumor surgery in the PACU: a secondary finding from a randomized, controlled trial. J Neurosurg Anesthesiol. 2016;28:309–15.
Peng Y, Zhang W, Zhou X, Ji Y, Kass IS, Han R. Lidocaine did not reduce neuropsychological-cognitive decline in patients 6 months after supratentorial tumor surgery: a randomized, controlled trial. J Neurosurg Anesthesiol. 2016;28:6–13.
Samaha T, Ravussin P, Claquin C, Ecoffey C. Prevention of increase of blood pressure and intracranial pressure during endotracheal intubation in neurosurgery: esmolol versus lidocaine. Ann Fr Anesth Reanim. 1996;15:36–40.
Beaussier M, Parc Y, Guechot J, Cachanado M, Rousseau A, Lescot T, CATCH study investigators. Ropivacaine preperitoneal wound infusion for pain relief and prevention of incisional hyperalgesia after laparoscopic colorectal surgery. Colorectal Dis. 2018;20:509–19.
Hamill JF, Bedford RF, Weaver DC, Colohan AR. Lidocaine before endotracheal intubation: intravenous or laryngotracheal? Anesthesiology. 1981;55:578–81.
Pandey CK, Raza M, Ranjan R, Singhal V, Kumar M, Lakra A, Navkar DV, Agarwal A, Singh RB, Singh U, Singh PK. Intravenous lidocaine 0.5 mg kg−1 effectively suppresses fentanyl-induced cough. Can J Anaesth. 2005;52:172–5.
Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology. 2007;106:11–8.
Senturk M, Pembeci K, Menda F, Ozkan T, Gucyetmez B, Tugrul M, Camci E, Akpir K. Effects of intramuscular administration of lidocaine or bupivacaine on induction and maintenance doses of propofol evaluated by bispectral index. Br J Anaesth. 2002;89(6):849–52.
Lauwick S, Kim DJ, Michelagnoli G, Mistraletti G, Feldman L, Fried G, Carli F. Intraoperative infusion of lidocaine reduces postoperative fentanyl requirements in patients undergoing laparoscopic cholecystectomy. Can J Anaesth. 2008;55:754–60.
Gaughen CM, Durieux M. The effect of too much intravenous lidocaine on bispectral index. Anesth Analg. 2006;103:1464–5.
Neal JM, Barrington MJ, Fettiplace MR, Gitman M, Memtsoudis SG, Mörwald EE, Rubin DS, Weinberg G. The third american society of regional anesthesia and pain medicine practice advisory on local anesthetic systemic toxicity: executive summary 2017. Reg Anesth Pain Med. 2018;43:113–23.
Swenson BR, Gottschalk A, Wells LT, Rowlingson JC, Thompson PW, Barclay M, Sawyer RG, Friel CM, Foley E, Durieux ME. Intravenous lidocaine is as effective as epidural bupivacaine in reducing ileus duration, hospital stay, and pain after open colon resection: a randomized clinical trial. Reg Anesth Pain Med. 2010;35:370–6.
Ganta R, Fee JP. Pain on injection of propofol: comparison of lignocaine with metoclopramide. Br J Anaesth. 1992;69:316–7.
Masaki Y, Tanaka M, Nishikawa T. Physicochemical compatibility of propofol-lidocaine mixture. Anesth Analg. 2003;97:1646–51.
Ring J, Franz R, Brockow K. Anaphylactic reactions to local anesthetics. Chem Immunol Allergy. 2010;95:190–200.
Mertes PM, Laxenaire MC, GERAP. Anaphylactic and anaphylactoid reactions occurring during anaesthesia in France. Seventh epidemiologic survey (January 2001–December 2002). Ann Fr Anesth Reanim. 2004;23:1133–43.
Fuzier R, Lapeyre-Mestre M, Mertes PM, Nicolas JF, Benoit Y, Didier A, Albert N, Montastruc JL, French Association of Regional Pharmacovigilance Centers. Immediate- and delayed-type allergic reactions to amide local anesthetics: clinical features and skin testing. Pharmacoepidemiol Drug Saf. 2009;18:595–601.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article. MB: Consulting fees from Baxter, MSD, Aguettant and Fresenius. AD: Consulting fees from Aguettant. Payment for lecture by BBraun and Gamida. Participation to clinical research with Sandoz and Bayer. AMZ: Consulting fees from Aguettant. CE: consulting fees from Aguettant. LM: Consulting fees from BBraun and Aguettant.
Funding
No funding was received for this manuscript.
Rights and permissions
About this article
Cite this article
Beaussier, M., Delbos, A., Maurice-Szamburski, A. et al. Perioperative Use of Intravenous Lidocaine. Drugs 78, 1229–1246 (2018). https://doi.org/10.1007/s40265-018-0955-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0955-x