Abstract
Intravenous landiolol [Rapibloc® (EU)], an ultra short-acting highly cardioselective β1-blocker, is approved in the EU for the rapid short-term control of tachyarrhythmias in the perioperative and intensive care settings. It has long been used in Japan to treat perioperative tachyarrhythmias. The efficacy of landiolol has been demonstrated in a large number of randomized controlled clinical trials. Landiolol significantly reduced heart rate in patients with postoperative or intraoperative supraventricular tachycardia relative to placebo and in those with atrial fibrillation/flutter and left ventricular dysfunction relative to digoxin. It was more effective than diltiazem in converting postoperative atrial fibrillation (POAF) to normal sinus rhythm. Perioperative prophylactic administration of landiolol significantly reduced the incidence of POAF during the first week after cardiac and other surgeries, compared with diltiazem, placebo or no landiolol treatment. Landiolol also attenuated adverse haemodynamic and other responses to invasive procedures such as percutaneous coronary intervention, tracheal intubation, extubation and electroconvulsive therapy. Landiolol was generally well tolerated, with a relatively low risk of hypotension and bradycardia. Landiolol has more favourable pharmacological properties than esmolol, a short-acting β-blocker commonly used for the rapid control of heart rate. Although additional comparative studies are warranted to define the place of landiolol relative to esmolol, current evidence suggest that landiolol is a useful option for the rapid short-term control of tachyarrhythmias. Landiolol offers a simple dosage scheme and is available in two easy-to-use formulations (concentrate and powder).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intravenous ultra short-acting β1-blocker, with 8-fold greater cardioselectivity than esmolol |
Simple dosage scheme relative to esmolol; available in two easy-to-use formulations (concentrate and powder) |
Effective in heart rate and/or rhythm control in the perioperative and heart failure settings |
Prophylactic use reduces the risk of postoperative atrial fibrillation in cardiac and other surgeries |
Attenuates adverse haemodynamic and other responses to invasive procedures |
Generally well tolerated |
1 Introduction
β-adrenoceptor antagonists (β-blockers) are effective agents for both treatment and prevention of tachyarrhythmias in a range of clinical situations [1,2,3]. Landiolol [Rapibloc® (EU)] is an intravenous, ultra short-acting, cardioselective β1-blocker that was recently approved in the EU for supraventricular tachycardia (SVT), rapid control of ventricular rate in patients with atrial fibrillation or atrial flutter in perioperative, postoperative or other clinical settings where short-term control of the ventricular rate with a short-acting agent is desirable, and for noncompensatory sinus tachycardia that requires specific intervention in the physician’s judgment [4, 5]. In the EU, landiolol is available as concentrate solution (20 mg/2 ml) for injection [4] and powder (300 and 600 mg) for solution for infusion [5]. The drug has long been used in Japan (available only as 50 mg powder) to treat intraoperative and postoperative tachyarrhythmias (reviewed previously in Drugs [6]). The pharmacological properties of landiolol have been reviewed in detail [6] and are summarized in Table 1. This review is written from the EU perspective, focusing on the efficacy and tolerability of landiolol in the rapid short-term control of tachyarrhythmias.
2 Therapeutic Efficacy of Landiolol
2.1 Treatment of Supraventricular Tachycardia
2.1.1 Postoperative Supraventricular Tachycardia
Landiolol was effective in treating postoperative SVT in a randomized, double-blind, placebo-controlled, multicentre trial [7]. Eligible patients had a high risk of myocardial ischaemia or had undergone highly invasive surgery. SVT was defined as heart rate ≥ 120 beats/min (bpm) for ≥ 3 min (for sinus tachycardia) or ≥ 1 min (for all other SVT). Patients received one of two landiolol dosages (low-medium or medium–high) or placebo (Table 2). There were no significant differences between the treatment groups in patient demographic and baseline clinical characteristics. The majority of patients had undergone cardiovascular surgery (63–66%) or resection of oesophageal cancer (22–31%), and the most common types of SVT were sinus tachycardia (54–67%) or paroxysmal atrial fibrillation (26–46%) [7].
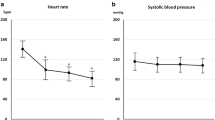
The tachycardia improvement rate was significantly higher in both landiolol groups versus placebo in the full analysis set (FAS) population (Table 2; primary endpoint), with no significant difference between the two landiolol groups [7]. Results for the per-protocol set were consistent with those of the FAS. In stratified subgroup analyses, tachycardia improvement rate tended to decrease with an increase in baseline heart rate. In both landiolol groups, heart rate significantly (p ≤ 0.0002 vs. placebo) decreased 6 min after initiation of treatment, reached the maximum reduction immediately or within 5 min after completion of treatment and increased to the level seen with placebo 30 min post treatment. Decreases in the rate pressure product (RPP, an index of cardiac load) followed a similar trend to that of heart rate, suggesting the potential of landiolol for reducing the risk of myocardial ischaemia [7].
These results are generally supported by several prospective, noncomparative or retrospective studies in patients with postoperative SVT after oesophagectomy, pulmonary resection or other invasive surgeries. For example, in a prospective study in the oesophagectomy setting, 10 of 13 (77%) patients treated with landiolol (60 µ/kg/min for 1 min then 10–40 µg/kg/min to attain the target heart rate of 20% reduction from baseline or < 100 bpm) achieved the primary endpoint of heart rate control without adverse events [8]. Similarly, a representative retrospective study in this setting showed that landiolol (started at 3–10 µg/kg/min then titrated to control the heart rate at < 100 bpm; n = 11) was significantly (p < 0.05) more effective than conventional agents (n = 13) with respect to percent reduction from baseline in heart rate 1 h post treatment (28.5 vs. 12.3%), conversion rate to normal sinus rhythm (NSR) within 2 h (62.5 vs. 7.7%) and time to conversion to NSR (3.6 vs. 23.3 h) [9].
Catecholamines are used to support cardiac contraction after weaning from cardiopulmonary bypass; however, they may cause tachycardia after weaning [10]. In a randomized trial in this setting (n = 30), combined administration of landiolol 3–5 µg/kg/min and catecholamines significantly (p < 0.05 vs. control) decreased heart rate without affecting blood pressure and cardiac index [10].
2.1.1.1 Postoperative Atrial Fibrillation
As reviewed earlier [6], landiolol was more effective than diltiazem in converting POAF after open heart surgery to NSR (primary endpoint) in the JL-KNIGHT study (Table 2) [11]. These results are generally supported by retrospective studies in patients who developed POAF after open heart surgery [12], oesophageal cancer surgery [13], pulmonary resection for lung cancer [14] or during the early postoperative period in the ICU [15]. Landiolol (n = 69) was more effective than conventional anti-arrhythmic agents (n = 65) after open heart surgery in terms of the proportion of patients achieving conversion to NSR within 90 min of administration and maintaining it for 24 h (73.9 vs. 56.9%; p < 0.05; primary efficacy endpoint) or those achieving a 20% reduction from baseline in ventricular rate (97.1 vs. 49.2%; p < 0.001) [12]. Conversion rates to NSR with landiolol appeared to be higher in patients who had undergone off-pump coronary artery bypass grafting (CABG) than in those who had undergone cardiopulmonary bypass surgery [12]. First-line therapy with landiolol was generally associated with good rates of conversion to NSR within 72 h in patients who had undergone transthoracic oesophagectomy [13]. In ICU patients, the estimated median time to conversion to NSR was significantly (p = 0.0355) shorter with landiolol (n = 32) than amiodarone (n = 23) [75 vs. 150 min; primary outcome], although there was no significant between-group difference in rates of conversion to, or maintenance of, NSR [15].
2.1.2 Intraoperative Supraventricular Tachycardia
The efficacy of landiolol in the treatment of intraoperative SVT has been demonstrated in several randomized trials [6]. Results from the most recent double-blind, multicentre, placebo-controlled phase 2 study showed that landiolol was effective in treating SVT during anaesthesia [16]. Study treatments were started 30 min after surgery if heart rate was ≥ 100 bpm for > 3 min (for sinus tachycardia) or > 1 min (for all other SVT). If the heart reduction did not reach a prespecified target, rescue medication (esmolol) was administered. The proportion of patients receiving rescue medication (primary endpoint) was significantly lower in the landiolol than placebo group (Table 2). Landiolol was also significantly (p < 0.0001) better than placebo with respect to SVT improvement rate (74.58 vs. 9.84%), time to > 10% reduction from baseline in heart rate (2.65 vs. 4.58 min), mean heart rate 5 min after treatment (85.98 vs. 105.14 bpm) and mean heart rate reduction from baseline after 5 min (21.89 vs. 4.34%). Over a 11-min observation period, landiolol significantly (p < 0.05) decreased systolic blood pressure (SBP) during the first 5 min and RPP at multiple time points versus placebo [16].
2.1.3 Tachyarrhythmia in Heart Failure
Landiolol 1–10 µg/kg/min was more effective than digoxin in controlling rapid heart rate during atrial fibrillation/flutter in patients with left ventricular dysfunction (LVD) in the J-LAND trial [17]. Eligible patients had heart failure [New York Heart Association (NYHA) class III or IV], atrial fibrillation/flutter, a left ventricular ejection fraction (LVEF) of 20–50% and heart rate ≥ 120 bpm. There were no significant differences between the treatment groups in patient baseline demographic and disease characteristics. Significantly more landiolol than digoxin recipients achieved successful heart rate control at 2 h after initiation of treatment (primary endpoint; Table 2) [17]. Similar results were seen regardless of baseline patient characteristics (age, sex, heart rate, SBP, LVEF, previous use of oral β-blockers, estimated glomerular filtration rate) [18]. Significantly (p < 0.001) more landiolol than digoxin recipients achieved the primary endpoint in the NYHA class III subgroup (52.3 vs. 13.8%), with favourable but not statistically significant results seen in the class IV subgroup (35.3 vs. 9.1%). Landiolol was regarded as particularly useful in patients with renal impairment as it can be uptitrated to achieve the target heart rate regardless of the degree of renal impairment [18].
In prospective noncomparative trials (n = 23–52), landiolol as an adjunct to conventional therapy (diuretics, vasodilators and inotropes such as dopamine, dobutamine and milrinone) was effective in reducing heart rate without decreasing blood pressure in patients with acute decompensated heart failure (ADHF) and atrial fibrillation [19, 20], ADHF and tachycardia [21] or heart failure and SVT (30, 45 and 25% had paroxysmal or persistent atrial fibrillation, or atrial tachycardia, respectively) [22]. Landiolol-induced heart rate reduction was significantly (p < 0.05) greater in diastolic than systolic heart failure at 1 and 2 h after treatment (but not at later time points) [19], was significantly (p < 0.05) greater in patients with preserved LVEF (≥ 40%) than reduced LVEF (< 40%) [20] and occurred despite previous treatment with amiodarone [22]. Landiolol treatment was also associated with improvements in LVEF and NYHA class, with the latter improving further following additional therapy such as oral β-blockers, pulmonary vein catheter ablation or cardiac resynchronisation therapy [22]. A low dosage of landiolol (1.5 µg/kg/min) in combination with milrinone improved cardiac haemodynamic parameters and eliminated pulsus alternans in patients with ADHF and tachycardia [21]. The cardioprotective mechanism of landiolol is linked, at least in part, to correction of abnormal intracellular Ca2+ handling in failing cardiomyocytes [23].
Supportive data for the use of landiolol to control heart rate in patients with heart failure are available from several retrospective studies [24,25,26,27,28]. Landiolol was more effective than diltiazem in reducing heart rate in patients with heart failure and SVT [24]. Furthermore, in hospitalized patients with acute heart failure and SVT, switching to oral β-blocker therapy was achieved significantly (p = 0.002) earlier with landiolol than with diltiazem (2 vs. 4 days) although there was no significant between-group difference in the length of hospital stay [25]. Landiolol was effective in treating both atrial tachyarrhythmias and refractory ventricular tachyarrhythmias in patients with heart failure; the predictors of response to landiolol were a preserved LVEF in atrial tachyarrhythmias and a smaller left ventricular diastolic or systolic diameters in ventricular tachyarrhythmias [26]. However, when the bradycardic effect of landiolol was assessed in different types of atrial tachyarrhythmias in patients with LVD, landiolol was effective in atrial fibrillation but was largely ineffective in atrial flutter/tachycardia [27]. Of note, co-administration of landiolol with dobutamine did not appear to affect the negative chronotropic action of landiolol in patients with acute heart failure syndrome and atrial tachyarrhythmia [28]. Besides being effective in heart failure, landiolol also effectively reduced heart rate without increasing arterial pressure in patients with severe sepsis, SVT and arrhythmias [29].
2.2 Prevention of Postoperative Atrial Fibrillation
2.2.1 Cardiac Surgery
The efficacy of landiolol in the prevention of POAF was evaluated in several randomized trials in patients undergoing CABG, valvuloplasty or valve replacement, either off-pump or on cardiopulmonary bypass (Table 3) [30,31,32,33,34,35,36]. Exclusion criteria included cardiogenic shock [34, 35], sinus bradycardia [30, 34, 35] or sick sinus syndrome [33], 2nd- or 3rd-degree atrioventricular block [30, 33,34,35,36], arrhythmias [30, 31, 33,34,35] and thyroid dysfunction [30, 34, 35]. While some trials excluded patients with an ejection fraction of < 20% [33] or a LVEF of < 30–40% [32, 36], the PLATON trial included patients with LVD (LVEF of ≤ 35%) [30]. Timing, duration and dosage of landiolol administration varied across trials (Table 3). The primary endpoint was the incidence of POAF within 7 days post-surgery in most trials. Atrial fibrillation deemed to have occurred if it persisted for ≥ 1 min [36], ≥ 5 min [30, 31, 34, 35] or ≥ 10 min [32, 33], or required treatment because of haemodynamic changes [30, 31, 33,34,35].
Landiolol was more effective than diltiazem, placebo or no landiolol treatment in preventing POAF in patients undergoing a cardiac surgery (Table 3) [30,31,32,33,34, 36]. A relatively low dose of landiolol significantly decreased the incidence of POAF compared with diltiazem following CABG [31]. In PASCAL, the incidence of POAF was significantly lower in the landiolol than placebo group [34]. The follow-up BABYLON trial evaluated a higher landiolol dosage and landiolol plus bisoprolol, compared with placebo (Table 3); this trial was stopped early because a significant difference between landiolol plus bisoprolol and placebo groups was reached, while the incidence of adverse events did not differ among the treatment groups [35]. Landiolol followed by oral carvedilol after CABG significantly decreased the incidence of POAF relative to placebo followed by oral carvedilol [33]. Landiolol treatment was also associated with a lower POAF incidence compared with no landiolol treatment in the PLATON trial in patients with LVD undergoing a cardiac surgery [30].
In addition to reducing the POAF risk, landiolol showed other benefits in patients undergoing a cardiac surgery [30,31,32,33,34,35,36]. Although there was no significant difference between landiolol and diltiazem in haemodynamic parameters [31], landiolol significantly (p < 0.05) decreased heart rate versus placebo or no landiolol treatment, without significantly affecting blood pressure [30, 33,34,35,36]. Furthermore, in PASCAL [34] and BABYLON [35], landiolol significantly (p < 0.05 vs. placebo) decreased levels of biomarkers for myocardial ischemia [creatine kinase isoenzyme MB (CK-MB), troponin-I, human heart fatty acid binding protein (H-FABP)], inflammation [interleukin-6 and -8, high-sensitive C-reactive protein (CRP), Pentraxin-3], oxidative stress (asymmetric dimethylarginine) and heart failure [brain natriuretic peptide (BNP)] at various postoperative time points. Similar results were reported for troponin-I, H-FABP, high-sensitive CRP and BNP in the PLATON trial [30] and for CRP in another trial [32]. In some studies, landiolol showed favourable effects on CK-MB (vs. no landiolol treatment) or troponin-I levels (vs. placebo), although statistical significance was not reached [30, 32, 33]. Landiolol was also associated with a significantly (p < 0.05) shorter hospital stay in PASCAL (mean 11.2 vs. 14.0 days in the placebo group) [34] and PLATON (median 12.0 vs. 14 days in the no landiolol group) [30], with significantly (p < 0.05) lower average medical cost relative to placebo in PASCAL [34].
Results from randomized trials were generally supported by a number of retrospective studies and meta-analyses. For example, in the most recent meta-analysis of six fully published randomized trials (n = 571), the incidence of POAF 1 week after cardiac surgery was significantly lower in the landiolol group relative to the control group (placebo or no landiolol treatment) [odds ratio 0.27; 95% CI 0.18–0.42]; in three trials reporting in-hospital mortality and postoperative complications, there were no significant differences between the groups [37]. A large network meta-analysis (n = 2157) did not find significant differences among eight β-blockers (atenolol, betaxolol, bisoprolol, carvedilol, landiolol, landiolol plus bisoprolol, metoprolol, propranolol) in preventing POAF after CABG, although the estimated probability ranking for efficacy was the highest for bisoprolol and landiolol plus bisoprolol [38].
2.2.2 Other Surgeries
Several randomized trials evaluated the efficacy of landiolol in POAF prevention in patients undergoing oesophageal cancer surgery [39,40,41] or pulmonary lobectomy [42] (Table 3). Exclusion criteria included arrhythmias [40,41,42], 2nd- or 3rd-degree atrioventricular block [39, 40, 42], heart failure [39, 42], myocardial infarction [41, 42], cardiac shock [39] and hypotension [42]. The primary or main endpoint was POAF incidence at various postoperative time points. Atrial fibrillation was considered to have occurred if it lasted for ≥ 5 min [39, 40], 10 min [41] or ≥ 30 min [42]. Some trials also assessed postoperative tachycardia incidence [39, 41].
Landiolol significantly reduced the incidence of POAF in patients undergoing oesophagectomy (in 2 of 3 trials) [40, 41] or pulmonary lobectomy [42] compared with placebo or no landiolol treatment (Table 3). Furthermore, landiolol significantly reduced heart rate [40], sinus tachycardia after surgery (0 vs. 25% of patients) [41], grade II or greater postoperative complications (40 vs. 60% of patients) [40] and interleukin-6 levels [40, 41], compared with control (p < 0.05 for all outcomes). In one trial involving oesophagectomy, the POAF incidence was too low to detect any statistical difference between the landiolol and no landiolol groups (Table 3) while there was no significant between-group difference in the postoperative tachycardia incidence (12.5 vs. 12.8%) [39].
In a randomized, double-blind, placebo-controlled trial in postoperative patients recovering in the ICU, landiolol 5 µg/kg/min administered from midnight until 6 a.m. prevented an increase of QT dispersion (QTD), demonstrating its potential antiarrhythmic effect by improving ventricular repolarization [43].
2.3 Treatment or Prevention of Adverse Haemodynamic and Other Responses to Invasive Procedures
2.3.1 Percutaneous Coronary Intervention
In the percutaneous coronary intervention (PCI) setting, landiolol treatment was associated with improvements in myocardial oxygen demand, myocardial injury and reperfusion status in the acute phase, and cardiac function in the chronic phase [44,45,46,47]. In a randomized open-label trial in 70 patients undergoing elective PCI, landiolol significantly (p ≤ 0.04 vs. saline control) reduced the incidence of myocardial injury (56 vs. 79%) and myocardial infarction (41 vs. 70%), defined as cardiac troponin-I levels of ≥ 0.05 and ≥ 0.12 ng/ml at 24 h after PCI, respectively [45]. Landiolol was administered at an intracoronary dosage of 60 µg/kg for 1 min before and after balloon inflation, followed by an intravenous infusion of 20 µg/kg/min from the time of stent placement until 6 h after PCI [45].
Landiolol improved reperfusion status [44] and cardiac function [46] in patients undergoing primary PCI for ST-elevated myocardial infarction (STEMI). In a prospective trial, landiolol 3 µg/kg/min from just before reperfusion to 6–12 h after PCI (n = 55) was associated with significantly (p < 0.05) higher rates of ST-resolution (64 vs. 42%) and myocardial blush grade 2 or 3 after reperfusion (64 vs. 45%), and significantly (p < 0.05) lower rates of non-sustained ventricular tachycardia (27 vs. 50%) and progression to Killip class grade III or IV (0 vs. 10%) relative to historical control (n = 60) [44]. In a randomized trial, landiolol 3 µg/kg/min from just after PCI until 24 h (n = 44) significantly (p = 0.01) improved LVEF from 2 weeks to 6 months after PCI (49.1 vs. 52.0%) whereas no significant change in LVEF was seen in the no landiolol group (n = 47) [46]. Furthermore, the left ventricular end-diastolic volume index significantly (p = 0.02) increased during the same time period in the control group but did not change significantly in the landiolol group, suggesting that landiolol may inhibit cardiac remodelling in the chronic phase of PCI [46].
According to a noncomparative pilot trial (n = 22), landiolol may reduce myocardial oxygen demand by reducing heart rate without lowering SBP or diastolic blood pressure (DBP) in patients undergoing PCI for acute coronary syndrome [47]. The prospective [44] and randomized [46] trials in the PCI setting have also confirmed that landiolol significantly (p ≤ 0.01) reduced heat rate, although its effect on BP varied depending upon when it was used. Significant reductions (p < 0.05 vs. control) in BP were noted when landiolol was administered before and after PCI (change from admission time to just after PCI − 24.0% vs. − 15.5% for SBP, − 26.4 vs. − 18.4% for DBP) [44] but not when it was used only after PCI [46].
2.3.2 Other Invasive Procedures
The efficacy of landiolol in suppressing adverse haemodynamic and other responses to invasive procedures during noncardiac surgery and electroconvulsive therapy (ECT) has been reviewed in detail previously [6]; therefore, a brief overview is presented here, with results from representative randomized trials summarized in Table 4 [48,49,50,51,52,53,54].
In randomized controlled trials, landiolol attenuated the increase in heart rate in response to intubation relative to placebo, without markedly affecting (and improving in some trials) blood pressure (Table 4) [48, 50,51,52, 54]. These results are generally supported by a systematic review, indicating a lower maximum change from baseline with landiolol versus placebo in heart rate (11.1 vs. 42.7%), SBP (− 0.3 vs. 16.0%) and mean blood pressure (28.7 vs. 39.1%) following laryngoscopy and tracheal intubation [55]. The efficacy of landiolol in attenuating haemodynamic changes associated with intubation was generally similar to that of esmolol [52], remifentanil [50] or propofol [49] and possibly greater than that of nicardipine [49] (Table 4). Bispectral index (BIS) values increased significantly (p < 0.05) 1 min after intubation in the control group but remained unchanged in the landiolol or esmolol groups [52]. However, as could be expected with anaesthetics, propofol [49] and remifentanil [50] were associated with lower BIS values relative to landiolol after intubation. Landiolol has also shown the potential to reduce the risk of cardiac arrhythmias during induction of anaesthesia and intubation by prolonging the RR interval and shortening the QT interval, QTc interval and QTD [56].
Landiolol prevented the increase in heart rate associated with emergence from anaesthesia and extubation in general surgery patients in randomized trials [6]. For example, in patients undergoing craniotomy, the increase in heart rate from baseline (before anaesthesia) to immediately after extubation was smaller in the landiolol than in the control group (Table 4) [48]. Landiolol also attenuated the increase in blood pressure associated with extubation, although the effect was somewhat varied across clinical trials [6]. In a randomized study in elderly patients undergoing gastric surgery, landiolol and esmolol were generally similar in preventing an increase in heart rate and mean arterial pressure during perioperative period [57]. In the elderly, landiolol 125 µg/kgmin for 1 min then 40 µg/kg/min may be effective in attenuating extubation-related increase in heart rate and SBP in normotensive patients, whereas a higher dosage (250 µg/kg/min for 1 min then 80 µg/kg/min) may be required in hypertensive patients [6].
Landiolol also attenuated haemodynamic responses to other invasive procedures such as endotracheal suctioning in intubated ICU patients [58], local epinephrine infiltration during vaginal total hysterectomy [59] and pin fixation during craniotomy [48]. Furthermore, it was associated with a lower requirement of anaesthetics such as sevoflurane and propofol during hip, abdominal or general surgery and a lower intraoperative fentanyl requirement during craniotomy [6]. In elderly patients undergoing gastric surgery, landiolol- and esmolol-related reduction in sevoflurane dose was associated with a shorter time to eye opening and extubation, and a quicker recovery in cognitive function, compared with placebo [57].
Landiolol attenuated the increase in heart rate (and blood pressure in some cases) associated with ECT in psychiatric patients in several randomized trials [6]. For example, in the largest randomized crossover trial, landiolol significantly decreased heart rate and mean arterial pressure associated with ECT (Table 4), without affecting seizure duration or recovery times [53]. In a small open-label trial, both landiolol and esmolol prevented tachycardia associated with ECT without affecting cerebral blood flow, but only esmolol also attenuated the increase in blood pressure [60].
3 Tolerability of Landiolol
Landiolol was generally well tolerated in clinical trials and postmarketing studies [4]. The most common adverse events reported in landiolol recipients were hypotension and bradycardia. In controlled clinical trials, the incidence of hypotension in landiolol (n = 948), active comparator, no landiolol and placebo groups was 8.5, 8.5, 5.7 and 2.1%, respectively; the corresponding incidence of bradycardia was 2.1, 2.5, 2.4 and 0%. In uncontrolled trials, hypotension and bradycardia occurred in 8.6 and 0.5% of 581 landiolol recipients. However, in postmarketing studies (n = 1257), the incidence of hypotension was relatively lower (0.8%), with bradycardia reported in 0.7% of patients. All cases of hypotension and bradycardia improved or resolved without any intervention or within minutes after discontinuation of landiolol with or without additional treatment [4].
Some serious adverse events have been reported with landiolol in clinical and postmarketing studies [4]. Perioperative use of landiolol in a clinical trial was associated with shock due to severe hypotension in one patient with heavy bleeding; this event resolved 10 min after discontinuation of landiolol, prostaglandine and isoflurane. Cardiac arrest, complete atrioventricular block, sinus arrest and severe bradycardia have occurred with landiolol, mainly in elderly patients or in those with complications of hypertension or cardiac diseases [4].
In controlled clinical studies, changes in laboratory parameters occurred in 8.7 and 13.6% of patients in the landiolol and control groups (n = 241 and 243), with abnormal changes in ALT, AST or bilirubin reported in 5 and 7% of patients in the respective groups [4]. The changes in laboratory parameters resolved or remitted and were not clinically relevant [4].
In the JL-KNIGHT study, landiolol was associated with a significantly (p < 0.05) lower incidence of hypotension (11.4 vs. 30.6%) and bradycardia (0 vs. 11.1%) than diltiazem [11]. In J-LAND, landiolol did not differ significantly from digoxin with respect to the overall incidence of adverse events (32.3 vs. 32.7%) or the incidence of hypotension (7.5 vs. 3.7%), although adverse events occurred more frequently in the landiolol group during the initial 2 h treatment period (8.6 vs. 1.9%; p = 0.029) [17]. Following bolus administrations, the tolerability profile of landiolol was generally similar to that of esmolol in healthy Caucasian volunteers [61]. Following 24-h infusions, the incidence of local reactions was significantly (p value not reported) lower with landiolol 12 mg/mL than with esmolol 10 mg/mL in healthy Caucasian volunteers (16 vs. 50%) [62].
4 Dosage and Administration of Landiolol
Landiolol is not intended for use in chronic settings and should be administered by a well-qualified healthcare professional in a monitored setting [4, 5]. For short-term heart rate control, the recommended starting dosage is 0.1–0.2 mg/kg bolus injection which provides a bradycardic effect that may last for 5–20 min; if the efficacy is not sufficient, the dosage can be increased up to 0.2 or 0.3 mg/kg [4]. The maximum recommended dosage is 100 mg/patient/day divided into 5–15 doses per day [4].
For longer term administration, a landiolol intravenous infusion prepared from the powder formulation should be used [5]. When rapid (within 2–4 min) onset of bradycardic effect is required, the infusion should be initiated with a loading dose of 100 µg/kg for 1 min, followed by a maintenance dose of 10–40 µg/kg/min. When rapid onset of bradycardic effect is not required, starting the infusion with the maintenance dose without the loading dose will provide the effect within 10–20 min. The maintenance dose may be increased up to 80 µg/kg/min if the efficacy is not sufficient and the cardiovascular status of the patient requires and allows such an increase. The maximum recommended daily dose is 8064 mg/patient/day. Once adequate heart rate control and a stable clinical status is achieved with landiolol, switching to an alternative drug (e.g. oral antiarrhythmics) may be accomplished in a stepwise manner. Reconstituting 300 and 600 mg landiolol powder in 50 mL (i.e. 6 and 12 mg/mL) allows easy flow rate (mL/h) calculation for any given dosage; for example, for an 80 kg individual requiring 10 µg/kg/min, the flow rate for the 6 mg/mL strength is 8 mL/h [5].
Landiolol dosage should be adjusted to individual patient needs and to manage adverse events, and it should be done with extra caution in patients with low SBP [4, 5]. For longer term administration in patients with LVD (LVEF < 40%, cardiac index < 2.5 L/min/m2, NYHA class 3–4) such as after cardiac surgery, during ischemia or in a septic state, starting the maintenance dose at 1 µg/kg/min and increased up to 10 µg/kg/min in a stepwise manner under close blood pressure monitoring has been shown to achieve heart rate control [5]. Dosage adjustment is not needed when landiolol is given to the elderly or patients with renal impairment. Since data are limited for patients with hepatic impairment, careful administration of landiolol, starting with a lower dose is recommended in this population [4, 5]. The concentrate formulation contains ethanol and therefore, is not recommended for the paediatric population [4]. The powder formulation may be used in this population but a dosage recommendation cannot be made because of limited clinical data [4, 5].
Contraindications to landiolol include: severe forms of bradycardia, sick sinus syndrome, 2nd- or 3rd-degree atrioventricular block, hypotension and uncorrectable metabolic acidosis; cardiogenic shock; decompensated heart failure unrelated to arrhythmia; pulmonary hypertension; untreated phaeochromocytoma; and, acute asthmatic attack [4, 5]. Local prescribing information should be consulted for detailed information on contraindications, special warnings and precautions, and use in special patient populations.
5 Place of Landiolol in the Acute Management of Tachyarrhythmias
The European Society of Cardiology treatment guidelines recommend β-blockers as a treatment option for supraventricular arrhythmias [3], POAF [2] and atrial fibrillation in patients with heart failure [1]. Although numerous oral and intravenous β-blockers are available for heart rate and/or rhythm control, ultra short-acting β-blockers such as landiolol or esmolol are well suited for the rapid short-term control of tachyarrhythmias. Landiolol is a newer generation agent, with more favourable pharmacological characteristics than esmolol in terms of β1/β2 selectivity, bradycardic potency, negative inotropic potential and pharmacochaperoning activity (Table 1).
The onset of bradycardic effect, ease of administration, dosage titratability and quick reversal of β-blockade are important factors in selecting β-blockers for haemodynamic management during emergency situations. In clinical studies, landiolol exhibited a fast onset (1–6 min) and offset (5–10 min) of action, and a short terminal half-life of 3–5 min (Table 1). Thus, it is readily titratable and its effects are rapidly reversible upon discontinuation of the drug. Furthermore, the two available formulations of landiolol allow for an easy dosage scheme. While the concentrate formulation allows for rapid preparation of the required dosage during emergency situations, calculating hourly flow rate for the powder formulation is easy when reconstituted in 50 mL (reconstituted strength 6 and 12 mg/mL; Sect. 4). Flow rate calculation and posology of landiolol is simpler in the EU than in Japan, where landiolol is available only as 50 mg powder (reconstituted strength 10 mg/ml). The posology of landiolol is also relatively simple compared with that of esmolol [61].
Landiolol was more effective than placebo with respect to postoperative SVT improvement rate in patients with a high risk of myocardial ischemia or in those who have undergone a highly invasive surgery; landiolol also decreased RPP in these patients, thereby reducing the risk of myocardial ischemia (Sect. 2.1.1). In patients with POAF following open heart surgery, significantly more landiolol than diltiazem recipients achieved conversion to NSR within 8 h of treatment (Sect. 2.1.1.1). Landiolol effectively controlled intraoperative SVT during induction of anaesthesia, with minimal effect on SBP (Sect. 2.1.2). Landiolol was more effective than digoxin in controlling rapid heart rate during atrial fibrillation/flutter in patients with heart failure and LVD; landiolol may be particularly beneficial in this setting in patients with impaired renal function (Sect. 2.1.3).
Perioperative prophylactic administration of landiolol was more effective than diltiazem, placebo or no landiolol treatment in reducing the incidence of POAF during the first week after cardiac surgery, oesophagectomy or pulmonary lobectomy (Sect. 2.2). This effect was thought to be related to anti-ischemic, anti-inflammatory and antioxidant properties of landiolol in addition to its β-blockade [34, 35].
Landiolol attenuated adverse haemodynamic and other response to invasive procedures such as PCI, tracheal intubation, extubation and ECT (Sect. 2.3). In the PCI setting, landiolol decreased myocardial injury and myocardial infarction, and improved reperfusion status and LVEF (Sect. 2.3.1). The effect of landiolol in attenuating an increase in heart rate and blood pressure associated with intubation was generally similar to that of esmolol, remifentanil and propofol and possibly greater than that of nicardipine (Sect. 2.3.2).
Landiolol was generally well tolerated (Sect. 3). The risk of hypotension and bradycardia with landiolol was relatively low and similar to, or lower than, that of active comparators. Because of its lesser potent negative inotropic effect (Table 1), landiolol may carry a lower risk of hypotension than esmolol.
Although some head-to-head comparative studies of landiolol and esmolol are available, additional studies are warranted to clearly define the role landiolol relative to esmolol in the acute management of tachyarrhythmias in postoperative and critically ill patients. Robust cost effectiveness analyses of landiolol would also be of interest. According to a pharmacoeconomic model (abstract [63]), landiolol may reduce total hospital costs compared with no intervention, standard-of-care or esmolol when used for the prevention of POAF.
In conclusion, intravenous landiolol is an ultra-short acting highly cardioselective β1-blocker, which has been proven effective and well tolerated for the rapid control of heart rate in a variety of perioperative and intensive care situations. It offers a relatively simple posology and is available in two easy-to-use formulations (concentrate and powder). Although additional comparative studies are warranted to definitively place landiolol relative to esmolol, current evidence suggest that landiolol is a useful option for the rapid short-term control of tachyarrhythmia.
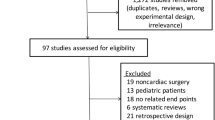
Data Selection Landiolol: 237 records identified
Duplicates removed | 47 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 22 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 99 |
Cited efficacy/tolerability articles | 57 |
Cited articles not efficacy/tolerability | 12 |
Search Strategy: EMBASE, MEDLINE and PubMed from 2013 to present. Previous Adis Drug Evaluation published in 2013 was hand-searched for relevant data. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Landiolol, ONO-1101, Atrial fibrillation, Tachyarrhythmia, Tachycardia. Records were limited to those in English language. Searches last updated 30 Jan 2018. | |
References
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail. 2016;18(8):891–975.
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42(18):1493–531.
Rapibloc 20 mg/2 ml concentrate for solution for injection: summary of product characteristics. 2017. http://www.medicinesauthority.gov.mt. Accessed 21 Dec 2017.
Rapibloc 300 mg and 600 mg powder for solution for infusion: summary of product characteristics. 2017. https://mri.cts-mrp.eu. Accessed 24 Jan 2018.
Plosker GL. Landiolol: a review of its use in intraoperative and postoperative tachyarrhythmias. Drugs. 2013;73(9):959–77.
Taenaka N, Kikawa S. The effectiveness and safety of landiolol hydrochloride, an ultra-short-acting β1-blocker, in postoperative patients with supraventricular tachyarrhythmias: a multicenter, randomized, double-blind, placebo-controlled study. Am J Cardiovasc Drugs. 2013;13(5):353–64.
Mori K, Yamada K, Fukuda T, et al. Landiolol hydrochloride for early postoperative tachycardia after transthoracic esophagectomy. Surg Today. 2014;44(5):848–54.
Niwa Y, Koike M, Iwata N, et al. Effect of landiolol hydrochloride on tachyarrhythmia after esophagectomy. Hepatogastroenterology. 2014;61(134):1546–51.
Hamaguchi S, Nagao M, Takahashi Y, et al. Low dose landiolol combined with catecholamine can decrease heart rate without suppression of cardiac contraction after cardiopulmonary bypass. Dokkyo J Med Sci. 2014;41(1):27–33.
Sakamoto A, Kitakaze M, Takamoto S, et al. Landiolol, an ultra-short-acting β1-blocker, more effectively terminates atrial fibrillation than diltiazem after open heart surgery: prospective, multicenter, randomized, open-label study (JL-KNIGHT study). Circ J. 2012;76(5):1097–101.
Nishi H, Sakaguchi T, Miyagawa S, et al. Efficacy of landiolol hydrochloride for atrial fibrillation after open heart surgery. Heart Vessels. 2013;28(4):490–6.
Ojima T, Iwahashi M, Nakamori M, et al. Atrial fibrillation after esophageal cancer surgery: an analysis of 207 consecutive patients. Surg Today. 2014;44(5):839–47.
Nojiri T, Yamamoto K, Maeda H, et al. Efficacy of low-dose landiolol, an ultrashort-acting β-blocker, on postoperative atrial fibrillation in patients undergoing pulmonary resection for lung cancer. Gen Thorac Cardiovasc Surg. 2011;59(12):799–805.
Shibata SC, Uchiyama A, Ohta N, et al. Efficacy and safety of landiolol compared to amiodarone for the management of postoperative atrial fibrillation in intensive care patients. J Cardiothorac Vasc Anesth. 2016;30(2):418–22.
Xiao J, He P, Zou Q, et al. Landiolol in the treatment of the intraoperative supraventricular tachycardia: a multicenter, randomized, double-blind, placebo-controlled study. J Clin Anesth. 2015;27(2):120–8.
Nagai R, Kinugawa K, Inoue H, et al. Urgent management of rapid heart rate in patients with atrial fibrillation/flutter and left ventricular dysfunction: comparison of the ultra-short-acting β1-selective blocker landiolol with digoxin (J-Land Study). Circ J. 2013;77(4):908–16.
Kinugawa K, Nagai R, Inoue H, et al. Impacts of patient characteristics on the effectiveness of landiolol in AF/AFL patients complicated with LV dysfunction: subgroup analysis of the J-Land study. Adv Ther. 2014;31(4):426–39.
Kobayashi S, Murakami W, Myoren T, et al. A low-dose β1-blocker effectively and safely slows the heart rate in patients with acute decompensated heart failure and rapid atrial fibrillation. Cardiology. 2014;127(2):105–13.
Ozaki T, Yamada T, Morita T, et al. Urgent control of rapid atrial fibrillation using landiolol in patients with acute decompensated heart failure with reduced or preserved left ventricular ejection fraction [abstract no. P6352]. Eur Heart J. 2016;37(Suppl.):1319.
Kobayashi S, Susa T, Tanaka T, et al. Low-dose beta-blocker in combination with milrinone safely improves cardiac function and eliminates pulsus alternans in patients with acute decompensated heart failure. Circ J Off J Jpn Circ Soc. 2012;76(7):1646–53.
Adachi T, Sato A, Baba M, et al. Novel use of the ultra-short-acting intravenous beta1-selective blocker landiolol for supraventricular tachyarrhythmias in patients with congestive heart failure. Heart Vessels. 2014;29(4):464–9.
Kobayashi S, Susa T, Ishiguchi H, et al. A low-dose β1-blocker in combination with milrinone improves intracellular Ca2+ handling in failing cardiomyocytes by inhibition of milrinone-induced diastolic Ca2+ leakage from the sarcoplasmic reticulum. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0114314.
Kimura Y, Aga C, Hayashi H, et al. Efficacy and safety of landiolol in heart failure patients with supraventricular tachycardia compared to diltiazem [abstract no. O01-3]. J Card Fail. 2016;22(9 Suppl. 1):167.
Kiuchi S, Aikawa H, Hisatake S, et al. Efficacy of intravenous administration of landiolol in patients with acute heart failure and supraventricular tachyarrhythmia. J Clin Med Res. 2017;9(5):426–32.
Wada Y, Aiba T, Tsujita Y, et al. Practical applicability of landiolol, an ultra-short-acting beta1-selective blocker, for rapid atrial and ventricular tachyarrhythmias with left ventricular dysfunction. J Arrhythm. 2016;32(2):82–8.
Oka E, Iwasaki Y, Fujimoto Y. Differential effectiveness of landiolol among atrial fibrillation and atrial flutter/tachycardia in the patients with left ventricular dysfunction [abstract no. PE-776]. In: In: 81st Annual Scientific Meeting of the Japanese Circulation Society. 2017.
Yoshima S. Concomitant administration of landiolol and dobutamine in acute heart failure syndrome with atrial tachyarrhythmia [abstract no. P2699]. Eur Heart J. 2017; 38(Suppl).
Okajima M, Takamura M, Taniguchi T. Landiolol, an ultra-short-acting beta1-blocker, is useful for managing supraventricular tachyarrhythmias in sepsis. World J Crit Care Med. 2015;4(3):251–7.
Sezai A, Osaka S, Yaoita H, et al. Safety and efficacy of landiolol hydrochloride for prevention of atrial fibrillation after cardiac surgery in patients with left ventricular dysfunction: Prevention of Atrial Fibrillation After Cardiac Surgery With Landiolol Hydrochloride for Left Ventricular Dysfunction (PLATON) trial. J Thorac Cardiovasc Surg. 2015;150(4):957–64.
Nagaoka E, Arai H, Tamura K, et al. Prevention of atrial fibrillation with ultra-low dose landiolol after off-pump coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2014;20(2):129–34.
Ogawa S, Okawa Y, Goto Y, et al. Perioperative use of a beta blocker in coronary artery bypass grafting. Asian Cardiovasc Thorac Ann. 2013;21(3):265–9.
Fujii M, Bessho R, Ochi M, et al. Effect of postoperative landiolol administration for atrial fibrillation after off pump coronary artery bypass surgery. J Cardiovasc Surg. 2012;53(3):369–74.
Sezai A, Minami K, Nakai T, et al. Landiolol hydrochloride for prevention of atrial fibrillation after coronary artery bypass grafting: new evidence from the PASCAL trial. J Thorac Cardiovasc Surg. 2011;141(6):1478–87.
Sezai A, Nakai T, Hata M, et al. Feasibility of landiolol and bisoprolol for prevention of atrial fibrillation after coronary artery bypass grafting: a pilot study. J Thorac Cardiovasc Surg. 2012;144(5):1241–8.
Sakaguchi M, Sasaki Y, Hirai H, et al. Efficacy of landiolol hydrochloride for prevention of atrial fibrillation after heart valve surgery. Int Heart J. 2012;53(6):359–63.
Tamura T, Yatabe T, Yokoyama M. Prevention of atrial fibrillation after cardiac surgery using low-dose landiolol: a systematic review and meta-analysis. J Clin Anesth. 2017;42:1–6.
Ji T, Feng C, Sun L, et al. Are beta-blockers effective for preventing post-coronary artery bypass grafting atrial fibrillation? Direct and network meta-analyses. Ir J Med Sci. 2016;185(2):503–11.
Yoshida T, Furukita Y, Yamamoto Y, et al. A randomized, open label study of the efficacy of prophylactic 24-h low-dose landiolol for atrial fibrillation in transthoracic esophagectomy. Esophagus. 2017;14(1):97–103.
Ojima T, Nakamori M, Nakamura M, et al. Randomized clinical trial of landiolol hydrochloride for the prevention of atrial fibrillation and postoperative complications after oesophagectomy for cancer. Br J Surg. 2017;104(8):1003–9.
Horikoshi Y, Goyagi T, Kudo R, et al. The suppressive effects of landiolol administration on the occurrence of postoperative atrial fibrillation and tachycardia, and plasma IL-6 elevation in patients undergoing esophageal surgery: a randomized controlled clinical trial. J Clin Anesth. 2017;38:111–6.
Yagi K, Usuda J, Sakamoto A. Perioperative landiolol infusion reduces the incidence of atrial fibrillation after pulmonary lobectomy: postoperative randomized controlled study. Open J Anesthesiol. 2016;6:119–23.
Suzuki K, Numaguchi A, Adachi YU, et al. Continuous administration of landiolol reduced QT dispersion in postoperative patients. J Clin Anesth. 2014;26(6):438–42.
Kiyokuni M, Konishi M, Sakamaki K, et al. Beneficial effect of early infusion of landiolol, a very short-acting beta-1 adrenergic receptor blocker, on reperfusion status in acute myocardial infarction. Int J Cardiol. 2016;221:321–6.
Park H, Otani H, Noda T, et al. Intracoronary followed by intravenous administration of the short-acting β-blocker landiolol prevents myocardial injury in the face of elective percutaneous coronary intervention. Int J Cardiol. 2013;167(4):1547–51.
Hanada K, Higuma T, Nishizaki F, et al. Randomized study on the efficacy and safety of landiolol, an ultra-short-acting β1-adrenergic blocker, in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J. 2012;76(2):439–45.
Hoshi T, Sato A, Nishina H, et al. Acute hemodynamic effects of landiolol, an ultra-short-acting beta-blocker, in patients with acute coronary syndrome: preliminary study. J Cardiol. 2012;60(4):252–6.
Kawaguchi M, Kawaraguchi Y, Yamamoto Y, et al. Effects of landiolol on systemic and cerebral hemodynamics and recovery from anesthesia in patients undergoing craniotomy. J Anesth. 2010;24(4):503–10.
Miyazaki M, Kadoi Y, Takashi S, et al. Comparative effects of propofol, landiolol, and nicardipine on hemodynamic and bispectral index responses to endotracheal intubation: a prospective, randomized, double-blinded study. J Clin Anesth. 2008;24(4):257–62.
Kawaguchi M, Takamatsu I, Masui K, et al. Effect of landiolol on bispectral index and spectral entropy responses to tracheal intubation during propofol anaesthesia. Br J Anaesth. 2008;101(2):273–8.
Goyagi T, Tanaka M, Nishikawa T. Landiolol attenuates the cardiovascular response to tracheal intubation. J Anesth. 2005;19(4):282–6.
Oda Y, Nishikawa K, Hase I, et al. The short-acting β1-adrenoceptor antagonists esmolol and landiolol suppress the bispectral index response to tracheal intubation during sevoflurane anesthesia. Anesth Analg. 2005;100(3):733–7.
Wajima Z, Shiga T, Imanaga K, et al. Prophylactic continuous administration of landiolol, a novel β1 blocker, blunts hyperdynamic responses during electroconvulsive therapy without altering seizure activity. Int J Psychiatry Clin Pract. 2010;14(2):132–6.
Kitamura A, Sakamoto A, Inoue T, et al. Efficacy of an ultrashort-acting β-adrenoceptor blocker (ONO-1101) in attenuating cardiovascular responses to endotracheal intubation. Eur J Clin Pharmacol. 1997;51(6):467–71.
Inoue S, Tanaka Y, Kawaguchi M, et al. The efficacy of landiolol for suppressing the hyperdynamic response following laryngoscopy and tracheal intubation: a systematic review. Anaesth Intensive Care. 2009;37(6):893–902.
Kaneko M, Yamaguchi S, Hamaguchi S, et al. Effects of landiolol on QT interval and QT dispersion during induction of anesthesia using computerized measurement. J Clin Anesth. 2009;21(8):555–61.
Yang X, Li S. Analysis of esmolol and landiolol on elderly patients in the perioperative period with gastric surgery. Int J Clin Exp Pathol. 2016;9(12):12755–60.
Tochikubo J, Adachi YU, Ejima T, et al. Landiolol reduces hemodynamic responses to bronchoscopy-assisted suctioning in intubated ICU patients. J Intensive Care. 2014;2(6):1–4.
Hirota K, Baba S, Fukushi S, et al. Efficacy of landiolol in attenuating hemodynamic responses to local epinephrine infiltration in patients undergoing vaginal total hysterectomy. J Anesth. 2005;19(1):17–20.
Saito S, Nishihara F, Akihiro T, et al. Landiolol and esmolol prevent tachycardia without altering cerebral blood flow. Can J Anaesth. 2005;52(10):1027–34.
Krumpl G, Ulc I, Trebs M, et al. Bolus application of landiolol and esmolol: comparison of the pharmacokinetic and pharmacodynamic profiles in a healthy Caucasian group. Eur J Clin Pharmacol. 2017;73(4):417–28.
Krumpl G, Ulc I, Trebs M, et al. Pharmacokinetics and -dynamics of low, intermediate and high dose landiolol and esmolol during long term infusion in healthy Caucasians. J Cardiovasc Pharmacol. 2017. https://doi.org/10.1097/FJC.0000000000000554.
Walter E, Schalle K. Cost-effectiveness of landiolol, an ultra-short-acting beta-blocker, for prevention of postoperative atrial fibrillation in Germany [abstract no. PCV84]. Value Heath. 2017;20(9).
Nasrollahi-Shirazi S, Sucic S, Yang Q, et al. A comparison of the β-adrenergic receptor antagonists landiolol and esmolol: receptor selectivity, partial agonism and pharmacochaperoning actions. J Pharmacol Exp Ther. 2016;359(1):73–81.
Ikeshita K, Nishikawa K, Toriyama S, et al. Landiolol has a less potent negative inotropic effect than esmolol in isolated rabbit hearts. J Anesth. 2008;22(4):361–6.
Shibata S, Okamoto Y, Endo S, et al. Direct effects of esmolol and landiolol on cardiac function, coronary vasoactivity, and ventricular electrophysiology in guinea-pig hearts. J Pharmacol Sci. 2012;118(2):255–65.
Sasao J, Tarver SD, Kindscher JD, et al. In rabbits, landiolol, a new ultra-short-acting beta-blocker, exerts a more potent negative chronotropic effect and less effect on blood pressure than esmolol. Can J Anesth. 2001;48(10):985–9.
Krumpl G, Ulc I, Trebs M, et al. Pharmacodynamic and -kinetic behavior of low-, intermediate-, and high-dose landiolol during long-term infusion in Whites. J Cardiovasc Pharmacol. 2017;70(1):42–51.
Krumpl G, Ulc I, Trebs M, et al. Pharmacokinetics and pharmacodynamics of two different landiolol formulations in a healthy Caucasian group. Eur J Pharm Sci. 2016;92:64–73.
Acknowledgments
During the peer review process, the manufacturer of landiolol was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Funding
The preparation of this review was not supported by any external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yahiya Y. Syed is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information about this Adis Drug Review can be found at http://www.medengine.com/Redeem/8F1DF0605D713619.
Additional information
The manuscript was reviewed by: T. Hoshi, Department of Cardiology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan; G. Krumpl, MRN Medical Research Network GmbH, Vienna, Austria; Z. Wajima, Department of Anesthesiology, Tokyo Medical University Hachioji Medical Center, Tokyo, Japan
Rights and permissions
About this article
Cite this article
Syed, Y.Y. Landiolol: A Review in Tachyarrhythmias. Drugs 78, 377–388 (2018). https://doi.org/10.1007/s40265-018-0883-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0883-9