Abstract
As kidney disease progresses, phosphorus retention also increases, and phosphate binders are used to treat hyperphosphatemia. Clinicians prescribe phosphate binders thinking that reducing total body burden of phosphorus may decrease risks of mineral and bone disorder, fractures, cardiovascular disease, progression of kidney disease, and mortality. Recent meta-analyses suggest that sevelamer use results in lower mortality than use of calcium-containing phosphate binders. However, studies included in meta-analyses show significant heterogeneity, and exclusion or inclusion of specific studies alters results. Since no long-term studies have been conducted to determine whether treatment with any phosphate binder is better than placebo on any hard clinical endpoint (including mortality), it is unclear whether possible benefit with sevelamer represents net benefit of sevelamer, net harm with calcium-containing phosphate binders, or both. Although one meta-analysis suggested that calcium acetate may be more efficacious gram for gram than calcium carbonate as a binder, calcium acetate did not reduce hypercalcemia, and gastrointestinal intolerance was higher. Data are insufficient to determine whether calcium acetate provides lower risk of vascular calcification than calcium carbonate. Fears of lanthanum accumulation in the central nervous system or bone with long-term treatment do not appear to be warranted. Newer iron-containing phosphate binders have potential benefits, such as lower pill burden (sucroferric oxyhydroxide) and improved iron parameters (ferric citrate). The biggest challenge to phosphate binder efficacy is non-adherence. This article reviews the current knowledge regarding safety, effectiveness, and adherence with currently marketed phosphate binders and those in development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Phosphate binders have been approved in many countries specifically for treatment of hyperphosphatemia. They are commonly used in dialysis patients and late-stage non-dialysis-dependent chronic kidney disease patients with the hope of positive effects on important clinical outcomes, despite lack of solid evidence from placebo-controlled trials. |
Since some evidence suggests that sevelamer products may have survival benefits over calcium-containing phosphate binders, many clinicians prescribe sevelamer products versus calcium-containing phosphate binders, in the absence of conclusive evidence of harms versus benefits of these agents compared with placebo or with each other. |
Phosphate binders, especially newer ones, represent a significant cost burden on national health care budgets. In the US alone, for example, phosphate binders contribute almost 1 billion dollars per year to Medicare Part D expenditures for dialysis patients. |
It is imperative that well-designed, long-term, placebo-controlled, randomized comparative trials evaluating hard clinical endpoints be conducted with commonly used phosphate binders. |
1 Introduction
Phosphorus balance is a key component of mineral and bone homeostasis and is altered in patients with chronic kidney disease (CKD). Phosphorus is essential for metabolic and enzymatic functions throughout the body, including adenosine triphosphate generation. Excess phosphorus is associated with increased vascular calcification and poor cardiovascular (CV) outcomes [1]. Hyperphosphatemia is a common complication of CKD and progressively worsens as kidney function declines [2]. Among patients with end-stage renal disease (ESRD), 37 and 42% of hemodialysis and peritoneal dialysis patients, respectively, had serum phosphorus concentrations above 5.5 mg/dL based on US data from December 2014 [3].
In the general population, elevated serum phosphorus concentration has been correlated with atherosclerosis, vascular calcification, CV events, and increased mortality [4,5,6,7,8]. The putative relationship between CV events and elevated serum phosphorus concentrations serves as a basis for treating hyperphosphatemia in CKD, where phosphorus accumulation is substantial. Observational or cohort studies in non-dialysis-dependent (NDD)-CKD, kidney transplant, or dialysis patients demonstrate that hyperphosphatemia is a risk factor for CV disease/events [1, 9,10,11,12]; however, recent evidence suggests gender differences with regard to risk [13]. Several studies in the general population have shown differences in risk associated with hyperphosphatemia by gender; the relationship between phosphorus and CV risk factors, morbidity, and mortality appears to be consistent in studies of men but not women in the general population [14,15,16]. Additional research on the gender differences in clinical outcomes associated with hyperphosphatemia in CKD is warranted.
Most [1, 10, 12, 17,18,19,20,21], but not all [22], observational or cohort studies also show that increased levels of phosphorus in CKD patients (NDD-CKD, dialysis, transplant) are associated with increased all-cause mortality or a composite endpoint of all-cause mortality and ESRD. In the dialysis or NDD-CKD populations, no prospective randomized trial evaluating effects of varying phosphorus concentration targets on clinical outcomes has been conducted. Prospective comparative trials of phosphate binders in dialysis patients have been conducted for various clinical outcomes, but results from single studies have been conflicting and have not clearly identified superior agents. Results from these trials have been combined in several recent systematic reviews and meta-analyses and will be evaluated in this review.
Results from a randomized placebo controlled trial (RCT) in stage 3b–4 NDD-CKD normophosphatemic patients showed that treatment with three phosphate binders (lanthanum carbonate, sevelamer carbonate, or calcium acetate) reduced serum phosphorus and urinary phosphate excretion compared with placebo, but coronary and aortic calcification increased in the active treatment group with no progression in the placebo group [23]. A subgroup analysis showed that calcification was associated with calcium acetate treatment, but neither lanthanum nor sevelamer was superior to placebo for this endpoint. A randomized placebo cross-over study in eight stage 3–4 NDD-CKD normophosphatemic patients on a controlled phosphorus diet with or without calcium carbonate supplementation showed that calcium carbonate produced a positive calcium balance while not affecting phosphorus balance or serum phosphorus concentrations. In addition, calcium kinetic data suggested soft-tissue deposition of calcium [24]. This study supported data from an earlier study [25]. Thus, available evidence from single studies is not definitive regarding whether any phosphate binder positively affects any hard clinical outcome aside from lowering phosphorus concentrations, and there is some evidence of harm with calcium-containing phosphate binder (CCPB) treatment in NDD-CKD patients.
The current standard of care is to treat hyperphosphatemia in dialysis patients and later stages of NDD-CKD using a combination of non-pharmacologic, dialytic, and pharmacologic interventions [2].
1.1 Non-pharmacologic and Dialytic Approaches
Non-pharmacologic approaches to managing hyperphosphatemia are often the first-line interventions for patients with CKD. Identifying and limiting exogenous sources of phosphorus may be effective in controlling hyperphosphatemia in some patients and enhance phosphorus control among patients requiring phosphate-binding medications. Phosphorus is found in high concentrations in certain foods or beverages (e.g., colas, dairy products, meats, etc.); intake of these foods should be generally limited in patients with hyperphosphatemia. “Hidden” phosphate may make limiting phosphorus intake difficult for some patients, as phosphorus is a common additive in processed foods and may also be found in medication excipients [26]. While food additives can substantially increase phosphorus content, medication additives containing phosphorus are generally not considered of great importance to overall phosphorus intake [26, 27]. However, this warrants further study as few data describe the clinical impact of phosphorus content in medication products [26, 28].
Phosphorus is removed during dialysis, which contributes to overall phosphorus balance among ESRD patients. During hemodialysis, the serum phosphorus concentration drops within the first 1–2 h, then remains nearly constant throughout the remainder of the session. Phosphorus continues to be removed throughout treatment, but also continues to move from the intracellular compartment into the vascular compartment [29]. Phosphorus removal during hemodialysis averages 800–1000 mg per treatment, but significant inter-patient variation may occur even with patients of similar weights or dialysis prescriptions [30]. This variability may reflect differences in rates of phosphorus moving from the intracellular to the vascular space, where it can be removed by dialysis. Differences in pre-dialysis serum phosphorus concentrations may also affect total dialytic removal; the higher the concentration in the serum, the more is available for removal during hemodialysis. Therefore, for patients who maintain lower serum phosphorus, much less than 800 mg of phosphate may be removed during hemodialysis. Finally, the hemodialysis prescription affects phosphorus removal. For example, increasing dialysis membrane surface area and frequency of hemodialysis sessions may lead to larger total phosphorus removal than increasing treatment duration. Peritoneal dialysis also contributes to phosphorus removal. However, prediction of phosphorus transport is difficult. A recent study of 87 patients on peritoneal dialysis showed that peritoneal creatinine transporter status and creatinine clearance were poor predictors of peritoneal phosphorus transport. Investigators also found that patients using continuous ambulatory peritoneal dialysis, compared with automated intermittent peritoneal dialysis, had greater peritoneal phosphate clearance [31].
1.2 Phosphate Binders
Phosphate binders have remained the predominant pharmacologic intervention for phosphorus control since the 1970s, when aluminum-based phosphate binders were used [32]. Currently, a range of phosphate-binding medications are available in a variety of dosage forms, including aluminum salts, CCPBs, sevelamer hydrochloride (Renagel®, Sanofi; available in generic form in some countries), sevelamer carbonate (Renvela®, Sanofi; available in generic form in some countries), lanthanum carbonate (Fosrenol®, Shire) and new iron-containing phosphate binders (ICPBs). All are effective at lowering serum phosphorus in ESRD patients, but key clinical outcomes including CV mortality, CV events, and/or hospitalizations may differ. Although phosphate binders are used in patients with high CV risk, the effect of phosphate binders on CV events has not been a primary endpoint in clinical trials. In the USA, phosphate binders are approved following phase III trials focusing on phosphate lowering, with no information on hard clinical outcomes in CKD. This is in contrast to medications to treat diabetes, for example, for which the Food and Drug Administration (FDA) has required large clinical trials to assess major adverse cardiac event risk for all new diabetes medications approved since 2008 [33]. This requirement was in response to data suggesting increased risk of CV events with rosiglitazone, despite its efficacy in glucose lowering. Such studies are not required for phosphate-binding medications, despite the high CV risk of the patient population in which these drugs are used.
Phosphate binders are recommended by the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines to treat hyperphosphatemia in patients with NDD-CKD stages 3 through 5 and stage 5 on dialysis [2]. While these medications are approved for use in patients with ESRD, not all are approved for use in NDD-CKD patients. In the USA, no phosphate binder is FDA-approved for use in NDD-CKD patients. However, based on increasing surrogate outcomes data suggesting the possibility of harm with calcium-based binders, draft KDIGO CKD mineral and bone disorder (MBD) guidelines suggest restricting CCPB doses [34].
2 Phosphate Binder Safety
2.1 Timeline of Phosphate Binder Safety Concerns Driving New Therapies
A relative timeline of safety concerns from marketed phosphate binders is depicted in Fig. 1. Safety evidence with phosphate binders is covered in current KDIGO CKD-MBD clinical practice guidelines [35] and new draft guidelines to be released in 2017 [34]. The main issues and findings from these guidelines are summarized here. Although aluminum-containing phosphate binders are highly effective at binding phosphorus, aluminum exposure has been linked to central nervous system toxicity, microcytic anemia, and osteomalcia in dialysis patients. Use should be restricted to the short term (days) and to situations in which high phosphorus levels must be reduced quickly. Magnesium-containing phosphate binders have dose-limiting adverse effects (diarrhea and hypermagnesemia), and are little used. The main concern with CCPBs is increased body load of calcium, increasing risks of hypercalcemia and vascular, aortic, and soft tissue calcification. Sevelamer hydrochloride has been shown to increase risk of metabolic acidosis, but availability of sevelamer carbonate, which has similar efficacy, has alleviated this problem. Accumulation of lanthanum in bones and the central nervous system has been a primary reason clinicians have been more reluctant to prescribe it, but a study evaluating cognitive function showed similar decline in lanthanum users compared to standard of care recipients [36]. Several lines of evidence suggest that long-term lanthanum use does not result in aluminum-like bone disease. There is little information on long-term adverse effects of new ICPBs. One concern with ferric citrate is that the citrate can increase gastrointestinal aluminum absorption; this may be moot if use of aluminum-based phosphate binders is restricted.
Evidence regarding safety effects has been generated from RCTs comparing placebo with active drug, and randomized comparative studies between two phosphate binders or classes. Several recent systematic reviews and meta-analyses, including network meta-analyses, give new insight into comparative safety across phosphate binder classes or specific agents.
2.2 Comparative Safety (Systematic Reviews and Meta-analysis)
Four separate groups published systematic reviews with meta-analyses in 2015 and 2016 comparing the safety of various phosphate binders in dialysis and NDD-CKD patients [37,38,39,40]. Importantly, side effects may be under-reported in clinical trials (and thus in meta-analyses combining results from clinical trials) because most trials employ exclusions that result in select populations. For more information, see Sect. 5.1. In addition, some information in this section and in Sect. 3.3 comes from two network meta-analyses by two research groups [37, 41]. Network meta-analysis differs from conventional pair-wise meta-analysis in which two or more RCTs comparing the same two interventions are grouped together for analysis. Network meta-analysis compares multiple treatments (three or more) using direct comparisons of interventions within RCTs and indirect comparisons across RCTs based on a common comparator. The risk of bias from poor design and execution of clinical trials can be magnified through network meta-analysis, as bias in the effect estimate from any single RCT may affect several pooled effect estimates within a network, in contrast to affecting a single effect estimate, as in conventional meta-analyses [42]. These caveats must be considered when interpreting the results below.
2.2.1 Hypercalcemia
Increased hypercalcemic risk occurred with CCPBs compared with sevelamer products [38, 39] and lanthanum carbonate [39]. Despite a finding that phosphorus reduction was greater with calcium acetate than with carbonate, there was no difference between the two CCPBs in calcium levels or hypercalcemia episodes at 4 or 8 weeks [40].
2.2.2 Gastrointestinal Events
In a comparison of multiple phosphate binder classes in a network meta-analysis, sevelamer ranked highest for constipation, lanthanum increased nausea compared with ICPBs or CCPBs, and ICPBs increased diarrhea compared with CCPBs [37]. In two conventional meta-analyses comparing sevelamer with CCPBs, combined gastrointestinal adverse events (nausea, vomiting, diarrhea, abdominal bloating) trended higher with sevelamer, but results were not statistically significant [38, 39]. In other conventional meta-analyses, combined gastrointestinal adverse events [39] and vomiting [43] were higher with lanthanum versus CCPBs [39]. A meta-analysis comparing calcium carbonate with calcium acetate showed a higher risk of intolerance with calcium acetate (more patients dropped out of the calcium acetate groups) and a trend toward more gastrointestinal effects with calcium acetate [40].
3 Incremental Progress in Effectiveness
3.1 Should We Expect More than Phosphorus-Lowering Effect?
In retrospective studies, higher serum phosphorus levels in people with normal or near normal kidney function have been associated with CV events [8], and with increased mortality and higher likelihood of ESRD or CKD progression in CKD patients [12, 44, 45]. Nephrology practitioners prescribe phosphate binders primarily in dialysis patients to lower phosphorus, thinking that positive benefits will result. Various phosphate binders have been approved by regulatory bodies in the USA, Europe, Canada, and other countries for the indication of hyperphosphatemia. A recent network meta-analysis showed that all phosphate binders but colestilan significantly lowered serum phosphorus levels compared with placebo [37]. Results also showed that ICPBs (iron magnesium hydroxycarbonate, ferric citrate, SBR759, sucroferric oxyhydroxide) increased the odds of attaining phosphorus targets compared with CCPBs, sevelamer, and lanthanum [37]. In contrast, Habbous et al. showed similar phosphorus levels with ICPBs and other phosphate binder groups [39]. Phosphate-lowering abilities between agents are difficult to evaluate using meta-analyses since target phosphate levels, dosing, and adherence may vary between studies. However, Wang et al. found that phosphorus lowering was greater with calcium acetate than with calcium carbonate, despite the elemental calcium dose being equal or higher in the calcium carbonate group [40]. See Sect. 5.3 for information on phosphate binder equivalency compiled from single studies.
The questions are whether lowering phosphorus with phosphate binders in CKD patients (dialysis and NDD-CKD) prevents adverse outcomes such as fractures, death, or CV events, and if so, are specific phosphate binders more effective than others. These are important questions, as about $1 billion was spent on prescription phosphate binders in Medicare-covered dialysis patients in the USA in 2014 [3, 46]. Sevelamer carbonate (Renvela®, Sanofi) was listed as one of the top 10 drugs in the US contributing to explosive growth in Medicare Part D expenditures in 2010–2015 during the catastrophic coverage phase [47] of that program.
3.2 Phosphate Binder Effects in Chronic Kidney Disease (CKD) Compared with Standard Care, No Treatment, or Placebo (Meta-Analyses and Observational Studies)
Two comprehensive network meta-analyses compared effects on mortality with standard care (phosphate-lowering diet), no treatment, or placebo versus CCPBs [calcium acetate, carbonate, citrate (Sekercioglu et al. only)], sevelamer (hydrochloride, carbonate), ICPBs [ferric citrate, sucroferric oxyhyrdroxide, iron magnesium hydroxycarbonate (Palmer et al. only), SBR759 (Palmer et al. only)], colestilan (Palmer et al. only), and some combinations [37, 41]. Data were insufficient to evaluate magnesium carbonate, bixalomer, or nicotinic acid. Findings showed no evidence that any drug class lowered all-cause mortality compared with placebo or standard care; however, the quality of evidence was judged to be low [41]. In addition, these trials were of short duration (1–3 months), so were likely insufficient to evaluate mortality effect. These results are supported by results from a large observational study of the Cleveland Clinic CKD registry, which showed that any phosphate binder use in NDD-CKD stage 3–4 patients was not significantly associated with mortality in adjusted analyses or in a propensity-score matched cohort of patients treated for longer than 6 months [48], and results from a smaller study of incident dialysis patients that evaluated only CCPBs versus no treatment [49]. However, other observational studies have shown increased survival of incident hemodialysis patients [50] and male NDD-CKD veterans who received any phosphate binder versus those who did not [51]. The short-term nature of clinical trials and conflicting results from observational studies demonstrate the need for a well-designed, adequately powered, longer-term RCT to evaluate whether commonly used phosphate binders versus placebo in NDD-CKD and dialysis patients reduces hard outcomes such as fractures, CV events, mortality, or hospitalizations.
3.3 Comparative Effectiveness of Phosphate Binders (Meta-Analyses)
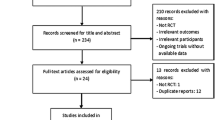
Five separate research groups published systematic reviews with meta-analyses in 2015 and 2016 comparing the effectiveness of various phosphate binders in dialysis and NDD-CKD patients and evaluating numerous outcomes [37,38,39,40,41]. All included RCTs and some included quasi-RCTs. Tables 1 and 2 provide a description and key results from these meta-analyses and selected others published before 2015. Results from the most recent studies (2015/2016) are reviewed below as earlier meta-analyses did not include recent RCTs. Results from recent meta-analyses were not always congruent and potential explanations are provided below along with key results for selected outcomes.
3.3.1 Mortality
Several recent meta-analyses have compared various phosphate binders and effect on all-cause mortality. Three meta-analyses showed lower mortality rates in patients receiving sevelamer than in those receiving CCPBs [37, 38, 41]. Habbous et al. found a nonsignificant trend toward lower mortality with sevelamer [39]. The meta-analyses included different numbers of trials (8–29). Habbous et al. included the most trials, as they had no explicit criteria regarding study duration and used imputation and digitalization of graphs when numerical data were unavailable. Due to the former approach, they included several very short-duration trials with few or no events (i.e., no deaths in either study group), with the justification that exclusion of such studies may overestimate treatment effects. Simulation studies support this approach only when treatment effects are judged a priori to be unlikely [52]. There was moderate to high heterogeneity between the studies evaluated for the mortality endpoint when calcium products (carbonate, acetate) were grouped together [37,38,39, 41], but low heterogeneity when calcium carbonate or calcium acetate were separately compared with sevelamer [38, 39]. When calcium carbonate trials were separated from calcium acetate trials, sevelamer showed a mortality benefit compared with calcium carbonate, but not with calcium acetate [38, 39]. In sensitivity analyses with studies comparing sevelamer with CCPBs, Habbous et al. removed the Dialysis Clinical Outcomes Revisited (DCOR) trial [53] because patient attrition in that large study was high; they then observed a significant mortality benefit with sevelamer versus all CCPBs [39]. Importantly, a significant number of patients crossed over to the alternative treatment in this open-label trial, attenuating differences between sevelamer and calcium groups. In contrast, in another sensitivity analysis, Palmer et al. removed the INDEPENDENT study [54], which showed a much larger benefit of sevelamer versus CCPBs than other studies. Once this study was excluded, study heterogeneity changed from moderate–high to low, and sevelamer no longer showed a significant positive mortality effect compared with CCPBs. Overall, data from these meta-analyses suggest that sevelamer products reduce mortality in CKD patients compared with CCPBs, but statistical significance lost or gained by removing a single clinical trial is concerning. Mortality benefits of one phosphate binder versus another would be expected to appear only longer term. All of these meta-analyses included short- and longer-duration trials; the Habbous et al. meta-analysis [39] in particular included many more short-term trials with low or no events, likely explaining a non-significant trend toward fewer deaths with sevelamer versus CCPBs.
Results from three of four meta-analyses [37, 38, 41] are supported by a comparative effectiveness observational study, which showed that treatment with sevelamer was associated with a 6% lower risk of death compared with calcium acetate in 35,251 incident US hemodialysis patients, using propensity-score matched cohorts [55]. They used linked data from the United States Renal Data System (USRDS) and Medicare Part D; the main limitation was that laboratory data were not included, so it is unclear whether baseline phosphorus and calcium levels were similar in both cohorts. Strengths are the large numbers and data representing real-world use rather than RCT conditions where medication adherence may be better. The effect size in this study was modest and translated to approximately 44 patients needed to treat at 2 years [56] to prevent one death. However, since no phosphate binder type has been demonstrated to reduce mortality compared with no treatment/standard care/placebo in clinical trials, none of these studies can determine whether the lower mortality rate with sevelamer compared with CCPBs represents a superior sevelamer effect or harm from CCPBs or both.
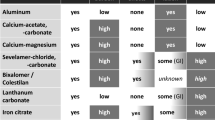
No other phosphate binder types were shown to be superior with regard to mortality endpoints in these meta-analyses. Figure 2 shows results of a pair-wise comparison from Palmer et al.’s network meta-analysis [37]. However, fewer trials compared lanthanum-, iron-, and magnesium-based binders to CCPB or sevelamer products.

Reprinted with permission under the terms of the Creative Commons Attribution-Non-Commercial-No Derivatives License (CC By ND ND); http://creativecommons.org/licenses/by-nc-nd/4.0. Figure citation is Palmer et al. [37]
Network estimated odds (ORs) of phosphate binders on all-cause mortality. Values are given as OR (95% CI). The table should be read from left to right. Risk estimate is for the column-defining treatment compared to the row-defining treatment. An OR of <1 indicates the column treatment is associated with a lower odds of mortality than the row treatment. For example, sevelamer treatment lowers the odds of all-cause mortality compared to calcium treatment (OR 0.39, 95% CI 0.21–0.74). Bolded numerals indicate statistically significant results. The heterogeneity tau (τ) for the network analysis was 0.74 (indicative of moderate-high heterogeneity). There were 20 studies involving 6376 participants included in the network. OR odds ratio, CI confidence interval.
3.3.2 Cardiovascular Mortality and Vascular Calcification
The main hypothesized putative mechanisms for improved survival with sevelamer versus calcium are reduced progressive vascular and coronary artery calcification (CAC). Six of nine studies found that CCPBs produced more severe and/or rapid CAC increases than sevelamer [38]. Although two meta-analyses also showed a significant CAC reduction with sevelamer versus CCPBs [37, 39], no meta-analysis has shown that CV mortality is significantly reduced [37,38,39]. This is unsurprising given the heterogeneity between studies. In addition, the power to detect differences is less for CV mortality than for all-cause mortality.
A large open-label Japanese RCT is in progress comparing lanthanum carbonate and calcium carbonate regarding survival time free of CV events, which may clarify the relative CV effects of this non-CCPB [57].
3.3.3 Hospitalization
In meta-analyses evaluating hospitalization, calcium was significantly associated with increased hospitalizations versus sevelamer [39], but not versus non-CCPBs [41]. St. Peter et al. conducted a secondary analysis of DCOR trial data, the largest long-term RCT to date comparing sevelamer with CCPBs. They linked DCOR clinical data with USRDS registry data to obtain more hospitalization data than were collected through case report forms, as many patients terminated the study early and were lost to follow-up [58, 59]. In an intent-to-treat analysis, they found that sevelamer versus CCPBs was associated with an 11% reduction in multiple hospitalizations (p = 0.02) and a 12% reduction in hospital days (p = 0.03) in a mean of 2.1 years of follow-up.
3.3.4 Interpretation of Comparative Effectiveness Literature
Interpretation of findings from meta-analyses must be tempered by the limitations of the underlying studies. Many studies providing data for meta-analyses had several limitations (Table 1), including inadequate blinding and duration too short to allow assessment of several outcomes. These meta-analyses included short- and longer-duration trials, and they had different criteria for including trials. For instance, the Habbous et al. meta-analysis [39] included many more short-term trials with low or no events, likely explaining a non-significant trend toward fewer deaths with sevelamer versus CCPBs. There was often significant heterogeneity between studies, particularly for meta-analyses evaluating mortality as an outcome. Sensitivity analyses from two meta-analyses showed that statistical significance for mortality effects could be lost or gained by removing a single clinical trial. Results from meta-analyses are only as good as the clinical trials that underlie them, and the overall quality of clinical trials in the phosphate binder space is not great. Meta-analysis cannot make up for poorly designed trials or trials carried out with inadequate study duration or power to assess hard clinical endpoints.
4 Potential Value-Added Therapy: Iron-Containing Phosphate Binders
As ICPBs are relatively new to the market, too few data are available to evaluate them in meta-analyses for hard clinical endpoints. Anemia is a ubiquitous complication of CKD, and it affects most patients with ESRD requiring dialysis. Treatment includes both erythropoiesis-stimulating agents (ESAs) and intravenous (IV) iron. While ESAs have led to decreased need for blood transfusions in CKD patients, multiple RCTs have demonstrated that ESA treatment targeted to normal hemoglobin levels (13–15 g/dL) increases risks of death, CV complications, and stroke in CKD [60,61,62]. Additional concerns relate to increased use of IV iron, including the potential risk of infection and limited information regarding long-term safety. Novel strategies to reduce ESA and IV iron use may therefore improve clinical outcomes in dialysis patients. Recently, two iron-based phosphate binders, sucroferric oxyhydroxide and ferric citrate, became available in clinical practice and may provide an approach that simultaneously addresses hyperphosphatemia and anemia.
4.1 Sucroferric Oxyhydroxide
Sucroferric oxyhydroxide (Velphoro®, Vifor Fresenius Medical Care Renal Pharma) was approved by the US FDA in November 2013 and by the European Medicines Agency (EMA) in August 2014, with indications only in dialysis patients. In a phase III trial including 1059 hemodialysis patients randomly assigned to sucroferric oxyhydroxide or sevelamer carbonate, effects on serum phosphate were similar [63]. There was no significant difference between treatment groups in serum ferritin (a measure of storage iron) at 24 weeks, but there was a modest, significant effect of sucroferric oxyhydroxide on transferrin saturation (+4.0% points) [64]. This effect was concentrated in patients with low serum ferritin (<310 ng/mL) at baseline. There were also modest reductions with sucroferric oxyhydroxide in percentages of patients receiving IV iron and ESAs. Results from the extension study (28 additional weeks) indicated no differential effects on serum phosphate, intact parathyroid hormone, or calcium [65]. Effects of sucroferric oxyhydroxide on serum ferritin, transferrin saturation, and hemoglobin were also non-significant. This study demonstrated that iron absorption is not significant with this product.
Phase II and III studies in Japanese hemodialysis patients have shown that sucroferric oxyhydroxide reduced serum phosphate in a dose-dependent manner, with decreases of 1.8, 2.7, 3.2, and 3.8 mg/dL with dosages of 750, 1500, 2250, and 3000 mg/day, respectively [66]. Relative to dosages of 750 or 1500 mg/day, dosages of 2250 or 3000 mg/day more strongly increased calcium and decreased intact parathyroid hormone. However, no dose-dependent effects of sucroferric oxyhydroxide on anemia parameters have been observed. Relative to sevelamer hydrochloride, sucroferric oxyhydroxide significantly increased the percentage of patients with serum phosphate in the target range (82.0 vs. 67.4%) with decreased pill burden (5.6 vs. 18.7 tablets/day) [67].
4.2 Ferric Citrate
Ferric citrate (Auryxia®, Keryx Biopharmaceuticals) was approved by the US FDA in September 2014 and by the EMA in September 2015. Indications in the USA are only for dialysis patients, whereas indications in Europe are for dialysis and NDD-CKD patients. Among 151 hemodialysis patients in a phase II study, ferric citrate reduced serum phosphate in a dose-dependent manner, with little reduction at one tablet/day and significantly larger reductions at six to eight tablets/day [68]. In a phase III trial of 441 hemodialysis patients randomly assigned to ferric citrate or placebo control for 4 weeks and active control with calcium acetate and/or sevelamer carbonate for 52 weeks, ferric citrate versus placebo control significantly reduced serum phosphate, but ferric citrate versus active control had no effect on serum phosphate [69]. Relative to active control, ferric citrate significantly increased transferrin saturation (+9.5%), serum ferritin concentration (+282 ng/mL), and hemoglobin (+0.33 g/dL). Moreover, ferric citrate decreased IV iron use by 12.5 mg/week and ESA use by 1191 IU/week [70]. At the end of the trial, 3.9% of patients with ferric citrate and 14.1% with active control were receiving more than 70 mg/week of IV iron.
Interestingly, during the active control phase, 34.6% of ferric citrate users were hospitalized at least once, whereas 45.6% of active control users were hospitalized at least once (risk reduction, 24.2%) [71]. Hospitalization rates were 0.63 admissions per patient-year with ferric citrate and 0.83 admissions per patient-year with active control, although this difference was nominally non-significant (p = 0.08).
In Asia, ferric citrate hydrate (Riona®, Torii Pharmaceutical Company) has been compared with sevelamer hydrochloride in several studies. In a trial of 230 Japanese hemodialysis patients, ferric citrate hydrate versus sevelamer hydrochloride had no significant effect on serum phosphorus, a small positive effect on calcium, and no effect on intact parathyroid hormone. However, ferric citrate hydrate significantly increased serum ferritin, transferrin saturation, and hemoglobin [72]. Conversion of 27 Taiwanese hemodialysis patients from sevelamer hydrochloride to ferric citrate hydrate significantly decreased serum intact FGF23 and increased serum intact parathyroid hormone after 12 weeks [73]. Finally, ferric citrate hydrate also appeared to effectively lower serum phosphorus in peritoneal dialysis patients [74].
Both ferric citrate and ferric citrate hydrate have been studied in NDD-CKD patients. In an RCT including 149 NDD-CKD patients [estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2], ferric citrate decreased serum phosphorus, increased transferrin saturation, and increased hemoglobin [75]. In a more recent and larger trial, significantly more NDD-CKD patients on ferric citrate (52%) than on placebo (19%) achieved a 1.0 g/dL or more hemoglobin increase at any time during 16 weeks of follow-up [76]. In a phase III trial of 90 NDD-CKD patients (mean eGFR 9.2 mL/min/1.73 m2) in Japan, ferric citrate hydrate versus placebo reduced serum phosphorus by 1.3 mg/dL [77]. Both ferritin and transferrin saturation increased with ferric citrate hydrate versus placebo, but the effect of ferric citrate hydrate on hemoglobin was not significant.
One potential safety concern with ferric citrate is iron overload. In the phase III trial of ferric citrate in hemodialysis patients, 10.4% of patients on ferric citrate achieved serum ferritin >1500 ng/mL more than once during the trial, compared with 1.3% of patients on active control [78]. One case of hemochromatosis was confirmed by liver biopsy among patients on ferric citrate; this patient did not undergo genetic testing for hereditary hemochromatosis [70]. Furthermore, transferrin saturation of >80% was observed only in patients on ferric citrate, although occurrences were rare [70]. Because of the potential for iron accumulation, the US FDA suggests that ferritin and transferrin saturation levels should be monitored regularly in ferric citrate users.
Another potential safety concern with ferric citrate is citrate itself. Citrate is known to increase absorption of dietary aluminum, possibly leading to tissue accumulation of aluminum in CKD patients, especially those who are anuric [79]. In the phase III trial of ferric citrate in dialysis patients, median serum aluminum increased from 6.0 mcg/L at baseline to 7.0 mcg/L after 52 weeks of ferric citrate, while median serum aluminum was unchanged with active control; the difference was nominally non-significant (p = 0.1), but power was limited by sample size (n = 185) [80].
In summary, sucroferric oxyhydroxide and ferric citrate represent potentially useful ICPBs. Sucroferric oxyhydroxide has limited effects on anemia parameters or IV iron use. Alternatively, ferric citrate appears to exert positive effects on anemia parameters, while lowering concomitant use of IV iron and ESAs. Results regarding ICPBs are limited by a dearth of data in clinical applications outside of protocol-driven trials. Post-market studies of both agents are needed to better understand real-world health and economic effects.
5 Incremental Improvements in Adherence
5.1 Key Reasons for Non-adherence with Phosphate Binders
A recent systematic review noted that non-adherence to phosphate binders ranged from 13.9 to 98.6% with an average of 52.5% [81]. Medication factors significantly associated with non-adherence include total pill burden, knowledge about phosphate binder medicines, total number of phosphate binders prescribed, medication regimen complexity (frequency and dosage schedule), and medication cost. Beliefs about the necessity of phosphate binders, poor tolerance or side effects, and large tablet size were the most common reasons given by patients to explain non-adherence [81].
A large US hemodialysis organization reviewed 30,933 patient records that gave a reason for phosphate binder discontinuation. The most common reasons related to hypophosphatemia and hypercalcemia. The second most common reason was patient inability to tolerate the medication. Lanthanum accounted for 14% of total discontinuations and 40% of discontinuations due to inability to tolerate. Lanthanum was also associated with a higher proportion of discontinuations due to difficulty chewing/swallowing pills (49% lanthanum; 36% sevelamer; 14% calcium acetate) and patients “refusing” (47% lanthanum; 36% sevelamer; 16% calcium acetate) [82]. These results are consistent with a small comparative study of patients switching from sevelamer to lanthanum carbonate, which noted that 31% of patients returned to sevelamer because of dislike of the chewable tablet formulation, despite lanthanum’s significantly lower pill burden (13.9 tablets vs. 7.7 tablets) [83]. A study of 7299 US Medicare hemodialysis patients found that sevelamer patients were significantly more adherent by prescription refills and had fewer gaps in medication possession than calcium acetate patients. Comparison with lanthanum was not performed [84]. The phase III trial of ferric citrate noted more discontinuations in ferric citrate versus active control arm (33 vs. 23%), largely due to gastrointestinal side effects (diarrhea, bloating). In this trial, patients with a previous intolerance to calcium acetate or sevelamer carbonate were excluded, so the discontinuation rate may be higher in real-world use [69]. These studies indicate that adverse effects and insurance coverage should be considered and followed up to aid adherence.
5.2 Patient Preference in Phosphate Binder Selection
Patient phosphate binder preferences were examined in a study of patients currently receiving a combination of two or three phosphate binders or who had been recently switched from high-dose sevelamer to lanthanum carbonate; 54.5% did not like their prescribed phosphate binder. These patients had a significantly greater risk of high phosphate levels, which was linked to non-adherence by a validated patient questionnaire. Calcium acetate was the preferred phosphate binder for 47.1%, lanthanum carbonate for 40%, sevelamer for 20.6%, and aluminum hydroxide for 19.4%. Lanthanum received negative ratings because patients did not like the chewable tablets (17.7%), sevelamer because the tablets were too large (13.2%) and many tablets were required daily (27.2%), and aluminum hydroxide because of gastric intolerance (19.4%) and bad taste (22.2%). Calcium acetate received little patient complaint (<5%). Interestingly, non-adherent patients demonstrated significantly greater knowledge of the use and importance of their phosphate binders, likely because they had received more education on phosphorus from their hemodialysis health care team [85].
5.3 Phosphate Binder Dose Equivalency and Pill Burden
Pill burden differs between phosphate binders depending on phosphate binding efficacy. Table 3 outlines the equivalent doses of each phosphate binder relative to the phosphorus binding capacity of 1 g calcium carbonate. The only agents with a higher binding capacity and, hence, lower pill burden than calcium carbonate are lanthanum and sucroferric oxyhydroxide. However, as noted, lanthanum was associated with a high proportion of discontinuations due to intolerance. Thus, pill burden alone is not enough to ensure adherence; the drug must also be well tolerated with few side effects. Tablet for tablet, sucroferric oxyhydroxide has the highest phosphate binding capacity and the lowest phosphate binder equivalent dose among several phosphate binders, thereby reducing pill burden and increasing the likelihood of achieving target serum phosphorus [86, 87]. However, gastrointestinal side effects, including diarrhea and fecal discoloration, were much more common with sucroferric oxyhydroxide than with sevelamer carbonate in a phase III trial. Importantly, more treatment-emergent adverse events leading to discontinuation occurred with sucroferric oxyhydroxide (15.7%) than with sevelamer carbonate (6.6%). Unfortunately, this significantly lower pill burden (five tablets/day less with sucroferric oxyhydroxide) produced an absolute adherence improvement of only 5.4% compared with sevelamer carbonate over 24 weeks [63].
The binding efficacies in Table 3 should be considered only a general guide, as phosphate removal can vary widely among individual patients [30]. For example, high-dose (4.3-g) calcium acetate was given before a test meal containing 345 mg of phosphate. The observed reduction in phosphate absorption ranged from 97.5 to 234 mg per dose, a 2.4-fold difference between patients [30, 88]. Another little-recognized issue is the possible nonlinear relationship between phosphate binder dose and efficacy [30]. This has been demonstrated for sevelamer; doses exceeding nine tablets per day are associated with significantly decreased phosphate binding per tablet compared with fewer tablets per day. A study of 24 healthy individuals under controlled conditions found that phosphate binding assessed by urinary phosphate excretion was 246 mg with 7.5 g (approximately nine tablets) of sevelamer and 341 mg with 15 g (approximately 18 tablets). Doubling the dose led to only an additional 95 mg of phosphate binding [30, 89]. Thus, even if patients are adherent to very high prescribed doses of phosphate binders, the benefit may be minimal.
5.4 Patient Empowerment in Determining Daily Phosphate Binder Dose
A unique approach to phosphate binder prescription allows for patient empowerment with self-adjustment of phosphate binders based on the phosphorus content of each meal, similar to patients with diabetes adjusting insulin dosing based on carbohydrates. The Phosphate Education Program provides phosphorus units (PU), 1 PU per 100 mg phosphorus, for food groups (e.g., meat, cheese, vegetables, dairy). After estimating the meal PU content (e.g., any meat, 150 g = 3 PU), patients self-adjust their phosphate binder doses according to a prescribed phosphate binder-to-PU ratio. This ratio is adjusted by measuring serum phosphate levels and correcting until phosphate targets are obtained [90]. In a small prospective study of 16 children with NDD-CKD stage 4–5 or receiving hemodialysis or peritoneal dialysis, serum phosphate levels above 1.78 mmol/L (>5.5 mg/dL) decreased from 63 to 31% and the mean daily intake of phosphate binders increased from 6.3 to 8.2 tablets per day with no reduction in dietary phosphate intake. The children were able to give up significantly fewer favorite foods high in phosphate such as meat, fast food, and chocolate [91]. Studies examining the effects of the Phosphate Education Program on adherence in more patients are needed. This approach would not be effective for uncooperative or unmotivated patients.
5.5 Association of Phosphate Binder Adherence with Mortality
Adherence and mortality were examined in a large observational cohort study of elderly incident hemodialysis patients in the USA who were started on calcium acetate or sevelamer hydrochloride or carbonate [55]. Adherence was determined based on prescription record refill records. All-cause mortality rates were significantly lower for adherent calcium acetate and adherent sevelamer patients than for non-adherent patients. These results are unsurprising; many observational studies have shown that outcomes are better for medication-adherent than for non-adherent patients, but some of this has been attributed to a healthy user effect [92]. Despite patients being well-matched for known characteristics, unmeasured characteristics that differ for adherent and non-adherent patients confound the relationship between medication adherence and clinical outcomes. Of more interest was the finding of no survival advantage for adherent sevelamer versus adherent calcium acetate users [55]. If the putative mechanism underlying the advantage of sevelamer over CCPBs is lower vascular and coronary calcification over time, then adherent CCPB users should be increasingly disadvantaged over time with increased cumulative calcium body burden. The limitation of this study was that laboratory values were not available, so patients could not be matched on baseline calcium, phosphorus, or intact parathyroid hormone concentrations, which may have affected findings.
The important relationship between medication non-adherence and CV or mortality outcomes is difficult to determine because most RCTs in dialysis patients do not adequately or consistently report medication adherence. A recent systematic review noted that only five of 21 RCTs examining CV or mortality endpoints in dialysis patients reported medication adherence [93].
6 Incremental Cost-Effectiveness of Phosphate Binders
6.1 Hemodialysis
A recent systematic review examined the cost-effectiveness of phosphate binders in adult hemodialysis patients and concluded that a CCPB, calcium acetate, appeared to be the most cost-effective therapy for first-line use in prevalent patients [incremental cost-effectiveness ratio (ICER) £8197 (US$11,818)/quality-adjusted life year (QALY) gained] [94]. Sevelamer hydrochloride and carbonate and lanthanum carbonate were the only non-CCPBs included. In prevalent patients, their cost-effectiveness was inconsistent between studies, with ICERs from US$26,835 to over US$100,000/QALY gained. In incident patients, CCPBs were cost-effective first line, but second-line lanthanum carbonate offered good value for money in two studies, with ICERs ranging from US$11,461 to US$11,525/QALY gained [94]. The major limitation of these lanthanum studies was that lanthanum effectiveness was based on changes in a surrogate marker, serum phosphorus [95]. The cost-effectiveness of lanthanum needs confirmation by a model based on clinical trials with mortality or other hard clinical endpoints as the primary outcome [95]. Systematic review authors noted that the overall quality of included studies was suboptimal, especially studies funded by pharmaceutical companies, which were the majority (67%). These studies were also significantly more likely to report ICERs favoring the sponsor’s product [94]. Firm conclusions were not possible in the systematic review due to study quality heterogeneity.
The National Institute for Health and Care Excellence (NICE) hyperphosphatemia in CKD cost-effectiveness analysis received a perfect quality assessment score in the aforementioned systematic review [94, 96, 97]. This analysis favored first- and second-line calcium acetate use in prevalent dialysis patients [96]. This cost-effectiveness model found that sevelamer resulted in an ICER of £87,916 (US$107,139)/QALY gained. Lanthanum carbonate accrued marginally greater health gains but at a much higher cost. Lanthanum was “extendedly dominated” so that regardless of the maximum acceptable ICER, better value was achieved by using calcium acetate or sevelamer hydrochloride. The authors also noted that if receiving calcium acetate indefinitely was a clinically appropriate option, switching to a non-CCPB would be hard to justify, as the ICERs for a switch are £38,078 (US$46,403)/QALY gained and £42,683 (US$52,246)/QALY gained for sevelamer hydrochloride and lanthanum carbonate, respectively. Even when a total serum calcium level of 3 mmol/L (12 mg/dL) was used as a switching point, the ICER for sevelamer hydrochloride remained above £30,000 (US$36,721)/QALY gained. The authors noted that it was unlikely that health gains provided by non-CCPBs were sufficient to counterbalance the extra expense unless society’s maximum acceptable ICER threshold is £40,000 (US$48,962)/QALY gained [96].
A cost-effectiveness study of sucroferric oxyhydroxide versus sevelamer carbonate in hemodialysis patients showed that quality-adjusted survival was less with sucroferric oxyhydroxide; the ICER was £22,621 (US$27,689)/QALY gained compared with sevelamer. Future studies are needed, as assumptions regarding mortality and discontinuations due to adverse events were made [98]. Only cost-savings, not cost-effectiveness, models of ferric citrate have been published [71, 99,100,101]. In the context of 2013 Medicare reimbursement rates for phosphate binders, a reduction in hospitalization rates using ferric citrate could save approximately $3000 per patient per year [71]. Based on data from a phase III trial, conversion from active control to ferric citrate reduced annual ESA use by roughly 130,000 IU per patient and annual IV iron use by roughly 2000 mg per patient. Again, in the context of 2013 Medicare reimbursement rates, these reductions could save approximately $2100 per patient per year [100]. A Monte Carlo analysis suggested that total conversion of the US dialysis population from prevailing phosphate binders to ferric citrate could save between $3 and $4 billion per year [99]. However, these models are limited in that no large-scale phase III or IV studies confirm the cost-savings associated with ESAs, IV iron, and reduced hospitalization costs associated with the ferric citrate use [69]. Studies are also needed to confirm the efficacy of ferric citrate in improving anemia in patients with significant or long-standing iron deficiency [69]. The economic consequences of lower utilization with ferric citrate may be substantial, although ferric citrate may be a double-edged sword, as low adherence may result in inadequate control of both hyperphosphatemia and anemia.
In summary, the inconsistent results from these cost-effectiveness studies are due to different patient populations (e.g., prevalent vs. incident), study designs (e.g., Markov model vs. trial-based), source of efficacy (e.g., phosphorus control vs. survival), costs included (e.g., dialysis), different drugs compared, survival assumptions and studies conducted in several countries with different health care system costs [94].
6.2 Non-dialysis-Dependent CKD
Cost-effectiveness studies in NDD-CKD patients have been published [102,103,104,105]. They have numerous limitations including limited efficacy data for this population. Patient-level data in these studies was derived from 107 patients treated with sevelamer [103, 105], 14 [104] to 105 treated with calcium carbonate [103, 105], 14 treated with calcium acetate [104], and 56 treated with lanthanum [102,103,104]. As noted in the NICE hyperphosphatemia guideline update, the evidence for phosphate binders in NDD-CKD patients is insufficient to provide a worthwhile cost-effectiveness model [106]. Current clinical guidelines for NDD-CKD patients no longer recommend specific phosphate targets, as definitive evidence of the benefits of reducing phosphate levels is lacking [34]. However, specific phosphate targets of less than 4.6 mg/dL or less than 5.5 mg/dL were included in these models. Of note, the cost-effectiveness of non-CCPBs in NDD-CKD patients is mainly driven by the assumption that improved phosphate control has a direct effect on delaying the start of dialysis. However, evidence is needed to confirm this assumption [106]. For example, in a study that concluded that first-line sevelamer was cost effective versus calcium carbonate, the results were most sensitive to assumptions regarding the impact of sevelamer on dialysis initiation [103, 107]. Another study concluded that lanthanum carbonate was cost effective as a second-line agent again due to delayed CKD progression and dialysis initiation [102]. However, in this study, CCPBs were less costly and more effective at lowering serum phosphorus even as second-line therapy [107], as only 18.8% of patients with elevated serum phosphorus levels responded to lanthanum and the remaining 81.2% were switched back to CCPBs [102]. All NDD-CKD studies have been funded by pharmaceutical companies, and it has been noted that cost-effectiveness studies sponsored by industry significantly favor the sponsor’s product [94, 108,109,110]. The lack of country-specific data for cost-effectiveness modeling inputs is another limitation. Country-specific practice pattern data and drug cost data are needed as race, health care system, and other patient characteristics vary the results [95, 111].
6.3 Summary for Cost-Effectiveness of Phosphate Binders
Future high-quality, cost-effectiveness evaluations are needed to confirm the findings noted for hemodialysis and NDD-CKD patients. The basis of excellent cost-effectiveness analyses is results from well-designed, high-quality, placebo-controlled, comparative clinical trials evaluating important clinical outcomes; these are sadly lacking for phosphate binders. Thus results of these cost-effectiveness studies cannot be considered definitive due to the limitations mentioned and should be interpreted with caution [95, 104, 107]. Medication adherence and influence of pill burden on quality of life were not included in any of the models due to lack of information. Sevelamer hydrochloride and carbonate are off patent in many countries, and generic formulations may significantly reduce the acquisition cost and thus cost-effectiveness calculations [112].
7 Potential Incremental Effectiveness or Safety of Phosphate-Binding Agents in Development
Newer agents to reduce phosphorus have been evaluated in CKD patients and include resin-based binders, salivary phosphorus-binding agents, and agents that target intestinal phosphate transporters. While consideration of new agents is encouraging, comparative effectiveness data are sparse. Overall, these agents have thus far not offered advantages over sevelamer, the binder that has been evaluated in some smaller comparative studies to date.
7.1 Targeting Intestinal Phosphate Transport
7.1.1 Nicotinamide
Nicotinamide is an amide derivative of niacin (nicotinic acid) that inhibits sodium-dependent phosphate co-transport in the renal proximal tubule (Na/Pi2a) and in the intestine (Na/Pi2b) to decrease phosphorus uptake. Nicotinamide has less risk of causing a flushing reaction, making it a more viable option for long-term administration. Trials to date in relatively small numbers of ESRD patients have shown that nicotinamide when added to other phosphate-binding agents lowers phosphate in dialysis patients while also increasing high-density lipoprotein cholesterol, although flushing reactions were reported [113,114,115]. Doses ranged from 100 to 750 mg (200–1500 mg per day).
Limited data are available on the effect of nicotinamide as a single agent. Recent results from the NICOREN study showed similar phosphate-lowering effects of nicotinamide compared with sevelamer in 100 hemodialysis patients after 24 weeks of treatment in this open-labeled study; however, adverse effects increased in the nicotinamide group, leading to greater treatment discontinuation [116]. One concern with nicotinamide is accumulation of the metabolite N-methyl-2-pyridone-5-carboxamide (2PY), a potential uremic toxin with effects including thrombocytopenia [117]. This metabolite was increased during the treatment period in the NICOREN study. Potential adverse effects reported with nicotinamide include flushing, diarrhea, nausea, and thrombocytopenia [118].
Nicotinamide effectiveness for phosphate lowering in the NDD-CKD population has not been extensively explored. Currently, the CKD Optimal Management with Binders and Nicotinamide (COMBINE) trial is underway. It will compare nicotinamide 1500 mg daily, lanthanum carbonate 1000 mg three times daily, combined therapy, and double placebo in approximately 200 individuals with eGFR 20–45 mL/min/1.73 m2 [118]. The primary outcomes are changes in serum phosphate and FGF23 over the 12-month treatment period. Secondary outcomes include changes in bone and mineral metabolism markers (i.e., parathyroid hormone, calcitriol, klotho), surrogate CV disease markers (left ventricular mass index), and surrogate measures of CKD progression and inflammation. Results are expected in 2018.
7.1.2 Tenapanor
Tenapanor inhibits the gastrointestinal sodium/hydrogen exchanger isoform 3 (NHE23) to reduce sodium and phosphate absorption; they are not appreciably absorbed. These attributes have led to investigation of this agent for treatment of hyperphosphatemia and for constipation-predominant irritable bowel syndrome in human trials [119, 120]. Dose-dependent reductions in serum phosphate were observed in a placebo-controlled trial of tenapanor in 162 hemodialysis patients with hyperphosphatemia using six different regimens: 3 or 30 mg administered once daily or 1, 3, 10, or 30 mg administered twice daily (range 2–60 mg daily), taken before meals [119]. There was significant reduction in serum phosphate compared with placebo; after 4 weeks of treatment, the largest reduction in phosphate was with 10 and 30 mg twice daily dosing. The main adverse effect of tenapanor was diarrhea. Completion rates were lower for tenapanor (50–83%) compared with placebo (85%), with adverse effects accounting for study discontinuation in 27% of tenapanor patients. Tenapanor’s phosphate-binding effect has been shown to be similar whether it is administered before or after meals. Drug interactions with drugs metabolized by the CYP450 3A4 pathway are not expected with tenapanor based on drug interaction studies with midazolam [121]. Future studies providing more information on dosing and adverse effects are needed before this agent can be approved for use in CKD patients with hyperphosphatemia.
7.2 Resin-Based Binders (Colestilan, Bixalomer)
Colestilan (BindRen®, Mitsubishi Tanabe Pharma Corporation) is a non-absorbable, non-ionic, ion-exchange resin that binds phosphorus and bile acids in the gastrointestinal tract [122]. It is marketed for hypercholesterolemia in Japan and for hyperphosphatemia in Austria, Germany, Portugal, and the UK. Reduction in blood glucose and hemoglobin A1c levels has also been reported. The recommended starting dosage for hyperphosphatemia is 6–9 g daily with a maximum dosage of 15 g per day. Studies have shown colestilan to be effective in lowering phosphorus as well as low-density lipoprotein cholesterol, effects that were sustained over longer-term (52-week) treatment [122, 123]. In general, colestilan is well tolerated, with gastrointestinal effects including nausea, vomiting, and diarrhea the most common adverse events reported [123]. Potential advantages may include the pleiotropic effects from observed low-density lipoprotein cholesterol reductions in addition to uric acid level reductions; however, direct comparison studies with CCPBs and sevelamer have not been conducted to date and further development of this agent for hyperphosphatemia is not being pursued by the company. It is currently no longer available in Europe.
Bixalomer (Kiklin®, Astellas Pharma Inc.) is an amine-functional polymer available in Japan since 2012. It is effective in lowering phosphorus and may have fewer gastrointestinal adverse effects, including less diarrhea, reflux, constipation, and abdominal pain, a finding observed in hemodialysis patients switched from sevelamer hydrochloride to bixalomer [124]. However, the improvement in gastrointestinal symptoms is not a consistent finding among trials [125]. The potential differences in gastrointestinal side effects may be due, in part, to less expansion of bixalomer in the gastrointestinal tract, compared with sevelamer, from lower water adsorption. Bixalomer is currently available only in Japan.
7.3 Salivary Phosphorus-Binding Agents (Chitosan)
Agents that bind salivary phosphorus were investigated based on the fact that salivary phosphorus levels are higher than serum levels, particularly in patients with advanced NDD-CKD and ESRD [126]. Chitosan is a polymer of glucosamine and is derived from chitin, a natural fiber from crustacean shells. The polymer and amino residue of chitosan binds with phosphorus, which was the basis for developing a chewing gum (HS219) containing 40 mg of chitosan. Earlier studies showed that a gum containing 20 mg of chitosan when chewed for 1 h twice daily for 2 weeks was effective in lowering phosphorus in dialysis patients (31% reduction in serum phosphorus). Unfortunately, these results have not been duplicated in subsequent studies [127, 128]. The phosphate binding capacity of this agent is relatively low (estimated as 0.87 mg of phosphate bound with a 20-mg dose of chitosan gum) [129]. Chitosan is not being pursued as a viable phosphate-binding agent.
7.4 Other Phosphate-Binding Agents in Development
TRK-390 [copoly(allylamine/N 1,N 3-diallylpropane-1,3-diamine) acetate] is a polymer with higher selectivity for phosphate than sevelamer, with phosphate binding less affected by fat compared with sevelamer [130]. Another polymer under development is Genz-6444470, a non-absorbed polymer that has been studied in hemodialysis patients. It was effective in lowering phosphorus with a dose-dependent effect, but did not offer any advantage regarding phosphate lowering or tolerability compared with sevelamer [131].
SBR759 is a polymeric complex composed of iron (III) and starch that has been studied in phase I clinical trial in 44 hemodialysis patients [132]. In this open-label study, patients previously on a stable dose of sevelamer hydrochloride or a CCPB were given SBR759 in dosage levels ranging from 3.75 to 22.5 g/day for 4 weeks. Doses were titrated based on safety and tolerability up to 15 g/day. The highest dosage, 22.5 g/day, was used to test tolerability at supratherapeutic doses. More adverse reactions were experienced at this dose. Serum phosphorus decreased significantly across the dose range evaluated, and this drug was well tolerated. This agent has shown comparable phosphate-lowering effects with lower pill burden and adverse events than sevelamer hydrochloride in a 12-week study in Japanese and Taiwanese hemodialysis patients [133].
8 Overall Summary
All currently marketed phosphate binders have been shown to reduce serum phosphorus compared with placebo, which is the indication for which phosphate binders are marketed worldwide. Phosphate binders are routinely prescribed to dialysis patients to reduce serum phosphorus based on the hope of limiting progression of CKD-MBD and potentially reducing bone fractures, mortality and CV outcomes, and progression of kidney disease. Many, but not all, observational studies in the general population and in CKD patients associate higher serum phosphorus levels with higher mortality and CV events. Data are scarce for other important outcomes. No adequately powered, long-term, placebo-controlled comparative trials have been performed to demonstrate that any phosphate binder or class in dialysis patients reduces fractures or progression of CKD, improves survival, or reduces CV events.
Recent meta-analyses based on RCTs have generally found that sevelamer use results in higher survival compared with CCPBs. However, included studies have shown significant heterogeneity and exclusion of single trials have changed results from significant to nonsignificant (or vice versa), which is concerning. Since no evidence from placebo-controlled trials shows that sevelamer reduces mortality in dialysis or in NDD-CKD patients, it is unclear whether lower mortality with sevelamer versus CCPBs represents a net benefit of sevelamer, net harm with CCPBs, or both (or neither). Studies have been insufficiently powered to evaluate differences in CV events and most trials have not evaluated fracture events, despite reduction in progression of CKD-MBD being the main rationale for using phosphate binders. There has been much less evaluation of phosphate binder use and outcomes in NDD-CKD patients. However, evidence from some small trials suggests that phosphate binders may not be efficacious and CCPBs may even be harmful in this population.
The main challenge in long-term lowering of serum phosphorus with phosphate binders is medication non-adherence. Pill burden and medication intolerance are two main identified factors that influence phosphate binder adherence. Lanthanum carbonate and sucroferric oxyhydroxide have lower pill burden than other phosphate binders, but have higher discontinuation rates than some due to patient intolerance. The lack of adherence data from most clinical trials makes it more difficult to interpret conflicting outcome results. Although newer phosphate binders are expensive, in the USA, cost is not a main driver of non-adherence for most dialysis patients, since most are covered by Medicare and most Medicare-covered dialysis patients are enrolled in Medicare Part D, which provides coverage for phosphate binders. Low-income patients receive highly subsidized medications through Part D, so out-of-pocket costs are relatively low to many patients. However, costs to the US Medicare program are substantial, reaching almost a billion dollars per year. Results from cost-effectiveness analyses must be viewed with caution, since most relied on effectiveness assumptions that may not be valid. New phosphate binders in clinical testing or under development do not appear to offer any significant advantages over currently available phosphate binders.
9 Conclusion
Phosphate binders may be valuable, particularly in treatment of hyperphosphatemia in dialysis patients, but their value should be derived not just from lowering phosphorus, but from improving hard clinical outcomes such as fractures, CKD progression, CV events, or mortality, similar to FDA guidance for evaluating CV outcomes—not just hemoglobin A1c in trials of new diabetes agents. Phosphate binders may also be useful in NDD-CKD patients, but more data are needed. Given the cost burden of newer phosphate binders on national health care budgets and out-of-pocket costs to patients, it is imperative that well-designed, randomized, blinded, adequately powered, long-term, placebo-controlled trials be conducted evaluating hard clinical endpoints. The same holds true for head-to-head comparative trials with phosphate binders. Based on the available evidence, the first priority should be a three-arm clinical trial evaluating placebo versus calcium acetate and sevelamer carbonate in dialysis patients. It is essential that these trials be blinded (a major limitation to most available evidence) and that adherence is accurately measured. Agencies that provide regulatory approval for drugs should consider providing guidance to industry to evaluate at a minimum the risk of fractures and CV events for any new phosphate binder in clinical development.
Change history
07 August 2017
An erratum to this article has been published.
References
Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–18.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;76(113):S24.
United States Renal Data System. 2016 USRDS annual data report: epidemiology of kidney disease in the United States. 2016 ed. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
Dominguez JR, Kestenbaum B, Chonchol M, Block G, Laughlin GA, Lewis CE, et al. Relationships between serum and urine phosphorus with all-cause and cardiovascular mortality: the Osteoporotic Fractures in Men (MrOS) Study. Am J Kidney Dis. 2013;61:555–63.
Foley RN, Collins AJ, Herzog CA, Ishani A, Kalra PA. Serum phosphorus levels associate with coronary atherosclerosis in young adults. J Am Soc Nephrol. 2009;20:397–404.
Tuttle KR, Short RA. Longitudinal relationships among coronary artery calcification, serum phosphorus, and kidney function. Clin J Am Soc Nephrol. 2009;4:1968–73.
Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G. Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation. 2005;112:2627–33.
Dhingra R, Sullivan LM, Fox CS, Wang TJ, D’Agostino RB Sr, Gaziano JM, et al. Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med. 2007;167:879–85.
Ganesh SK, Stack AG, Levin NW, Hulbert-Shearon T, Port FK. Association of elevated serum PO(4), Ca x PO(4) product, and parathyroid hormone with cardiac mortality risk in chronic hemodialysis patients. J Am Soc Nephrol. 2001;12:2131–8.
Eddington H, Hoefield R, Sinha S, Chrysochou C, Lane B, Foley RN, et al. Serum phosphate and mortality in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:2251–7.
McGovern AP, de LS, van VJ, Liyanage H, Tomson CR, Gallagher H, et al. Serum phosphate as a risk factor for cardiovascular events in people with and without chronic kidney disease: a large community based cohort study. PLoS One. 2013;8(9):e74996.
Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger SL, Young B, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol. 2005;16:520–8.
Martin M, Valls J, Betriu A, Fernandez E, Valdivielso JM. Association of serum phosphorus with subclinical atherosclerosis in chronic kidney disease. Sex makes a difference. Atherosclerosis. 2015;241:264–70.
Saab G, Whooley MA, Schiller NB, Ix JH. Association of serum phosphorus with left ventricular mass in men and women with stable cardiovascular disease: data from the Heart and Soul Study. Am J Kidney Dis. 2010;56:496–505.
Slinin Y, Blackwell T, Ishani A, Cummings SR, Ensrud KE. Serum calcium, phosphorus and cardiovascular events in post-menopausal women. Int J Cardiol. 2011;149:335–40.
Onufrak SJ, Bellasi A, Cardarelli F, Vaccarino V, Muntner P, Shaw LJ, et al. Investigation of gender heterogeneity in the associations of serum phosphorus with incident coronary artery disease and all-cause mortality. Am J Epidemiol. 2009;169:67–77.
Chartsrisak K, Vipattawat K, Assanatham M, Nongnuch A, Ingsathit A, Domrongkitchaiporn S, et al. Mineral metabolism and outcomes in chronic kidney disease stage 2–4 patients. BMC Nephrol. 2013;14:14.
Connolly GM, Cunningham R, McNamee PT, Young IS, Maxwell AP. Elevated serum phosphate predicts mortality in renal transplant recipients. Transplantation. 2009;87:1040–4.
Fouque D, Roth H, Pelletier S, London GM, Hannedouche T, Jean G, et al. Control of mineral metabolism and bone disease in haemodialysis patients: which optimal targets? Nephrol Dial Transplant. 2013;28:360–7.
Fukagawa M, Kido R, Komaba H, Onishi Y, Yamaguchi T, Hasegawa T, et al. Abnormal mineral metabolism and mortality in hemodialysis patients with secondary hyperparathyroidism: evidence from marginal structural models used to adjust for time-dependent confounding. Am J Kidney Dis. 2014;63:979–87.
Moore J, Tomson CR, Tessa SM, Borrows R, Ferro CJ. Serum phosphate and calcium concentrations are associated with reduced patient survival following kidney transplantation. Clin Transplant. 2011;25:406–16.
Floege J, Kim J, Ireland E, Chazot C, Drueke T, de FA, et al. Serum iPTH, calcium and phosphate, and the risk of mortality in a European haemodialysis population. Nephrol Dial Transplant. 2011;26:1948–55.
Block GA, Wheeler DC, Persky MS, Kestenbaum B, Ketteler M, Spiegel DM, et al. Effects of phosphate binders in moderate CKD. J Am Soc Nephrol. 2012;23:1407–15.
Hill KM, Martin BR, Wastney ME, McCabe GP, Moe SM, Weaver CM, et al. Oral calcium carbonate affects calcium but not phosphorus balance in stage 3–4 chronic kidney disease. Kidney Int. 2013;83:959–66.
Spiegel DM, Brady K. Calcium balance in normal individuals and in patients with chronic kidney disease on low- and high-calcium diets. Kidney Int. 2012;81:1116–22.
Cupisti A, Moriconi D, D’Alessandro C, Verde F, Marchini M, Saba A, et al. The extra-phosphate intestinal load from medications: is it a real concern? J Nephrol. 2016;29:857–62.
Benini O, D’Alessandro C, Gianfaldoni D, Cupisti A. Extra-phosphate load from food additives in commonly eaten foods: a real and insidious danger for renal patients. J Ren Nutr. 2011;21:303–8.
Sherman RA, Ravella S, Kapoian T. A dearth of data: the problem of phosphorus in prescription medications. Kidney Int. 2015;87:1097–9.
Leypoldt JK. Kinetics of beta2-microglobulin and phosphate during hemodialysis: effects of treatment frequency and duration. Semin Dial. 2005;18:401–8.
Sherman RA. Hyperphosphatemia in dialysis patients: beyond nonadherence to diet and binders. Am J Kidney Dis. 2016;67:182–6.
Courivaud C, Davenport A. Phosphate removal by peritoneal dialysis: the effect of transporter status and peritoneal dialysis prescription. Perit Dial Int. 2016;36:85–93.
Friedman EA. An introduction to phosphate binders for the treatment of hyperphosphatemia in patients with chronic kidney disease. Kidney Int Suppl. 2005;96:S2–6.
US Food and Drug Administration. Guidance for industry: diabetes mellitus—evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. 2008. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm071627.pdf. Accessed 27 Jan 2017.
Kidney Disease Improving Global Outcomes (KDIGO). KDIGO 2016 clinical practice guideline update on diagnosis, evaluation, prevention and treatment of CKD-MBD: public review draft. August 2016. http://www.kdigo.org/clinical_practice_guidelines/CKD-MBD%20Update/KDIGO%20CKD-MBD%20Update_Public%20Review_Final.pdf. Accessed 22 Jan 2017.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009;76(Supplement 113):S50–99.
Altmann P, Barnett ME, Finn WF. Cognitive function in Stage 5 chronic kidney disease patients on hemodialysis: no adverse effects of lanthanum carbonate compared with standard phosphate-binder therapy. Kidney Int. 2007;71:252–9.
Palmer SC, Gardner S, Tonelli M, Mavridis D, Johnson DW, Craig JC, et al. Phosphate-binding agents in adults with CKD: a network meta-analysis of randomized trials. Am J Kidney Dis. 2016;68:691–702. doi:10.1053/j.ajkd.2016.05.015.
Patel L, Bernard LM, Elder GJ. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in ckd: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016;11:232–44.
Habbous S, Przech S, Acedillo R, Sarma S, Garg AX, Martin J. The efficacy and safety of sevelamer and lanthanum versus calcium-containing and iron-based binders in treating hyperphosphatemia in patients with chronic kidney disease: a systematic review and meta-analysis. Nephrol Dial Transplant. 2017;32:111–25.
Wang C, Liu X, Zhou Y, Li S, Chen Y, Wang Y, et al. New conclusions regarding comparison of sevelamer and calcium-based phosphate binders in coronary-artery calcification for dialysis patients: a meta-analysis of randomized controlled trials. PLoS One. 2015;10(7):e0133938.
Sekercioglu N, Thabane L, Diaz Martinez JP, Nesrallah G, Longo CJ, Busse JW, et al. Comparative effectiveness of phosphate binders in patients with chronic kidney disease: a systematic review and network meta-analysis. PLoS One. 2016;11(6):e0156891.
Li T, Puhan MA, Vedula SS, Singh S, Dickersin K, The Ad Hoc Network Meta-analysis Methods Meeting Working Group. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. http://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-79. Accessed 5 Jan 2017.
Zhang C, Wen J, Li Z, Fan J. Efficacy and safety of lanthanum carbonate on chronic kidney disease-mineral and bone disorder in dialysis patients: a systematic review. BMC Nephrol. 2013;14:226.
Foley RN, Collins AJ, Ishani A, Kalra PA. Calcium-phosphate levels and cardiovascular disease in community-dwelling adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2008;156:556–63.
Zoccali C, Ruggenenti P, Perna A, Leonardis D, Tripepi R, Tripepi G, et al. Phosphate may promote CKD progression and attenuate renoprotective effect of ACE inhibition. J Am Soc Nephrol. 2011;22:1923–30.
Centers for Medicare and Medicaid Services. Medicare provider utilization and payment data: part D prescriber data CY 2014. Drug summary table: “Part D Prescriber National Summary table. CY2014. Microsoft Excel (.xlsx)”. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/PartD2014.html. Accessed 27 Jan 2017.
Department of Health and Human Services OoIG. High-price drugs are increasing federal payments for Medicare Part D catastrophic coverage. OIG Report: OEI-02-16-00270. https://oig.hhs.gov/oei/reports/oei-02-16-00270.pdf. Accessed 6 Jan 2017.
Navaneethan SD, Sakhuja A, Arrigain S, Sharp J, Schold JD, Nally JV Jr. Practice patterns of phosphate binder use and their associations with mortality in chronic kidney disease. Clin Nephrol. 2014;82:16–25.
Winkelmayer WC, Liu J, Kestenbaum B. Comparative effectiveness of calcium-containing phosphate binders in incident US dialysis patients. Clin J Am Soc Nephrol. 2011;6:175–83.
Isakova T, Gutierrez OM, Chang Y, Shah A, Tamez H, Smith K, et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009;20:388–96.
Kovesdy CP, Kuchmak O, Lu JL, Kalantar-Zadeh K. Outcomes associated with phosphorus binders in men with non-dialysis-dependent CKD. Am J Kidney Dis. 2010;56:842–51.
Cheng J, Pullenayegum E, Marshall JK, Iorio A, Thabane L. Impact of including or excluding both-armed zero-event studies on using standard meta-analysis methods for rare event outcome: a simulation study. BMJ Open. 2016;6(8):e010983.
Suki WN, Zabaneh R, Cangiano JL, Reed J, Fischer D, Garrett L, et al. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients. Kidney Int. 2007;72:1130–7.
Di Iorio B, Molony D, Bell C, Cucciniello E, Bellizzi V, Russo D, et al. Sevelamer versus calcium carbonate in incident hemodialysis patients: results of an open-label 24-month randomized clinical trial. Am J Kidney Dis. 2013;62:771–8.
Yusuf AA, Weinhandl ED, St Peter WL. Comparative effectiveness of calcium acetate and sevelamer on clinical outcomes in elderly hemodialysis patients enrolled in Medicare part D. Am J Kidney Dis. 2014;64:95–103.
Altman DG, Andersen PK. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ. 1999;319(7223):1492–5.
Ogata H, Fukagawa M, Hirakata H, Kaneda H, Kagimura T, Akizawa T. Design and baseline characteristics of the LANDMARK study. Clin Exp Nephrol. 2016. doi:10.1007/s10157-016-1310-8.
St Peter WL, Liu J, Weinhandl E, Fan Q. A comparison of sevelamer and calcium-based phosphate binders on mortality, hospitalization, and morbidity in hemodialysis: a secondary analysis of the Dialysis Clinical Outcomes Revisited (DCOR) randomized trial using claims data. Am J Kidney Dis. 2008;51:445–54.
St Peter WL, Liu J, Weinhandl ED, Fan Q. Linking Centers for Medicare and Medicaid Services data with prospective DCOR trial data: methods and data comparison results. Hemodial Int. 2008;12:480–91.
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, et al. Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med. 2006;355:2085–98.
Drueke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med. 2006;355:2071–84.
Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de ZD, Eckardt KU, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019–32.
Floege J, Covic AC, Ketteler M, Rastogi A, Chong EM, Gaillard S, et al. A phase III study of the efficacy and safety of a novel iron-based phosphate binder in dialysis patients. Kidney Int. 2014;86:638–47.
Covic AC, Floege J, Ketteler M, Sprague SM, Lisk L, Rakov V, et al. Iron-related parameters in dialysis patients treated with sucroferric oxyhydroxide. Nephrol Dial Transplant. 2016. doi:10.1093/ndt/gfw242. [Epub ahead of print].
Floege J, Covic AC, Ketteler M, Mann JF, Rastogi A, Spinowitz B, et al. Long-term effects of the iron-based phosphate binder, sucroferric oxyhydroxide, in dialysis patients. Nephrol Dial Transplant. 2015;30:1037–46.
Koiwa F, Terao A. Dose–response efficacy and safety of PA21 in Japanese hemodialysis patients with hyperphosphatemia: a randomized, placebo-controlled, double-blind, Phase II study. Clin Exp Nephrol. 2016. doi:10.1007/s10157-016-1299-z. [Epub ahead of print].
Koiwa F, Yokoyama K, Fukagawa M, Terao A, Akizawa T. Efficacy and safety of sucroferric oxyhydroxide compared with sevelamer hydrochloride in Japanese haemodialysis patients with hyperphosphataemia: a randomised, open-label, multicentre, 12-week phase III study. Nephrology (Carlton). 2017;22:293–300.
Dwyer JP, Sika M, Schulman G, Chang IJ, Anger M, Smith M, et al. Dose-response and efficacy of ferric citrate to treat hyperphosphatemia in hemodialysis patients: a short-term randomized trial. Am J Kidney Dis. 2013;61:759–66.
Lewis JB, Sika M, Koury MJ, Chuang P, Schulman G, Smith MT, et al. Ferric citrate controls phosphorus and delivers iron in patients on dialysis. J Am Soc Nephrol. 2015;26:493–503.
Umanath K, Jalal DI, Greco BA, Umeukeje EM, Reisin E, Manley J, et al. Ferric citrate reduces intravenous iron and erythropoiesis-stimulating agent use in ESRD. J Am Soc Nephrol. 2015;26:2578–87.
Rodby R, Umanath K, Niecestro R, Jackson JH, Sika M, Lewis JB, et al. Phosphorus binding with ferric citrate is associated with fewer hospitalizations and reduced hospitalization costs. Expert Rev Pharmacoecon Outcomes Res. 2015;15:545–50.
Yokoyama K, Akiba T, Fukagawa M, Nakayama M, Sawada K, Kumagai Y, et al. A randomized trial of JTT-751 versus sevelamer hydrochloride in patients on hemodialysis. Nephrol Dial Transplant. 2014;29:1053–60.
Iguchi A, Kazama JJ, Yamamoto S, Yoshita K, Watanabe Y, Iino N, et al. Administration of ferric citrate hydrate decreases circulating FGF23 levels independently of serum phosphate levels in hemodialysis patients with iron deficiency. Nephron. 2015;131:161–6.
Yokoyama K, Akiba T, Fukagawa M, Nakayama M, Hirakata H. JTT-751 for treatment of patients with hyperphosphatemia on peritoneal dialysis. Nephron Clin Pract. 2014;128:135–40.
Block GA, Fishbane S, Rodriguez M, Smits G, Shemesh S, Pergola PE, et al. A 12-week, double-blind, placebo-controlled trial of ferric citrate for the treatment of iron deficiency anemia and reduction of serum phosphate in patients with CKD Stages 3-5. Am J Kidney Dis. 2015;65:728–36.
Fishbane S, Block GA, Loram L, Neylan J, Pergola PE, Uhlig K, et al. Effects of ferric citrate in patients with nondialysis-dependent CKD and iron deficiency anemia. J Am Soc Nephrol. 201. doi:10.1681/ASN.2016101053. [Epub ahead of print].
Yokoyama K, Hirakata H, Akiba T, Fukagawa M, Nakayama M, Sawada K, et al. Ferric citrate hydrate for the treatment of hyperphosphatemia in nondialysis-dependent CKD. Clin J Am Soc Nephrol. 2014;9:543–52.
US Food and Drug Administration. Ferric citrate tablets. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/205874Orig1s000TOC.cfm. Accessed 11 Apr 2017.
Gupta A. Ferric citrate hydrate as a phosphate binder and risk of aluminum toxicity. Pharmaceuticals (Basel). 2014;7:990–8.
Van Buren PN, Lewis JB, Dwyer JP, Greene T, Middleton J, Sika M, et al. The phosphate binder ferric citrate and mineral metabolism and inflammatory markers in maintenance dialysis patients: results from prespecified analyses of a randomized clinical trial. Am J Kidney Dis. 2015;66:479–88.
Ghimire S, Castelino RL, Lioufas NM, Peterson GM, Zaidi ST. Nonadherence to medication therapy in haemodialysis patients: a systematic review. PLoS One. 2015;10(12):e0144119.
Wang S, Anum EA, Ramakrishnan K, Alfieri T, Braunhofer P, Newsome B. Reasons for phosphate binder discontinuation vary by binder type. J Ren Nutr. 2014;24:105–9.
Arenas MD, Rebollo P, Malek T, Moledous A, Gil MT, Alvarez-Ude F, et al. A comparative study of 2 new phosphate binders (sevelamer and lanthanum carbonate) in routine clinical practice. J Nephrol. 2010;23:683–92.
Yusuf AA, St Peter WL. Medication adherence in hemodialysis patients treated with phosphate binders. Value Health. 2012;15:A153 (abstract PUK6).
Arenas MD, Malek T, Alvarez-Ude F, Gil MT, Moledous A, Reig-Ferrer A. Phosphorus binders: preferences of patients on haemodialysis and its impact on treatment compliance and phosphorus control. Nefrologia. 2010;30:522–30.
Daugirdas JT, Finn WF, Emmett M, Chertow GM. The phosphate binder equivalent dose. Semin Dial. 2011;24:41–9.
Coyne DW, Larson DS, Delmez JA. Bone Disease. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis. 5th ed. Philadelphia: Wolters Kluwer Health; 2015. p. 665–92.
Sheikh MS, Maguire JA, Emmett M, Santa Ana CA, Nicar MJ, Schiller LR, et al. Reduction of dietary phosphorus absorption by phosphorus binders. A theoretical, in vitro, and in vivo study. J Clin Invest. 1989;83:66–73.
Burke SK, Slatopolsky EA, Goldberg DI. RenaGel, a novel calcium- and aluminium-free phosphate binder, inhibits phosphate absorption in normal volunteers. Nephrol Dial Transplant. 1997;12:1640–4.
Kuhlmann MK. Management of hyperphosphatemia. Hemodial Int. 2006;10:338–45.
Ahlenstiel T, Pape L, Ehrich JH, Kuhlmann MK. Self-adjustment of phosphate binder dose to meal phosphorus content improves management of hyperphosphataemia in children with chronic kidney disease. Nephrol Dial Transplant. 2010;25:3241–9.
Stuart BC, Dai M, Xu J, Loh FH, Dougherty S. Does good medication adherence really save payers money? Med Care. 2015;53:517–23.
Murali K, Mullan J, Roodenrys S, Chen J, Lonergan M. Treatment adherence in clinical trials evaluating cardiovascular or mortality outcomes in dialysis patients: a systematic review. Nephrology. 2015;20(Supp. S3):32 (Abstract 053).
Rizk R, Hiligsmann M, Karavetian M, Evers SM. Economic evaluations of interventions to manage hyperphosphataemia in adult haemodialysis patients: a systematic review. Nephrology (Carlton). 2016;21:178–87.
Goto S, Komaba H, Fukagawa M, Nishi S. Optimizing the cost-effectiveness of treatment for chronic kidney disease-mineral and bone disorder. Kidney Int Suppl. 2013;3:457–61.
National Institute for Health and Care Excellence (NICE). Appendix F: full health economic report. NICE clinical guideline 157-hyperphosphataemia in chronic kidney disease. 2013. https://www.nice.org.uk/guidance/cg157/evidence/appendix-f-full-health-economic-report-189805647. Accessed 26 Oct 2016.
National Institute for Health and Care Excellence (NICE). Chronic kidney disease (stage 4 or 5): management of hyperphosphataemia: clinical guideline [CG157]. https://www.nice.org.uk/guidance/cg157. Accessed 26 Oct 2016.
Gutzwiller FS, Pfeil AM, Ademi Z, Blank PR, Braunhofer PG, Szucs TD, et al. Cost effectiveness of sucroferric oxyhydroxide compared with sevelamer carbonate in the treatment of hyperphosphataemia in patients receiving dialysis, from the perspective of the National Health Service in Scotland. Pharmacoeconomics. 2015;33:1311–24.
Thomas A, Peterson LE. Reduction of costs for anemia-management drugs associated with the use of ferric citrate. Int J Nephrol Renovasc Dis. 2014;7:191–201.
Rodby RA, Umanath K, Niecestro R, Bond TC, Sika M, Lewis J, et al. Ferric citrate, an iron-based phosphate binder, reduces health care costs in patients on dialysis based on randomized clinical trial data. Drugs R D. 2015;15:271–9.
Mutell R, Rubin JL, Bond TC, Mayne T. Reduced use of erythropoiesis-stimulating agents and intravenous iron with ferric citrate: a managed care cost-offset model. Int J Nephrol Renovasc Dis. 2013;6:79–87.
Vegter S, Tolley K, Keith MS, Postma MJ. Cost-effectiveness of lanthanum carbonate in the treatment of hyperphosphatemia in chronic kidney disease before and during dialysis. Value Health. 2011;14:852–8.
Thompson M, Bartko-Winters S, Bernard L, Fenton A, Hutchison C, Di IB. Economic evaluation of sevelamer for the treatment of hyperphosphatemia in chronic kidney disease patients not on dialysis in the United Kingdom. J Med Econ. 2013;16:744–55.
Gros B, Galan A, Gonzalez-Parra E, Herrero JA, Echave M, Vegter S, et al. Cost effectiveness of lanthanum carbonate in chronic kidney disease patients in Spain before and during dialysis. Health Econ Rev. 2015;5:49.
Nguyen HV, Bose S, Finkelstein E. Incremental cost-utility of sevelamer relative to calcium carbonate for treatment of hyperphosphatemia among pre-dialysis chronic kidney disease patients. BMC Nephrol. 2016;17:45.
National Institute for Health and Care Excellence (NICE). Hyperphosphataemia in chronic kidney disease: evidence update December 2014. https://www.nice.org.uk/guidance/cg157/evidence/evidence-update-18980175. Accessed 27 Oct 2016.
Rizk R. Cost-effectiveness of phosphate binders among patients with chronic kidney disease not yet on dialysis: a long way to go. BMC Nephrol. 2016;17:75.
John-Baptiste A, Bell C. Industry sponsored bias in cost effectiveness analyses. BMJ. 2010;341:c5350.
Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ. 2003;326(7400):1167–70.
Evers SM, Hiligsmann M, Adarkwah CC. Risk of bias in trial-based economic evaluations: identification of sources and bias-reducing strategies. Psychol Health. 2015;30:52–71.
Goeree R, Burke N, O’Reilly D, Manca A, Blackhouse G, Tarride JE. Transferability of economic evaluations: approaches and factors to consider when using results from one geographic area for another. Curr Med Res Opin. 2007;23:671–82.
Perry CM, Plosker GL. Sevelamer carbonate: a review in hyperphosphataemia in adults with chronic kidney disease. Drugs. 2014;74:771–92.
Cheng SC, Young DO, Huang Y, Delmez JA, Coyne DW. A randomized, double-blind, placebo-controlled trial of niacinamide for reduction of phosphorus in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:1131–8.
Young DO, Cheng SC, Delmez JA, Coyne DW. The effect of oral niacinamide on plasma phosphorus levels in peritoneal dialysis patients. Perit Dial Int. 2009;29:562–7.
El Borolossy R, El Wakeel LM, El Hakim I, Sabri N. Efficacy and safety of nicotinamide in the management of hyperphosphatemia in pediatric patients on regular hemodialysis. Pediatr Nephrol. 2016;31(2):289–96.
Lenglet A, Liabeuf S, El EN, Brisset S, Mansour J, Lemaire-Hurtel AS, et al. Efficacy and safety of nicotinamide in haemodialysis patients: the NICOREN study. Nephrol Dial Transplant. 2016. doi:10.1093/ndt/gfw042.
Lenglet A, Liabeuf S, Bodeau S, Louvet L, Mary A, Boullier A, et al. N-methyl-2-pyridone-5-carboxamide (2PY)-major metabolite of nicotinamide: an update on an old uremic toxin. toxins (Basel). 2016;8. doi:10.3390/toxins8110339.
Ginsberg C, Ix JH. Nicotinamide and phosphate homeostasis in chronic kidney disease. Curr Opin Nephrol Hypertens. 2016;25:285–91.
Block GA, Rosenbaum DP, Leonsson-Zachrisson M, Astrand M, Johansson S, Knutsson M, et al. Effect of tenapanor on serum phosphate in patients receiving hemodialysis. J Am Soc Nephrol. 2017. doi:10.1681/ASN.2016080855. [Epub ahead of print].
Chey WD, Lembo AJ, Rosenbaum DP. Tenapanor treatment of patients with constipation-predominant irritable bowel syndrome: a phase 2, randomized, placebo-controlled efficacy and safety trial. Am J Gastroenterol. 2017. doi:10.1038/ajg.2017.41. [Epub ahead of print].
Johansson SA, Knutsson M, Leonsson-Zachrisson M, Rosenbaum DP. Effect of food intake on the pharmacodynamics of tenapanor: a phase 1 study. Clin Pharmacol Drug Dev. 2017. doi:10.1002/cpdd.341. [Epub ahead of print].
Locatelli F, Dimkovic N, Spasovski G. Efficacy of colestilan in the treatment of hyperphosphataemia in renal disease patients. Expert Opin Pharmacother. 2014;15:1475–88.
Locatelli F, Spasovski G, Dimkovic N, Wanner C. Long-term evaluation of colestilan in chronic kidney disease stage 5 dialysis patients with hyperphosphataemia. Blood Purif. 2016;41:247–53.
Ito K, Takeshima A, Shishido K, Wakasa M, Kumata C, Matsuzaka K, et al. Treatment of hyperphosphatemia with bixalomer in Japanese patients on long-term hemodialysis with gastrointestinal symptoms. Ther Apher Dial. 2014;18(Suppl 2):19–23.
Gen S, Sasaki T, Saito K, Nobe K, Nodaira Y, Ikeda N. Clinical effects of the new phosphorus binder, bixalomer in hemodialysis patients switched from sevelamer hydrochloride. Ther Apher Dial. 2014;18(Suppl 2):8–12.
Savica V, Calo LA, Monardo P, Davis PA, Granata A, Santoro D, et al. Salivary phosphate-binding chewing gum reduces hyperphosphatemia in dialysis patients. J Am Soc Nephrol. 2009;20:639–44.
Block GA, Persky MS, Shamblin BM, Baltazar MF, Singh B, Sharma A, et al. Effect of salivary phosphate-binding chewing gum on serum phosphate in chronic kidney disease. Nephron Clin Pract. 2013;123:93–101.
Akizawa T, Tsuruta Y, Okada Y, Miyauchi Y, Suda A, Kasahara H, et al. Effect of chitosan chewing gum on reducing serum phosphorus in hemodialysis patients: a multi-center, randomized, double-blind, placebo-controlled trial. BMC Nephrol. 2014;15:98.
Oh MS, Uribarri J. What can we learn from the saga of chitosan gums in hyperphosphatemia therapy? Clin J Am Soc Nephrol. 2014;9:967–70.
Nakaki J, Yamaguchi S, Torii Y, Inoue A, Minakami S, Kanno T, et al. Effect of fatty acids on the phosphate binding of TRK-390, a novel, highly selective phosphate-binding polymer. Eur J Pharmacol. 2013;714:312–7.
Moustafa M, Lehrner L, Al-Saghir F, Smith M, Goyal S, Dillon M, et al. A randomized, double-blind, placebo-controlled, dose-ranging study using Genz-644470 and sevelamer carbonate in hyperphosphatemic chronic kidney disease patients on hemodialysis. Int J Nephrol Renovasc Dis. 2014;7:141–52.
Block GA, Brillhart SL, Persky MS, Amer A, Slade AJ. Efficacy and safety of SBR759, a new iron-based phosphate binder. Kidney Int. 2010;77:897–903.
Chen JB, Chiang SS, Chen HC, Obayashi S, Nagasawa M, Hexham JM, et al. Efficacy and safety of SBR759, a novel calcium-free, iron(III)-based phosphate binder, in Asian patients undergoing hemodialysis: A 12-week, randomized, open-label, dose-titration study versus sevelamer hydrochloride. Nephrology (Carlton). 2011;16:743–50.
Takei T, Otsubo S, Uchida K, Matsugami K, Mimuro T, Kabaya T, et al. Effects of sevelamer on the progression of vascular calcification in patients on chronic haemodialysis. Nephron Clin Pract. 2008;108:c278–83.
Navaneethan SD, Palmer SC, Vecchio M, Craig JC, Elder GJ, Strippoli GF. Phosphate binders for preventing and treating bone disease in chronic kidney disease patients. Cochrane Database Syst Rev. 2011;2:CD006023.
Jamal SA, Vandermeer B, Raggi P, Mendelssohn DC, Chatterley T, Dorgan M, et al. Effect of calcium-based versus non-calcium-based phosphate binders on mortality in patients with chronic kidney disease: an updated systematic review and meta-analysis. Lancet. 2013;382:1268–77.
Jamal SA, Fitchett D, Lok CE, Mendelssohn DC, Tsuyuki RT. The effects of calcium-based versus non-calcium-based phosphate binders on mortality among patients with chronic kidney disease: a meta-analysis. Nephrol Dial Transplant. 2009;24:3168–74.
Navaneethan SD, Palmer SC, Craig JC, Elder GJ, Strippoli GF. Benefits and harms of phosphate binders in CKD: a systematic review of randomized controlled trials. Am J Kidney Dis. 2009;54:619–37.
Coyne DW, Larson DS, Delmez JA. Bone disease. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis. 5th ed. Philadelphia: Wolters Kluwer Health; 2015. p. 673 (Table 36.3).
Acknowledgements
The authors thank Anne Shaw for manuscript preparation and Nan Booth, MSW, MPH, ELS, for manuscript editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There were no sources of funding for this manuscript.
Conflict of interest
Katie E. Cardone declares she has served on an advisory panel for AstraZeneca and her spouse is employed by Fresenius Medical Care. Eric Weinhandl is also employed by NxStage Medical, but there are no conflicts of interest with the content of this article. Wendy L. St. Peter, Joanna Q. Hudson and Lori D. Wazny declare that they have no conflict of interest.
Additional information
An erratum to this article is available at https://doi.org/10.1007/s40265-017-0798-x.
Rights and permissions
About this article
Cite this article
Peter, W.L.S., Wazny, L.D., Weinhandl, E. et al. A Review of Phosphate Binders in Chronic Kidney Disease: Incremental Progress or Just Higher Costs?. Drugs 77, 1155–1186 (2017). https://doi.org/10.1007/s40265-017-0758-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0758-5