Abstract
Crizotinib (Xalkori®) is an orally active, small molecule inhibitor of multiple receptor tyrosine kinases, including anaplastic lymphoma kinase (ALK), c-Met/hepatocyte growth factor receptor and c-ros oncogene 1. In the EU, crizotinib has been conditionally approved for the treatment of adults with previously treated, ALK-positive, advanced non-small cell lung cancer (NSCLC). This approval has been based on objective response rate and tolerability data from two ongoing phase I/II studies (PROFILE 1001 and PROFILE 1005); these results have been substantiated and extended by findings from an ongoing phase III study (PROFILE 1007) in patients with ALK-positive, advanced NSCLC who had received one prior platinum-based regimen. Those treated with crizotinib experienced significant improvements in progression-free survival, objective response rate, lung cancer symptoms and global quality of life, as compared with those treated with standard second-line chemotherapy (pemetrexed or docetaxel). The relative survival benefit with crizotinib is unclear, however, as the data are still immature and likely to be confounded by the high cross-over rate among chemotherapy recipients. Crizotinib treatment was generally well tolerated in the three PROFILE studies, with liver transaminase elevations and neutropenia being the most common grade 3 or 4 adverse events. Crizotinib is the standard of care in terms of the treatment of patients with ALK-positive, advanced NSCLC; while the current EU approval is for second (or subsequent)-line use only, the first-line use of the drug is being evaluated in ongoing phase III studies. Key issues relating to the use of crizotinib in clinical practice include identifying the small subset of eligible patients, the almost inevitable development of resistance and the high cost of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anaplastic lymphoma kinase (ALK) gene rearrangement is the ‘oncogenic driver’ in a small subset of patients with advanced NSCLC (≈2–7 %) The first-in-class ALK inhibitor crizotinib is the standard of care for patients with ALK-positive, advanced NSCLC; currently, it has been granted conditional approval in the EU for use as a second (or subsequent)-line therapy A high proportion – around one-half to two-thirds – of eligible (i.e. ALK-positive) patients respond to crizotinib treatment; however, responders almost inevitably develop (secondary) resistance |
Eligible patients may be identified using a two-tiered approach (prescreening with immunohistochemistry [IHC] followed by fluorescence in-situ hybridization confirmation of IHC-positive cases) |
1 Introduction
Lung cancer is the second most common cancer in the EU (e.g. 206,874 newly diagnosed cases in 2008) and, moreover, the most frequent cause of cancer-related mortality in this region (e.g. 26.4 % of all cancer-related deaths in 2008) [1]. Non-small cell lung cancer (NSCLC) accounts for 80–85 % of cases of lung cancer [2]; the majority of patients (≈80 %) present with locally advanced (stage IIIA/B) or metastatic (stage IV) disease and have a very poor prognosis, despite aggressive multimodal therapy (e.g. reported 5-year survival rates of 8–14 % for stage IIIA disease and 1–5 % for both stage IIIB and stage IV disease [3]).
Historically, the standard of care for advanced NSCLC has been platinum-based combination chemotherapy. However, this ‘one-size-fits-all’ approach to treatment has reached an efficacy plateau [4, 5] and been largely supplanted by a ‘personalized’ (pharmacogenomic-driven) approach, primarily due to the discovery that certain subsets of patients have identifiable and potentially targetable genomic alterations that are responsible for the initiation and maintenance of their cancer [6–11]. These so-called ‘oncogenic drivers’ include the following:
-
KRAS (V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog) gene mutations (in 15–36 % of patients [8]);
-
EGFR (epidermal growth factor receptor) gene mutations (in 10–15 % of [Caucasian] patients [8]);
-
MET (mesenchymal-epithelial transition factor) gene amplification (in 4–7 % of patients [12]);
-
ALK (anaplastic lymphoma kinase) gene rearrangements (in ≈2–7 % of patients [13]);
-
BRAF (v-raf murine sarcoma viral oncogene homolog B1) gene mutations (in 1–5 % of patients) [14, 15];
-
HER2 (human epidermal growth factor receptor 2) gene mutations (in 2 % of patients) [16];
-
RET (rearranged during transfection) gene rearrangements (in ≈2 % of patients) [17]; and
-
ROS1 (c-ros oncogene 1) gene rearrangements (in ≈1–2 % of patients) [18, 19].
Among the aforementioned, the ALK gene codes for ALK, a receptor tyrosine kinase (RTK) that belongs to the insulin receptor superfamily [20]. Briefly, ALK gene rearrangements involve the fusion of the ALK gene with another gene (predominantly the echinoderm microtubule-associated protein-like 4 [EML4] gene); the resulting (fusion) oncogene codes for an ALK fusion protein (e.g. EML4-ALK) that possesses unregulated constitutive tyrosine kinase activity, and thereby promotes tumour cell growth. Multiple chimeric variants of EML4-ALK (i.e. possessing the same portion of ALK [including the intracellular tyrosine kinase domain], but different portions of EML4) have been identified [21, 22].
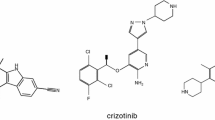
Crizotinib (Xalkori®) is an orally active, small-molecule, multitargeted tyrosine kinase inhibitor (TKI) [23]. Although originally developed as an inhibitor of MET (which, like ALK, is a RTK), crizotinib was subsequently shown to be a potent inhibitor of ALK [22]. Indeed, it is now regarded as being the first-in-class ALK inhibitor, i.e. targeting ALK-rearranged (ALK-positive) NSCLC [23, 24]. The Committee on Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) has granted ‘conditional approval’ to crizotinib for the treatment of adults with previously treated, ALK-positive, advanced NSCLC [25]. This article is written from a European perspective; therefore, it reviews the pharmacological characteristics of crizotinib and its therapeutic efficacy and tolerability in patients with previously treated, ALK-positive, advanced NSCLC.
2 Pharmacodynamic Properties
This section provides an updated overview of the key pharmacodynamic (anticancer) properties of crizotinib, which have been reviewed previously [22]. The effects of crizotinib on cardiac electrophysiology (i.e. QT interval and heart rate) are discussed in Sects. 3.2 and 5.1; its effects on testosterone levels in males are also considered in Sect. 5.1.
Crizotinib is a small molecule (molecular weight 450 Da), adenosine triphosphate (ATP)-competitive inhibitor of RTKs, including MET (also known as c-Met/hepatocyte growth factor receptor), ALK, Recepteur d’Origine Nantais (RON) and ROS1 [22, 29, 31]. By preventing ATP from binding, crizotinib inhibits autophosphorylation of the RTK, which is required for enzyme activation [32].
Crizotinib is highly selective for ALK and MET; when evaluated against a panel of >120 kinases in biochemical assays and 12 cell-based phosphorylation assays, it was nearly 20-fold more selective for ALK and MET compared with other kinases evaluated [23, 27, 33].
Key preclinical data pertaining to the anticancer properties of crizotinib in NSCLC are summarized in Table 1. Crizotinib inhibited autophosphorylation of EML4-ALK [26, 28] and MET [27] in a concentration or dose-dependent manner; it inhibited downstream signalling targets of these aberrant or overexpressed RTKs in a similar fashion [29, 30] (see Table 1). The drug displayed cytoreductive antitumour efficacy in murine xenograft models generated from EML4-ALK-positive [26, 28] or MET amplification-positive [27, 30] cell lines (see Table 1); this activity was dose-dependent and correlated strongly with inhibition of autophosphorylation of the rearranged or overexpressed RTK in vivo [26, 27]. According to a pharmacodynamic/pharmacokinetic modelling study [34], the half-maximal effective concentration (EC50) for ALK inhibition approximately corresponded to the EC50 for tumour growth inhibition in murine xenograft models generated from ALK-positive cell lines, suggesting that >50 % ALK inhibition is required for significant (>50 %) antitumour efficacy. Greater than 70 % ALK inhibition is projected to occur in patients with NSCLC who are treated with the recommended dosage of crizotinib (250 mg twice daily; see Sect. 6).
Crizotinib likely exerts its antitumour activity through multiple distinct mechanisms arising from inhibition of ALK- or MET-dependent signalling; these include direct negative effects on cell growth and survival [27, 33] (see Table 1). Notably, the drug exhibited a marked antitumour action in NSCLC cells bearing MET amplification, although it showed no such effect in NSCLC cells without MET amplification, including those with a MET gene mutation [30].
Crizotinib has also demonstrated inhibitory activity against an NSCLC cell line harbouring a ROS1 fusion protein (SLC34A2-ROS1) [18, 29]. Crizotinib reduced the phosphorylation of SLC34A2-ROS1 and its downstream signalling targets [29], and adversely affected cell growth [18, 29] and survival [29] (see Table 1). However, the extent of the antiproliferative effect of crizotinib in this cell line appeared to be somewhat less than that in an NSCLC cell line harbouring an ALK fusion protein (EML4-ALK) [18, 29]. For example, at concentrations of 0.1 and 1.0 μmol/L, crizotinib inhibited the proliferation of SLC34A2-ROS1-positive HCC78 cells by 31.1 and 58.1 %, respectively, whereas it inhibited proliferation of EML4-ALK-positive H3122 cells by 48.6 and 80.3 %, respectively [29].
There are conflicting results regarding the interaction, if any, between crizotinib and ionizing radiation [28, 35]. One research group reported that the drug acted as a radiation sensitizer in two EML4-ALK-positive NSCLC cell lines (H3122 and H2228) and an H3122 xenograft model [28]. However, another group found that crizotinib did not enhance radiation sensitivity in five NSCLC cell lines (including EML4-ALK-positive [H3122 and H2228] and MET amplification-positive [H1993 and H2228] cells) or three xenograft models (including H3122 and H2228 models) [35].
3 Pharmacokinetic Properties
The key pharmacokinetic properties of oral crizotinib have been reviewed previously [22] and are summarized in Table 2. Most of the data in this section have been obtained from the EU summary of product characteristics (SPC) [25] and/or abstracts [36, 37, 40, 41].
Maximum plasma concentration (Cmax) and area under the plasma concentration-time curve (AUC) values for crizotinib have not been reported, for example in the EU SPC [25] or US prescribing information [38]. That noted, in a phase I study in which patients with NSCLC received the recommended dosage of crizotinib (250 mg twice daily; see Sect. 6), the median trough plasma concentration at steady state (256 ng/mL) exceeded the target efficacy levels predicted for the inhibition of ALK and MET based on preclinical models [40].
Coadministration with food (standard high-fat meal) had no clinically relevant effect on crizotinib exposure after a single oral dose of 250 mg in healthy volunteers [25] or patients with NSCLC [40]; crizotinib can be taken without regard to meals [25]. Distribution of crizotinib into tissues from the plasma is extensive [25], although penetration of the blood-brain barrier by the drug appears limited [39] (see Table 2).
Crizotinib is predominantly metabolized by cytochrome P450 (CYP) 3A4/5; the main metabolic pathways are oxidation of the piperidine ring to crizotinib lactam and O-dealkylation (with subsequent conjugation of the O-dealkylated metabolites) [25]. Autoinhibition of CYP3A by crizotinib likely accounts for the observation that the mean apparent clearance of crizotinib is lower after multiple doses than it is after a single dose [36] (see Table 2).
Faecal/biliary excretion is the major route of elimination of crizotinib (and its metabolites) [37]. Following administration of a single oral radiolabelled dose of crizotinib 250 mg to healthy volunteers, 63 % of the dose was eliminated via the faeces (53 % as unchanged drug) and 22 % in the urine (1.3–2.3 % as unchanged drug) [25, 37].
3.1 Special Patient Populations
According to the results of population pharmacokinetic models, starting dose adjustments of crizotinib are not required on the basis of age, gender, bodyweight or race [41]. This notwithstanding, there is a 97 % probability that a typical AUC value at steady state in an Asian patient will be >25 % higher than the corresponding value in a non-Asian patient [41].
The pharmacokinetics of crizotinib have not been studied in patients with hepatic impairment; however, as crizotinib is extensively metabolized by the liver, plasma levels of the drug are likely to be increased in these patients [22]. Crizotinib should be used cautiously in patients with mild or moderate hepatic impairment; it is contraindicated in patients with severe hepatic impairment [25]. Notably, patients with alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels greater than two-and-a-half times the upper limit of normal (ULN) or, if due to underlying malignancy, greater than five times the ULN or with total bilirubin levels greater than one-and-a-half times the ULN, were excluded from clinical trials [25].
In phase I/II studies (see Sect. 4 for study design details), neither mild nor moderate renal dysfunction (creatinine clearance [CLCR] 60–90 and 30–60 mL/min, respectively) appeared to alter steady-state trough concentrations of crizotinib, which, in these two patient groups, were similar to those observed in patients with normal renal function (CLCR >90 mL/min) [25]. Accordingly, no starting dose adjustment is recommended for patients with mild or moderate renal impairment [25]. No data are available in patients with severe renal dysfunction or end-stage renal disease; therefore, no formal dosing recommendations have been made [25].
3.2 Drug Interactions
Potential pharmacokinetic and pharmacodynamic drug interactions between crizotinib and coadministered agents are summarized in Table 3.
Consistent with CYP3A4/5 being the major enzymes involved in the metabolic clearance of crizotinib (Table 2), crizotinib exposure may be increased when the drug is coadministered with potent CYP3A inhibitors, and decreased when it is coadministered with potent CYP3A inducers [25]. Compared with the corresponding values when crizotinib was administered alone, values for the crizotinib Cmax and AUC from time zero to infinity (AUC∞) were increased by ≈1.4- and 3.2-fold, respectively, when a single dose of crizotinib (150 mg) was coadministered with multiple doses of the strong CYP3A inhibitor ketoconazole (200 mg twice daily), and decreased by 69 and 82 %, respectively, when a single dose of crizotinib (250 mg) was coadministered with multiple doses of the strong CYP3A inducer rifampicin (600 mg once daily), in specific drug interaction studies conducted in healthy volunteers [25]. Moreover, there is both in vitro and in vivo evidence to suggest that crizotinib is itself a moderate inhibitor of CYP3A and, accordingly, may increase exposure to other CYP3A substrates when given concomitantly. In patients with cancer who were treated with crizotinib 250 mg twice daily for 28 days, coadminstration of a single oral dose of midazolam 2 mg increased the midazolam AUC by 3.7-fold relative to that observed when midazolam was administered alone [25].
There are also in vitro data suggesting that crizotinib is a substrate for P-glycoprotein, demonstrating that it is an inhibitor of CYP2B6, and indicating that it has only a low potential to inhibit or induce CYP1A2 (and therefore to interact with coadministered CYP1A2 substrates) [25].
QT interval prolongation has been observed in patients receiving crizotinib in clinical trials (see Sect. 5.1); a pharmacokinetic/pharmacodynamic analysis suggests that there is a relationship between Fridericia-corrected QT interval and crizotinib plasma concentrations [25]. Accordingly, crizotinib should be administered with caution to patients who have a history of, or predisposition for, corrected QT interval prolongation, or who are taking medications known to prolong the QT interval [25] (see Table 3).
Bradycardia has also been observed in patients receiving crizotinib in clinical trials (Sect. 5.1). According to the EU SPC [25], caution should be exercised in combining crizotinib with other bradycardic agents, due to the risk of excessive bradycardia. In comparison, the US prescribing information [38] recommends that combining crizotinib with other bradycardic agents be avoided.
4 Therapeutic Efficacy
The efficacy of oral crizotinib in patients (adults aged ≥18 years) with advanced, ALK-positive NSCLC has been evaluated in three ongoing, open-label, multinational trials: a randomized, controlled phase III study comparing crizotinib with single-agent pemetrexed or docetaxel (PROFILE 1007; Sect. 4.1); and two uncontrolled phase I/II and II studies (PROFILE 1001 and PROFILE 1005, respectively; Sect. 4.2). PROFILE 1007 and PROFILE 1005 exclusively enrolled previously treated patients; whereas PROFILE 1001 enrolled both treatment-naïve and previously treated patients, only results for the former are considered herein. Findings from PROFILE 1007 are available from published reports (i.e. abstracts [42, 43] plus a full paper [44]) and/or an online database [45]. In contrast, the majority of the findings from PROFILE 1005 and all relevant results from PROFILE 1001 are contained in the EU SPC [25] and/or the European Public Assessment Report (EPAR) for crizotinib [46]. Some findings from PROFILE 1005 are only available from an abstract [47].
4.1 Phase III Trial
Patients were eligible to enrol in PROFILE 1007 if they had the following: locally-advanced or metastatic NSCLC that was positive for ALK rearrangements; Eastern Cooperative Oncology Group (ECOG) performance status of 0–2; and progressive disease (PD) after one prior platinum-based chemotherapy regimen. Patients with stable brain metastases that were either previously treated or previously untreated and asymptomatic were permitted to enter the trial [44].
347 enrollees were randomized to receive oral crizotinib 250 mg twice daily or intravenous chemotherapy (either pemetrexed 500 mg/m2 or docetaxel 75 mg/m2) every 3 weeks; they were also stratified according to ECOG performance status (0 or 1 vs. 2), the presence or absence of brain metastases and prior or no prior EGFR TKI single agent therapy [44].
Demographic and baseline characteristics for the intent-to-treat (ITT) population are shown in Table 4; these parameters were well balanced between the crizotinib and chemotherapy groups (and, additionally, between the pemetrexed and docetaxel subgroups in the chemotherapy group [data not shown]). Most patients had adenocarcinoma of the lung (95 %), were aged <65 years (86 %) and had never smoked (63 %) [44]. Nearly half (45 %) were of Asian ethnicity [44] (Table 2).
The primary endpoint was progression-free survival (PFS), as assessed by independent radiological review. Secondary endpoints included objective response rate (ORR; based on Response Evaluation Criteria in Solid Tumors [RECIST]), as assessed by independent radiological review, and overall survival (OS). PFS, OS and, except where indicated, ORR, were analyzed in the ITT population [44].
Patients were treated until disease progression, unacceptable toxicity, withdrawal or death. Crizotinib recipients with documented disease progression could continue treatment at the discretion of the investigator. Chemotherapy recipients with documented disease progression could also continue treatment at the discretion of the investigator or, alternatively, cross-over to receive crizotinib as part of the ongoing PROFILE 1005 study (see Sect. 4.2) [44].
Single-agent crizotinib demonstrated superior efficacy to standard chemotherapy with either pemetrexed or docetaxel in patients with previously treated, ALK-positive, advanced NSCLC. At the cut-off date (i.e. the time of the final analysis of PFS), median PFS was more than two-fold longer in crizotinib recipients compared with chemotherapy recipients (Table 5); the hazard ratio (HR) for disease progression or death with crizotinib was 0.49 (95 % confidence interval [CI] 0.37–0.64; p < 0.001) [44].
In subgroup analyses, crizotinib significantly (p < 0.001) improved median PFS when compared with pemetrexed and docetaxel separately (HRs for disease progression or death of 0.59 [95 % CI 0.43–0.80] and 0.30 [95 % CI 0.21–0.43], respectively) [44]. Additionally, a positive impact of crizotinib on PFS was observed in most patient subgroups defined according to baseline characteristics or stratification factors. These subgroups were as follows (HR [95 % CI] for disease progression or death with crizotinib; number of patients): age ≥65 years (0.54 [0.27–1.08]; n = 50); age <65 years (0.49 [0.37–0.65]; n = 297); male (0.52 [0.35–0.77]; n = 153); female (0.48 [0.34–0.68]; n = 194; non-Asian (0.45 [0.30–0.66]; n = 190); Asian (0.53 [0.36–0.76]; n = 157); non-smoker (0.45 [0.32–0.63]; n = 219); smoker or ex-smoker (0.53 [0.34–0.83]; n = 127); adenocarcinoma (0.50 [0.38–0.66]; n = 328); non-adenocarcinoma (0.12 [0.01–1.02]; n = 12); ECOG performance status 0 or 1 (0.48 [0.36–0.63]; n = 313); ECOG performance status 2 (0.31 [0.12–0.86]; n = 34); brain metastases present (0.67 [0.44–1.03]; n = 120); brain metastases absent (0.43 [0.30–0.60]; n = 227); prior EGFR TKI therapy (0.48 [0.22–1.03]; n = 41); and no prior EGFR TKI therapy (0.49 [0.37–0.66]; n = 306) [44].
As anticipated, OS data were not mature by the cut-off date, with only 96 (40 %) of the 241 deaths required for the final analysis of OS having occurred after a median follow-up period of ≈12 months. A prespecified interim analysis did not show a significant difference in median OS between the crizotinib and chemotherapy groups (Table 5); the HR for death with crizotinib was 1.02 (95 % CI 0.68–1.54) [44]. However, this analysis was not only immature, but also likely to have been confounded by the high cross-over rate affecting the chemotherapy group (112 [64 %] of the 174 patients originally assigned to chemotherapy subsequently received crizotinib outside the study, i.e. in PROFILE 1005) [44].
Crizotinib therapy was associated with a high ORR that was more than three-fold greater than that with standard chemotherapy (65 vs. 20 %); all but one of the 113 responses observed with crizotinib were partial responses (Table 5). In an analysis of the as-treated population, the ORR to crizotinib (66 % [95 % CI 58–73]) was significantly (p < 0.001) higher than that to both pemetrexed (29 % [95 % CI 21–39]) and docetaxel (7 % [95 % CI 2–16]) [42, 44]. Of note, tumour responses to crizotinib were both rapid (the median time to response of 6.3 weeks was half that observed with chemotherapy) and durable (the median duration of response of 32.1 weeks was one-third longer than that with chemotherapy) [Table 5].
Patient-reported outcomes (PROs) were also assessed in PROFILE 1007. Crizotinib recipients reported a significantly (p < 0.001) greater overall improvement from baseline in global quality of life (QOL), as assessed using the European Organization for Research and Treatment of Cancer (EORTC) quality of life questionnaire (QLQ-C30), compared with chemotherapy recipients [44]. EORTC QLQ-C30 global QOL scores range from 0 to 100, with higher scores indicating better global QOL. The mean global QOL score increased by ≈4.4 points from baseline in the crizotinib group, whereas it decreased by ≈5.4 points from baseline in the chemotherapy group (figures estimated from a graph) [44]. The improvement in global QOL seen with crizotinib was significantly (p < 0.01) greater than that observed with either pemetrexed or docetaxel individually [43].
In addition, compared with chemotherapy-treated patients, crizotinib-treated patients reported a significantly (p ≤ 0.01) greater overall improvement from baseline in four of the five functional scales of the EORTC QLQ-C30, namely physical, social, role and emotional functioning. The fifth scale, namely cognitive functioning, was essentially unchanged from baseline with crizotinib; while it decreased from baseline with chemotherapy, the between-group difference did not reach statistical significance (p = 0.06) [44].
Compared with patients receiving chemotherapy, those receiving crizotinib also experienced significantly (p < 0.001) greater overall reductions from baseline in a number of symptoms that were assessed using the EORTC QLQ-C30 or its corresponding module for lung cancer (QLQ-LC13), namely alopecia, cough, dyspnoea, fatigue, chest pain, arm or shoulder pain, and pain in other parts of the body [44]. The median time to deterioration with respect to a composite of three of these symptoms—cough, dyspnoea or chest pain—was 5.6 months with crizotinib versus 1.4 months with chemotherapy (HR 0.54 [95 % CI 0.40–0.71]; p < 0.001) [44, 45]. Similar results were seen when crizotinib was compared with either pemetrexed or docetaxel individually (HRs of 0.66 [95 % CI 0.48–0.92] and 0.37 [95 % CI 0.26–0.54], respectively; both p ≤ 0.013) [43].
Consistent with the results for the overall study population, crizotinib treatment showed significantly greater improvements in PFS (p = 0.0003; see result reported earlier in this section), ORR (p < 0.0001), global QOL (p < 0.05) and lung cancer symptoms (e.g. cough, dyspnoea, fatigue, chest pain, arm or shoulder pain, and pain in other parts of the body; all p < 0.05) compared with chemotherapy in the large subgroup of Asian patients [42].
4.2 Phase I/II Trials
Protocol amendments affecting enrollment into the single-arm PROFILE 1001 and PROFILE 1005 studies since their respective inceptions have been reviewed elsewhere [23]. This section primarily focuses on data from a subset of patients in each trial (n = 125 and 261 in PROFILE 1001 and PROFILE 1005, respectively) who had locally-advanced or metastatic, ALK-positive NSCLC and who had received at least one prior systemic therapy [25, 46]. These results are notable, as they led to crizotinib gaining conditional approval for this indication in the EU; this occurred prior to the availability of data from PROFILE 1007. In contrast to PROFILE 1007, ORR was the primary endpoint in the PROFILE 1001 and PROFILE 1005 studies; PFS was a secondary endpoint [22].
Demographic and baseline characteristics of the study populations are shown in Table 4; as in PROFILE 1007, the majority of patients across the two trials had adenocarcinoma of the lung (94 %), were aged <65 years (88 %) and had never smoked (69 %) [Table 4]. With respect to prior systemic therapies, 38, 25 and 38 % of patients in PROFILE 1001 and 10, 35 and 55 % of patients in PROFILE 1005 had received one, two, or at least three treatment regimens, respectively [25, 46]. At the time of the data cut-off, the median duration of crizotinib treatment was 42 and 25 weeks in PROFILE 1001 and PROFILE 1005, respectively [25, 46].
Results from PROFILE 1001 and PROFILE 1005 are largely concordant with those from PROFILE 1007 (Table 5), thus confirming the benefit of single-agent crizotinib in previously treated, ALK-positive, advanced NSCLC. As observed in PROFILE 1007, ORRs to crizotinib were high; tumour responses to crizotinib were rapid and durable (Table 5).
More than one-third of the participants in PROFILE 1005 were Asian (Table 4). According to an exploratory subgroup analysis presented in an abstract [47], the ORR to crizotinib appeared to be higher in Asian than in non-Asian patients (70 % [95 % CI 60–79 %] vs. 54 % [95 % CI 46–62]). The response-evaluable population for this particular analysis comprised 259 of the first 261 patients enrolled [47]; it consisted of 255 patients for the other analyses quoted in this section [25, 46] (Table 5).
Regarding other patient populations of interest, ORRs for patients with or without brain metastases are available from PROFILE 1005, which, in contrast to PROFILE 1001, required baseline brain imaging [46]. The ORR in the CNS involvement subgroup (57 % [95 % CI 44–70]; n = 61) was similar to that in the non-CNS involvement subgroup (52 % [95 % CI 45–59]; n = 194), albeit the early death rate in the former was more than three times that in the latter (9.8 vs. 3.1 %) [46]. Seventeen patients had asymptomatic, unirradiated brain metastases and were evaluable for both brain metastasis and systemic tumour responses. Of these, eight had a brain response that matched or exceeded the systemic response (including two complete brain responses); the remaining nine had a systemic response that exceeded the brain response [25, 46]. The ORR was 31 % among a total of 29 evaluable patients with non-adenocarcinoma histology who were enrolled in either PROFILE 1005 or PROFILE 1001 [25].
Consistent with PROFILE 1007, PFS data from PROFILE 1001 and PROFILE 1005 had matured at the time of the data cut-off; however OS data were (and still are) immature. In PROFILE 1005, median PFS was 8.5 (95 % CI 6.5–9.9) months in an analysis performed after 41.8 % of the PFS events had occurred (Table 5); it was 8.1 (95 % CI 6.8–9.7) months in an updated analysis performed after 65.5 % of the PFS events had occurred [46]. In PROFILE 1001, median OS was not reached in an analysis based on 43 (34.4 %) deaths among 125 patients analysed (Table 5; result reported in both the EU SPC [25] and EPAR [46]); it was 29.6 (95 % CI 18.0 to not reached) months in an updated analysis based on 55 (42.3 %) deaths among 130 patients analysed (result reported only in the EPAR [46]). Both analyses yielded a 1-year survival probability estimate of 72.3 % [46].
5 Tolerability
The following tolerability profile of crizotinib in patients with previously treated, ALK-positive, NSCLC is largely based on pooled data from the noncomparative, phase I/II PROFILE 1001 and PROFILE 1005 studies [25, 48], as well as comparative results from the phase III PROFILE 1007 study of crizotinib versus standard chemotherapy [44] (see Sect. 4 for study design details). Table 6 summarises the incidences of frequent and/or notable treatment-related adverse events in these studies.
5.1 General Profile
Crizotinib was generally well tolerated in the three PROFILE studies, with most adverse events being grade 1 or 2 in severity [25, 44].
The most common (incidence >20 %) any-grade adverse events of any cause in patients who received crizotinib in either PROFILE 1001 or PROFILE 1005 were vision disorders (i.e. visual impairment, diplopia, photopsia, blurred vision and vitreous floaters), gastrointestinal disturbances (nausea, diarrhoea, vomiting, oedema and constipation) and fatigue [25] (Table 6).
Although frequent, visual disturbances were mostly transient (i.e. lasting ≤1 min), with no or minimal impact on patients’ activities of daily living, as assessed using a specially developed seven-item visual symptom assessment questionnaire [49]. No patient in either study required a dose reduction or permanent discontinuation of crizotinib treatment as a result of experiencing a visual disorder [25].
The most frequent grade 3 or 4 adverse events of any cause in patients who received crizotinib in either PROFILE 1001 or PROFILE 1005 were neutropenia (7 %) and elevated ALT levels (5 %) [25] [Table 6].
Grade 3 or 4 elevations in ALT were generally asymptomatic and reversible with interruption of crizotinib treatment; patients usually resumed therapy at a lower dosage without recurrence [25, 48]. According to the larger of two analyses considered herein, only four (<1 %) of 588 evaluable patients in the phase I/II studies have been required to permanently discontinue crizotinib treatment as a result of a grade 3 or 4 elevation in ALT [48]. This analysis [48] yielded rates of all-cause ALT elevations (all-grade, 14.6 %; grade 3 or 4, 5.1 %) and AST elevations (all-grade, 10.7 %; grade 3 or 4, 2.4 %) that were similar to those arising from a smaller analysis, which was based on 386 evaluable patients [25] (see Table 6). However, only the larger analysis reported rates of treatment-related ALT elevations (all-grade, 12.4 %; grade 3 or 4, 4.1 %) and AST elevations (all-grade, 8.8 %; grade 3 or 4, 1.7 %) [48]. Transaminase elevations generally occurred within 2 months of starting crizotinib treatment [25, 48].
In a separate analysis [25], concurrent elevation of ALT (to greater than three times the ULN) and total bilirubin (to greater than two times the ULN) in the absence of elevation of alkaline phosphatase was observed in only one (<0.5 %) of the 375 evaluable patients.
Crizotinib is uncommonly associated with severe hepatotoxicity, which was reported in <1 % of patients (i.e. a total of five cases), according to one analysis [48]. Presenting symptoms included fatigue, nausea, anorexia, weakness and abdominal pain; two of the five cases eventually proved fatal. In four cases, the time to onset of hepatotoxicity was <6 weeks; in one case, significant transaminase elevation was observed after 6 months. Four patients had baseline transaminase levels that were normal or just above the norm; one patient (who was one of the two eventually fatal cases) had abnormal transaminase levels and significant hepatic metastases at baseline [48].
The tolerability profile of crizotinib in PROFILE 1007 was qualitatively similar to that of the drug in the pooled PROFILE 1001 and PROFILE 1005 trials (Table 6). The most common grade 3 or 4 adverse event of any cause in PROFILE 1007 was an elevation of liver aminotransferase levels (16 %) [Table 6]. However, the incidences of elevated ALT and AST levels have not (yet) been reported separately and therefore cannot be compared with the corresponding incidences in the pooled PROFILE 1001 and PROFILE 1005 studies. The second most common grade 3 or 4 adverse event in PROFILE 1007 was neutropenia (13 %); the incidence of this adverse event was almost double that observed in the pooled PROFILE 1001 and PROFILE 1005 studies (Table 6). The third most common grade 3 or 4 adverse event in PROFILE 1007 was pulmonary embolism (5 %) [Table 6].
As regards other notable adverse events associated with crizotinib treatment, pneumonitis was observed in 1 % of patients in the pooled phase I/II studies (Table 6); all four cases (including three severe or life-threatening [grade 3 or 4] cases and one fatal [grade 5] case) occurred within 2 months of initiating treatment [25]. There have also been two cases of fatal treatment-related pneumonitis or interstitial lung disease among crizotinib recipients in PROFILE 1007 (see Sect. 5.2). Grade 3 or 4 QT prolongation was observed in <1 % of patients in the pooled PROFILE 1001 and PROFILE 1005 studies, as compared with 4 % of patients in PROFILE 1007 (Table 6).
Grade 1 or 2 bradycardia was reported in 4 % of patients in the pooled phase I/II studies (Table 6) and was therefore classified as being common in terms of frequency [25]. Of note, heart rate (HR) changes during crizotinib treatment have been retrospectively analysed at a single centre in the US [50]. 38 (≈90 %) of 42 crizotinib-treated patients with ALK-rearranged or MET-amplified NSCLC (all of whom were enrolled in PROFILE 1005 or PROFILE 1001) experienced at least one episode of a decrease in HR of >10 beats per minute (bpm) from pretreatment baseline. 29 patients (69 %) experienced at least one episode of sinus bradycardia (HR <60 bpm); among these were 13 patients (44.8 %) who experienced at least one episode of profound sinus bradycardia (HR <50 bpm). However, none of the patients who experienced sinus bradycardia or profound sinus bradycardia were symptomatic or had ECG changes (e.g. corrected QT interval prolongation). The mean maximum decrease in HR for all (42) patients was 26.1 bpm [50].
Treatment with crizotinib reportedly reduced testosterone levels to below the lower limit of normal (LLN) in male patients with NSCLC; this reduction appeared to be rapid (over a period of weeks) and reversible (over a period of days) on commencement and cessation of crizotinib therapy, respectively [51, 52]. In the largest study to date [52], mean total testosterone levels were significantly (p ≤ 0.0012) lower in two groups of 32 and 19 patients who received the drug when both series were compared (separately) with a third group of 19 patients who did not receive the drug. Most (90 %) of the crizotinib-treated patients had a mean testosterone level below the LLN, as compared with only approximately one-third (32 %) of the non-crizotinib-treated patients [52]. Among a subset of 25 crizotinb-treated patients (with both total and free testosterone data), 20 (80 %) manifested symptoms of hypogonadism, as assessed using the Androgen Deficiency in Aging Males (ADAM) questionnaire [52]. Levels of albumin and sex hormone-binding globulin (which both bind testosterone) declined rapidly with crizotinib; the absence of a compensatory increase in follicle-stimulating hormone or luteinizing hormone levels suggested that the mechanism of testosterone reduction included a central effect of crizotinib on the hypothalamic-pituitary axis [52].
The rates of treatment-related adverse events resulting in permanent discontinuation of crizotinib were 2, 4 and 6 % in PROFILE 1001, PROFILE 1005 and PROFILE 1007, respectively [25, 44].
5.2 Comparative Tolerability
The tolerability profile of crizotinib in PROFILE 1007 was distinct from that of standard chemotherapy. As regards any-grade adverse events of any cause, vision disorders, nausea, diarrhoea, vomiting, constipation, oedema, dizziness, elevated liver aminotransferase levels, dysgeusia and upper respiratory tract infection were reported numerically more frequently in crizotinib recipients than in chemotherapy recipients, whereas alopecia, dyspnoea, fatigue and rash were reported numerically more frequently in chemotherapy-treated patients than in crizotinib-treated patients (Table 6). That noted, the median treatment duration was almost three-fold longer with crizotinib than with chemotherapy (Table 6); after adjusting for this difference, the rates of nausea, constipation, oedema, dizziness, elevated transaminases and upper respiratory tract infection were not significantly different between the two groups [53]. The exposure-adjusted incidence rates of vision disorders, diarrhoea, vomiting and dysgeusia, however, remained significantly higher in crizotinib recipients compared with chemotherapy recipients (all p ≤ 0.045) [53].
The overall incidence of treatment-related grade 3 or 4 adverse events was similar in the two groups (33 and 32 % with crizotinib and chemotherapy, respectively), as was the overall incidence of treatment-related serious adverse events (SAEs) [12 and 14 %, respectively] [44]. Additionally, there was no significant difference between the crizotinib and chemotherapy groups in terms of the exposure-adjusted incidence rate of non-fatal SAEs (440 and 640 per 1000 patient-years of exposure, respectively) [53]. In the crizotinib group, treatment-related SAEs included (among others) four cases of interstitial lung disease and two cases of pneumonia, while in the chemotherapy group, treatment-related SAEs were mainly related to haematological toxicity [46]. The rates of treatment-related adverse events resulting in permanent discontinuation were 6 and 10 % in crizotinib and chemotherapy recipients, respectively [25, 44].
The 96 deaths that occurred by the cut-off date (see Sect. 4.1) included 32 fatal (grade 5) adverse events of any cause (25 and 7 in the crizotinib and chemotherapy groups, respectively) [44]. The most common grade 5 adverse event was disease progression (in 14 and 3 crizotinib and chemotherapy recipients, respectively); three grade 5 adverse events in crizotinib-treated patients (one case of ventricular arrhythmia and two cases of interstitial lung disease or pneumonitis), as compared with one grade 5 adverse event in chemotherapy-treated patients (one case of sepsis), were considered to be treatment-related [44].
6 Dosage and Administration
In the EU, orally administered crizotinib is conditionally approved for the treatment of adults with previously treated, ALK-positive, advanced NSCLC [25]. The recommended dosage is 250 mg twice daily; treatment should be continued until disease progression or unacceptable toxicity. Prolongation of treatment after objective disease progression in selected patients may be considered on an individual basis (see Sect. 7); however, no additional benefit has been demonstrated [25].
Local prescribing information for crizotinib should be consulted for further information regarding posology and method of administration (including recommended dose adjustments in patients experiencing haematological or non-haematological toxicities), contraindications, special warnings and precautions for use, and drug interactions.
7 Place of Crizotinib in the Management of Non-Small Cell Lung Cancer
Crizotinib received conditional approval in the EU for the treatment of adults with previously treated, ALK-positive, advanced NSCLC approximately 5 years after the initial discovery of ALK rearrangements in NSCLC; the rapid development of the drug, including the history of the first in-human phase I/II trials (PROFILE 1001 and PROFILE 1005), has been described in detail elsewhere [23]. A conditional approval in the EU is similar to an accelerated approval in the US; crizotinib has been granted accelerated approval for the treatment of patients with locally-advanced or metastatic NSCLC that is ALK positive (as detected by an FDA-approved test) [38].
Crizotinib is the first – and so far only – ALK inhibitor to be approved in the EU and US; it is also approved in Canada and Japan [54]. Other, second-generation ALK inhibitors currently in clinical development include LDK378 [55], CH5424802 [56, 57] and AP-26113 [58]. The investigational heat shock protein 90 inhibitors ganetespib [59] and retaspimycin [60] have also demonstrated clinical activity in pretreated patients with advanced NSCLC, particularly among those harbouring ALK rearrangements.
In the EU, as in the US, approval of crizotinib was based on ORR and tolerability data from the PROFILE 1001 and PROFILE 1005 studies (Sect. 4.2), and occurred prior to the availability of results from the phase III PROFILE 1007 study (Sect. 4.1). Updated results from PROFILE 1001 (which included both pretreated and untreated patients) have been published in full [61]; initial findings from PROFILE 1005 have been published in preliminary form [62].
Briefly, the results of PROFILE 1007 both substantiated and extended those of PROFILE 1005 and PROFILE 1001. That is, a high proportion (approximately two-thirds) of patients with previously treated, ALK-positive, advanced NSCLC responded to crizotinib treatment; these responses were typically rapid and durable (Sect. 4.1). Moreover, patients receiving crizotinib demonstrated a significantly higher ORR, a significantly longer PFS, a significant reduction in lung cancer symptoms and a significant improvement in global QOL, as compared with those receiving standard second-line chemotherapy with either docetaxel or pemetrexed (Sect. 4.1). Crizotinib was generally well tolerated in the three PROFILE studies, with most adverse events (e.g. vision disorders, gastrointestinal disturbances and oedema) being of grade 1 or 2 severity (Sect. 5.1). Liver transaminase elevations and neutropenia were the most frequent grade 3 or 4 adverse events, e.g. in PROFILE 1007 (Sect. 5.1).
A retrospective analysis of data from PROFILE 1001 suggested that OS was significantly prolonged in ALK-positive patients receiving crizotinib as a second- or third-line treatment, as compared with ALK-positive crizotinib-naïve controls [63]. In comparison, PROFILE 1007 has (thus far) not shown a survival benefit for crizotinib over chemotherapy; however, the OS data are still immature and, moreover, likely to be confounded by the high cross-over rate among patients in the chemotherapy group (Sect. 4.1). The use of a cross-over design is ethically appropriate, but (according to some authors) makes it highly improbable that a survival advantage of crizotinib over chemotherapy will ever be demonstrated [24]. Cross-over has similarly complicated the analysis of OS in phase III studies of EGFR TKIs in patients with EGFR mutation-positive, advanced NSCLC [44].
The major difference between the EU and the US is that crizotinib is (currently) reserved for use as a second- or subsequent-line therapy in the former, but not in the latter. Indeed, the National Comprehensive Cancer Network (NCCN) guidelines recommend crizotinib as a first-line therapy in patients with locally-advanced or metastatic NSCLC who are ALK positive [64]. The use of crizotinib in the first-line setting is being evaluated in two ongoing phase III studies in which previously untreated patients aged ≥18 years with ALK-positive, advanced NSCLC are being randomized in an open-label fashion to receive crizotinib or standard chemotherapy (with pemetrexed plus either cisplatin or carboplatin) [65, 66]. The primary endpoint in both trials is PFS; patients assigned to chemotherapy are allowed to cross-over to crizotinib when they experience disease progression [65, 66]. The larger of the two studies, PROFILE 1014 (NCT01154140) [65], has an estimated enrollment of 334 patients; the smaller of the two studies, NCT01639001 [66], has an estimated enrollment of 200 (East Asian) patients.
Based on the current evidence, crizotinib should only be prescribed to patients with advanced NSCLC who are positive for ALK rearrangements (and possibly also to patients with advanced NSCLC who are positive for ROS1 rearrangements – see discussion later in this section). This clear demarcation of patients into those who are appropriate to treat and those who are not appropriate to treat means that crizotinib can usually be regarded as being complimentary to, rather than in direct competition with, biological therapies that target other genetic abnormalities involved in the pathogenesis of NSCLC, such as the first-generation EGFR TKIs, gefitinib and erlotinib. Molecular abnormalities such as rearrangements of ALK and mutations in EGFR or KRAS are virtually [67, 68] (albeit not entirely [69]) mutually exclusive in Western patients with NSCLC; therefore, testing for the presence of these mutations and tailoring therapy accordingly (i.e. the ‘personalized’ approach to treatment – see Sect. 1) is now widely accepted as being standard practice.
Table 7 presents a summary of selected targeted agents (including crizotinib) in the treatment of advanced NSCLC, including their approval status in the EU, where applicable. Several agents, such as the oral, small molecule TKIs dabrafenib, nintedanib and sorafenib, and the monoclonal antibodies necitumumab, ramucirumab and traztuzumab, remain investigational or, in the case of vandetanib (a vascular endothelial growth factor receptor [VEGFR]/EGFR/RET TKI), tivantinib (a MET TKI) and cetuximab (an anti-EGFR monoclonal antibody) have either ceased to be or are not being currently investigated in this indication (Table 7). At present, the anti-VEGF-A monoclonal antibody bevacizumab is the only targeted therapy apart from gefitinib and erlotinib to have gained EU approval for the treatment of advanced NSCLC (Table 7). However, the second-generation EGFR TKI afatinib recently received a positive opinion from the CHMP for the treatment of EGFR TKI-naïve adult patients with EGFR mutation-positive, locally-advanced or metastatic NSCLC [70].
In terms of targeting KRAS mutation-positive NSCLC, the search for a direct inhibitor of KRAS signalling has so far proven unsuccessful [88]. However, inhibitors of signalling downstream from KRAS have also been explored [88]; selumetinib, an oral, small molecule inhibitor of mitogen-activated protein kinase kinases appears to be a promising candidate in this regard [75] (Table 7).
Accepting that crizotinib is the current standard of care for patients with ALK-positive, advanced NSCLC [89], there are three main issues that relate to the use of the drug in clinical practice:
-
Identifying appropriate patients for treatment (i.e. screening);
-
The development of resistance to treatment; and
-
The cost-effectiveness of treatment (including screening).
Ideally, all patients diagnosed with advanced NSCLC should be screened, such that none of the ALK-positive cases who are eligible to receive (and potentially benefit from) crizotinib are missed, even though they represent only a small subset of the total population of patients with advanced NSCLC (≈2–7 %; see Sect. 1). That noted, the vast majority of ALK-positive NSCLCs are adenocarcinomas (e.g. 93–98 % across the three PROFILE studies; see Sect. 4); accordingly, ALK testing should be done primarily (but not exclusively) on adenocarcinomas [90]. ALK rearrangement is also associated with certain clinical features, such as younger age and never/light-smoking history [91]. However, these are not absolute associations [91]; patients with adenocarcinomas who have different demographic characteristics should not be excluded from ALK testing on that basis [90, 92].
Since NSCLCs harbouring EGFR mutations and ALK rearrangements are effectively mutually exclusive (in Western patients), a sequential approach has been proposed, whereby newly diagnosed patients are initially screened for an EGFR mutation (the more common of the two abnormalities); those testing negative in this respect are then screened for the presence of an ALK rearrangement [91, 92]. Spanish guidelines are consistent with this suggestion, while in France and Switzerland, ALK testing is proposed only for patients with adenocarcinoma who have already been found to be KRAS mutation-negative followed by EGFR mutation-negative in that order [93]. With regard to enriching clinical trials with ALK-positive patients, it has been suggested that just over one-third of patients with advanced NSCLC who have tumours with adenocarcinoma histology, and who have never smoked, and who are known to be both KRAS and EGFR mutation-negative, will be ALK-positive [94].
Current approaches to detecting ALK gene rearrangements or the resulting fusion proteins in tumor specimens include fluorescence in-situ hybridization (FISH), reverse transcriptase polymerase chain reaction (RT-PCR) and immunohistochemistry (IHC). Detailed discussion of the relative advantages and disadvantages of each of these companion diagnostic tests is beyond the scope of this article, but is available elsewhere [24, 90, 91, 93, 95].
Briefly, FISH is the gold standard, primarily because it is the only test correlated with clinical response (as a result of its use in the PROFILE clinical trials). However, this technique is time consuming, comparatively costly and requires a level of technical and professional expertise that is not always readily available [24]. RT-PCR is also technically challenging and not in wide usage. In comparison, IHC is a rapid, relatively inexpensive and routine technique, and, as such, has the potential to improve the accessibility and cost-effectiveness of ALK screening [91]. The reported sensitivity and specificity of IHC ALK testing has ranged from 67–100 % and from 93–100 %, respectively (using FISH as the standard procedure) [24, 90]; IHC has a very high negative predictive value (≥98.9 %) [90]. Two ALK monoclonal antibodies in particular, D5F3 (by Ventana/Roche Tissue Diagnostics, Switzerland) and 5A4 (by Novocastra, UK), both of which are commercially available within the EU, are reported to be highly accurate and reliable in predicting ALK rearrangement in NSCLC patients [96, 97].
To a greater or lesser extent, IHC may eventually replace FISH for ALK testing [24]. Several authors have proposed that a two-tiered approach may be appropriate, whereby all patients are initially screened using IHC [92, 93, 95, 96]. Those with faint, moderate or intense staining indicative of ALK gene expression (i.e. IHC score of 1+, 2+ or 3+, respectively, on a scale of 0–3+) are then tested by FISH for confirmation of ALK positivity [92, 93, 96]. Alternatively, only patients with an IHC score of 1+ or 2+ are subjected to confirmatory testing by FISH, while those with an IHC score of 3+ are considered ALK-positive (and are therefore not retested, theoretically reducing costs) [95]. In both algorithms, patients with no staining indicative of ALK gene expression (i.e. IHC score of 0) are considered ALK-negative and are therefore not retested [93, 95, 96]. Such approaches do, however, require clinical validation in large-scale studies [90].
The EU SPC for crizotinib [25] does not specify that a particular diagnostic test for ALK rearrangement must be used, in contrast to the US prescribing information for the drug [38], which states that an FDA-approved test must be used.
As noted earlier in this section, not all ALK-positive patients respond to treatment with crizotinib (i.e. their tumours display intrinsic or primary resistance). Moreover, as has been observed with other targeted therapies (e.g. EGFR TKIs), patients that do respond almost invariably become resistant to the drug (i.e. their tumours develop acquired or secondary resistance), leading to disease progression [98–100]. Consistent with the limited penetration of the blood-brain barrier by crizotinib (see Sect. 3), the CNS is a common site of disease progression in crizotinib-treated patients with ALK-positive NSCLC [61, 101, 102]. That noted, among 613 patients with advanced, ALK-positive NSCLC who had no detectable brain metastases at baseline, only 55 (9 %) developed symptomatic brain metastases after starting crizotinib treatment, according to a recently published retrospective analysis of the PROFILE 1005 and PROFILE 1007 studies [103]. Of the remaining 275 patients that were included in this analysis, 109 and 166 had, respectively, previously untreated and previously treated asymptomatic brain metastases at baseline [103]. At week 12, the intracranial disease control rate (DCR) and intracranial ORR were 56 and 7 %, respectively, in previously untreated patients, as compared with 62 and 7 %, respectively, among previously treated patients. The overall intracranial DCR in patients with brain metastases at baseline (≈60 % at week 12) was similar to the systemic DCR in patients with or without brain metastases at baseline [103]. Prospective studies may help to determine if, compared with other systemic therapies, crizotinib can delay or prevent the natural occurrence or progression of brain metastases in patients with advanced, ALK-positive NSCLC [103].
Mechanisms underlying acquired resistance to TKIs fall into three general categories: (i) secondary mutation of the target RTK; (ii) gene amplification or overexpression of the target RTK; and (iii) compensatory upregulation of another RTK (oncogenic driver) – either in the same or in different tumour cells – that signals through the same or through a different downstream pathway [98, 99]. Secondary mutations within the tyrosine kinase domain of the EML4-ALK rearrangement that confer resistance to crizotinib include L1196M [104], C1156Y [104], L1152R [105], G1269A [98], F1174C [106] and D1203N [106]. In one case series [106], six (40 %) of 15 evaluable crizotinib-treated patients with ALK-positive NSCLC who experienced (extra-CNS) progression demonstrated one such point mutation on biopsy. Two patients (including one with a point mutation) exhibited new-onset ALK gene copy number gain and four demonstrated the presence of another oncogenic driver (KRAS or EGFR), with or without a persistent ALK rearrangement. Three retained ALK positivity with no identifiable resistance mechanism [106]. In vitro, concurrent (‘bypass’) signalling mediated by human epidermal growth factor (HER)/EGFR has been observed in cell lines established from patients with EML4-ALK-positive NSCLC who have acquired resistance to crizotinib [105, 107]. Given the potential for multiple different mechanisms of resistance to occur, rebiopsying and reanalysing crizotinib-refractory tumours might become central to the process of selecting a subsequent therapeutic strategy [98, 99].
The above notwithstanding, the majority (≈60 %) of PROFILE 1001 or PROFILE 1005 participants with investigator-defined PD on crizotinib have continued to receive the drug because of reasonable evidence of ongoing clinical benefit in the investigator's opinion [102, 108]. Indeed, the results of a recent retrospective analysis suggested that, among patients who experienced PD on crizotinib (n = 194), those who continued to receive the drug (n = 120) had a significant improvement in OS from the time of PD (median 16.4 vs. 3.9 months; HR 0.27; 95 % CI 0.17, 0.45; p < 0.0001), as well as from the time of initial crizotinib treatment (median 29.6 vs. 10.8 months; HR 0.28; 95 % CI 0.18, 0.44; p < 0.0001), compared with those who did not continue to receive the drug (n = 74) [108]. Prolonged PFS on initial crizotinib treatment, good ECOG performance status at the time of PD, and PD in the brain and/or bone were common clinicopathological characteristics in patients who benefitted from continuing crizotinib treatment beyond PD [108].
Current standard practice at the time of PD (e.g. while receiving crizotinib) is to administer cytotoxic chemotherapy for systemic metastasis and/or palliative radiotherapy for CNS metastasis [109–111]. An alternative strategy has been proposed for patients with ALK-positive NSCLC who progress while on crizotinib, either within the CNS and/or at limited systemic sites (oligoprogressive disease), namely continuation of crizotinib following local ablative therapy of the oligoprogressive disease [110, 112]. It is also interesting to note that there is a report of a patient with ALK-positive NSCLC responding to retreatment with crizotinib (this individual having previously discontinued the drug due to the development of acquired resistance and, in the interim, tried [two] other treatments unsuccessfully) [111]. This phenomenon, in which a temporary cessation of treatment after the development of drug resistance (‘drug holiday’) appears to lead to the regaining of drug sensitivity, has also been observed with the EGFR TKI erlotinib [113].
The activity of second-generation ALK inhibitors in patients with crizotinib-resistant ALK-positive NSCLC is currently being assessed in ongoing studies [55, 56]. In one of these investigations [55], the ORR to LDK378 was 60 % among 78 evaluable patients with or without crizotinib-resistant disease [55]; it was 60 % in the subset of 64 patients with crizotinib-resistant disease [114]. As such, LDK378 represents a potentially promising treatment strategy for patients who relapse on crizotinib.
Novel targeted anticancer therapies are often expensive and offer low cost effectiveness [115]. On the other hand, while per-patient test and therapy costs are relatively high, the overall budget impact is very likely comparatively low, given the low prevalence of ALK gene rearrangement (≈2–7 % of patients; see Sect. 1), thus presenting public and private payers with a challenging policy decision [24]. Recently, the National Institute for Health and Clinical Excellence (NICE) in the UK issued a final appraisal determination not recommending the use of crizotinib (within the National Health Service [NHS]) in patients with previously treated, ALK-positive, advanced NSCLC, on the grounds that it did not represent cost-effective use of NHS resources [116]. NICE appraisal committees normally recommend treatments that cost around £20,000–30,000 per quality-adjusted life-year (QALY) gained or less, or, as history has shown, up to around £50,000 per QALY gained in the case of drugs that meet NICE’s supplementary criteria for life-extending end-of-life treatments [117]. In this instance, the relevant committee concluded that, notwithstanding the drug was a clinically efficacious treatment for ALK-positive NSCLC that met the end-of-life criteria, the cost per QALY gained was >£100,000 for crizotinib compared with docetaxel and >£50,200 for crizotinib compared with best supportive care. These incremental cost-effectiveness ratios (ICERs) were based on a model submitted by the manufacturer that incorporated estimates of treatment effectiveness (PFS and OS) from the PROFILE 1007 and PROFILE 1005 studies and included a patient access scheme. However, as with all pharmacoeconomic analyses, this model is subject to limitations, the major one being the uncertainty surrounding the exact magnitude of the OS gain with crizotinib versus chemotherapy (and therefore of the resulting ICER), due to the lack of mature OS data from PROFILE 1007 and PROFILE 1005 and the confounding impact of chemotherapy recipients crossing-over to crizotinib in PROFILE 1007 (see discussion earlier in this section) [116]. Any future (re)appraisal of crizotinib by NICE will likely involve the submission by the manufacturer of a revised cost-effectiveness model that incorporates more mature (and therefore more reliable) OS data from PROFILE 1007, once available.
Assessments of the cost-effectiveness of crizotinib (or any other targeted therapy) should also address the cost of detecting genomic marker-positive patients [94]. In this regard, a generalized model specifically developed to evaluate joint companion diagnostics and associated targeted therapies has been used to compare health economic and outcome results (per person tested) with various ALK screening strategies, adopting a payer perspective in France [24]. The strategies of ‘reflex IHC to FISH’ (i.e. FISH confirmation of IHC-positive cases) and ‘enrichment’ (i.e. FISH performed in EGFR mutation- and KRAS mutation-negative cases) were similar in terms of test cost (€106 and 107, respectively); both strategies were associated with a lower total cost (i.e. test cost plus [crizotinib] therapy cost) relative to ‘IHC [using] D5F3’, a strategy with a lower test cost (€94) [€2,950 and 2,852 vs. 3,261]. Moreover, the reflex IHC to FISH and enrichment approaches yielded more QALYs (0.0142 and 0.0137 vs. 0.0114) and lower cost per QALY gained estimates (€207, 600 and 207, 953 vs. 285, 684) than the IHC using D5F3 approach [24]. In comparison, test and total costs for a fourth strategy (a ‘gold standard’ test assumed to be perfectly accurate at identifying ALK rearrangement) were €150 and €2995, respectively. This testing strategy yielded 0.0142 QALYs and a cost per QALY gained of €210,709. The cost-effectiveness of each strategy was particularly sensitive to the cost-effectiveness of crizotinib therapy in general (i.e. crizotinib therapy costs accounted for >95 % of the total costs) and also to the specificity of the test strategy [24]. No other economic analyses of crizotinib in EU countries appear to be available at this time.
Despite sharing a similar biological defect, predominant histology and patient demographic profile, ROS1 and ALK rearrangements in NSCLC appear to be mutually exclusive [18]. ROS1 rearrangements are also slightly less common than ALK rearrangements (see Sect. 1). Although ROS1 and ALK share only ≈50 % amino acid sequence homology in the kinase domain, several ALK inhibitors, including crizotinib, have demonstrated in vitro inhibitory activity against ROS1 [31] (see Sect. 2). The efficacy of crizotinib in the treatment of ROS1-rearranged, advanced NSCLC is being investigated in an expansion cohort of PROFILE 1001; preliminary findings from this trial suggest that the drug (at a dosage of 250 mg twice daily) is an effective therapy in this genomic subset of patients [118]. Briefly, 35 of 40 patients with ROS1-positive, advanced NSCLC (median age 51 years; 80 % never smokers; 98 % adenocarcinoma histology; 0–6 prior treatments) were evaluable for response at the time of data cut-off. The ORR was 60 % (including 2, 19 and 10 patients with complete response, partial response and stable disease, respectively); the 8- and 16-week systemic DCRs were 80 and 66 %, respectively. Median PFS had not been reached; however, the 6-month PFS probability was 76 % [118]. Crizotinib is not approved for the treatment of ROS1-rearranged, advanced NSCLC in the EU; while this is also true in the US, NCCN guidelines from that country specify that ROS1-positive patients may be treated with crizotinib [64].
In conclusion, crizotinib is the current standard of care in terms of the treatment of ALK-positive, advanced NSCLC; while the current EU approval is for second (or subsequent)-line use only, the first-line use of the drug is being evaluated in ongoing phase III studies. Key issues relating to the use of crizotinib in clinical practice include identifying the small subset of eligible patients, the invariable development of resistance and the high cost of treatment.
Data selection sources:
Relevant medical literature (including published and unpublished data) on crizotinib was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 31 October 2013], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Crizotinib, non-small cell lung cancer, carcinoma, non-small cell lung, lung non small cell cancer, NSCLC.
Study selection: Studies in patients with previously treated, anaplastic lymphoma kinase-positive NSCLC who received crizotinib. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
International Agency for Research on Cancer. GLOBOCAN 2008: estimated cancer incidence, mortality, prevalence and disability-adjusted life years (DALYs) worldwide in 2008. http://globocan.iarc.fr/. Accessed 31 Jul 2013.
D’Addario G, Fruh M, Reck M, et al. Metastatic non-small-cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v116–9.
Ozkaya S, Findik S, Dirican A, et al. Long-term survival rates of patients with stage IIIB and IV non-small cell lung cancer treated with cisplatin plus vinorelbine or gemcitabine. Exp Ther Med. 2012;4(6):1035–8.
Bonanno L, Favaretto A, Rugge M, et al. Role of genotyping in non-small cell lung cancer treatment: current status. Drugs. 2011;71(17):2231–46.
Felip E, Cedres S, Checa E, et al. How to integrate current knowledge in selecting patients for first line in NSCLC? Ann Oncol. 2010;21(Suppl 7):vii230–3.
Larsen JE, Cascone T, Gerber DE, et al. Targeted therapies for lung cancer: clinical experience and novel agents. Cancer J. 2011;17(6):512–27.
Pao W, Girard N. New driver mutations in non-small-cell lung cancer. Lancet Oncol. 2011;12(2):175–80.
Thomas R, Wolf J. Personalized therapy of lung cancer. Onkologie. 2012;35(Suppl 1):14–9.
Vadakara J, Borghaei H. Personalized medicine and treatment approaches in non-small-cell lung carcinoma. Pharmgenomics Pers Med. 2012;5:113–23.
Villaruz LC, Socinski MA. Personalized therapy for non-small cell lung cancer: which drug for which patient? Semin Thorac Cardiovasc Surg. 2011;23(4):281–90.
Vincent MD, Kuruvilla MS, Leighl NB, et al. Biomarkers that currently affect clinical practice: EGFR, ALK, MET. KRAS. Curr Oncol. 2012;19(Suppl 1):S33–44.
Rafael Sierra J, Tsao M-S. c-MET as a potential therapeutic target and biomarker in cancer. Ther Adv Med Oncol. 2011;3(Suppl 1):S21–S35.
Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363(18):1693–703.
Cardarella S, Ogino A, Nishino M, et al. Clinical, pathological and biological features associated with BRAF mutations in non-small cell lung cancer. Clin Cancer Res. 2013;19(16):4532–40.
Peters S, Michielin O, Zimmermann S. Dramatic response induced by vemurafenib in a BRAF V600E-mutated lung adenocarcinoma. J Clin Oncol. 2013;31(20):e341–4.
Mazières J, Peters S, Lepage B, et al. Lung cancer that harbors an HER2 mutation: epidemiologic characteristics and therapeutic perspectives. J Clin Oncol. 2013;31(16):1997–2003.
Lipson D, Capelletti M, Yelensky R, et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nat Med. 2012;18(3):382–4.
Bergethon K, Shaw AT, Ou SHI, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–70.
Davies KD, Le AT, Theodoro MF, et al. Identifying and targeting ROS1 gene fusions in non-small cell lung cancer. Clin Cancer Res. 2012;18(17):4570–9.
Minoo P, Wang H-Y. ALK-immunoreactive neoplasms. Int J Clin Exp Pathol. 2012;5(5):397–410.
Chiarle R, Voena C, Ambrogio C, et al. The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat Rev Cancer. 2008;8(1):11–23.
Curran MP. Crizotinib: in locally advanced or metastatic non-small cell lung cancer. Drugs. 2012;72(1):99–107.
Ou SHI. Crizotinib: a novel and first-in-class multitargeted tyrosine kinase inhibitor for the treatment of anaplastic lymphoma kinase rearranged non-small cell lung cancer and beyond. Drug Des Devel Ther. 2011;5:471–85.
Lee JA, Bubendorf L, Stahel RA, et al. Testing for anaplastic lymphoma kinase rearrangement to target crizotinib therapy: oncology, pathology and health economic perspectives. Expert Rev Anticancer Ther. 2013;13(5):625–36.
Pfizer Limited. Xalkori 200 mg hard capsules: EU summary of product characteristics. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002489/WC500134759.pdf. Accessed 3 Jul 2013.
Zou HY, Li Q, Lee J, et al. Antitumor efficacy of crizotinib (PF-02341066), a potent and selective ALK and c-Met RTK inhibitor, in EML4-ALK driven NSCLC tumors in vitro and in vivo [abstract no. LB-390]. 102nd Annual Meeting of the American Association for Cancer Research; 2–6 Apr 2011; Orlando (FL).
Zou HY, Li Q, Lee JH, et al. An orally available small-molecule inhibitor of c-Met, PF-2341066, exhibits cytoreductive antitumor efficacy through antiproliferative and antiangiogenic mechanisms. Cancer Res. 2007;67(9):4408–17.
Sun Y, Nowak KA, Zaorsky NG, et al. ALK inhibitor PF02341066 (crizotinib) increases sensitivity to radiation in non-small cell lung cancer expressing EML4-ALK. Mol Cancer Ther. 2013;12(5):696–704.
Yasuda H, de Figueiredo-Pontes LL, Kobayashi S, et al. Preclinical rationale for use of the clinically available multitargeted tyrosine kinase inhibitor crizotinib in ROS1-translocated lung cancer. J Thorac Oncol. 2012;7(7):1086–90.
Tanizaki J, Okamoto I, Okamoto K, et al. MET tyrosine kinase inhibitor crizotinib (PF-02341066) shows differential antitumor effects in non-small cell lung cancer according to MET alterations. J Thorac Oncol. 2011;6(10):1624–31.
Ou SHI, Tan J, Yen Y, et al. ROS1 as a ‘druggable’ receptor tyrosine kinase: lessons learned from inhibiting the ALK pathway. Expert Rev Anticancer Ther. 2012;12(4):447–56.
Bang YJ. The potential for crizotinib in non-small cell lung cancer: a perspective review. Ther Adv Med Oncol. 2011;3(6):279–91.
Christensen JG, Zou HY, Arango ME, et al. Cytoreductive antitumor activity of PF-2341066, a novel inhibitor of anaplastic lymphoma kinase and c-Met, in experimental models of anaplastic large-cell lymphoma. Mol Cancer Ther. 2007;6(12 Pt. 1):3314–22.
Yamazaki S, Vicini P, Shen Z, et al. Pharmacokinetic/pharmacodynamic modeling of crizotinib for anaplastic lymphoma kinase inhibition and antitumor efficacy in human tumor xenograft mouse models. J Pharmacol Exp Ther. 2012;340(3):549–57.
Tumati V, Kumar S, Yu L, et al. Effect of PF-02341066 and radiation on non-small cell lung cancer cells. Oncol Rep. 2013;29(3):1094–100.
Li C, Alvey C, Bello A, et al. Pharmacokinetics (PK) of crizotinib (PF-02341066) in patients with advanced non-small cell lung cancer (NSCLC) and other solid tumors. J Clin Oncol. 2011;29(Suppl; abstract no. e13065).
Johnson TR, Goulet L, Smith EB, et al. Metabolism, excretion and pharmacokinetics of [14C]crizotinib following oral administration to healthy subjects [abstract no. P83]. Drug Metab Rev. 2011;43:77.
Pfizer Inc. XALKORI® (crizotinib) capsules, oral. US prescribing information. 2013. http://labeling.pfizer.com/showlabeling.aspx?id=676. Accessed 3 Jul 2013.
Costa DB, Kobayashi S, Pandya SS, et al. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J Clin Oncol. 2011;29(15):e443–5.
Tan W, Wilner KD, Bang YJ, et al. Pharmacokinetics of PF-02341066, a dual ALK/MET inhibitor after multiple oral doses to advanced cancer patients. J Clin Oncol. 2010;28 (Suppl; abstract no. 2596).
Wang E, Nickens D, Bello A, et al. Clinical implication of a population pharmacokinetic analysis of XALKORI (crizotinib) in 1,182 patients with non-small cell lung cancer (NSCLC) and 32 patients with other solid tumors [abstract no. MO07.04 plus oral presentation]. International Association for the Study of Lung Cancer, 15th World Conference on Lung Cancer; 27–30 Oct 2013; Sydney.
Nishio M, Hirsh V, Kim D-W, et al. Efficacy, safety, and patient-reported outcomes (PROs) with crizotinib versus chemotherapy in Asian patients in a phase III study of previously treated advanced ALK-positive non-small cell lung cancer (NSCLC) [abstract no. O16.05 plus oral presentation]. International Association for the Study of Lung Cancer, 15th World Conference on Lung Cancer; 27–30 Oct 2013; Sydney.
Hirsh V, Blackhall FH, Kim D-W, et al. Impact of crizotinib on patient-reported symptoms and quality of life (QOL) compared with single-agent chemotherapy in a phase III study of advanced ALK + non-small cell lung cancer. J Clin Oncol. 2013;31(Suppl; abstract no. 8108).
Shaw AT, Kim DW, Nakagawa K, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368(25):2385–94.
Pfizer Limited. An investigational drug, PF-02341066 is being studied versus standard of care in patients with advanced non-small cell lung cancer with a specific gene profile involving the anaplastic lymphoma kinase (ALK) gene [ClinicalTrials.gov identifier NCT00932893]. US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/ct2/show/results/NCT00932893. Accessed 3 Jul 2013.
European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP). CHMP assessment report: Xalkori. International non-proprietary name: crizotinib. Procedure no. EMEA/H/C/002489. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002489/WC500134761.pdf. Accessed 3 Jul 2013.
Hida T, Shi Y, Ahn MJ, et al. Exploratory subgroup analysis of crizotinib efficacy and safety in Asian and non-Asian patients with advanced ALK-positive non-small cell lung cancer (NSCLC) enrolled in a global phase II study [abstract]. J Thorac Oncol. 2012;7(11 Suppl 5):S454–5.
Schnell P, Safferman AZ, Bartlett CH, et al. Clinical presentation of hepatotoxicity-associated crizotinib in ALK-positive (ALK+) advanced non-small cell lung cancer (NSCLC). J Clin Oncol. 2012;30(Suppl; abstract no. 7598).
Salgia R, Solomon BJ, Shaw AT, et al. Visual effects in anaplastic lymphoma kinase (ALK)-positive advanced non-small cell lung cancer (NSCLC) patients treated with crizotinib. J Clin Oncol. 2012;30(Suppl; abstract no. 7596).
Ou SHI, Tong WP, Azada M, et al. Heart rate decrease during crizotinib treatment and potential correlation to clinical response. Cancer. 2013;119:1969–75.
Weickhardt AJ, Rothman MS, Salian-Mehta S, et al. Rapid-onset hypogonadism secondary to crizotinib use in men with metastatic nonsmall cell lung cancer. Cancer. 2012;118(21):5302–9.
Weickhardt AJ, Doebele RC, Purcell WT, et al. Symptomatic reduction in free testosterone levels secondary to crizotinib use in male cancer patients. Cancer. 2013;119(30):2383–90.
Shaw AT, Solomon BJ, Mok T, et al. Effect of treatment duration on incidence of adverse events (AEs) in a phase III study of crizotinib versus chemotherapy in advanced ALK-positive non-small cell lung cancer (NSCLC) [abstract no. P2.11-041 plus poster]. International Association for the Study of Lung Cancer, 15th World Conference on Lung Cancer; 27–30 Oct 2013; Sydney.
Nelson R. Crizotinib receives conditional marketing approval in Europe. 2012. http://www.medscape.com/viewarticle/773280. Accessed 22 Aug 2013.
Novartis International AG. Novartis breakthrough therapy LDK378 shows a marked clinical response in patients with ALK+ non-small cell lung cancer [media release]. 3 June 2013. http://hugin.info/134323/R/1706664/565008.pdf.
Seto T, Kiura K, Nishio M, et al. CH5424802 (RO5424802) for patients with ALK-rearranged advanced non-small-cell lung cancer (AF-001JP study): a single-arm, open-label, phase 1-2 study. Lancet Oncol. 2013;14:590–8.
Nakagawa K, Kiura K, Nishio M, et al. A phase I/II study with a highly selective ALK inhibitor CH5424802 in ALK-positive non-small cell lung cancer (NSCLC) patients: updated safety and efficacy results from AF-001JP. J Clin Oncol. 2013;31(Suppl; abstract no. 8033).
Camidge DR, Bazhenova L, Salgia R, et al. First-in-human dose-finding study of the ALK/EGFR inhibitor AP26113 in patients with advanced malignancies: updated results. J Clin Oncol. 2013;31(Suppl; abstract no. 8031).
Socinski MA, Goldman J, El-Hariry I, et al. A multicenter phase II study of ganetespib monotherapy in patients with genotypically defined advanced non-small cell lung cancer. Clin Cancer Res. 2013;19(11):3068–77.
Sequist LV, Gettinger S, Senzer NN, et al. Activity of IPI-504, a novel heat-shock protein 90 inhibitor, in patients with molecularly defined non-small-cell lung cancer. J Clin Oncol. 2010;28(33):4953–60.
Camidge DR, Bang Y-J, Kwak EL, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011–9.
Crinò L, Kim D-W, Riely GJ, et al. Initial phase 2 results with crizotinib in advanced ALK-positive non-small cell lung cancer (NSCLC): PROFILE 1005. Proc Am Soc Clin Oncol 2011;29(Suppl; abstract no. 7514).
Shaw AT, Yeap BY, Solomon BJ, et al. Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 2011;12(11):1004–12.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines): non-small cell lung cancer. Version 2. 2013. http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 20 Aug 2013.
Pfizer. A clinical trial testing the efficacy of crizotinib versus standard chemotherapy pemetrexed plus cisplatin or carboplatin in patients with ALK positive non squamous cancer of the lung (PROFILE 1014) [ClinicalTrials.gov identifier NCT01154140]. US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/show/NCT01154140. Accessed 19 Aug 2013.
Pfizer. A study of crizotinib versus chemotherapy in previously untreated East Asian non-small cell lung cancer patients [ClinicalTrials.gov identifier NCT01639001]. US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/show/NCT01639001. Accessed 19 Aug 2013.
Gainor JF, Varghese AM, Ou SHI, et al. ALK rearrangements are mutually exclusive with mutations in EFGR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin Cancer Res. 2013;19(15):4273–81.
Shaw A, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27(26):4247–53.
Kris MG, Johnson BE, Kwiatkowski A, et al. Identification of driver mutations in tumor specimens from 1,000 patients with lung adenocarcinoma: the NCI’s Lung Cancer Mutation Consortium (LCMC). J Clin Oncol. 2011;29(Suppl; abstract no. CRA7506).
Boehringer Ingelheim. Afatinib receives positive CHMP opinion for patients with EGFR mutation positive lung cancer in European Union [media release]. 26 July 2013. http://www.boehringer-ingelheim.com/news/news_releases/press_releases/2013/26_july_2013_oncology.html.
GlaxoSmithKline. A phase II study of the selective BRAF kinase inhibitor GSK2118436 in subjects with advanced non-small cell lung cancer and BRAF mutations [ClinicalTrials.gov identifier NCT01336634]. US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/ct2/show/NCT01336634. Accessed 12 Sep 2013.
Roche. Tarceva 25 mg film-coated tablets. EU summary of product characteristics. 2010. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000618/WC500033994.pdf. Accessed 20 Aug 2013.
AstraZeneca AB. IRESSA 250 mg film-coated tablets. EU summary of product characteristics. 2009. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001016/WC500036358.pdf. Accessed 20 Aug 2013.
Boehringer Ingelheim. LUME-Lung 1: nintedanib plus chemotherapy extends the life of lung cancer patients with adenocarcinoma [media release]. 3 June 2013. http://www.boehringer-ingelheim.com/news/news_releases/press_releases/2013/03_june_2013_oncology.html.
Janne PA, Shaw AT, Pereira JR, et al. Selumetinib plus docetaxel for KRAS-mutant advanced non-small-cell lung cancer: a randomized, multicentre, placebo-controlled, phase 2 study. Lancet Oncol. 2013;14(1):38–47.
Metro G, Minotti V, Crino L. Years of sorafenib investigation in advanced non-small cell lung cancer: is there a ‘NExUS’ linking an unsuccessful treatment and a potentially active one? J Thorac Dis. 2012;4(6):635–8.
European Society for Medical Oncology. ESMO 2012 press release: phase III MISSION trial. Sorafenib does not extend overall survival as third or fourth line therapy in lung cancer, EGFR status may help select patients who will benefit most. http://www.esmo.org/Conferences/Past-Conferences/ESMO-2012-Congress/News-Press-Releases/ESMO-2012-Press-Releases/Phase-III-MISSION-trial. Accessed 20 Aug 2013.
ArQule Inc. ArQule and Daiichi Sankyo announce discontinuation of phase 3 MARQUEE clinical trial in non-small cell lung cancer [media release]. 2 October 2012. http://investors.arqule.com/releasedetail.cfm?ReleaseID=710618.
Platt A, Elvin P, Morten J, et al. Retrospective evaluation of RET biomarker status and outcome to vandetanib in four phase III randomized NSCLC trials. J Clin Oncol. 2013;31 (Suppl; abstract no. 8045).
Langer CJ, Mok T, Postmus PE. Targeted agents in the third-/fourth-line treatment of patients with advanced (stage III/IV) non-small cell lung cancer (NSCLC). Cancer Treat Rev. 2013;39(3):252–60.
Roche. Avastin 25 mg/ml concentrate for solution for infusion. EU summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000582/WC500029271.pdf. Accessed 20 Aug 2013.
Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomized phase III trial. Lancet. 2009;373(9764):1525–31.
European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP). Assessment report for erbitux. International non-proprietary name/common name: cetuximab. Procedure no. EMEA/H/C/558/II/0029. 2010. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000558/WC500075683.pdf. Accessed 20 Aug 2013.
European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP). Merck KGaA withdraws its application for an extension of the indication for Erbitux (cetuximab) [press release] 19 Sep 2012. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000558/wapp/Post-authorisation/human_wapp_000145.jsp&mid=WC0b01ac058001d128.
Eli Lilly and Company. Lilly announces phase III necitumumab study meets primary endpoint of overall survival [media release]. 13 Aug 2013. http://newsroom.lilly.com/releasedetail.cfm?releaseid=784772.
Eli Lilly and Company. Lilly releases phase II results for monoclonal antibody ramucirumab in lung cancer [media release]. 29 September 2012. http://newsroom.lilly.com/releasedetail.cfm?releaseid=710172.
Eli Lilly and Company. A study of chemotherapy and ramucirumab vs. chemotherapy alone in second line non-small cell lung cancer participants who received prior first line platinum based chemotherapy [ClinicalTrials.gov identifier NCT01168973]. US National Institutes of Health, ClinicalTrials.gov. 2013. http://clinicaltrials.gov/show/NCT01168973. Accessed 20 Aug 2013.
Villaflor VM, Salgia R. Targeted agents in non-small cell lung cancer therapy: what is there on the horizon? J Carcinog. 2013;12:7. Available from: http://www.carcinogenesis.com/text.asp?2013/12/1/7/109253.
Casaluce F, Sgambato A, Maione P, et al. ALK inhibitors: a new targeted therapy in the treatment of advanced NSCLC. Target Oncol. 2013;8(1):55–67.
Yi ES, Chung J-H, Kulig K, et al. Detection of anaplastic lymphoma kinase (ALK) gene rearrangement in non-small cell lung cancer and related issues in ALK inhibitor therapy: a literature review. Mol Diagn Ther. 2012;16(3):143–50.
Shaw AT, Solomon B, Kenudson MM. Crizotinib and testing for ALK. J Natl Compr Canc Netw. 2011;9(12):1335–41.
Lindeman NI, Cagle PT, Beasley MB, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8(7):823–59.
Thunnissen E, Bubendorf L, Dietel M, et al. EML4-ALK testing in non-small cell carcinomas of the lung: a review with recommendations. Virchows Arch. 2012;461(3):245–57.
Atherly AJ, Camidge DR. The cost-effectiveness of screening lung cancer patients for targeted drug sensitivity markers. Br J Cancer. 2012;106(6):1100–6.
Weickhardt AJ, Aisner DL, Franklin WA, et al. Diagnostic assays for identification of anaplastic lymphoma kinase-positive non-small cell lung cancer. Cancer. 2013;119(8):1467–77.
Conklin CMJ, Craddock KJ, Have C, et al. Immunohistochemistry is a reliable screening tool for identification of ALK rearrangement in non-small-cell lung carcinoma and is antibody dependent. J Thorac Oncol. 2013;8:45–51.
Martinez P, Hernandez-Losa J, Montero MA, et al. Fluourescent in situ hybridization and immunohistochemistry as diagnostic methods for ALK positive non-small cell lung cancer patients. PLoS ONE. 2013;8(1):e52261. doi:10.1371/journal.pone.0052261.
Doebele RC, Pilling AB, Aisner DL, et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin Cancer Res. 2012;18(5):1472–82.
Voena C, Chiarle R. The battle against ALK resistance: successes and setbacks. Expert Opin Investig Drugs. 2012;21(12):1751–4.
Sasaki T, Janne PA. New strategies for treatment of ALK-rearranged non-small cell lung cancers. Clin Cancer Res. 2011;17(23):7213–8.
Otterson GA, Riely GJ, Shaw AT, et al. Clinical characteristics of ALK + NSCLC patients (pts) treated with crizotinib beyond disease progression (PD): potential implications for management. J Clin Oncol. 2012;30(Suppl; abstract no. 7600).
Ou SHI, Zhou C, Ahn MJ, et al. Treatment of ALK-positive non-small cell lung cancer patients with crizotinib beyond disease progression: Clinical assessment and potential management implications [abstract]. J Thorac Oncol. 2012;7(11 Suppl 5):S446.
Crino L, Ahn MJ, Ou SHI, et al. Clinical experience with crizotinib in patients with advanced ALK-positive non-small cell lung cancer and brain metastases [abstract 3413 plus poster]. European Cancer Congress 2013; 27 Sep–1 Oct 2013; Amsterdam.
Choi YL, Soda M, Yamashita Y, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363:1734–9.
Sasaki T, Koivunen J, Ogino A, et al. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Cancer Res. 2011;71(18):6051–60.
Doebele RC, Aisner DL, Le AT, et al. Analysis of resistance mechanisms to ALK kinase inhibitors in ALK+ NSCLC patients. J Clin Oncol. 2012;30(Suppl; abstract no. 7504).
Tanizaki J, Okamoto I, Okabe T, et al. Activation of HER family signaling as a mechanism of acquired resistance to ALK inhibitors in EML4-ALK-positive non-small cell lung cancer. Clin Cancer Res. 2012;18(22):6219–26.
Ou SHI, Riely GJ, Tang Y, et al. Clinical benefit of continuing crizotinib beyond initial disease progression in patients with advanced ALK-positive non-small-cell lung cancer [abstract no. MO07.01 plus oral presentation]. International Association for the Study of Lung Cancer, 15th World Conference on Lung Cancer; 27–30 Oct 2013; Sydney.
Shaw AT, Solomon B. Anaplastic lymphoma kinase (ALK) fusion oncogene positive non-small cell lung cancer. 2013. http://www.uptodate.com/contents/anaplastic-lymphoma-kinase-alk-fusion-oncogene-positive-non-small-cell-lung-cancer#H4. Accessed 19 Aug 2013.
Takeda M, Okamoto I, Nakagawa K. Clinical impact of continued crizotinib administration after isolated central nervous system progression in patients with lung cancer positive for ALK rearrangement. J Thorac Oncol. 2013;8(5):654–7.
Matsuoka H, Kurata T, Okamoto I, et al. Clinical response to crizotinib retreatment after acquisition of drug resistance. J Clin Oncol. 2013;31(19):e322–3.
Weickhardt AJ, Scheier B, Burke JM, et al. Local ablative therapy of oligoprogressive disease prolongs disease control by tyrosine kinase inhibitors in oncogene-addicted non-small-cell lung cancer. J Thorac Oncol. 2012;7(12):1807–14.
Becker A, Crombag L, Heideman DA, et al. Retreatment with erlotinib: regain of TKI sensitivity following a drug holiday for patients with NSCLC who initially responded to EGFR-TKI treatment. Eur J Cancer. 2011;47(17):2603–6.
Data on file, Pfizer Inc., 2013.
van de Vooren K, Curto A, Garattini L. Optional copayments on anti-cancer drugs. BMJ. 2013;346:f349.
National Institute for Health and Care Excellence. Final appraisal determination: crizotinib for previously treated non-small cell lung cancer associated with an anaplastic lymphoma kinase fusion gene. 2013. http://www.nice.org.uk/nicemedia/live/13639/64900/64900.pdf. Accessed 21 Aug 2013.
National Institute for Health and Care Excellence. NICE consults on new draft recommendations for lung cancer drug [press release]. 26 March 2013. http://www.nice.org.uk/newsroom/pressreleases/CrizotinibACD.jsp. 2013.
Ou SHI, Kim D-W, Camidge DR, et al. Crizotinib therapy for patients with advanced ROS1-rearranged non-small cell lung cancer (NSCLC) [abstract no. MO07.03 plus oral presentation]. International Association for the Study of Lung Cancer, 15th World Conference on Lung Cancer; 27–30 Oct 2013; Sydney.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: S.H. Ou, Chao Family Comprehensive Cancer Center, University of California Irvine Medical Center, Orange, CA, USA; P.E. Postmus, Department of Pulmonary Diseases, VU University Medical Center, Amsterdam, The Netherlands; N. Reinmuth, Department of Thoracic Oncology, Lungenclinic Großhansdorf, Großhansdorf, Germany; R. Rosell, Catalan Institute of Oncology, Hospital Germans Trias i Pujol, Badalona, Spain.
Rights and permissions
About this article
Cite this article
Frampton, J.E. Crizotinib: A Review of Its Use in the Treatment of Anaplastic Lymphoma Kinase-Positive, Advanced Non-Small Cell Lung Cancer. Drugs 73, 2031–2051 (2013). https://doi.org/10.1007/s40265-013-0142-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-013-0142-z