Abstract
In recent years the use of the opioid oxycodone has increased markedly and replacing morphine as the first-line choice of opioid in several countries. There are formulations for oral immediate, oral extended release and intravenous use. The bioavailability is higher than for morphine and less variable. Oxycodone is primarily metabolized in the liver by the cytochrome P450 (CYP) enzymes with CYP3A as the major metabolic pathway and CYP2D6 as the minor metabolic pathway to noroxycodone, oxymorphone and noroxymorphone. Oxycodone exerts its analgesic effect via the µ-opioid receptor. The metabolism of CYP2D6 substrates varies to a large degree between individuals as a result of allele functionality. Poor metabolizers (PM) have two non-functional alleles, extensive metabolizers (EM) are homozygous with two functional alleles or heterozygous with one functional allele and ultrarapid metabolizers (UM) have more than two functional alleles. There are pronounced interethnic differences in the allele distribution. On the basis of studies performed thus far, oxycodone concentrations in comparison with EM are similar in PM and reduced in UM. The pharmacokinetics in UM are insufficiently investigated. Simultaneous inhibition of both CYP3A and CYP2D6 results in increased oxycodone concentrations and such a combination should be avoided. A similar effect is to be expected with use of a CYP3A inhibitor in CYP2D6 PM. Concomitant use of enzyme inducers such as rifampicin, St John’s wort and carbamazepine should be avoided because of the risk of subtherapeutic concentrations of oxycodone. When the dosage of morphine may result in unpredictable bioavailability, like in patients with severe hepatic cirrhosis, oxycodone might be beneficial because it has higher and less variability in bioavailability between patients than morphine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Oxycodone is a semi-synthetic opioid developed from the opium derivative thebaine in 1916 [1]. Today it is marketed in a number of different formulations to be used either as single products or as combinations with other analgesics such as paracetamol (acetaminophen). In North America and also in countries like Australia, Denmark and Sweden, use of oxycodone has increased in recent years [2, 3]. Today oxycodone has replaced morphine as the most used opioid among general practitioners as well as among hospital physicians, e.g. when initiating analgesic therapy in opioid-naïve patients in Odense Healthcare Region in Denmark [2]. Therefore it is not surprising that the international trade of oxycodone has increased 130-fold during the past 20 years, whereas that of morphine has increased only 5-fold [4].
Recently there have been concerns raised that an intense marketing of oxycodone can explain the increased use despite no apparent advantages as an opioid as compared to other compounds [5, 6].
The literature on basic characteristics and clinical use of oxycodone has been growing markedly since early 1990. In particular many studies on the pharmacokinetics, pharmacogenetics and metabolism have been published in last 10 years. Therefore it is timely to summarize the present state of knowledge about pharmacogenetic and drug metabolic facts of importance for the rational use of oxycodone in controlling severe pain [7–24].
2 Literature Search Methodology
A pharmacist with great experience in literature searching (MLA) performed a literature search using PubMed. The used search terms included the MeSH term oxycodone combined with any of the following text words: genetic OR genetics OR pharmacogenetics OR cytochrome OR CYP OR allele OR mutation, interactions OR interacts OR interactions OR interact OR drug interactions, pharmacokinetics OR metabolism OR kinetics. Oxycodone was also searched with the subheadings Blood, Pharmacokinetics, Pharmacodynamics, Metabolism. All titles were reviewed and all relevant articles were read, evaluated and summarized. All articles included in PubMed before 28 January 2013 were evaluated. The quality of the studies on oxycodone varies.
3 Analgesic Characteristics of Oxycodone and its Metabolites
Oxycodone and one of its main metabolites, oxymorphone, present in humans (Fig. 1) are μ-opioid receptor agonists and seem to be as potent as morphine on the basis of studies in rats and after systemic administration [25]. These findings are under debate [26]. It is doubtful if oxycodone and its metabolites have any major κ-agonist activity as reported in a few studies [27]. The potency of μ-opioid receptor binding is in the order of highest for oxymorphone, intermediate for noroxymorphone, lower for oxycodone and very low for noroxycodone [28]. Still most of the analgesic effect of oxycodone is represented by the drug itself because noroxymorphone poorly penetrates into the CNS and the plasma concentrations of oxymorphone are low in man after systemic exposure [10, 28].
A schematic overview of the metabolism of oxycodone and its main metabolites with the major metabolic pathway CYP3A4 and the minor metabolic pathway CYP2D6. The oxycodone metabolism through the CYP3A pathway should represent well over half of the metabolism of oxycodone in most patients. Based in particular on references [7, 8, 10, 11, 24, 28]. The chemical basic structures were downloaded from ChemSpider (http://www.chemspider.com) on 7 October 2012. CYP cytochrome P450
The metabolites oxymorphone and noroxymorphone (the latter also suggested to be a μ-opioid receptor agonist) induce potent experimental analgesia in rats after spinal administration [27, 29, 30]. This is in contrast to the low analgesic potency of oxycodone administered by the spinal route in rats in experimental studies [27]. It is unlikely that noroxymorphone and noroxycodone, another major metabolite in humans, provide major analgesic effects after systemic administration of oxycodone in humans. This is likely to be explained by poor penetration of these two metabolites across the blood–brain barrier [28]. In cancer patients there are no documented relationships between measured plasma concentrations of either oxycodone or its metabolites (oxymorphone or noroxymorphone) and the degree of analgesia or the risk to develop various adverse effects [31].
4 Brief Summary of the Pharmacokinetics and Metabolism of Oxycodone
4.1 Pharmacokinetics
Oxycodone is available in several different preparations for oral immediate, oral extended release and for intravenous use. Basic pharmacokinetic data of oxycodone after intravenous and oral immediate and extended release administration are summarized in Table 1. Recently the active metabolite oxymorphone was registered as oral immediate and oral extended release preparations [32].
Immediate release preparations achieve peak concentrations within a few hours. Oxycodone has apparently higher bioavailability than morphine in the range of 60–90 % owing to less extensive first-pass metabolism than for morphine [33, 34]. Most likely first-pass metabolism occurs in the liver and not in the gastrointestinal tract [10]. This can explain why oxycodone can give slightly higher oral bioavailability when used in severely hepatically ill patients as compared to administration to healthy subjects [1, 10]. The extended release preparations are bioequivalent to immediate release preparations allowing dosing every 12 h [33, 35]. Oxycodone has an apparent volume of distribution around 2–3 L/kg, plasma clearance around 0.8 L/min and a mean terminal elimination half-life around 4 h (varying between 2 and 8 h) in healthy adult subjects [32, 34, 36]. Oxycodone is extensively metabolized with variation between subjects as discussed below (Sects. 4.2, 5.1). In humans, oxycodone is mainly excreted in urine after metabolism with limited amounts of oxycodone excreted as unchanged drug [28, 33]. Systemic exposure of oxycodone after oral administration is about 50–80 % higher in patients above 70 years of age as compared to those of 20–40 years of age [37, 38]. This can be explained by decreased clearance in the elderly group of patients.
In patients with severely decreased kidney functions, the pharmacokinetics of oxycodone varied extensively between patients, with the terminal half-life of oxycodone in the range of 1.8–25.7 h as compared to 1.3–4.0 h in healthy control subjects [39]. The mean elimination half-life was prolonged owing to a combination of increased volume of distribution and reduced clearance. The hydrophilic metabolite noroxycodone had higher concentrations in plasma in the uraemic patients that also had reduced amounts of noroxycodone and oxycodone excreted in urine as compared to the control subjects.
4.2 Metabolism
The metabolism of oxycodone is summarized in Fig. 1. The major metabolic pathway in vivo in man is by N-dealkylation through cytochrome P450 (CYP) 3A, (similar intrinsic clearance for 3A4 and 3A5 in vitro) [10] forming the weak analgesic metabolite noroxycodone [10, 36, 40]. Noroxycodone is further metabolized to noroxymorphone most likely by CYP2D6 [41]. Present data support the notion that CYP3A-mediated metabolism represents well over half of the route for metabolism of oxycodone in man [10]. The minor metabolic pathway of oxycodone is controlled by CYP2D6 by forming the active metabolite oxymorphone available as a drug itself presently [32]. Oxymorphone is further metabolized to noroxymorphone through most likely unknown pathways [28]. The importance of the CYP3A pathway for oxycodone metabolism is shown by an estimated in vitro intrinsic clearance 2- to 14-fold higher for N-dealkylation as compared to O-demethylation through CYP2D6 [10, 28]. As much as 80 % of an oral dose can be recovered in urine as metabolites with about 40 % of an oral dose as conjugated metabolites [28]. Analgesic and non-analgesic effects seem mainly to be mediated by oxycodone because the oxymorphone pathway is of minor importance. This is also supported by the finding that no documented decrease in psychomotor performance was registered in healthy volunteers administered oxycodone in combination with quinidine, a powerful blocking agent of CYP2D6-mediated formation of oxymorphone [10].
5 Variability in Drug Response due to Pharmacogenetics
5.1 Drug Metabolism
Oxycodone is primarily metabolized via CYP3A4/3A5 and to a lesser extent via CYP2D6 (Fig. 1, [10, 28]).
5.1.1 CYP3A-Mediated Metabolism
CYP3A is the dominant pathway for the metabolic elimination of drugs [42]. CYP3A expression is present in the gastrointestinal tract and in the liver, and the enzymatic activity varies up to 40-fold in vitro in both locations. CYP3A-mediated metabolism is multifactorial and is presently understood as complex gene–environmental interactions. The most abundant enzymes in adults include CYP3A4 and CYP3A5 where expression of CYP3A5 activity is strongly influenced by ethnic factors [42].
In a Japanese study of 62 cancer patients the median trough plasma concentration of noroxycodone was lower in CYP3A5*3/*3 subjects compared to *1 and these patients had larger dose escalation, whereas oxycodone and oxymorphone concentrations were not affected for these patients [41]. In the non-escalation group, the given oxycodone dose was lower. This study supports the view that different CYP3A5 alleles can affect needs of oxycodone dosage. The study needs to be confirmed to exclude that the findings are due to bias in the recruitment of patients.
Twelve CYP2D6 EM received placebo, the CYP3A4 inhibitor ketoconazole or the CYP2D6 inhibitor paroxetine before administration of a single oral dose of oxycodone (0.2 mg/kg) [9]. Pretreatment with ketoconazole more than doubled the area under the concentration–time curve (AUC) for oxycodone compared with placebo or paroxetine, supporting the importance of CYP3A4 for oxycodone metabolism.
5.1.2 CYP2D6 Polymorphism
The genetic polymorphism of CYP2D6 causes high interindividual and interethnic variability in the rate of metabolism of CYP2D6 substrates. One classical example is the opioid codeine which requires activation to its active metabolite morphine to exert an analgesic effect [43]. CYP2D6 genotypes are classified according to predicted enzymatic activity into the phenotypes poor metabolizers (PM) with two non-functional alleles, extensive metabolizers (EM) that are homozygous if they have two functional alleles and heterozygous if they have one functional allele and lastly ultrarapid metabolizers (UM) with more than two functional alleles. Sometimes the term intermediate metabolizers (IM) is used, referring to persons with at least one allele with reduced function. If measured by ratios of parent to metabolite concentration, they differ 5- to 15-fold for PM and UM compared with EM [43].
Today more than 100 different CYP2D6 alleles have been identified [44]. The wild-type alleles have full functionality, whereas other alleles have no activity and other alleles have different degrees of decreased activity causing a wide spectrum of activity depending on the combinations of alleles in a specific person. Alleles lacking activity include *3, *4, *5, *6, *7, *8, *11, *12, *13, *14, *15, *18, *19, *20, *21, *31, *38, *40, *42 and *44, whereas alleles with decreased activity include *10, *17, *29, *36 and *41 (Table 2) [43, 44]. The distribution patterns of CYP2D6 alleles differ between ethnic groups. In Caucasians the wild-type allele is the most frequent, followed by *4, and then *10 and *41, the wild-type *1 allele constitutes 35 % in Blacks and *4, *5, *10, *17 and *29 are common, whereas in Asians *10 is far most common (almost 70 %) followed by *5 [43]. Consequently, different outcomes in plasma drug concentrations and therapeutic effects for CYP2D6 substrates can be expected between ethnic groups.
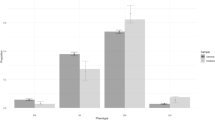
In Caucasians, PM constitute about 7 % of the population, whereas UM are rare and EM the vast majority. There is a north–south geographic gradient for UM (see Fig. 2 [45]), being most prevalent in northern Africa and in the Middle East. In Scandinavia, subjects with duplicated or multiduplicated CYP2D6 alleles constitute about 1 % [46, 47]. In a Swedish man and in his two children the CYP2D6*2 allele had been amplified 12-fold [48]. In a study with subjects from Southern Spain, 7 % had the predicted UM phenotype [49]. This is in contrast to the frequency of 1 % in Northern Europe. In Ethiopians, 29 % had duplicated or multiduplicated CYP2D6 genes [50]. But no more than 5 % in the more southerly country Tanzania [51].
Geographical distribution of CYP2D6 phenotype classes predicted from genotypes. (Reproduced from Sistonen et al. [71], with permission). Similar findings were also presented by Johansson et al. [45]. CYP cytochrome P450, EM extensive metabolizers, IM intermediate metabolizers, PM poor metabolizers, UM ultrarapid metabolizers
In a study of 10 persons, the mean maximum plasma concentration of oxymorphone and noroxymorphone decreased by 62 and 90 % in the two PM/IM compared with the six EM [12]. The mean plasma concentrations of oxymorphone and noroxycodone decreased compared to those in EM subjects. In the two UM, the maximum plasma concentrations of oxymorphone and noroxymorphone increased, whereas noroxycodone exposure was decreased.
5.1.3 CYP2D6 and Dose Requirements of Oxycodone
In a cross-sectional study of 450 cancer patients genotyped for CYP2D6 a total of 27 PM, 413 EM and 10 UM subjects were identified [16]. Oxycodone and noroxycodone plasma concentrations did not differ between phenotypes. PM had lower median plasma concentrations of oxymorphone and noroxymorphone compared with EM. The daily intake of oxycodone did not differ between subjects being PM, EM or UM (70–80 mg/day).
In one study 24 PM and 246 EM patients received intravenous oxycodone for 24 h post-operatively and 5 mg morphine as escape medication [13]. A loading dose of 5 mg oxycodone was given at the end of the surgical procedure; thereafter, an additional 5 mg could be given once or twice and as self-medication of 2 mg oxycodone via a patient-controlled analgesic pump. In PM, the mean plasma concentration of oxymorphone was significantly lower whereas the mean plasma oxycodone concentration was similar compared with those in EM.
Genetic variants did not significantly alter trough plasma concentrations for oxycodone or noroxycodone in 62 Japanese cancer patients administered 5 mg oxycodone twice daily as an initial dose with the possibility of dose escalation. In contrast significantly lower oxymorphone concentrations were detected in the 16 IM compared with the 46 EM [41].
In one study 41 patients undergoing orthopaedic surgery were given a single dose of 5 mg of intravenous oxycodone [52]. The group of two PM and one IM had quite similar concentrations of oxycodone and noroxycodone compared to the 37 EM. The one UM had lower oxycodone and noroxycodone concentrations over time, and the oxymorphone concentration was 2-fold higher.
In a cross-over study of 12 healthy volunteers with different CYP2D6 phenotypes [53], a daily dose of 200 mg of the CYP3A4 inhibitor itraconazole or placebo was administered for 5 days [53]. On the fourth day, oxycodone (0.1 mg/kg) was given. After a wash-out period of 4 weeks, the 5-day dosing was repeated and 10 mg of oxycodone was administered. The authors concluded that the three IM and the one PM had slighter higher oxycodone and noroxycodone and lower oxymorphone AUC than the seven EM both with and without itraconazole. The results were not tested for statistical significance and are not conclusive. The UM appeared to have AUC ratios in the same range as those of the EM.
Plasma concentrations of oxycodone and its oxidative metabolites were measured for 48 h in 11 healthy subjects administered the CYP3A4 inhibitor (and CYP2D6 inhibitor according to the authors) telithromycin (800 mg) or placebo orally for 4 days and given 10 mg of oxycodone on the third day [54]. Telithromycin increased the AUC of oxycodone by 80 % and reduced the AUC of noroxycodone by 46 %. According to the authors, the two UM seemed to have higher oxymorphone, lower oxycodone and noroxycodone AUC values than the nine EM both with and without telithromycin, although the differences were not statistically significant. These data were not presented, only AUC ratios comparing metabolite with oxycodone.
The CYP2D6 substrate nortriptyline (25 mg) was given twice a day for 3 weeks to five UM; in addition the CYP2D6 inhibitor paroxetine was administered after the first week which resulted in increased nortriptyline concentrations, indicating a normalized CYP2D6 metabolic status [55]. Most likely, oxycodone metabolism in UM could be normalized in a similar manner by CYP2D6 inhibitor substances.
5.1.4 Other CYP Enzymes
Repeated administration of oxycodone modified the gene expression of several drug-metabolizing enzymes in rats. Expression of glutathione S-transferase A-5 (rGSTA5) was increased 6.5-fold and that of CYP3A2 was decreased 7-fold, and the protein levels were also affected [56]. There are no in vivo data supporting that long-term administration with oxycodone will diminish the rate of metabolism of other drugs.
5.1.5 Summary
Data on the influence of CYP2D6 genotype on the metabolism of oxycodone and its metabolites are scarce both using in vitro and in vivo approaches. There is no evidence that plasma oxycodone concentrations are affected in PM compared to EM. These results are most likely explained by the large metabolic capacity of CYP3A4 for oxycodone metabolism compensating for the loss of the CYP2D6 pathway, and by a clear reduction of oxymorphone formation and increased noroxycodone that was seen in a study when the CYP2D6 inhibitor quinidine was given [24]. In PM subjects, influence on noroxycodone plasma concentration differs compared with EM subjects, whereas oxymorphone and noroxymorphone concentrations are slightly reduced. It is plausible that the CYP3A4-generated metabolite noroxycodone increases and the CYP2D6-generated metabolite oxymorphone decreases in PM as a larger amount of oxycodone is metabolized through the CYP3A4 pathway (Fig. 1). As expected for UM with their increased CYP2D6 metabolism, oxycodone concentrations are lower compared with EM, whereas oxymorphone concentrations are increased. Further, the plasma concentration of oxycodone and the CYP3A4-generated metabolite noroxycodone is affected by CYP3A4 inhibition and CYP3A4/5 polymorphism, respectively. When CYP3A4 is inhibited, a higher percentage of oxycodone is metabolized via CYP2D6 and in UM higher oxymorphone, lower oxycodone and noroxycodone concentrations are found. For PM subjects, oxycodone and noroxycodone are increased, whereas oxymorphone is decreased.
6 Clinically Important Drug–Drug Interactions
6.1 Induction and Inhibition of the Metabolism of Oxycodone
6.1.1 Alterations in Oxycodone Metabolism and Pharmacological Effects by CYP2D6 Inhibitors
Administration of oxycodone together with potent inhibitors of CYP2D6 such as paroxetine and quinidine does not cause significant alterations of the plasma concentrations of either oxycodone or of the major metabolite noroxycodone [7, 8, 12]. The exposure to the active metabolite oxymorphone is reduced by approximately 44–66 % and the exposure to the noroxymorphone metabolite is also reduced to a minor extent. Several studies have investigated the effect of CYP2D6 inhibitors on the pharmacodynamic effects of oxycodone [7–9, 11] and indicate that inhibition of CYP2D6 does not influence the analgesic efficacy of oxycodone.
6.1.2 CYP3A4 Induction and its Effect on Metabolism of Oxycodone
Induction of CYP3A4 activity may cause drastically decreased plasma concentrations of the substrates of this enzyme [57]. CYP3A4 is expressed in most human tissues and is extensively expressed in the gut and in the liver. The activity of CYP3A4 in the gut is largely responsible for the degradation of substrates decreasing the bioavailability of many drugs [58]. Likewise many drugs that are substrates of CYP3A4 are substrates of the efflux pump P-glycoprotein (P-gp). P-gp transports absorbed drug back to the intestinal lumen and thereby decreases the bioavailability of the substance. Many inducers of CYP3A4 are also inducers of P-gp activity. Drugs metabolized by CYP3A4 and with a low bioavailability are to a large extent biodegraded in the gut [59].
The effect of enzyme induction on the pharmacokinetics of oxycodone was investigated in a study using 600 mg rifampicin taken orally and daily. Both the effect on oral and intravenous oxycodone was studied. The AUC of oral oxycodone decreased by 86 % and the AUC after intravenous dosage decreased by 53 %. The oral bioavailability decreased significantly from 69 to 21 %. The maximum plasma concentration of noroxycodone was increased 2.7-fold after intravenous oxycodone and 2.2-fold when oxycodone was given by the oral route. The AUC of oxymorphone decreased by 90–95 %, whereas the maximum plasma concentration of noroxymorphone increased 2-fold. Five out of 12 subjects had no detectable oxymorphone after rifampicin ingestion [60]. All pharmacodynamic effects of oxycodone were significantly decreased after rifampicin treatment. St John’s wort is known to be a pronounced inducer of CYP3A4 activity causing loss of efficacy of CYP3A4 substrates. In a clinical trial, the AUC of oxycodone (single dose) decreased by 50 % after 14 days of concomitant intake of St John’s wort. The AUC and maximum plasma concentration of noroxycodone were significantly increased, the AUC of oxymorphone decreased by 46 % and the maximum plasma concentration of noroxymorphone increased 1.9-fold. The self-reported drug effect was lower in the St John’s wort phase but no significant change was observed in measured pharmacodynamic effects [61].
In the aforementioned rifampicin study, the pharmacokinetics of oxycodone were investigated after 6 days of rifampicin therapy. It is a shorter time than required to achieve maximal induction which can require weeks of rifampicin treatment [62]. It is therefore possible that the effect may be more pronounced after more days of treatment.
It is likely that drugs inducing the metabolism of oxycodone may cause decreased efficacy of the drug. The interaction could possibly be handled by increasing the oxycodone dose but because the effect and side effects of the metabolites noroxycodone and noroxymorphone are not known the interaction may cause unexpected side effects. Other opioids such as morphine should probably be preferred over oxycodone in patients who are in need of treatment with a CYP3A4 inducer.
Other drugs that are known to induce CYP3A4 and thereby are likely to decrease the efficacy of oxycodone include the enzyme-inducing anticonvulsants (carbamazepine, phenytoin, phenobarbital, primidone) and the non-nucleoside reverse transcriptase inhibitors (NNRTIs) nevirapine and efavirenz [63, 64]. Rifabutin is also an inducer of CYP3A4 but to a lesser extent than rifampicin and could therefore be a better choice in patients in need of rifamycin therapy.
6.1.3 CYP3A4 Inhibition and Alterations in Metabolism of Oxycodone
Several studies have investigated the effect of CYP3A4 inhibitors on the pharmacokinetics of oxycodone [9, 12, 54, 65–68]. All of them have shown that both the maximum plasma concentration and AUC of the parent compound increase. The AUC of oxycodone is about 2- to 3-fold higher when a CYP3A4 inhibitor is administered concomitantly. Maximum plasma concentration is increased by 9–69 %. The increase in oxycodone concentrations is followed by a decrease in the formation of noroxycodone. No uniform effect of CYP3A4 inhibitors on the pharmacokinetics of the active metabolite oxymorphone has been observed. The maximum plasma concentration and AUC have increased in some studies but decreased in others. The concentrations of the metabolites oxymorphone and noroxymorphone decrease when CYP3A4 activity is inhibited. Concomitant use has been associated with higher self-reported pharmacodynamic effects but the effect on the cold pressor test has been small and not observed at all in most studies.
All studies investigating the effect of CYP3A4 inhibitors on the pharmacokinetics and pharmacodynamic effects of oxycodone have been performed in healthy subjects. Oxycodone has been administered in a relatively low dose, 10 mg or 0.2 mg/kg, and only given as a single dose. The influence of CYP3A4 inhibitors on the effect and adverse effects in patients is therefore still unknown. In the published studies the effect of the interaction has been low if seen at all. Retrospectively, cases of coadministration of oxycodone and the CYP3A4 inhibitor voriconazole have been investigated [69]. It was found that adverse effects of oxycodone were observed in 7 out of 9 patients after voriconazole treatment had been added to their ongoing oxycodone treatment. Drowsiness, vomiting and hypopnoea were the most common adverse effects. Voriconazole is expected to be a weak inhibitor of CYP2D6 and may therefore alter the metabolism of oxycodone in another manner than a pure CYP3A4 inhibitor. This is supported by one study [65] that showed that the pharmacokinetics of oxycodone are more and differently altered by voriconazole than shown in studies using other CYP3A4 inhibitors without inhibition of CYP2D6 activity.
The plasma concentrations of oxycodone are markedly increased when both CYP3A4 and CYP2D6 enzyme activities are inhibited. Such situations could occur in patients treated with a CYP2D6 inhibitor, such as fluoxetine, paroxetine, bupropion or terbinafine [63] and in need of treatment with the CYP3A4 inhibitors erythromycin or itraconazole to treat an infection. The pharmacodynamic effects of oxycodone have then been shown to increase in healthy subjects. Since parts of the population lack functional CYP2D6, the pharmacokinetics and pharmacodynamics of oxycodone are expected to be similar in those patients when they are administered a CYP3A4 blocker, thereby exposing them to a risk of severe adverse effects.
6.2 Induction and Inhibition of Drug Metabolism by Oxycodone
No published studies have investigated the effect of oxycodone on the pharmacokinetics of other drugs that are metabolized by CYP3A4 and/or CYP2D6. There is no evidence that oxycodone is an inhibitor of CYP2D6 or CYP3A4 or an inducer of CYP3A4. The capacity of both CYP2D6 and CYP3A4 is high and an interaction caused by competition between substrates is rather uncommon and generally lacks clinical importance with the exception of interactions with some drugs with a narrow therapeutic index. Since CYP3A4 is the main enzyme responsible for oxycodone metabolism and the metabolism by CYP2D6 is less, the risk of a competitive interaction with any CYP2D6 substrate is less likely.
7 Clinical Implications: Importance of Differences in CYP2D6 and CYP3A4 Genotypes for Selection and Treatment with Oxycodone and Handling of Drug–Drug Interactions
CYP2D6 genotypes cause expected differences in pharmacokinetics [13, 14, 16, 41], but they have no major pharmacodynamic consequences or clinical implications [13, 16]. In most studies, CYP2D6 genotypes did not influence the analgesic effect of oxycodone [16] nor dose requirement in a clinically significant way [13, 16, 41], which probably is explained by increased metabolism using the high capacity CYP3A4 pathway when CYP2D6 metabolism is inhibited. However, two of the studies lend some support for oxymorphone having a clinically significant analgesic effect. In one of them, PM had lower pain tolerance in one test and CYP2D6 UM had a tendency towards increased pharmacodynamic effects [11], which is in accordance with the hypothesis that oxymorphone would have a clinically relevant analgesic effect. In the other study, in one of three tests the pain decrease was less in PM compared with EM after administration of oxycodone [14]. In CYP2D6 EM, ketoconazole doubled the AUC of oxycodone and increased its analgesic effect, whereas paroxetine was similar in effect to placebo [9]. The study indicates that CYP3A4, but not CYP2D6, activity is important for oxycodone effect in the individual.
It has not been demonstrated that oxycodone dosage requirement differs between CYP2D6 PM, EM or UM. It is possible that prescription of oxycodone to PM should consist of somewhat higher doses to achieve similar effects as in EM, whereas for UM lower than normal doses would be optimal owing to production of greater amounts of oxymorphone and concomitantly a greater risk of adverse drug reactions. Today, data are too scarce and contradictory to recommend different dosing regimens of oxycodone according to genotype. Instead, the same dosing regimen across genotypes seems plausible. Decreased oxymorphone concentrations do not seem to have any significant clinical impact.
Concomitant administration of drugs inhibiting CYP2D6 activity does not affect oxycodone’s analgesic effect. The use of CYP3A4 inhibitors, such as erythromycin and ketoconazole [63], and oxycodone should to the largest possible extent be avoided as it results in increases in oxycodone exposure, effect and risk of adverse events and the interaction may be clinically important in patients that are CYP2D6 PM. Concomitant use of enzyme inducers such as rifampicin, St John’s wort and carbamazepine should be avoided because of the risk of subtherapeutic concentrations of oxycodone and reduced analgesic effect; in these patients other opioids are a better choice. Oxycodone dosing may as be difficult in patients treated with HIV protease inhibitors or NNRTIs, and other opioids such as morphine may theoretically be easier to titrate.
Oxycodone is a potent opioid agonist with similar effect and adverse effects as morphine but the advantages compared with morphine are not clear. Oxycodone might have some advantages in patients where dosage of morphine might be difficult to titrate because of unpredictable bioavailability as in those with severe hepatic cirrhosis. In conclusion CYP2D6 is not important for the clinical effect of oxycodone. This is in contrast to CYP3A4, but not surprising as it is the major metabolic pathway for oxycodone.
References
Kalso E. Oxycodone. J Pain Symptom Manage. 2005;29(5 Suppl):S47–56.
Poulsen KK, Andersen SE, Moreno SI, et al. General practitioners’ and hospital physicians’ preference for morphine or oxycodone as first-time choice for a strong opioid: a National Register-based study. Basic Clin Pharmacol Toxicol. 2013;112(2):110–5.
Roxburgh A, Bruno R, Larance B, et al. Prescription of opioid analgesics and related harms in Australia. Med J Aust. 2011;195(5):280–4.
The International Narcotics Control Board. Availability of Internationally controlled drugs: ensuring adequate access for medical and scientific purposes. 2011. http://www.incb.org/documents/Publications/AnnualReports/AR2010/Supplement-AR10_availability_English.pdf. Accessed 10 Nov 2012.
Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health. 2009;99(2):221–7.
Lexchin J, Kohler JC. The danger of imperfect regulation: oxycontin use in the United States and Canada. Int J Risk Saf Med. 2011;23(4):233–40.
Gronlund J, Saari TI, Hagelberg NM, et al. Effect of inhibition of cytochrome P450 enzymes 2D6 and 3A4 on the pharmacokinetics of intravenous oxycodone: a randomized, three-phase, crossover, placebo-controlled study. Clin Drug Investig. 2011;31(3):143–53.
Gronlund J, Saari TI, Hagelberg NM, et al. Exposure to oral oxycodone is increased by concomitant inhibition of CYP2D6 and 3A4 pathways, but not by inhibition of CYP2D6 alone. Br J Clin Pharmacol. 2010;70(1):78–87.
Kummer O, Hammann F, Moser C, et al. Effect of the inhibition of CYP3A4 or CYP2D6 on the pharmacokinetics and pharmacodynamics of oxycodone. Eur J Clin Pharmacol. 2011;67(1):63–71.
Lalovic B, Phillips B, Risler LL, et al. Quantitative contribution of CYP2D6 and CYP3A to oxycodone metabolism in human liver and intestinal microsomes. Drug Metab Dispos. 2004;32(4):447–54.
Samer CF, Daali Y, Wagner M, et al. Genetic polymorphisms and drug interactions modulating CYP2D6 and CYP3A activities have a major effect on oxycodone analgesic efficacy and safety. Br J Pharmacol. 2010;160(4):919–30.
Samer CF, Daali Y, Wagner M, et al. The effects of CYP2D6 and CYP3A activities on the pharmacokinetics of immediate release oxycodone. Br J Pharmacol. 2010;160(4):907–18.
Zwisler ST, Enggaard TP, Mikkelsen S, et al. Impact of the CYP2D6 genotype on post-operative intravenous oxycodone analgesia. Acta Anaesthesiol Scand. 2010;54(2):232–40.
Zwisler ST, Enggaard TP, Noehr-Jensen L, et al. The hypoalgesic effect of oxycodone in human experimental pain models in relation to the CYP2D6 oxidation polymorphism. Basic Clin Pharmacol Toxicol. 2009;104(4):335–44.
Madadi P, Avard D, Koren G. Pharmacogenetics of opioids for the treatment of acute maternal pain during pregnancy and lactation. Curr Drug Metab. 2012;13(6):721–7.
Andreassen TN, Eftedal I, Klepstad P, et al. Do CYP2D6 genotypes reflect oxycodone requirements for cancer patients treated for cancer pain? A cross-sectional multicentre study. Eur J Clin Pharmacol. 2012;68(1):55–64.
Klepstad P, Fladvad T, Skorpen F, et al. Influence from genetic variability on opioid use for cancer pain: a European genetic association study of 2294 cancer pain patients. Pain. 2011;152(5):1139–45.
Zwisler ST, Enggaard TP, Mikkelsen S, et al. Lack of association of OPRM1 and ABCB1 single-nucleotide polymorphisms to oxycodone response in postoperative pain. J Clin Pharmacol. 2012;52(2):234–42.
Stamer UM, Zhang L, Stuber F. Personalized therapy in pain management: where do we stand? Pharmacogenomics. 2010;11(6):843–64.
Foster A, Mobley E, Wang Z. Complicated pain management in a CYP450 2D6 poor metabolizer. Pain Pract. 2007;7(4):352–6.
de Leon J, Dinsmore L, Wedlund P. Adverse drug reactions to oxycodone and hydrocodone in CYP2D6 ultrarapid metabolizers. J Clin Psychopharmacol. 2003;23(4):420–1.
Jannetto PJ, Wong SH, Gock SB, et al. Pharmacogenomics as molecular autopsy for postmortem forensic toxicology: genotyping cytochrome P450 2D6 for oxycodone cases. J Anal Toxicol. 2002;26(7):438–47.
Lurcott G. The effects of the genetic absence and inhibition of CYP2D6 on the metabolism of codeine and its derivatives, hydrocodone and oxycodone. Anesth Prog. 1998;45(4):154–6.
Heiskanen T, Olkkola KT, Kalso E. Effects of blocking CYP2D6 on the pharmacokinetics and pharmacodynamics of oxycodone. Clin Pharmacol Ther. 1998;64(6):603–11.
Volpe DA, McMahon Tobin GA, Mellon RD, et al. Uniform assessment and ranking of opioid mu receptor binding constants for selected opioid drugs. Regul Toxicol Pharmacol. 2011;59(3):385–90.
Kalso E. How different is oxycodone from morphine? Pain. 2007;132(3):227–8.
Lemberg KK, Kontinen VK, Siiskonen AO, et al. Antinociception by spinal and systemic oxycodone: why does the route make a difference? In vitro and in vivo studies in rats. Anesthesiology. 2006;105(4):801–12.
Lalovic B, Kharasch E, Hoffer C, et al. Pharmacokinetics and pharmacodynamics of oral oxycodone in healthy human subjects: role of circulating active metabolites. Clin Pharmacol Ther. 2006;79(5):461–79.
Lemberg KK, Siiskonen AO, Kontinen VK, et al. Pharmacological characterization of noroxymorphone as a new opioid for spinal analgesia. Anesth Analg. 2008;106(2):463–70. table of contents.
Chen ZR, Irvine RJ, Somogyi AA, et al. Mu receptor binding of some commonly used opioids and their metabolites. Life Sci. 1991;48(22):2165–71.
Andreassen TN, Klepstad P, Davies A, et al. Is oxycodone efficacy reflected in serum concentrations? A multicenter, cross-sectional study in 456 adult cancer patients. J Pain Symptom Manag. 2012;43(4):694–705.
Sloan PA, Barkin RL. Oxymorphone and oxymorphone extended release: a pharmacotherapeutic review. J Opioid Manag. 2008;4(3):131–44.
Lugo RA, Kern SE. The pharmacokinetics of oxycodone. J Pain Palliat Care Pharmacother. 2004;18(4):17–30.
Poyhia R, Seppala T, Olkkola KT, et al. The pharmacokinetics and metabolism of oxycodone after intramuscular and oral administration to healthy subjects. Br J Clin Pharmacol. 1992;33(6):617–21.
Mandema JW, Kaiko RF, Oshlack B, et al. Characterization and validation of a pharmacokinetic model for controlled-release oxycodone. Br J Clin Pharmacol. 1996;42(6):747–56.
Poyhia R, Olkkola KT, Seppala T, et al. The pharmacokinetics of oxycodone after intravenous injection in adults. Br J Clin Pharmacol. 1991;32(4):516–8.
Liukas A, Kuusniemi K, Aantaa R, et al. Plasma concentrations of oral oxycodone are greatly increased in the elderly. Clin Pharmacol Ther. 2008;84(4):462–7.
Saari TI, Ihmsen H, Neuvonen PJ, et al. Oxycodone clearance is markedly reduced with advancing age: a population pharmacokinetic study. Br J Anaesth. 2012;108(3):491–8.
Kirvela M, Lindgren L, Seppala T, et al. The pharmacokinetics of oxycodone in uremic patients undergoing renal transplantation. J Clin Anesth. 1996;8(1):13–8.
Poyhia R, Vainio A, Kalso E. A review of oxycodone’s clinical pharmacokinetics and pharmacodynamics. J Pain Symptom Manag. 1993;8(2):63–7.
Naito T, Takashina Y, Yamamoto K, et al. CYP3A5*3 affects plasma disposition of noroxycodone and dose escalation in cancer patients receiving oxycodone. J Clin Pharmacol. 2011;51(11):1529–38.
Lamba JK, Lin YS, Schuetz EG, et al. Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev. 2012;54(10):1271–94.
Andersson T, Flockhart DA, Goldstein DB, et al. Drug-metabolizing enzymes: evidence for clinical utility of pharmacogenomic tests. Clin Pharmacol Ther. 2005;78(6):559–81.
Karolinska Institutet. The Human Cytochrome P450 (CYP) Allele Nomenclature Database Stockholm updated 22-Feb-2012. http://www.cypalleles.ki.se/. Accessed 20 Oct 2012.
Johansson I, Ingelman-Sundberg M. CNVs of human genes and their implication in pharmacogenetics. Cytogenet Genome Res. 2008;123(1–4):195–204.
Dahl ML, Johansson I, Bertilsson L, et al. Ultrarapid hydroxylation of debrisoquine in a Swedish population. Analysis of the molecular genetic basis. J Pharmacol Exp Ther. 1995;274(1):516–20.
Bathum L, Johansson I, Ingelman-Sundberg M, et al. Ultrarapid metabolism of sparteine: frequency of alleles with duplicated CYP2D6 genes in a Danish population as determined by restriction fragment length polymorphism and long polymerase chain reaction. Pharmacogenetics. 1998;8(2):119–23.
Johansson I, Lundqvist E, Bertilsson L, et al. Inherited amplification of an active gene in the cytochrome P450 CYP2D locus as a cause of ultrarapid metabolism of debrisoquine. Proc Natl Acad Sci U S A. 1993;90(24):11825–9.
Agundez JA, Ledesma MC, Ladero JM, et al. Prevalence of CYP2D6 gene duplication and its repercussion on the oxidative phenotype in a white population. Clin Pharmacol Ther. 1995;57(3):265–9.
Aklillu E, Persson I, Bertilsson L, et al. Frequent distribution of ultrarapid metabolizers of debrisoquine in an Ethiopian population carrying duplicated and multiduplicated functional CYP2D6 alleles. J Pharmacol Exp Ther. 1996;278(1):441–6.
Wennerholm A, Johansson I, Massele AY, et al. Decreased capacity for debrisoquine metabolism among black Tanzanians: analyses of the CYP2D6 genotype and phenotype. Pharmacogenetics. 1999;9(6):707–14.
Liukas A, Kuusniemi K, Aantaa R, et al. Elimination of intravenous oxycodone in the elderly: a pharmacokinetic study in postoperative orthopaedic patients of different age groups. Drugs Aging. 2011;28(1):41–50.
Saari TI, Gronlund J, Hagelberg NM, et al. Effects of itraconazole on the pharmacokinetics and pharmacodynamics of intravenously and orally administered oxycodone. Eur J Clin Pharmacol. 2010;66(4):387–97.
Gronlund J, Saari T, Hagelberg N, et al. Effect of telithromycin on the pharmacokinetics and pharmacodynamics of oral oxycodone. J Clin Pharmacol. 2010;50(1):101–8.
Laine K, Tybring G, Hartter S, et al. Inhibition of cytochrome P4502D6 activity with paroxetine normalizes the ultrarapid metabolizer phenotype as measured by nortriptyline pharmacokinetics and the debrisoquin test. Clin Pharmacol Ther. 2001;70(4):327–35.
Myers AL, Hassan HE, Lee IJ, et al. Repeated administration of oxycodone modifies the gene expression of several drug metabolising enzymes in the hepatic tissue of male Sprague-Dawley rats, including glutathione S-transferase A-5 (rGSTA5) and CYP3A2. J Pharm Pharmacol. 2010;62(2):189–96.
Liu YT, Hao HP, Liu CX, et al. Drugs as CYP3A probes, inducers, and inhibitors. Drug Metab Rev. 2007;39(4):699–721.
Kato M. Intestinal first-pass metabolism of CYP3A4 substrates. Drug Metab Pharmacokinet. 2008;23(2):87–94.
Kivisto KT, Niemi M, Fromm MF. Functional interaction of intestinal CYP3A4 and P-glycoprotein. Fundam Clin Pharmacol. 2004;18(6):621–6.
Nieminen TH, Hagelberg NM, Saari TI, et al. Rifampin greatly reduces the plasma concentrations of intravenous and oral oxycodone. Anesthesiology. 2009;110(6):1371–8.
Nieminen TH, Hagelberg NM, Saari TI, et al. St John’s wort greatly reduces the concentrations of oral oxycodone. Eur J Pain. 2010;14(8):854–9.
Fromm MF, Busse D, Kroemer HK, et al. Differential induction of prehepatic and hepatic metabolism of verapamil by rifampin. Hepatology. 1996;24(4):796–801.
SFINX. Swedish Finnish interaction x-referencing. http://www.janusinfo.se. Accessed 7 Feb 2013.
Bottiger Y, Laine K, Andersson ML, et al. SFINX—a drug–drug interaction database designed for clinical decision support systems. Eur J Clin Pharmacol. 2009;65(6):627–33.
Hagelberg NM, Nieminen TH, Saari TI, et al. Voriconazole drastically increases exposure to oral oxycodone. Eur J Clin Pharmacol. 2009;65(3):263–71.
Liukas A, Hagelberg NM, Kuusniemi K, et al. Inhibition of cytochrome P450 3A by clarithromycin uniformly affects the pharmacokinetics and pharmacodynamics of oxycodone in young and elderly volunteers. J Clin Psychopharmacol. 2011;31(3):302–8.
Nieminen TH, Hagelberg NM, Saari TI, et al. Grapefruit juice enhances the exposure to oral oxycodone. Basic Clin Pharmacol Toxicol. 2010;107(4):782–8.
Nieminen TH, Hagelberg NM, Saari TI, et al. Oxycodone concentrations are greatly increased by the concomitant use of ritonavir or lopinavir/ritonavir. Eur J Clin Pharmacol. 2010;66(10):977–85.
Watanabe M, Homma M, Momo K, et al. Effects of voriconazole co-administration on oxycodone-induced adverse events: a case in the retrospective survey. Eur J Clin Pharmacol. 2011;67(8):859–61.
Kokki M, Valitalo P, Rasanen I, et al. Absorption of different oral dosage forms of oxycodone in the elderly: a cross-over clinical trial in patients undergoing cystoscopy. Eur J Clin Pharmacol. 2012;68(10):1357–63.
Sistonen J, Sajantila A, Lao O, et al. CYP2D6 worldwide genetic variation shows high frequency of altered activity variants and no continental structure. Pharmacogenet Genomics. 2007;17(2):93–101.
Acknowledgments
This work was in part supported by grants from Karolinska Institutet, the Swedish Foundation for Clinical Pharmacology and Pharmacotherapy and the Swedish Research Council (number 2007-5681). All authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Söderberg Löfdal, K.C., Andersson, M.L. & Gustafsson, L.L. Cytochrome P450-Mediated Changes in Oxycodone Pharmacokinetics/Pharmacodynamics and Their Clinical Implications. Drugs 73, 533–543 (2013). https://doi.org/10.1007/s40265-013-0036-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-013-0036-0