Abstract
Introduction
Previous observational studies have associated benzodiazepine use with an increased risk of dementia. However, limitations in the study methods leave questions unanswered regarding the interpretation of the findings.
Methods
A case–control analysis was conducted using data from the UK-based Clinical Practice Research Datalink (CPRD). A total of 26,459 patients aged ≥65 years with newly diagnosed Alzheimer’s disease (AD) or vascular dementia (VaD) between 1998 and 2013 were identified and matched 1:1 to dementia-free controls on age, sex, calendar time, general practice, and number of years of recorded history. Adjusted odds ratios (aORs) were calculated with 95 % confidence intervals (CIs) of developing AD or VaD in relation to previous benzodiazepine use, stratified by duration and benzodiazepine type.
Results
The aOR (95 % CI) of developing AD for those who started benzodiazepines <1 year before diagnosis was 2.20 (1.91–2.53), and fell to the null for those who started between 2 and <3 years before [aOR 0.99 (0.84–1.17)]. The aOR (95 % CI) of developing VaD for those who started benzodiazepines <1 year before diagnosis was 3.30 (2.78–3.92), and fell close to the null for those who started between 3 and <4 years before [aOR 1.16 (0.96–1.40)]. After accounting for benzodiazepine use initiated during this prodromal phase, long-term use of benzodiazepines was not associated with an increased risk of developing AD [aOR 0.69 (0.57–0.85)] or VaD [aOR 1.11 (0.85–1.45)].
Conclusion
After taking a prodromal phase into consideration, benzodiazepine use was not associated with an increased risk of developing AD or VaD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This large, observational study suggests that long-term benzodiazepine use is not associated with an increased risk of Alzheimer’s disease or vascular dementia. |
Previously reported increased risks of dementia associated with benzodiazepine use are likely distorted by use of benzodiazepines in the early clinical phase of dementia. |
This finding is of substantial clinical relevance because benzodiazepines are commonly prescribed (on a long-term basis) for various indications, such as insomnia or anxiety, particularly in elderly people who are at an increased risk of dementia. |
1 Introduction
Benzodiazepines are widely used for the treatment of insomnia and anxiety. In 2012, approximately 16 million prescriptions were issued for these drugs in general practice in England, at an annual cost of approximately ₤40 million [1]. Because of concerns raised by well-known short-term side effects on memory and cognition [2], a number of studies have investigated whether the use of benzodiazepines is associated with an increased risk of dementia, despite the lack of a mechanistic hypothesis. Most of these studies have found evidence for an increased risk in long-term users [3, 4], although with inconsistent findings regarding the timing of use [5–7]. The association between benzodiazepine use and dementia is subject to distortion due to protopathic bias, also called reverse causation [8], as benzodiazepines are often prescribed to treat prodromal symptoms of dementia, such as anxiety and insomnia [9]. One common method to control for this sort of bias is to account for induction time by moving the diagnosis date back in time to ensure that exposure is ascertained prior to the disease onset. This method removes the period of time between disease onset and disease diagnosis from the analysis, i.e. a time period in which the drug was likely prescribed to treat early symptoms of the disease [10].
Moreover, there is only very limited and inconsistent information on the association between benzodiazepine use and the risk of specific dementia subtypes, such as Alzheimer’s disease (AD) or vascular dementia (VaD) [11–13].
The aim of this study was to explore the association between benzodiazepine use and the risk of AD or VaD using a large, well-established primary care database from the UK, and to simultaneously control for protopathic bias by defining an appropriate induction period.
2 Methods
2.1 Study Design and Data Source
A case–control analysis was conducted using data from the UK-based Clinical Practice Research Datalink (CPRD), formerly known as the General Practice Research Database (GPRD). The CPRD encompasses approximately 10 million computerized longitudinal medical records of patients enrolled with general practitioners (GPs). These GPs are responsible for primary healthcare and for referrals of their patients to specialists or hospitals. They record patient demographics, diagnoses, and drug prescriptions, as well as some lifestyle information (e.g. smoking status) and personal characteristics (e.g. body mass index [BMI]). Information on drug exposure and diagnoses in the CPRD has been validated repeatedly and proven to be of high quality [14–17]. The CPRD is managed by the UK National Health Service’s (NHS) National Institute for Health Research (NIHR), and the Medicines and Healthcare Products Regulatory Agency (MHRA). Patients enrolled in the CPRD are representative of the UK population with regard to age, sex, geographic distribution, and annual turnover rate. CPRD data have been used in previous studies on dementia, AD, and VaD [18–22].
The study was approved by the Independent Scientific Advisory Committee (ISAC) for MHRA database research (protocol number 13_221R).
2.2 Case Identification and Validation
Cases were patients aged 65 years or older who had a first-time diagnosis of AD, VaD, or any unspecified dementia (based on Read codes) recorded between January 1998 and July 2013, or who received a first-time prescription for an acetylcholinesterase inhibitor (i.e. donepezil, rivastigmine, galantamine, or tacrine) or the N-methyl-d-aspartate (NMDA) receptor antagonist memantine, i.e. drugs specifically licensed for the treatment of AD. The date of the first diagnosis or the first prescription for one of the above-mentioned drugs, whichever came first, will subsequently be referred to as the ‘diagnosis date’. Patients with less than 3 years of active history in the database prior to the diagnosis date were excluded, as were those with a diagnosis of HIV/AIDS, alcoholism, drug abuse, multiple sclerosis, motor neuron disease, or Down’s syndrome. To increase the probability of including only well-defined AD or VaD cases, a validated algorithm was applied, described in detail elsewhere [23]. In brief, this algorithm was based on recordings of specific dementia tests [e.g. Mini-Mental State Examination (MMSE), Clock Drawing Test (CDT), or Abbreviated Mental Test (7-Minute Screen)], referrals to specialists (e.g. neurologists, geriatricians or psycho-geriatricians), brain imaging [computed tomography (CT), magnetic resonance imaging (MRI), or single photon emission computed tomography (SPECT)], or dementia symptoms (memory impairment, aphasia, apraxia, or agnosia) supportive of a diagnosis of a specific dementia subtype (i.e. AD or VaD).
To validate this algorithm, a questionnaire was sent to GPs for a random sample of 60 AD and 60 VaD cases to gather additional information on the clinical circumstances and diagnostic steps taken. In 79 % of the AD cases, the GPs confirmed the recorded AD diagnosis, whereas in the other AD cases, the diagnosed dementia subtype was either different, not further specified, or the case did not have confirmed dementia. For VaD, the corresponding confirmation rate was 74 %.
2.3 Controls
For each case of AD or VaD, we identified at random one control patient without dementia and with no prescriptions for one of the above-mentioned AD-specific drugs before the diagnosis date. Controls were matched to cases on age (same year of birth), sex, calendar time (i.e. controls were assigned the diagnosis date of their corresponding cases), general practice, and number of years of recorded history in the database prior to the diagnosis date. The same exclusion criteria were applied to controls as to cases.
2.4 Introduction of Induction Time: Assessment of Prodromal Symptoms
We assumed that first-time prescriptions of benzodiazepines close to the diagnosis date were likely issued for symptomatic treatment of prodromal symptoms of early dementia (i.e. anxiety or insomnia). Controlling for this induction time was achieved by shifting the diagnosis date back in time to the onset of symptoms of early dementia. Optimal induction time was determined by systematically exploring the risk of AD or VaD in relation to the first benzodiazepine prescription prior to the diagnosis date by 1-year intervals going back 10 years in time. The induction period was defined as 2 years for AD and 3 years for VaD, and the diagnosis date was shifted backwards accordingly (for cases and controls). From here on, the term ‘index date’ will refer to this shifted date.
2.5 Exposure to Benzodiazepines
Cases and controls were classified as users if they had ever received a benzodiazepine prescription before the index date. All others were considered non-users. We further assessed the number of benzodiazepine prescriptions [including the benzodiazepine receptor agonists (BzRAs) zolpidem, zopiclon, and zaleplon] prior to the index date, categorized as 1–9, 10–29, 30–59, 60–99, 100–149, or ≥150 prescriptions. Number of prescriptions is a widely used proxy for exposure duration; a benzodiazepine prescription in our study population covers, on average, 28 days; thus, as an example, 150 prescriptions would cover a period of 4200 days, or approximately 11.5 years, given that the drug was taken on a regular basis (which is usually the case with benzodiazepines used to treat insomnia).
We further assessed whether users had only one type of benzodiazepine prescribed during the entire exposure period, either based on the WHO Anatomical Therapeutic Chemical (ATC) classification system (i.e. only classical benzodiazepines or BzRAs) or on the estimated duration of action (i.e. only ultrashort-acting, short to intermediate-acting, or long-acting benzodiazepines) [24], and we stratified users according to duration of use by assessing the number of recorded prescriptions (same as above).
2.6 Covariates
We matched cases and controls for the potential confounders age, sex, calendar time (i.e. controls were assigned the diagnosis date of their corresponding cases), general practice, and number of years of recorded history in the database. We further adjusted the analyses for BMI (<18.5, 18.5–<25, 25–<30, ≥30 kg/m2, or unknown; closest to the index date), smoking status (non-smoker, current smoker, ex-smoker, or unknown; closest to the index date), and depression [25] in the multivariate model. Other potential confounders such as arterial hypertension, diabetes mellitus (and/or use of antidiabetic drugs), dyslipidemia, atrial fibrillation, and heart failure, as well as use of antihypertensives, statins, platelet aggregation inhibitors, or anticoagulants within the 365 days prior to the index date were also tested in bivariate analyses; however, as they had no material impact (<10 % change) on the risk estimates for the association of interest, they were not included in the final multivariate model.
2.7 Statistical Analysis
Conditional logistic regression analyses were conducted to explore the association between exposure to benzodiazepines and the risk of AD or VaD, expressed as odds ratios (ORs) with 95 % confidence intervals (CIs) at a two-sided p value of 0.05. All statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA). We compared users of benzodiazepines in general, users of only classical benzodiazepines or BzRAs, as well as users of only ultrashort-acting, short to intermediate-acting, or long-acting benzodiazepines, with non-users of benzodiazepines.
3 Results
3.1 Case Selection
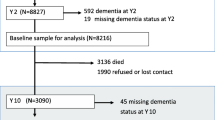
Within the CPRD, we identified 126,146 patients aged 65 years or older with a first-time diagnosis of AD, VaD, or unspecified dementia, or a first-time prescription for a drug to treat AD at any time during the study period. From these patients, 66,204 were excluded because they had less than 3 years of active history or one or more of the exclusion diagnoses prior to the diagnosis date. After applying the above-described algorithm on the remaining 59,942 patients, 19,463 well-defined AD and 11,916 VaD cases remained (Fig. 1).
3.2 Determination of Induction Time
The adjusted OR (aOR) (95 % CI) of developing AD for those who started benzodiazepines <1 year before the diagnosis was 2.20 (1.91–2.53), and fell to the null for those who started between 2 and <3 years before [aOR 0.99 (0.84–1.17)]. The aOR (95 % CI) of developing VaD for those who started benzodiazepines <1 year before the diagnosis was 3.30 (2.78–3.92), and fell close to the null for those who started between 3 and <4 years before [aOR 1.16 (0.96–1.40)] (Fig. 2). Thus, the appropriate induction time was determined as 2 years prior to the AD diagnosis date and 3 years prior to the VaD diagnosis date.
3.3 Study Population
After shifting the diagnosis date accordingly, and applying all study criteria, there remained 16,823 cases with AD and 9636 with VaD (Fig. 1), which, together with the corresponding number of matched dementia-free controls, formed the study population. Mean age was closely similar in AD and VaD cases [mean age (±SD) 78.8 (±6.3) vs. 79.6 (±6.3) years). The detailed age- and sex-distribution, BMI, and smoking status, as well as various comorbidities and co-medications for AD or VaD cases and their corresponding controls, are displayed in Table 1.
3.4 Benzodiazepines and Risk of Alzheimer’s Disease
Among AD cases and corresponding controls, 4878 (29.0 %) and 4794 (28.5 %) used benzodiazepines at some point in time prior to the index date. The median observation time [interquartile range (IQR)] between the first benzodiazepine prescription and the index date was 8.0 [3.0–12.5] years for cases and 7.9 [3.2–12.6] years for controls.
Benzodiazepine use was not associated with an increased risk of AD compared with non-use [aOR 0.95 (0.90–1.00)]. On the contrary, long-term benzodiazepine users were at a lower relative risk of developing AD than non-users, a finding that was most pronounced in those with ≥150 prescriptions [aOR 0.69 (0.57–0.85)] (Table 2).
There was no substantial difference in the risk of AD for classical benzodiazepines only or users of BzRAs only; however, the number of exclusive long-term users of BzRAs was low (Table 3).
We also observed a decreased relative risk of AD in long-term users of long-acting or short to intermediate-acting benzodiazepines only, with a tendency towards lower ORs with longer-term use. The aORs (95 % CI) for users with 100–149 or ≥150 prescriptions of only long-acting benzodiazepines were 0.53 (0.30–0.95) and 0.70 (0.37–1.30), respectively; the corresponding aORs for users of only short to intermediate-acting benzodiazepines were 0.91 (0.69–1.21) and 0.70 (0.48–1.01), respectively. The number of long-term users of only ultrashort-acting benzodiazepines (mainly BzRAs) was too low for a meaningful interpretation of the corresponding aORs (Table 4).
3.5 Benzodiazepines and Risk of Vascular Dementia
Among VaD cases and corresponding controls, 2872 (29.8 %) and 2576 (26.7 %) used benzodiazepines at some point in time prior to the index date. The median observation time (IQR) between the first benzodiazepine prescription and the index date was 7.3 (2.9–12.1) years for cases and 7.4 (2.8–12.0) years for controls.
Benzodiazepine use was not associated with an increased risk of VaD compared with non-use [aOR 1.08 (1.01–1.15)]; however, in contrast to the association with AD, long-term users did not have a reduced risk of VaD compared with non-users; the aOR (95 % CI) for users with ≥150 prescriptions was 1.11 (0.85–1.45) [Table 2].
Similar results were observed for users of classical benzodiazepines only, whereas the number of long-term users of BzRAs only was too low for a meaningful interpretation of the corresponding aORs (Table 3).
We found no altered risk of VaD with increasing number of prescriptions for users of only long-acting or short to intermediate-acting benzodiazepines, whereas the number of long-term users of only ultrashort-acting benzodiazepines (mainly BzRAs) was again too low for a meaningful interpretation of the corresponding aORs (Table 4).
3.6 Additional Analyses
We also ran the analyses in the wider case population, containing all 59,942 cases (i.e. AD, VaD, and unspecified dementia) before application of the algorithm criteria (see Fig. 1). We therefore first ran the induction time analysis and determined the optimal induction period as 3 years; we then ran the main analysis with the diagnosis date shifted by 3 years. Also in the wider case population (containing 47,051 cases, after shifting the diagnosis date and applying all study criteria), benzodiazepine use was not associated with an increased risk of developing dementia (i.e. AD, VaD, or unspecified dementia) [see electronic supplementary material Table 1].
4 Discussion
In this large, case–control analysis, no evidence was found for an increased risk of either AD or VaD related to the use of benzodiazepines, after taking into consideration an appropriate induction time.
4.1 Comparison with Other Studies
These findings are in contrast with the results of previous studies that reported increased risks of dementia in users of benzodiazepines. However, the results of these studies have to be interpreted in light of methodological limitations. One study reported an increased risk of overall dementia in long-term users of benzodiazepines, but the observation period (maximum 3 years) was considerably shorter than in our study, and was thus prone to protopathic bias [4]. Two other studies included a longer observation period, and the authors stratified their analyses by the timing of benzodiazepine use. They found an increased risk of overall dementia in past users who had stopped benzodiazepines 2 or 3 years [6] and 13 [12] years prior to the dementia diagnosis. However, corresponding relative risk estimates were based on only 14 [6] and 12 [12] subjects, with unknown duration of benzodiazepine use, leading to imprecise risk estimates with broad CIs [aOR 2.3 (1.2–4.5) [6], and 2.64 (0.71–9.78) [12], respectively]. Furthermore, stratification by current and past use was arbitrary given the imprecise diagnosis date of a chronic disease such as dementia.
However, there are two recent studies with more statistical power that addressed the problem of protopathic bias by introducing an arbitrary benzodiazepine-free observation period of 3 years before follow-up [7] (to control for factors strongly associated with new use of benzodiazepines) or an induction time of 5 years prior to the dementia diagnosis [13]. They found, in contrast to our study, an approximately 50 % higher risk of dementia in new users [7] and an approximately 70 % higher risk of AD in users of benzodiazepines for >6 months between 5 and 10 years before the diagnosis of dementia compared with non-users of these drugs [13], respectively.
Of note, one early study found a lower incidence of AD among users of benzodiazepines compared with non-users [11]; however, the inclusion of past users into the referent group may have biased these results.
4.2 Possible Mechanism
We are not aware of an established mechanism, or even a mechanistic hypothesis, linking long-term use of benzodiazepines with the development of AD or VaD. It is well-known that use of benzodiazepines may induce cognitive impairment and psychosis [26], but such acute effects of benzodiazepines cannot be set equal with an increased risk of dementia.
In contrast to available evidence, and possibly explained by limited follow-up in previous studies, long-term users of benzodiazepines were at an even lower relative risk of AD than non-users. Fastbom et al. suggested a mechanism for such a possible ‘protective’ effect of benzodiazepines on AD, hypothesizing that benzodiazepines (by enhancing the activity of gamma-aminobutyric acid [GABA]) inhibit glutamatergic neurotransmission, and thereby possibly protect against the excitotoxic effects of glutamate, which is believed to be involved in the pathogenesis of AD [11]. Alternatively, and hypothetically, benzodiazepines may indirectly exert a protective effect against the development of AD by improving sleep (through their clinical effects on sleep latency, number of awakenings, and duration and quality of sleep), as sleep deprivation has been shown to increase cerebrospinal fluid levels of Aβ42 [27], one of the key proteins involved in the pathogenesis of AD. Such a mechanism would also be in line with our observation that use of benzodiazepines was not associated with an altered risk of VaD.
4.3 Strengths and Limitations
This study has several strengths. First, we used a large, well-established primary care database of high quality and completeness. Second, we were in a position to include a large number of patients with dementia (namely 16,823 well-defined AD patients and 9636 VaD patients, of whom approximately 30 % were benzodiazepine users) to study the association between benzodiazepine use and the risk of AD and VaD with substantial statistical power. This large number of subjects allowed us to study the risk of developing AD or VaD in mutually exclusive groups of users of classical benzodiazepines or BzRAs only. Third, we carefully addressed the issue of protopathic bias by identifying the relevant induction time between symptoms and diagnosis in the study population, and by shifting the diagnosis date accordingly. Fourth, compared with other investigations, the observation period in our study was long (median 8.0 years for AD cases, and 7.4 years for VaD cases), enabling us to thoroughly assess the effect of the long duration of benzodiazepine use on the risk of AD and VaD (>10 years) in contrast to a recently published investigation where use of benzodiazepines of >6 months (reflecting approximately two prescriptions in our study) was inadequately called ‘long-term’ benzodiazepine use [13]. Finally, by excluding patients with less than 3 years of recorded history in the database prior to the index date, we reduced the possibility of including prevalent rather than incident AD or VaD cases.
This study does have some limitations. First, we cannot rule out the possibility of some AD and VaD case misclassification as not all dementia diagnoses can be accurately assigned by subtype. However, to reduce the possibility of misclassification when classifying AD or VaD cases, we applied a published validated algorithm [23]. Second, we were not able to control for certain potential confounders, such as level of education, marital status, or socioeconomic status, since these factors are not routinely recorded in the CPRD. However, we matched cases and controls on general practice, which does control somewhat for socioeconomic status. Third, we cannot establish with certainty that patients who started to use benzodiazepines in the time period immediately preceding the diagnosis date indeed got these drugs to treat prodromal symptoms. Thus, in theory, induction of new-onset dementia by benzodiazepines in a subset of susceptible patients, and therefore a possible causal association between short-term benzodiazepine use and dementia risk, cannot be ruled out completely, even though this seems to be a highly unlikely alternative explanation for the observed phenomenon which we interpreted as protopathic bias.
5 Conclusions
No increased risk of AD or VaD associated with the use of benzodiazepines was found. On the contrary, long-term use of benzodiazepines was associated with a lower relative risk of developing AD, but not VaD, compared with non-users. While we do not want to over-interpret the observed reduced risk of AD associated with long-term use of benzodiazepines, we conclude that our results provide no evidence for the hypothesis that benzodiazepine use is associated with an increased risk of dementia. Nevertheless, restricted prescribing of benzodiazepines is still advised given other well-known adverse effects, particularly in the elderly, such as dependence, cognitive impairment, falls, sedation, or impairment of driving skills [28].
References
NHS Business Services Authority, NHS Prescription Services. Central nervous system national charts. 2014. Available at: http://www.nhsbsa.nhs.uk/PrescriptionServices/2584.aspx. Accessed 26 Apr 2015.
Buffett-Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des. 2002;8:45–58.
Wu C-S, Wang S-C, Chang I-S, Lin K-M. The association between dementia and long-term use of benzodiazepine in the elderly: nested case–control study using claims data. Am J Geriatr Psychiatry. 2009;17:614–20.
Chen P-L, Lee W-J, Sun W-Z, Oyang Y-J, Fuh J-L. Risk of dementia in patients with insomnia and long-term use of hypnotics: a population-based retrospective cohort study. PLoS One. 2012;7:e49113.
Wu C-S, Ting T-T, Wang S-C, Chang I-S, Lin K-M. Effect of benzodiazepine discontinuation on dementia risk. Am J Geriatr Psychiatry. 2011;19:151–9.
Lagnaoui R, Bégaud B, Moore N, Chaslerie A, Fourrier A, Letenneur L, et al. Benzodiazepine use and risk of dementia: a nested case–control study. J Clin Epidemiol. 2002;55:314–8.
Billioti de Gage S, Bégaud B, Bazin F, Verdoux H, Dartigues J-F, Pérès K, et al. Benzodiazepine use and risk of dementia: prospective population based study. BMJ. 2012;345:e6231.
Horwitz RI, Feinstein AR. The problem of “protopathic bias” in case–control studies. Am J Med. 1980;68:255–8.
Stella F, Radanovic M, Balthazar ML, Canineu PR, de Souza LC, Forlenza OV. Neuropsychiatric symptoms in the prodromal stages of dementia. Curr Opin Psychiatry. 2014;27:230–5.
Tamim H, Tahami Monfared AA, LeLorier J. Application of lag-time into exposure definitions to control for protopathic bias. Pharmacoepidemiol Drug Saf. 2007;16:250–8.
Fastbom J, Forsell Y, Winblad B. Benzodiazepines may have protective effects against Alzheimer disease. Alzheimer Dis Assoc Disord. 1998;12:14–7.
Gallacher J, Elwood P, Pickering J, Bayer A, Fish M, Ben-Shlomo Y. Benzodiazepine use and risk of dementia: evidence from the Caerphilly Prospective Study (CaPS). J Epidemiol Community Health. 2012;66:869–73.
Billioti de Gage S, Moride Y, Ducruet T, Kurth T, Verdoux H, Tournier M, et al. Benzodiazepine use and risk of Alzheimer’s disease: case–control study. BMJ. 2014;349:g5205.
Jick SS, Kaye JA, Vasilakis-Scaramozza C, Garcia Rodríguez LA, Ruigómez A, Meier CR, et al. Validity of the general practice research database. Pharmacotherapy. 2003;23:686–9.
Wood L, Martinez C. The general practice research database: role in pharmacovigilance. Drug Saf. 2004;27:871–81.
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69:4–14.
Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:e128–36.
Seshadri S, Zornberg GL, Derby LE, Myers MW, Jick H, Drachman DA. Postmenopausal estrogen replacement therapy and the risk of Alzheimer disease. Arch Neurol. 2001;58:435–40.
Davies NM, Kehoe PG, Ben-Shlomo Y, Martin RM. Associations of anti-hypertensive treatments with Alzheimer’s disease, vascular dementia, and other dementias. J Alzheimers Dis. 2011;26:699–708.
Jick H, Zornberg G, Jick S, Seshadri S, Drachman D. Statins and the risk of dementia. Lancet. 2000;356:1627–31.
Martinez C, Jones RW, Rietbrock S. Trends in the prevalence of antipsychotic drug use among patients with Alzheimer’s disease and other dementias including those treated with antidementia drugs in the community in the UK: a cohort study. BMJ Open. 2013;3:e002080.
Imfeld P, Bodmer M, Schuerch M, Jick SS, Meier CR. Risk of incident stroke in patients with Alzheimer disease or vascular dementia. Neurology. 2013;81:910–9.
Imfeld P, Brauchli Pernus YB, Jick SS, Meier CR. Epidemiology, co-morbidities, and medication use of patients with Alzheimer’s disease or vascular dementia in the UK. J Alzheimers Dis. 2013;35:565–73.
Greenblatt DJ, Shader RI, Divoll M, Harmatz JS. Benzodiazepines: a summary of pharmacokinetic properties. Br J Clin Pharmacol. 1981;11:11S–6S.
Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF. Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. 2013;202:329–35.
Lader M. Benzodiazepine harm: how can it be reduced? Br J Clin Pharmacol. 2014;77:295–301.
Ooms S, Overeem S, Besse K, Rikkert MO, Verbeek M, Claassen JA. Effect of 1 night of total sleep deprivation on cerebrospinal fluid β-amyloid 42 in healthy middle-aged men: a randomized clinical trial. JAMA Neurol. 2014;71:971–7.
Madhusoodanan S, Bogunovic OJ. Safety of benzodiazepines in the geriatric population. Expert Opin Drug Saf. 2004;3:485–93.
Acknowledgments
The authors would like to thank Pascal Egger for programming and technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflicts of interest
Patrick Imfeld, Michael Bodmer, Susan S. Jick, and Christoph R. Meier declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Imfeld, P., Bodmer, M., Jick, S.S. et al. Benzodiazepine Use and Risk of Developing Alzheimer’s Disease or Vascular Dementia: A Case–Control Analysis. Drug Saf 38, 909–919 (2015). https://doi.org/10.1007/s40264-015-0319-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-015-0319-3