Abstract
Background
A histamine-2 receptor antagonist (H2RA) is one of the common gastroprotective co-therapies used with non-steroidal anti-inflammatory drugs (NSAIDs) for the prevention or treatment of peptic ulcers (PUs). To date, no study has directly compared the prophylactic effectiveness between high-dose and low-dose H2RA.
Objective
Our objective was to compare the effectiveness of high-dose versus low-dose H2RAs in the primary prophylaxis of PUs among short-term NSAID users.
Methods
A retrospective cohort study was conducted using the Clinical Data Analysis and Reporting System (CDARS) in Hong Kong. Patients aged 18 years or above who received a single prescription of oral NSAID with oral H2RA were identified within the study period (1 January 2009–31 December 2012). Patients with a history of or risk factors for PU in the corresponding 2 years prior to the index date (of the first NSAID prescription) were excluded. Log binomial regression analysis was used to calculate the relative risk of PU among NSAID users with high-dose H2RA versus low-dose H2RA exposure.
Results
Among the NSAID cohort (n = 102,042), 77,509 (76 %) were on low-dose H2RA and 24,533 (24 %) were on high-dose H2RA. Of the total 69 PU cases identified during the drug exposure period, 64 (0.08 %) received low-dose-H2RA and five (0.02 %) received high-dose H2RA. The overall absolute risk of PUs for NSAID users whilst on H2RA was approximately 1 per 1,479 patients. The adjusted relative risk for NSAID users receiving high-dose H2RA versus low-dose H2RA was 0.32 (95 % confidence interval [CI] 0.13–0.79). Patients aged ≥65 years, receiving a longer duration of treatment, or with concomitant use of antiplatelet agents were found to be at higher risk of PU.
Conclusion
High-dose H2RA showed greater effectiveness than low-dose H2RA in the primary prophylaxis of NSAID-associated PUs in short-term new users.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The effectiveness of high-dose and low-dose histamine-2 receptor antagonists for the prevention of peptic ulcers has not been directly compared. |
The absolute risk of peptic ulcer among non-steroidal anti-inflammatory drug new users with concurrent use of histamine-2 receptor antagonists was approximately 0.07 %, and the incidence rate was approximately 11.4 per 1,000 patient-years. |
The high-dose histamine-2 receptor antagonist showed greater effectiveness than its low-dose form in the primary prophylaxis of non-steroidal anti-inflammatory drug-associated peptic ulcers in short-term new users. |
1 Introduction
Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed treatments for pain relief, fever, and rheumatic disorders such as rheumatoid arthritis, osteoarthritis, acute gout, and other inflammatory pain management [1–3]. However, as NSAIDs inhibit the production of prostaglandins and increase gastric acid secretion [4], their potential to cause peptic ulcers (PUs), including gastric and duodenal ulcers, remains a major concern [5]. A previous study showed that the baseline incidence of hospitalization with upper gastrointestinal (GI) events in patients receiving NSAIDs was about 2 % [6]. In addition, several risk factors for NSAID-associated PUs are well documented, including prior history of GI events; age of 65 years or older; use of high-dose NSAID; and concurrent use of corticosteroids, anticoagulants, and antiplatelet agents [7]. Gastroprotective agents (GPAs) such as histamine-2 receptor antagonists (H2RAs), proton pump inhibitors (PPIs), and misoprostol are commonly prescribed together with NSAIDs for the treatment or prevention of PUs [8–12].
A Cochrane review reported that both standard-dose H2RAs (ranitidine 300 mg/day or famotidine 40 mg/day) and high-dose H2RAs (ranitidine 600 mg/day or famotidine 80 mg/day) were effective compared with placebo in the prevention of NSAID-associated endoscopic PUs (i.e. peptic mucosal lesion observed under endoscopy [13]). The relative risk (RR) for standard-dose H2RA was 0.63 (95 % confidence interval [CI] 0.45–0.88) and 0.41 (95 % CI 0.26–0.63) for high-dose H2RA. As the 95 % CI overlapped in this indirect comparison, it is unclear whether high-dose H2RA is indeed more effective.
We were unable to identify any published head-to-head study comparing high-dose with standard-dose H2RA, as all data were based on indirect comparisons. Therefore, it is difficult to draw conclusions on the effectiveness of different doses of H2RAs in preventing NSAID-associated PUs. Most of the clinical trials investigating NSAID-associated PU prophylaxis/treatment included patients with a previous history of PU, i.e. secondary prophylaxis. For instance, all the patients included in the study by Wolde et al. [14] had a history of ulcer. The study by Hudson et al. [15] included 28 and 31 % of patients with previous ulcers in the placebo and H2RA treatment group, respectively. It is still unclear how effective different doses of H2RA are in primary prophylaxis. Finally, it has been argued that many endoscopic ulcers may, in fact, be asymptomatic with no clinical symptoms [13, 16, 17], which differs from clinical ulcers (i.e. symptomatic ulcers or ulcer complications). In addition, Yeomans et al. [18] demonstrated the difficulty with using endoscopic PU as an outcome in that a standard-dose H2RA (ranitidine 300 mg/day) group was almost 3.5 times more likely to develop endoscopic PU than the PPI group. However, they also reported no difference between PPI and standard-dose H2RA in preventing clinical PUs. These debates reveal a ‘translational evidence gap’ in the randomized control trial results and the clinical practice. Therefore, investigating the effectiveness of different doses of H2RA in preventing NSAID-associated PU in real-life practice becomes an important public health issue in places like Hong Kong, where H2RAs are the main prophylactic treatment prescribed [19].
The objective of our study therefore was to investigate the absolute risk and incidence rate of clinical PUs among NSAID users whilst receiving H2RAs and to compare the effect of high-dose versus low-dose H2RAs in the primary prophylaxis of NSAID-associated PUs in short-term users.
2 Methods
2.1 Data Sources
We used the Clinical Data Analysis and Reporting System (CDARS), a database developed by the Hong Kong Hospital Authority (HA). The HA is a statutory body that manages all publicly funded hospitals and their ambulatory clinics (primary and specialist outpatient) in Hong Kong [20]. Prescriptions obtained from HA ambulatory clinics must be dispensed by HA pharmacies because community pharmacies do not dispense HA prescriptions. As a publicly funded primary, secondary, and tertiary healthcare provider, the HA’s health service is available to all Hong Kong residents (over 7 million people) [21].
In 1995, the HA developed the Clinical Management System (CMS), a computerized clinical management system that allows clinicians to order, document, and review patient care through an electronic patient record. Patient data are recorded in CMS by trained clinicians, and typically include basic demographics, diagnosis, payment method, prescriptions, laboratory tests, and admission and discharge information, which are directly transferred to CDARS. Only trained clinicians are able to prescribe through CMS, where the drug name, dose, and frequency are stored. Prescriptions are forwarded to the corresponding pharmacy department and verified by a registered pharmacist who dispenses the drugs.
CDARS contains the records of all inpatients and outpatients attending HA clinics and hospitals, including data transferred from the Accident and Emergency Information System, Medical Record Abstract System, Inpatient Administration System, Pharmacy Management System/Corporate Drug Dispensing History. Patient records are anonymized (name, Hong Kong identification card number, address, and telephone number are withheld) to maintain confidentiality. A reference number is generated to facilitate data retrieval and further analysis. CDARS contains clinical data from 42 public hospitals and institutions via seven geographic clusters in Hong Kong [22] and has been used in several high-quality epidemiological studies [23–26].
2.2 Study Design
This is a retrospective cohort study to investigate the dose effect of H2RA in NSAID users with respect to the clinical outcome of PU.
2.3 Patient Identification
An inception cohort of patients aged 18 years or above prescribed NSAIDs with an H2RA issued by the ambulatory clinic between 1 January 2009 and 31 December 2012 (study period) was retrieved from the CDARS database. The NSAIDs and H2RAs included in the HA formulary are shown in Table 1. We defined the date of the first NSAID prescription during the study period as the index date. We specifically selected patients with only one prescription for consistency in the setting of numerous clinical possibilities, including treatment course definition of multiple NSAID prescriptions and switching between NSAIDs.
2.4 Exclusion Criteria
Patients with unknown date of birth, gender, prescription information, or with multiple or non-oral NSAID prescriptions during the study period were excluded. To obtain a new-user cohort, those who had received NSAIDs within the screening period (2 years prior to the index date) were excluded. Furthermore, patients with a previous diagnosis of PU or Helicobacter pylori infection, and those who received triple therapy for H. pylori eradication (Table 1) or a GI endoscopy procedure during the screening period were also excluded. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes used for identifying diseases and procedures are listed in Table 2. The flowchart in Fig. 1 illustrates patient inclusion and exclusion.
2.5 Definitions of Exposure
Based on the British National Formulary (63rd edition) [27], high-dose H2RA was defined as double dose or higher, and low-dose was defined as lower than double dose (including standard dose) (Table 3). The drug exposure period was defined as the prescription period in which patients were concurrently prescribed an NSAID with an H2RA. The observation was censored by the end of the prescription, diagnosis of PU, prescription of another GPA (e.g. PPI, misoprostol), death, or end of study period (31 December 2012), whichever was earliest.
2.6 Outcome
The outcome of interest in this study was PU within the drug exposure period during 2009–2012. PU diagnoses were identified from the primary diagnostic codes (ICD-9-CM 531, 532, 533, and 534) (Table 2), including acute or chronic PUs with or without mention of hemorrhage or perforation. A total of 96 % of the PU cases were confirmed with GI endoscopy, GI surgery or related diagnostic procedures (Table 2). All PU cases were confirmed with a record of hospital admission. Only the first episode of PU was counted, and observation was censored thereafter.
2.7 Covariates
The commonly reported risk factors for PU were considered in our study as covariates: age ≥65 years; concomitant use of corticosteroids, anticoagulants, or antiplatelet agents (Table 1); NSAID types (ibuprofen, diclofenac, naproxen, and others); NSAID doses (low, medium/high); and duration of NSAID exposure [6, 28]. Based on the British National Formulary (63rd edition) and existing literature [27, 29, 30], the dose of NSAID was categorized into low and medium/high dose (Table 3).
2.8 Statistical Analysis
The adjusted RR of PU in NSAID users receiving high-dose versus low-dose H2RAs and corresponding 95 % CIs were estimated using log-binomial regression. The effect of age, gender, and other covariates mentioned previously were also analysed.
The crude absolute risks (AR) and incidence rates (IR) of experiencing PU in comparative groups and overall patients were calculated based on the following equations:
The Wilson score interval was used to calculate the corresponding 95 % CI for the AR [31]. The 95 % CI of IR was calculated based on Rothman and Greenland’s method [32].
The number needed to treat (NNT) was calculated to illustrate the observed effect size using the equation NNT = 1/(risk among low-dose H2RA users with PU\( - \)risk among high-dose H2RA users with PU) [33].
2.9 Sample size calculation
We used the method of Kelsey et al. [34] to calculate the sample size required. Assuming that the background incidence of hospitalization with PUs is approximately 2 % [6], a minimum sample size of 6,223 and 18,668 patients in each arm is required, respectively, in order to detect an RR of 0.65 comparing high-dose with low-dose H2RA (the RR from Rostom et al. [17]) with 80 % power (two-sided 95 % CI).
2.10 Sensitivity and Subgroup Analyses
Three sensitivity analyses were performed to test the robustness of the study results. The first analysis addressed issues around the delayed effect of drug exposure and development of PU, as well as potential non-compliance scenarios by extending the follow-up period for 30 days. The second analysis included any PU diagnosis as an outcome instead of restricting them to diagnosis during hospitalization, to assess whether the inclusion of outpatient diagnosis would affect the conclusion. The final sensitivity analysis excluded any PU diagnosis without confirmation with GI endoscopy, GI surgery, or related diagnostic procedures.
Subgroup analysis was also performed to estimate the RR of high-dose versus low-dose H2RA in three groups of patients separately: elderly patients (aged 65 or above), and patients with longer treatment duration (30–60 days, or over 60 days).
Data analyses were performed using Statistical Analysis System (SAS) version 9.3 (SAS Inc., Cary, NC, USA). A significance level of 5 % was used in all statistical analyses.
3 Results
3.1 Patient Characteristics
Between 2009 and 2012, a total of 102,042 patients with a single prescription of oral NSAID with co-prescription of H2RA met the inclusion criteria (Fig. 1). Of these patients, 77,509 (76.0 %) were on low-dose H2RA (32,751 [42.3 %] male), and 24,533 (24.0 %) were on high-dose H2RA (10,463 [42.6 %] male).
Patient characteristics by exposure group of different doses of H2RA are detailed in Table 4. Over 99.9 % of patients were prescribed famotidine in clinical practice in Hong Kong. More than 20 % of patients were aged 65 years or older. Over 70 % of patients were receiving medium- or high-dose NSAIDs in both treatment groups. In NSAID users receiving low-dose H2RA, the most commonly prescribed oral NSAIDs were diclofenac, followed by naproxen and ibuprofen; diclofenac, ibuprofen, and naproxen were the most commonly prescribed NSAID in the high-dose H2RA group. In both groups, less than 10 % of patients were concurrently prescribed corticosteroids, anticoagulants, or antiplatelet agents, respectively. Over 80 % of the NSAID prescriptions were of short duration (i.e. less than 1 month) in both treatment groups, with a mean duration of 23 and 18 days in low-dose H2RA and high-dose H2RA groups, respectively.
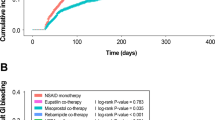
3.2 Crude Absolute Risks and Incidence Rates of PU Hospitalization
The ARs and IRs of PU are shown in Table 5. A total of 69 PU cases were identified during drug exposure in the study cohort, in which 64 patients received low-dose H2RA and five received high-dose H2RA. The AR of PU whilst on low-dose H2RA in NSAID users was 0.08 % (0.06–0.11), and the AR was 0.02 % (0.01–0.05) whilst on high-dose H2RA. The overall AR of PU was 0.07 % (0.05–0.09), approximately 1 per 1,479 patients.
The IR of PU in NSAID users whilst on low-dose H2RA was 13.3 per 1,000 patient-years (10.4–17.0), whereas the IR was 4.1 per 1,000 patient-years (1.7–9.9) whilst on high-dose H2RA. The overall IR of PU in these NSAID users was 11.4 per 1,000 patient-years (9.0–14.5).
3.3 Number Needed to Treat
The NNT to prevent PUs among NSAID users in Hong Kong would be 1/([64/77,509]−[5/24,533]) = 1,608, if the estimated effect was seen in a randomized trial. We estimated that an average of 48 cases of PU could have been prevented if all patients were given high-dose H2RA during the study period.
3.4 Adjusted Relative Risk of PU Hospitalization
The adjusted RR of PU comparing high-dose with low-dose H2RA in NSAID users was 0.32 (0.13–0.79), indicating the superior effectiveness of high-dose H2RA in preventing NSAID-associated PUs in this study population (Table 6).
Patients aged 65 years or above showed a significantly higher risk of experiencing PU, with a RR of 11.84 (6.34–22.14) compared with those under 65 years of age. Moreover, the risk of PU was significantly higher in patients with longer treatment duration. Compared with short-term treatment (less than 1 month), the respective RR was 3.94 (2.06–7.55) for 30–60 days’ treatment and 4.76 (2.75–8.23) for treatment longer than 2 months.
Patients receiving concurrent antiplatelet agents showed a significantly higher risk of PU than those who did not, with an RR of 1.85 (1.08–3.17).
Our results also demonstrate that female and male patients receiving an NSAID plus an H2RA showed a similar risk of PU, with a RR of 0.69 (0.43–1.11). In addition, there was no significant difference in PU risk for patients receiving different doses or types of NSAID.
3.5 Sensitivity and Subgroup Analyses
All sensitivity analyses yielded similar results to those of the main analysis (Table 6). In terms of subgroup analysis, 24,117 patients were aged 65 or above, 7,469 patients had 30–60 days of treatment, and 8,469 patients had over 60 days of treatment. Subgroup analysis showed that, among elderly patients, high-dose H2RA was able to significantly lower the PU risk compared with low-dose H2RA, with an RR of 0.36 (0.15–0.91) (Table 1 of the electronic supplementary material). High-dose H2RA users of longer duration (30–60 days or over 60 days) were less likely to experience PU than low-dose H2RA users; however, the results were not statistically significant.
4 Discussion
4.1 Comparisons with Other Studies and Implications of Results
Indirect comparison from the Cochrane meta-analysis shows that high-dose H2RAs are not significantly more effective than low-dose H2RAs in the prophylaxis of endoscopic PUs [17]. To our knowledge, our study was the first to demonstrate that the risk of clinical PU was significantly lower among new NSAID users prescribed with high-dose compared with low-dose H2RAs. H2RAs suppress both the basal and stimulated acid secretion by blocking histamine type-2 receptors on the parietal cells, therefore serving as GPAs commonly used for prophylaxis or treatment of NSAID-associated PU. As an inverse agonist and competitive antagonist of histamine, the dose-dependent effect of H2RAs may be the reason that high-dose H2RA has higher efficacy for the prophylaxis of NSAID-associated PU [35–37].
Current guidelines recommend that for patients at high risk (e.g. prior PU or more than two GI risk factors) or moderate risk (one to two GI risk factors) of PU, NSAID plus misoprostol or PPIs should be used rather than H2RAs [28, 38, 39]. However, Ho et al. [19] reported that of the NSAID users who developed ulcer bleeds while on GPA prophylaxis, approximately 80 % received an H2RA rather than a PPI in Hong Kong. The choice of H2RA over PPI is likely to be influenced by the fact that PPI costs up to 30 times more than H2RA in Hong Kong. A pharmacoeconomic study conducted by Brown et al. [40] also concluded that the optimal strategy for PU prophylaxis in NSAID users depends on ‘willingness-to-pay’, and co-therapy with H2RAs is the least costly strategy. Another economic analysis even suggested that H2RAs be co-prescribed to all NSAID users for ulcer prophylaxis, especially among patients with low to average PU risk [11]. To date, H2RAs are much more commonly prescribed than PPIs in Hong Kong due to cost constraints; however, studies report that PPI prescriptions have overtaken those of H2RAs in NSAID users in other countries such as Australia, the Netherlands, and Spain [41–43].
However, our results showed that among the NSAID users concurrently receiving H2RAs, 76 % received low-dose H2RAs as primary prophylaxis for PU compared with 24 % of patients receiving high-dose H2RAs. This might be of concern for clinical practice in Hong Kong, since high-dose H2RAs should be preferred given the evidence of greater prophylactic effect compared with low dose [8]. Although the choice of H2RAs for PU prophylaxis among NSAID users is to some extent reasonable in Hong Kong, high-dose H2RAs should be prescribed over low-dose H2RAs.
The overall AR of PU in users prescribed an NSAID with an H2RA was 69 per 102,042 patients (0.07 %), which is much lower than that reported in the literature [6, 44]. The most probable explanation for this low absolute PU risk is due to the ‘new user’ and ‘new patient’ design of our study. Since patients with prior PU, NSAID/GPA exposure, H. pylori infection, or previous GI endoscopy procedures at the screening period were excluded, it is not surprising that PU risks among these new patients are much lower.
In line with previous studies, our results showed that patients aged 65 or above posed a significantly higher risk of NSAID-associated PU, with a RR of 11.84 (6.34–22.14). Furthermore, longer NSAID treatment duration led to an approximately three- to fourfold higher risk of PU. Subgroup analysis showed the greater protective effect of high-dose compared with low-dose H2RAs in the elderly subgroup. High-dose H2RA users of longer duration (30–60 days or over 60 days) were also less likely to experience PU than low-dose-H2RA users; however, the results did not reach significance, possibly due to the low number of patients with PU in the subgroup. Nevertheless, these findings highlight the importance of an appropriate approach to PU prophylaxis in clinical practice among elderly NSAID users. Shorter NSAID treatment duration is preferred and high-dose H2RAs should be used for PU prophylaxis.
Previous studies and guidelines have stated that concurrent use of corticosteroids, anticoagulants, or antiplatelet agents are well established risk factors for NSAID-associated GI events [28, 45–47]. Our results show that concomitant use of antiplatelet agents resulted in a higher risk of clinical PU among NSAID users, despite the dosage of H2RA. However, there was no significant difference in PU risk between patients with and without concurrent treatment of corticosteroids or anticoagulants. The study is not adequately powered to detect the difference, due to the scant number of PU cases and small proportion of concomitant use of these drugs (less than 10 %) among these new users of NSAIDs plus H2RAs.
MacDonald et al. [6] reported that patients receiving medium- or high-dose NSAIDs had a higher risk of developing complicated GI events, with RRs of 1.41 (1.03–1.93) and 1.92 (1.18–3.14), respectively. However, medium- or high-dose NSAIDs posed similar risks for overall GI events as low-dose NSAIDs, with RRs of 1.25 (0.98–1.58) and 1.39 (0.93–2.07). From our findings, a slight tendency was also shown towards a non-significantly higher risk of PU in patients receiving medium/high-dose NSAIDs, with an RR of 1.05 (0.37–2.94). In addition, MacDonald et al. [6] showed that, compared with ibuprofen, the RR of an upper GI adverse event was 1.35 (0.69–2.62) among diclofenac users and 1.44 (0.92–2.45) among naproxen users. Our results also demonstrated that diclofenac and naproxen had a statistically non-significant higher PU risk than ibuprofen.
4.2 Strengths and Limitations of Study
To our knowledge, this is the first pharmacoepidemiological study comparing high-dose versus low-dose H2RAs in the prophylaxis of NSAID-associated PU. One major advantage of our study is that the diagnosis of PU was identified by ICD-9-CM diagnostic codes as an outcome rather than the endoscopic PU commonly used in clinical trials. Therefore, our study adds significant knowledge to the role of H2RAs in the prophylaxis of NSAID-associated PU in real-life practice. Further, we chose the ‘new user’ [48] and ‘new patient’ study design, which focused on the primary prophylaxis of PU in patients with no previous drug exposures or PU history. This allowed us to specifically investigate new users with a low risk of PU, contributing important knowledge to guide current practice. By applying the new-user design, as all subjects enter the study at the same time with no previous drug exposures or outcomes, we avoid ‘survival bias’, providing a more accurate estimation of risk [48].
Several limitations should be acknowledged. Similar to databases from clinical healthcare management systems in Europe, such as the Clinical Practice Research Datalink (CPRD, previously known as the General Practice Research Database [GPRD]) [49], CDARS does not include over-the-counter (OTC) medicines and data from private healthcare providers. This might have led to a potential underestimation of NSAID or GPA use among the study population. However, as the Hong Kong HA provides territory-wide healthcare, which is available to all residents, the impact of missing private or OTC prescriptions is likely to be minimal [50]. Similar to other pharmacoepidemiological studies using databases, since we used the prescription record as a reflection of drug exposure, non-adherence cannot be directly addressed. However, we addressed this issue using sensitivity analysis and our conclusions are robust. There is a possibility that patients who were ‘perceived’ to be at higher PU risk might have been prescribed high-dose H2RA. Therefore, our study might be biased against high-dose H2RA and may have underestimated its protective effects. Finally, we focused on a group of short-term users who received a single prescription for an NSAID; thus, our findings may not be generalizable to other patient groups, such as those on long-term NSAID treatment. Further investigation involving patients with multiple NSAID prescriptions for long-term conditions/treatment using propensity scores could be conducted to evaluate different patient groups.
5 Conclusion
High-dose H2RA showed greater effectiveness than low-dose H2RA in the primary prophylaxis of PU in short-term new users of NSAIDs. The co-prescribing rate of low-dose H2RA was threefold that of high-dose H2RA for the primary prophylaxis of NSAID-associated PUs in Hong Kong, and such practice should be discouraged.
Authorship
Guarantor of the article: YH, EWC and ICKW.
YH, EWC and ICKW contributed to the conception, development and design of the study. YH reviewed the literature. YH, KKCM and WCYL contributed to the analysis of data. YH, EWC, KKCM, WCYL, WKL, LMH, and ICKW contributed to the interpretation of data. YH drafted the article. EWC, KKCM, WCYL, WKL, LMH, and ICKW revised it critically for important intellectual content. EWC and ICKW provided oversight for all aspects of this study. All authors had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of data analysis. All authors provided final approval of the version to be published.
References
Lee YC. Effect and treatment of chronic pain in inflammatory arthritis. Curr Rheumatol Rep. 2013;15(1):300.
Kingsbury SR, Hensor EM, Walsh CA, Hochberg MC, Conaghan PG. How do people with knee osteoarthritis use osteoarthritis pain medications and does this change over time? Data from the osteoarthritis initiative. Arthritis Res Ther. 2013;15(5):R106.
Rott KT, Agudelo CA. Gout. JAMA. 2003;289(21):2857–60.
Grosser T, Smyth E, FitzGerald GA. Anti-inflammatory, antipyretic, and analgesic agents; pharmacotherapy of gout. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman & Gilman’s. The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011.
Patrignani P, Tacconelli S, Bruno A, Sostres C, Lanas A. Managing the adverse effects of nonsteroidal anti-inflammatory drugs. Expert Rev Clin Pharmacol. 2011;4(5):605–21.
MacDonald TM, Morant SV, Robinson GC, Shield MJ, McGilchrist MM, Murray FE, et al. Association of upper gastrointestinal toxicity of non-steroidal anti-inflammatory drugs with continued exposure: cohort study. BMJ. 1997;315(7119):1333–7.
Lanza FL. A guideline for the treatment and prevention of NSAID-induced ulcers. Members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. Am J Gastroenterol. 1998;93(11):2037–46.
Rostom A, Muir K, Dube C, Lanas A, Jolicoeur E, Tugwell P. Prevention of NSAID-related upper gastrointestinal toxicity: a meta-analysis of traditional NSAIDs with gastroprotection and COX-2 inhibitors. Drug Healthc Patient Saf. 2009;1(1):47–71.
Hooper L, Brown TJ, Elliott RA, Payne K, Roberts C, Symmons D. The effectiveness of five strategies for the prevention of gastrointestinal toxicity induced by non-steroidal anti-inflammatory drugs: systematic review. BMJ. 2004;329(7472):948–52.
Lancaster-Smith MJ, Jaderberg ME, Jackson DA. Ranitidine in the treatment of non-steroidal anti-inflammatory drug associated gastric and duodenal ulcers. Gut. 1991;32(3):252–5.
Elliott RA, Hooper L, Payne K, Brown TJ, Roberts C, Symmons D. Preventing non-steroidal anti-inflammatory drug-induced gastrointestinal toxicity: are older strategies more cost-effective in the general population? Rheumatology. 2006;45(5):606–13.
Lazzaroni M, Porro GB. Management of NSAID-induced gastrointestinal toxicity focus on proton pump inhibitors. Drugs. 2009;69(1):51–69.
Moore A, Bjarnason I, Cryer B, Garcia-Rodriguez L, Goldkind L, Lanas A, et al. Evidence for endoscopic ulcers as meaningful surrogate endpoint for clinically significant upper gastrointestinal harm. Clin Gastroenterol Hepatol. 2009;7(11):1156–63.
Wolde ST, Dijkmans BA, Janssen M, Hermans J, Lamers CB. High-dose ranitidine for the prevention of recurrent peptic ulcer disease in rheumatoid arthritis patients taking NSAIDs. Aliment Pharmacol Ther. 1996;10(3):347–51.
Hudson N, Taha AS, Russell RI, Trye P, Cottrell J, Mann SG, et al. Famotidine for healing and maintenance in nonsteroidal anti-inflammatory drug-associated gastroduodenal ulceration. Gastroenterology. 1997;112(6):1817–22.
Graham DY. Endoscopic ulcers are neither meaningful nor validated as a surrogate for clinically significant upper gastrointestinal harm. Clin Gastroenterol Hepatol. 2009;7(11):1147–50.
Rostom A, Dube C, Wells GA, Tugwell P, Welch V, Jolicoeur E, McGowan J, Lanas A. Prevention of NSAID-induced gastroduodenal ulcers (Review). The Cochrane Collaboration; 2011(6):1–176.
Yeomans ND, Tulassay Z, Juhasz L, Racz I, Howard JM, van Rensburg CJ, et al. A comparison of omeprazole with ranitidine for ulcers associated with nonsteroidal antiinflammatory drugs. Acid suppression trial: ranitidine versus omeprazole for NSAID-associated Ulcer Treatment (ASTRONAUT) Study Group. N Engl J Med. 1998;338(11):719–26.
Ho CW, Tse YK, Wu B, Mulder CJ, Chan FK. The use of prophylactic gastroprotective therapy in patients with nonsteroidal anti-inflammatory drug- and aspirin-associated ulcer bleeding: a cross-sectional study. Aliment Pharmacol Ther. 2013;37(8):819–24.
Hospital Authority. Introduction (Accessed on: 15 November 2013). Available from: http://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10008&Lang=ENG&Dimension=100&Parent_ID=10004.
Information Services Department HKSARG. Hong Kong: The facts 2013 (Accessed on:15 November 2013). Available from: http://www.gov.hk/en/about/abouthk/factsheets/docs/population.pdf.
Hospital Authority. Clusters, Hospitals & Institutions (Accessed on:15 November 2013). Available from: http://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10036&Lang=ENG&Dimension=100&Parent_ID=10004.
Wong MC, Tam WW, Cheung CS, Tong EL, Sek AC, John G, et al. Initial antihypertensive prescription and switching: a 5 year cohort study from 250,851 patients. PLoS One. 2013;8(1):e53625.
Mok CC, Kwok CL, Ho LY, Chan PT, Yip SF. Life expectancy, standardized mortality ratios, and causes of death in six rheumatic diseases in Hong Kong. China. Arthritis Rheum. 2011;63(5):1182–9.
Cheuk BL, Cheung GC, Cheng SW. Epidemiology of venous thromboembolism in a Chinese population. Br J Surg. 2004;91(4):424–8.
Chui CS, Man KK, Cheng CL, Chan EW, Lau WC, Cheng VC et al. An investigation of the potential association between retinal detachment and oral fluoroquinolones: a self-controlled case series study. J Antimicrob Chemother. Epub ahead of print 2014 May 15.
Joint Formulary Committee. British National Formulary (BNF). 63rd ed. London: BMJ Group and Pharmaceutial Press; 2012.
Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728–38.
Gutthann SP, Garcia Rodriguez LA, Raiford DS. Individual nonsteroidal antiinflammatory drugs and other risk factors for upper gastrointestinal bleeding and perforation. Epidemiology. 1997;8(1):18–24.
Langman MJ, Weil J, Wainwright P, Lawson DH, Rawlins MD, Logan RF, et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994;343(8905):1075–8.
Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Statist Assoc. 1927;22(158):209–12.
Rothman KJ, Greendland S. Modern Epidemiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1998.
Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ. 1995;310(6977):452–4.
Kelsey JL, Whittemore AS, Evans AS, Thompson WD. Methods in Observational Epidemiology. 2nd ed. New York: Oxford University Press; 1996.
Tuskey A, Peura D. The use of H2 antagonists in treating and preventing NSAID-induced mucosal damage. Arthritis Res Ther. 2013;15(Suppl 3):S6.
Mejia A, Kraft WK. Acid peptic diseases: pharmacological approach to treatment. Expert Rev Clin Pharmacol. 2009;2(3):295–314.
Chan FK, Sung JJ. Role of acid suppressants in prophylaxis of NSAID damage. Best Pract Res Clin Gastroenterol. 2001;15(3):433–45.
National Institute for Health and Care Excellence. NSAIDs: prescribing issues summary 2013 (Accessed on: 3 Nov 2013). Available from: http://cks.nice.org.uk/nsaids-prescribing-issues#!scenariorecommendation:3.
Rostom A, Moayyedi P, Hunt R. Canadian consensus guidelines on long-term nonsteroidal anti-inflammatory drug therapy and the need for gastroprotection: benefits versus risks. Aliment Pharmacol Ther. 2009;29(5):481–96.
Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al. A comparison of the cost-effectiveness of five strategies for the prevention of non-steroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling. Health Technol Assess. 2006;10(38):1–183.
Barozzi N, Tett SE. Gastroprotective drugs in Australia: utilization patterns between 1997 and 2006 in relation to NSAID prescribing. Clin Ther. 2009;31(4):849–61.
Valkhoff VE, van Soest EM, Sturkenboom MC, Kuipers EJ. Time-trends in gastroprotection with nonsteroidal anti-inflammatory drugs (NSAIDs). Aliment Pharmacol Ther. 2010;31(11):1218–28.
Lopez-Pintor E, Lumbreras B. Use of gastrointestinal prophylaxis in NSAID patients: a cross sectional study in community pharmacies. Int J Clin Pharm. 2011;33(2):155–64.
Laine L. Approaches to nonsteroidal anti-inflammatory drug use in the high-risk patient. Gastroenterology. 2001;120(3):594–606.
Kang JM, Kim N, Lee BH, Park HK, Jo HJ, Shin CM, et al. Risk factors for peptic ulcer bleeding in terms of Helicobacter pylori, NSAIDs, and antiplatelet agents. Scand J Gastroenterol. 2011;46(11):1295–301.
Laine L, Curtis SP, Cryer B, Kaur A, Cannon CP. Risk factors for NSAID-associated upper GI clinical events in a long-term prospective study of 34,701 arthritis patients. Aliment Pharmacol Ther. 2010;32(10):1240–8.
Laine L. GI risk and risk factors of NSAIDs. J Cardiovasc Pharmacol. 2006;47(Suppl 1):S60–6.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Masclee GM, Valkhoff VE, van Soest EM, Schade R, Mazzaglia G, Molokhia M, et al. Cyclo-oxygenase-2 inhibitors or nonselective NSAIDs plus gastroprotective agents: what to prescribe in daily clinical practice? Aliment Pharmacol Ther. 2013;38(2):178–89.
WHO and Hong Kong Department of Health. Hong Kong (China) Health Service Delivery Profile 2012 (Accessed on:15 Novermber 2013). Available from: http://www.wpro.who.int/health_services/service_delivery_profile_hong_kong_%28china%29.pdf.
Acknowledgments
The authors thank Dr. Vincent C.C. Cheng for his support on the verification of ICD-9-CM codes for related diagnosis/procedures in this study. We also thank Lisa Wong for proofreading and editing the manuscript.
Declaration of funding interests
None to declare.
Declaration of competing interest
Ying He, Esther W. Chan, Kenneth K.C. Man, Wallis C.Y. Lau, Wai K. Leung, Lai M. Ho, and Ian C.K. Wong declare no support from any organization for the submitted work; no financial relationships with any organization that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval
The study protocol was approved by Institutional Review Board of the University of Hong Kong/HA Hong Kong West Cluster (IRB reference number: UW 12-196).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, Y., Chan, E.W., Man, K.K.C. et al. Dosage Effects of Histamine-2 Receptor Antagonist on the Primary Prophylaxis of Non-Steroidal Anti-Inflammatory Drug (NSAID)-Associated Peptic Ulcers: A Retrospective Cohort Study. Drug Saf 37, 711–721 (2014). https://doi.org/10.1007/s40264-014-0209-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-014-0209-0