Abstract
Biosimilars are biological medicines, the active substances of which are highly similar to those of biologics that have already been authorized. As for any other medicine, the applicant of the biosimilar marketing authorization must submit a risk-management plan (RMP)/pharmacovigilance plan. The pharmacovigilance plan should take into account risks identified during product development, the potential risks and how those risks will be addressed after authorization of the product.
Recently, new European Pharmacovigilance legislation has been implemented, ensuring proper risk management through the recording of suspected adverse drug reactions and data collection from all stakeholders. The new regulation entails a reduction of the administrative burden on companies and regulatory agencies, as obligations of the responsible parties are clearly established and duplication of effort avoided.
This article analyzes the new European Pharmacovigilance System requirements, with special focus on those medicines requiring additional monitoring, such as biosimilars, which are priorities for pharmacovigilance. Further, it provides the new obligations to marketing authorization holders, such as the continuous benefit–risk assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Implications of the New European Pharmacovigilance Legislation
Pharmacovigilance is the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other medicine-related problem. According to this definition, the objective of the EU legislation for pharmacovigilance is to prevent harm from adverse reactions in humans arising from the use of authorized medicinal products within or outside the terms of marketing authorization or from occupational exposure; promoting the safe and effective use of medicinal products through timely information about the safety to patients, healthcare professionals and the public. In December 2010, the European Parliament and European Council adopted new pharmacovigilance legislation [1, 2]. This legislation, which has been effective since July 2012, is the biggest change to the regulation of human medicines in the EU since 1995.
With the application of the new pharmacovigilance legislation, Volume 9A of Eudralex [3], containing pharmacovigilance guidelines for medicinal products, is replaced by the good pharmacovigilance practice (GVP) guidelines released by the European Medicines Agency (EMA or the Agency). However, in cases where GVP modules have not yet been developed, Volume 9A remains the reference.
The new legislation has significant implications for applicants and holders of EU marketing authorizations. The legislation aims to:
-
make roles and responsibilities clear;
-
minimise duplication of effort;
-
free up resources by rationalizing and simplifying periodic safety update reports (PSURs) and adverse drug reaction (ADR) reporting; and
-
establish a clear legal framework for post-authorization monitoring.
The term ‘adverse reaction’ has been amended to ensure that it covers noxious and unintended effects resulting not only from the authorised use of a medicinal product at normal doses, but also from medication errors and uses outside the terms of the marketing authorization, including the misuse and abuse of the medicinal product [2]. Thus, the new definition of ‘adverse reaction’ is as follows: a response to a medicinal product which is noxious and unintended.
The EMA is responsible for implementing most of the new legislation. The pharmacovigilance legal requirements and GVP apply to all medicinal products authorized in the EU.
2 Structure of the Good Pharmacovigilance Practices
Pharmacovigilance activities comprise distinct but connected processes, organized in 16 modules [4], and each GVP module features one major pharmacovigilance process. Table 1 shows the list of GVP modules, with the effective date of the finalized modules and those currently under development. Most modules are available in their final version.
In order to strengthen the safety monitoring of medicinal products, the 2010 EU Pharmacovigilance legislation, further amended in 2013 [5], has established a risk-balanced framework to enhance data collection of post-authorized medical products, including the concept of additional monitoring for certain medicinal products.
The concept of additional monitoring originates primarily from the need to enhance the ADR reporting rates for newly authorised products for which the safety profile might not be fully characterised or for products with newly emerging safety concerns that also need to be better characterised. The main goals are to collect additional information as early as possible to further elucidate the risk profile of products when used in clinical practice and thereby informing the safe and effective use of medicinal products.
The additional monitoring status is particularly important when granting marketing authorization for medicinal products containing a new active substance and for all biological medicinal products, including biosimilars for which there is limited post-marketing experience. The approval pathway for a biosimilar is based on the determination of its similarity to an approved biologic based on fewer patient data than were required for the initial approval of the reference product [6]. This abbreviated approval pathway for biosimilars entails the need for collection of safety data through effective post-approval safety surveillance systems that accurately track and trace all biopharmaceuticals [7].
Competent authorities may also require additional monitoring status for a medicinal product that is subject to specific obligations, e.g., the conduct of a post-authorization safety study or restrictions with regards to the safe and effective use of the medicinal product. In April 2013, the EMA published the initial list of medicines that are subject to additional monitoring [8].
Medicines subject to additional monitoring will have to display an inverted black triangle (▼) followed by the statement “This medicinal product is subject to additional monitoring” in their package leaflet and in the information for healthcare professionals (the summary of product characteristics [SmPC]), together with a short sentence explaining what the triangle means.
If a medicine is labelled with the inverted black triangle, it does not mean that it is unsafe; the purpose of the symbol is to actively encourage healthcare professionals and patients to report any suspected adverse reactions observed with the medicine, either because the medicine is new to the market or because there is a limitation to the data available on its safety. It is important to note that the additional monitoring status needs to be communicated to healthcare professionals and patients in such a way that it increases reporting of suspected adverse reactions without creating undue alarm. This can be achieved, for example, by highlighting the need to better characterise the safety profile of a new medicinal product by identifying additional risks but placing those potential risks in the context of the known benefits for this product. A medicine can be included on this list when it is approved for the first time or at any time during its life cycle. It remains under additional monitoring for 5 years or until the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) decides to remove it from the list, usually because studies have further established the safety profile of the product concerned. The PRAC is the body mandated to review risk-management plans (RMPs, which is a detailed description of the risk-management system) and make recommendations on their content and on the suitability of proposed pharmacovigilance activities and risk-minimisation measures (measures to prevent or minimise the risks). For centrally authorised products, only additional risk-minimisation measures that are recommended by the PRAC and subsequently agreed by the Committee for Medicinal Products for Human Use (CHMP) will be allowed in the risk-minimisation plan.
3 Risk Management
GVP Module V specifies the monitoring conditions in the risk-management system. Risk management aims to ensure that the benefits of a particular medicinal product (including biosimilars) exceed the risks by the greatest achievable margin for the individual patient and for the target population as a whole.
Marketing authorization holders (MAHs) should plan pharmacovigilance measures for each individual medicinal product in the context of a risk-management system. The measures should be proportionate to the identified risks, the potential risks, and the need for additional information on the medicinal product. It should also be ensured that any key measures included in a risk-management system are made conditions of the marketing authorisation.
There are specific terms used in the new European pharmacovigilance legislation (Table 2).
In general, risk management has several stages:
-
1.
Characterisation of the safety profile of the medicinal product, including what is known and not known.
-
2.
Planning of pharmacovigilance activities to characterise risks and identify new risks and increase the knowledge in general about the safety profile of the medicinal product.
-
3.
Planning and implementation of risk minimisation and mitigation and assessment of the effectiveness of these activities.
Risk management can be represented as a cycle with various steps (Fig. 1).
However, the actions and responsibilities within each step of the cycle will vary according to whether the stakeholder is the MAH, competent authorities, a healthcare professional or a patient. Other players may be involved in risk–benefit management (e.g. patient organisations, health authorities, national safety organisations, environmental advisors, pharmaceutical distributors, etc.), but their roles will usually be smaller and complementary to that of the main players (stakeholders).
3.1 Responsibilities for Risk Management
The main organisations directly involved in the RMPs of medicinal products are applicants/MAH and the regulatory authorities. Within the EU, responsibility for authorisation and supervision of medicinal products is shared between competent authorities in the member states of the European Commission and the EMA.
3.2 Marketing Authorisation Holders and Applicants
In relation to risk management of its biosimilar products, an applicant/MAH is responsible for:
-
ensuring that it constantly monitors the risks of its medicinal products in compliance with relevant legislation and reporting the results of this process, as required, to the appropriate competent authorities;
-
taking all appropriate actions to minimise the risks of the medicinal product and maximising the benefits, including ensuring the accuracy of all information produced by the company in relation to its medicinal products, and actively updating and promptly communicating it when new information becomes available.
4 Risk-Management Plan (RMP)
RMPs are normally required for new active substances, biosimilars, and medicinal products for paediatric use and for medicinal products for human use involving a significant change in the marketing authorisation, including a new manufacturing process of a biotechnologically derived medicinal product.
Although the primary aim and focus of the RMP remains that of risk management, the evaluation of the need for efficacy studies and their integration, where necessary, in the RMP may enable resources to be used more efficiently and for risks to be put into context.
Producing an RMP requires the input of different specialists and departments within and/or outside an organisation. The product safety specification may require involvement of toxicologists, clinical pharmacologists, clinical research physicians, pharmacoepidemiologists and pharmacovigilance experts (Fig. 2). The input required for the pharmacovigilance plan may require any of these experts depending upon the safety concerns identified in the safety specification and the types of activities planned to address them. Regardless of who prepares the RMP, the responsibility for the content and accuracy of the RMP remains with the applicant/MAH. Someone with the appropriate scientific background within the company has to ensure oversight.
4.1 Objectives of the RMP
An RMP has the following goals:
-
describing what is known and not known about the safety profile of a medicine;
-
planning how to characterise the safety profile of the medicine further;
-
putting measures in place to prevent or minimise risks associated with the product and assessing the effectiveness of those interventions;
-
documenting the need for efficacy studies and maximising the benefit–risk balance of the product for the individual patient and for the target population as a whole, and facilitating integration of benefit–risk planning;
-
indicating the level of certainty with which efficacy shown in clinical trial populations will be seen when the biosimilar is used in the wider target populations, and documenting the need for studies on efficacy in the post-authorisation phase;
-
describing how the effectiveness of risk-minimisation measures will be assessed.
To achieve these goals, the RMP must contain some elements in order to:
-
identify or characterise the safety profile of the biosimilar product concerned;
-
indicate how to characterise the safety profile of the biosimilar product further;
-
document measures to prevent or minimise the risks associated with the biosimilar product;
-
document post-authorisation obligations that have been imposed as a condition of the marketing authorisation.
The RMP is a dynamic, stand-alone document that should be updated throughout the life-cycle of the biosimilar product.
4.2 Structure of the RMP
The RMP consists of seven parts (Table 3) [4]. Some of these parts, such as the safety specification, are subdivided into modules so the content can be tailored to the specifics of the biosimilar product and modules added/removed or re-used in other documents (e.g. PSURs) (Table 4). It should be noted that module SI (Epidemiology of the indication[s] and target population[s]) is not required for biosimilar marketing applications.
The risk-management system shall be proportional to the identified risks and the potential risks of the biosimilar product, and the need for post-authorisation safety data.
The purpose of the safety specification is to provide a synopsis of the safety profile of the biosimilar product and should include what is known and not known about that product. It should be a summary of the important identified risks of the biosimilar product, important potential risks, and important missing information. It should also address the populations potentially at risk, and outstanding safety questions that ensure further investigation to refine understanding of the risk–benefit profile during the post-authorisation period. In the RMP, the safety specification will form the basis of the pharmacovigilance plan, and the risk minimisation plan.
Depending on the nature of the biosimilar product and its development programme, additional elements can be included in the safety specification. Elements that need to be incorporated include the following:
-
quality aspects, if relevant in relation to the safety and efficacy of the product, e.g. characterisation of glycosylation and validation of potency assays;
-
the disposal of the product where it might pose a particular risk because of remaining active substance (e.g. patches);
-
innovative pharmaceutical forms; or
-
use with a medical device.
The RMP module SIV should discuss which sub-populations within the expected target population have not been studied or have only been studied to a limited degree in the clinical trial population. The implications, with respect to predicting the safety of the product in the marketplace, of any of these populations with limited or no research, should be explicitly discussed. Populations to be considered should include the following:
-
paediatric population;
-
elderly population;
-
pregnant or breast-feeding women;
-
patients with hepatic impairment;
-
patients with renal impairment;
-
patients with other relevant co-morbidity;
-
patients with disease severity different from that studied in clinical trials;
-
sub-populations carrying known and relevant genetic polymorphisms;
-
patients of different racial and/or ethnic origins.
Module SVII of the RMP safety specification (Part II) should provide concise information on the important identified and potential risks. Normally, any risk that is clinically important and is, or is likely to be, included in the contraindications or warnings and precautions section of the SmPC should be included here.
Detailed risk data should include the following:
-
frequency;
-
public health impact (severity and seriousness/reversibility/outcomes);
-
impact on the individual patient (effect on quality of life);
-
risk factors (patient factors, dose, additive or synergistic factors);
-
preventability (i.e. predictability of a risk, whether risk factors have been identified, or possibility of detection at an early stage);
The pharmacovigilance plan (RMP part III) intends to discuss how the applicant/MAH plans to identify and/or characterise the risks identified in the safety specification. It provides a structured plan for:
-
the identification of new safety concerns;
-
further characterisation of known safety concerns including elucidation of risk factors;
-
the investigation of whether a potential safety concern is real or not;
-
how important missing information will be sought.
In order to allow all competent authorities to receive, access simultaneously and share pharmacovigilance information for medicinal products for human use authorised in the EU, several European medicines databases will be strengthened [9]: EudraVigilance (central EMA computer database designed to manage information on medicines safety reports), EudraPharm (database of medicinal products authorised in the EU), the European Pharmacovigilance issues Tracking Tool (EPITT, which facilitates the sharing of safety information of medicines between the national competent authorities and the Agency), as well as the European safety portal to better inform the public on all safety issues. Specifically, EudraVigilance allows the EMA to manage the electronic data exchange of Individual Case Safety Reports (ICSRs, documents providing the most complete information related to individual cases at a certain point of time) and to support EU pharmacovigilance activities. The product information at EudraVigilance should be fully and permanently accessible to the Member States, the Agency and the Commission, and accessible to an appropriate extent to MAHs and the public. That information is received in the form of the Extended EudraVigilance Medicinal Product Dictionary (XEVMPD), enabling the Agency to populate Eudrapharm with all medicinal products across the EU.
As for the ‘Plans for post-authorisation efficacy studies’, it needs to be considered that efficacy, as assessed at the time of authorisation, is based on data from clinical trials, which, by their nature, are of relatively limited duration. Whereas it is recognised that many risks will be identified post-authorisation, there is an implicit assumption that efficacy remains relatively constant over time. This may not always be valid.
For many medicines, there will not be a need for post-authorisation efficacy studies. However, there may be circumstances where efficacy may vary over time and also patients for whom this assumption of constant efficacy may not be true and where longer-term efficacy data post-authorisation is necessary.
On the basis of the safety specification, an applicant/MAH should assess what risk-minimisation activities are needed for each safety concern. The risk-minimisation plan should provide details of the risk-minimisation measures that will be taken to reduce the risks associated with individual safety concerns. Each safety concern needs to be considered on a case-by-case basis and will depend upon the severity of the risk, the healthcare setting, the indication, the pharmaceutical form and the target population.
In order to measure the effectiveness of risk-minimisation measures, post-authorisation safety studies are included in the pharmacovigilance plan against the specific safety concern(s) as well as described in detail in the risk-minimisation plan. The MAH shall monitor the data generated while the study is being conducted. Any new information that may affect the risk–benefit balance of the medicinal product should be communicated immediately as an emerging safety issue to competent authorities of the member states in which the product is authorised and to the Agency.
The primary post-authorisation pharmacovigilance documents will be the RMP and the PSUR. Although there is some overlap between the documents, the main objectives of the two are different, and the situations in which they are required are not always the same. The main purpose of the PSUR is integrated, post-authorisation risk–benefit assessment, whilst that of the RMP is pre- and post-authorisation risk–benefit management and planning. The PSUR examines the overall safety profile as part of an integrated benefit–risk evaluation of the medicinal product at set time periods and as such will consider the overall benefit–risk profile of the medicinal product. According to the new legislation, any PSUR will follow the new procedure involving the PRAC as detailed in the GVP Module VII. The PSURs have a modular structure that has been introduced to provide structured evaluation.
4.3 Assessment of RMPs
When preparing or reviewing a RMP, there are several points to be considered (Table 5) [4].
Safety specification, pharmacovigilance plan, plans for post-authorisation studies on efficacy and risk-minimisation measures. Table 5 highlights the different aspects to be taken into account for each of these issues. One of the most important factors that influence the success of an RMP is the adequacy in delivering the proposed plan. Therefore, this aspect should also be considered when analysing an RMP.
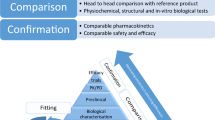
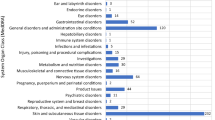
5 Implications for Biosimilars
Biopharmaceuticals are a highly complex category of drugs that are manufactured using living cells. They are manufactured using unique cell lines and proprietary processes that are not available in the public domain. Biosimilars are biological medicines, the active substances of which are highly similar, but not identical, to those of biologics that have already been authorised (the reference product). They have different starting materials and manufacturing processes, which means they can have different characteristics, such as ADRs, that may not be detectable in conventional clinical trials. As for the remainder of recombinant proteins, clinical safety must be monitored closely after their authorisation. Biosimilars are approved via a stringent regulatory pathway demonstrating quality, safety and efficacy comparable to the original product. An increasing number of biosimilar products are under development at the European level, particularly biosimilar monoclonal antibodies. The applicant of the biosimilar marketing authorisation must submit an RMP/pharmacovigilance plan as for other medicines, except for Module SI from Part II (Safety specification), which is not required for biosimilars, as stated in Table 4. The pharmacovigilance plan should take into account risks identified during product development, potential risks and how those risks will be addressed after authorisation of the product. Furthermore, any safety monitoring required for the reference product should be taken into account in the RMP [6].
The approval of a medicinal product is based on a satisfactory balance of benefits and risks within the conditions specified in the product labelling. This decision is based on the information available at the time of approval [10]. The knowledge related to the safety profile of the product can change over time through expanded use in terms of patient characteristics and the number of patients exposed. In particular, during the early post-marketing period, the product might be used in settings different from clinical trials, and a much larger population might be exposed in a relatively short timeframe. Therefore, the pharmacovigilance system should ensure the ability to identify any biopharmaceutical product that is marketed at European level and the subject of adverse reaction reports.
The basic principle in the development of a biosimilar is to establish the similarity between the biosimilar and the reference product by means of the best available techniques, which would guarantee that the safety and efficacy of the reference drug could be extrapolated to the biosimilar. Therefore, it is assumed that the biosimilars that have been granted marketing authorisation at the European level feature safety and efficacy comparable to that of the reference product. Nevertheless, tight pharmacovigilance procedures are required to detect potential differences in safety signals between biosimilars and their reference products. Along with pharmacovigilance activities, prescribing practitioners must ensure that data are consistent and safety signals are assigned to the correct product.
Accordingly, the European legislation requires that, for all ADR reports, all appropriate measures should be taken to identify the brand name and batch number (besides the international nonproprietary name [INN]) of the product concerned. This is especially important for biosimilars [11].
According to the new regulation (EU) No 1235/2010 and Directive 2010/84/EU [1, 2], when considering how to maximise, or assess, the risk–benefit balance, risks need to be understood in the context of benefit. After granting of a marketing authorisation, the competent authority may impose an obligation on the MAH to conduct (i) post-authorisation safety studies if there are concerns about the risks of the authorised medicinal product (the aim of biosimilar risk identification and characterisation is to allow for risk minimisation or mitigation wherever possible); or (ii) post-authorisation efficacy studies, if previous efficacy evaluations might have to be significantly revised (such studies may be aimed at collecting data to enable the assessment of safety or efficacy of medicinal products for human use in everyday medical practice).
The marketing authorisation shall be varied to include the obligation as a condition of the marketing authorisation, and the risk-management system shall be adapted accordingly. Once the product is marketed, new information will be generated that can have an impact on the benefits or risks of the product; evaluation of this information should be a continuous process, in consultation with regulatory authorities. Planning of the necessary pharmacovigilance activities to characterise the safety profile of the biosimilar product will be improved if it is more closely based on specific issues identified from pre- or post-authorisation data and from pharmacological principles.
In terms of the packaging, although biosimilars are centrally authorised products, the information specific to a Member State should be accommodated on the label in a single boxed area, the so-called ‘blue box’, to appear on one side of the pack. Each ‘blue box’ should only be presented in the official language or languages of the Member State concerned and should state the name of that Member State. Nevertheless, where the medicinal product is not intended to be delivered directly to the patient, or where there are problems in respect of the availability of the medicinal product, the competent authorities may grant a full or partial exemption to the obligation that the labelling and the package leaflet must be in an official language or official languages of the Member State where the medicinal product is placed on the market.
6 Clinical Safety of Approved Biosimilars
The primary safety concern, not only for biosimilars but also for all biotechnological medicinal products, is usually immunogenicity, which may be due to different mechanisms such as glycosylation, contamination or changes in the three-dimensional structure, although variation in potency can also raise safety issues in the case of substitution of the original molecule with biosimilars, e.g. variability in haemoglobin values seen with original epoetin [12] and its possible association with increased mortality in dialysis patients [13].
One important factor is potential contamination during manufacturing of biopharmaceuticals. This was the cause of an increasing incidence of antibody-mediated pure red cell aplasia (PRCA), which revealed that a small change in the formulation of an innovator biopharmaceutical product (epoetin alfa) with extensive patient-years experience might have significant clinical consequences [14]. The sharp increase in incidence occurred among patients treated with Eprex® and coincided with replacement of human serum albumin as a stabiliser by polysorbate 80. A modification in the three-dimensional structure of a protein may also have important effects on immunogenicity. In another example, a clinical trial evaluating the immunogenicity of HX575, a recombinant human erythropoietin-alfa biosimilar, was discontinued following the development of neutralising antibodies in two of 163 patients [15]. The manufacturer concluded that the high levels of tungsten, probably leached from the pins used in the manufacturing of the pre-filled syringes, were the possible cause of this rise in immunogenicity. Increasing tungsten levels in the syringes may have contributed to denaturation and aggregation of HX575 proteins [16]. Nevertheless, some adverse effects may take several months to appear [17], and even very small changes in manufacturing can have major consequences for a product’s adverse effects [18, 19].
Any specific safety monitoring imposed on the original product (reference product) or product class should be taken into consideration in the RMP for the biosimilar product. Moreover, potential additional risks identified during the review of the data obtained with the biosimilar should be subject to further safety monitoring (e.g. increased immunogenicity that might result from a difference in the glycosylation profile).
Manufacturers should ensure that, at the time of the marketing authorisation, they have an appropriate pharmacovigilance system in place, including the services of a qualified person responsible for monitoring pharmacovigilance and the necessary means for the notification of adverse reactions that occur in any of the countries in which the product is marketed. Pharmacovigilance systems (as defined in the current EU legislation) and procedures (including traceability as described in the current EU guidelines) to achieve this monitoring should be in place when a marketing authorisation is granted.
Once the marketing authorisation is obtained, compliance of manufacturers with their marketing commitments, where appropriate, and with their pharmacovigilance obligations, will be closely monitored.
7 Conclusions
There is a need for carefully designed pharmacovigilance programmes to monitor all biopharmaceuticals, including innovator products and biosimilars, for safety and efficacy issues during the post-approval period. The new European pharmacovigilance legislation has clarified the responsibilities of the MAHs in this area. The MAH should be responsible for continuously monitoring the safety of its medicinal products for human use, for informing the authorities of any changes that might have an impact on the marketing authorisation, and for ensuring that the product information is kept up to date. All pharmacovigilance referrals are discussed by the new PRAC and the CHMP.
The new EU pharmacovigilance system ensures proper risk-management through the recording of suspected ADRs and data collection in the form of post-authorisation safety studies (PASS). At the same time, the administrative burden on biosimilar companies is reduced, as obligations of the responsible parties are clearly established and duplication of efforts is avoided.
Likewise, this regulation has amended the scope of PSURs so that they present an analysis of the risk–benefit balance of a medicinal product rather than a detailed listing of individual case reports already submitted to the EudraVigilance database. Obligations imposed in respect of PSURs should be proportionate to the risks posed by medicinal products.
At the approval stage of any biological medicinal product, including biosimilars, there is limited clinical experience. Accurate pharmacovigilance and correct attribution of adverse events is vital and therefore an adequate system is necessary to ensure specific identification of the biosimilar. Therefore, an adverse reaction report for a biosimilar product should specify, besides the INN, the brand name, company’s name and lot number, in order to guarantee its traceability.
References
Regulation (EU) No 1235/2010 of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance of medicinal products for human use, Regulation (EC) No 726/2004 laying down Community procedures for the authorisation and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency, and Regulation (EC) No 1394/2007 on advanced therapy medicinal products. Official Journal of the European Union L 348/1, 31/12/2010.
Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance, Directive 2001/83/EC on the Community code relating to medicinal products for human use. Official Journal of the European Union L 348/74, 31/12/2010.
EudraLex [Homepage]. Volume 9A guidelines on pharmacovigilance for medicinal products for human use. In: The rules governing medicinal products in the European Union. 2007. http://ec.europa.eu. Accessed 1 Jul 2013.
EMA/838713/2011. Guideline on good pharmacovigilance practices (GVP). Module V: risk management systems. 2012. http://www.ema.europa.eu. Accessed 1 Jul 2013.
Amendments to the pharmacovigilance legislation: new notification requirements for marketing-authorisation holders. 2013. http://www.ema.europa.eu. Accessed 1 Jul 2013.
Zuñiga L, Calvo B. Biosimilars: pharmacovigilance and risk management. Pharmacoepidem Drug Saf. 2010;19:661–9.
Casadevall N, Edwards IR, Felix T, Graze PR, Litten JB, Strober BE, Warnock DG. Pharmacovigilance and biosimilars: considerations, needs and challenges. Expert Opin Biol Ther. 2013;13:1039–47.
EMA/144772/2013. Patient Health Protection. Implementation plan for the introduction of the new pharmacovigilance legislation requirements into the product information of centrally approved medicinal products. 2013. http://www.ema.europa.eu. Accessed 1 Jul 2013.
Borg JJ, Aislaitner G, Pirozynski M, Mifsud S. Strengthening and rationalizing pharmacovigilance in the EU: where is Europe heading to? A review of the new EU legislation on pharmacovigilance. Drug Saf. 2011;34:187–97.
International Conference of Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH E2E: Pharmacovigilance Planning. 2004. http://www.ich.org. Accessed 1 Jul 2013.
Pharmacovigilance Focus. Biosimilar medicines and safety: new challenges for pharmacovigilance. WHO Drug Inf. 2009; 23:87–94. http://www.who.int/druginformation. Accessed 1 Jul 2013.
Berns JS, Elzein H, Lynn RI, Fishbane S, Meisels IS, Deoreo PB. Hemoglobin variability in epoetin-treated hemodialysis patients. Kidney Int. 2003;64:1514–21.
Yang W, Israni RK, Brunelli SM, Joffe MM, Fishbane SC, Feldman HI. Hemoglobin variability and mortality in ESRD. J Am Soc Nephrol. 2007;18:3164–70.
Casadevall N, Nataf J, Viron B, Kolta A, Kiladjian JJ, Martin-Dupont P, Michaud P, Papo T, Ugo V, Teyssandier I, Varet B, Mayeux P. Pure red-cell aplasia and anti-erythropoietin antibodies in patients treated with recombinant erythropoietin. N Engl J Med. 2002;346:469–75.
Haag-Weber M, Eckardt KU, Hörl WH, Roger SD, Vetter A, Roth K. Safety, immunogenicity and efficacy of subcutaneous biosimilar epoetin-alpha (HX575) in non-dialysis patients with renal anemia: a multi-center, randomized, double-blind study. Clin Nephrol. 2012;77:8–17.
Seidl A, Hainzl O, Richter M, Fischer R, Böhm S, Deutel B, Hartinger M, Windisch J, Casadevall N, London GM, Macdougall I. Tungsten-induced denaturation and aggregation of epoetin alfa during primary packaging as a cause of immunogenicity. Pharm Res. 2012;29:1454–67.
Schellekens H. The first biosimilar epoetin: but how similar is it? Clin J Am Soc Nephrol. 2008;3:174–8.
Bennett CL, Luminari S, Nissenson AR, Tallman MS, Klinge SA, McWilliams N, McKoy JM, Kim B, Lyons EA, Trifilio SM, Raisch DW, Evens AM, Kuzel TM, Schumock GT, Belknap SM, Locatelli F, Rossert J, Casadevall N. Pure red-cell aplasia and epoetin therapy. N Eng J Med. 2004;351:1403–8.
Schellekens H, Jiskoot W. Eprex-associated pure red cell aplasia and leachates. Nat Biotechnol. 2006;24:613–4.
Acknowledgments
No sources of funding were used to assist in the preparation of this article. Begoña Calvo and Leyre Zuñiga have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calvo, B., Zuñiga, L. EU’s New Pharmacovigilance Legislation: Considerations for Biosimilars. Drug Saf 37, 9–18 (2014). https://doi.org/10.1007/s40264-013-0121-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0121-z