Abstract
Drug-induced torsade de pointes (TdP) is a potentially fatal iatrogenic entity. Its reporting rate in association with non-cardiac drugs increased exponentially from the early 1990s and was associated with an increasing number of new non-cardiac drugs whose proarrhythmic liability was not appreciated pre-marketing. This epidemic provoked a comprehensive global response from drug regulators, drug developers and academia, which resulted in stabilization of the reporting rate of TdP. This commentary reviews the chronology and nature of, and the reasons for, this response, examines its adequacy, and proposes future strategies for dealing with such iatrogenic epidemics more effectively. It is concluded that the response was piecemeal and lacked direction. No one entity was responsible, with the result that important contributions from regulators, industry and academia lacked coordination. While the process of dealing with QT crisis seemed to have worked reasonably well in this instance, it does not seem wise to expect the next crisis in drug development to be managed as well. Future crises will need better management and the challenge is to implement a system set up to respond globally and efficiently to a perceived drug-related hazard. In this regard, we discuss the roles of new tools the legislation has provided to the regulators and the value of an integrated expert assessment of all pre-approval data that may signal a potential safety issue in the postmarketing period. We also discuss the roles of other bodies such as the WHO Collaborating Centre for International Drug Monitoring, CIOMS and the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Prolongation of QT interval of the surface ECG had long been believed to be a marker of an antiarrhythmic mechanism. Excessive prolongation of the QT interval in the right setting can, however, trigger a potentially fatal ventricular tachyarrhythmia, typically of the torsade de pointes (TdP) type. When sustained, TdP is associated with syncope and other symptoms of impaired cerebral perfusion, and may resolve leaving no trace or degenerate into fatal ventricular fibrillation. Since sudden unexpected deaths leave no pathological signature, the relationship to a drug effect may not be suspected. Since TdP is, more often than not, a transient arrhythmia, its incidence in association with a drug is difficult to quantify.
This review traces the history of the unfolding of a drug safety issue at a global level and on an epidemic scale, resulting from unexpected QT prolongation by non-cardiac drugs, often associated with a fatal proarrhythmia. It also examines the extent to which the response to this crisis serves as a model for future drug-related crises.
2 Unfolding of the Epidemic
Until the introduction of thioridazine in 1958 for the treatment of schizophrenia, the only drug known to induce QT prolongation and syncope was quinidine. In one of the earliest large series of 168 cases of QT prolongation reported in 1951, the only drug to feature in the list of causes was quinidine (in eight patients) [1]. Since 1958 through to the mid-1990s, the number of non-cardiac drugs that were found to prolong QT and induce TdP had progressively but imperceptibly increased.
Until the late 1970s, most of these drugs were psychoactive drugs such as neuroleptics and antidepressants, indicated for disabling conditions. By the late 1970s, QT prolongation and TdP were also reported in association with non-antiarrhythmic cardiovascular drugs such as prenylamine, bepridil and lidoflazine, all indicated for angina. Once this was recognized, their use declined markedly or was approached with caution. Gradually, antiarrhythmic drugs such as sotalol and lorcainide also disclosed their potential to prolong the QT and induce TdP. Beginning in the late 1980s, concerns on the potential of non-cardiovascular drugs to induce TdP, often with fatal outcome, rose sharply when a number of these drugs, indicated for relatively benign and self-limiting conditions, came to be reported with this adverse reaction. These drugs included terfenadine and astemizole, indicated for hay fever, and terodiline, indicated for urinary incontinence.
Regulatory concerns on the potential of drugs to increase the duration of the QT interval gathered momentum during the period 1988–1991, when three drugs were withdrawn from the UK and other European markets because they caused QT prolongation and TdP. The drugs concerned were prenylamine (withdrawn from the market in 1988), lidoflazine (1989) and terodiline (1991). None of these drugs were approved or marketed in the US. These concerns intensified further with the addition of two new drugs belonging to completely new therapeutic classes, halofantrine (an antimalarial drug) and cisapride (a gastric prokinetic drug), both also approved and marketed in the US. The details have been reviewed previously [2].
In the aftermath of the QT-related proarrhythmic potential of terfenadine that began to unfold in 1989, and before the US approval of cisapride in 1993, there took place what was probably the first meeting between academic investigators, physicians from the US FDA and clinical scientists from the pharmaceutical industry who gathered in Philadelphia to review and discuss the implications of a prolonged QT interval for patient safety and drug development [3]. The main theme of the meeting (the ‘1993 meeting’) was whether QT prolongation was beneficial or harmful. From a regulatory perspective, three important points to emerge were that (i) there was a lack of sufficient evidence to suggest that prolongation of the QT interval was necessarily beneficial; (ii) drug-induced QT prolongation must be considered to affect adversely the benefit-risk profile of a drug [4]; and (iii) QT prolongation was not a good indicator of whether or not a class III antiarrhythmic will suppress a target arrhythmia; however, exaggerated QT prolongation was a precursor of TdP [5]. Furthermore, during discussion, surprise was also expressed that quinidine had not already been taken off the market, although it was recognized that it is difficult to take drugs off the market and that the benefit-risk profile of all antiarrhythmic drugs was, in any case, slender. Lipicky [4] and Botstein [6] from the FDA emphasized the importance of proper pharmacologic study design and dose-QT response relationship, with careful attention given to the metabolic profile of such drugs to identify subpopulations at risk of QT prolongation, especially those resulting from drug interactions.
In November 1994, the SWORD study with d-sotalol, the sotalol enantiomer that acts exclusively by prolonging the QT, was also terminated prematurely because of increased mortality associated with its use compared with placebo [7]. This study not only highlighted the role of chirality, but also resolved QT prolongation generally as an adverse effect. The balance between the therapeutic antiarrhythmic versus the potentially fatal proarrhythmic prolongations of the QT was recognized by all accounts as being a very delicate one.
Two summary statistics testify to the contention that drug-induced QT prolongation with TdP was a new iatrogenic epidemic. Fung et al. [8] searched the FDA safety database from 1969 to 1998 for all adverse events mapped to QT prolongation and TdP. Of the 2194 cases identified, 0.6 % occurred during 1969–1978, 6.6 % during 1979–1988 and 92.8 % during 1989–1998. Overall, 61.1 % of these cases were associated with hospitalization. In 9.8 %, the outcome was fatal. Figure 1 illustrates the number of reports of TdP received by the FDA since 1990. It represents our current best estimate of the number of distinct cases of TdP reported in the FDA’s adverse event reporting system (AERS), after algorithmic removal of cases likely to be duplicates. The process sometimes removes some unique cases that may not be duplicates. The steep increase from 1993 is self-evident. During the period 1993–1999 when cisapride was marketed in the US, the FDA received 341 individual patients affected by QT prolongation, TdP and other serious arrhythmias following the use of cisapride [9]. These included 117 reports of QT prolongation and 107 of TdP. The outcome was fatal in 80 (23 %) of these 341 patients. One hundred and twenty-six (37 %) of the 341 patients had taken concomitant drugs known to inhibit cytochrome P450 (CYP) 3A4, the enzyme that metabolizes cisapride. In a list of the top 20 drugs to cause TdP (as a percentage of the total reports), cisapride ranked fourth overall after ibutilide, sotalol and bepridil (all class III drugs), and led all other non-cardiac drugs [10].
It was soon apparent that this potentially lethal adverse reaction was dose-related, or more precisely, concentration-related, and that drugs could be investigated during their preapproval period for this liability. The role of drug interactions that gave rise to high plasma concentrations of the culprit drugs such as cisapride, resulting from inhibition of their metabolic elimination, was also much clearer following drug interaction studies with inhibitors of CYP3A4. A large number of drugs were found to inhibit this enzyme, which also metabolized terfenadine and a number of other QT-prolonging drugs [11]. Certain other risk factors that predisposed to TdP, such as electrolyte imbalance, pre-existing QT prolongation or bradycardia, cardiac disease and female sex, were also identified. In principle, therefore, the risk could at least theoretically be managed by appropriate preapproval testing and labelling restrictions. Yet, despite the earlier withdrawal of prenylamine and lidoflazine immediately prior to 1990, 10 (26.3 %) of the 38 drugs withdrawn globally from the market between 1990 and March 2006 were withdrawn because of their potential to prolong QT interval and/or induce TdP (Table 1) [12]. This toxicity ranked second only to drug-induced hepatotoxicity, which accounted for the withdrawal of 14 (36.8 %) drugs from the market during the same period [12].
Against this background of a gradually unfolding global epidemic, it is worth examining whether the response of the stakeholders to deal with the crisis was adequate, timely and well coordinated, and whether it serves as a good model for future drug-related crises.
3 Stakeholder Responses to the Unfolding Epidemic
In this section, we review how stakeholders responded to the global epidemic as it unfolded. We emphasize that in a brief review such as this, it has not proved feasible to detail all the important contributions made by many individual scientists and organizations, which we acknowledge at the outset. Even at the risk of fragmenting the chronology of responses (Fig. 2), we believe it is helpful to group the responses by categories of stakeholders, beginning with regulatory authorities who are mandated to protect public safety. In doing so, we acknowledge that this categorization is artificial and only for convenience since many contributions are collaborative endeavors of these stakeholders (i.e. between the industry and academia, regulators and academia, or the industry and regulators).
Timeline of responses by regulators, academia and industry to the unfolding epidemic of drug-induced QT prolongation. CPMP Committee for Proprietary Medicinal Products, CRADA Cooperative Research and Development Agreements, DCRI Duke Clinical Research Institute, HC Health Canada, HL7 Health Level Seven International, ICH International Conference on Harmonization, QT-IRT QT Interdisciplinary Review Team, TQT Thorough QT study
A vast majority of the decisions to withdraw a drug are made on the basis of spontaneous reports received by the authorities during the postmarketing period [13, 14]. Given that the reporting rate is in the order of 10–20 %, postmarketing spontaneous reports raise a serious concern. Physicians often report retrospectively once they are sensitized to the association. Both these points are best illustrated by terodiline and recently with ondansetron (where a Thorough QT [TQT] study confirmed the signal raised by the spontaneous reports). It is worth pointing out that depending on the local culture, extent of hazard and experience, prescribing practices (e.g. doses and co-medications) and availability of alternatives, differences in regional approaches are common, not only regarding drug approvals (terodiline, lidoflazine, sertindole) but also drug withdrawals (levacetylmethadol). EU and US authorities frequently differ in these respects [12]. Although there may be a regulatory imperative to remove a hazardous drug from the market, most decisions on drug withdrawals are made jointly by the regulator and the sponsor when it becomes clear that risk minimization strategies through labelling have failed to contain the risk. On rare occasions, regulatory decision to withdraw a drug from the market is challenged, as, for example, with withdrawal of two products containing dextropropoxyphene in Australia [15].
It seems that directly or indirectly, cisapride provided the trigger to a long-perceived need for a globally harmonized guidance to identify the potential of new drugs for their torsadogenic risk well before submitting an application to market the drug. Although cisapride was approved in the EU about 5 years earlier in 1988, it was not as much of a safety issue in Europe as it was in North America. A vast majority of the reports of proarrhythmias came from the US where the approved dose of cisapride was twice that in the Europe (80 mg vs 40 mg maximum daily dose). The reporting rate in the US was about 10-fold higher [16]. With regard to serious ventricular arrhythmias and sudden death, doses greater than 40 mg daily were used more frequently in the US compared with the EU (28.7 % vs 14.2 %) [16].
3.1 Regulatory Authorities
The three authorities that had been the most proactive were the European Medicines Agency, Health Canada and the FDA.
3.1.1 European Medicines Agency and the Committee for Proprietary Medicinal Products (December 1997)
In December 1997, the Committee for Proprietary Medicinal Products (CPMP) became the first regulatory authority to issue points to consider during preapproval investigation of new non-cardiovascular drugs with regard to their potential to prolong the QT interval. This document was entitled ‘The Assessment of the Potential for QT Interval Prolongation by Non-Cardiovascular Medicinal Products’ [17]. It cautioned the sponsors that the potential of non-cardiac medicinal products to prolong the QT and induce TdP had significant implications for their future development. It recommended a set of in vitro electrophysiological studies prior to the first use of new drugs in humans. The clinical strategy provided guidance on ECG documentation and the number of subjects to be studied. This included techniques of recording ECGs, evaluation of these ECGs manually by cardiologists experienced in such evaluations, appropriate correction of measured QT interval for changes in heart rate and correlating ECG changes with plasma concentrations of the parent drug and the most significant metabolites as appropriate. In view of the normal variability in QTc interval during drug-free periods [18], the document suggested a set of categorical responses as a general guide, which should be considered as ‘signal’ values of QT changes from baseline that might represent a drug-induced effect. The strategies described therein generated considerable acrimony from industry and clinical investigators because of the increased ECG testing and analysis requirements imposed in clinical research, but were nevertheless the forerunners of internationally harmonized guidelines, International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) S7B and ICH E14 described later.
The stimulus to the above response from the CPMP was not only the concern about the potential significance of drug-induced QT interval but also to develop a pan-European approach to evaluation of QT-prolonging drugs. During 1995–1996, the UK drug regulatory authority had approved two new drugs (sertindole, an atypical neuroleptic agent, and mizolastine, another non-sedating antihistamine), which were both associated with QT prolongation in a small number of patients in clinical trials [2]. Whereas the QT prolongation with sertindole was quite marked (over 20 ms) [19], the effect of mizolastine was modest [20]. Although neither drug was reported to have induced TdP in clinical trials, there was considerable difference in the benefit-risk evaluation of these drugs among the various Member States of the EU [20]. The events that followed the development of the ‘Points to Consider’ document have been summarized previously [2]. Given the pivotal role of drug interactions with regard to drug-induced QT prolongation, it should not come as a surprise that during the same meeting of December 1997, the CPMP also adopted the first regulatory guidance on investigation of drug interaction potential of a drug, entitled ‘Note for Guidance on the Investigation of Drug Interactions’. [21].
3.1.2 Health Canada (March 2001)
The Canadian regulatory authority, Health Canada (HC), followed up the CPMP initiative, and in March 2001 released their guidance document entitled ‘Assessment of the QT Prolongation Potential of Non-Antiarrhythmic Drugs’ for consultation. This guidance also recommended a strategy of preclinical in vitro studies and clinical studies in order to characterize the risk.
The preclinical strategy proposed was more detailed than, but broadly similar to, that advocated in the CPMP document. It also acknowledged that drug effect on IKr current (being the principal repolarizing current in ventricular myocardial cells) could also be studied using a suitable heterologous system expressing the cloned human IKr channel. In terms of clinical strategy, it provided detailed guidance on design and conduct of studies, measurement of QT interval, more robust approaches to its correction for heart rate, QT-related discontinuation of subjects from studies, and subset analysis. It recognized the limitations of analysis by central tendency using only the time-averaged variable and retained outlier analysis very much in line with the CPMP document.
The regulatory concerns and implications were stated in uncompromising terms. It emphasized that “QT prolongation, with or without documented arrhythmia may be the basis for non-approval of a drug or discontinuation of its clinical development” and that “failure to perform an adequate non-clinical and clinical assessment … may likewise be adequate justification to delay or deny marketing authorization”. The concept of benefit-risk was also clearly detailed. Drugs that prolong the QT at recommended therapeutic doses should not be candidates for clinical development or license approval unless they provide benefits for serious diseases or diseases not amenable to treatment with safer drugs or have demonstrated efficacy in patients refractory or intolerant to the alternative drugs.
Finally, it is recommended that prior to the launch of any QT-prolonging drug, a letter should be issued to healthcare professionals advising them of the cardiotoxic risks associated with the new agent and appropriate risk management strategies.
The stimulus to developing this key guidance with such uncompromising clarity and detail is unclear. Although HC had reported on severe and fatal adverse reactions experienced by patients taking cisapride, through the Canadian Adverse Drug Reaction Newsletter in July 1996, January 1998 and January 2000, the authority was criticized for apparent inaction beyond that [22].
3.1.3 FDA, USA (June 2001–2002)
Although the FDA had not released any official guidance, the scientific staff at the FDA had composed a draft document entitled ‘Development of drugs that alter ventricular repolarization’. The detailed draft document dated 2 September 1999 outlined various methodological approaches to evaluation of the QT liability of a drug, including a range of preclinical studies. The key elements of this were published much later in 2002 [23].
In November 2001, the Cardio-Renal Division of the FDA called for a formal meeting inviting industry, academia, and regulators to discuss what has become known as the FDA Digital ECG Initiative. In that meeting the FDA called for better quality ECG data in drug development rather than obtaining site-generated ECG data. Improved ECG analysis was promoted with the realization that each site uses different ECG analysis methodology, there is a lack of training and consistency between physician interpreters for determining QT duration [24], and lack of attention to assess ECG changes at periods of maximum drug exposure. The FDA requested that all ECGs in clinical trials be obtained, processed, analysed and reported digitally. The FDA also further declared that it would require the submission of the raw ECG data in digital form and that appropriate data standards would be developed for submission to an FDA ECG warehouse (see below).
With regard to the development of guidance on assessing drugs for their potential to cause TdP, the FDA and HC issued a jointly agreed ‘Preliminary Concept Paper’ in November 2002 [25]. The key concepts of the November 2001 digital ECG meeting were detailed and a mandatory study design was proposed, requiring drug developers to perform a dedicated robust ECG study that would definitively determine the ECG effects of new drugs during their development. The plan for an FDA ECG Warehouse to receive raw digital ECG data was also detailed. The ‘Preliminary Concept Paper’ was extensively discussed in a consultation workshop held at the University of Maryland at Shady Grove, MD, USA, in January 2003. Following this workshop, this concept paper was revised and presented for further discussion at the ICH with a view to harmonizing the approach to identifying this risk during drug development across the three ICH regions (EU, US and Japan).
3.1.4 International Conference on Harmonization (2003–2005)
The ICH Steering Committee creates an Expert Working Group (EWG) when a new topic is proposed and accepted for harmonization. The EWG is charged with developing a harmonized guideline that meets the objectives outlined in the Concept Paper and Business Plan. Each of the six official ICH parties nominates official representatives to each EWG and, unless otherwise specified by the Steering Committee, the official membership is limited to two officials per party per working group and one representative per ICH observer, and also, if applicable, one per interested party. Almost all other regions of the world are actively engaged with the ICH through a subcommittee of its Steering Group, known as the Global Cooperation Group [26].
An ICH EWG began working on a guideline (ICH S7B) on a preclinical strategy to identify drugs with QT liability, in May 2001. The discussions were proceeding well, but before this guideline could be finalized, ICH was presented with the joint FDA/HC concept paper in February 2003. This concept paper focused almost exclusively on clinical strategy. Another EWG was created to explore the possibility of a harmonized clinical strategy (which later came to be known as ICH E14). As a result, it was decided to progress both guidelines – preclinical S7B and clinical E14 – concurrently. The two EWGs, one dealing with the non-clinical guideline and the other the clinical guideline, met regularly and maintained a close working link throughout. Ultimately, both guidelines were adopted on 12 May 2005. Each is essentially a self-standing guideline making no reference to the strategy described in the other.
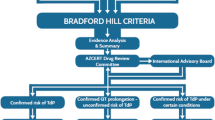
ICH S7B promotes a concept of integrated risk assessment [27] based on the chemical and pharmacological class of the drug together with data from two core tests – in vitro IKr assay and an in vivo study in a suitable species. The integrated risk assessment also takes into account follow-up studies specially investigating the electrophysiology of the drug (action potential duration [APD] assay and various proarrhythmia models) as well as other data from studies investigating toxicology, pharmacodynamics, pharmacokinetics, tissue distribution and accumulation and drug interactions.
The focus of ICH E14 is a specific TQT study, typically conducted in healthy volunteers, as the primary method for evaluating the potential effect of non-cardiac agents on cardiac repolarization during drug development [28]. This guideline is intended to apply to almost all the new drugs with systemic bioavailability but may also be applicable to established drugs under certain conditions exemplified in the guideline.
These two guidelines are unique in the sense that among well over 60 ICH guidelines adopted so far, they are the only ones that address a specific safety issue. ICH E14 is also unique since there was a strong desire to fast-track it and it took just 2 years to completion, in contrast to the usual 3–4 years required to complete most ICH guidelines.
When adopting ICH S7B and E14, the ICH Steering Committee established an E14 Implementation Working Group, constituted from the membership of S7B and E14 EWGs. This Group was charged with developing question and answer (Q&A) documents, providing clarity on aspects of the guideline that might appear ambiguous, and responding to issues on which there were uncertainties or evolution in thinking. In June 2008, the Group issued its first Q&A document [29]. In March 2010, it adopted a set of issues for further discussion or where ICH E14 could be refined in view of advances in science and technology, resulting in clarification of a set of further issues in May 2012 [29].
3.1.5 2006 FDA QT-Interdisciplinary Review Team Set Up as a Formal Body Under Manual of Policy and Procedures 6020.14
A centralized QT Interdisciplinary Review Team (QT-IRT) was formed within the FDA Center for Drug Evaluation and Research to implement the ICH E14 guideline. The QT-IRT team includes clinical, pharmacology, statistical and clinical pharmacology reviewers who collaboratively provide expert advice both to the FDA’s review divisions and to the sponsors on the design, analysis and interpretation of TQT studies. During 2006–2011, the QT-IRT reviewed and provided advice on over 400 TQT study protocols, 250 reports and 400 other submission types (e.g. ECG monitoring proposals, TQT study waivers, meeting packages), as shown in Fig. 3. The team also includes data managers and regulatory project managers who maintain a tracking system and an integrated database of clinical trial data and results.
Another important mission of the team is to develop the science of evaluating drug effects on cardiac repolarization by refining the methods recommended in ICH E14. Contributions have included (i) concentration-QT modelling to evaluate the proarrhythmic potential of new drugs [30]; (ii) testing of the positive control [31]; (iii) validation of TQT study design features based on response to the positive control, moxifloxacin [32, 33]; (iv) a QT knowledge management system to increase efficiency of QT reviews by leveraging knowledge from previous experiences [34]; and (v) developing quality control metrics based on drug-free QT measurements [35].
3.1.6 ECG Warehouse
In the November 2001 digital ECG meeting noted in Sect. 3.1.3, the Cardio-Renal Division of the FDA specifically declared that it would request the submission of the raw ECG data in digital form and that appropriate data standards would be developed.
Although the FDA proposed a data standard for ECG data at that meeting, this was more of a statement of scope for such a standard than a serious effort to represent one, and the FDA had no role in organizing a group that had formed by January 2002 to address this problem. Health Level Seven International (HL7) is the global authority on standards for interoperability of health information technology, with members in over 55 countries [77]. With organizational leadership by Scott Getzin at Eli Lilly and engineering leadership by Barry Brown of Mortara Instruments, the group, which included representatives from ECG machine manufacturers, pharmaceutical companies, academia and clinical research organizations, interacted frequently through teleconferences during much of 2002 and put forward specifications to the HL7 standard in December 2002 with full passage in January 2003. Unusually, there was a publicly available viewer released for the data standard, a product of one of the standard’s team members.
Before the data standard had completed its review cycle with HL7, the FDA was approached by two companies marketing ECG equipment with proposals to develop a unified repository for these data. Both parties submitted their proposals as Cooperative Research and Development Agreements (CRADAs) [see Federal Technology Transfer Act of 1986], and the one from Mortara Instruments was accepted in June 2004. At nearly 18 months, the CRADA process had a longer incubation period than did development of the data standard itself, and, because the CRADA partner did not wait for the agreement to start work, a prototype review tool was available for testing within a few months and reviewable submissions a few months after that.
The above ongoing public-private partnership with Mortara Instruments has resulted in the creation of a digital ECG repository that contains approximately 6.1 million ECGs and has enabled FDA online review of over 250 TQT studies.
The ECG Warehouse stores the 10-second annotated ECGs from all submissions in an online system. The FDA reviewer is provided with a web-based interface to these data that allows for navigation to the submission, subject and timepoint of interest. It allows the reviewer to plot data with or without the sponsor’s measurement annotations, expand parts of the recording, view the leads individually or overlaid, and make their own measurements using on-screen calipers. In addition, the supporting system provides additional data quality assessments, some of which are based upon comparison of the reported results with the Mortara VERITAS™ algorithm for QT quality and signal assessment. The ECG Warehouse facilitates the organization and easy retrieval of ECGs, resulting in efficient review of tracings within the FDA’s submission review process. The ECGs are easily accessible by authorized FDA reviewers on any system within the FDA’s network.
Although frequently the ECG data in TQT are obtained from continuous recordings, the ECG Warehouse currently only stores a series of 12-lead, 10-second recordings taken at protocol-specified timepoints. There are several limitations to storing only 10-second extractions, namely (i) the process for selecting the 10-second recording within the protocol-defined analysis window is not subject to audit; (ii) the pre-specified nominal timepoints may not be adequate for characterization of drug effects; and (iii) there is inherently more information in the recordings than is captured in 10-second snapshots. Furthermore, review of continuous ECG data would be invaluable in other applications. For example, these data can provide information on the initiation of arrhythmias, allowing the assessment of efficacy and risk of new antiarrhythmic drugs or devices. From a research perspective, new analytical methods based on continuous data in the ECG Warehouse will increase the efficiency of TQT studies and allow for the evaluation of new biomarkers for cardiovascular safety.
In 2010, the FDA and Mortara Instruments initiated the expansion and upgrade of tools for submitting continuous ECG data to the ECG Warehouse. The continuous ECG Warehouse will contain new features that will allow for easy viewing of annotated ECG measurements for drug effects within the recording as well as detection of arrhythmias. The upgraded ECG Warehouse provides new opportunities to improve the cardiovascular safety evaluation of new medical products with continuous recordings.
3.2 Academia
Academia had been busy developing various models of proarrhythmias, such as the perfused canine left ventricular ‘wedge’ preparation investigating the effect of the drug on transmural dispersion of repolarization [36], isolated perfused female rabbit hearts investigating the effect of the drug on triangulation, reverse use-dependence, instability and dispersion of the APD (features referred to as TRIaD) [37] and conscious dogs with chronic atrioventricular block with or without diuretic-induced hypokalaemia [38]. The year 1994 witnessed the first description of the human ether-a-go-go (hERG) channel, encoded by the KCNH2 gene [39]. This was a major step since the vast majority of drugs associated with acquired QT prolongation are known to inhibit the hERG subunit, which is the key component of IKr. Since this discovery, hERG expression studies have allowed for preclinical in vitro evaluation of a drug’s potential to induce QT prolongation, at least as a means to screen numerous candidate molecules.
As noted above, one of the first responses of academia in the early 1990s, following the knowledge that non-cardiac drugs could cause an increase in deaths through an unexpected effect of increasing QT duration, came when academic investigators, physicians from the US FDA and clinical scientists from the pharmaceutical industry were invited to gather informally in Philadelphia to review and discuss the implications of a prolonged QT interval for patient safety and drug development [3]. While that meeting produced no clear resolution to the issue, emerging reports of cisapride-induced QT prolongation [40–42] gave rise to an editorial in 1998 which, in the aftermath of the CPMP ‘Points to Consider’ document, expressed concerns that almost every week a new agent was being added to the list of drugs associated with acquired long QT syndrome and TdP, and recommended that the exclusion of potassium channel blocking properties might be considered in the future as a requirement before new molecules were approved for marketing, and more strict warnings in the package insert of drugs with known repolarization prolonging activity could be enforced [43].
In June 1999, the European Society of Cardiology convened a Policy Conference on drug-induced QT prolongation to enable discussion of various issues among experts from basic science, clinical cardiology, drug development and regulatory authorities [44]. The discussions at this conference detailed a clearer delineation of the factors predisposing to abnormal prolongation of repolarization and TdP, and a more precise quantification of the torsadogenic potency of individual drugs, which was aimed to prevent, or at least minimize, the incidence of this potentially lethal adverse effect of certain drugs. The Policy Report from this meeting proposed a flowchart of studies necessary to assess the potential of drugs to prolong ventricular repolarization. Details on the degree of risk, the role of preclinical cardiac safety determinations, the role of pharmacokinetics and drug-drug interactions and the need for more precise QT measurements and clinical trial designs to detect this phenomenon were emphasized [45–47]. A similar expert meeting in August 2000, convened in the US by the Duke Clinical Research Institute/American Heart Journal, also reached similar conclusions [48].
In the early 2000–2003 timeframe, before the acceptance of the ICH E14 concepts, clinical trials in drug development began to emphasize the importance of determining the QT liability of new non-cardiac drugs. One of the first studies in 2002 was conducted by Novartis on darifenacin (an antimuscarinic agent for overactive bladder) with the design and ECG analysis [49]. There were four treatment groups consisting of placebo, a positive control using moxifloxacin to define assay sensitivity and two doses (clinical and supratherapeutic) for the evaluation of this new agent. Later, this design was to become a common standard for conducting the usual TQT study (ICH E14).
Shortly thereafter, another trial aimed at defining the effects of vardenafil (a new agent for erectile dysfunction) employed a novel design that used not only a placebo and positive control group (moxifloxacin) but also compared the new agent with the one widely used (sildenafil) in a robust crossover trial [50]. At about the same time, there was a TQT study for alfuzosin, an α-adrenergic blocker for the symptomatic treatment of benign prostatic hypertrophy. This trial utilized placebo and moxifloxacin controls, conventional 12-lead and continuous (Holter) ECG recordings, subject-specific correction of QT for heart rate, and Holter bin analysis [51]. Both studies were presented at the same Cardio-Renal Advisory Committee hearing of the FDA in May 2003 and established many of the common design standards later embodied in the ICH E14 TQT document.
While these trials were ongoing in 2002, a need was identified to find a more efficient method of obtaining frequent ECGs during the conduct of a TQT, which would require thousands of ECGs, to determine the ECG effects of the new agent. Technological advances in digital 12-lead ECG records onto flash cards had just become available (Mortara Instruments, Milwaukee, WI, USA), but there were no data to suggest that the QT measurements obtained from paper ECGs and measured manually on a digital board to identify the QT liability of drugs such as terfenadine [52] would be comparable to QT measurements obtained by digital recordings on a flash card measured by calipers on a cathode ray tube. To that end, a scientific collaboration between a core ECG laboratory, Pharmacia phase I unit and Mortara Instruments allowed for the conduct of a trial that employed a QT-prolonging agent in healthy volunteers with dual snap electrodes to record ECGs by both recording methods simultaneously and to subject them to different analysis methods. That trial showed that the manual ECG measurements by both recording techniques produced identical results for heart rate and QT duration data across a wide range of QT measurements, thus establishing the use of these newer technologies to make possible the robust determinations required in the TQT study [53].
During 2004–2008, the International Life Sciences Institute (Health and Environmental Sciences Institute [HESI]) sanctioned, developed and oversaw the conduct of a series of prospective studies with 12 drugs which evaluated three of the most highly accepted non-clinical assays of prolonged cardiac repolarization, namely hERG assay, repolarization assay using Purkinje fibres isolated from dogs and the QT/QTc interval studied in conscious telemetered dogs [54]. Its Proarrhythmia Models Projects Committee recognized that there was little practical understanding of the relationship between drug effects on ventricular repolarization and the rare clinical event of TdP. This concern led it to host a workshop ‘Moving Towards Better Predictors of Drug-Induced Torsade de Pointes (TdP)’ in Crystal City, VA, USA, on 2–3 November 2005. The primary objective of the workshop was to develop a better fundamental understanding of the emerging science, trends, and methods and methodologies that relate to predicting drug-induced TdP [55].
With the digital ECG archive looming in the near future, Chris Cabell of Duke University began discussions with the FDA in late 2004 to establish a non-partisan group to use these data for the common good in drug and device development. This proposal was codified in a Memorandum of Agreement between the Duke Clinical Research Institute and the FDA in September 2006, and led to the founding of the Cardiac Safety Research Consortium (CSRC) in 2006–7 [56, 78]. This Consortium now has more than 30 corporate members, has organized think-tank style meetings, sponsored evaluation of automated ECG algorithms, and has produced a series of white papers on diverse topics spanning an ever-broadening scope of cardiac safety issues [57–60].
3.3 Industry
Although there was initially a sense of hostility towards the CPMP ‘Points to Consider’ document, the industry soon responded positively once it acknowledged the problem and the scale of it. The contribution from the industry, on both sides of the Atlantic and Japan, has been very significant, both qualitatively and quantitatively. In a brief summary such as the one that follows, we hope to highlight only the key contributions we consider relevant to this review.
In 1999, the FDA and the Pharmaceutical Research and Manufacturers of America (PhRMA) decided to form a joint task force to define a preclinical threshold to serve as a predictor for the risk of drug-associated QT prolongation [61]. It contributed to the development of preclinical models of proarrhythmias. One major step taken by scientists in the industry globally was to conduct an industry-wide survey of the prevailing and widely diverse practices of investigating the effect of drugs on cardiac repolarization [62]. This was followed in 2002 by sponsorship of an independent task force of academics, which reported in detail on how to evaluate the risk of TdP during drug development, highlighting the techniques and limitations of various preclinical studies [63]. This task force also recommended that early drug trials in humans must include some evaluation of the effect of the new drug on the QT interval, providing a whole range of recommendations to this end and concluding with benefit-risk analysis. Nevertheless, the task force acknowledged that the situation in terms of detecting the clinical risk was unsatisfactory. Redfern et al. [64] also reported the relationships between preclinical cardiac electrophysiology, clinical QT prolongation and TdP for a broad range of drugs and adduced evidence for a provisional safety margin in drug development.
Concurrently with the efforts of HESI, a project named ‘QT Interval Prolongation: Project for Database Construction (QT PRODACT)’ was organized in Japan by pharmaceutical companies belonging to the Japan Pharmaceutical Manufacturers Association and contract laboratories belonging to the Japan Association of Contract Laboratories for Safety Evaluation. This project designed several studies to construct a database of cardiac safety pharmacology. The Japanese investigators tested 22 drugs of clinically positive and negative agents and employed additional non-clinical assays of cardiac ventricular repolarization. All the QT PRODACT studies were published in a special issue of the Journal of Pharmacological Sciences [79], and the experience resulting from this project has been reviewed by Hashimoto [65].
Statisticians from the industry had already highlighted the significance of statistical approaches to study design and analysis of the data [66]. During the development of ICH E14, the industry provided further statistical expertise and solutions with regard to the issues that warranted consideration when designing an ICH E14-compliant TQT study [67].
The Metrics Champion Consortium was founded in 2004 by a clinical research organization’s ECG core laboratory to alleviate the organizational need to provide customized metric reports for its clients [80]. It has since grown into an independent consortium of sponsor and service providers to establish and promote a standard set of industry-wide performance metrics to improve the quality and efficiency of data collection and reporting.
3.4 Governmental Authorities
In order to fulfill its obligation under the Treaty of Amsterdam, the EU has created Framework Programmes for Research and Technological Development, also called Framework Programmes (eight of them so far), abbreviated FP1 through FP8. These funding programmes are created to support and encourage research in the European Research Area.
Under FP7, the EU has funded two research projects directly associated with drug-induced QT interval prolongation. These are ‘Computational Prediction of Drug Cardiac Toxicity’ (preDiCT) and ‘Arrhythmogenic Potential of Drugs’ (ARITMO).
The preDiCT project, with funding of €4.1 million, officially began on 1 June 2008, with a 3-year mission to model, simulate and ultimately predict the impact of pharmacological compounds on the heart’s rhythm using computer models. It is one of several projects as part of the EU’s support for the development of a Virtual Physiological Human. The project, which included collaborators from industry and academia, was coordinated by the Department of Physiology, Anatomy and Genetics and the Computing Laboratory of The University of Oxford, Oxford, UK, under the leadership of Professor Denis Noble. The PreDICT project exceeded expectations. The model frameworks developed for in silico simulation of cardiac toxicity of potential drug compounds are cutting-edge technology. The project has created model frameworks with potential commercial value in both healthcare and pharmacology, and established liaison with the FDA and several major pharmaceutical companies, paving the way for in silico testing and approval of drugs developed in the future. In February 2011, a workshop was convened in Oxford, bringing together the preDiCT team, regulators and industry researchers with a view to discussing the feasibility of in silico modelling approaches and the achievements of the preDiCT project, and gathering the regulators’ advice towards assimilation of simulation into routine regulatory activities.
The ARITMO project, with funding of just under €2.75 million, aims to analyse the arrhythmic potential of >250 drugs in the therapeutic classes of antipsychotics, anti-infectives and H1-antihistamines, both globally and in specific subgroups (age, co-morbidity, genetically). The ARITMO Consortium has 17 partners from seven Member States. The project is coordinated by Professor Miriam Sturkenboom (Erasmus Medical Centre, Rotterdam, the Netherlands) and is scheduled to run from 1 January 2010 to 31 December 2012. The strategy being followed consists of using existing data and generating a wealth of new data through field, database and in silico studies. From the literature and a variety of databases, information on the risk of QTc prolongation, TdP, ventricular fibrillation and sudden death will be obtained and analysed at a pre-clinical, clinical and postmarketing level. An international prospective case-control surveillance network will run in the UK, Germany, Italy and the Netherlands, and will collect data on risk factors as well as blood samples for candidate gene analyses. The collection of these data is harmonized, extended and continued during the study and is expected to provide unique opportunities to assess both the associations with specific drugs as well as the interaction with genetic factors. Finally, all information generated will be integrated in order to provide lists that will allow ranking the arrhythmic potential of these drugs by selected parameters.
4 Assessing the Success of the Response
The response from the late 1990s through to the present to the public health risk posed by the QT liability of non-cardiac drugs was not the result of a coordinated effort with any one agency or group of individuals responsible for it. The regulatory response was dedicated to obtaining better ECG data so that the ECG effects of a new agent could be more accurately determined and quantified before marketing application to enable a fair decision to be made on approvability or labelling restrictions after considering the benefit-risk profile of the drug. The emergence of the ICH E14 guidance for study conduct and for the assessment of raw ECG data was the final result, but differences still exist between different regulatory regions of the world. The drug development industry contributed to the development of these regulatory-led efforts for better quality of clinical data and their interpretation. Technological advances in ECG recording and analysis led manufacturers and core ECG laboratories to evaluate and provide robust and efficient capabilities to allow the sponsors of new drugs to meet the new regulatory requirements. Preclinical scientific advances helped guide the transition from the bench to the clinic, and academia is not only leading the effort for better biomarkers of a torsadogenic agent but also newer methods to potentially analyse ECG data in the future.
Regulatory authorities require a positive benefit-risk before approval for all drugs with any toxicity. Prolongation of the QT interval by a drug is only one aspect of its benefit-risk analysis. Therefore, it should not be assumed that a drug that prolongs QT interval will, or should, not be approved. The critical issue is the regulatory response when the benefit-risk is perceived to have changed adversely during the postmarketing period. Regulatory approaches to evaluation of the drugs that prolong QT have been criticized on the basis of the undeniably inadequate correlation between QT interval and induction of TdP. It is true that not all drugs that induce TdP prolong QT to an equivalent degree, and drugs that do prolong QT interval to an equivalent degree do not always carry equivalent risk of TdP; the fact remains, however, that TdP, the ultimate clinical outcome that matters, is invariably preceded by QT prolongation. This has further galvanized academia and the industry to look for better repolarization-based biomarkers to predict the clinical risk [68, 69]. Therefore, there are of course a number of ways one can judge the success of the QT-related responses that have emerged and chronologically described above. There is also an additional issue concerning the time interval that should elapse after implementing a response to a safety concern before one legitimately evaluates the success of the measure. We discuss these aspects below.
Determining the parameters of success of regulatory decisions for withdrawing problem drugs (between the years 1997 and 2005) is a difficult task. It could include any one or more of the following:
-
expected lives saved due to market withdrawal of the drug;
-
increased reporting of QT-prolonging medicines due to better awareness of this unique problem in clinical practice;
-
pharmacovigilance system better able to catch more related cases and elucidate the mechanisms of action;
-
development of new methods to harmonized ECG evaluation;
-
decrease in the time interval from approval to detection of increased QT length and then to market withdrawal.
Whilst these are highly desirable parameters, they are often impractical or not feasible. Therefore, the most obvious and simplest approach would be to examine how many non-cardiac drugs have been withdrawn from the market in relation to the measure enacted. As can be seen from Table 1, no new non-cardiac drug approved after the implementation of the CPMP ‘Points to Consider’ strategy in 1998 has been withdrawn from the market. The tireless efforts that followed from HC, the FDA and ICH provided the much-needed international dimension to this strategy in successfully containing the QT/TdP disaster. The only drug to be withdrawn (only in the EU) after 1998 was dofetilide, which, by design, was a QT-prolonging drug, approved in 1999 and withdrawn in 2004. However, it was not commercialized in the EU, most probably in view of its interaction potential and the complex algorithm that had to be followed for its dosing regimen [70, 71] and, if used inappropriately, it was known from preapproval clinical trials to induce dose-dependent TdP. Although withdrawn from the European market, dofetilide is still available in US.
A slightly different approach to evaluating the success of the strategies implemented might be to consider the number of spontaneous reports of TdP received by the regulatory authorities. Although one cannot deny the limitations of the systems of spontaneous reporting, the trends identified by the FDA AERS database (Fig. 1) are perhaps less encouraging. Although TdP continues to be reported, the rate of reporting seems to have stabilized after about 2001 – just about the time when cisapride was withdrawn from the market. This residual reporting probably reflects the continued use of other non-cardiac QT-prolonging drugs that remain on the market due to their favorable benefit-risk profile. However, the recent increase may also reflect better awareness of drug-induced TdP. It is also important to be certain that authorities, having issued the guidance, are not shying away from withdrawing any recently approved non-cardiac drug for fear of exposing any deficiency of the response.
Determining whether the response is successful also needs to take account of the labelling of drugs that have been subject to TQT studies. Labelling relating to the risk is now more informative, and TQT results have served to define doses with better benefit-risk ratio. An example is the recent label change for citalopram, restricting the maximum daily dose to 40 mg daily, although this restriction does not help those patients who have tolerated the 60 mg dose well. Another example of the beneficial effect of the response is palonosetron, a selective 5-HT3 receptor antagonist. This drug carried restrictive warnings on the basis of class labelling; however, following a negative TQT study, the restrictive warnings were removed. On the other hand, some drugs appear positive in TQT studies, but present little proarrhythmic risk either because the true effect is small or because there are stabilizing effects on inward ionic currents. Unnecessarily restrictive labelling can result in denial of the drug to potential beneficiaries. For obvious reasons, there is no information on this aspect of the response.
The response, if successful, can only be considered partially successful when one considers that a number of older torsadogens continue to remain available when safer alternatives have been developed. Probably the best examples are citalopram (alternative escitalopram), saquinavir (alternative other protease inhibitors), haloperidol (alternative other neuroleptics), ondansetron (alternatives granisetron and palonosetron), domperidone (alternative other gastric prokinetic agents) and venlafaxine (alternative desvenlafaxine).
Perhaps the most worrying (and unknowable) aspect that emerges from analysing the success of the aforementioned regulatory strategies is how many otherwise valuable drugs may have been terminated from development because of the sponsors’ concerns regarding the drugs’ perceived proarrhythmic risk, regulatory approaches to their evaluation, approvability and prescribing restrictions. In the aftermath of the implementation of the regulatory response, the findings communicated by one major pharmaceutical company were most worrying [72]. The company revealed that resulting directly from the implementation of the strategy in the CPMP ‘Points to Consider’ document, 11 new chemical entities were found, over the 18-month period to November 1999, to have an effect on QT – representing an attrition rate of 10 %. Of these, eight were dropped from further development and three projects had to be slowed down. None of these compounds were intended to have an effect on ion channels. These 11 were non-cardiovascular as well as cardiovascular drugs, covering a range of therapeutic and chemical classes. Bass et al. [55] have also reported similar concerns – owing to fears that a drug will have a QT effect and that this will result in significant drug development challenges and regulatory hurdles, many companies are stopping at earlier stages the development of new chemical entities that have a non-clinical signal suggesting QT liability. Thus, while it is true that no new drug will induce TdP if the regulatory thresholds of QT concern are set at a conservatively very low level, there are legitimate questions concerning the impact of these guidelines on the promotion of public health, an equally important goal of regulatory authorities.
It is likely that sponsors use hERG assays to drop compounds from development, failing to take into consideration the compound’s effects on other ion channels, the electrophysiological consequences of which might be to mitigate proarrhythmic risk. While all typical torsadogens are high-potency hERG blockers, not all hERG blockers are torsadogens [64, 73–75]. For example, both verapamil and ranolazine are hERG blockers and prolong QT, but appear not to be proarrhythmic, because of effects on calcium (verapamil) or late sodium (ranolazine) currents.
An equally pertinent issue concerns the timing of the evaluation of success or otherwise of the response. During the early 1990s, regulators had been very concerned at the long interval that had elapsed between the year of approval of a torsadogenic drug and the year when this risk first became apparent (Table 2). A number of QT-prolonging drugs have been approved since 2006 because their overall benefit-risk profile has been determined to be favourable at the time of approval. Such drugs include sunitinib and posaconazole, whereas others also have a QT-related box warning (nilotinib and vandetanib). At present, all these drugs appear to be used safely by prescribers. Nevertheless, it may be prudent to pause for a while before considering whether the measures implemented during 1997–2005 and the resulting more informative labelling on QT liability of new drugs have been successful.
5 Proposal for the Future
What we have described above has the properties of a sensibly engineered response to a public health problem related to drug development and the clinical use of drugs to promote public health. The response has many laudable features, including centralized collection of data pertinent to the evolution of guidance, parties primarily associated with the acquisition of those data, an organized community of stakeholders to help evaluate accumulating data, processes to evolve the guidance, and parties tasked with its implementation and monitoring. However, the appearance of being well engineered is an illusion wrought by a small number of individuals who, without much discourse among them, saw elements that needed doing and did them.
The chronology of the response to QT crisis seems to lack any sense of direction that the situation demanded. The initial response appears piecemeal until there was a cluster of non-cardiac drugs that shared a liability to prolong the QT interval. Cisapride was the final trigger with the number of reports of QT prolongation and/or related arrhythmias increasing almost monthly. The number of these reports received by the FDA were 12 (by January 1995), 34 (April 1996), 131 (June 1997), 273 (May 1998), 288 (September 1999) and 341 (January 2000) [9]. This is something that must be avoided with the next crisis. Indeed, one must question whether the next crisis is already upon us, with the number of drugs attracting attention with regard to increased mortality.
While the process of dealing with QT crisis seemed to have worked reasonably well in this instance, it does not seem wise to expect the next crisis in drug development to be managed as well. Whose job is it to watch for crises and ensure that the next crisis gets at least as good a response, if not better? It is no one’s, because, as the situation stands today, no specific entity, a group or an individual is mandated with this responsibility. There is no central body analogous to the USA’s Federal Emergency Management Agency or Homeland Security to set the next response in motion and to help put the necessary infrastructure in place. Perhaps this is not altogether surprising since, in reality, the response is often reactionary in nature.
One approach that has served well the pre-approval assessment of a potential toxicity signal is an integrated assessment of all the relevant data in a single report written by an independent expert. This would be similar to an integrated summary of efficacy or safety. In this context, clinicians and ethics professionals who sit on trials’ review boards also have a valuable role in adding to the regulatory, industry and academic expertise. Regulatory authorities are also empowered to require the sponsors of new drugs to conduct post-authorization safety studies and to put in place risk minimization strategies. Greater use of these studies ought to result in safe and effective use of medicinal products with potential toxicity issues identified during pre-approval assessment, and contribute to generating further information that the regulators require to be able to monitor the postmarketing benefit-risk profile of the drug.
The WHO Collaborating Centre for International Drug Monitoring has been at the heart of international medicinal safety since its formation in 1978 in Uppsala, Sweden [81]. The Centre works by collecting, assessing and communicating information from member countries’ national pharmacovigilance programmes in regard to the benefits, harm, effectiveness and risks of drugs. First established in 1968, it currently enjoys a membership of 106 countries and may have a role in monitoring and coordinating responses to future crises. However, one of the problems with this body acting as a coordinating body is that it receives data from regions after a substantial lag period and the vast majority of the reports have come from the EU and US. It follows, therefore, that the originating authorities are better placed to act faster. Nevertheless, the WHO Collaborating Centre is uniquely placed to help implement pharmacovigilance activities and identify regional differences in risk.
Any system set up to respond to a perceived global drug-related hazard requires a body of experts to monitor carefully and globally the progress of the potential hazard, and another group of experts who can recommend the required studies and state-of the-art remedial measures. This group should be constituted of regulators, academics and the industry. Whose job it ought to be to set up such groups is not clear. No national regulatory body is resourced for this task but whatever body is charged with this responsibility, it must have the required authority and infrastructure. Two bodies immediately come to mind – CIOMS [82] and the ICH [83].
CIOMS is an international, non-governmental, not-for-profit organization established jointly by the WHO and UNESCO in 1949. It serves the scientific interests of the international biomedical community in general and has been active in promulgating guidelines for the ethical conduct of research, among other activities. Its EWGs are composed of regulators, academics and the industry, and although it has no legal authority as such, its outputs have generally found their way into drug regulation and implementation of measures to improve drug safety. Among such key initiatives are the reporting requirements for drug reactions and developments of Periodic Safety Update Reports (for post-approval safety) and, recently, Development Safety Update Reports (for safety during clinical trials). Recently, it has published its report on ‘Practical Aspects of Signal Detection in Pharmacovigilance’ [76].
The ICH, formally set up in 1990, also has its roots in coordinating diverse requirements from regulatory authorities of different regions. Its recent activities have focused heavily on monitoring the postmarketing safety of drugs. Resource requirements would seem to be fairly modest at first, since the main requirement of such a group would be the expertise related to the specific matter at hand and this would have to be recruited as needed.
Hence, the challenge is to implement a system set up to respond to a perceived global drug-related hazard requiring a body to monitor the progress of the hazard and a group of experts who can recommend the required state-of-the-art studies and remedial measures.
6 Conclusions
With the recognition that TdP increased exponentially from the early 1990s, associated with an increasing number of new non-cardiac drugs whose cardiac liability was not appreciated pre-marketing, there followed a comprehensive global response from drug regulators, drug developers in industry and academia. Notwithstanding the uncoordinated nature of this response and lack of a unified leadership in dealing with this crisis, there followed a stabilization in the reporting rate of TdP. While the above approach to dealing with this QT crisis seems to have worked reasonably well, it does not seem wise to expect a similar approach to the next crisis in drug safety to be equally effective in containing the risk. Future crises will need better management and the challenge is to implement a system set up to respond globally and efficiently to a perceived drug-related hazard. In this regard, new regulatory legislation and the value of an integrated expert assessment of all pre-approval data to signal a potential safety issue in the postmarketing period could be helpful. There may also be valuable roles for other bodies such as the WHO Collaborating Centre for International Drug Monitoring, CIOMS and the ICH to effect this process.
References
Bellet S, Finkelstein D. Significance of QT prolongation in the electrocardiogram: based on the study of 168 cases. Am J Med Sci. 1951;222:263–78.
Shah RR. Cardiac repolarisation and drug regulation: assessing cardiac safety 10 years after the CPMP guidance. Drug Saf. 2007;30:1093–110.
Morganroth J. QT interval prolongation: is it beneficial or harmful? Am J Cardiol. 1993;72:1–59B.
Lipicky RJ. A viewpoint on drugs that prolong the QT interval. Am J Cardiol. 1993;72:53–54B.
Roden DM. Current status of class III antiarrhythmic drug therapy. Am J Cardiol. 1993;72:44–49B.
Botstein P. Is QT interval prolongation harmful? A regulatory perspective. Am J Cardiol. 1993;72:50–52B.
Waldo AL, Camm AJ. deRuyter H, et al. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction. The SWORD Investigators. Survival with oral d-Sotalol. Lancet. 1996;348:7–12.
Fung MC. Hsiao-hui Wu H, Kwong K, et al. Evaluation of the profile of patients with QT prolongation in spontaneous adverse event reporting over the past three decades – 1969–98. Pharmacoepidemiol Drug Saf. 2000;9(Suppl. 1):S24–5.
Wysowski DK, Corken A, Gallo-Torres H, et al. Postmarketing reports of QT prolongation and ventricular arrhythmia in association with cisapride and Food and Drug Administration regulatory actions. Am J Gastroenterol. 2001;96:1698–703.
Yap YG, Camm AJ. Drug-induced QT prolongation and torsades de pointes. Heart. 2003;89:1363–72.
Bohets H, Lavrijsen K, Hendrickx J, et al. Identification of the cytochrome P450 enzymes involved in the metabolism of cisapride: in vitro studies of potential co-medication interactions. Br J Pharmacol. 2000;129:1655–67.
Shah RR. Can pharmacogenetics help rescue drugs withdrawn from the market? Pharmacogenomics. 2006;7:889–908.
Clarke A, Deeks JJ, Shakir SAW. An assessment of the publicly disseminated evidence of safety used in decisions to withdraw medicinal products from the UK and US markets. Drug Saf. 2006;29:175–81.
Olivier P, Montastruc J-L. The nature of the scientific evidence leading to drug withdrawals for pharmacovigilance reasons in France. Pharmacoepidemiol Drug Saf. 2006;15:808–12.
Therapeutic Goods Administration, Australia. Update on TGA decision to cancel prescription pain-killers. 21 Jun 2012. Available from URL: http://www.tga.gov.au/newsroom/media-2012-dextropropoxyphen-120621.htm. Accessed 20 Jul 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Proprietary Medicinal Products (CPMP). Opinion following an article 31 referral (cisapride). EMEA/CPMP/24844/02. London, 7 Oct 2002. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Cisapride_31/WC500013943.pdf. Accessed 5 Apr 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Proprietary Medicinal Products (CPMP). Points to consider: the assessment of the potential for QT interval prolongation by non-cardiovascular medicinal products. CPMP/986/96. London, 17 Dec 1997. Available from URL: http://www.fda.gov/ohrms/dockets/ac/03/briefing/pubs/cpmp.pdf. Accessed 5 Apr 2012.
Pratt CM, Ruberg S, Morganroth J, et al. Dose-response relation between terfenadine (Seldane) and the QTc interval on the scalar electrocardiogram: distinguishing a drug effect from spontaneous variability. Am Heart J. 1996;131:472–80.
Food and Drug Administration. Briefing document for NDA 20-644 (Serdolect) Psychopharmacologic Drugs Advisory Committee (PDAC) Meeting. 7 Apr 2009. Available from URL: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM161901.pdf. Accessed 20 Jul 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Proprietary Medicinal Products (CPMP). Opinion of the Committee for Proprietary Medicinal Products pursuant to article 10 of Council Directive 75/319/EEC as amended. Mizollen (CPMP/1034/96-EN). London, 18 Dec 1996. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Mizollen_29/WC500011164.pdf. Accessed 5 Apr 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Proprietary Medicinal Products (CPMP). Note for guidance on the investigation of drug interactions. CPMP/EWP/560l95. London, 17 Dec 1997. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002966.pdf. Accessed 5 Apr 2012.
Lessons from cisapride [editorial]. CMAJ 2001; 164: 1269.
Fenichel RR. Development of drugs that alter ventricular repolarization. Am J Ther. 2002;9:127–39.
Specification for annotated electrocardiographic waveform data in electronic format: request for comments. Fed Register 2003; 68: 22719.
Food and Drug Administration. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. Preliminary concept paper for discussion purposes only (Nov 15, 2002). Available from URL: http://www.fda.gov/ohrms/dockets/ac/03/briefing/pubs%5Cprelim.pdf. Accessed 23 Jul 2012.
International Conference on Harmonization. Organization of ICH: Global Cooperation Group. Available from URL: http://www.ich.org/about/organisation-of-ich/coopgroup.html. Accessed 20 Jul 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Medicinal Products for Human Use. ICH note for guidance on the nonclinical evaluation of the potential for delayed ventricular repolarization (QT interval prolongation) by human pharmaceuticals (ICH S7B). CHMP/ICH/423/02. London, Nov 2005. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002841.pdf. Accessed 5 Apr 2012.
European Agency for the Evaluation of Medicinal Products, Committee for Medicinal Products for Human Use. ICH note for guidance on the clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs (ICH E14). CHMP/ICH/2/04). London, Nov 2005. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002879.pdf. Accessed 5 Apr 2012.
European Medicines Agency, Committee for Medicinal Products for Human Use. ICH Topic E14. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs: questions and answers. EMEA/CHMP/ICH/310133/2008. London, Jun 2008. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002878.pdf. Accessed 5 Apr 2012.
Garnett CE, Beasley N, Bhattaram VA, et al. Concentration-QT relationships play a key role in the evaluation of proarrhythmic risk during regulatory review. J Clin Pharmacol. 2008;48:13–8.
Zhang J. Testing for positive control activity in a thorough QTc study. J Biopharm Stat. 2008;18:517–28.
Yan LK, Zhang J, Ng MJ, et al. Statistical characteristics of moxifloxacin-induced QTc effect. J Biopharm Stat. 2010;20:497–507.
Florian JA, Tornøe CW, Brundage R, et al. Population pharmacokinetic and concentration – QTc models for moxifloxacin: pooled analysis of 20 thorough QT studies. J Clin Pharmacol. 2011;51:1152–62.
Tornøe CW, Garnett CE, Wang Y, et al. Creation of a knowledge management system for QT analyses. J Clin Pharmacol. 2011;51:1035–42.
Malik M, Zhang J, Johannesen L, et al. Assessing electrocardiographic data quality and possible replacement of pharmacologic positive control in thorough QTc studies by investigations of drug-free QTc stability. Heart Rhythm. 2011;8:1777–85.
Antzelevitch C, Sun ZQ, Zhang ZQ, et al. Cellular and ionic mechanisms underlying erythromycin-induced long QT intervals and torsade de pointes. J Am Coll Cardiol. 1996;28:1836–48.
Hondeghem LM, Carlsson L, Duker G. Instability and triangulation of the action potential predict serious proarrhythmia, but action potential duration prolongation is antiarrhythmic. Circulation. 2001;103:2004–13.
Weissenburger J, Davy JM, Chézalviel F. Experimental models of torsades de pointes. Fundam Clin Pharmacol. 1993;7:29–38.
Warmke JW, Ganetzky B. A family of potassium channel genes related to eag in drosophila and mammals. Proc Natl Acad Sci USA. 1994;91:3438–42.
Ahmed SR, Wolfe SM. Cisapride and torsades de pointes. Lancet. 1995;345:508.
Hoover CA, Carmichael JK, Nolan PE Jr, et al. Cardiac arrest associated with combination cisapride and itraconazole therapy. J Cardiovasc Pharmacol Ther. 1996;1:255–8.
Rampe D, Roy ML, Dennis A, et al. A mechanism for the proarrhythmic effects of cisapride (Propulsid): high affinity blockade of the human cardiac potassium channel HERG. FEBS Lett. 1997;417:28–32.
Priori SG. Exploring the hidden danger of noncardiac drugs. J Cardiovasc Electrophysiol. 1998;9:1114–6.
Haverkamp W, Breithardt G, Camm AJ, et al. The potential for QT prolongation and proarrhythmia by non-antiarrhythmic drugs: clinical and regulatory implications. Report on a policy conference of the European Society of Cardiology. Eur Heart J. 2000;21:1216–31.
Sponer G. Prolongation of repolarization in pre-clinical investigations and phase I/II clinical trials: what should be done? Eur Heart J Supplements. 2001;3(Suppl. K):K101–4.
Morganroth J. Focus on issues in measuring and interpreting changes in the QTc interval duration. Eur Heart J Supplements. 2001;3(Suppl. K):K105–11.
Carlsson L. Drug-induced torsade de pointes: the perspectives of industry. Eur Heart J Supplements. 2001;3(Suppl. K):K114–20.
Anderson MD, Al-Khatib SM, Roden DM, et al. Cardiac repolarization: current knowledge, critical gaps, and new approaches to drug development and patient management. Am Heart J. 2002;144:769–81.
Serra DB, Affrime MB, Bedigian MP, et al. QT and QTc interval with standard and supratherapeutic doses of darifenacin, a muscarinic M3 selective receptor antagonist for the treatment of overactive bladder. J Clin Pharmacol. 2005;45:1038–47.
Morganroth J, Ilson BE, Shaddinger BC, et al. Evaluation of vardenafil and sildenafil on cardiac repolarization. Am J Cardiol. 2004;93:1378–83.
Extramiana F, Maison-Blanche P, Cabanis MJ, et al. Clinical assessment of drug-induced QT prolongation in association with heart rate changes. Clin Pharmacol Ther. 2005;77:247–58.
Honig PK, Wortham DC, Hull R, et al. Itraconazole affects single-dose terfenadine pharmacokinetics and cardiac repolarization pharmacodynamics. J Clin Pharmacol. 1993;33:1201–6.
Sarapa N, Morganroth J, Couderc JP, et al. Electrocardiographic identification of drug-induced QT prolongation: assessment by different recording and measurement methods. Ann Noninvasive Electrocardiol. 2004;9:48–57.
Hanson LA, Bass AS, Gintant G, et al. ILSI-HESI cardiovascular safety subcommittee initiative: evaluation of three non-clinical models of QT prolongation. J Pharmacol Toxicol Methods. 2006;54:116–29.
Bass AS, Darpo B, Breidenbach A, et al. International Life Sciences Institute (Health and Environmental Sciences Institute, HESI) initiative on moving towards better predictors of drug-induced torsades de pointes. Br J Pharmacol. 2008;154:1491–501.
Food and Drug Administration. Cardiac Safety Research Consortium (CSRC). Available from URL: http://www.fda.gov/AboutFDA/PartnershipsCollaborations/PublicPrivatePartnershipProgram/ucm231121.htm. Accessed 5 Apr 2012.
Rock EP, Finkle J, Fingert HJ, et al. Assessing proarrhythmic potential of drugs when optimal studies are infeasible. Am Heart J. 2009;157:827–36.
Min SS, Turner JR, Nada A, et al. Evaluation of ventricular arrhythmias in early clinical pharmacology trials and potential consequences for later development. Am Heart J. 2010;159:716–29.
Kligfield P, Green CL, Mortara J, et al. The Cardiac Safety Research Consortium electrocardiogram warehouse: thorough QT database specifications and principles of use for algorithm development and testing. Am Heart J. 2010;160:1023–8.
Rodriguez I, Erdman A, Padhi D, et al. Electrocardiographic assessment for therapeutic proteins: scientific discussion. Am Heart J. 2010;160:627–34.
FDA/PhRMA Task Force to assess QT risk by preclinical markers. Pink Sheet 1999; 61: 15.
Hammond TG, Carlsson L, Davis AS, et al. Methods of collecting and evaluating non-clinical cardiac electrophysiology data in the pharmaceutical industry: results of an international survey. Cardiovasc Res. 2001;49:741–50.
Fenichel RR, Malik M, Antzelevitch C, et al. Drug-induced torsades de pointes and implications for drug development. J Cardiovasc Electrophysiol. 2004;15:475–95.
Redfern WS, Carlsson L, Davis AS, et al. Relationships between preclinical cardiac electrophysiology, clinical QT interval prolongation and torsade de pointes for a broad range of drugs: evidence for a provisional safety margin in drug development. Cardiovasc Res. 2003;58:32–45.
Hashimoto K. Torsades de pointes liability inter-model comparisons: the experience of the QT PRODACT initiative. Pharmacol Ther. 2008;119:195–8.
Dmitrienko A, Smith BP. Analysis of the QT interval in clinical trials. Drug Inf J. 2002;36:269–79.
Patterson SD, Agin M, Anziano R, et al. Investigating drug-induced QT and QTc prolongation in the clinic: a review of statistical design and analysis considerations. Report from the Pharmaceutical Research and Manufacturers of America QT Statistics Expert Team. Drug Inf J. 2005;39:243–66.
Antzelevitch C, Oliva A. Amplification of spatial dispersion of repolarization underlies sudden cardiac death associated with catecholaminergic polymorphic VT, long QT, short QT and Brugada syndromes. J Intern Med. 2006;259:48–58.
Jacobson I, Carlsson L, Duker G. Beat-by-beat QT interval variability, but not QT prolongation per se, predicts drug-induced torsades de pointes in the anaesthetised methoxamine-sensitized rabbit. J Pharmacol Toxicol Methods. 2011;63:40–6.
LaPointe NM, Kramer JM, Weinfurt KP, et al. Practitioner acceptance of the dofetilide risk-management program. Pharmacotherapy. 2002;22:1041–6.
LaPointe NM, Chen A, Hammill B, et al. Evaluation of the dofetilide risk-management program. Am Heart J. 2003;146:894–901.
Shah RR. Drug-induced QT interval prolongation: regulatory perspectives and drug development. Ann Med. 2004;36(Suppl. 1):47–52.
De Bruin ML, Pettersson M, Meyboom RH, et al. Anti-HERG activity and the risk of drug-induced arrhythmias and sudden death. Eur Heart J. 2005;26:590–7.
Oshiro C, Thorn CF, Roden DM, et al. KCNH2 pharmacogenomics summary. Pharmacogenet Genomics. 2010;20:775–7.
Gintant G. An evaluation of hERG current assay performance: translating preclinical safety studies to clinical QT prolongation. Pharmacol Ther. 2011;129:109–19.
CIOMS. Practical aspects of signal detection in pharmacovigilance. Report of CIOMS Working Group VIII. 2010. ISBN 92 9036 082 8. Available from URL: http://www.cioms.ch/publications/blurbs/WGVIIIblurbDRAFT.pdf. Accessed 25 Apr 2012.
Health Level Seven International. Available from URL: www.hl7.org. Accessed 3 Jan 2013.
Cardiac Safety Research Consortium. Available from URL: www.cardiac-safety.org. Accessed 3 Jan 2013.
Hayashi S, Kii Y, Tabo M, et al. QT PRODACT: a multi-site study of in vitro action potential assays on 21 compounds in isolated guinea-pig papillary muscles. J Pharmacol Sci. 2005;99(5):423–541.
Metrics Champion Consortium. Available from URL: www.metricschampion.org. Accessed 3 Jan 2013.
The WHO Uppsala Monitoring Centre. Available from URL: www.who-umc.org. Accessed 3 Jan 2013.
CIOMS. Available from URL: www.cioms.ch. Accessed 3 Jan 2013.
International Conference on Harmonization. Available from URL: www.ich.org. Accessed 3 Jan 2013.
Acknowledgments
The authors have not received any financial support for writing this commentary. Norman Stockbridge and Christine Garnett have no other affiliations or interests except at the FDA. Christine Garnett’s current affiliation is Certara, Cary, NC, USA. Joel Morganroth is the Chief Cardiac Consultant of eResearch Technology Inc. (ERT), Philadelphia, PA, USA, which provides cardiac safety services to the drug development community. Rashmi Shah was formerly a Senior Clinical Assessor at the Medicines and Healthcare products Regulatory Agency, London, UK, and the ICH E14 Topic Leader, representing the EU. Both Joel Morganroth and Rashmi Shah now provide expert consultancy services on the development of new drugs to a number of pharmaceutical companies.
Disclaimer
The views and opinions expressed in this review are those of the authors and do not necessarily represent the views or opinions of their affiliate organizations, any of the regulatory authorities or their advisory committees.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stockbridge, N., Morganroth, J., Shah, R.R. et al. Dealing with Global Safety Issues. Drug Saf 36, 167–182 (2013). https://doi.org/10.1007/s40264-013-0016-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0016-z