Abstract
Multiple sclerosis is a chronic inflammatory disease that affects the central nervous system and can cause various types of pain including ongoing extremity pain, Lhermitte’s phenomenon, trigeminal neuralgia, and mixed pain. Neuropathic pain is a major concern for individuals with multiple sclerosis as it is directly linked to myelin damage in the central nervous system and the management of neuropathic pain in multiple sclerosis is challenging as the options available have limited efficacy and can cause unpleasant side effects. The literature search was conducted across two databases, PubMed, and Google Scholar. Eligible studies included clinical trials, observational studies, meta-analyses, systematic reviews, and narrative reviews. The objective of this article is to provide an overview of literature on pharmacological and non-pharmacological strategies employed in the management of neuropathic pain in multiple sclerosis. Pharmacological options include cannabinoids, muscle relaxants (tizanidine, baclofen, dantrolene), anticonvulsants (benzodiazepines, gabapentin, phenytoin, carbamazepine, lamotrigine), antidepressants (duloxetine, venlafaxine, tricyclic antidepressants), opioids (naltrexone), and botulinum toxin variants, which have evidence from various clinical trials. Non-pharmacological approaches for trigeminal neuralgia may include neurosurgical methods. Non-invasive methods, physical therapy, and psychotherapy (cognitive behavioral therapy, acceptance and commitment therapy and mindfulness-based stress reduction) may be recommended for patients with neuropathic pain in multiple sclerosis. The choice of treatment depends on the severity and type of pain as well as other factors, such as patient preferences and comorbidities. There is a pressing need for healthcare professionals and researchers to prioritize the development of better strategies for managing multiple sclerosis-induced neuropathic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anticonvulsants and antidepressants are the first line of treatment for neuropathic pain in multiple sclerosis, while opioids, cannabinoids, muscle relaxants, and nanomedicine may have potential effects. |
Transcutaneous electrical nerve stimulation, noninvasive brain stimulation, psychotherapy, and physical therapy may be recommended for treating neuropathic pain associated with multiple sclerosis as an addition to medications. |
Neurosurgical methods are usually used to treat trigeminal neuralgia in patients with multiple sclerosis. |
1 Introduction
Multiple sclerosis (MS) is a chronic progressive immunological inflammatory disease that affects myelinated axons in the central nervous system (CNS) [1]. Nearly three million people globally have MS [2]. Multiple sclerosis is a major cause of non-traumatic neurological disability in young people in many countries [3]. Because of the complicated pathophysiology and widespread nature of MS, both its clinical presentation and course are extremely diverse. Symptoms of MS include mobility, visual and sensory disturbances, cerebellar symptoms, sphincter control irregularities, fatigue, memory, and cognitive and emotional issues. Pain is one of the most common symptoms among people with MS. Its prevalence could vary up to 90%. Patients with MS may feel pain of numerous causes and locations [4, 5]. The pain experienced by patients with MS can be either acute or chronic in nature. Based on the pathophysiological mechanisms, the pain in MS is categorized as nociceptive (pain associated with optic neuritis, musculoskeletal pain secondary to postural anomalies, low back pain, migraine, tension-type headache, and treatment-induced pain), neuropathic pain (NP) in the form of ongoing extremity pain, Lhermitte’s phenomenon, trigeminal neuralgia, or mixed pain (painful tonic spasms and spasticity pain) [6, 7]. Over last decade, NP has become a major concern for individuals with MS owing to its direct connection to myelin damage in the CNS, which creates significant obstacles to treatment [8]. The overall prevalence of NP in the MS population is reported up to 29% [9]. As for the types of NP, ongoing extremity pain is present in 12–28% [6, 10], Lhermitte’s phenomenon in 9-41% [11], and trigeminal neuralgia in 5–35% of patients with MS [12, 13]. In MS (even in the early stages of the disease), NP is strongly linked to fatigue, depression, and disability [14,15,16], it also interferes with the majority of daily activities, thereby reducing the quality of life [15, 17]. Although depression does not cause pain, it might make it feel more intense [18]. There has been a paucity of well-controlled trials in patients with MS to examine the efficacy of recognized pain-relieving medications [19]. As a result, management recommendations for NP in MS are generally guided by results of NP treatment in other diseases, therefore treatment options include: tricyclic antidepressant amitriptyline, gabapentinoids (pregabalin and gabapentin), serotonin-norepinephrine reuptake inhibitor medications (venlafaxine and duloxetine), cannabinoids, opioids, botulinum toxin, and non-medication-based treatment methods (targeted physical therapy, psychotherapy, acupuncture, radiotherapy, transcutaneous electroneurostimulation [tENS], functional neurosurgery) [4, 20]. The significant occurrence of NP in MP, its early onset, and its detrimental effect on patients require careful attention. There are limited options available to manage MS-related NP, and their application is frequently accompanied by unpleasant side effects. As a result, there is an urgent medical need to find new pharmacological and non-pharmacological targets that have better tolerance, lower toxicity, and increased efficacy.
2 Methodology
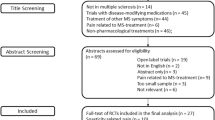
This narrative review aims to explore and discuss the literature on pharmacological and non-pharmacological strategies employed in the management of NP among individuals afflicted with MS. To identify relevant studies, a comprehensive search was performed across two databases, PubMed and Google Scholar. The search date ranged from the earliest available date to August 2023. The search query used included keywords: “Multiple Sclerosis,” “Neuropathic Pain,” “Chronic Central Pain,” “Ongoing Extremity Pain,” “Lhermitte's Phenomenon,” “Trigeminal Neuralgia,” “Medications,” “Pharmacological treatment,” “Non-Invasive,” “Neurosurgical Treatment,” “Psychotherapy,” “Psychological Interventions,” “Physical Therapy,” “Rehabilitation,” and “Physical Exercise.” The eligible studies included clinical trials, observational studies, meta-analyses, systematic reviews, and narrative reviews. The selection of these publication types aimed to ensure a thorough review and appraisal of available evidence. Specific exclusion criteria included studies that were not published in English, animal studies, and research protocols. Furthermore, studies, articles, or sources that did not substantively address NP management in the context of MS, and those that did not fall within the scope or relevance of the review were excluded from consideration. The subsequent sections of this narrative review present a synthesis of the findings derived from the selected studies and offer insights into NP in MS and its management.
3 Review of Literature
3.1 Central NP Syndromes in MS: Pathogenesis and Clinical Features
The majority of patients with MS experience NP and other pain syndromes throughout disease progression. The three main types of central NP in MS are ongoing extremity pain, Lhermitte’s phenomenon, and trigeminal neuralgia [7]. Central NP can be identified in MS at any stage of the disease: at the outset, during an exacerbation, or weeks and months later [21].
Truini et al. suggest the mechanism-based classification of pain syndromes includes nine main types that are pathogenetically associated with MS [7]. Regardless of the type of pain, there is a relationship between pain and the course of the disease, its duration, and patient age [22]. At the same time, there is no convincing evidence that the prevalence or type of pain in patients with MS is related to the type of disease, duration of the disease, or demographics, but rather depends on the part of the nervous system involved. Most pain in MS is attributed to central NP [23, 24], which can be continuous, develop suddenly and without warning (paroxysmal), be triggered by mechanical or thermal stimulation, or most commonly, manifest as a mix of these variables (most commonly) independent of the localization of lesions in the CNS. Similarly, central NP can be deep, superficial, or a combination of both. It generally has moderate-to-severe severity and restricts patients’ functioning skills [25].
Pathophysiological changes and chronicization of NP in MS include increased neuronal excitability in pain conduction pathways. Neuronal hyperexcitability is an important mechanism underlying hypersensitivity to pain in various pathological conditions [26]. The sensory pathway involves primary sensory neurons in the posterior root ganglia that detect harmful stimuli through their peripheral projections, and send pain information to the posterior horns of the spinal cord through central projections. In addition, second-order sensory neurons and excitatory or inhibitory interneurons in the posterior horns receive projections from supraspinal sites that control pain transmission, combine signals in the posterior horns, and send them to different brain regions, where pain perception and emotional responses to pain are formed [27]. The areas of the brain associated with painful symptoms include the cingulate and insular cortex, amygdala, and brainstem [28].
The study comparing neuroimaging signs in patients with MS with and without central pain found no association between central pain and the localization of demyelination in the CNS. The authors suggest that central pain in MS may be associated not with the lesions’ localization, but with changes at the cellular level. At the same time, patients with MS pain mostly had an intact thalamo-cortical pathway, which ensured the perception and awareness of pain by the patient, indicating the importance of its function in the formation of pain syndrome [29]. Another study found a predominance of bilateral periventricular posterior lesions in patients with NPs in MS, which can damage the transmission of nociceptive impulses through the thalamocortical pathway, which manifests clinically with persistent pain. At the same time, a lower probability of NP was demonstrated in patients with right dorsolateral prefrontal area lesions [30]. Central sensitization is manifested by increased sensitivity to harmless (allodynia) or harmful (hyperalgesia) stimuli, or spontaneous pain. This can occur in MS and is independent of damage to the peripheral nervous system [31]. Central sensitization is associated with excessive processing of impulses from nociceptors in the CNS, one such mechanism is glutamate NMDA receptor-mediated sensitization [32]. Baron et al. suggest that it is due to the increased release of glutamate, impaired glutamate uptake, and glutamate receptor overactivation in the neurons of the posterior horns involved in pain processing that increases the efficiency of excitatory synapses [33]. Increased activity, expression, and trafficking of ionotropic glutamate receptors, such as α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid and N-methyl-d-aspartate receptors, have also been observed in second-order sensory organs of hindbrain neurons [34]. Metabotropic glutamate receptors also induce the release of Ca2+ from intracellular stores and activate kinases such as phosphatidylinositol-3-kinase and mitogen-activated protein kinase. Activated kinases, in turn, phosphorylate ion channels and receptors involved in pain mechanisms, changing their activity, leading to increased synaptic efficiency [35]. These processes increase neuronal excitability and reduce the inhibitory activity of GABAergic interneurons and additional extra-neuronal actions. In other words, activated glia and infiltrating immune cells secrete pro-stimulatory cytokines, such as tumor necrosis factor-α and interleukin-1β, which increase excitatory currents and decrease inhibitory currents in the dorsal horn neurons. Reactive astrocytes are associated with hyperalgesia owing to this pathogenesis are shown in Fig. 1 [36].
Proposed mechanisms of central neuropathic pain in multiple sclerosis. APC adenomatous polyposis coli, ATP adenosine triphosphate, BDNF brain-derived neurotrophic factor, CK1α casein kinase 1α, DAMPs damage-associated molecular patterns, GSK-3β glycogen synthase kinase 3β, IL interleukin, NCX Na+–Ca2+-exchanger, NMDA N-Methyl-D-aspartate, mGluR metabotropic glutamate receptors, PAMPs pathogen-associated molecular patterns, PMCA2 plasma membrane Ca2+ ATPase 2, RNS reactive nitrogen species, ROS reactive oxygen species, TCF/LEF T-cell factor/lymphoid enhancer-binding factor, TNF tumor necrosis factor, TRK B tropomyosin receptor kinase B
The central sensitization also involves the system of circadian rhythm regulation through the interaction of glial and neuronal cells in the spinal cord and neuroinflammation [37,38,39]. In addition, descending noradrenergic and serotonergic projections to the dorsal horn inhibit or facilitate pain transmission, respectively. Thus, damage to the descending pain pathways modulates chronic pain [40, 41]. Patients with MS often have lesions in the periaqueductal gray matter, which is an important center that controls the modulation and spread of pain along the descending pathways and has an analgesic effect during stimulation [42]. Meanwhile, GABAergic cells in the ventral medial horn project to the dorsal horn and contribute to mechanical nociception by inhibiting spinal GABAergic interneurons [43]. It is important to mention that supraspinal glia also contribute to NP modulation via descending pathways through the release of soluble mediators. It was found that the expression of sodium channels is increased in demyelinating lesions of MS [44].
3.2 Ongoing Extremity Pain
Because of some ambiguity in the terminology of sensory disorders, it was proposed in 2011 that the condition in MS is characterized by “persistent (and often burning) pain, primarily in the legs and feet” is classified as ongoing extremity pain rather than dysesthetic pain [45]. Ongoing extremity pain affects 12–28% of patients with MS, is more prevalent in progressive MS, can be detected as early as disease onset, and is one of the most severe types of pain [6, 10]. Patients usually describe an unpleasant painful sensation of cold, tingling, itching, numbness, and pulsations, mainly in the lower legs and feet, which may indicate the central mechanisms of pain formation. However, symmetrical bilateral pain with distal localization is known to be more characteristic of peripheral polyneuropathy. There is convincing evidence to exclude peripheral nerve damage in MS as the cause of ongoing extremity pain [46].
The exact mechanisms underlying ongoing extremity pain are not fully understood. This may be explained by the anatomy of the sensory pathways. Specifically, the relevant spinal thalamic fibers are lengthy, increasing their susceptibility to demyelination in superficially located spinal lesions. Thalamocortical fibers for facial sensations diverge laterally, while those for the feet run closer to the lateral ventricle, making them more vulnerable to the pathological process, particularly in the presence of periventricular lesions typical of MS [47, 48]. Additionally, spinal cord lesions can disrupt spinothalamic pain transmission or result from the dysfunction of GABAergic interneurons. This is confirmed by the detection of areas of demyelination in the cervical and thoracic spinal cord using neuroimaging [8].
3.3 Lhermitte’s Phenomenon
Lhermitt’s phenomenon is defined as “an attack-like sensation or NP that can develop as a result of direct or indirect demyelinating lesions of the brain and/or spinal cord and is caused by flexion or movement of the neck.” Patients also describe their sensations as “a transient, short-term sensation associated with bending the neck, which is felt in the back of the neck, lower back, or other parts of the body” [6, 49]. There are a few studies showing the prevalence of Lhermitte’s phenomenon in MS, with the incidence range from 9 to 41% [7, 11]. Currently, the pathophysiology of Lhermitte’s phenomenon is considered to be associated with demyelination of the dorsal columns of the spinal cord in the cervical region. As a result of focal demyelination of ascending sensory pathways, areas of depolarization and hyperexcitability of axon membranes are formed, which in turn become a source of pathological ectopic impulsion and cause paroxysmal neuropathic sensations, and neck movement activates ascending demyelinated spinal thalamic pathways at the cervical level [50]. Magnetic resonance imaging data confirms this hypothesis, namely, lesion formation in the cervical spine was detected in 95% of patients with Lhermitte’s phenomenon compared with52% of patients without this symptom [51]. Current studies on the pathogenesis of Lhermitte’s phenomenon have revealed dysfunction of GABAergic systems, microglial activation, and proinflammatory cytokines, as well as molecular mechanisms of CREB phosphorylation and other transcription factors in the CNS, which increase hyperexcitability and pain. The reduction in tumor necrosis factor-alpha concentration in Lhermitte’s phenomenon has also received attention, as it may enhance impulse activity in unmyelinated Ad and C fibers, which play a role in nociception [8, 23, 52].
It should be noted that Lhermitte’s phenomenon is not specific to MS; it occurs under many other conditions [49]. It is temporary, manifesting for a few weeks, and it disappears spontaneously; therefore, a careful differential diagnosis should be made, especially with pathological processes at the cervical level [10, 51]. The current diagnosis of Lhermitte’s phenomenon is mainly based on the characteristic clinical picture and anamnesis, as there are no routine objective tests for its evaluation or treatment.
3.4 Trigeminal Neuralgia
The current classification of trigeminal neuralgia is divided into idiopathic (no cause can be identified), classic (due to vascular compression of one or more trigeminal roots), and secondary (due to neurological disease (MS lesion) or tumor compression of the angle of the cerebellar bridge). Multiple sclerosis is the most common cause of secondary trigeminal neuralgia, as suggested by the findings of a 20-fold increased risk of trigeminal neuralgia in patients with MS [53, 54]. For a long time, it was assumed that the main cause of trigeminal fiber demyelination in trigeminal neuralgia was vascular compression in the area before the nerve enters the pons, and trigeminal neuralgia in MS is associated with demyelinating plaques in the area immediately after entering the pons [55, 56]. Modern neuroimaging techniques have shown that trigeminal neuralgia can also be caused by lesions along the nerve in MS [57]. There is often concomitant neurovascular compression of the trigeminal nerve in MS in addition to demyelinating plaque at the entrance to the trigeminal root of the pons, causing a “double crush” [58]. Therefore, neurovascular compression of the trigeminal nerve in patients with MS can accelerate demyelination via mechanical and inflammatory mechanisms, leading to symptoms of trigeminal neuralgia [54, 59]. As a result of demyelination and subsequent membrane depolarization, the root axon becomes hyperexcitable, and ectopic impulsion is formed, followed by the development of ephaptic transmission of nerve impulses and central sensitization of neurons in the n. tractus spinalis and in the overlying parts of the central nervous system [60, 61].
Clinically, classical and secondary trigeminal neuralgia are very similar: it is more common in women, predominantly right-sided, involves the second and third branches of the trigeminal nerve [62,63,64], and can be seen as up to 50 unilateral attacks with sudden short pain, similar to an electric shock caused by harmless stimuli [59, 65]. The specific features of trigeminal neuralgia in MS include an earlier onset, possible isolated lesion of one branch of the trigeminal nerve, and bilateral localization of pain in 18% of patients [61]. It should also be noted that there is a sensory trigeminal deficit in MS, but it may not be detected in the background of demyelination lesions [66]. Verification of secondary trigeminal neuralgia in MS is based on neuroimaging methods to detect lesions in the ventrolateral parts of the pons, where the primary afferents of the trigeminal nerve pass, and lesions of the pars oralis of the nucleus spinalis of the trigeminal nerve are also typical [56].
Traditional magnetic resonance imaging revealed signs of demyelination in trigeminal neuralgia in the trigeminal root entry zone, intrapontine tracts, and to the trigeminal nucleus. Microstructural changes in the trigeminal nerve in trigeminal neuralgia in patients with MS have also been reported by diffusion tractography [67].
3.5 Pharmacological Treatments for NP in MS
The treatment of NP involves pharmacological approaches. One single-center cross-sectional study demonstrated that specific long-lasting treatment was prescribed for only 24% of patients with chronic pain in MS and 33% of patients with NP in MS. Anticonvulsants and antidepressants were usually used [68]. Table 1 summarizes medications that can be used for NP in patients with MS.
3.5.1 Antidepressants
None of the conventional pain therapies has proven to provide more than 50% pain relief in randomized clinical trials in patients with MS with chronic NP [8]. In 2015, the Neuropathic Pain Special Interest Group of the International Association for the Study of Pain published guidelines for NP treatment, excluding trigeminal neuralgia, as its protocol differs. A meta-analysis of double-blind studies found that topical or oral pharmacological therapy can effectively treat NP [90]. Recommendations for antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs), as first-line medications for NP have been well stated by Neuropathic Pain Special Interest Group [90], with duloxetine, a serotonin and norepinephrine reuptake inhibitor, and amitriptyline, a TCA, with greatest efficacy [91]. The number needed to treat (NNT) for 50% of pain relief and the confidence interval for NP ranges between 3.6 (3.0–4.4) and 6.4 (5.2–8.4) for serotonin and norepinephrine reuptake inhibitors and TCAs, respectively, making them a good choice for first-line treatment [91]. These drugs prevent the reuptake of serotonin and norepinephrine neurotransmitters, which are postulated to be involved in NP modulation at the nerve synapse [92], thereby modulating pain management. Tricyclic antidepressants also block alpha-adrenergic, serotonergic, histamine, and muscarinic receptors, preventing their action at the synapse [83]. Amitriptyline, a common TCA used to manage neuropathic pain, and its metabolite nortriptyline, after first-pass metabolism, have been shown to be more effective in pain management than placebo at dosages of 90 mg/day and 73 mg/day, in patients with diabetes and non-diabetic patients; however, the data providing clarity in its use in managing NP in patients with MS is not available [85]. However, in a double-blind randomized clinical trial involving 239 adult patients with NP MS, it was shown that taking 30 mg per day for 1 week and then 60 mg per day for 5 weeks of duloxetine is useful and leads to a significant reduction in average pain intensity [83]. Venlafaxine is also being considered for its ability to manage NP in patients with MS, although there are not enough clinical trials to support this proposition [93]. A 2021 review by Stamoula et al. studied the effects of antidepressants on MS using in vitro and in vivo models and revealed that venlafaxine and phenelzine, monoamine oxidase inhibitors, showed anti-nociceptive effects in both models [94]. The side effects of these drugs, specifically TCAs, include orthostatic hypotension, dry mouth, cardiotoxicity, and dizziness owing to their antihistamine effect. In elderly patients with NP, an electrocardiogram is recommended before medication commencement, and dosages of amitriptyline and other tertiary amines of less than 75 mg/day are advised because of sedative and cardiotoxic effects [95]. These side effects are commonly observed with amitriptyline; however, nortriptyline and other secondary amines cause less sedation [91].
Selective serotonin reuptake inhibitors for the treatment of NP in MS are thought to be less effective and hence and hence are prescribed less compared with other antidepressants. This is because only a few clinical studies have detailed their analgesic effects [96, 97]. Although SSRIs can manage pain, paroxetine and citalopram have been shown to moderate pain resolution in painful diabetic neuropathy, whereas other SSRIs have no therapeutic effect [98]. Healthcare professionals must consider potential side effects and drug interactions when prescribing antidepressants to patients with MS. Overall, antidepressants can significantly improve quality of life and provide significant pain relief.
Folle et al., in 2022, conducted a double-blind randomized controlled trial of 445 participants with secondary progressive MS. This study explored the efficacy of fluoxetine, riluzole, and amiloride in NP and found no significant improvement in pain scores or management [99].
3.5.1.1 Anticonvulsants
Anticonvulsants have been used to treat NP patients with MS. These drugs suppress the rapid and excessive firing of neurons during seizures; however, studies have shown that they can manage MS-associated NP [100]. Drugs such as phenytoin, gabapentin, carbamazepine, and its analog, lamotrigine, can suppress neuronal hyperexcitability, thereby alleviating NP [101]. Intravenous phenytoin has been shown to reduce acute exacerbation of NP, at a dosage of 15 mg/kg over 2 h [80]. Carbamazepine presented similar results to phenytoin in relieving pain in patients with MS. A double-blind, randomized, placebo-controlled study of patients with MS and peripheral NP showed that carbamazepine was more effective in pain management than placebo and morphine (p = 0.038); however, the lower morphine dosages used should not be misinterpreted as indicating greater efficacy in pain management [81]. Lamotrigine is also useful in the management of NP in MS; however, it is dose dependent; it is only effective at doses greater than 300 mg/dL [102]. An open-label study conducted by Cianchetti et al. examined the effect of lamotrigine as an add-on therapy to pain medications in 21 patients, 15 of whom had central neuropathic pain. The study reported improvement in pain within a 1-year period with no deleterious side effects [82]. In a randomized placebo-controlled trial, O’Connor et al. investigated the efficacy of pregabalin in patients with MS and neuropathic pain. The trial included 183 patients who received pregabalin or a placebo for 12 weeks. The study found that pregabalin effectively reduced pain scores compared with placebo [6]. Various randomized controlled trials have postulated the use of gabapentin for the treatment of NP in MS [79, 103]. A trial study observed a mean reduction in pain score of 2.05 points on an 11-point numerical rating scale compared with a reduction of 0.94 points with patients receiving a placebo [79]. The NNT for gabapentin in NP ranges from to 4.1 to 6.8 for high to low doses, and the number needed to harm for withdrawal of this medication ranges from 14.1 to 170 [103]. In conclusion, anticonvulsants have shown promising results in reducing NP in patients with MS. Healthcare professionals should consider the individual needs and circumstances of each patient when deciding on appropriate treatment plans. While more research is needed to fully understand the role of anticonvulsants in treating NP in MS, current evidence supports their use as a valuable tool for managing this debilitating symptom.
3.5.1.2 Opioids
Opioids such as naltrexone have also been used as pain relievers in patients with MS. The paradoxical effects of low-dose naltrexone are an example of the contradictory effect of agonism, where the medication prolongs the action potential duration [104]. This mechanism of action is based on the cellular dose response to opioids. Once long-term opioid exposure is achieved, the coupled mu-opioid receptor G protein shifts from Gi to Gs, leading to an activated state. This effect can be shifted by the co-administration of low-dose opioid antagonists with morphine [86]. Two studies intended to evaluate the efficacy of naltrexone on pain relief, measuring outcomes in the MSQoL-54 questionnaire, and the pain effect scale and bodily pain measures in a quality-of-life scale. The type of pain evaluated in these studies was unspecified, and no positive results were shown [87, 105]. A 17-week study evaluated quality of life and observed improvement in the perception of participants regarding personal health; however, no improvements in pain, energy levels, or physical function were observed [105]. Another pilot study was performed, in which 40 patients were treated with low-dose naltrexone for 6 months. There was a statistically significant decrease in pain and spasticity, and the drug was well tolerated [88].
Morphine has also been studied; a trial evaluated responsiveness in a group of patients with MS; intravenous morphine reported reduced pain compared with saline placebo [106]. In two trials that studied opioids, side effects were similar, with sedation being the most common [105, 106]. The role of endogenous opioids in MS has been previously evaluated in the context of disease progression. Although MS-related pain remains relatively unexplored, some evidence indicates that opioid system dysregulation may be one of the causes for the development and maintenance of pain [107].
A retrospective study in Manitoba, Canada, published in 2023, reported that 226 out of every 1000 patients with MS used opioid analgesics in the long-term management of NP. However, this study states that the duration of opioid use is also correlated with mood and anxiety disorders as an adverse effect and their use is therefore not recommended as first-line management [108].
3.5.1.3 Cannabinoids
For millions of years, plants have been used to treat various diseases. The development of therapeutics for the treatment of chronic pain has been accelerated by the legalization of medicinal cannabis in some countries. Cannabinoids, both endogenous and those generated from plants, may act separately or in combination to produce an analgesic effect through cannabinoid and other receptors, including glutamatergic, purinergic, serotoninergic, and glycinergic [109]. In contrast to pure tetrahydrocannabinol (THC), full-spectrum products contain naturally occurring cannabinoids and are reported to show better efficacy or tolerability owing to the synergy of cannabinoids and other components of the cannabis plant [110, 111].
The use of cannabinoids such as THC and cannabidiol (r) has been proposed as a potential treatment for NP in patients with MS [112]. Cannabinoids act via CB1 and CB2 receptors within the endocannabinoid system, which plays a role in pain management. Although its full benefits for NP are still under investigation, data suggest that cannabis with a CBD:THC ratio of 1:1 or higher can reduce pain in patients with MS [113]. The use of cannabinoids and their safety profile as beneficial in NP management have been established by the American Academy of Neurology [114]. Some benefits of using cannabis as an alternative to prescription drugs, such as opioids and antidepressants, includes a reduction of side effects [112]. A crossover trial by Svendsen et al. in 2004, using a total of 23 participants, showed that patients treated with a CBD/THC combination had a reduction in NP with the added benefit of improved sleep quality compared with participants given a placebo [72]. A 2015 study with a sample size of 15 patients with MS and NP found that adding a synthetic oral THC mimic to gabapentin was effective in pain reduction and tolerated [115].
In 2005, Rog et al. found that patients with MS who received oral THC experienced a significant reduction in pain compared with patients who had received a placebo [69]. Inhaled cannabis has also been postulated to effectively manage pain in patients with MS. Although there are not enough clinical trials to confirm its use, a few studies have supported this theory. A crossover trial study conducted in 2008 using cannabis cigarettes as a means of inhalation in patients with MS documented a reduction in NP compared with patients in the placebo group [70]. Another study conducted in 2013 evaluated 39 patients with NP (central and peripheral) who were administered medium-dose (3.53%), low-dose (1.29%), or placebo cannabis via inhalation. The NNT attained 30% pain reduction between the placebo and medium dose, and the high dose was 3.2 and 2.9, respectively. The NNT for the medium versus high dose was 25, showing that patients with MS can use inhaled cannabis to manage NP [71]. While the use of cannabis in treating NP is promising, more clinical trials must be conducted to determine its dosage, efficacy, and tolerance. A 2017 study showed that over 77% of patients who initially used opioids to manage their pain significantly reduced their use of opioids after adding to cannabis for pain management [116]. A systematic review conducted in 2018 by Nielsen et al. evaluated seven other reviews on the effectiveness of cannabis in managing MS-induced NP [117]. Although this study had mixed reviews, two of the reviewed papers stated that there was some evidence that THC and THC:CBD/nabiximol were effective in pain reduction in MS [114, 118].
In contrast, other reviews concluded that the findings were insufficient or had mixed results concerning cannabis management of NP in patients with MS. In 2023, Link et al. assessed the use of cannabis for long-term pain management in 242 participants with MS. Of these, 27% reported using cannabis for pain management. However, these individuals reported higher median pain intensity scores, higher levels of neuropathic pain, and pain interference scores when compared with the participants who were non-users, which could serve as a reason for the use of cannabis in pain management [119]. A systematic review of clinical trials in which cannabinoids were utilized in MS NP management by Sirbu et al. in 2023 reported that cannabinoids could promote remyelination and reduce inflammation, thereby slowing the demyelination process [120]. However, Hansen et al., in a randomized controlled trial in 2022–23, stated that there was a decrease in mean pain intensity scores in all study groups, although there was no significant difference between pain scores between the placebo group and test groups [121]. While the use of cannabis in treating NP is promising, more clinical trials must be conducted to determine its dosage, efficacy, and tolerance.
3.5.1.4 Muscle Relaxants
Pain for patients with MS often arises as an indirect consequence of the disease [22]. When pain is primarily secondary to spasticity, it manifests as muscle spasms, resistance to passive stretching, and tightness. Management of this condition has proven to be partially effective but may result in diverse adverse events [24]. Tizanidine, a central a2-adrenoceptor agonist, has been shown to be effective in managing spasticity, not just MS [122]. Higher plasma concentrations are related to better anti-spasticity effects, and adverse effects include somnolence, fatigue, dry mouth, dizziness, and hypotension [123]. Oral baclofen, a GABA-B receptor activator, may show an improvement in spasticity and showed comparable efficacy to diazepam, but a major decrease in spasticity compared to placebo. Side effects such as drowsiness, weakness, paresthesia, and dry mouth are common and limit the maximum dose that can be tolerated [122]. Diazepam and clonazepam are benzodiazepines that enhance GABA and suppress neuronal activity in the reticular formation, which can contribute to muscle relaxation [20]. Gabapentin enhances GABA activity by binding receptors in the neocortex and hippocampus, the effect of this medication has been proven to decrease the Ashworth score, but have no effect on clonus, reflexes, or response to noxious stimuli [4]. Dantrolene acts on the contractile portion of the skeletal muscle, and studies have proven its non-inferiority compared to diazepam in patients with MS, although with an increased frequency of side effects [122].
3.5.1.5 Nanomedicine
Over the past decades, there has been an increase in the number of scientific studies of nanoparticles' role in the treatment of NP. The use of nanomedicine may be appropriate in pharmacy to improve the pharmacokinetic and pharmacodynamic properties of drugs, in the combined and adjuvant therapy of NP [124, 125]. Nanomedicine in pain management can lead to improved treatment outcomes, reduced doses of painkillers [126]. Nanotechnology can help cure chronic pain by delivering medications to precise sites and targets. Nanoformulation can considerably improve the effectiveness of some analgesics while reducing toxicity. The medicinal use of nanotechnologies for medications such as doxepin, morphine, baclofen, and amitriptyline are good examples [127]. Nano-therapeutic approaches for the treatment of MS may be a path to overcoming known barriers for ideal treatment and decreased disease progression in NP management.
Thus, the use of nanomaterials may provide a better therapeutic strategy.
-
1.
Improving drug solubility and bioavailability
-
2.
Enabling targeted delivery and a control in release
-
3.
More effective routes of administration
-
4.
Decrease in toxicity
Acting as carriers and triggering immunomodulatory effects may be beneficial mechanisms for this proposed therapy [128]. Particularly in MS, nano vectors have been investigated as drug delivery systems and for antigen-specific immunomodulation.
Hunter et al. developed biodegradable poly nanoparticles that carried myelin antigens once injected into mouse models, and were capable of inducing tolerance and long-term disease progression [129]. Further studies could confirm the application of ag-polymer-PLGA in mice in vivo to induce the regulation of dendritic cells, T-helper cells, and T cells. Other administrations, such as solid lipid nanoparticles loaded with methylthioadenosine, have also demonstrated positive results, with longer half-lives and improved bioavailability [130]. Breaking through physiological barriers, such as the blood–brain barrier, may be a route for future scientific research. Bioengineering, biology, medicine, pharmacology, and other fields may apply nanotechnology to the treatment of MS. Many designs for the modulation of inflammation, delivery of drugs, remyelination, and neuroprotection may certainly benefit patients with this disease.
Belousov et al. found that biocompatible magnetic nanoparticles, specifically micromage-B, not only improved neural function but also reduced demyelination foci, suggesting a potential promising effect in pain management for patients with MS [131]. Gold nanoparticles have also been shown to be clinically applicable in the management of MS, can be administered via different routes of administration, and used as a treatment for relapsing MS [132]. Although nanomedicine has possible potential for use in patients with MS and has demonstrated some effect in pain, there are currently no studies of the effectiveness of nanoparticles in the treatment of NP in MS.
3.6 Non-pharmacological Treatment Approaches for NP in MS
Various non-pharmacological approaches may be used to treat NP in MS, including non-invasive, neurosurgical, psychological, and physiotherapeutic interventions, as shown in Fig. 2.
3.6.1 Non-invasive Methods
Neuropathic pain places a significant burden on the healthcare system owing to its high financial cost and impaired quality of life. Despite the wide range of medications available, pharmacological treatments sometimes produce disappointing results due to insufficient response or resistance to certain drugs. At the same time, there are no methods to prevent or control the onset of pain [133].
Transcutaneous electrical nerve stimulation is a non-pharmacological therapy that has been used for more than 50 years to treat various types of pain. One of its main advantages is the absence of side effects associated with pharmacological intervention. Transcutaneous electrical nerve stimulation therapy is used to treat many diseases of the nervous and musculoskeletal system [134, 135]. A systematic review of four studies by Sawant et al. indicated a medium effect of TENS for the treatment of central NP in patients with MS, regardless of frequency [136]. Treatment duration is important when performing TENS. It has been shown that conventional TENS at 100 Hz for 14 days, 8 hours per day, had a significant effect on pain in patients with MS, while 1 hour per day had no analgesic effect. The efficacy of 4 Hz of TENS and 110 Hz of TENS twice a day for 6 weeks in the form of 45-minute treatments for patients with chronic pain and MS has also been reported [137]. A more recent randomized, controlled, single-blinded study demonstrated the equal effectiveness of TENS and interferential currents in reducing NP in patients with MS, but low-frequency TENS was more effective in improving the quality of life [138].
Noninvasive brain stimulation techniques that may have analgesic effects include repetitive transcranial magnetic stimulation and transcranial direct current stimulation. They cause changes in the excitability of the cerebral cortex by applying short high-intensity magnetic fields or low-amplitude direct currents. Most studies have examined the effect of include repetitive transcranial magnetic stimulation on spasticity and other MS-related symptoms, although one study reported a reduction in pain in the high-frequency include repetitive transcranial magnetic stimulation group [139,140,141,142]. Transcranial direct current stimulation could be a potential tool for controlling central chronic pain in MS by improving the sensory, cognitive, and emotional aspects [143]. Transcranial direct current stimulation has been demonstrated to have an analgesic effect on the prefrontal area of patients with MS. The authors concluded that this effect is explained by the influence of the second-order and third-order networks of the pain matrix, which are responsible for pain awareness and perception in accordance with expectations and emotions [144]. Subsequent studies have shown that the effectiveness of transcranial direct current stimulation on central NP in patients with MS may be due to modulation of spinal nociception and may persist for up to 14 days [145] and up to 1 month in cases of transcutaneous spinal direct current stimulation [146].
Two case reports have reported the successful treatment of NP in MS using of spinal cord stimulation; therefore, its effectiveness remains unknown [147, 148]. One other randomized, sham-controlled, cross-over study which included 16 patients with MS examined transcranial random noise stimulation in patients with MS and demonstrated a decrease in pain-associated evoked potentials and pain scores [149]. The evidence of the potential effectiveness of non-invasive brain and spinal stimulation methods is promising, but their effectiveness is limited by the small number of studies, small patient samples, and heterogeneity of the techniques used.
3.6.2 Neurosurgical Methods
Neurosurgical methods are widely used to treat trigeminal neuralgia in patients with MS. Ablation and radiosurgery methods are available.
Rhizolysis, or glycerol rhizotomy (glycerol injections), is a type of transcutaneous treatment for pain, particularly in MS, that damages nerve fibers to block pain impulses. Transcutaneous glycerol resorption (rhizotomy) reduces pain in patients with MS. However, in some patients, pain syndrome may recur. This technique has been used to treat MS-related trigeminal neuralgia [150, 151].
Radiofrequency ablation (rhizotomy) is another potential treatment for trigeminal neuralgia in patients with MS. This manipulation consists of controlled thermal destruction of peripheral nerve structures, which further prevents the transmission of sensory impulses and development of pain paroxysms, which are common complications in MS. Complications of radiofrequency ablation are minimal, and its effectiveness is quite high, even after the first procedure. The most common reason for using this technique is the resistant chronic pain syndrome in trigeminal neuralgia in patients with MS [152, 153].
Balloon compression is another minimally invasive percutaneous neurosurgical procedure used to treat pain in MS, particularly trigeminal neuralgia. Balloon compression is performed under general anesthesia and involves the insertion of a balloon into the affected nerve through a special catheter, followed by inflation of the balloon, which leads to controlled compression and damage to the nerve to prevent pain signals from the affected nerve from reaching the brain. Unfortunately, in most cases, the effect of the procedure is temporary, and pain can resume within 1–2 years [154, 155].
Radiofrequency thermocoagulation is a safe, effective, and minimally invasive procedure for the treatment of trigeminal neuralgia, the basic principle of which is to block the conduction of pain signals with high temperatures to destroy the nerve or modulate the nociceptive nerve function of the trigeminal nerve [156]. The efficacy of radiofrequency thermocoagulation in patients with MS with persistent idiopathic facial pain has been reported. 61.5% of patients experienced temporary pain relief, which lasted an average of 60 days without severe complications [157]. Another study included 63 patients with trigeminal neuralgia in MS and 759 with idiopathic trigeminal neuralgia shown that 72% of patients with trigeminal neuralgia in MS were pain free without medication after 36 treatments of radiofrequency thermocoagulation. There was no significant difference in pain relief between glycerol rhizotomy and radiofrequency thermocoagulation for patients with trigeminal neuralgia in MS [158]. Ablative percutaneous approaches, such as balloon compression, glycerol rhizolysis, and radiofrequency ablation, often provide rapid pain relief, but a recent meta-analysis found no statistically significant differences in the effectiveness or complication rates between these techniques; however, balloon compression is more often associated with mastication weakness [159].
Gamma knife is a radiosurgical technique that can be used in patients with MS-related NP [151]. Gamma knife demonstrated its effectiveness in the treatment of trigeminal neuralgia in patients with MS, but the duration of the effect was shorter than that in patients with idiopathic neuralgia. Therefore, the probability of pain relapse after gamma knife radiosurgery should be considered [160, 161]. The duration of pain control with different neurosurgical techniques remains valid. Several recent studies have indicated a greater efficacy of stereotactic radiosurgery compared with percutaneous techniques, while another study demonstrated a shorter time to recurrence with a gamma knife [162]. One single-center retrospective study of 29 patients with trigeminal neuralgia in MS shown that rates of pain reduction at 1, 3, and 5 years were 70%, 57%, and 57%, respectively [162].
Deep brain stimulation is a method for treating diseases of the nervous system by stimulating certain parts of the brain with special impulses transmitted from a generator to electrodes located in deep brain structures. This method is used for a number of neurological and mental disorders, including Parkinson’s disease, MS, essential tremor, dystonia, epilepsy, Tourette’s syndrome, obsessive-compulsive disorder, endogenous depressive disorders, and chronic NP syndrome [163]. Although some studies have reported the analgesic properties of deep brain stimulation in neuropathic pain, there is currently no evidence in patients with MS [151, 164].
3.6.3 Psychotherapy and Psychological Interventions
It is commonly acknowledged that psychological approaches to treating chronic pain are crucial parts of a comprehensive, evidence-based, patient-centered, multimodal, and interdisciplinary treatment strategy. Psychological treatments for chronic pain that embrace the biopsychosocial model of pain and its management are now essential and effective parts of interdisciplinary pain care. The relationship between pain and other mental disorders, such as stress, anxiety, depression, and sleep disturbances, explains the need for psychological therapies [38, 165, 166]. It is well recognized that anxiety or depression can increase sleep problems and pain and that pain can accelerate mental disturbances and contribute to poor sleep quality [167,168,169,170]. In addition, anxiety, depression, and pain perception may depend on the patient’s personality traits, which also makes psychological interventions for chronic pain appropriate [171,172,173]. Multiple sclerosis is distinguished by mental health issues, sleep disturbances, and chronic pain, in addition to motor dysfunctions such as paresis, spasticity, and gait disorders. At the same time, depression, anxiety, fatigue, and poor sleep may also have an impact on NP in MS [174, 175]. Psychotherapy for NP can target not only the pain syndrome itself but also the factors that impact it, such as sleep difficulties and mental illness (Fig. 3). Thus, psychological therapies are theoretically reasonable for individuals with MS and NP.
Despite overwhelming data supporting the efficacy and usefulness of psychological treatments for chronic non-cancer pain, their use in practical situations is still limited. Patients may actively or passively decline psychological treatment for chronic NP because they are unaware of their potential advantages [176].
Cognitive behavioral therapy (CBT) is the main psychological therapy for chronic pain. A third wave of cognitive-behavioral therapy has arisen as a result of advances in knowledge, and it encompasses several methodologies, including acceptance and commitment therapy (ACT), mindfulness-based cognitive therapy, and metacognitive therapy. Cognitive behavioral therapy is an effective intervention that targets maladaptive cognitive abilities, leading to a reduction in emotional stress and unhealthy behaviors. It is a widely used approach in treating NP associated with a range of disorders, including spinal cord injuries and diabetic peripheral neuropathy, among others [177, 178].
However, CBT is still not widely used as a treatment for MS despite being proven to help treat chronic pain in general. A study was conducted to determine the effectiveness of CBT for chronic pain in patients with MS. This study found that patients who underwent 12 sessions of CBT reported clinically significant progress in achieving their personal goals. However, no significant differences were found between the outcomes of CBT and MS-related education. Therefore, both methods have potential for further use [179].
A recent systematic review confirmed that ACT is efficacious and equivalent, if not better, than other existing active therapies for chronic pain [180]. Positive results were obtained for the treatment of pain in MS using a hybrid intervention of ACT and CBT in a small pilot study included seven patients with MS [181]. It has been discovered that mindfulness-based stress reduction and ACT have a positive impact on the paresthesia experienced by patients with MS. Acceptance and commitment therapy and mindfulness-based stress reduction reduce pain perception over time, which may be explained by considering paresthesia as an indicator of cognitive-emotional pain processing [182].
A recent meta-analysis showed a significant improvement in pain intensity in patients with MS after mind-body therapy, mindfulness, hypnosis, and cognitive-behavioral therapy. However, the reduction in pain in patients with MS is not significantly affected by relaxation therapy [183].
Currently, CBT and ACT psychotherapy are the most effective psychological interventions for chronic pain in patients with MS. However, their effectiveness is limited because of the small number of clinical trials. Further studies are needed to determine factors that may affect patient outcomes.
3.6.4 Physical Exercise
Physical therapy is a component of the comprehensive management of MS that focuses on function and includes nonpharmacological treatments. Physical therapy and rehabilitation for patients with MS are carried out to improve and maintain their general physical condition, eliminate problems with coordination, and adapt to society [184].
Rehabilitation efforts are carried out in a comprehensive manner, involving not only the patient and medical staff but also family members or caregivers. The rehabilitation program for patients with MS is tailored to individual needs and includes physical therapy, including exercise and occupational therapy, aqua therapy, physiotherapy, mechanotherapy, reflexology, massage, speech and swallowing therapy, cognitive rehabilitation, psychological support, vocational rehabilitation, and pre-therapy [185]. For patients with MS, exercise should be considered a reliable and effective form of rehabilitation [186].
Yoga and aerobic exercise can reduce pain in patients with MS [187]. A recent meta-analysis of ten randomized clinical trials demonstrated a moderate effect on pain reduction in patients with MS. Evidence has shown that exercise helps relieve pain regardless of its type, intensity, or duration [188]. The findings of one study clearly showed that precision reflexology results in a statistically significant and clinically significant reduction in pain. Moreover, the observed pain reduction persisted for an additional 10 weeks after the intervention period [189]. Despite some reports on the possibility of relieving pain in MS through physical therapy, no study has specifically targeted neuropathic pain.
At the same time, the study of multidisciplinary interventions that combine exercise and psychological interventions is an urgent issue [176]. Psychologically informed physical therapy, which combines CBT with traditional physiotherapy, is gaining popularity. Recent findings imply that physical therapy based on CBT or ACT approaches may hold prospects [190, 191]; however, these strategies have not yet been explored in the MS population.
4 Conclusions and Future Perspectives
This review provides an overview of NP management in MS. There is a pressing need for healthcare professionals and researchers to prioritize the development of better strategies for managing MS-induced NP and improving the quality of life of those affected by this condition. There are a limited number of controlled trials in patients with MS that examine the efficacy of pain-relieving medications, and management recommendations for NP in MS are generally guided by extrapolation of the results of NP treatment for other diseases. This dearth of dedicated research poses a substantial challenge for healthcare professionals seeking evidence-based approaches to alleviate the suffering of patients with MS. Based on the data in our review, we suggest an algorithm in Fig. 4 for the selection of pharmacological management of NP in patients with MS.
The future of MS-induced NP management should prioritize several key aspects. First, it is crucial to conduct trials that directly address the efficacy of pain-relieving medications in the MS population. Second, personalized treatment plans should be developed utilizing biomarkers and individual patient data to tailor interventions. Additionally, non-pharmacological approaches should be explored further to determine their effectiveness in managing MS-induced neuropathic pain. Patient education is integral to helping individuals make informed decisions regarding pain management. Interdisciplinary collaboration among healthcare professionals is essential, and longitudinal studies tracking pain progression in MS can provide valuable insights into this condition. Overall, a comprehensive approach to address NP in MS, aiming for more effective and patient-centric strategies is required.
References
Leray E, Moreau T, Fromont A, Edan G. Epidemiology of multiple sclerosis. Rev Neurol (Paris). 2016;172:3–13. https://doi.org/10.1016/j.neurol.2015.10.006.
Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, et al. Rising prevalence of multiple sclerosis worldwide: insights from the atlas of MS, third edition. Mult Scler J. 2020;26:1816–21. https://doi.org/10.1177/1352458520970841.
Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV, et al. Atlas of multiple sclerosis 2013: a growing global problem with widespread inequity. Neurology. 2014;83:1022–4. https://doi.org/10.1212/WNL.0000000000000768.
Chisari CG, Sgarlata E, Arena S, D’Amico E, Toscano S, Patti F. An update on the pharmacological management of pain in patients with multiple sclerosis. Expert Opin Pharmacother. 2020;21:2249–63. https://doi.org/10.1080/14656566.2020.1757649.
Svendsen KB, Jensen TS, Overvad K, Hansen HJ, Koch-Henriksen N, Bach FW. Pain in patients with multiple sclerosis. Arch Neurol. 2003;60:1089. https://doi.org/10.1001/archneur.60.8.1089.
O’Connor AB, Schwid SR, Herrmann DN, Markman JD, Dworkin RH. Pain associated with multiple sclerosis: systematic review and proposed classification. Pain. 2008;137:96–111. https://doi.org/10.1016/j.pain.2007.08.024.
Truini A, Barbanti P, Pozzilli C, Cruccu G. A mechanism-based classification of pain in multiple sclerosis. J Neurol. 2013;260:351–67. https://doi.org/10.1007/s00415-012-6579-2.
Khan N, Smith MT. Multiple sclerosis-induced neuropathic pain: pharmacological management and pathophysiological insights from rodent EAE models. Inflammopharmacology. 2014;22:1–22. https://doi.org/10.1007/s10787-013-0195-3.
Foley PL, Vesterinen HM, Laird BJ, Sena ES, Colvin LA, Chandran S, et al. Prevalence and natural history of pain in adults with multiple sclerosis: systematic review and meta-analysis. Pain. 2013;154:632–42. https://doi.org/10.1016/j.pain.2012.12.002.
Nurmikko TJ, Gupta S, Maclver K. Multiple sclerosis-related central pain disorders. Curr Pain Headache Rep. 2010;14:189–95. https://doi.org/10.1007/s11916-010-0108-8.
Feketová S, Waczulíková I, Valkovič P, Mareš J. Central pain in patients with multiple sclerosis. J Mult Scler. 2017. https://doi.org/10.4172/2376-0389.1000208.
Solaro C, Cella M, Signori A, Martinelli V, Radaelli M, Centonze D, et al. Identifying neuropathic pain in patients with multiple sclerosis: a cross-sectional multicenter study using highly specific criteria. J Neurol. 2018;265:828–35. https://doi.org/10.1007/s00415-018-8758-2.
Drulovic J, Basic-Kes V, Grgic S, Vojinovic S, Dincic E, Toncev G, et al. The prevalence of pain in adults with multiple sclerosis: a multicenter cross-sectional survey. Pain Med. 2015;16:1597–602. https://doi.org/10.1111/pme.12731.
Heitmann H, Haller B, Tiemann L, Mühlau M, Berthele A, Tölle TR, et al. Longitudinal prevalence and determinants of pain in multiple sclerosis: results from the German National Multiple Sclerosis Cohort study. Pain. 2020;161:787–96. https://doi.org/10.1097/j.pain.0000000000001767.
Kahraman T, Özdoğar AT, Ertekin Ö, Özakbaş S. Frequency, type, distribution of pain and related factors in persons with multiple sclerosis. Mult Scler Relat Disord. 2019;28:221–5. https://doi.org/10.1016/j.msard.2019.01.002.
Karakas H, Kaya E, Abasiyanik Z, Ozdogar AT. Investigation of neuropathic pain distribution and related factors in people with multiple sclerosis. J Mult Scler Res. 2022;2:46–51. https://doi.org/10.4274/jmsr.galenos.2022.2022-7-2.
Kasap Z, Uğurlu H. Pain in patients with multiple sclerosis. Turk J Phys Med Rehabil. 2023;1:31–9. https://doi.org/10.5606/tftrd.2022.10524.
Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127:35–41. https://doi.org/10.1016/j.pain.2006.07.015.
Murphy KL, Bethea Jr, Fischer R. Neuropathic pain in multiple sclerosis: current therapeutic intervention and future treatment perspectives. In: Zagon IS, McLaughlin PJ, editors. Multiple sclerosis: perspectives in treatment and pathogenesis. Brisbane: Codon Publications; 2017, p. 53–69. https://doi.org/10.15586/codon.multiplesclerosis.2017.ch4.
Aboud T, Schuster NM. Pain management in multiple sclerosis: a review of available treatment options. Curr Treat Opt Neurol. 2019;21:62. https://doi.org/10.1007/s11940-019-0601-2.
Watson JC, Sandroni P. Central neuropathic pain syndromes. Mayo Clin Proc. 2016;91:372–85. https://doi.org/10.1016/j.mayocp.2016.01.017.
Solaro C, Brichetto G, Amato MP, Cocco E, Colombo B, D’Aleo G, et al. The prevalence of pain in multiple sclerosis: a multicenter cross-sectional study. Neurology. 2004;63:919–21. https://doi.org/10.1212/01.WNL.0000137047.85868.D6.
Racke MK, Frohman EM, Frohman T. Pain in multiple sclerosis: understanding pathophysiology, diagnosis, and management through clinical vignettes. Front Neurol. 2022;12: 799698. https://doi.org/10.3389/fneur.2021.799698.
Urits I, Adamian L, Fiocchi J, Hoyt D, Ernst C, Kaye AD, et al. Advances in the understanding and management of chronic pain in multiple sclerosis: a comprehensive review. Curr Pain Headache Rep. 2019;23:59. https://doi.org/10.1007/s11916-019-0800-2.
Klit H, Finnerup NB, Andersen G, Jensen TS. Central poststroke pain: a population-based study. Pain. 2011;152:818–24. https://doi.org/10.1016/j.pain.2010.12.030.
Mirabelli E, Elkabes S. Neuropathic pain in multiple sclerosis and its animal models: focus on mechanisms, knowledge gaps and future directions. Front Neurol. 2021;12: 793745. https://doi.org/10.3389/fneur.2021.793745.
Browne TJ, Hughes DI, Dayas CV, Callister RJ, Graham BA. Projection neuron axon collaterals in the dorsal horn: placing a new player in spinal cord pain processing. Front Physiol. 2020;11: 560082. https://doi.org/10.3389/fphys.2020.560802.
Dworsky-Fried Z, Faig CA, Vogel HA, Kerr BJ, Taylor AMW. Central amygdala inflammation drives pain hypersensitivity and attenuates morphine analgesia in experimental autoimmune encephalomyelitis. Pain. 2022;163:e49-61. https://doi.org/10.1097/j.pain.0000000000002307.
Svendsenl KB, Sørensenl L, Jensenl TS, Hansenl HJ, Bachl FW. MRI of the central nervous system in MS patients with and without pain. Eur J Pain. 2011;15:395–401. https://doi.org/10.1016/j.ejpain.2010.09.006.
Plantone D, Vollono C, Pardini M, Primiano G, Myftari V, Vitetta F, et al. A voxel-based lesion symptom mapping analysis of chronic pain in multiple sclerosis. Neurol Sci. 2021;42:1941–7. https://doi.org/10.1007/s10072-020-04745-3.
Doolen S, Iannitti T, Donahue RR, Shaw BC, Grachen CM, Taylor BK. Fingolimod reduces neuropathic pain behaviors in a mouse model of multiple sclerosis by a sphingosine-1 phosphate receptor 1-dependent inhibition of central sensitization in the dorsal horn. Pain. 2018;159:224–38. https://doi.org/10.1097/j.pain.0000000000001106.
Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926. https://doi.org/10.1016/j.jpain.2009.06.012.
Baron R, Hans G, Dickenson AH. Peripheral input and its importance for central sensitization. Ann Neurol. 2013;74:630–6. https://doi.org/10.1002/ana.24017.
Tao Y-X. AMPA receptor trafficking in inflammation-induced dorsal horn central sensitization. Neurosci Bull. 2012;28:111–20. https://doi.org/10.1007/s12264-012-1204-z.
Mao L-M, Liu X-Y, Zhang G-C, Chu X-P, Fibuch EE, Wang LS, et al. Phosphorylation of group I metabotropic glutamate receptors (mGluR1/5) in vitro and in vivo. Neuropharmacology. 2008;55:403–8. https://doi.org/10.1016/j.neuropharm.2008.05.034.
Tang J, Bair M, Descalzi G. Reactive astrocytes: critical players in the development of chronic pain. Front Psychiatry. 2021;12: 682056. https://doi.org/10.3389/fpsyt.2021.682056.
Warfield AE, Prather JF, Todd WD. Systems and circuits linking chronic pain and circadian rhythms. Front Neurosci. 2021;15: 705173. https://doi.org/10.3389/fnins.2021.705173.
Aborode AT, Pustake M, Awuah WA, Alwerdani M, Shah P, Yarlagadda R, et al. Targeting oxidative stress mechanisms to treat Alzheimer’s and Parkinson’s disease: a critical review. Oxid Med Cell Longev. 2022;2022:1–9. https://doi.org/10.1155/2022/7934442.
Boiko DI, Shkodina AD, Hasan MM, Bardhan M, Kazmi SK, Chopra H, et al. Melatonergic receptors (Mt1/Mt2) as a potential additional target of novel drugs for depression. Neurochem Res. 2022;47:2909–24. https://doi.org/10.1007/s11064-022-03646-5.
Zhuo M. Descending facilitation. Mol Pain. 2017;13:174480691769921. https://doi.org/10.1177/1744806917699212.
Ossipov MH, Morimura K, Porreca F. Descending pain modulation and chronification of pain. Curr Opin Support Palliat Care. 2014;8:143–51. https://doi.org/10.1097/SPC.0000000000000055.
Papadopoulou A, Naegelin Y, Weier K, Amann M, Hirsch J, von Felten S, et al. MRI characteristics of periaqueductal lesions in multiple sclerosis. Mult Scler Relat Disord. 2014;3:542–51. https://doi.org/10.1016/j.msard.2014.01.001.
François A, Low SA, Sypek EI, Christensen AJ, Sotoudeh C, Beier KT, et al. A brainstem-spinal cord inhibitory circuit for mechanical pain modulation by GABA and enkephalins. Neuron. 2017;93:822-39.e6. https://doi.org/10.1016/j.neuron.2017.01.008.
Max MB, Hagen NA. Do changes in brain sodium channels cause central pain? Neurology. 2000;54:544–5. https://doi.org/10.1212/wnl.54.3.544.
Truini A, Galeotti F, Cruccu G. Treating pain in multiple sclerosis. Expert Opin Pharmacother. 2011;12:2355–68. https://doi.org/10.1517/14656566.2011.607162.
Nefedov OO, Kalbus OI. Mechanisms of occurrence and chronicity of neuropathic pain in multiple sclerosis in clinical and experimental conditions. Ukr Med J. 2022;147–148:7–11. https://doi.org/10.32471/umj.1680-3051.147.226789.
Morales Y, Parisi JE, Lucchinetti CF. The pathology of multiple sclerosis: evidence for heterogeneity. Adv Neurol. 2006;98:27–45.
Quiton RL, Masri R, Thompson SM, Keller A. Abnormal activity of primary somatosensory cortex in central pain syndrome. J Neurophysiol. 2010;104:1717–25. https://doi.org/10.1152/jn.00161.2010.
Khare S, Seth D. Lhermitte’s sign: the current status. Ann Indian Acad Neurol. 2015;18:154. https://doi.org/10.4103/0972-2327.150622.
Sá MJ. Physiopathology of symptoms and signs in multiple sclerosis. Arq Neuropsiquiatr. 2012;70:733–40. https://doi.org/10.1590/S0004-282X2012000900016.
Al-Araji AH, Oger J. Reappraisal of Lhermitte’s sign in multiple sclerosis. Mult Scler J. 2005;11:398–402. https://doi.org/10.1191/1352458505ms1177oa.
Zhang L, Berta T, Xu Z-Z, Liu T, Park JY, Ji R-R. TNF-alpha contributes to spinal cord synaptic plasticity and inflammatory pain: distinct role of TNF receptor subtypes 1 and 2. Pain. 2011;152:419–27. https://doi.org/10.1016/j.pain.2010.11.014.
Cruccu G, Finnerup NB, Jensen TS, Scholz J, Sindou M, Svensson P, et al. Trigeminal neuralgia. Neurology. 2016;87:220–8. https://doi.org/10.1212/WNL.0000000000002840.
Di Stefano G, Maarbjerg S, Truini A. Trigeminal neuralgia secondary to multiple sclerosis: from the clinical picture to the treatment options. J Headache Pain. 2019;20:20. https://doi.org/10.1186/s10194-019-0969-0.
Peker S, Kurtkaya Ö, Üzün İ, Pamir MN. Microanatomy of the central myelin-peripheral myelin transition zone of the trigeminal nerve. Neurosurgery. 2006;59:354–9. https://doi.org/10.1227/01.NEU.0000223501.27220.69.
Cruccu G, Biasiotta A, Di Rezze S, Fiorelli M, Galeotti F, Innocenti P, et al. Trigeminal neuralgia and pain related to multiple sclerosis. Pain. 2009;143:186–91. https://doi.org/10.1016/j.pain.2008.12.026.
Godazandeh K, Martinez Sosa S, Wu J, Zakrzewska JM. Trigeminal neuralgia: comparison of characteristics and impact in patients with or without multiple sclerosis. Mult Scler Relat Disord. 2019;34:41–6. https://doi.org/10.1016/j.msard.2019.06.015.
Truini A, Prosperini L, Calistri V, Fiorelli M, Pozzilli C, Millefiorini E, et al. A dual concurrent mechanism explains trigeminal neuralgia in patients with multiple sclerosis. Neurology. 2016;86:2094–9. https://doi.org/10.1212/WNL.0000000000002720.
Gerwin R. Chronic facial pain: trigeminal neuralgia, persistent idiopathic facial pain, and myofascial pain syndrome: an evidence-based narrative review and etiological hypothesis. Int J Environ Res Public Health. 2020;17:7012. https://doi.org/10.3390/ijerph17197012.
Obermann M, Yoon M-S, Ese D, Maschke M, Kaube H, Diener H-C, et al. Impaired trigeminal nociceptive processing in patients with trigeminal neuralgia. Neurology. 2007;69:835–41. https://doi.org/10.1212/01.wnl.0000269670.30045.6b.
Truini A, Garcia-Larrea L, Cruccu G. Reappraising neuropathic pain in humans—how symptoms help disclose mechanisms. Nat Rev Neurol. 2013;9:572–82. https://doi.org/10.1038/nrneurol.2013.180.
Maarbjerg S, Gozalov A, Olesen J, Bendtsen L. Concomitant persistent pain in classical trigeminal neuralgia: evidence for different subtypes. Headache J Head Face Pain. 2014;54:1173–83. https://doi.org/10.1111/head.12384.
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211. https://doi.org/10.1177/0333102417738202.
Benoliel R, Svensson P, Evers S, Wang S-J, Barke A, Korwisi B, et al. The IASP classification of chronic pain for ICD-11: chronic secondary headache or orofacial pain. Pain. 2019;160:60–8. https://doi.org/10.1097/j.pain.0000000000001435.
Zakrzewska JM. Multi-dimensionality of chronic pain of the oral cavity and face. J Headache Pain. 2013;14:37. https://doi.org/10.1186/1129-2377-14-37.
Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008;15:1013–28. https://doi.org/10.1111/j.1468-1331.2008.02185.x.
Mazhari A. Multiple sclerosis-related pain syndromes: an imaging update. Curr Pain Headache Rep. 2016;20:63. https://doi.org/10.1007/s11916-016-0594-4.
Ferraro D, Plantone D, Morselli F, Dallari G, Simone AM, Vitetta F, et al. Systematic assessment and characterization of chronic pain in multiple sclerosis patients. Neurol Sci. 2018;39:445–53. https://doi.org/10.1007/s10072-017-3217-x.
Rog D, Nurmikko T, Young C. Oromucosal Δ9-tetrahydrocannabinol/cannabidiol for neuropathic pain associated with multiple sclerosis: an uncontrolled, open-label, 2-year extension trial. Clin Ther. 2007;29:2068–79. https://doi.org/10.1016/j.clinthera.2007.09.013.
Wilsey B, Marcotte T, Tsodikov A, Millman J, Bentley H, Gouaux B, et al. A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain. 2008;9:506–21. https://doi.org/10.1016/j.jpain.2007.12.010.
Wilsey B, Marcotte T, Deutsch R, Gouaux B, Sakai S, Donaghe H. Low-dose vaporized cannabis significantly improves neuropathic pain. J Pain. 2013;14:136–48. https://doi.org/10.1016/j.jpain.2012.10.009.
Svendsen KB, Jensen TS, Bach FW. Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised double blind placebo controlled crossover trial. BMJ. 2004;329:253. https://doi.org/10.1136/bmj.38149.566979.AE.
Smith C, Birnbaum G, Carter JL, Greenstein J, Lublin FD. Tizanidine treatment of spasticity caused by multiple sclerosis: results of a double-blind, placebo-controlled trial. US Tizanidine Study Group. Neurology. 1994;44:S34–42 (discussion S42–3).
Vakhapova V, Auriel E, Karni A. Nightly sublingual tizanidine HCl in multiple sclerosis. Clin Neuropharmacol. 2010;33:151–4. https://doi.org/10.1097/WNF.0b013e3181daad7d.
Sachais BA. Baclofen, a new antispastic drug. Arch Neurol. 1977;34:422. https://doi.org/10.1001/archneur.1977.00500190056008.
From A, Heltberg A. A double-blind trial with baclofen (Lioresal®) and diazepam in spasticity due to multiple sclerosis. Acta Neurol Scand. 2009;51:158–66. https://doi.org/10.1111/j.1600-0404.1975.tb01366.x.
Cartlidge NEF, Hudgson P, Weightman D. A comparison of baclofen and diazepam in the treatment of spasticity. J Neurol Sci. 1974;23:17–24. https://doi.org/10.1016/0022-510X(74)90137-3.
Cutter NC, Scott DD, Johnson JC, Whiteneck G. Gabapentin effect on spasticity in multiple sclerosis: a placebo-controlled, randomized trial. Arch Phys Med Rehabil. 2000;81:164–9. https://doi.org/10.1016/s0003-9993(00)90135-7.
Bennett MI, Simpson KH. Gabapentin in the treatment of neuropathic pain. Palliat Med. 2004;18:5–11. https://doi.org/10.1191/0269216304pm845ra.
McCleane GJ. Intravenous infusion of phenytoin relieves neuropathic pain: a randomized, double-blinded, placebo-controlled, crossover study. Anesth Analg. 1999;89:985. https://doi.org/10.1097/00000539-199910000-00030.
Harke H, Gretenkort P, Ladleif HU, Rahman S, Harke O. The response of neuropathic pain and pain in complex regional pain syndrome I to carbamazepine and sustained-release morphine in patients pretreated with spinal cord stimulation: a double-blinded randomized study. Anesth Analg. 2001. https://doi.org/10.1097/00000539-200102000-00039.
Cianchetti C, Zuddas A, Randazzo AP, Perra L, Marrosu MG. Lamotrigine adjunctive therapy in painful phenomena in MS: preliminary observations. Neurology. 1999;53:433. https://doi.org/10.1212/WNL.53.2.433.
Vollmer TL, Robinson MJ, Risser RC, Malcolm SK. A randomized, double-blind, placebo-controlled trial of duloxetine for the treatment of pain in patients with multiple sclerosis. Pain Pract. 2014;14:732–44. https://doi.org/10.1111/papr.12127.
Aiyer R, Barkin RL, Bhatia A. Treatment of neuropathic pain with venlafaxine: a systematic review. Pain Med. 2016. https://doi.org/10.1093/pm/pnw261.
Vrethem M, Boivie J, Arnqvist H, Holmgren H, Lindström T, Thorell L-H. A comparison of amitriptyline and maprotiline in the treatment of painful polyneuropathy in diabetics and nondiabetics. Clin J Pain. 1997;13:313–23. https://doi.org/10.1097/00002508-199712000-00009.
Wang H-Y, Frankfurt M, Burns LH. High-affinity naloxone binding to filamin A prevents mu opioid receptor–Gs coupling underlying opioid tolerance and dependence. PLoS ONE. 2008;3: e1554. https://doi.org/10.1371/journal.pone.0001554.
Cree BAC, Kornyeyeva E, Goodin DS. Pilot trial of low-dose naltrexone and quality of life in multiple sclerosis. Ann Neurol. 2010. https://doi.org/10.1002/ana.22006.
Gironi M, Martinelli-Boneschi F, Sacerdote P, Solaro C, Zaffaroni M, Cavarretta R, et al. A pilot trial of low-dose naltrexone in primary progressive multiple sclerosis. Mult Scler J. 2008;14:1076–83. https://doi.org/10.1177/1352458508095828.
Hyman N. Botulinum toxin (Dysport(R)) treatment of hip adductor spasticity in multiple sclerosis: a prospective, randomised, double blind, placebo controlled, dose ranging study. J Neurol Neurosurg Psychiatry. 2000;68:707–12. https://doi.org/10.1136/jnnp.68.6.707.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–73. https://doi.org/10.1016/S1474-4422(14)70251-0.
Attal N. Pharmacological treatments of neuropathic pain: the latest recommendations. Rev Neurol (Paris). 2019;175:46–50. https://doi.org/10.1016/j.neurol.2018.08.005.
Sansone RA, Sansone LA. Pain, pain, go away: antidepressants and pain management. Psychiatry (Edgmont). 2008;5:16–9.
Liampas A, Rekatsina M, Vadalouca A, Paladini A, Varrassi G, Zis P. Pharmacological management of painful peripheral neuropathies: a systematic review. Pain Ther. 2021;10:55–68. https://doi.org/10.1007/s40122-020-00210-3.
Stamoula E, Siafis S, Dardalas I, Ainatzoglou A, Matsas A, Athanasiadis T, et al. Antidepressants on multiple sclerosis: a review of in vitro and in vivo models. Front Immunol. 2021;12: 677879. https://doi.org/10.3389/fimmu.2021.677879.
American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–94. https://doi.org/10.1111/jgs.15767
Max MB, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med. 1992;326:1250–6. https://doi.org/10.1056/NEJM199205073261904.
Sindrup SH, Gram LF, Brøsen K, Eshøj O, Mogensen EF. The selective serotonin reuptake inhibitor paroxetine is effective in the treatment of diabetic neuropathy symptoms. Pain. 1990;42:135–44. https://doi.org/10.1016/0304-3959(90)91157-E.
Colombo B, Annovazzi POL, Comi G. Medications for neuropathic pain: current trends. Neurol Sci. 2006;27:s183–9. https://doi.org/10.1007/s10072-006-0598-7.
Foley P, Parker RA, de Angelis F, Connick P, Chandran S, Young C, et al. Efficacy of fluoxetine, riluzole and amiloride in treating neuropathic pain associated with secondary progressive multiple sclerosis: pre-specified analysis of the MS-SMART double-blind randomised placebo-controlled trial. Mult Scler Relat Disord. 2022;63: 103925. https://doi.org/10.1016/j.msard.2022.103925.
Falah M, Madsen C, Holbech JV, Sindrup SH. A randomized, placebo-controlled trial of levetiracetam in central pain in multiple sclerosis. Eur J Pain. 2012;16:860–9. https://doi.org/10.1002/j.1532-2149.2011.00073.x.
Jensen TS. Anticonvulsants in neuropathic pain: rationale and clinical evidence. Eur J Pain. 2002;6:61–8. https://doi.org/10.1053/eujp.2001.0324.
McCleane GJ. Lamotrigine in the management of neuropathic pain: a review of the literature. Clin J Pain. 2000;16:321–6. https://doi.org/10.1097/00002508-200012000-00008.
Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain. 2005;118:289–305. https://doi.org/10.1016/j.pain.2005.08.013.
Kim PS, Fishman MA. Low-dose naltrexone for chronic pain: update and systemic review. Curr Pain Headache Rep. 2020;24:64. https://doi.org/10.1007/s11916-020-00898-0.
Sharafaddinzadeh N, Moghtaderi A, Kashipazha D, Majdinasab N, Shalbafan B. The effect of low-dose naltrexone on quality of life of patients with multiple sclerosis: a randomized placebo-controlled trial. Mult Scler J. 2010;16:964–9. https://doi.org/10.1177/1352458510366857.
Kaiman S, Österberg A, Sörensen J, Boivie J, Bertler Å. Morphine responsiveness in a group of well-defined multiple sclerosis patients: a study with i.v. morphine. Eur J Pain 2002;6:69–80. https://doi.org/10.1053/eujp.2001.0307.
Dworsky-Fried Z, Chadwick CI, Kerr BJ, Taylor AMW. Multiple sclerosis and the endogenous opioid system. Front Neurosci. 2021;15: 741503. https://doi.org/10.3389/fnins.2021.741503.
Marrie RA, Fisk JD, Walld R, Bolton JM, Sareen J, Patten SB, et al. Prescription opioid use in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2023;94:167–9. https://doi.org/10.1136/jnnp-2022-329508.
Campos RMP, Aguiar AFL, Paes-Colli Y, Trindade PMP, Ferreira BK, de Melo Reis RA, et al. Cannabinoid therapeutics in chronic neuropathic pain: from animal research to Human treatment. Front Physiol. 2021;12: 785176. https://doi.org/10.3389/fphys.2021.785176.
Anand U, Pacchetti B, Anand P, Sodergren MH. Cannabis-based medicines and pain: a review of potential synergistic and entourage effects. Pain Manag. 2021;11:395–403. https://doi.org/10.2217/pmt-2020-0110.
Aborode AT, Awuah WA, Mikhailova T, Abdul- Rahman T, Pavlock S, Nansubuga EP, et al. OMICs Ttchnologies for natural compounds-based drug development. Curr Top Med Chem. 2022;22:1751–65. https://doi.org/10.2174/1568026622666220726092034.
Rudroff T, Sosnoff J. Cannabidiol to improve mobility in people with multiple sclerosis. Front Neurol. 2018;9:183. https://doi.org/10.3389/fneur.2018.00183.
Rog DJ, Nurmikko TJ, Friede T, Young CA. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology. 2005;65:812–9. https://doi.org/10.1212/01.wnl.0000176753.45410.8b.
Koppel BS, Brust JCM, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014;82:1556–63. https://doi.org/10.1212/WNL.0000000000000363.
Turcotte D, Doupe M, Torabi M, Gomori A, Ethans K, Esfahani F, et al. Nabilone as an adjunctive to gabapentin for multiple sclerosis-induced neuropathic pain: a randomized controlled trial. Pain Med. 2015;16:149–59. https://doi.org/10.1111/pme.12569.
Piper BJ, DeKeuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. 2017;31:569–75. https://doi.org/10.1177/0269881117699616.
Nielsen S, Germanos R, Weier M, Pollard J, Degenhardt L, Hall W, et al. The use of cannabis and cannabinoids in treating symptoms of multiple sclerosis: a systematic review of reviews. Curr Neurol Neurosci Rep. 2018;18:8. https://doi.org/10.1007/s11910-018-0814-x.
Karst M, Wippermann S, Ahrens J. Role of cannabinoids in the treatment of pain and (painful) spasticity. Drugs. 2010;70:2409–38. https://doi.org/10.2165/11585260-000000000-00000.
Link K, Knowles LM, Alschuler KN, Ehde DM. Characterizing cannabis use in a sample of adults with multiple sclerosis and chronic pain: an observational study. Mult Scler Relat Disord. 2023;75: 104742. https://doi.org/10.1016/j.msard.2023.104742.
Sirbu C-A, Georgescu R, Pleşa FC, Paunescu A, Marilena Ţânţu M, Nicolae AC, et al. Cannabis and cannabinoids in multiple sclerosis: from experimental models to clinical practice: a review. Am J Ther. 2023;30:e220–31. https://doi.org/10.1097/MJT.0000000000001568.
Hansen JS, Gustavsen S, Roshanisefat H, Kant M, Biering-Sørensen F, Andersen C, et al. Cannabis-based medicine for neuropathic pain and spasticity: a multicenter, randomized, double-blinded, placebo-controlled trial. Pharmaceuticals. 2023;16:1079. https://doi.org/10.3390/ph16081079.
Otero-Romero S, Sastre-Garriga J, Comi G, Hartung H-P, Soelberg Sørensen P, Thompson AJ, et al. Pharmacological management of spasticity in multiple sclerosis: systematic review and consensus paper. Mult Scler J. 2016;22:1386–96. https://doi.org/10.1177/1352458516643600.
Di Stefano G, De Stefano G, Di Lionardo A, Cruccu G, Truini A. Pharmacotherapeutic options for managing pain in multiple sclerosis. CNS Drugs. 2020;34:749–61. https://doi.org/10.1007/s40263-020-00731-7.
Yu B, Wu K, Xu X, Liu Y, Jiang J. Recent advances in nanoplatforms for the treatment of neuropathic pain. Spinal Cord. 2022;60:594–603. https://doi.org/10.1038/s41393-021-00746-x.
Bidve P, Prajapati N, Kalia K, Tekade R, Tiwari V. Emerging role of nanomedicine in the treatment of neuropathic pain. J Drug Target. 2020;28:11–22. https://doi.org/10.1080/1061186X.2019.1587444.
Zhu Y, Yao Y, Kuang R, Chen Z, Du Z, Qu S. Global research trends of nanotechnology for pain management. Front Bioeng Biotechnol. 2023. https://doi.org/10.3389/fbioe.2023.1249667.
Kuthati Y, Navakanth Rao V, Busa P, Tummala S, Davuluri Venkata Naga G, Wong CS. Scope and applications of nanomedicines for the management of neuropathic pain. Mol Pharm. 2020;17:1015–27. https://doi.org/10.1021/acs.molpharmaceut.9b01027.
Tkach M, Théry C. Communication by extracellular vesicles: where we are and where we need to go. Cell. 2016;164:1226–32. https://doi.org/10.1016/j.cell.2016.01.043.
Hunter Z, McCarthy DP, Yap WT, Harp CT, Getts DR, Shea LD, et al. A biodegradable nanoparticle platform for the induction of antigen-specific immune tolerance for treatment of autoimmune disease. ACS Nano. 2014;8:2148–60. https://doi.org/10.1021/nn405033r.
Pearson RM, Casey LM, Hughes KR, Wang LZ, North MG, Getts DR, et al. Controlled delivery of single or multiple antigens in tolerogenic nanoparticles using peptide-polymer bioconjugates. Mol Ther. 2017;25:1655–64. https://doi.org/10.1016/j.ymthe.2017.04.015.
Belousov AN, Belousova EY, Lekomtseva YV. Prospects for the application of nanotechnology in the treatment of multiple sclerosis. Int J Clin Med Case Rep. 2023;2:1–8. https://doi.org/10.31579/2834-8664/017.
Yao L, Bojic D, Liu M. Applications and safety of gold nanoparticles as therapeutic devices in clinical trials. J Pharm Anal. 2023;13:960–7. https://doi.org/10.1016/j.jpha.2023.06.001.
Chen ML, Yao L, Boger J, Mercer K, Thompson B, Jiang N. Non-invasive brain stimulation interventions for management of chronic central neuropathic pain: a scoping review protocol. BMJ Open. 2017;7: e016002. https://doi.org/10.1136/bmjopen-2017-016002.
Johnson MI, Walsh DM. Continued uncertainty of TENS’ effectiveness for pain relief. Nat Rev Rheumatol. 2010;6:314–6. https://doi.org/10.1038/nrrheum.2010.77.
Kannan P, Bello UM, Winser SJ. Physiotherapy interventions may relieve pain in individuals with central neuropathic pain: a systematic review and meta-analysis of randomised controlled trials. Ther Adv Chronic Dis. 2022;13:204062232210786. https://doi.org/10.1177/20406223221078672.
Sawant A, Dadurka K, Overend T, Kremenchutzky M. Systematic review of efficacy of TENS for management of central pain in people with multiple sclerosis. Mult Scler Relat Disord. 2015;4:219–27. https://doi.org/10.1016/j.msard.2015.03.006.
Mokhtari T, Ren Q, Li N, Wang F, Bi Y, Hu L. Transcutaneous electrical nerve stimulation in relieving neuropathic pain: basic mechanisms and clinical applications. Curr Pain Headache Rep. 2020;24:14. https://doi.org/10.1007/s11916-020-0846-1.
Katirci Kirmaci Zİ, Adigüzel H, Göğremiş M, Kirmaci YŞ, İnanç Y, Tuncel BD. The effect of transcutaneous electrical nerve stimulation (TENS) and interferential currents (IFC) on pain, functional capacity, and quality of life in patients with multiple sclerosis: a randomized controlled, single-blinded study. Mult Scler Relat Disord. 2023;71: 104541. https://doi.org/10.1016/j.msard.2023.104541.
Lefaucheur J-P, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018). Clin Neurophysiol. 2020;131:474–528. https://doi.org/10.1016/j.clinph.2019.11.002.
Comi G, Solari A, Leocani L, Centonze D, Otero-Romero S. Italian consensus on treatment of spasticity in multiple sclerosis. Eur J Neurol. 2020;27:445–53. https://doi.org/10.1111/ene.14110.
Aloizou A-M, Pateraki G, Anargyros K, Siokas V, Bakirtzis C, Liampas I, et al. Transcranial magnetic stimulation (TMS) and repetitive TMS in multiple sclerosis. Rev Neurosci. 2021;32:723–36. https://doi.org/10.1515/revneuro-2020-0140.
Palm U, Ayache SS, Padberg F, Lefaucheur J-P. Non-invasive brain stimulation therapy in multiple sclerosis: a review of tDCS, rTMS and ECT results. Brain Stimul. 2014;7:849–54. https://doi.org/10.1016/j.brs.2014.09.014.
Mori F, Codecà C, Kusayanagi H, Monteleone F, Buttari F, Fiore S, et al. Effects of nodal transcranial direct current stimulation on chronic neuropathic pain in patients with multiple sclerosis. J Pain. 2010;11:436–42. https://doi.org/10.1016/j.jpain.2009.08.011.
Ayache SS, Palm U, Chalah MA, Al-Ani T, Brignol A, Abdellaoui M, et al. Prefrontal tDCS decreases pain in patients with multiple sclerosis. Front Neurosci. 2016;10:147. https://doi.org/10.3389/fnins.2016.00147.
Young J, Zoghi M, Khan F, Galea MP. The effect of transcranial direct current stimulation on chronic neuropathic pain in patients with multiple sclerosis: randomized controlled trial. Pain Med. 2020;21:3451–7. https://doi.org/10.1093/pm/pnaa128.
Berra E, Bergamaschi R, De Icco R, Dagna C, Perrotta A, Rovaris M, et al. The effects of transcutaneous spinal direct current stimulation on neuropathic pain in multiple sclerosis: clinical and neurophysiological assessment. Front Hum Neurosci. 2019;13:31. https://doi.org/10.3389/fnhum.2019.00031.
Provenzano DA, Williams JR, Jarzabek G, DeRiggi LA, Scott TF. Treatment of neuropathic pain and functional limitations associated with multiple sclerosis using an MRI-compatible spinal cord stimulator: a case report with two year follow-up and literature review. Neuromodulation Technol Neural Interface. 2016;19:406–13. https://doi.org/10.1111/ner.12409.
Lam CM, Monroe BR. Successful treatment of central pain and spasticity in patient with multiple sclerosis with dorsal column, paresthesia-free spinal cord stimulator: a case report. A&A Pract. 2019;12:308–12. https://doi.org/10.1213/XAA.0000000000000918.
Palm U, Chalah MA, Padberg F, Al-Ani T, Abdellaoui M, Sorel M, et al. Effects of transcranial random noise stimulation (tRNS) on affect, pain and attention in multiple sclerosis. Restor Neurol Neurosci. 2016;34:189–99. https://doi.org/10.3233/RNN-150557.
Harries AM, Mitchell RD. Percutaneous glycerol rhizotomy for trigeminal neuralgia: safety and efficacy of repeat procedures. Br J Neurosurg. 2011;25:268–72. https://doi.org/10.3109/02688697.2011.558946.
Patwardhan RV, Minagar A, Kelley RE, Nanda A. Neurosurgical treatment of multiple sclerosis. Neurol Res. 2006;28:320–5. https://doi.org/10.1179/016164106X98224.
Berk C, Constantoyannis C, Honey CR. The treatment of trigeminal neuralgia in patients with multiple sclerosis using percutaneous radiofrequency rhizotomy. Can J Neurol Sci/J Can Des Sci Neurol. 2003;30:220–3. https://doi.org/10.1017/S0317167100002626.
Mousavi SH, Gehling P, Burchiel KJ. The long-term outcome of radiofrequency ablation in multiple sclerosis-related symptomatic trigeminal neuralgia. Neurosurgery. 2022;90:293–9. https://doi.org/10.1227/NEU.0000000000001817.
Martin S, Teo M, Suttner N. The effectiveness of percutaneous balloon compression in the treatment of trigeminal neuralgia in patients with multiple sclerosis. J Neurosurg. 2015;123:1507–11. https://doi.org/10.3171/2014.11.JNS14736.
Noorani I, Lodge A, Vajramani G, Sparrow O. The effectiveness of percutaneous balloon compression, thermocoagulation, and glycerol rhizolysis for trigeminal neuralgia in multiple sclerosis. Neurosurgery. 2019;85:E684–92. https://doi.org/10.1093/neuros/nyz103.
Hong T, Ding Y, Yao P. Long-term efficacy and complications of radiofrequency thermocoagulation at different temperatures for the treatment of trigeminal neuralgia. Biochem Res Int. 2020;2020:1–10. https://doi.org/10.1155/2020/3854284.
Al Barim B, Lemcke L, Schwake M, Schipmann S, Stummer W. Repetitive percutaneous radiofrequency thermocoagulation for persistent idiopathic facial pain and central neuropathic pain attributed to multiple sclerosis: a retrospective monocentric analysis. Acta Neurochir (Wien). 2020;162:2791–800. https://doi.org/10.1007/s00701-020-04486-4.
Bender MT, Pradilla G, Batra S, See AP, James C, Pardo CA, et al. Glycerol rhizotomy and radiofrequency thermocoagulation for trigeminal neuralgia in multiple sclerosis. J Neurosurg. 2013;118:329–36. https://doi.org/10.3171/2012.9.JNS1226.
Texakalidis P, Xenos D, Karras CL, Rosenow JM. Percutaneous surgical approaches in multiple sclerosis-related trigeminal neuralgia: a systematic review and meta-analysis. World Neurosurg. 2021;146:342-50.e1. https://doi.org/10.1016/j.wneu.2020.11.006.
Spina A, Nocera G, Boari N, Iannaccone S, Mortini P. Efficacy of Gamma knife radiosurgery in the management of multiple sclerosis-related trigeminal neuralgia: a systematic review and meta-analysis. Neurosurg Rev. 2021;44:3069–77. https://doi.org/10.1007/s10143-021-01507-3.
Leduc W, Mathieu D, Adam E, Ferreira R, Iorio-Morin C. Gamma knife stereotactic radiosurgery for trigeminal neuralgia secondary to multiple sclerosis: a case-control study. Neurosurgery. 2023;93:453–61. https://doi.org/10.1227/neu.0000000000002440.
Franzini A, Tropeano MP, Olei S, De Robertis M, Rossini Z, Attuati L, et al. Gamma knife radiosurgery for the treatment of trigeminal neuralgia in patients with multiple sclerosis: a single-center retrospective study and literature review. World Neurosurg. 2021;149:e92-100. https://doi.org/10.1016/j.wneu.2021.02.074.
Serhan A, Kiwan A, Abushukair H, Yassin A. Deep brain stimulation use in treating multiple sclerosis tremor: a practical approach for meta-analyses. Mult Scler Relat Disord. 2022;58: 103491. https://doi.org/10.1016/j.msard.2022.103491.
Pereira EAC, Aziz TZ. Neuropathic pain and deep brain stimulation. Neurotherapeutics. 2014;11:496–507. https://doi.org/10.1007/s13311-014-0278-x.
Naranjo C, Del Reguero L, Moratalla G, Hercberg M, Valenzuela M, Failde I. Anxiety, depression and sleep disorders in patients with diabetic neuropathic pain: a systematic review. Expert Rev Neurother. 2019;19:1201–9. https://doi.org/10.1080/14737175.2019.1653760.
Boiko DI, Chopra H, Bilal M, Kydon PV, Herasymenko LO, Rud VO, et al. Schizophrenia and disruption of circadian rhythms: an overview of genetic, metabolic and clinical signs. Schizophr Res. 2024;264:58–70. https://doi.org/10.1016/j.schres.2023.12.002.
Humo M, Lu H, Yalcin I. The molecular neurobiology of chronic pain-induced depression. Cell Tissue Res. 2019;377:21–43. https://doi.org/10.1007/s00441-019-03003-z.
Shkodina AD, Zhyvotovska AI, Boiko DI. Sleep and armed conflict: future complications of war in Ukraine. Rev Neurol (Paris). 2022;178:869–71. https://doi.org/10.1016/j.neurol.2022.09.002.
Boiko DI, Skrypnikov AM, Shkodina AD, Hasan MM, Ashraf GM, Rahman MH. Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19. Environ Sci Pollut Res. 2022;29:28062–9. https://doi.org/10.1007/s11356-021-18384-4.
Boiko DI, Shyrai PO, Mats OV, Karpik ZI, Rahman MH, Khan AA, et al. Mental health and sleep disturbances among Ukrainian refugees in the context of Russian-Ukrainian war: a preliminary result from online-survey. Sleep Med. 2024;113:342–8. https://doi.org/10.1016/j.sleep.2023.12.004.
Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: the first step in pain neuroscience education. Physiother Theory Pract. 2016;32:368–84. https://doi.org/10.1080/09593985.2016.1194651.
Boiko DI, Kachur RV, Ajala OM, Bodnar LA, Zhyvotovska LV. Characteristics of anxiety and depressive manifestations in patients with acute myocardial infarction taking into account their personal accentuations. Azerbaijan Med J. 2021;2:25–31. https://doi.org/10.34921/amj.2021.2.004.
Abu Alhaija ES, AlDaikki A, Al-Omairi MK, Al-Khateeb SN. The relationship between personality traits, pain perception and attitude toward orthodontic treatment. Angle Orthod. 2010;80:1141–9. https://doi.org/10.2319/012710-59.1.
Heitmann H, Biberacher V, Tiemann L, Buck D, Loleit V, Selter RC, et al. Prevalence of neuropathic pain in early multiple sclerosis. Mult Scler J. 2016;22:1224–30. https://doi.org/10.1177/1352458515613643.
Delva M, Skoryk K, Delva I. Predictors of neuropathic dysesthetic pain occurrence and chronification in multiple sclerosis (2-year prospective study). Acta Biomed. 2023;94:e2023229. https://doi.org/10.23750/abm.v94i6.14609.
Driscoll MA, Edwards RR, Becker WC, Kaptchuk TJ, Kerns RD. Psychological interventions for the treatment of chronic pain in adults. Psychol Sci Public Interest. 2021;22:52–95. https://doi.org/10.1177/15291006211008157.
Li C, Hou W, Ding D, Yang Y, Gu S, Zhu Y. Evidence mapping based on systematic reviews of cognitive behavioral therapy for neuropathic pain. Neural Plast. 2023;2023:2680620. https://doi.org/10.1155/2023/2680620.
Hayes SC. Acceptance and commitment therapy: towards a unified model of behavior change. World Psychiatry. 2019;18:226–7. https://doi.org/10.1002/wps.20626.
Gromisch ES, Kerns RD, Czlapinski R, Beenken B, Otis J, Lo AC, et al. Cognitive behavioral therapy for the management of multiple sclerosis-related pain. Int J MS Care. 2020;22:8–14. https://doi.org/10.7224/1537-2073.2018-023.
Ma T-W, Yuen AS-K, Yang Z. The efficacy of acceptance and commitment therapy for chronic pain. Clin J Pain. 2023;39:147–57. https://doi.org/10.1097/AJP.0000000000001096.
Harrison AM, McCracken LM, Jones K, Norton S, Moss-Morris R. Using mixed methods case-series evaluation in the development of a guided self-management hybrid CBT and ACT intervention for multiple sclerosis pain. Disabil Rehabil. 2017;39:1785–98. https://doi.org/10.1080/09638288.2016.1209580.
Sadeghi-Bahmani D, Esmaeili L, Mokhtari F, Sadeghi Bahmani L, Afsharzadeh M, Shaygannejad V, et al. Effects of acceptance and commitment therapy (ACT) and mindfulness-based stress reduction (MBSR) on symptoms and emotional competencies in individuals with multiple sclerosis. Mult Scler Relat Disord. 2022;67: 104029. https://doi.org/10.1016/j.msard.2022.104029.
Hadoush H, Alawneh A, Kassab M, Al-Wardat M, Al-Jarrah M. Effectiveness of non-pharmacological rehabilitation interventions in pain management in patients with multiple sclerosis: systematic review and meta-analysis. NeuroRehabilitation. 2022;50:347–65. https://doi.org/10.3233/NRE-210328.
Kubsik A, Klimkiewicz P, Klimkiewicz R, Janczewska K, Woldańska-Okońska M. Rehabilitation in multiple sclerosis. Adv Clin Exp Med. 2017;26:709–15. https://doi.org/10.17219/acem/62329.
Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2019;1:CD012732. https://doi.org/10.1002/14651858.CD012732.pub2.
Halabchi F, Alizadeh Z, Sahraian MA, Abolhasani M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017;17:185. https://doi.org/10.1186/s12883-017-0960-9.
Hasanpour DA. Influence of yoga and aerobics exercise on fatigue, pain and psychosocial status in patients with multiple sclerosis: a randomized trial. J Sports Med Phys Fitness. 2016;56:1417–22.
Demaneuf T, Aitken Z, Karahalios A, Leong TI, De Livera AM, Jelinek GA, et al. Effectiveness of exercise interventions for pain reduction in people with multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2019;100:128–39. https://doi.org/10.1016/j.apmr.2018.08.178.
Hughes C, Smyth S, Lowe-Strong A. Reflexology for the treatment of pain in people with multiple sclerosis: a double-blind randomised sham-controlled clinical trial. Mult Scler J. 2009;15:1329–38. https://doi.org/10.1177/1352458509345916.
Archer KR, Coronado RA, Wegener ST. The role of psychologically informed physical therapy for musculoskeletal pain. Curr Phys Med Rehabil Rep. 2018;6:15–25. https://doi.org/10.1007/s40141-018-0169-x.
Coronado RA, Brintz CE, McKernan LC, Master H, Motzny N, Silva FM, et al. Psychologically informed physical therapy for musculoskeletal pain: current approaches, implications, and future directions from recent randomized trials. Pain Rep. 2020;5: e847. https://doi.org/10.1097/PR9.0000000000000847.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by Poltava State Medical University (research projects Nos. 0120U104165, 0121U108235, 0124U000094).
Conflicts of interest/competing interests
Anastasiia D. Shkodina, Hitesh Chopra, Onyekachi Emmanuel Anyagwa , Mainak Bardhan, Viktoriia A. Pinchuk, Kateryna V. Hryn, Anzhelina M. Kryvchun, Dmytro I. Boiko, Vinay Suresh, Amogh Verma, and Mykhailo Yu. Delva have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Authors’ contributions
ADS: conceptualization, methodology, writing—original draft, project administration, writing—review and editing; HC: writing—original draft, writing—review and editing; OEA: writing—original draft; MB: conceptualization, methodology, writing—review and editing; VAP: writing—original draft, KVH: writing—original draft; AMK: writing—original draft; DIB: writing—original draft, writing—review and editing; VS: resources, software, supervision, validation, writing—review and editing; AV: visualization, resources, software, validation; MYD: conceptualization, supervision, validation, writing—original draft.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shkodina, A.D., Bardhan, M., Chopra, H. et al. Pharmacological and Non-pharmacological Approaches for the Management of Neuropathic Pain in Multiple Sclerosis. CNS Drugs 38, 205–224 (2024). https://doi.org/10.1007/s40263-024-01072-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-024-01072-5