Abstract
Objective
To investigate the association between antipsychotic drug use and the development of first-time seizures in patients with schizophrenia, affective disorders, or dementia.
Methods
We used data from the UK-based Clinical Practice Research Datalink database to conduct a follow-up study with a nested case–control analysis between 1998 and 2013. We identified patients with schizophrenia, affective disorders, or dementia, and estimated incidence rates of seizures among users of four antipsychotic drug subclasses, defined according to existing hypotheses on their seizure-inducing potential (1, olanzapine or quetiapine; 2, amisulpride, aripiprazole, risperidone, or sulpiride; 3, low-to-medium potency first-generation antipsychotic drugs [chlorpromazine, zuclopenthixol, flupenthixol, pericyazine, promazine, thioridazine]; 4, medium-to-high potency first-generation antipsychotic drugs [haloperidol, prochlorperazine, trifluoperazine]), and among those who did not use antipsychotic drugs. To adjust for confounding, we estimated odds ratios for seizures separately among patients with affective disorders or dementia, stratified by antipsychotic drug use and timing of use.
Results
In the total cohort of 60,121 patients (who had schizophrenia, affective disorders, or dementia), the incidence rate of seizures per 10,000 person-years was 32.6 (95 % confidence interval [CI] 22.6–42.6) in users of olanzapine or quetiapine, 24.1 (95 % CI 13.2–34.9) in users of amisulpride, aripiprazole, risperidone, or sulpiride, 49.4 (95 % CI 27.7–71.0) in users of low-to-medium potency antipsychotic drugs, 59.1 (95 % CI 40.1–78.2) in users of medium-to-high potency antipsychotic drugs, and 11.7 (95 % CI 10.0–13.4) in non-users of antipsychotic drugs. Patients with dementia had significantly higher incidence rates of first-time seizures compared with patients with affective disorders, irrespective of antipsychotic drug use. In patients with affective disorders, current use of medium-to-high potency first-generation antipsychotic drugs was associated with an increased risk of seizures (adjusted odds ratio 2.51 [95 % CI 1.51–4.18]) compared with non-use, while use of other antipsychotic drugs was not associated with seizures. In patients with dementia, current use of olanzapine or quetiapine (adjusted odds ratio 2.37 [95 % CI 1.35–4.15]), low-to-medium potency first-generation antipsychotic drugs (adjusted odds ratio 3.08 [95 % CI 1.34–7.08]), and medium-to-high potency first-generation antipsychotic drugs (adjusted odds ratio 2.24 [95 % CI 1.05–4.81]) was associated with an increased risk of seizures compared with non-use, but current use of amisulpride, aripiprazole, risperidone, or sulpiride (adjusted odds ratio 0.92 [95 % CI 0.48–1.75]) was not. Use of antipsychotic drugs in patients with schizophrenia could not be investigated because of small numbers.
Conclusions
Current use of medium-to-high potency first-generation antipsychotic drugs was associated with a 2.5-fold increased risk of seizures compared with non-use of antipsychotic drugs in patients with affective disorders. In these patients, current use of all other antipsychotic drug subclasses was not associated with seizures. In patients with dementia, current and past use of all antipsychotic drug subclasses, except amisulpride, aripiprazole, risperidone, or sulpiride, was associated with an increased risk of seizures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with dementia had significantly higher incidence rates of first-time seizures compared with patients with affective disorders, irrespective of antipsychotic drug use. |
Use of medium-to-high potency first-generation antipsychotic drugs (haloperidol, prochlorperazine, and trifluoperazine) was associated with a more than twofold increased risk of first-time seizures compared with non-use of antipsychotic drugs in patients with affective disorders. |
Use of second-generation antipsychotic drugs amisulpride, aripiprazole, risperidone, or sulpiride, did not increase the risk of first-time seizures compared with non-use of antipsychotic drugs in patients with dementia. |
1 Introduction
Antipsychotic drugs are commonly used in patients with schizophrenia, affective disorders, or dementia [1]. These drugs have been associated with seizures, especially if high doses are applied, if a rapid dose increase occurs, or if other risk factors for seizures are present [2, 3].
Across first-generation antipsychotic drugs, low-potency drugs with strong sedation (particularly aliphatic phenothiazines) have been associated with a higher risk of seizures than high-potency drugs [3–6]. The evidence on this association is scarce and is mainly based on one observational study in hospitalized psychiatric patients published almost 50 years ago [6]. In this study, the overall incidence of seizures over 4.5 years was 1.2 % among 859 phenothiazine users, while no seizures occurred among 669 non-users of phenothiazines [6].
Among second-generation antipsychotic drugs, clozapine has repeatedly been associated with the highest risk of seizures [7–10]. In a meta-analysis of clinical trials including a limited number of patients observed over a short time period, the incidence rate of seizures was higher in users of clozapine, olanzapine, and quetiapine compared with placebo, but not in users of risperidone or ziprasidone [9]. Additionally, users of clozapine, olanzapine, and quetiapine more frequently reported seizures than users of other second-generation antipsychotic drugs (such as risperidone, amisulpride, or aripiprazole) in two studies based on pharmacovigilance data susceptible to reporting bias and confounding [11, 12].
Using primary care observational data collected in the UK over a time span of 15 years, we aimed to explore the association between antipsychotic drug use and the development of first-time seizures in a large population of adult patients with schizophrenia, affective disorders, or dementia. We further aimed to investigate the role of the underlying indication on the risk of seizures in antipsychotic drug users.
2 Methods
2.1 Study Design and Data Source
We used data from the UK-based Clinical Practice Research Datalink (CPRD) database to conduct a retrospective population-based follow-up study with a nested case–control analysis. The CPRD was established more than 25 years ago and encompasses data on some eight million people who are registered with approximately 700 general practitioners (GPs), as described in detail elsewhere [13–16]. The GPs record information on demographics, lifestyle variables, medical diagnoses (recorded as ‘Read codes’), hospitalizations, and drug prescriptions in a standardized anonymous form. The records on drug exposure and diagnoses have repeatedly been validated and proven to be of high quality [17, 18]. The CPRD has been the data source for several observational studies on antipsychotic drug use [19–21] and on seizures [22–25]. This study was approved by the Independent Scientific Advisory Committee for Medicines and Healthcare products Regulatory Agency research (London, UK).
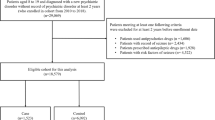
2.2 Study Population
We identified all patients aged 18–89 years between January 1998 and December 2011, who (1) had a first-time diagnosis of schizophrenia, affective disorders, or dementia, followed by an antipsychotic drug prescription at any time thereafter, or (2) a first-time prescription for an antipsychotic drug, provided that a first-time diagnosis of schizophrenia, affective disorders, or dementia followed within 1 year. Schizophrenia, affective disorders, and dementia were defined by codes corresponding to the International Classification of Diseases version 10 (ICD-10) codes F20–29 ‘Schizophrenia, schizotypal and delusional disorders’, F30–39 ‘Mood [affective] disorders’, and F00–F03 ‘Dementia in Alzheimer’s disease’, ‘Vascular dementia’, ‘Dementia in other diseases classified elsewhere’, and ‘Unspecified dementia’. The date of (1) or (2), whichever came first, will subsequently be called the ‘start date’. We excluded patients with a diagnosis of seizures or epilepsy, or any records of antiepileptic prescriptions, prior to the start date. Additionally, we excluded patients with recorded major risk factors for seizures such as a history of alcoholism, drug abuse, head trauma, intracerebral bleeding, brain tumor, brain abscess, sinus vein thrombosis, meningitis, encephalitis, human immunodeficiency virus, or cancer prior to the start date. Patients were required to have had at least 1 year of active history in the database prior to the start date and those with codes suggesting a history of schizophrenia, affective disorders, or dementia prior to the start date were excluded.
2.3 Follow-up and Definition of Seizure Cases
We followed all patients from the start date until they had (1) a first-time diagnosis of seizure or epilepsy (corresponding to ICD-10 codes G40 ‘Epilepsy’, G41 ‘Status epilepticus’, or R56.8 ‘Other and unspecified convulsions’), (2) a first-time prescription for an antiepileptic drug followed by a first-time diagnosis of seizure or epilepsy [as defined under (1)] within 3 months thereafter, (3) a first-time prescription for an antiepileptic drug preceded or followed by a code of a suspected seizure within 3 months before or after, provided that a first-time diagnosis of seizure of epilepsy [as defined under (1)] followed at any time thereafter, (4) until they turned 90 years old, (5) died, (6) left the database, (7) reached the end of last data collection (December 2013), or (8) until 1 month prior to a first-time record of a major risk factor for seizures (as described under ‘study population’), whichever came first. Patients whose follow-up ended because of (1), (2), or (3) will subsequently be called ‘cases’, and their date of follow-up end will be referred to as the ‘index date’.
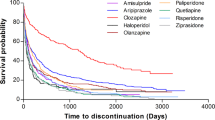
2.4 Person-time Analysis
We assessed person time for four antipsychotic drug subclasses according to existing hypotheses on their seizure-inducing potential (as described in the “Introduction”). We included individual drugs in these subclasses if they encompassed at least 100 person-years of accumulated use. Subclasses included: (1) second-generation drugs associated with a high risk of seizures (olanzapine or quetiapine), (2) other second-generation drugs (amisulpride, aripiprazole, risperidone, and sulpiride), (3) low-to-medium potency first-generation drugs (chlorpromazine, zuclopenthixol, flupenthixol, pericyazine, promazine, thioridazine), and (4) medium to high potency first-generation drugs (haloperidol, prochlorperazine, trifluoperazine). We classified first-generation drugs into low-to-medium or medium-to-high potency according to The American Psychiatric Publishing Textbook of Psychopharmacology [26].
Person time was accumulated as follows: (1) no exposure to antipsychotic drugs (‘no antipsychotic drug treatment’) was defined as the period between the first diagnosis of affective disorders, schizophrenia, or dementia, and the first prescription for an antipsychotic drug, provided that the diagnosis occurred prior to the prescription; (2) current exposure to only one antipsychotic drug (‘mono use’) was defined as use from the day of the prescription through the expected end of treatment plus 7 days, provided that no other antipsychotic drug was prescribed in this period. Patients who switched between different antipsychotic drugs but had no period of overlapping treatment contributed person time to mono use of these different antipsychotic drugs; (3) current exposure to more than one antipsychotic drug concomitantly (‘mixed use’) was defined as use from the day when at least two antipsychotic drugs were prescribed concomitantly through the expected end of treatment of all or all but one antipsychotic drug plus 90 days. Patients who remained treated with one antipsychotic drug after the period of mixed use contributed person time to mono use for the remaining drug thereafter; and (4) past exposure after stopping antipsychotic drug treatment (‘past use’) was defined as the time after mono- or mixed use had elapsed. The duration of treatment was derived from the recorded quantity of tablets, injections, or oral liquids, and the dose instructions. If no quantity or dose instruction was recorded, we used default values in the following order: (1) the quantity and/or dose instruction recorded for the same drug at the closest visit prior to the previous visit, or, if no information was available at any time before, (2) the quantity and/or dose instruction most frequently recorded among our study population for the same drug.
2.5 Nested Case–control Analysis
For each case, we identified up to four controls from the study population with no seizures during the study period. Controls were matched to cases on age (year of birth ± 2 years), sex, index date, and duration of history in the database prior to the index date (±2 years). Additionally, controls were matched to cases on underlying schizophrenia, affective disorders, or dementia. If patients had diagnoses for more than one of these disorders prior to the index date, they were matched according to the following order based on smallest chance of remission/recovery and strongest association with seizures: (1) dementia, (2) schizophrenia, and (3) affective disorders [22, 27, 28].
Case and control exposure to antipsychotic drugs was classified according to the timing of antipsychotic drug use prior to the index date; ‘non-users’ were those who had no antipsychotic drug prescriptions prior to the index date; ‘current users’ and ‘past users’ were those who had received the last prescription ≤90 days or >90 days prior to the index date, respectively. Additionally, current users were stratified by exposure duration (‘short-term users’ and ‘long-term users’ were those who had received the first prescription ≤90 days or >90 days prior to the index date, respectively). Because incidence rates of seizures differed significantly between patients with affective disorders and patients with dementia in the follow-up part of the study, we conducted the nested case–control analysis among cases and controls with underlying affective disorders or dementia separately (number of patients with schizophrenia was too low for a separate analysis). We evaluated individual antipsychotic drugs if there were at least five exposed subjects in each exposure level. Where possible we classified each antipsychotic drug by the dose prescribed at the index date (≤1 defined daily dose, >1 defined daily dose) [29].
2.6 Statistical Analysis
We conducted a crude person-time analysis to estimate incidence rates of seizures, with 95 % confidence intervals (CIs), for the following exposures: any mono use, mono use of different antipsychotic drug subclasses, mono use of individual drugs, past use of antipsychotic drugs, and no use of antipsychotic drugs. Incidence rates were estimated among the whole cohort of patients with schizophrenia, affective disorders, or dementia, and separately among patients who had diagnoses of affective disorders or dementia only.
In the nested case–control analysis, we used SAS statistical software (version 9.4; SAS Institute, Cary, NC, USA) to conduct conditional logistic regression analyses. Relative risk estimates of antipsychotic drug use among cases and controls were calculated as odds ratios with 95 % CIs. Our reference group comprised patients with no antipsychotic drug treatment prior to the index date. Based on preexisting literature, we a priori adjusted multivariate models for alcohol consumption (none, 1–14 units/week, >14 units/week, unknown), compulsive disorders, Parkinson’s disease, stroke and/or transient ischemic attack (TIA), suicidal ideation/attempts, and current or past use of antidepressants, anticonvulsants, opioids, benzodiazepines, or antipsychotic drugs other than those studied [2, 27, 30, 31]. We tested as additional potential confounders a history of cardiovascular diseases, diabetes mellitus, hypertension, hyperlipidemia, hypothyroidism, sleep disorders, renal diseases, or migraine, and concurrent use of antibiotics, anti-malarial drugs, stimulants, and immunosuppressant or antiarrhythmic drugs, but we did not include them in the final model as they did not alter the risk estimates by more than 5 %.
To assess potential effect modification we stratified cases and controls by history of stroke and/or TIA, or of underlying disorders (affective disorders, dementia) and age (18–59 years, 60–90 years).
In sensitivity analyses, we explored whether risk estimates of seizures associated with the use of antipsychotic drug subclasses differed if the reference group included non-users of the respective antipsychotic drug subclass (who potentially used other subclasses) prior to the index date. Additionally, we excluded users of prochlorperazine from the exposed group, to explore whether the risk of seizures associated with the use of medium-to-high potency first-generation antipsychotic drugs changed because this drug is often used to treat nausea rather than psychotic symptoms.
3 Results
We identified 60,121 patients who met our inclusion criteria, of whom 79.6 % were diagnosed with affective disorders, 11.2 % with dementia, 3.0 % with schizophrenia, and 6.2 % with more than one disorder. Of these patients, 583 had a first-time diagnosis of seizure during follow-up. We also conducted a nested case–control analysis of 334 cases and 1336 controls, all of whom had an affective disorder, and 202 cases and 773 controls, all of whom had dementia. Mean age (±standard deviation) at the index date of patients with affective disorders or dementia was 47.7 (±18.5) years and 76.7 (±8.1) years, respectively.
3.1 Incidence Rates
Among the entire study population, the estimated incidence rates of seizures per 10,000 person-years (PYs) were 38.0 (95 % CI 31.1–44.9), 11.7 (95 % CI 10.0–13.4), and 12.4 (95 % CI 10.9–13.8) in current mono users, non-users, or past users of antipsychotic drugs, respectively (Table 1). The highest incidence rate of seizures was among users of medium-to-high potency first-generation drugs (59.1 per 10,000 person-years [95 % CI 40.1–78.2]), and lowest for users of the second-generation drugs amisulpride, aripiprazole, risperidone, or sulpiride (24.1 per 10,000 person-years [95 % CI 13.2–34.9]). Among individual drugs, use of haloperidol was associated with the highest incidence rate of seizures (115.4 per 10,000 person-years [95 % CI 50.1–180.7]). Incidence rates of seizures were significantly higher in patients with dementia than in patients with affective disorders, irrespective of antipsychotic drug treatment (Table 1). Incidence rates of seizures were similar in non-use and past use of antipsychotic drugs among patients with affective disorders, while in patients with dementia, past use of antipsychotic drugs was associated with significantly higher incidence rate of seizures than non-use.
3.2 Nested Case–control Analysis
In the nested case–control analysis, history of suicide attempt and/or suicidal ideation, migraine, or stroke/TIA, and concurrent use of opioids, benzodiazepines, anticonvulsants, or antidepressants were associated with an increased risk of seizures in patients with affective disorders (Table 2). History of stroke/TIA and concurrent use of benzodiazepines were associated with an increased risk of seizures in patients with dementia.
Current use of first-generation medium-to-high potency antipsychotic drugs (adjusted odds ratio 2.51 [95 % CI 1.51–4.18]) was associated with an increased risk of seizures compared with non-use of antipsychotic drugs in patients with affective disorders (Table 3). In these patients, current use of all other antipsychotic drug subclasses was not associated with seizures. In patients with dementia, current and past use of all first-generation antipsychotic drugs and olanzapine and quetiapine, was associated with an increased risk of seizures compared with non-use of antipsychotic drugs, while use of amisulpride, aripiprazole, risperidone, or sulpiride was not associated with seizures (Table 3). Owing to the small numbers of patients with current antipsychotic drug use, we could not calculate meaningful odds ratios for current use stratified by exposure duration.
Table ESM 1 displays odds ratios of seizures associated with the most frequently prescribed, individual antipsychotic drugs in patients with affective disorders or dementia, respectively. Current use of prochlorperazine was associated with an increased risk of seizures compared with non-use of antipsychotic drugs in patients with affective disorders (Table ESM 1). Current use of all individual antipsychotic drugs except risperidone and past use of all individual antipsychotic drugs were associated with increased risks of seizures compared with non-use of antipsychotic drugs in patients with dementia (Table ESM 1). Most users of antipsychotic drugs were prescribed doses that were lower than or equal to the defined daily dose at the index date (88.0 % of olanzapine or quetiapine users, 92.4 % of amisulpride, aripiprazole, risperidone, or sulpiride users, 97.8 % of low-to-medium potency first-generation antipsychotic drug users, and 100 % of medium-to-high potency first-generation antipsychotic drug users). Thus, we were unable to assess a potential dose–effect relationship of antipsychotic drug use in relation to the risk of seizures.
Because of the low numbers of patients with a history of stroke/TIA, potential effect modification by indication (affective disorders or dementia) could not be assessed in this subgroup. However, in the whole study population, the effects of antipsychotic drug use on the risk of seizures did not differ materially between those with and without a history of stroke/TIA (Table ESM 2).
Current use of medium-to-high potency first-generation antipsychotic drugs was associated with increased risks of seizures in all age groups (adjusted odds ratios 2.20 [95 % CI 1.18–4.09] and 4.97 [95 % CI 1.68–14.67] in patients aged less than 60 years or 60 years or over, respectively) [data not shown]. Most patients with dementia (94.6 %) were aged 60 years or over while 1233 (73.2 %) patients with affective disorders were aged less than 60 years, and 447 (26.8 %) were aged 60 years or over at the index date.
When the reference group was defined as non-use of the respective subclass of antipsychotic drugs, the results were closely similar (Table ESM 3) to those of the main analysis (Table 3). Excluding prochlorperazine from the subclass of first-generation medium-to-high potency antipsychotic drugs yielded a higher odds ratio of seizures in patients with affective disorders (adjusted odds ratio 12.56 [95 % CI 3.31–47.67]) compared with the estimate from the main analysis (Table 3), although the difference was not statistically significant.
4 Discussion
In this observational study using data from a UK based primary care database, we observed that current mono users of antipsychotic drugs had two- to threefold higher risks of seizures compared with non-users of antipsychotic drugs. Current users of medium-to-high potency first-generation antipsychotic drugs had significantly higher risks of seizures than current users of the second-generation antipsychotic drugs amisulpride, aripiprazole, risperidone, or sulpiride. Irrespective of antipsychotic drug use, patients with dementia experienced seizures more frequently than patients with affective disorders. The number of patients with schizophrenia was too limited to estimate separate incidence rates for these patients.
After adjusting for potential confounding and stratifying by underlying affective disorders or dementia, we observed that current use of medium-to-high potency first-generation antipsychotic drugs was associated with a more than twofold increased risk of seizures compared with non-use of antipsychotic drugs in patients with affective disorders. In these patients, current use of all other antipsychotic drugs was not associated with seizures. In patients with dementia, current use of all first-generation antipsychotic drugs and the second generation antipsychotic drugs olanzapine and quetiapine, was associated with an increased risk of seizures compared with non-use of antipsychotic drugs. This effect was also seen in past users of antipsychotic drugs in those with dementia, suggesting that the association may be because of dementia progression or severity, leading to antipsychotic drug use, rather than a causal effect of antipsychotic drugs. Notably, current use of amisulpride, aripiprazole, risperidone, or sulpiride was not associated with the occurrence of seizures in patients with dementia.
Our results do not corroborate existing evidence for a higher seizure risk in association with strongly sedating low-potency first-generation drugs (especially aliphatic phenothiazines) compared with less sedating high-potency first-generation drugs [2, 3, 5, 8, 31, 32]. However, this evidence is based mainly on one observational study conducted between 1960 and 1965, which reported a higher seizure incidence among phenothiazine (especially chlorpromazine) users compared with non-users [6]. As the group of non-users in that study comprised patients who used other first-generation antipsychotic drugs as well as those who did not use any antipsychotic drugs, a comparison of seizure risk associated with different first-generation antipsychotic drugs was not possible [6]. Additionally, in contrast to our study, patients with major direct risk factors for seizures were not excluded from this study [6]. We observed slightly higher incidence rates of seizures in users of medium-to-high potency first-generation antipsychotic drugs (mainly haloperidol and prochlorperazine) than in users of low-to-medium potency first-generation antipsychotic drugs (mainly flupenthixol, chlorpromazine, and promazine), although differences did not reach statistical significance. After adjusting for potential confounding, current use of medium-to-high potency, but not low-to-medium potency first-generation antipsychotic drugs, was associated with an increased risk of seizures compared with non-use of antipsychotic drugs in patients with affective disorders.
In contrast to the available literature that describes a higher risk of seizures associated with clozapine, olanzapine, and quetiapine (three structurally related antipsychotic drugs) compared with other second-generation antipsychotic drugs [9, 11, 12], our rates of seizures were not significantly different between users of olanzapine or quetiapine and users of other second-generation antipsychotic drugs. However, we could not investigate the risk of seizures associated with clozapine use, the second-generation antipsychotic drug reported to be most strongly associated with seizures [7, 9, 10] because treatment with clozapine in the UK takes place almost exclusively in secondary care and there was little use captured in the CPRD. Yet, among patients with dementia, we did observe an increased risk of seizure with current use of olanzapine or quetiapine compared with non-use. This effect was not present for current use of other second-generation antipsychotic drugs.
To our knowledge, no other study to date has investigated the risk of first-time seizures associated with use of antipsychotic drugs in such a large population of patients over such a long observation period. The available studies on the risk of seizures in association with antipsychotic drugs had no control group and were prone to bias and confounding [6, 11, 12], or had only a very small control group [9]. Moreover, these studies did not assess the risk of seizures in association with antipsychotic drugs separately for each underlying disorder.
In this study, we observed that patients with dementia were at a significantly increased risk of seizures compared with patients with affective disorders, irrespective of whether they used antipsychotic drugs or not. This finding is consistent with the results of another observational study from our group based on data from the CPRD that reported that dementia is a major risk factor for developing seizures [22]. Notably, current use of drugs of the subclass amisulpride, aripiprazole, risperidone, and sulpiride (especially the single drug risperidone), was not associated with the development of seizures in patients with dementia. Thus, with regard to seizure risk, our results support that risperidone has to date been the only antipsychotic drug in the UK licensed for short-term use in patients with dementia [33].
In this study, we aimed to minimize confounding by excluding patients with major risk factors for seizures. Additionally, we controlled for further confounding by matching controls to cases on age, sex, calendar time, and underlying disorder, which presumably led to the prescription of antipsychotic drugs. Last, we adjusted our analyses for additional potential confounders such as alcohol consumption, relevant comorbidities, or concomitantly used drugs. However, there may still be some residual confounding by unmeasured risk factors for seizures such as disease severity. Non-users of antipsychotic drugs could potentially have been at a less severe disease stage than current users of antipsychotic drugs. However, the sensitivity analysis in which we redefined the reference group as non-users of the respective drug subclass did not yield considerably different results than the main analysis.
We were not able to investigate a potential relationship between antipsychotic drug dose and the development of seizures, although the risk of seizures in association with antipsychotic drugs has been reported to be dose dependent [6, 10, 34]. However, antipsychotic drugs were prescribed almost exclusively in doses equal to or lower than the defined daily dose, irrespective of the drug subclass. Therefore, the increased risk of seizures associated with current use of medium-to-high potency antipsychotic drugs in patients with affective disorders could not be because of higher doses prescribed in this subclass compared with other subclasses. Because of limited numbers of current users of antipsychotic drugs, we could not assess whether seizure risk was dependent on exposure duration. Additionally, some antipsychotic drugs, especially prochlorperazine, could have been prescribed for nausea rather than psychosis. However, excluding prochlorperazine users from the group of medium-to-high potency antipsychotic drug users led to an even higher risk estimate of seizures than the main analysis.
There may have been some outcome misclassification in this study, either if the seizure was missed by the GP or by the patient, or if a patient had a medical condition other than a seizure that was misreported as a seizure. However, potential misclassification of seizures was most likely not related to the antipsychotic drug used. Additionally, our algorithm to define a first-time seizure was developed by reviewing a random sample of 120 patient profiles, in which we assessed the likelihood of a seizure taking into account codes of antiepileptic drug prescriptions or codes of suspected seizures preceding the actual seizure code. Thus, any misclassification was unlikely to materially affect our results. In addition, the validity of affective disorders diagnoses has not formally been investigated in the CPRD, but the database has proven to be of high validity with regard to many acute or chronic diseases in numerous previous studies [17, 18].
5 Conclusion
We observed that the risk of seizures associated with use of antipsychotic drugs strongly differed according to the underlying disorder of the patient: It was considerably higher in patients with dementia than in patients with affective disorders, irrespective of antipsychotic drug use. In patients with affective disorders, current use of medium-to-high potency first-generation antipsychotic drugs was associated with a more than twofold increased risk of seizures compared with non-use of antipsychotic drugs, while current use of other antipsychotic drugs was not associated with seizures. In patients with dementia, current use of amisulpride, aripiprazole, risperidone, and sulpiride, was not associated with an altered risk of seizures, while current use of all other antipsychotic drugs was associated with an increased risk of seizures, compared with non-use of antipsychotic drugs.
References
Meyer JM. Pharmacotherapy of psychosis and mania. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s pharmacological basis of therapeutics. 12th ed. New York: McGrawHill Medical; 2011. p. 417–51.
Block F, Dafotakis M. Drug-induced seizures. Fortschr Neurol Psychiatr. 2013;81:28–34. doi:10.1055/s-0032-1325332.
Pisani F, Oteri G, Costa C, Di Raimondo G, Di Perri R. Effects of psychotropic drugs on seizure threshold. Drug Saf. 2002;25:91–110.
Ruffmann C, Bogliun G, Beghi E. Epileptogenic drugs: a systematic review. Expert Rev Neurother. 2006;6:575–89. doi:10.1586/14737175.6.4.575.
Itil TM, Soldatos C. Epileptogenic side effects of psychotropic drugs: practical recommendations. JAMA. 1980;244:1460–3.
Logothetis J. Spontaneous epileptic seizures and electroencephalographic changes in the course of phenothiazine therapy. Neurology. 1967;17:869–77.
Fitzsimons J, Berk M, Lambert T, Bourin M, Dodd S. A review of clozapine safety. Expert Opin Drug Saf. 2005;4:731–44. doi:10.1517/14740338.4.4.731.
Hedges D, Jeppson K, Whitehead P. Antipsychotic medication and seizures: a review. Drugs Today (Barc). 2003;39:551–7.
Alper K, Schwartz KA, Kolts RL, Khan A. Seizure incidence in psychopharmacological clinical trials: an analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biol Psychiatry. 2007;62:345–54. doi:10.1016/j.biopsych.2006.09.023.
Williams AM, Park SH. Seizure associated with clozapine: incidence, etiology, and management. CNS Drugs. 2015;29:101–11. doi:10.1007/s40263-014-0222-y.
Kumlien E, Lundberg PO. Seizure risk associated with neuroactive drugs: data from the WHO adverse drug reactions database. Seizure. 2010;19:69–73. doi:10.1016/j.seizure.2009.11.005.
Lertxundi U, Hernandez R, Medrano J, Domingo-Echaburu S, García M, Aguirre C. Antipsychotics and seizures: higher risk with atypicals? Seizure. 2013;22:141–3. doi:10.1016/j.seizure.2012.10.009.
Jick H. A database worth saving. Lancet. 1997;350:1045–6. doi:10.1016/S0140-6736(05)70451-7.
Lawson DH, Sherman V, Hollowell J. The general practice research database: Scientific and Ethical Advisory Group. QJM. 1998;91:445–52.
Wood L, Martinez C. The general practice research database: role in pharmacovigilance. Drug Saf. 2004;27:871–81.
The Clinical Practice Research Datalink. http://www.cprd.com. Accessed 15 July 2015.
Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the general practice research database: a systematic review. Br J Clin Pharmacol. 2010;69:4–14. doi:10.1111/j.1365-2125.2009.03537.x.
Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the general practice research database: a systematic review. Br J Gen Pract. 2010;60:e128–36. doi:10.3399/bjgp10X483562.
Ishiguro C, Wang X, Li L, Jick S. Antipsychotic drugs and risk of idiopathic venous thromboembolism: a nested case–control study using the CPRD. Pharmacoepidemiol Drug Saf. 2014;23:1168–75. doi:10.1002/pds.3699.
Brauer R, Smeeth L, Anaya-Izquierdo K, Timmis A, Denaxas SC, Farrington CP, et al. Antipsychotic drugs and risks of myocardial infarction: a self-controlled case series study. Eur Heart J. 2015;36(16):984–92. doi:10.1093/eurheartj/ehu263.
Laredo L, Vargas E, Blasco AJ, Aguilar MD, Moreno A, Portolés A. Risk of cerebrovascular accident associated with use of antipsychotics: population-based case–control study. J Am Geriatr Soc. 2011;59:1182–7. doi:10.1111/j.1532-5415.2011.03479.x.
Imfeld P, Bodmer M, Schuerch M, Jick SS, Meier CR. Seizures in patients with Alzheimer’s disease or vascular dementia: a population-based nested case–control analysis. Epilepsia. 2013;54:700–7. doi:10.1111/epi.12045.
Martinez C, Sullivan T, Hauser WA. Prevalence of acute repetitive seizures (ARS) in the United Kingdom. Epilepsy Res. 2009;87:137–43. doi:10.1016/j.eplepsyres.2009.08.006.
Gasse C, Derby L, Vasilakis-Scaramozza C, Jick H. Incidence of first-time idiopathic seizures in users of tramadol. Pharmacotherapy. 2000;20:629–34.
Jick SS, Jick H, Knauss TA, Dean AD. Antidepressants and convulsions. J Clin Psychopharmacol. 1992;12:241–5.
Nasrallah H, Tandon R. Classic antipsychotic medications. In: Schatzberg A, Nemeroff C (eds) The American psychiatric publishing textbook of psychopharmacology, 4th edn. Arlington; 2009. p. 533–54.
Hesdorffer DC, Ishihara L, Mynepalli L, Webb DJ, Weil J, Hauser WA. Epilepsy, suicidality, and psychiatric disorders: a bidirectional association. Ann Neurol. 2012;72:184–91. doi:10.1002/ana.23601.
Hyde TM, Weinberger DR. Seizures and schizophrenia. Schizophr Bull. 1997;23:611–22.
World Health Organization. ATC/DDD Index 2015. 2015. http://www.whocc.no/atc_ddd_index/. Accessed 15 July 2015.
Wilden JA, Cohen-Gadol AA. Evaluation of first nonfebrile seizures. Am Fam Physician. 2012;86:334–40.
Lee KC, Finley PR, Alldredge BK. Risk of seizures associated with psychotropic medications: emphasis on new drugs and new findings. Expert Opin Drug Saf. 2003;2:233–47.
Koch-Stoecker S. Antipsychotic drugs and epilepsy: indications and treatment guidelines. Epilepsia. 2002;43(Suppl 2):19–24.
National Institute for Health and Care Excellence. Low-dose antipsychotics in people with dementia. 2015. http://www.nice.org.uk/advice/ktt7/resources/non-guidance-lowdose-antipsychotics-in-people-with-dementia-pdf. Accessed 15 July 2015.
Devinsky O, Honigfeld G, Patin J. Clozapine-related seizures. Neurology. 1991;41:369–71.
Acknowledgments
We thank Pascal Egger for the help with the programming of this study.
Author contributions
Bloechliger M: study conception and design, statistical analysis and interpretation of data, drafting the manuscript. Rüegg S: study conception and design, editing the manuscript. Jick SS: acquisition of data, editing the manuscript. Meier CR: study conception and design, acquisition of data, analysis and interpretation of data, editing the manuscript. Bodmer M: study conception and design, analysis and interpretation of data, editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Independent Scientific Advisory Committee for Medicines and Healthcare products Regulatory Agency research. For this type of study formal consent is not required.
Conflicts of interest
Ms. Bloechliger, Dr. Rüegg, Prof. Jick, Prof. Meier, and Dr. Bodmer declare that they have no conflict of interest.
Funding
This study was not funded.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Rights and permissions
About this article
Cite this article
Bloechliger, M., Rüegg, S., Jick, S.S. et al. Antipsychotic Drug Use and the Risk of Seizures: Follow-up Study with a Nested Case–Control Analysis. CNS Drugs 29, 591–603 (2015). https://doi.org/10.1007/s40263-015-0262-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-015-0262-y