Abstract
Over the past two decades there has been increasing interest in including patients’ self-reports in the management of their illness. Among the many reasons for such recent interest has been a rising consumer movement over the past few decades, which has led patients, their caregivers and their families to press for more meaningful sharing with physicians in the clinical decision-making process, with the clear expectations of better therapies and improved outcomes. Patients as consumers of services, their views, attitudes towards healthcare, as well as their level of satisfaction with care, have become increasingly recognized. The recent interest by the US Food and Drug Administration (FDA), as well as other regulatory agencies, in patient-reported outcomes (PROs) in the process of developing and testing new antipsychotics, has also added more impetus. It is clear that including patients in the decision-making process about the management of their psychiatric conditions also broadens the concept of ‘recovery’, by empowering patients to be active participants and gives a clear message that successful treatment in schizophrenia is more than a symptomatic improvement, but also includes improved functional status. Additionally, the recent interest in personalized medicine puts the patient in the centre of such development. Since 2004, when we published our review about the impact of new antipsychotics on quality of life in CNS Drugs, a number of newer antipsychotics have been introduced and include ziprasidone, aripiprazole, paliperidone, asenapine, iloperidone and lurasidone. The current review is based on 31 selected publications that cover the years 2004–2012, and deals with the impact of such newer antipsychotics on specific domains of PROs, such as subjective tolerability, quality of life, medication preference, satisfaction and social functioning. Most of the available data deal with ziprasidone, aripiprazole and paliperidone. Though the great majority of the studies indicate the newer antipsychotics have favourably impacted on aspects of PROs, such a conclusion can only be considered a trend due to the many design and methodological limitations of many of these studies. It is interesting to note, as the field awaits more rigorous studies, that there seems to be a unifying core that exists among the various subjective outcomes and that tends to generalize from one subjective outcome to other subjective outcomes. The patient who experiences good subjective tolerability to medications tends generally to be more satisfied and has a strong medication preference. The identification of such a unifying core can prove helpful, not only in the development of appropriate scales, but also in informing and guiding the process of development of new antipsychotics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In the majority of psychiatric disorders, particularly in the absence of a clear etiological and pathological basis, we have to rely mostly, in both diagnosis and management, on what our patients tell us. Schizophrenia is no exception, except that it poses a number of challenges related to the nature of the illness and its impact on several important mental functions that include thinking, affect and cognition. In essence, psychiatrists rely on prescribing medications and assessing outcomes in response to those medications on what our patients voluntarily report, or in response to the physicians’ probing questions. Why then has there been a recent increase in interest in including patients’ reports in the management of their psychiatric conditions? A number of reasons that have evolved over the past two to three decades have contributed to such a rise in interest:
-
the rising consumer movement over the past few decades has led patients, their caregivers and their families to press for more meaningful sharing with physicians in the clinical decision-making process, with the clear expectations of better therapies and improved outcomes,
-
patients are no longer being viewed as passive recipients of treatment, but have become active participants in their own care,
-
as consumers of clinical services, their views, attitudes towards care and health, and illness, in particular, as well as their level of satisfaction with care, has become exceedingly important,
-
the recent expression of interest by the US Food and Drug Administration (FDA) and other regulatory agencies in patient-reported outcomes (PROs) in the process of developing and testing new antipsychotics have added more impetus,
-
the continuing increase in health costs, as well as the introduction of an increasing number of new and relatively expensive medications, have added a pharmacoeconomic perspective,
-
such concerns have led to more recognition of patients’ subjective responses and their preferences as a guide to improving outcomes, and as a handle on costs, particularly in the case of ‘me too’ medications,
-
including patients in the decision-making process about their management, broadens the concept of ‘recovery’ by empowering patients to be active participants in their recovery process and gives a clear message that successful treatment in schizophrenia is more than symptomatic improvement, but also includes improved functional status,
-
the recent interest in personalized medicine puts the patient in the centre of such developments.
What then is the difference between what has traditionally been happening in psychiatry, in contrast to what is meant these days by PROs? Recently, the FDA defined PROs as “any report coming directly from patients about their health condition and its treatment” [1]. In the case of clinical trials, the definition relates to a clinical trial participant. In essence, a ‘patient-reported outcome’ is based on a patient’s perception of a disease and its treatment, as expressed by the patient without interpretation by a clinician or research investigator.
2 Challenges in Implementation of Patient-Reported Outcomes (PROs) in Studies
2.1 Specific Issues Related to Schizophrenia
Schizophrenia is a long-term recurring chronic and disabling condition that can impact important mental functions, as well as general behaviour and the ability to have a productive role. Symptoms include a vast array of positive symptoms such as hallucinations, delusions and disturbed thinking. It also includes negative and deficit symptoms, as patients are frequently socially withdrawn and hedonic, lacking spontaneity and initiative. Cognitively, patients with schizophrenia can experience a lack of insight and impaired judgement. Such a wide array of symptoms has contributed concerns and doubts about whether patients with schizophrenia are capable of reliably assessing their inner feelings, and accurately expressing their preferences and level of satisfaction. Such a conclusion has been supported by a number of researchers [2–5]. Yet, the subjective/objective dichotomy continues to be a controversial subject of debate [3]. In several definitive and ground-breaking neuroimaging studies, it was demonstrated that what patients with schizophrenia express as their subjective responses to antipsychotic medications, is in reality well correlated with observable neurobiological changes in dopamine functioning in the nigrostriatal area of the brain [6–9]. In other words, though subjective responses may be modified by other factors, they are the expression of a real neurochemical change in the brain and not a random reaction.
2.2 Issues Related to the Role of Antipsychotic Medications in Schizophrenia
In a previous publication in this journal [10], we identified the aim of antipsychotic medications in the treatment of schizophrenia as including symptomatic improvement, low or no side effects, prevention of relapse, improved quality of life (QOL) and functional status, as well as cost effectiveness. The introduction of chlorpromazine and the subsequent development of a broad range of similar typical antipsychotics provided for the first time specific agents that proved effective in symptomatic improvement. Unfortunately, the broad range of side effects, including the inconveniencing extrapyramidal symptoms, as well as irreversible neurological symptoms, have limited the impact of the typical antipsychotics and, generally, impacted negatively on functional issues, as well as QOL [11]. Additionally, all available antipsychotics do not impact equally on all psychopathological domains of the illness. In 2004, we contributed a review in this journal about the impact of atypical antipsychotics on the QOL of patients with schizophrenia, focusing on the available antipsychotics at that time, mostly risperidone, olanzapine, quetiapine and clozapine [12]. Since then, other antipsychotics have been introduced and approved for use, including, in the order of their approval, ziprasidone, aripiprazole, paliperidone, asenapine, iloperidone and lurasidone. Though there have been rather extensive publications and reviews about such newer antipsychotics in terms of efficacy and side effects [13–17], there have been many fewer publications about their impact on important aspects of PROs that matter most to the patients, such as QOL, subjective tolerability, satisfaction, medication preferences, and social functioning, which are the subject of this review. In spite of the paucity of reliable data from well designed studies, it is hoped that this review can increase the interest of researchers, clinicians and policy makers in enhancing and improving clinical and research approaches in such important aspects of psychiatric care.
2.3 Challenges in the Design and Implementation of PROs
Issues such as the purpose of the study, the outcomes tested, and the measurement tools need to be clearly defined:
-
1.
It is important to define the purpose of PRO measurement and whether it is for clinical purposes or as part of a clinical trial protocol; each one has a particular focus. PROs need to be integrated in patient care. Patients’ characteristics, as well as the stage of the illness, have to be defined. Outcomes in the acute or sub-acute stages are different than outcome expectations in the stable chronic phase. Clinical trials for the purpose of approval for new antipsychotics, or for comparison of new versus standard antipsychotics, or among the new antipsychotics themselves, may require different populations. Not only efficacy, but also effectiveness, as well as relapse prevention, are the major outcomes of such studies.
-
2.
The most common outcomes in schizophrenia that need to be clearly defined a priori include the following:
-
self-reported QOL,
-
subjective tolerability of medications,
-
preferences, values and attitudes towards health and illness,
-
satisfaction with medications and care, in general.
-
-
3.
It is important to define the appropriate measurement tools, which are not only reliable and validated, but possess well known psychometrics. Measurement tools have to be appropriate to the population, which, generally, in schizophrenia may have a varying degree of cognitive disability. The measurement tools have to be appropriate to the stage of the illness and, preferably, based on a theoretical and conceptual framework supporting the clinical domain chosen.
Unfortunately, a large number of available scales have several shortcomings and limitations, and may prove not optimal or practical for the intended purpose. An example is the frequent use of the Quality of Life Scale (QLS) in several studies included in this review as a QOL scale. Though this scale has its historical merits as a tool for assessment of deficit state, only two of its factors qualify as QOL measures. The scale requires specially trained interviewers. Indeed, most of the available scales also suffer from floor and ceiling effects. In a recent review, we strongly argued and recommended that development of new scales has to make use of new approaches based on item response theory, item banks and computer adaptive testing [18]. This approach can also provide a standardized common metric that allows for meaningful comparison of data. We also argued that scale development needs to be based on an appropriate conceptual model or clinical framework [19].
Measurement tools can be either generic or specific to schizophrenia. They can be unidimensional or, most preferably, multidimensional.
3 PROs and the Impact of Newer Antipsychotics
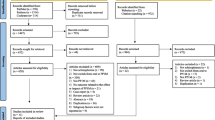
For the purpose of this review, we searched the literature using MEDLINE, PubMed and manual searches. Our search criteria included studies related to one or more of the newer atypicals, information about the source of funding (if any), characterization of the population used, as well as identification of the measuring tools for PROs. Thirty-one reports published in English between 2004 and 2012 were selected and provided the basis for information included in this review [20–50].
Of all PROs, QOL has been the most frequent domain investigated and reported. Overall, there is a noticeable paucity in publications about the impact of newer atypical antipsychotics, particularly for the most recently introduced: iloperidone, asenapine and lurasidone.
4 Quality of Life and the Newer Antipsychotics
Over the past three decades, QOL has emerged as the new ideal for modern medicine. Improved QOL is what the patient and the physician aspires to achieve, as a result of medical intervention, including antipsychotic treatment in schizophrenia. QOL is complex and, as we argued in a recent review, has to be approached as a biopsychosocial construct [18]. Antipsychotics, by themselves, cannot directly influence QOL, but can certainly make it possible for patients with schizophrenia to benefit from other psychosocial, vocational and economic interventions, as a result of improvement in symptomatology, as well as fewer or no inconveniencing side effects. The subjective nature of the construct of QOL, puts patients’ self-reports at the centre of any definition of QOL.
A few years ago, we proposed a conceptual model for QOL specifically related to the role of medications [19]. Such a model integrates the impact of symptomatology, medication effects and side effects, as well as psychosocial performance in a circular model, that emphasizes the interactive nature of these factors and their impact on each other. The purpose of such a model has been to facilitate the design and measurement of QOL in clinical trials of antipsychotics. Unfortunately, in reviewing clinical trials of the newer antipsychotics and their impact on self-reported QOL, similar to the earlier atypical antipsychotics, there is a paucity of controlled and appropriately designed clinical trials (Table 1).
The majority of the reports so far have dealt with the impact of ziprasidone [20, 22, 24, 28, 32, 37, 40, 42, 47, 50], aripiprazole [25, 26, 30, 31, 33, 35, 36, 41, 43, 45, 46] and, to a lesser extent, paliperidone [21, 23, 29, 30]. Much less is known about the impact of asenapine [27, 35], iloperidone and lurasidone, likely as a result of being recently approved.
Unfortunately, most of the studies reviewed suffered from serious shortcomings. Many studies are open-label uncontrolled, and frequently of short duration. Measurement tools frequently are not adequate or sensitive enough to pick up the relatively small changes expected in a relatively short clinical trial. Of note, one of the frequently used measurement tools has been the QLS, which has been criticized by some as not being an appropriate PRO measure. Though it may not be the most appropriate QOL scale, it includes a combination of patient-reported subjective experiences, as well as an interviewer-rated component. Most of the studies are supported in total or partly by the manufacturer and, generally, the few large efficacy studies to have included some aspects of patient-reported assessments seem to have included such assessments as an after-thought.
Balancing all the information available so far about the impact of newer atypical antipsychotics on QOL, it is clear that the field requires more rigorous, well designed and purpose-specific studies. The available evidence can only suggest a trend towards improvement in QOL with ziprasidone, aripiprazole and, possibly, paliperidone. For the other newer atypicals—asenapine, iloperidone and lurasidone—one cannot yet make any reliable inferences. The Canadian Drug Expert Committee (CDEC) that recently approved asenapine for use in Canada included inferences in their final report to QOL assessment data from a number of manufacturers’ submitted studies using QLS, the Quality of Life Enjoyment and Satisfaction (Q-LES-12), and the Short Form Health Survey (SF-12), comparing asenapine with olanzapine or placebo, with the conclusion: no notable between-treatment differences in QOL. We are not aware of whether such data are under publication. Additionally, in two recent asenapine studies, one reported improvement in QOL [33] and the other had equivocal results [26]. For iloperidone and lurasidone, no reliable data are yet available.
4.1 Subjective Tolerability and the Newer Atypical Antipsychotics
Negative subjective responses to antipsychotic medication have been well recognized since shortly after the introduction of the first antipsychotic medication chlorpromazine in the early 1950s. Patients frequently reported feeling like zombies, dysphoric, unable to think straight and, generally, developed a dislike of medications. A number of clinical studies consistently confirmed such observations; however, the impact of these early observations has been somewhat lost, as the phenomenon was invariably labelled as behavioural toxicity, akinetic depression, neuroleptic-induced dysphoria, negative subjective responses, etc. [51]. It was not until the late 1970s and early 1980s that the construct of subjective response to antipsychotics was clarified after two groups in the USA and Canada published a series of focused clinical studies that defined the concept of subjective responses and also drew attention to its serious consequences, in terms of medication adherence behaviour and outcome [52–57]. The development of the Drug Attitude Inventory (DAI) as a reliable and validated measure for subjective responses to antipsychotics expanded the field and provided a tool to quantify such responses [53]. Since then, the DAI has continued to be the gold standard for measuring subjective responses and has also become the most frequently used tool in clinical trials of antipsychotic medications. Other measuring tools were introduced afterwards, modeled on the original DAI, and include the Subjective Well-being on Neuroleptics (SWN) [58], and the Personal Evaluation of Transition in Treatment (PETiT) [59], which both join the DAI as the common instruments for evaluation of subjective tolerability of antipsychotics. Though dopamine has always been suspected of being implicated in the emergence of dysphoric responses, based on similar observations in other conditions, such as Tourette syndrome, which also requires treatment with antipsychotics, it was not until the development of neuroimaging techniques that it became possible to study the neurobiology of subjective tolerability. One of the earliest studies was our dopamine D2 depletion SPECT study, experimentally manipulating dopamine in the brain using alpha para-amino tyrosine [6]. Such an approach allowed us for the first time to report a negative correlation between dysphoric responses and the dopamine binding ratio in the nigrostriatal area. It allowed us to observe the cascade of subjective and behavioural events that follow dopamine blockade, as happens after ingestion of the antipsychotic medication. The earliest experience that follows within hours has been a change in subjective feelings, followed by affective, motor and cognitive changes [8]. In essence, what was initially thought of as simply a dysphoric affective reaction to antipsychotic medications proved to be more complex and also included motor and cognitive changes. One of the implications of that study was the better understanding of the variability in experiencing such dysphoric responses, depending on the dopamine-blocking effects of variable antipsychotics. Several other neuroimaging studies have confirmed the earlier observations and have led to more recognition of the role of subjective tolerability to medications in achieving better outcomes [7–9].
Table 1 includes a number of the studies with individual newer antipsychotics that included a measure of subjective tolerability, mostly the DAI, SWN and the PETiT [20, 22, 24, 27, 32, 34, 38, 40]. As with QOL studies, the majority of subjective tolerability studies are limited by similar significant methodological limitations. However, at this point, one can conclude that there is a trend towards improved subjective tolerability with the newer antipsychotics, mostly with ziprasidone and more so with aripiprazole. For paliperidone [23] and asenapine [27], the favourable impact can only be considered as preliminary and awaits further studies. Similarly, recent unpublished data analysis from a switch long-term outpatient extension study with lurasidone indicates a favourable subjective tolerability, as measured by the PETiT (unpublished data).
4.2 Medication Preferences and the Newer Antipsychotics
Medication preference is a rather complex construct that incorporates not only acceptance, but also ability to make decisions about choices, and, as such, requires some affective and cognitive intactness. Preferences do not happen in a vacuum, but draw on a number of factors, including the experience of being on medication and the response to it, as well as previous experiences and individual expectations. Unfortunately, there is no reliable conceptual model specific to medications that can clarify the role of many factors that are inherent in the process of forming a preference.
At present, the most commonly used measuring tool is the Preference of Medication Questionnaire (POM) [60, 61].
Table 1 includes a number of the reviewed studies that included a measure of medication preference [20, 26, 31, 36, 41, 46]. Overall, as with other PROs, there are no reliable data derived from well designed head-to-head studies. It is interesting that almost all of the published studies report positive preferences for all the newer antipsychotics investigated, particularly with aripiprazole. With the methodological limitations, one can only conclude that, at present, there seems to be only a trend towards more preference for the newer antipsychotics, and, once more, more studies assigned a favourable preference for aripiprazole [26, 30, 35, 41, 46]. It is possible that the unique pharmacological properties of aripiprazole, being an agonist/antagonist, as compared with the other newer antipsychotics convey a favourable preference, possibly through its impact on subjective tolerability. It is also possible that there may be a selection bias, in terms of more aripiprazole studies including a measure for preference.
4.3 Satisfaction and the Newer Antipsychotics
Similar to many other subjective constructs, satisfaction poses significant challenges in its definition and assessment. The concept, similar to that of QOL, is too broad to be meaningful unless it is anchored to a specific purpose, such as medications or clinical care, or tenure in the community, etc. [62]. As in medication preferences, satisfaction conveys acceptance, and, as such, it can be positive or negative, depending on the individual’s final synthesis of the complex interaction between the illness, its treatment and its outcomes. The absence of a reliable conceptual model for satisfaction, specific to the use of antipsychotics, limits the understanding of the important factors that contribute to the construct and also does not allow for the development of evaluative tools grounded in valid theoretical constructs. A few years ago, we proposed a clinically intuitive conceptual model for satisfaction with medications, which defined satisfaction as the net outcome of the interaction between symptoms and their severity, side effects, subjective tolerability to medications and state of QOL [62]. Such a model awaits further confirmation, establishing its validity, as well as identifying the relative contribution of its main factors.
A number of useful scales for measuring satisfaction with medication have been introduced and include the Satisfaction with Antipsychotic Medication scale [63], the Quality of Life Enjoyment and Satisfaction scale [64], and the more recently validated Medication Satisfaction Questionnaire (MSQ) [65]. The MSQ has recently been used to measure satisfaction as a primary outcome in a blinded initiation study of paliperidone extended release in patients sub-optimally responsive to risperidone [29]. At the 2-week point, significantly more participants in the immediate initiation group reported satisfaction (67.7 %), compared with those in the delayed initiation group (45.3 %; p < 0.002). An interesting finding in that study is that reported feeling of satisfaction with medications was the earliest reported change before any symptomatic changes were demonstrated. Such an observation is consistent with our neuroimaging studies, demonstrating that changes in subjective feelings were the earliest reported change [8]. It is possible that what the MSQ measures is in large part the result of improved subjective tolerability.
Table 1 includes a brief description of the only studies that included a measure of satisfaction [25, 29, 39].
With the exception of the paliperidone study [29], which used satisfaction as primary outcome, the field appears to be deficient and awaits further development.
4.4 Social Functioning and the Newer Atypical Antipsychotics
A decline in psychosocial functioning is well recognized as a core aspect of the schizophrenia process and one that can antedate the appearance of the earliest psychotic symptoms [66]. Though there is no agreement on a general definition, it is understood that any definition of social functioning has to include the capacity of the person to function in different roles in society [66]. Such roles can be vocational, recreational or other interpersonal activities. It also includes an element of being able to derive some satisfaction in the ability of the person to fulfill a meaningful and integrative role in society. Such a broad definition poses a number of challenges, not only in its assessment, but also in understanding its components and the factors that underlie such an ability to function [67]. In schizophrenia, neurocognitive, as well as negative and deficit symptoms have been implicated as predictors and contributors of social functioning [66]. However, it is understood that both negative symptoms and cognitive deficits are considered to be somewhat independent from other positive symptoms. Yet the relationship between cognition and negative symptoms continues to be unclear. In an earlier study we demonstrated the weak relationship between subjective QOL and neurocognitive functioning [68], underscoring the possibility that subjective and objective constructs can be different, although possibly overlapping. Recently, the traditional notion that improvement in positive symptoms can enhance aspects of social functioning has been questioned [69]. It is also unclear which specific aspects of cognition have more influence on social functioning. A good deal of recent data implicate social cognition as an important mediator [70]. Additionally, other symptoms such as depression can have a more significant impact on social functioning [66]. Such complexity complicates efforts to conceptually understand the role and impact of antipsychotics, bearing in mind the limited role of antipsychotics in treating cognitive deficits, as well as improving negative symptoms [70]. In essence, any significant improvement in social functioning likely requires additional interventions, besides antipsychotic medications. Antipsychotics can play a mediating role in making it possible for the person to benefit from other rehabilitation and vocational interventions. On the other hand, a recent report that requires further confirmation suggested a possible independent effect of paliperidone extended release on social functioning beyond its effect on positive and negative symptoms of schizophrenia [71]. An important issue that is frequently overlooked in clinical trials with antipsychotics is the availability or lack of adequate individual psychosocial resources. The frequent absence of such resources serves as a barrier for adequate social functioning. Such a concern has led to the notion of measuring the person’s potential, rather than relying completely on demonstrated social activities [72].
Table 1 includes brief characteristics of the studies that included a measure of social functioning as an outcome of the newer antipsychotics [21, 30, 34, 37, 50]. Generally, as in previous outcomes, studies of social outcomes suffer from the same limitations: small, uncontrolled, mostly non-comparative open-label, frequently industry supported and of relatively short duration. The most common scale used in the reviewed studies is the Personal Social Performance scale (PSP) [73]. Another approach employed is the use of a modified Positive and Negative Symptom Scale (PANSS) Pro-Social items (active social avoidance, emotional withdrawal, passive/apathetic, social withdrawal, stereotyped thinking, hallucinatory behaviour, and suspiciousness/persecution) [50]. More recently, other studies employed further modified pro-social items (active social avoidance, emotional withdrawal, passive/apathetic, social withdrawal, difficulty in abstract thinking) [33]. As indicated in Table 1, all the reported data are mostly for ziprasidone, aripiprazole and, to a lesser extent, paliperidone, as all of these studies point to improvement in social functioning, which can only be considered at present as a trend. With lurasidone, unpublished preliminary data using the PETiT in an outpatient extension switch study that included 235 patients point to a general improvement in aspects of social functioning, as well as subjective tolerability (unpublished data).
5 Synthesis and Discussion
Recently, though there has been general recognition of the importance of including patients’ perspectives and their views about the clinical care they are receiving, including their response to medication, the published data available thus far seem to be deficient, both in quantity and quality. As a number of the newer atypical antipsychotics are relatively new, being recently introduced, most of the emphasis, so far, has been to demonstrate efficacy and side-effect profiles. Many of the studies that included a measure for PROs suffer from methodological deficiencies that make it impossible to reach a firm conclusion or make meaningful comparisons. The timeframe for measurement of certain outcomes is frequently inappropriate. A 6- to 8-week clinical trial is not going to reveal too much of significance in terms of changes in QOL or social functioning, as such parameters require longer time to change. On the other hand, other outcomes, such as subjective tolerability or medication preferences, can be elicited early in the course of treatment and can provide valuable information. Early literature has identified early subjective response, as well as early symptom changes, as valid predictors of the eventual outcome of treatment [74]. Many of the instruments used are frequently not appropriate, in terms of lack of adequate psychometrics and, also, not being applicable to different stages of the illness. Frequently, they are either too lengthy and tax the already limited cognitive ability of patients with schizophrenia, or are too short to be meaningful.
It is also clear that for certain outcomes, such as improvement in social, vocational or occupational functioning, medications alone are not enough to make a difference. Other measures, such as vocational, educational rehabilitation and economic support, as well as opportunities in real life are needed in order to achieve improvement. It also makes it difficult, particularly in multicentre clinical trials, to compare data. It is conceivable that various centres have different capabilities and resources to provide such additional rehabilitation efforts. Such concern is frequently overlooked in the design and can confound the interpretation of results.
In spite of the many limitations, the available data do demonstrate a favourable trend for the impact of newer atypical antipsychotics on a number of PROs. So far, most of the available data relate to ziprasidone, aripiprazole and, to a lesser extent, paliperidone. The field certainly requires more rigorous methodology, more appropriate measuring tools and head-to-head comparisons.
It is also important to develop theoretical and conceptual models for specific outcomes, such as medication preferences or satisfaction with medications, which can help in better understanding of the issues underpinning such constructs and also allow for better development of appropriate measures. A good example has been in the area of subjective tolerability, as there is already a reasonable conceptual model that not only allowed for better development of scales, but also defined the boundaries of such subjective constructs and expanded research interests. One of the interesting observations we are left with in conducting this review is the apparent generalizability of benefits from one subjective outcome extending to other outcomes. Patients who, for example, experience positive subjective tolerability to medications tend also to have better adherence behaviour, are likely satisfied and have positive medication preferences. One wonders whether there is a central core common to a number of these subjective outcomes. It would be exceedingly important to learn more about any such specific core that is common in all such outcomes and that makes the difference for the patient. It may be possible, then, to develop a single instrument that can tap into such a common core, or, at least, inform and guide new drug development.
As we concluded in a previous paper on QOL assessment, implementing a standard process for eliciting, in this case PROs, is expected to generate a good deal of information, which can raise a number of challenges [18]. Assessment is only the first step and needs to be followed by a process for integration of such information in care plans [75]. Additionally, there has to be a mechanism for appropriate storage of such data.
Another challenge is how to incorporate caregivers’ perspectives on care. As PROs are expected to expand over the next few years, the participation of patients and their caregivers in clinical trials and clinical trials committees are also expected to increase. This requires development of specific programmes to train patients and caregivers in how to serve as members of such committees and to become partners in care and research [76].
Finally, the phenomenal expansion of electronic technology has made it possible and feasible to illicit patient self-reports through remote electronic means, which can facilitate the process of evaluation in real time. It can enhance recruitment of adequate samples, and also reduce cost. We believe the field has to quickly move in adopting such new technology.
6 Conclusion
Though the majority of published studies about the impact of newer atypicals on PROs have been largely compromised by significant methodological limitations that preclude any firm conclusions on PROs, one can detect a favourable trend on a number of such outcomes. Most of the data relate to ziprasidone, aripiprazole and paliperidone in terms of their impact on a number of patient-reported domains. For asenapine, the few data available indicate limited or equivocal impact on QOL. For iloperidone, no data are yet available. For lurasidone, preliminary unpublished data from a longitudinal long-term study assign a favourable impact on subjective tolerability and social functioning. The field urgently needs more rigorous studies and, also, the development of approaches on how to integrate such outcome assessments in the process of care and policy decision making. Issues such as QOL, subjective tolerability, satisfaction and medication preferences are outcomes in their own right. However, the field also has to move beyond such outcomes, in terms of demonstrating their impact mediating other outcomes, such as improved adherence behaviour, utilization of psychiatric resources, hospitalization and visits to crisis centres and, ultimately, better recovery and community integration.
References
U.S. Food and Drug Administration Guidance for Industry. Patient-Reported Outcome Measures; use in medical product development to support labelling claims, FDA (2006).
Voruganti LNP, Heselgrave RS, Awad AG, et al. Quality of life measurement in schizophrenia: reconciling the question of subjectivity with the question of reliability. Psychol Med. 1998;28:165–72.
Awad AG, Voruganti LNP. The subjective/objective dichotomy: relevance to nosology, research and management. In: Gaebel W, editor. Zukunftsperspekiven in psychiatries und psychothezapie. Dormstadt: Stienkopff Verlog; 2002. p. 21–7.
Wehmeier PM, Kluge M, Schacht A, et al. Correlation of physician and patient related quality of life during antipsychotic treatment in outpatients with schizophrenia. Schizophr Res. 2007;91:178–86.
Awad AG, Voruganti LNP. Intervention research in psychosis: issues related to assessment of quality of life. Schizophr Bull. 2000;26:557–64.
Voruganti LNP, Slomka P, Zabel P, et al. Subjective effect of AMPT-induced dopamine depletion in schizophrenia: Correlation between dysphoric responses and striatal D2 binding ratios in SPECT imaging. Neuropsychopharmacology. 2001;25:642–50.
De Haan L, Lavalaye J, Linszend D, et al. Subjective experience and striatal dopamine D2 receptor occupancy in patients with schizophrenia stabilized by olanzapine or risperidone. Am J Psychiatry. 2000;157:1019–20.
Voruganti LNP, Awad AG. Subjective and behavioural consequences of striatal dopamine depletion in schizophrenia: findings from in vivo SPECT study. Schizophr Res. 2006;88:179–86.
Mizrahi R, Mamo D, Pausion P, et al. The relationship between subjective well-being and dopamine D2 receptors in patients treated with dopamine partial agonist and a full antagonist antipsychotic. Int J Neuropsychopharmacol. 2009;5:715–21.
Awad AG, Voruganti LNP, Heselgrave RJ. The aim of antipsychotic medications: What are they and are they being achieved? CNS Drugs. 1995;4:8–16.
Ritsner M, Kurs R. Impact of antipsychotic agents and their side-effects on the quality of life in schizophrenia. Expert Rev Pharmacoecon Outcomes Res. 2002;2:89–98.
Awad AG, Voruganti LNP. Impact of atypical antipsychotics on quality of life in patients with schizophrenia. CNS Drugs. 2004;18:877–93.
Zacher JL, Holmes JC. Second-generation antipsychotics: a review of recently approved agents and drugs in the pipeline. Formulary. 2012;47:106–12
Tuanainen A, Wahlbeck K. Newer atypical antipsychotic medication versus clozapine for schizophrenia. Cochrane Database Syst Rev. 2000; (2): CD000966.
Citrome L. Iloperidone, asenapine and lurasidone: a brief overview of three new second-generation antipsychotics. Postgrad Med. 2011;123:153–62.
Edwards SJ. Tolerability of atypical antipsychotics in the treatment of adults with schizophrenia or bipolar disorder: a mixed treatment comparisons of randomized controlled trials. Clin Ther. 2009;31:1345–59.
Agency for Health Care Research and Quality (AHRQ). First generation versus second generation antipsychotics in adults: Comparative effectiveness. Executive Summary, Publication No. 12—EHC054-EF, 2012. http://www.effectivehealthcare.ahrg.gov/reports/final.cfm.
Awad AG, Voruganti LNP. Measuring quality of life in patients with schizophrenia—an update. Pharmacoeconomics. 2012;30:183–95.
Awad AG, Voruganti LNP, Heselgrave RJ. Preliminary validation of a conceptual model to assess quality of life in schizophrenia. Qual Life Res. 1997;6:21–6.
Mencaccic on behalf of all investigators. Efficacy and tolerability of switching to ziprasidone in Italian patients with acute exacerbation of schizophrenia—an open-label study. Pharmacopsychiatry. 2012;45:236–40.
Huang M-W, Yang T-T, Ten P-R, et al. Effects of paliperidone extended release on the symptoms and functioning of schizophrenia. BMC Clin Pharmacol. 2012;12:1–11.
Grootens KP, van Vellen NM, Peuskens J, et al. Ziprasidone versus olanzapine in recent-onset schizophrenia and schizoaffective disorder—double-blind randomized controlled trial. Schizophr Bull. 2011;37:352–61.
Jui-Kang T, Wen-Kuo L, For-Wey L. Social interaction and drug attitude effectiveness in patients with schizophrenia. Psychiatr Q. 2011;82:343–51.
Liu-Seifert H, Osuntokun O, Godfrey J, et al. Patient perspectives on antipsychotic treatments and their association with clinical outcomes. Patient Prefer Adherence. 2010;4:369–77.
Docherty JP, Baker RA, Eudicone J, et al. Effect of aripiprazole versus haloperidone on PANSS Prosocial items in early episode patients with schizophrenia. Schizophr Res. 2010;120:199–203.
Ming-Hong H, Wei-Wen L, Shao-Tsu C, et al. A 64-week multicentre, open-label study of aripiprazole effectiveness in the management of patients with schizophrenia or schizoaffective disorder in a general psychiatric outpatient setting. Ann Gen Psychiatry. 2010;9:35. doi:10.1186/1744-859X-9-35.
Shoemaker J, Naber D, Vrifland P, et al. Long-term assessment of asenapine versus olanzapine in patients with schizophrenia or schizoaffective disorder. Pharmacopsychiatry. 2010;43:138–46.
Stahl SM, Malla A, Newcomer JW, et al. A post hoc analysis of negative symptoms and psychosocial function in patients with schizophrenia: a 40-week randomized double-blind study of ziprasidone versus haloperidol followed by a 3-year double-blind extension trial. Clin Psychopharmacol. 2010;30:425–50.
Canuso C, Grinspan A, Kalali A, et al. Medication satisfaction in schizophrenia: a blinded initiation study of paliperidone extended release in patients suboptimally responsive to risperidone. Int Clin Psychopharmacol. 2010;25:155–64.
Burns P, Morasini P, Gagnon DD, et al. Measuring social functioning with the personal and social performance scale in patients with acute symptoms of schizophrenia: interpretation of results of pooled analysis of three phase III trials of paliperidone extended release tablets. Clin Ther. 2010;32:275–92.
de Oliveira IR, Elkis H, Gattaz WF, et al. Aripiprazole for patients with schizophrenia and schizoaffective disorder: an open-label, randomized study versus haloperidol. CNS Spectr. 2009;14:93–102.
Kobayashi H, Morita K, Takeshi K, et al. Effects of aripiprazole on insight and subjective experience in individuals with an at-risk mental state. J Clin Psychopharmacol. 2009;5:421–5.
Potkin SG, Weiden PJ, Loebel AD, et al. Remission in schizophrenia: 196-week double-blind treatment with risperidone versus haloperidol. Int J Neuropsychopharmacol. 2009;9:1233–48.
Kim SW, Shin JS, Kim JM, et al. Effectiveness of switching to aripiprazole from atypical antipsychotics in patients with schizophrenia. Clin Neuropharmacol. 2009;32:243–9.
Schooler N. Long-term treatment with asenapine versus olanzapine in subjects with predominant persistent negative symptoms of schizophrenia. 2009, Abstract SCR-26-076.
Taylor D, Hanssens L, Loze JY, et al. Preference of medicine and patient-reported quality of life in community-treated schizophrenic patients receiving aripiprazole versus standard of care, results from the STAR study. J Eur Psychiatry. 2008;23:336–43.
Nasralla H, Morosini P, Gagnon DD. Reliability, validity and ability to detect change of the personal and social performance scale in patients with stable schizophrenia. Psychiatry Res. 2008;161:213–24.
Rossi A, Vita A, Tiradritti P, et al. Assessment of clinical and metabolic status, and subjective well-being in schizophrenia patients switched from typical to atypical antipsychotics to ziprasidone. Int Clin Psychopharmacol. 2008;4:216–22.
Ritsner M, Yorkov V, Ratner Y, et al. The effectiveness of ziprasidone in treating impaired quality of life in schizophrenia—a 12-month open-label, flexible-dose naturalistic observational study of patients undergoing usual care. Progr Neuro-Psycho Pharmacol Biol Psychiatry. 2007;31:1470–7.
Arang C, Gomez-Beneyto M, Brenlla J, et al. A 6-month prospective observational, naturalistic uncontrolled study to evaluate the effectiveness and tolerability of oral ziprasidone in patients with schizophrenia. Euro Neropsychopharmacol. 2007;17:456–63
Kerwin R, Millet B, Herman E, et al. A multicentre, randomized, naturalistic open-label study between aripiprazole and standard of care in the management of community-treated schizophrenic patients—Schizophrenia Trial of aripiprazole: (STAR) study. Eur Psychiatry. 2007;7:433–43.
Swartz MS, Perkins DO, Stroup TS, et al. Effects of antipsychotic medications on psychosocial functioning in patients with chronic schizophrenia: findings from the NIMH CATIE study. AM J Psychiatry. 2007;164:428–36.
Kane JM, Meltzer HY, Carson WH, et al. Aripiprazole for treatment resistant schizophrenia: a double-blind comparison study versus perphenazine. J Clin Psychiatry. 2007;68:213–23.
Kudla D, Lambert M, Domin S, et al. Effectiveness, tolerability and safety of aripiprazole in patients with schizophrenia or schizoaffective disorder: results of multicentre observational trial. Eur Psychiatry. 2007;22:195–202.
Mitsonis CI, Dimopoulos NP, Mitropoulos PA, et al. Aripiprazole augmentation in the management of residual symptoms in clozapine-treated outpatients with chronic schizophrenia—an open-label pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:373–7.
Tandon R, Marcus RN, Stock EG, et al. A prospective multicentre randomized parallel-group open-label study of aripiprazole in the management of patients with schizophrenia or schizoaffective disorder in general psychiatric practice: broad effectiveness study trial with aripiprazole (BETA). Schizophr Res. 2006;84:77–89.
Rosenbeck RA, Leslie D, Sendelar J, et al. Cost-effectiveness of second generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry. 2006;163:2080–9.
Philips GA, Van Brunt DL, Roychowdhury SM, et al. The relationship between quality of life and clinical efficacy from a randomized trial comparing olanzapine and ziprasidone. J Clin Psychiatry. 2006;67:1397–403.
Breier A, Berg PH, Thakore JH, et al. Olanzapine versus ziprasidone: results of a 28-week double-blind study in patients with schizophrenia. Am J Psychiatry. 2005;162:1879–87.
Loebel A, Siu C, Romanos S. Improvement in prosocial functioning after a switch to ziprasidone treatment. CNS Spectr. 2004;9:357–64.
Voruganti LNP, Awad AG. Neuroleptic dysphoria: towards a new synthesis. Psychopharmacology (Berlin). 2004;171:121–32.
Van Putten T, May PRA, Marder SR, et al. Subjective response to antipsychotic drugs. Arch Gen Psychiatry. 1981;38:187–90.
Hogan TP, Awad AG, Eastwood MR. A self-report predictive of drug compliance in schizophrenia: reliability and discriminative validity. Psychol Med. 1983;13:177–83.
Hogan TP, Awad AG. Subjective response to neuroleptics and outcome in schizophrenia: a re-examination of two measures. Psychol Med. 1992;22:347–52.
Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophr bull. 1993;19:609–18.
Awad AG, Voruganti LNP. Neuroleptic dysphoria, comorbid abuse in schizophrenia and the emerging science of subjective tolerability. J Dual Design. 2005;1:83–95
Awad AG. Subjective tolerability of antipsychotic medications and the emerging science of subjective tolerability disorders. Expert Rev Pharmcoecon Outcomes Res. 2010;10:1–4.
Naber DA. Self-rating scale to measure subjective effects of neuroleptic drugs, relationship to objective psychopathology, quality of life and other clinical variables. Int J Clin Psychopharmacol. 1995; 10(suppl)30: 123–133.
Voruganti LNP, Awad AG. Personal evaluation of transitions in treatment (PETiT) a scale to measure subjective aspects of antipsychotic drug therapy in schizophrenia. Schizophr Res. 2002;56:37–48.
Petall EA, Cooper H, Robinson C. The effects of choice on intrinsic motivation and related outcomes: a meta analysis of research findings. Psychol Bull. 2008;134:270–300.
Rosenbeck R, Stroup S, Keefe RS, et al. Measuring outcome priorities and preferences in people with schizophrenia. Brit J Psychiatry. 1005;187:529–36.
Awad AG. Antipsychotic medications: how satisfied are our patients? Clear Perspective, Management Issues in Schizophrenia 1999; 2: 1–6.
Rofail D, Gray R, Gowrnay K, et al. The development and internal consistency of the satisfaction with antipsychotic scale. Psychol Med. 2005;35:1063–72.
Endicott J, Nee J, Harrison W, et al. Quality of life enjoyment and satisfaction questionnaire. Psychopharmacol Bull. 1993;29:321–8.
Vernon MK, Revicki DA, Awad AG, et al. Psychometric evaluation of the Medication Satisfaction Questionnaire (MSQ) to assess satisfaction with antipsychotic medication among schizophrenia patients. Schizophr Res. 2010;118:271–8.
Brissos S, Molodynski A, Dias VV, et al. The importance of measuring psychosocial functioning in schizophrenia. Ann Gen Psychiatry. 2011;10:1–7.
Figueira M, Brissos S. Measuring psychosocial outcomes in schizophrenia patients. Curr Opin Psychiatry. 2001;24:91–9.
Heselgrave RJ, Awad AG, Voruganti LNP. The influence of neurocognitive deficits and symptoms on quality of life in schizophrenia. J Psychiatry Neuro Sci. 1997;22:235–43.
Juckel G, Morosini PL. The new approach: psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry. 2008;21:630–9.
Bell M, Tsang HW, Greig TE, et al. Neurocognition, social cognition, perceived social discomfort and vocational outcomes in schizophrenia. Schizophr Bull. 2009;35:738–47.
Hugh D, Nuamah IF, Lim P, et al. Independent effect of paliperidone extended release on social functioning beyond its effects on positive and negative symptoms of schizophrenia: a mediation analysis. J Clin Psychopharmacol. 2009;29:496–7.
Patterson TL, Goldman S, McKibbin CL, et al. UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–45.
Kawata T, Rivicki D. Psychometric properties of the personal and social performance scale (PSP) among individuals with schizophrenia living in the community. Qual Life Res. 2008;17:1247–56.
Awad AG, Hogan TP. Early treatment events and prediction of response to neuroleptics in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 1985;9:585–8.
Snyder CF, Aaronson NK, Choucair AK, et al. Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res. 2011;. doi:10-1007/s11136-011-0054-x.
Staniszewska S, Haywood K, Brett J, et al. Patient and public involvement in patient-reported outcome measures: evolution not revolution. Patient. 2012;5:79–87.
Acknowledgement
No sources of funding were used to assist with the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review. The opinions expressed in this review are the authors’ own.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Awad, A.G., Voruganti, L.N.P. The Impact of Newer Atypical Antipsychotics on Patient-Reported Outcomes in Schizophrenia. CNS Drugs 27, 625–636 (2013). https://doi.org/10.1007/s40263-013-0070-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-013-0070-1