Abstract
Haemodynamic, metabolic, and biochemical derangements in critically ill patients affect drug pharmacokinetics and pharmacodynamics making dose optimisation particularly challenging. Appropriate therapeutic dosing depends on the knowledge of the physiologic changes caused by the patient’s comorbidities, underlying disease, resuscitation strategies, and polypharmacy. Critical illness will result in altered drug protein binding, ionisation, and volume of distribution; it will also decrease oral drug absorption, intestinal and hepatic metabolism, and renal clearance. In contrast, the resuscitation strategies and the use of vasoactive drugs may oppose these effects by leading to a hyperdynamic state that will increase blood flow towards the major organs including the brain, heart, kidneys, and liver, with the subsequent increase of drug hepatic metabolism and renal excretion. Metabolism is the main mechanism for drug clearance and is one of the main pharmacokinetic processes affected; it is influenced by patient-specific factors, such as comorbidities and genetics; therapeutic-specific factors, including drug characteristics and interactions; and disease-specific factors, like organ dysfunction. Moreover, organ support such as mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation may contribute to both inter- and intra-patient variability of drug pharmacokinetics. The combination of these competing factors makes it difficult to predict drug response in critically ill patients. Pharmacotherapy targeted to therapeutic goals and therapeutic drug monitoring is currently the best option for the safe care of the critically ill. The aim of this paper is to review the alterations in drug pharmacokinetics associated with critical illness and to summarise the available evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Haemodynamic, metabolic, and biochemical derangements in critically ill patients affect drug pharmacokinetics (PK) and pharmacodynamics (PD). |
Organ support such as mechanical ventilation (MV), renal replacement therapy (RRT), and extracorporeal membrane oxygenation (ECMO) may contribute to both inter- and intra-patient variability to the drug’s pharmacokinetics. |
Target drug therapy and goal-directed therapy remain the best tools for personalised and safe drug dosing in critically ill patients. |
1 Introduction
Appropriate drug dosing in the intensive care unit (ICU) is crucial for therapeutic success. Nevertheless, the level of pharmacotherapy complexity in ICU populations is increased by the heterogeneity of patients admitted with a broad spectrum of diseases [1, 2]. Drug pharmacodynamics (PD) will depend on the achieved concentration of the active compounds at the target site. This concentration will be the result of the drug’s pharmacokinetic (PK) characteristics, including absorption, distribution, metabolism, and excretion (ADME) [3, 4]. While diverse factors affect critically ill patients’ drug ADME (Table 1), there are three key determinants for PK/PD alterations [5]. First, in ICU patients, multiple medications are often required to treat the underlying disorder and coexisting comorbidities, increasing the risk of drug-drug interactions (DDIs) and adverse drug events (ADEs) [1, 2, 6, 7]. Second, critical illness results in pathophysiologic changes that may modify the medications’ exposure [3]. For instance, haemodynamic, metabolic, and biochemical derangements in critically ill patients modify drug PK/PD making dose optimisation particularly challenging [1, 2]. As an example, impaired piperacillin penetration to muscle and adipose tissues has been described in patients with septic shock, leading to higher rates of therapeutic failures. Finally, organ support such as mechanical ventilation (MV), renal replacement therapy (RRT), and extracorporeal membrane oxygenation (ECMO) can contribute to inter and intra-patient variability in the drug’s volume of distribution (Vd), metabolism, and clearance (Cl) [2, 8, 9].
For the aforementioned reasons, critically ill patients require a high degree of individualisation to achieve appropriate pharmacotherapy [2]. Understanding the PK/PD changes during critical illness may help to improve therapeutic success and decrease adverse events [7, 10]. However, there is limited evidence to guide bedside clinicians [2]. In addition, the implications of critical illness on drug metabolism are particularly relevant because this is the main mechanism for drug clearance [7, 10]. The aim of this paper is to review drug metabolism and pharmacokinetic alterations associated with critical illness and to summarise the evidence available.
1.1 Drug Metabolism and the Liver
Drugs need to be lipophilic to cross biological membranes, hence lipophilicity is one of the determinants of the drug’s volume of distribution (Vd). However, lipid-soluble compounds are difficult to excrete. As a result, lipophilic drugs generally have a high Vd, high tissue penetration, and low urine excretion [3, 11]. Drug metabolism is the process used by the body to modify a chemical compound, and, in most cases increase water solubility and enhance excretion [6]. The vast majority of drug metabolism occurs in the liver, and to a lesser extent, in other organs such as the small intestine, lungs, brain, and kidneys [2, 6]. Drug metabolism is influenced by patient-specific factors, such as comorbidities, obesity, age, sex, and genetics; therapeutic-specific factors, including drug characteristics and drug interactions; type of nutrition or feeding, and its effect on hepatic and intestinal blood flow; and disease-specific factors, like circulatory changes that impair organ perfusion and alter drug Vd [6, 7, 12].
The extent of hepatic drug metabolism results from three factors: hepatic blood flow, unbound or free drug concentration, and the enzymatic capacity of hepatocytes. The first two factors will determine the hepatic extraction ratio (ER). Extraction ratio is the fraction of drug cleared from the blood after passing through the liver. Drugs can be classified as having high (> 70%), intermediate (30–70%) or low (< 30%) ER [1, 2, 13]. Drugs with high ER, like propofol and fentanyl, will be highly affected by hepatic blood flow, but to a lesser degree by enzyme function. Conversely, drugs with low hepatic ER, like phenytoin and ceftriaxone, are relatively flow independent, and clearance is related to enzymatic activity and protein binding [2, 13,14,15].
The third relevant factor for metabolism, the enzymatic capacity of hepatocytes, is determined by the metabolic reactions. These reactions are classified into two groups: Phase I and Phase II; however, these are not necessarily sequential [2, 6, 7]. Phase I reactions are performed by cytochrome P450 enzymes (CYPs) that catalyse the oxidation, reduction, and hydrolysis of drugs, and endogenous compounds [7]. The CYP enzymes are located in the smooth endoplasmic reticulum of the hepatocytes, the villous epithelium of the small intestine, the lungs, kidneys and brain [7]. Phase II reactions consist of glucuronidation, sulfation, methylation, or acetylation reactions that add large polar molecules to the parent drugs or metabolites to increase renal excretion [2]. These Phase II enzymes are mainly expressed in the liver, kidneys, and small intestine [6, 7, 11, 16].
Cytochrome P450 enzyme activity results in increased hydrophilicity with different possible effects that include: an increase in efficacy by activating prodrugs, a decrease in drug activity or toxicity by compound inactivation, or increased toxicity by the generation of toxic metabolites [2, 12, 17]. The prediction of Phase I reactions is complex because a single CYP is capable of metabolising different substrates or metabolising one molecule at different sites producing multiple metabolites, also multiple CYPs can be involved in the metabolism of one drug (Table 2) [11]. Cytochrome P450 enzymes 3A4, 3A5, 2C9, 2C19, and 2D6 account for 80% of Phase I reactions, but CYP3A4 is responsible for the metabolism of 50% of currently marketed drugs [6, 7, 11, 17].
Cytochrome P450 enzyme 3A4 substrates are structurally diverse with a wide range of sizes and affinities, including atypical kinetic profiles with extensive possibilities for induction or inhibition [6, 11]. It has been suggested that the complex effects observed with substrates of CYP3A4 are attributable to its spacious active site that allows the oxidation of large molecules and the binding of multiple substrates at the same time within the active site [6, 11]. Hence, a substrate can be a potent inhibitor of one site but a weaker inhibitor of another binding site, making clinical assumptions unreliable [6, 11]. Plasma levels of CYP3A4 substrates can vary to about 400-fold when induced or inhibited by medications [6, 7]. These complex interactions are illustrated with opioid requirements in patients on long-term treatment with CYP inducers, such as carbamazepine and phenytoin, because CYP3A4 is responsible for fentanyl and sufentanil dealkylation, patients treated with these antiepileptics will require higher doses of opioids. Clinicians aware of these interactions may find a therapeutic alternative in remifentanil that is metabolised by non-specific plasma esterases [7]. Another example where caution is necessary is with calcineurin inhibitors used in transplant recipients. Inhibition of CYP3A4 can lead to excessive levels of tacrolimus and cyclosporin, leading to neurologic complications, renal failure, hypertension, and thrombotic microangiopathy. In addition, inadequate levels of these medications resulting from CYP3A4 induction may lead to graft rejection. Interestingly, case reports exist of the use of CYP3A4 inducers, such as phenytoin and phenobarbital, to treat tacrolimus overdose [7]. When patients are treated with CYP3A4 inducers, like rifampicin and macrolides (e.g., azithromycin, erythromycin), higher doses of corticosteroids, such as hydrocortisone and methylprednisolone are necessary [6, 7]. Patients treated with imidazoles (i.e., miconazole, fluconazole), and calcium antagonists (i.e., amlodipine), have a five times higher risk of QT-prolongation and sudden death [7]. The list of metabolic interactions described for CYP3A4 metabolised drugs, is as extensive as the possibilities of drug combinations [6, 7].
Furthermore, CYP polymorphisms are associated with diverse and sometimes unpredictable therapeutic responses and failures. For example, CYP2D6 is described with 1–3% of the population being ultra-rapid metabolisers and 5–10% of White Caucasians, and 2% of Asians and Black people being poor metabolisers. As a result, a serotonin-like syndrome has been described when paroxetine and dextromethorphan are used concomitantly in patients with poor CYP2D6 metabolism [6, 12, 18]. In contrast, ultra-rapid CYP2D6 metabolisers can experience accumulation of active metabolites due to codeine conversion to morphine, with the consequent secondary effects such as respiratory depression [19]. Other relevant CYP polymorphisms, such as CYP3A5 may be responsible for abnormalities in midazolam hydroxylation, lidocaine demethylation, dextromethorphan N-demethylation, and carbamazepine epoxidation [6].
2 Critical Illness and Disease-Specific Abnormalities
2.1 Liver Disease
Ischaemia-reperfusion injury after shock, surgery, haemorrhage, and massive transfusion is usually accompanied by a decrease in hepatic metabolism, protein expression, and CYP enzymatic activity [20]. To accentuate the level of complexity, the use of agents, such as inotropes (e.g., dobutamine) or vasodilators (e.g., nitroprusside), will increase portal and hepatic blood flow, while vasopressors (e.g., phenylephrine, norepinephrine, and epinephrine) will produce α-adrenergic-mediated vasoconstriction with the consequent reduction of blood flow [2, 13]. While liver failure has been associated with decreased CYP activity, only modest changes have been described for drugs that are metabolised by CYP2C9, and CYP3A4. Therefore, the specific effect of a particular drug will depend on the severity of liver disease and the enzymes responsible for its metabolism [16]. As an example, ketamine is metabolised by the CYPs to norketamine, an active metabolite with only one-third the potency of the parent compound; hence, the reduced metabolism in liver dysfunction will prolong its clinical effect [13]. In addition, cholestasis delays the biliary excretion of drugs and impairs CYP450 function [2]. Among the medications affected by hepatobiliary disease is rocuronium, which is mainly excreted in bile unchanged, so hepatic dysfunction leads to reduced clearance and prolonged action [10, 13]. Fentanyl and its derivatives (i.e., alfentanil, sufentanil and remifentanil) are highly liposoluble and are metabolised by the liver into inactive metabolites. As a result, these also accumulate when there is liver impairment [10].
2.2 Acute Kidney Injury
Up to 50% of critically ill patients will suffer from acute kidney injury (AKI) [21]. Acute kidney injury not only decreases the ability to excrete water-soluble compounds through urine, but also affects metabolism independent from renal clearance. For instance, CYP3A4 activity has been inversely correlated to blood urea nitrogen (BUN) concentration [2, 21,22,23,24]. This phenomenon was illustrated by multiple studies that showed a 27% increase in CYP3A4 activity after 2 hours of dialysis, which may be related to a decrease in urea concentration [21, 23, 25]. Furthermore, numerous authors have shown that the human kidney has significant drug-metabolising capacity [26]. Cytochrome P450 enzymes 2B6, 3A4 and 3A5 have been documented to be expressed in the kidneys [24, 26, 27]. Propofol clearance provides a good example of the role of renal metabolism since its glucuronidation exceeds by 3 to 4 times what is possible through hepatic blood flow alone. Similarly, systemic clearance of morphine has been reported to exceed hepatic clearance by 38% [13, 24, 26]. Using immunohistochemistry, the expression of Phase II enzymes in the nephron has been shown in the kidney, where they are responsible for the glucuronidation of medications such as morphine and furosemide [26].
In addition to the reduced clearance and the prolonged half-life, patients with AKI have higher Vd. The combination of these factors increases the risk of drug accumulation, especially benzodiazepines and opioids in patients treated with continuous infusions. For example, midazolam in critically ill patients has a two-fold higher Vd, a three-fold prolonged half-life, and a three-fold lower Cl when compared to non-ICU patients [28, 29]. Morphine is metabolised to 3- and 6-glucuronides, the latter being the active metabolite that accumulates in renal failure [10, 13]. With this in mind, propofol and dexmedetomidine sedation protocols may be preferred for intensive care unit (ICU) patients [28, 30].
2.3 Gastrointestinal Disease
The gastrointestinal tract is affected by pathological or drug-induced haemodynamic alterations, with the consequent reduction in intestinal peristalsis, mucosal function, and drug metabolism [6]. Enteric absorption and drug availability in critically ill patients are unpredictable due to changes in gastric pH, gut oedema, loss of enteric architecture, loss of epithelial junctions, and cholestasis [13, 21]. Additionally, cellular dysfunction will lead to impaired enzymatic activity and decreased intestinal metabolism [8, 24]. The combination of these factors will result in decreased oral drug bioavailability. As a result, delayed and decreased oral paracetamol peak concentration and a reduction of more than 50% of antimicrobial absorption, namely ciprofloxacin, has been described in critically ill patients [31]. Conversely, increased daily protein intake has been linked to an increase in hepatic drug-metabolising capacity [8, 24].
2.4 Respiratory Failure
The lung is not a major pathway for drug metabolism with few exceptions such as propofol and catecholamines (e.g., norepinephrine). However, respiratory failure will produce hypoxaemia that can lead to liver dysfunction and hypercapnia that may result in acidosis with the consequent decrease in renal drug clearance and changes in drug ionisation [10]. The use of mechanical ventilation to correct respiratory disturbance will have its own physiological impact. The level of positive end-expiratory pressure (PEEP) leads to directly proportional decreases in cardiac output and hepatic blood flow [1]. Similarly, prone positioning in patients with moderate/severe acute respiratory distress syndrome (ARDS) needs to be carefully performed with appropriate support to avoid the reduction of hepatic blood flow [13].
2.5 Heart Failure
Hypoperfusion and neurohumoral activation in heart failure (HF) negatively affects the function of multiple organs, particularly by reducing blood flow to the gastrointestinal tract, the liver, and the kidneys [10, 32]. Consequently, reduced hepatic metabolic activity may potentially reduce clearance for drugs with high ER, including propofol, midazolam, and fentanyl. Because patients with HF may have reduced renal flow, clearance of drugs may decrease in proportion to the severity of haemodynamic decompensation [33]. For instance, patients with HF have 38% less clearance of propofol and almost a two-fold increase in blood concentrations [28]. Added to these disturbances, the fluid retention observed in congestive heart failure may increase the Vd of drugs [10]. Proof of this, is the four-fold increase in Vd observed in critically ill patients with a cardiac index below 1.5 L/min/m2 that resulted in dexmedetomidine accumulation and prolonged half-life [28].
2.6 Neurological Injury
During critical illness, inflammatory mediators bind to endothelium receptors causing alterations in the adhesion molecules, signalling pathways, and nitric oxide production [34, 35]. These changes disturb the blood–brain barrier and increase endothelium permeability with the consequent risk of free drug accumulation in the brain [34, 35]. For example, in meningitis, traumatic brain injury, and even non-neurological ICU patients, direct neurotoxicity has been described with the use of beta-lactams [9, 36]. Concentration-dependent neurological symptoms include delirium, decreased level of consciousness, myoclonus, seizures, confusion, aphasia, and coma [9, 36, 37]. Moreover, in patients with subarachnoid haemorrhage, there is increased penetration of morphine metabolites into the brain [35].
Prolonged administration of opioids and sedatives has been associated with tolerance, withdrawal syndrome, delirium, and worse patient outcomes [38,39,40]. Tolerance is believed to be multifactorial, it may occur due to increased expression of drug transporters with diverse affinities, desensitising of internal signalling, and up-regulation of P-glycoprotein that increases drug efflux from the central nervous system [38, 39]. Conversion of analgesia to intermittent bolus as well as sedative rotation are possible solutions to overcome this issue [38, 39]. The working hypothesis is that having drug receptors occupied for lower periods of time will decrease the incidence of tolerance and withdrawal [38, 39]. Also, receptor subtypes with different affinities can coexist, while one subtype may undergo desensitisation, other subtypes may be available for different sedatives [41]. For example, a protocol analysing the transition from fentanyl to hydromorphone was associated with a decrease in the amount of sedatives required including propofol and benzodiazepines [39]. In paediatric patients, a sedation rotation protocol showed a lower incidence of withdrawal, decreased time requiring opioid continuous infusion, and decreased ICU stay [38]. Enteral administration of methadone has also been associated with earlier discontinuation of fentanyl in mechanically ventilated patients [42].
2.7 Inflammation, Shock, and Resuscitation
For most drugs, the therapeutic effects are mediated by the free or unbound drug concentrations [2]. If plasma protein binding decreases, the free plasma fraction, Vd, and the half-life increase [3, 16]. In critically ill patients, changes to plasma protein levels are common. Increased vascular permeability, endothelial barrier dysfunction, and protein catabolism lead to hypoalbuminaemia; while inflammation increases alfa1-acid glycoprotein (AAG) and acute phase reactant concentrations [1, 2, 13, 21, 43]. Acidic drugs bind to the former, whereas basic drugs bind to the latter [1, 2, 13, 21, 43]. Due to low serum albumin, the free drug fraction of acidic drugs, such as ceftriaxone, daptomycin, ertapenem, and dexmedetomidine, increases with the consequent risk for toxicity [1, 13, 28, 30, 43]. For example, Boucher et al demonstrated an inverse relationship between free phenytoin and albumin concentrations [15]. Another study demonstrated an increase of valproic acid free fraction of 6 to 7 times in patients with trauma when concentrations of albumin decreased to 1.5 g/dL [15]. Moreover, in AKI the plasma protein binding to albumin is decreased due to competitive inhibition by uraemic toxins and decreased drug-albumin affinity [3]. As a result, highly protein-bound drugs that require minimal concentrations to achieve therapeutic effect may require reduced dosing, and monitoring of free concentrations of these medications is recommended [1, 43].
During shock, the release of inflammatory mediators and cytokines, metabolic acidosis, and microcirculatory impairment will result in organ hypoperfusion, cellular hypoxia, mitochondrial dysfunction, and finally multi-organ failure [2, 13, 14]. The reduction in blood perfusion to the gastrointestinal tract will result in impaired oral drug absorption, decreased hepatic blood flow may decrease drug metabolism, and the reduction of renal perfusion can affect drug elimination. In contrast to shock, the resuscitation strategies and the use of vasoactive drugs may counteract these effects by leading to a hyperdynamic state that will increase blood flow towards the major organs including the brain, heart, kidneys, and liver, with the subsequent increase of drug hepatic metabolism and renal excretion [2, 3, 13]. Additionally, hyperdynamic states increase drugs Vd, this is particularly relevant for hydrophilic antimicrobials (i.e., acyclovir, aminoglycosides, beta-lactams, fluconazole and glycopeptides) [10, 13].
Conditions such as sepsis, trauma, surgery, burns, and the use of vasopressors can lead to an increase in renal blood flow and increased renal drug clearance. Similarly, the elimination of drugs with high ER (i.e., fentanyl, morphine) is enhanced [30]. Furthermore, the inflammatory response associated with shock has been demonstrated to have a variable effect on hepatic CYP450 enzyme activity [2, 8, 44]. In trauma CYPs 2C19, 3A4, and 2E1 activity has been shown to be significantly depressed while there is an increase in CYP2C9 activity [2, 8, 44]. In sepsis, endotoxin mediated CYP inhibition has also been described [10]. Cytochrome P450 enzyme expression is also suppressed by fever and inflammatory mediators. The most important pro-inflammatory cytokines responsible for this process are interleukin 6 (IL-6) and tumour necrosis factor alfa (TNF-α) [6,7,8, 45]. The basis for this down-regulation of CYPs is not fully elucidated; however, a reduction in mRNA transcription has been suggested [17, 44]. Interleukin-6-mediated activation of the hypothalamus–pituitary–adrenal axis, also increases cortisol levels, which competitively inhibits the metabolism of CYP substrates [21]. In contrast, hypothermia has been associated with decreased blood flow towards the gastrointestinal tract, reducing drug absorption, decreasing the Vd, CYPs activity, and hepatic metabolism [2, 35].
3 ICU Interventions and Therapies
Because ECMO and RRT do not resolve the underlying diseases, effective pharmacotherapy is the cornerstone of treatment of the primary cause for the critical illness. However, conventional drug dosing may not suffice in patients with these supportive therapies, while aggressive regimens may expose patients to drug toxicity and adverse effects [5]. Other interventions, such as mechanical ventilation may increase the PK and PD complexity in ICU patients.
3.1 Mechanical Ventilation
Currently, there is a paucity of data on PK alterations associated with the use of mechanical ventilation (MV) [46]. However, MV has the capacity to decrease patients’ cardiac output resulting in renal perfusion changes and lower glomerular filtration rates [46]. For example in mechanically ventilated patients a 20% decrease in vancomycin clearance has been described [47]. In addition, reductions in hepatic blood flow may result in decreased drug metabolism of medications with high ER [48, 49].
3.2 Renal Replacement Therapy
When considering patients with renal replacement therapy (RRT), multiple modalities are used in the ICU, including intermittent or continuous haemodialysis, haemofiltration, and haemodiafiltration [25, 50]. Solute and drug removal are achieved by diffusion and convection while ultrafiltration is used for fluid removal [25, 50]. Three key drug properties predict dialysis removal: molecular weight (MW), Vd and protein binding [5, 25, 51]. Small, hydrophilic drugs such as ciprofloxacin, gentamicin and levetiracetam are easily removed by diffusion, while larger molecules such as vancomycin and daptomycin will be removed by convection [2, 25, 52]. Drugs with large MW, high Vd and protein binding are unlikely to be removed, examples include heparin, benzodiazepines and phenytoin [2, 25, 52]. In addition to drug properties and critical illness, blood clearance will be affected by membrane type, pore size, surface area, the dialysate flow rate, RRT efficiency (low vs high), blood flow rate and duration [25, 50]. However RRT impact on drug concentration is difficult to predict and, when available, therapeutic drug monitoring (TDM) may be necessary, especially for antimicrobials, since underdosing may lead to therapeutic failures and or increased drug resistance [5, 25]. For example, a 6-h low-efficiency dialysis session would remove approximately 60% of piperacillin tazobactam, but only 20% of meropenem [43]. Monitoring of antibiotic concentrations on patients with RRT showed subtherapeutic levels 15% of the time and up to 10% excessive dosing intervals [25]. After dialysis cessation, an increase in plasmatic drug concentrations may occur due to redistribution from peripheral to central compartments [50]. Additional roles for RRT include its use to treat toxic alcohol ingestion and drug overdose, including salicylates, lithium, metformin, and valproic acid. It may also be considered in the management of dabigatran toxicity when idarucizumab, the reversal agent, is not available. The use of RRT in these cases may affect the PK of medications concomitantly administered and dose adjustments must be taken into consideration [52, 53].
3.3 Extracorporeal Membrane Oxygenation (ECMO)
Pharmacokinetic alterations associated with extracorporeal circuit and assistant devices are complex. In general terms, the addition of extracorporeal circuits will increase the Vd, bind, or sequester drugs decreasing the concentration in plasma and reducing drug clearance [5, 54]. The intensity of binding is influenced by drug properties, such as molecular weight, plasma protein binding, degree of ionisation, and lipophilicity [3, 54, 55]. Sequestration can decrease over time due to saturation of the ECMO circuit, this may also result in drug release from the ECMO after stopping the medications [3, 54, 55]. Furthermore, when cardiac support is done by non-pulsatile devices, the renin-angiotensin system will be activated with the consequent increase in the circulating volume and decrease in drug elimination [3, 54, 55]. Therapeutic failures and insufficient concentrations of antimicrobials, analgesics, sedatives and even antiepileptics have been described for ECMO patients. However, this may reflect not only ECMO-induced changes but also critical illness PK alterations [56,57,58].
4 Drug interactions (DDIs)
Drug interaction risk increase as a function of the number of prescribed drugs, with a fourfold increased risk when seven medications are used, and up to eightfold when more than ten drugs are used [59]. In critically ill patients, an average of 30 different medications are administered during their ICU stay [60, 61]. Hence, DDI rates are higher than those in general wards but the incidence report is variable, mainly explained by a wide diverse population with countless possibilities of therapies and illness combinations [61]. Additionally, DDIs account for 4% of ICU admissions [7].
Most DDIs can be explained by metabolism alterations. Drugs can have either no impact, or induce/inhibit other drug metabolisms. Inhibition itself can be divided into three categories: reversible or competitive, quasi-irreversible, and irreversible inhibition. As a result, concomitant administration of drugs may result in alterations of their concentrations [6, 7, 11, 35]. Competitive inhibition is transient, it depends on the inhibitor concentration and its affinity for the enzyme and is solved once the inhibitor is excreted [6, 7, 11, 35]. In contrast, induction occurs when a substance enhances the synthesis or decreases the destruction of an enzyme, resulting in increased activity. This will result either in a decreased effect of medications metabolised by that enzyme or in increased effect of prodrugs that require activation [7].
Drug interactions in critically ill patients are easily studied in vitro but the effect in vivo is difficult to estimate since significant interindividual variability exists [6, 7]. Databases have been created to detect DDIs; however, only a 20% concordance in DDIs severity has been found when comparing among different databases. Furthermore, these are designed to consider the interaction of two concurrent medications but not multiple combinations [59].
5 Assessing Drug Therapy in Critical Illness
5.1 Goal-directed Therapy and Therapeutic Drug Monitoring
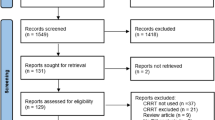
For the reasons described throughout the paper developing a robust drug-dosing regimen, in such a complex patient population as the critically ill, is highly challenging. Figure 1 illustrates the complex interactions of different factors in PK/PD changes in critically ill patients. As a solution to this problem, TDM and goal-directed therapy remain the best tool for personalised and safe drug dosing in critically ill patients [3, 21, 25]. Dosage adjustment is not only important to attain PK/PD targets but also to avoid overexposure in some patients and thus an increased risk of adverse effects [6].
Many drugs used in the ICU are dosed to effect. For example, vasopressors are often titrated to a goal mean arterial pressure; sedative doses should be guided by arousal scales; and analgesia should be directed to target pain scores [2]. However, monitoring drug concentrations should be considered for drugs without an observable clinical response and a narrow therapeutic range, i.e., antiepileptics and antimicrobials. These concentrations should be measured not only in blood but also at the target sites since plasma concentrations in critically ill patients do not necessarily reflect tissue concentrations [9, 35].
Currently, the greatest challenge exists in the management of antimicrobial therapy. Changes in the PK properties of many antimicrobials due to critical illness are difficult to predict and TDM is frequently used as a surrogate to clinical response [62]. A prospective study evaluating beta-lactams, whose effectiveness depends on the time above the minimum inhibitory concentration, showed that up to 74% of ICU patients required drug dose adjustment when concentrations were measured; including doses decrease due to high drug concentrations [3, 9, 13, 36, 63]. Aminoglycosides, such as gentamicin and tobramycin, have a peak dependent therapeutic effect and a narrow therapeutic window so monitoring blood concentrations is recommended [10, 36]. Conversely, other antibiotics like glycopeptides, fluoroquinolones and linezolid exhibit a combination of time- and dose-dependent PD targets [10, 36]. Moreover, institution-specific dosing guidelines should incorporate local epidemiology and antibiogram data to guarantee adequacy of therapy and simultaneously avoid overtreatment [50, 62].
The clinical use of TDM is complex because it requires continuous sample collection, prolonged turnaround times are necessary to measure drug concentrations, and some specific assays are not easily available [5, 62]. Besides TDM, computer-assisted dosing software has been developed to overcome some of these PK issues; however, their use requires dedicated drug concentration monitoring hindering their application and use [5, 10, 64]. Goal-directed therapy and TDM may not suffice for safe pharmacotherapy delivery in the ICU and the benefits of having a pharmacist as part of the interprofessional ICU team have been well demonstrated. Studies have shown that including critical-care pharmacists on daily ICU clinical rounds is associated with improved patient outcomes, reduced mortality and hospital stay [65]. Pharmacists can support clinicians with decision making for complex patients and situations by optimising medication safety systems and reducing the risk of medication errors and DDIs. Their scope of practice includes the use of computer-assisted PK and PD models and predictions, TDM, as well as educational and stewardship activities [66, 67].
6 Conclusion
Many variables influence drug PK in critically ill patients with the potential to either increase or decrease the pharmacologic effect of medications, leading to high incidence of therapeutic failures and/or adverse drug reactions. Most PK and metabolism data for drugs are derived from healthy volunteers and do not consider the complex interactions of different levels of coexisting organ dysfunction. In addition, extrapolating results from PK studies in critically ill patients is challenging because of the heterogeneous nature of critically ill patients, small sample sizes and diverse treatments and interventions. These factors make titration of pharmacotherapy based on clear goals and therapeutic drug monitoring the best option for the safe care of ICU patients.
References
McKindley DS, Hanes S, Boucher BA. Hepatic drug metabolism in critical illness. Pharmacotherapy. 1998;18(4):759–78.
Smith BS, Yogaratnam D, Levasseur-Franklin KE, Forni A, Fong J. Introduction to drug pharmacokinetics in the critically ill patient. Chest. 2012;141(5):1327–36.
Jamal JA, Roger C, Roberts JA. Understanding the impact of pathophysiological alterations during critical illness on drug pharmacokinetics. Anaesth Crit Care Pain Med. 2018;37(6):515–7.
Fan J, de Lannoy IA. Pharmacokinetics. Biochem Pharmacol. 2014;87(1):93–120.
Roberts JA, Bellomo R, Cotta MO, Koch BCP, Lyster H, Ostermann M, et al. Machines that help machines to help patients: optimising antimicrobial dosing in patients receiving extracorporeal membrane oxygenation and renal replacement therapy using dosing software. Intensive Care Med. 2022;48(10):1338–51.
Mouly S, Meune C, Bergmann JF. Mini-series: I. Basic science. Uncertainty and inaccuracy of predicting CYP-mediated in vivo drug interactions in the ICU from in vitro models: focus on CYP3A4. Intensive Care Med. 2009;35(3):417–29.
Spriet I, Meersseman W, de Hoon J, von Winckelmann S, Wilmer A, Willems L. Mini-series: II. clinical aspects. Clinically relevant CYP450-mediated drug interactions in the ICU. Intensive Care Med. 2009;35(4):603–12.
Boucher BA, Wood GC, Swanson JM. Pharmacokinetic changes in critical illness. Crit Care Clin. 2006;22(2):255–71 (vi).
Dhaese S, Van Vooren S, Boelens J, De Waele J. Therapeutic drug monitoring of beta-lactam antibiotics in the ICU. Expert Rev Anti Infect Ther. 2020;18(11):1155–64.
Power BM, Forbes AM, van Heerden PV, Ilett KF. Pharmacokinetics of drugs used in critically ill adults. Clin Pharmacokinet. 1998;34(1):25–56.
Uetrecht J, Trager W. Drug metabolism: chemical and enzymatic aspects. Informa Healthc. 2007;2007:33–140.
Frye RF, Zgheib NK, Matzke GR, Chaves-Gnecco D, Rabinovitz M, Shaikh OS, et al. Liver disease selectively modulates cytochrome P450–mediated metabolism. Clin Pharmacol Ther. 2006;80(3):235–45.
Charlton M, Thompson JP. Pharmacokinetics in sepsis. BJA Educ. 2019;19(1):7–13.
Kumar A, Remmel RP, Mann HJ, Beilman GJ. Drug metabolism in hemorrhagic shock: pharmacokinetics of selective markers of cytochrome-P450 2C9, 2D6, and 3A4 enzyme activities in a porcine model. J Surg Res. 2011;167(2):e231–43.
Rodighiero V. Effects of liver disease on pharmacokinetics: an update. Clin Pharmacokinet. 1999;37(5):399–431.
Lohr JW, Willsky GR, Acara MA. Renal drug metabolism. Pharmacol Rev. 1998;50(1):107–41.
El-Ghiaty MA, Shoieb SM, El-Kadi AOS. Cytochrome P450-mediated drug interactions in COVID-19 patients: current findings and possible mechanisms. Med Hypotheses. 2020;144: 110033.
Lane K, Dixon JJ, Lee T, Johnston A, van Schaik R, van Fessem M, et al. Hepatic drug metabolism by CYP2D6 in critically ill adults with AKI-effect of phenotype and AKI severity. Intensive Care Med Exp. 2015;3(suppl 1):A839.
Gasche Y, Daali Y, Fathu M, Chiappe A, Cottini S, Dayer P, et al. Codeine intoxication associated with ultrarapid CYP2D6 metabolism. N Engl J Med. 2004;351:2827–31.
Tokuno M, Taguchi K, Sakai H, Ohtsuki S, Yamasaki K, Otagiri M. Evaluation of cytochrome P450-based drug metabolism in hemorrhagic shock rats that were transfused with native and an artificial red blood cell preparation, Haemoglobin-vesicles. Drug Metab Pharmacokinet. 2020;35(5):417–24.
Blanco VE, Hernandorena CV, Scibona P, Belloso W, Musso CG. Acute kidney injury pharmacokinetic changes and its impact on drug prescription. Healthcare (Basel). 2019;7(1):1–10.
Lea-Henry TN, Carland JE, Stocker SL, Sevastos J, Roberts DM. Clinical pharmacokinetics in kidney disease: fundamental principles. Clin J Am Soc Nephrol. 2018;13(7):1085–95.
Vilay AM, Churchwell MD, Mueller BA. Clinical review: drug metabolism and nonrenal clearance in acute kidney injury. Crit Care. 2008;12(6):235.
Dixon J, Lane K, Macphee I, Philips B. Xenobiotic metabolism: the effect of acute kidney injury on non-renal drug clearance and hepatic drug metabolism. Int J Mol Sci. 2014;15(2):2538–53.
Jang SM, Awdishu L. Drug dosing considerations in continuous renal replacement therapy. Semin Dial. 2021;34(6):480–8.
Knights KM, Rowland A, Miners JO. Renal drug metabolism in humans: the potential for drug-endobiotic interactions involving cytochrome P450 (CYP) and UDP-glucuronosyltransferase (UGT). Br J Clin Pharmacol. 2013;76(4):587–602.
Braund R. Renal medicine and clinical pharmacy. 1st ed. New York: Springer International Publishing; 2020. p. 5–45.
Tse AHW, Ling L, Lee A, Joynt GM. Altered pharmacokinetics in prolonged infusions of sedatives and analgesics among adult critically ill patients: a systematic review. Clin Ther. 2018;40(9):1598-615 e2.
Jakob SM, Roukone E, Sarapohja RMGT, Garrat C, Pocock SJ, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation. JAMA. 2012;307(11):1151–60.
Abdul-Aziz MH, Alffenaar JC, Bassetti M, Bracht H, Dimopoulos G, Marriott D, et al. Antimicrobial therapeutic drug monitoring in critically ill adult patients: a position paper. Intensive Care Med. 2020;46(6):1127–53.
Tansley G, Hall R. Pharmacokinetic considerations for drugs administered in the critically ill. Br J Hosp Med. 2015;76(2):89–93.
Mangoni AA, Jarmuzewska EA. The influence of heart failure on the pharmacokinetics of cardiovascular and non-cardiovascular drugs: a critical appraisal of the evidence. Br J Clin Pharmacol. 2019;85(1):20–36.
Ogawa R, Stachnik JM, Echizen H. Clinical pharmacokinetics of drugs in patients with heart failure: an update (part 1, drugs administered intravenously). Clin Pharmacokinet. 2013;52(3):169–85.
Hughes CG, Pandharipande PP, Thompson JL, Chandrasekhar R, Ware LB, Ely EW, et al. Endothelial activation and blood-brain barrier injury as risk factors for delirium in critically ill patients. Crit Care Med. 2016;44(9):e809–17.
Roberts DJ, Hall RI. Drug absorption, distribution, metabolism and excretion considerations in critically ill adults. Expert Opin Drug Metab Toxicol. 2013;9(9):1067–84.
Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient–concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11.
Grahl JJ, Stollings JL, Rakhit S, Person AK, Wang L, Thompson JL, et al. Antimicrobial exposure and the risk of delirium in critically ill patients. Crit Care. 2018;22(1):337.
Sanavia E, Mencia S, Lafever SN, Solana MJ, Garcia M, Lopez-Herce J. Sedative and analgesic drug rotation protocol in critically ill children with prolonged sedation: evaluation of implementation and efficacy to reduce withdrawal syndrome. Pediatr Crit Care Med. 2019;20(12):1111–7.
Kovacevic MP, Szumita PM, Dube KM, DeGrado JR. Transition from continuous infusion fentanyl to hydromorphone in critically ill patients. J Pharm Pract. 2020;33(2):129–35.
Duprey MS, Dijkstra-Kersten SMA, Zaal IJ, Briesacher BA, Saczynski JS, Griffith JL, et al. Opioid use increases the risk of delirium in critically ill adults independently of pain. Am J Respir Crit Care Med. 2021;204(5):566–72.
Martyn JAJ, Mao J, Bittner EA. Opioid tolerance in critical illness. N Engl J Med. 2019;380(4):365–78.
Al-Qadheeb NS, Roberts RJ, Griffin R, Garpestad E, Ruthazer R, Devlin JW. Impact of enteral methadone on the ability to wean off continuously infused opioids in critically ill, mechanically ventilated adults: a case-control study. Ann Pharmacother. 2012;46(9):1160–6.
Brown P, Battistella M. Principles of drug dosing in sustained low efficiency dialysis (SLED) and review of antimicrobial dosing literature. Pharmacy (Basel). 2020;8(1):33.
Harbrecht BG, Frye RF, Zenati MS, Branch RA, Peitzman AB. Cytochrome P-450 activity is differentially altered in severely injured patients. Crit Care Med. 2005;33(3):541–6.
Anari MR, Renton KW. Modulatory effect of hyperthermia on hepatic microsomal cytochrome P450 in mice. Biochem Pharmacol. 1993;46(2):307–10.
Koyner JL, Murray PT. Mechanical ventilation and lung-kidney interactions. Clin J Am Soc Nephrol. 2008;3(2):562–70.
Medellin-Garibay SE, Romano-Moreno S, Tejedor-Prado P, Rubio-Alvaro N, Rueda-Naharro A, Blasco-Navalpotro MA, et al. Influence of mechanical ventilation on the pharmacokinetics of vancomycin administered by continuous infusion in critically ill patients. Antimicrob Agents Chemother. 2017;61(12):e01249-17. https://doi.org/10.1128/AAC.01249-17.
Richard C, Berdeaux A, Delion F, Riou B, Rimailho A, Giudicelli JF, et al. Effect of mechanical ventilation on hepatic drug pharmacokinetics. Chest. 1986;90(6):837–41.
Dasta J. Physiologic implications of mechanical ventilation on pharmacokinetics. Ann Pharmacother. 1989;23:316–22.
Hoff BM, Maker JH, Dager WE, Heintz B. Antibiotic dosing for critically ill adult patients receiving intermittent haemodialysis, prolonged intermittent renal replacement therapy, and continuous renal replacement therapy: an update. Ann Pharmacother. 2020;54:43–55.
Bunchman TE, Ferris ME. Management of toxic ingestions with the use of renal replacement therapy. Pediatr Nephrol. 2011;26(4):535–41.
Bouajram RH, Awdishu L. A clinician’s guide to dosing analgesics, anticonvulsants, and psychotropic medications in continuous renal replacement therapy. Kidney Int Rep. 2021;6(8):2033–48.
Mirrakhimov AE, Barbaryan A, Gray A, Ayach T. The role of renal replacement therapy in the management of pharmacologic poisonings. Int J Nephrol. 2016;2016:3047329.
Hahn J, Choi JH, Chang MJ. Pharmacokinetic changes of antibiotic, antiviral, antituberculosis and antifungal agents during extracorporeal membrane oxygenation in critically ill adult patients. J Clin Pharm Ther. 2017;42(6):661–71.
Raffaeli G, Pokorna P, Allegaert K, Mosca F, Cavallaro G, Wildschut ED, et al. Drug disposition and pharmacotherapy in neonatal ECMO: from fragmented data to integrated knowledge. Front Pediatr. 2019;7:360.
Kuhn D, Metz C, Seiler F, Wehrfritz H, Roth S, Alqudrah M, et al. Antibiotic therapeutic drug monitoring in intensive care patients treated with different modalities of extracorporeal membrane oxygenation (ECMO) and renal replacement therapy: a prospective, observational single-center study. Crit Care. 2020;24(1):664.
Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. J Crit Care. 2012;27(6):741 e9-741 e8.
Abdul-Aziz MH, Roberts JA. Antibiotic dosing during extracorporeal membrane oxygenation: does the system matter? Curr Opin Anaesthesiol. 2020;33(1):71–82.
Zakrzewski-Jakubiak H, Doan J, Lamoureux P, Singh D, Turgeon J, Tannenbaum C. Detection and prevention of drug-drug interactions in the hospitalized elderly: utility of new cytochrome p450-based software. Am J Geriatr Pharmacother. 2011;9(6):461–70.
Bakker T, Abu-Hanna A, Dongelmans DA, Vermeijden WJ, Bosman RJ, de Lange DW, et al. Clinically relevant potential drug-drug interactions in intensive care patients: a large retrospective observational multicenter study. J Crit Care. 2021;62:124–30.
Vanham D, Spinewine A, Hantson P, Wittebole X, Wouters D, Sneyers B. Drug-drug interactions in the intensive care unit: do they really matter? J Crit Care. 2017;38:97–103.
Lanckohr C, Boeing C, De Waele JJ, de Lange DW, Schouten J, Prins M, et al. Antimicrobial stewardship, therapeutic drug monitoring and infection management in the ICU: results from the international A-TEAMICU survey. Ann Intensive Care. 2021;11(1):131.
Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39(12):2070–82.
Gorham J, Taccone FS, Hites M. Ensuring target concentrations of antibiotics in critically ill patients through dose adjustment. Expert Opin Drug Metab Toxicol. 2022;18(3):177–87.
Lee H, Ryu K, Sohn Y, Kim J, Suh GY, Kim E. Impact on patient outcomes of pharmacist participation in multidisciplinary critical care teams: a systematic review and meta-analysis. Crit Care Med. 2019;47(9):1243–50.
Preslaski CR, Lat I, MacLaren R, Poston J. Pharmacist contributions as members of the multidisciplinary ICU team. Chest. 2013;144(5):1687–95.
MacLaren R, Devlin JW. The bedside critical care pharmacist: a mandatory ICU team member essential for patient care. Crit Care Med. 2019;47(9):1276–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflicts of interest/competing interests
Dr Morales Castro, Dr Dresser and Dr Granton have no conflicts of interest to disclose. Dr Fan reports personal fees from ALung Technologies, Aerogen, Baxter, Boehringer-Ingelheim, GE Healthcare, Inspira, and Vasomune outside the submitted work.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors agree with its submission and publication.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
D.M.C. performed the literature review and wrote the first draft. All authors were involved in the critical revision of the data, and the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morales Castro, D., Dresser, L., Granton, J. et al. Pharmacokinetic Alterations Associated with Critical Illness. Clin Pharmacokinet 62, 209–220 (2023). https://doi.org/10.1007/s40262-023-01213-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01213-x