Abstract
Background
Post-placement menstrual bleeding pattern changes with intrauterine contraceptives (IUCs), including levonorgestrel-releasing intrauterine systems (LNG-IUS), can be a reason for avoidance or early discontinuation. Prostaglandins play an important role in menstrual bleeding and pain. The key drivers of prostaglandin synthesis are cyclooxygenase (COX) enzymes, which are inhibited by non-steroidal anti-inflammatory drugs. In this study, we report the findings from pharmacokinetic (PK) analyses undertaken with an LNG-IUS (LNG-IUS 8) modified with an additional reservoir containing indomethacin (IND).
Methods
The IND/LNG-IUS 8 is a proof-of-concept device studied in a phase II proof-of-concept/dose-finding study. IND/LNG-IUS 8 contains the same LNG content as the unmodified LNG-IUS 8 (13.5 mg) but was prepared with three different IND doses (low, 6.5 mg; middle, 12.5 mg; and high, 15.4 mg), resulting in different daily release rates. Overall, 174 healthy, premenopausal women were randomized to one of the four treatment arms (low-, middle-, high-dose IND/LNG-IUS 8 or LNG-IUS 8). Initial and residual IND and LNG content were collected and the amount of IND and LNG released in vivo over the period of use was calculated. A subset of 62 participants underwent dense blood sampling for PK analysis. Concentrations of IND and LNG in plasma were determined by validated liquid chromatography-tandem mass spectrometry methods and plotted over time. Descriptive statistics were calculated for plasma drug concentrations and PK parameters.
Results
High-dose IND/LNG-IUS 8 initially released much higher levels of IND than expected based on in vitro release data, followed by a steep decline, with the reservoir emptied by 4.5 months. Middle- and low-dose IND/LNG-IUS 8 demonstrated steady sustained release of IND over time, emptying after 7.4 and 8.4 months, respectively. Peak plasma concentrations of IND for low- and middle-dose IND/LNG-IUS 8 remained below the 20% maximal inhibitory concentration (IC20) values for COX enzymes. The average daily IND release rate in vivo was 49 µg/day for low-dose and 112 µg/day for middle-dose IND/LNG-IUS 8. The IND release rate profile and IND plasma concentrations in vitro both decreased steadily over time with low- and middle-dose IND/LNG-IUS 8. The LNG release rate profile was comparable for all IND/LNG-IUS 8 dose groups and LNG-IUS 8.
Conclusion
This PK study demonstrates that two different drugs can be released at different rates from an IUS designed with two drug reservoirs. Inclusion of IND does not impact the LNG PK profile. Low- and middle-dose IND/LNG-IUS 8 were associated with a systemic IND exposure that should preclude the occurrence of adverse events typically observed after oral IND dosing.
Study Registration
ClinicalTrials.gov identifier number: NCT03562624
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A proof-of-concept study with a levonorgestrel-releasing intrauterine system (LNG-IUS) modified with the addition of an indomethacin (IND)-releasing reservoir was conducted in healthy, premenopausal women to investigate the pharmacokinetics (PK) and release of IND and LNG. |
PK analysis of in vitro and in vivo data indicated that two drugs can be released at different rates from an LNG-IUS designed with two reservoirs, and the inclusion of IND to an LNG-IUS does not have any effect on the LNG release profile. |
1 Introduction
Long-acting reversible contraceptives (LARCs) are the most effective methods of reversible contraception [1]. This effectiveness is in part attributable to the fact that LARC methods are not compliance-dependent; pregnancy rates with adherence-dependent methods, such as combined oral contraceptive pills, vary widely owing to differences in individual propensities to use such methods perfectly [2]. An LARC method particularly associated with high continuation and satisfaction rates is the hormonal levonorgestrel-releasing intrauterine system (LNG-IUS) [1, 3, 4]. As well as being a highly effective method of contraception, LNG-IUSs are associated with considerably lower levels of systemic exposure to LNG than LNG-containing oral contraceptives [5]. Despite such advantages, LARCs remain underused, although uptake rates are increasing [6, 7].
There are several possible reasons for the low uptake of LARCs. Among them is the fact that LNG-IUSs and other forms of intrauterine devices (IUDs) can be associated with bleeding pattern changes. Shortly after placement of an LNG-IUS, a woman’s menstrual bleeding profile may become less predictable, with more bleeding/spotting days than before placement [8, 9]. This is attributable to the local effects of LNG on the endometrium and the reaction to the introduction of a ‘foreign body’ [10, 11]. However, such changes are usually temporary and after about 3 months, bleeding and spotting often become lighter and less frequent [12,13,14]. These changes in bleeding profile can be bothersome, potentially affecting day-to-day activities [15,16,17,18]; notably, it has been shown that as menstrual bleeding increases, women’s satisfaction decreases [19, 20]. Such changes may lead to some women having an LNG-IUS removed [18, 21]. From a clinical perspective, increased bleeding/spotting after placement is seldom considered a major clinical issue and pre-insertion counseling can help women to prepare for such possible changes after placement [22]. However, measures to reduce bleeding in the post-placement phase would likely be welcomed by most women using an LNG-IUS for the first time, and not just those who find it sufficiently problematic to consider device removal.
Prostaglandins play an important role in menstrual bleeding and pain [23], and there is evidence of increased prostaglandin synthesis after IUS placement [10]. Thus, bleeding changes after IUS placement may be at least partly attributable to increases in prostaglandin levels. The cyclooxygenase (COX) enzymes are key drivers of prostaglandin synthesis, and inhibition of these enzymes by administration of certain non-steroidal anti-inflammatory drugs (NSAIDs) is used to reduce bleeding and pain during menses [23, 24] and for bleeding irregularity associated with copper IUDs (Cu-IUDs) [25]. Indeed, Cu-IUDs that release the NSAID COX inhibitor indomethacin (IND) are currently marketed in China [26, 27]. Although few data relating to the use of these products have been reported, some studies indicate that the release of IND from these devices mitigates the increased menstrual blood loss typically associated with Cu-IUDs [27]. Furthermore, the contraceptive efficacy of Cu-IUDs containing IND appears to be the same as or better than Cu-IUDs with no NSAID, and discontinuation attributable to bleeding/pain seems to be significantly lower [26, 27]. As an NSAID, IND is an attractive choice for this application because of its high potency on both COX enzymes (COX-1 and COX-2) [28, 29]. Only a relatively low dose is needed for efficacy, therefore a small drug reservoir is sufficient to accommodate the amount needed, and the size of the IUS does not need to change substantially to carry it.
Accordingly, we produced a modified IUS device containing both LNG and IND, with the aim of reducing bleeding changes post-placement relative to the device containing LNG only. In this study, we report the results of pharmacokinetic (PK) studies undertaken with a proof-of-concept device, IND/LNG-IUS 8, as part of a phase II clinical trial.
2 Methods
2.1 Indomethacin/Levonorgestrel-Releasing Intrauterine System (IND/LNG-IUS) 8 Device Overview
The proof-of-concept device, IND/LNG-IUS 8, was based on the marketed LNG-IUS 8 device (Jaydess®; Bayer AG, Germany; total LNG content, 13.5 mg) [30], but with a T-body modified to include a reservoir containing IND in addition to the reservoir containing LNG (Table 1). The IND reservoir was added below the LNG reservoir, and the silver ring on LNG-IUS 8 was removed so that the IND reservoir could be accommodated without substantially increasing the length of the T-body. Thus, the dimensions of IND/LNG-IUS 8 and LNG-IUS 8, and the insertion tubes used to place them, were identical (device width, 28 mm; device length, 30 mm; insertion tube diameter, 3.8 mm).
IND/LNG-IUS 8 devices with the same LNG content (13.5 mg) were prepared with three different IND contents (low dose, 6.5 mg; middle dose, 12.5 mg; high dose, 15.4 mg) and different IND release rates for efficacy, safety and plasma PK evaluation versus LNG-IUS 8 in a proof-of-concept phase II study. Efficacy and safety findings will be reported elsewhere.
2.2 In Vitro Release Rate Determination
To characterize the performance of the devices before insertion, the IND and LNG release rates were determined in vitro during incubation in aqueous 1% (w/v) 2-hydroxypropyl-β-cyclodextrin in a shaking water bath at 37°C. Sink conditions were maintained throughout release rate testing. The concentrations of IND and LNG were determined by reverse-phase high-performance liquid chromatography (RP-HPLC) with external calibration. The chromatographic conditions are shown below.
-
Instrument: U(H)PLC, e.g. Agilent 1290 UHPLC
-
Injection volume: 10 μL
-
Detector wavelength: 244 nm
-
Column: e.g. ACQUITY UPLC BEH C18 1.7 μm 2.1 × 50 mm
-
Mobile phase: 45/55 (v/v) acetonitrile/0.1% formic acid
-
Flow rate: 0.5 mL/min
-
Column temperature: 30 °C.
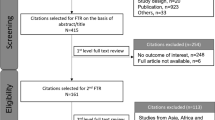
2.3 Phase II Study Overview
A multicenter, single-blinded, randomized controlled, phase II study was conducted in six centers in Germany and the UK between June 2018 and June 2019. Healthy, premenopausal women aged 18–45 years were enrolled. Inclusion criteria included a body mass index (BMI) of 18–32 kg/m2 at screening, no clinically relevant findings on pretreatment endometrial biopsy, and agreement to use a non-hormonal method of contraception if required during the pretreatment cycle and for 7 days before IUS insertion. Exclusion criteria included the use of short-acting hormonal contraceptives (oral, transdermal, intravaginal) during the pretreatment cycle, or long-acting hormonal preparations < 40 weeks before screening. Eligibility criteria and further aspects of study design are reported in detail elsewhere (Fels et al., Am J Obstet Gynecol. Accepted). Participants were randomized 1:1:1:1 to one of four parallel treatment arms (low-dose IND/LNG-IUS 8; middle-dose IND/LNG-IUS 8; high-dose IND/LNG-IUS 8; and LNG-IUS 8); enrolment of 36 women per treatment arm was planned (total n = 144). Approvals were obtained from the Institutional Review Boards and Independent Ethics Committees for each participating center, and the study was conducted in compliance with the Declaration of Helsinki and Good Clinical Practice guidelines. All participants provided written, informed consent prior to study start.
2.4 Data Collection for Pharmacokinetic Analysis
A subset of 62 volunteer participants underwent dense sampling for non-compartmental PK analysis. Blood samples for non-compartmental analyses of IND and LNG were collected post-placement on day 0 at 1, 3, 5, and 8 h, daily on days 1–6, then on days 13, 27, 41, 55, 69, 89 (± 2 days). LNG-IUSs were removed 89 days after placement (the same time as removal for all other study participants) and samples were taken 2, 4, and 7 days after removal to describe the elimination phase.
2.5 Determination of Initial and Residual Content of IND and LNG
Devices from batches used in the phase II study were analyzed to determine the actual initial content of IND and LNG, and devices collected after removal were washed and analyzed to determine the residual content of IND and LNG. The amount of IND and LNG released in vivo over the period of use was calculated from these initial and residual values. Based on the calculated amount released, an average daily release rate was estimated over the individual period of use. IND and LNG were extracted from elastomer material using tetrahydrofuran, then quantified using the RP-HPLC assay method.
-
Instrument: U(H)PLC, e.g. Agilent 1290 Infinity LC
-
Injection volume: 4 μL
-
Detector wavelength: 244 nm
-
Column: e.g. ACQUITY UPLC BEH C18 1.7 μm 2.1 × 50 mm
-
Mobile phase: 38/62 (v/v) acetonitrile/0.1% formic acid
-
Flow rate: 0.5 mL/min
-
Column temperature: 30°C.
2.6 Data Analysis
Concentrations of IND and LNG in plasma were determined using validated liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods. Method validations and analyses of the study samples were performed in compliance with the European Medicines Agency guideline on bioanalytical method validation [31], the US FDA guideline on bioanalytical method validation [32], the Reflection Paper for Laboratories that Perform the Analysis or Evaluation of Clinical Trial Samples [33], the regulations in Good Laboratory Practice [34] and Good Clinical Practice [35]. IND was determined in human EDTA K2 plasma after addition of the internal standard IND-d4 and protein precipitation with acetonitrile and solid phase extraction. Separation was achieved by means of a liquid chromatographic system.
For mass spectrometric detection, a triple quadrupole mass spectrometer in positive TurboIonSprayTM ionization mode was applied. The calibration range was from 10.0 ng/L (lower limit of quantification [LLQ]) to 10,000 ng/L (upper limit of quantification [ULQ]). Accuracy (calculated as a percentage of the nominal) and precision (coefficient of variation [CV]) were between 98.6% and 103.3%, and 4.65% and 5.26%, respectively. LNG was determined in human EDTA K2 plasma after addition of the internal standard LNG-d6 and automated liquid-liquid extraction with a mixture of methyl tert-butyl ether and hexanes. Separation was achieved by means of a liquid chromatographic system. For the mass spectrometric detection, a triple quadrupole mass spectrometer in positive TurboIonSpray™ ionization mode was applied. The calibration range was from 10.0 ng/L (LLQ) to 400 ng/L (ULQ). Accuracy (calculated as a percentage of the nominal) and precision (CV) were between 97.2% and 99.0%, and 2.10% and 6.92%, respectively. IND was determined in human EDTA K2 plasma after addition of the internal standard IND-d4 and protein precipitation with acetonitrile and solid-phase extraction. Separation was achieved by means of a liquid chromatographic system. For mass spectrometric detection, a triple quadrupole mass spectrometer in positive TurboIonSpray™ ionization mode was applied.
The PK parameters were calculated in accordance with current Bayer guidelines using the model-independent (non-compartmental) method and the PK WinNonlin software version 5.3 (Certara®, Princeton, NJ, USA) in conjunction with the Automation Extension (Bayer AG). Based on concentration-time data, the following parameters were calculated for IND and LNG: Cav (average plasma drug concentration during the period of use), Cav/D (Cav divided by the dose [the average amount of drug released per day over the period of use]), Clast (last concentration value above the LLQ), Cmax (maximum plasma drug concentration), AUC(89d) (area under the plasma drug concentration-time curve from time zero until device removal on day 89), tlast (time of Clast), and tmax (time to reach Cmax).
IND and LNG concentration data acquired from the dense sampling groups were plotted over time and the following descriptive statistics were calculated for plasma drug concentrations at each sampling point and for all PK parameters (except tmax): geometric mean, minimum, median, maximum, and number of measurements. Tmax was described using minimum, maximum, median, and frequency counts. Plasma concentrations of IND were compared with reported concentrations of IND that elicit 20% inhibition (IC20) of enzymes COX-1 (200 nM, equivalent to approximately 72 µg/L IND) and COX-2 (60 nM, equivalent to approximately 21 µg/L IND) [36]; systemic exposure to IND below these thresholds support the claim of no pharmacologically relevant systemic exposure. Exposure to IND was also compared with the reported Cmax for IND [37] achieved after a single 50 mg oral dose (c. 2.5 mg/L). Statistical analyses were based on the safety population, i.e. all treated participants. All available data were included in the statistical analyses; no missing data were imputed.
3 Results
3.1 In Vitro Release Rates for IND and LNG
Measurement of IND release rates over time in vitro from the low-, middle-, and high-dose IND/LNG-IUS 8 found that the high-dose device released initially higher levels of IND compared with the middle- and low-dose devices, which was followed by a steep decline over the first 2–3 months. The high-dose reservoir depleted after about 4.5 months (136 ± 2.9 days). This in vitro release rate decline was steeper than observed with the middle- and low-dose devices, both of which showed steady, sustained release of IND, with the middle-dose device depleting after about 7.5 months and the low-dose device after about 8.4 months (Fig. 1).
Concurrent in vitro measurement of LNG release rates over time from the three devices determined that addition of the second drug reservoir containing IND did not affect the LNG release rate profile seen with the control device LNG-IUS 8 (Fig. 2a). Furthermore, measurement of release rates in the longer term after the IND reservoirs were empty showed no effect on the LNG release rate profile (Fig. 2b).
3.2 Initial and Residual Content Analysis of IND and LNG in Devices
Analysis of actual initial drug content and of residual drug content after device removal at day 89 determined that 4.4, 9.8, and 16.0 mg of IND had been released from the low-, middle-, and high-dose IND/LNG-IUS 8 devices, respectively, during the period of use and that all device types had releases of 0.7–0.8 mg of LNG (Table 2).
3.3 Demographic and Population Characteristics in the Pharmacokinetic Set
In total, 62 women underwent dense sampling for non-compartmental PK analysis (low-dose IND/LNG-IUS 8, n = 22; middle-dose IND/LNG-IUS 8, n = 14; high-dose IND/LNG-IUS 8, n = 11; LNG-IUS 8, n = 15). Mean ± standard deviation (SD) age across the four groups was in the 33.2 ± 7.0 years range, and mean ± SD BMI was 23.5 ± 2.7 kg/m2; 58 (93.5%) women were of White ethnicity. The characteristics of the four groups at baseline were broadly representative of the overall safety population in the parent phase II study (n = 167; mean age, 33.4 years; mean BMI, 23.7 kg/m2; White, 163 [97.6%]) (Fels L, et al. Am J Obstet Gynecol 2021. Accepted). In total, one participant discontinued prematurely in the low-dose IND/LNG-IUS 8 group, with zero and four participants in the middle- and high-dose IND/LNG-IUS 8 groups, respectively, not completing the study. There were three participants in the LNG-IUS 8 group who discontinued before the end of the study. No participants in the PK analysis set discontinued prematurely.
3.4 Pharmacokinetics of IND and LNG
Non-compartmental PK analysis determined that maximum plasma IND concentration (Cmax) associated with the three IND/LNG-IUS 8 devices ranged from 1467 to 20,805 ng/L, and that the average plasma concentration over the period of use (Cav) ranged from 428 to 2892 ng/L (low-dose to high-dose IND/LNG-IUS 8) (Table 3).
As shown in Fig. 3, only the peak plasma IND concentration associated with high-dose IND/LNG-IUS 8 approached the IC20 value for one of the COX enzymes. At all other timepoints and at all IND/LNG-IUS 8 doses, plasma concentrations of IND remained below IC20 levels throughout the period of use. In Table 3, Cav for all three IND/LNG-IUS 8 doses was clearly below the IC20 for both COX enzymes. Moreover, the maximum plasma IND concentration achieved with high-dose IND/LNG-IUS 8 was approximately 100-fold lower than the maximum achieved following a single 50 mg dose of oral IND (Fig. 3). Geometric mean Cmax for plasma LNG in the four groups was in the 160–208 ng/L range and Cav was in the 118–155 ng/L range (Table 4). Consistent with the LNG release rate profiles seen in vitro (Fig. 2), no relevant differences in the plasma LNG PK profiles over time were evident among the three IND/LNG-IUS 8 devices and the control LNG-IUS 8 (Fig. 4).
Plasma concentration of IND in relation to IC20 levels. IND IC20 for COX-1 is approximately 72,000 ng/L; IND IC20 for COX-2 is approximately 21,000 ng/L. Cmax maximum (peak) plasma drug concentration, COX cyclooxygenase, IC20 drug concentration eliciting 20% maximal inhibition, IND indomethacin, IUS intrauterine system, LLQ lower limit of quantitation
Plasma concentrations of LNG during the period of use and during the elimination phase after removal for low-, middle- and high-dose IND/LNG-IUS 8 and LNG-IUS 8. Data are expressed as geometric mean and geometric SD. IND indomethacin, IUS intrauterine system, LLQ lower limit of quantitation, LNG levonorgestrel, LNG-IUS levonorgestrel-releasing intrauterine system, SD standard deviation
3.5 Comparison of In Vitro and In Vivo Properties of IND and LNG
The average daily IND release rate over the period of use in vivo was 49 µg/day for low-dose IND/LNG-IUS 8 and 112 µg/day for middle-dose IND/LNG-IUS 8 (Table 5). Based on plasma IND concentration over time, it can be assumed that the IND reservoir in the high-dose IND/LNG-IUS 8 was depleted shortly after 41 days of use. The estimated average daily release of IND over 90 days would have been approximately 180 µg/day but given the likely shorter timeframe of depletion, the average release rate in vivo was estimated to be approximately 390 µg/day.
The IND release rate profile in vitro (Fig. 5a) declined slowly over time and in parallel for low- and middle-dose IND/LNG-IUS. A similar decline was observed for the IND plasma concentrations for both dose groups in vivo (Fig. 5b). Thus, the observed decrease in plasma IND concentration over time in vivo with the low- and middle-dose IND/LNG-IUS 8 devices was in line with the concurrent decreasing daily in vitro release of IND.
Comparison of IND release over 3 months for low- and middle-dose IND/LNG-IUS 8 a in vitroa and b in vivo. aData are repeated from Fig. 1 to facilitate comparison between in vitro and in vivo data. Data are expressed as geometric mean/geometric SD. IND indomethacin, IUS intrauterine system, LLQ lower limit of quantitation, LNG-IUS levonorgestrel-releasing intrauterine system, SD standard deviation
The average daily release rate of LNG in vivo over the period of use was similar for all groups, in the 8.10–8.93 µg/day range (Table 5). In vitro (Fig. 2a) LNG release rate profiles and in vivo (Fig. 4) LNG plasma concentrations were well in line. LNG release from all IND/LNG-IUS 8 devices was similar to that observed for LNG-IUS 8.
4 Discussion
This study provides proof of principle that two different drugs (the progestogen, LNG; and the NSAID, IND) can be released at different rates from an IUS designed with two drug reservoirs, and that inclusion of the second drug and reservoir has no effect on the profile of release of LNG based on direct comparison with the marketed product (LNG-IUS 8) that contains only the LNG reservoir. Furthermore, at the low- and middle-dose levels of IND, the release rate profiles in vitro corresponded to the plasma IND concentration-time profiles observed in vivo over 3 months post-placement, indicating that the in vitro release rates at these dose levels are a good indicator of performance in vivo. On this basis, depletion of the low- and middle-dose IND reservoirs in vivo would be expected to occur within 9 months of device placement. Finally, Cmax for IND in participants fitted with the low- or middle-dose IND/LNG-IUS 8 devices (Cmax 1.5 µg/L and 4.1 µg/L, respectively), was at least 5-fold lower than the IC20 of IND for COX-2 and at least 17-fold lower than the IC20 for COX-1. The very low systemic concentrations of IND seen with the low-dose IND/LNG-IUS 8 would not be expected to elicit common adverse reactions typically associated with IND after oral dosing (typical Cmax in the region of 2.5 mg/L after a dose of 50 mg) [37, 38].
The excellent contraceptive effectiveness of LNG-IUSs is attributable to both the local effects of LNG-releasing IUSs and the lack of dependence on contraceptive compliance [2, 5]. Many women also prefer the prospect of very low systemic exposure to hormone compared with that associated with combined or progestin-only oral contraceptives [5]. Furthermore, there is now evidence from real-world settings to suggest that healthcare professionals use LNG-IUS differentially depending on the characteristics and medical needs of the women they see in clinical practice [39, 40]; therefore, being able to provide a variety of LNG-IUS options that can suit the differing needs and desires of individuals would be useful.
Evaluation of a two-reservoir IND/LNG-IUS device was undertaken because an opportunity exists to improve women’s experiences during the initial months following LNG-IUS placement. Unexpected or frequent bleeding during this interval can be bothersome and can have an impact on physical and emotional quality of life by disrupting work, exercise routines, as well as social and sexual activities. Oral NSAIDs are commonly used to treat menstrual bleeding and pain [23, 24] but this class of drugs is associated with adverse effects, most often headaches and gastrointestinal disturbances, such as indigestion, nausea, vomiting, and diarrhea [41]. By analogy with the concept that local delivery of LNG from LNG-IUSs provides effective contraception with minimal systemic drug exposure, we reasoned that local delivery of NSAIDs may mitigate the initial bleeding changes that can be associated with LNG-IUS placement, without causing the adverse reactions associated with systemic concentrations of drug that are reached during oral administration.
The choice of IND was informed by its high potency on both COX enzymes relative to other NSAIDs (thus reducing the amount of drug that might have to be accommodated in the second LNG-IUS reservoir) [28, 29], and by the precedent of Cu-IUDs that include an IND reservoir [26, 27]. Increased menstrual bleeding is common after Cu-IUD placement and is often a reason for device removal [42]; it has been reported that rates of discontinuation, bleeding and pain were lower among women using a Cu-IUD containing IND than among women using a control unmedicated Cu-IUD [27].
As well as the choice of NSAID, it was important to characterize its release rate profile. A clinical study of 738 women using different LNG-IUS devices found that the amount of bleeding and spotting was highest during the first 3 months after placement, reduced substantially during the second 3-month period, and stabilized after about 9 months [13]. Thus, release of NSAIDs has the potential to be most beneficial during the first 3 months and may be of more marginal benefit at 9 months post-placement, even though LNG-IUS 8 is indicated for 3 years of use [43]. As demonstrated here, the low- and middle-dose IND/LNG-IUS 8 devices were depleted of IND after 7–9 months in vitro. Based on the concordance between in vitro release rate and plasma IND concentrations over the first 3 months, it would be anticipated that the low- and middle-dose devices would continue to deliver IND for 7–9 months in vivo.
It was notable that the in vitro profile of IND release and the plasma concentrations of IND associated with high-dose IND/LNG-IUS 8 were discrepant, with depletion in vivo taking, on average, about 41 days (last observable plasma concentration after 56 days) compared with 136 days in vitro. This may have been attributable to differences in the configuration of the IND reservoir used in the high-dose device relative to those used in the low- and middle-dose devices. A polydimethylsiloxane (PDMS) polymer coating to control IND release was used in the latter devices, the thickness of which regulated the rate of IND release from the reservoir; in contrast, no coating was used in the high-dose IND/LNG-IUS 8 (Table 1). Bearing in mind that LNG-IUS 8 is indicated for 3 years of contraceptive use, it was also important to determine whether addition of the second reservoir with a second drug would alter the release profile of LNG. Within the limits of error, the plasma concentrations of LNG determined with LNG-IUS 8 or with the three IND/LNG-IUS devices were the same, and also the in vitro LNG release profiles of the four devices were essentially identical for up to 20 months (the last time point measured for low-dose IND/LNG-IUS 8).
5 Conclusions
The data reported here are from a parent phase II efficacy and safety study (NCT03562624) that investigated whether IND/LNG-IUS 8 reduces bleeding and spotting, compared with LNG-IUS 8, in women in the 90-day period after device placement. The present analysis investigated the PK of IND and LNG released from the new two-reservoir IUS. The release profile of LNG was unaffected by the addition of the second drug reservoir and the release rates of IND in the low- and middle-dose devices were associated with systemic IND exposure that should preclude the occurrence of adverse events that can be associated with oral administration of IND. Thus, neither the high contraceptive efficacy nor the favorable safety profile of the marketed device, LNG-IUS 8, should be compromised. Further information on the performance of IND/LNG-IUS 8 in reducing bleeding and spotting in the initial post-placement period and safety profile are anticipated (Fels et al. Am J Obstet Gynecol. In press).
References
Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007.
Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404.
Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117(5):1105–13.
Agostini A, Godard C, Laurendeau C, Benmahmoud Zoubir A, Lafuma A, Levy-Bachelot L, et al. Two-year continuation rates of contraceptive methods in France: a cohort study from the French national health insurance database. Eur J Contracept Reprod Health Care. 2018;23(6):421–6.
Hofmann B, Apter D, Bitzer J, Reinecke I, Serrani M, Höchel J, et al. Comparative pharmacokinetic analysis of levonorgestrel-releasing intrauterine systems and levonorgestrel-containing contraceptives with oral or subdermal administration route. Eur J Contracept Reprod Health Care. 2020;25(6):417–26.
Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: increasing use of long-acting reversible contraception. Hum Reprod Update. 2011;17(1):121–37.
Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009–2012. Obstet Gynecol. 2015;126(5):917–27.
Bahamondes L, Brache V, Meirik O, Ali M, Habib N, Landoulsi S, et al. A 3-year multicentre randomized controlled trial of etonogestrel- and levonorgestrel-releasing contraceptive implants, with non-randomized matched copper-intrauterine device controls. Hum Reprod. 2015;30(11):2527–38.
Weisberg E, Bateson D, McGeechan K, Mohapatra L. A three-year comparative study of continuation rates, bleeding patterns and satisfaction in Australian women using a subdermal contraceptive implant or progestogen releasing-intrauterine system. Eur J Contracept Reprod Health Care. 2014;19(1):5–14.
Critchley HO, Wang H, Kelly RW, Gebbie AE, Glasier AF. Progestin receptor isoforms and prostaglandin dehydrogenase in the endometrium of women using a levonorgestrel-releasing intrauterine system. Hum Reprod. 1998;13(5):1210–7.
Sheppard BL. Endometrial morphological changes in IUD users: a review. Contraception. 1987;36:1–10.
Apter D, Briggs P, Tuppurainen M, Grunert J, Lukkari-Lax E, Rybowski S, Gemzell-Danielsson K. A 12-month multicenter, randomized study comparing the levonorgestrel intrauterine system with the etonogestrel subdermal implant. Fertil Steril. 2016;106(1):151-7.e5.
Gemzell-Danielsson K, Schellschmidt I, Apter D. A randomized, phase II study describing the efficacy, bleeding profile, and safety of two low-dose levonorgestrel-releasing intrauterine contraceptive systems and Mirena. Fertil Steril. 2012;97(3):616-22.e1-3.
Gemzell-Danielsson K, Buhling KJ, Dermout SM, Lukkari-Lax E, Montegriffo E, Apter D. A Phase III, single-arm study of LNG-IUS 8, a low-dose levonorgestrel intrauterine contraceptive system (total content 13.5mg) in postmenarcheal adolescents. Contraception. 2016;93(6):507–12.
Bradley JE, Alam ME, Shabnam F, Beattie TSH. Blood, men and tears: keeping IUDs in place in Bangladesh. Cult Health Sex. 2009;11:543–58.
Higgins JA, Sanders JN, Palta M, Turok DK. Women’s sexual function, satisfaction, and perceptions after starting long-acting reversible contraceptives. Obstet Gynecol. 2016;128:1143–51.
Polis CB, Hussain R, Berry A. There might be blood: a scoping review on women’s responses to contraceptive-induced menstrual bleeding changes. Reprod Health. 2018;15:114.
Schmidt EO, James A, Curran KM, Peipert JF, Madden T. Adolescent experiences with intrauterine devices: a qualitative study. J Adolesc Health. 2015;57:381–6.
Carvalho NM, Chou V, Modesto W, Margatho D, Garcia EAL, Bahamondes L. Relationship between user satisfaction with the levonorgestrel-releasing intrauterine system and bleeding patterns. J Obstet Gynaecol Res. 2017;43(11):1732–7.
Sanders JN, Adkins DE, Kaur S, Storck K, Gawron LM, Turok DK. Bleeding, cramping, and satisfaction among new copper IUD users: a prospective study. PLoS ONE. 2018;13(11):e0199724.
Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol. 2013;122:1214–21.
Davie JE, Walling MR, Mansour DJ, Bromham D, Kishen M, Fowler P. Impact of patient counseling on acceptance of the levonorgestrel implant contraceptive in the United Kingdom. Clin Ther. 1996;18:150–9.
Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015;7:CD001751.
Grimes DA, Hubacher D, Lopez LM, Schulz KF. Non-steroidal anti-inflammatory drugs for heavy bleeding or pain associated with intrauterine-device use. Cochrane Database Syst Rev. 2006;4:CD006034.
Godfrey EM, Folger SG, Jeng G, Jamieson DJ, Curtis KM. Treatment of bleeding irregularities in women with copper-containing IUDs: a systematic review. Contraception. 2013;87(5):549–66.
Hu X, Li L, Zou Y, Wu S. A multicenter comparative study of UCu200, TCu380A, and medicated γ-IUD devices inserted immediately after vacuum aspiration. Int J Gynaecol Obstet. 2013;122(1):65–9.
Wang LY, Li SZ, Wu SY, Zhao YH, Wang Y. A random control study of indomethacin-containing MYCu intrauterine contraceptive device for 60 months [in Chinese]. Zhonghua Yi Xue Za Zhi. 2013;93(7):496–9.
Cryer B, Feldman M. Cyclooxygenase-1 and cyclooxygenase-2 selectivity of widely used nonsteroidal anti-inflammatory drugs. Am J Med. 1998;104:413–21.
Dannhardt G, Kiefer W. Cyclooxygenase inhibitors – current status and future prospects. Eur J Med Chem. 2001;36:109–26.
Jaydess Summary of Product Characteristics. Bayer. July 2020. https://www.medicines.org.uk/emc/product/5297/smpc. Accessed Oct 2021.
European Medicines Agency. Guideline on Bioanalytical Method Validation. European Medicines Agency; 2015. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-bioanalytical-method-validation_en.pdf. Accessed 27 Sep 2021.
US FDA. FDA CDER – Bioanalytical Method Validation – Guidance for Industry. US FDA; 2018. https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf. Accessed 27 Sep 2021.
European Medicines Agency, GCP Inspectors Working Group. Reflection Paper for Laboratories that Perform the Analysis or Evaluation of Clinical Trial Samples. February 28, 2012. European Medicines Agency; 2012. https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/reflection-paper-laboratories-perform-analysis-evaluation-clinical-trial-samples_en.pdf. Accessed 27 Sep 2021.
Organisation for Economic Co-operation and Development. OECD Principles on Good Laboratory Practice (ENV/MC/CHEM(98)17). Organisation for Economic Co-operation and Development; 1997. https://one.oecd.org/document/ENV/MC/CHEM(98)17/en/pdf. Accessed 27 Sept 2021.
International Council for Harmonisation. ICH Harmonised Tripartite Guideline, Guideline for Good Clinical Practice E6 (R2). ICH. 2016. https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf. Accessed 27 Sep 2021.
García Rodríguez LA, Tacconelli S, Patrignani P. Role of dose potency in the prediction of risk of myocardial infarction associated with nonsteroidal anti-inflammatory drugs in the general population. J Am Coll Cardiol. 2008;52:1628–36.
Indomethacin Summary of Product Characteristics. Ratiopharm. May 2013. https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/48289.pdf. Accessed Jul 2021.
INDOCIN prescribing information. March 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/016059s100lbl.pdf. Accessed Oct 2021.
Bastianelli C, Farris M, Rosato E, Varliero F, Del Savio MC, Facchinetti F, Grandi G. The use of different doses levonorgestrel-releasing intrauterine system (LNG-IUS): real-world data from a multicenter Italian study. Eur J Contracept Reprod Health Care. 2022;27:16–22.
Grandi G, De Fata R, Varliero F, Del Savio MC, Facchinetti F. Contemporary prescriptions pattern of different dose levonorgestrel-releasing intrauterine systems in an Italian service for family planning. Gynecol Endocrinol. 2020;36(12):1086–9.
Duckitt K, Collins S. Menorrhagia. BMJ Clin Evid. 2012;2012:0805.
Bateson D, Harvey C, Trinh L, Stewart M, Black KI. User characteristics, experiences and continuation rates of copper intrauterine device use in a cohort of Australian women. Aust N Z J Obstet Gynaecol. 2016;56(6):655–61.
Jaydess Prescribing Information. Bayer. July 2021. https://labeling.bayerhealthcare.com/html/products/pi/Skyla_PI.pdf. Accessed Oct 2021.
Acknowledgements
The authors would like to thank Isabel Reinecke (Bayer AB, Sweden) for providing additional insight and guidance on the PK methods and contributing to the development of the manuscript concept. Medical writing assistance was provided by Highfield, Oxford, UK, with funding from Bayer AG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The original phase II study was funded by Bayer AG, Berlin, Germany.
Conflict of interest
Birte Maria Hofmann, Lueder M. Fels, Stefan Klein and Bernhard Lindenthal are employees of Bayer AG, Berlin. Germany. Manja Ahola and Jyrki Pihlaja are employees of Bayer OY, Turku, Finland.
Ethics approval
The original phase II study was registered at https://clinicaltrials.gov/ct2/show/NCT03562624, clinical trial registration number NCT03562624. Approvals were obtained from the Institutional Review Boards and Independent Ethics Committees for each participating center and the study was conducted in compliance with the Declaration of Helsinki and Good Clinical Practice guidelines.
Consent to participate
All participants provided written, informed consent prior to study start.
Consent for publication
Not applicable.
Code availability
Not applicable.
Availability of data and material
Upon request from qualified scientific and medical researchers, Bayer (the study sponsor) will share patient-level clinical trial data, study-level clinical trial data, and protocols from clinical trials, as necessary for conducting legitimate research. Interested researchers can use www.clinicalstudydatarequest.com to request access to anonymized patient-level data and supporting documents from clinical studies to conduct further research that can help advance medical science or improve patient care. Data access will be granted to anonymized patient-level data, protocols, and clinical study reports after approval by an independent scientific review panel. Bayer is not involved in the decisions made by the independent review panel. Bayer will take all necessary measures to ensure that patient privacy is safeguarded.
Author contributions
Birte M. Hofmann, Lueder Fels, Stefan Klein, and Bernhard Lindenthal participated in the development of the study design, and analysis and critical discussion of data. Manja Ahola and Jyrki Pihlaja participated in the conduct of the in vitro characterization analyses and critical interpretation of data outputs. Michal Zvolanek participated in critical discussion of data. All authors contributed to the initial manuscript draft and critically appraised all subsequent drafts. All authors read and approved the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hofmann, B.M., Ahola, M., Fels, L.M. et al. Development of an Intrauterine Device Releasing Both Indomethacin and Levonorgestrel During the First Months of Use: Pharmacokinetic Characterization in Healthy Women. Clin Pharmacokinet 62, 113–126 (2023). https://doi.org/10.1007/s40262-022-01201-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01201-7