Abstract
Introduction
The dosages of many medications require adjustment for renal function. There is debate regarding which equation, the Chronic Kidney Disease Epidemiology (CKD-EPI) equation vs. the Cockcroft–Gault (CG) equation, should be recommended to estimate glomerular filtration rate.
Methods
We used a mathematical simulation to determine how patient characteristics influence discrepancies between equations and analyzed clinical data to demonstrate the frequency of such discrepancies in clinical practice. In the simulation, the modifiable variables were sex, age, serum creatinine, and weight. We considered estimated glomerular filtration rate results in mL/min, deindexed for body surface area, because absolute excretory function (rather than per 1.73 m2 body surface area) determines the rate of filtration of a drug at a given plasma concentration. An absolute and relative difference of maximum (±) 10 mL/min and 10 %, respectively, were considered concordant. Clinical data for patients aged over 60 years (n = 9091) were available from one hospital and 25 private laboratories.
Results
In the simulation, differences between the two equations were found to be influenced by each variable but age and weight had the biggest effect. Clinical sample data demonstrated concordance between CKD-EPI and CG results in 4080 patients (45 %). The majority of discordant results reflected a CG result lower than the CKD-EPI equation. With aging, the CG result became progressively lower than the CKD-EPI result. When weight increased, the opposite occurred.
Discussion
The choice of equation for excretory function adjustment of drug dosage will have different implications for patients of different ages and body habitus.
Conclusions
The optimum equation for drug dosage adjustment should be defined with consideration of individual patient characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is debate regarding whether the Cockcroft–Gault (CG) equation or the Chronic Kidney Disease Epidemiology (CKD-EPI) equation should be used for drug dosage adjustment. |
We illustrate both from a simulation and clinical data that age and weight are the main predictors of discrepancies between CG and CKD-EPI equation results. |
Optimum dosage adjustment strategies should be defined according to age and weight. |
1 Introduction
Excretory renal function plays a fundamental role both in the pharmacokinetics and pharmacodynamics of several drugs. This is particularly the case for water-soluble compounds and/or their active metabolites. Even for non-renally excreted drugs, severe chronic kidney disease can modify the pharmacokinetics by several mechanisms [1–4]. For this reason, it is now recommended that both pharmacokinetics and pharmacodynamics of every new drug be studied in the context of chronic kidney disease [5, 6]. Dosage adjustment according to excretory renal function is required for many medications. However, there is a debate in the literature regarding the best way to estimate excretory function or glomerular filtration rate (GFR) for the purpose of pharmacotherapy [7–11]. Ideally, GFR should be measured by a so-called reference method such as urinary or plasma clearance of inulin, 51Cr-EDTA, or iohexol. These methods are, however, difficult to implement in daily practice and GFR is thus estimated by creatinine-based equations [12]. Several publications have illustrated potential discrepancies in estimated GFR (eGFR) results and thus in dosage prescription if different equations are used [7, 8, 10, 13–38]. For drug dosage adjustment, the sharpest debate consists in choosing between the Cockcroft–Gault (CG) equation [39], frequently promoted by clinical pharmacologists and geriatricians, and the Chronic Kidney Disease Epidemiology (CKD-EPI) equation, promoted by nephrologists [40, 41]. From the nephrological point of view, the superiority of the CKD-EPI equation over the CG equation to estimate GFR is easy to demonstrate in the general population [12, 40–42]. Moreover, this equation truly estimates GFR, whereas the CG equation estimates creatinine clearance (eClCr), which, in itself, is only a poor estimation of real GFR. Indeed, eClCr overestimates GFR because of the contribution of tubular creatinine secretion [12, 43]. Finally, sensu stricto, the CG equation cannot be used with modern and calibrated serum creatinine (SCr) values whereas the CKD-EPI equation can be used with all creatinine assays traceable to isotope dilution mass spectrometry (IDMS) [40, 44–46]. Conversely, there are arguments to support the case for applying the CG equation [2, 47–50]. Indeed, the CG equation is the equation that has been used to elaborate drug dosage adjustments for the vast majority of drugs [22, 26, 48–51]. Furthermore, the CG equation better predicts the risk of adverse events for several drugs, notably cardiovascular therapies. This may reflect the presence of the variable ‘body weight’ in the CG equation, not in the CKD-EPI equation [10, 48, 52]. The CG equation has been reported to give systematically lower eClCr values than are obtained for eGFR with CKD-EPI, particularly in the older population [53, 54]. This is despite the fact that eClCr (reflecting filtration plus creatinine secretion) is greater than GFR, reflecting an underestimation bias of CG in older subjects [55]. However, this underestimation will lead to a more protective behavior in terms of drug dosage in this frail population [20, 21].
The goal of this work is to define the discrepancies that would impact drug dosage adjustment if the CKD-EPI equation vs. CG equation was applied. Two complementary strategies are used: (1) a mathematical simulation relating the characteristics of patients to discrepancies between the two equations and (2) analysis of clinical data to determine both the frequency and amplitude of these discrepancies in clinical practice according to patient demographic characteristics.
2 Methods
2.1 Theoretical Simulation
We undertook a simulation study showing the differences observed between CKD-EPI and CG results when variables involved in these equations are modified. In this simulation, the modifiable variables were sex, age, SCr, weight, and height (and by consequence body surface area [BSA]) [39, 41, 56]. We modified: age from to 20 to 80 years (with 10-year intervals), weight from 25 to 125 kg (with 5-kg intervals), and SCr from 0.5 to 3.0 mg/dL (44–264 µmol/L) (with 0.1-mg/dL or 9-µmol/L intervals). Because the influence of the ‘height’ variable is less important from a mathematical and epidemiological point of view, we considered a constant height of 177 and 165 cm for men and women (reflecting populations means), respectively [57]. The CG and CKD-EPI equations are given in Table 1. In clinical nephrology, the results of these equations are generally used as indexed for BSA. However, in the context of drug dosing adjustment and as recommended by the International Guidelines in Nephrology (KDIGO for Kidney Disease/Improving Global Outcomes), the US Food and Drug Administration, and the European Medicines Agency, we considered the non-indexed GFR results in mL/min [5, 6, 47]. Therefore, the absolute non-indexed result is considered for the CG equation and the de-indexed value is calculated for the CKD-EPI equation (Table 1). Indeed, because drug adjustment is the quintessence of personalized medicine, it seems logical to consider the GFR of the subject and not the GFR the subject would have if his/her BSA were 1.73 m2 [9, 58].
In this work, we consider both absolute and relative differences between equation results. We calculated absolute difference as the difference between CG results and CKD-EPI results. A negative result thus means that the CG result is lower than the CKD-EPI result. The relative difference was calculated as the absolute difference divided by the mean of the CG and CKD-EPI results. An absolute difference threshold of maximum (±) 10 mL/min and a relative difference of maximum 10 % were considered as acceptable. The choice of such thresholds is not purely arbitrary. Indeed, 10 % is the biological variation of measured GFR observed in the literature and 10 mL/min is the acceptable precision recommended for estimating GFR (when compared with measured GFR) [59, 60]. The implications of these absolute and relative thresholds will vary with GFR. Indeed, at a GFR of 10 mL/min, a relative difference of 10 % (i.e., 1 mL/min) and an absolute difference of 10 mL/min are not relevant.
In the simulation figures, red color corresponds to cases where the CG equation gives discordantly lower values than the CKD-EPI equation, blue color corresponds to cases where CG gives higher results, and green color corresponds to cases where results are concordant, i.e., within ±10 % or ±10 mL/min.
2.2 Clinical Data
In the second part of this work, we studied the prevalence of discrepancies observed from clinical data. We analyzed results from two different laboratories. The first laboratory cohort (LabU) was from a university hospital in France (Grenoble). SCr was measured by an enzymatic and IDMS-traceable method (Siemens Healthcare Diagnostics, Tarrytown, NY) [44]. Only data from hospitalized patients were considered. The second laboratory cohort (LabC) was obtained in a private laboratory (Oriade group) including 25 collecting centers in France (Grenoble and outskirts). SCr was measured by an enzymatic and IDMS traceable method (Roche Diagnostics, Mannheim, Germany) [44]. From these two laboratories, we systematically collected all data from subjects aged older than 60 years. We pooled the results from both laboratories to cover the expected creatinine range but limited the analysis of SCr results between 0.5 and 3.0 mg/dL (44–264 µmol/L) to be consistent with the simulation.
2.3 Statistics
Relative difference was calculated as the difference divided by the average of both equations. Descriptive statistics are presented as median (interquartile range). In Table 2, we used hypothesis tests (Fisher’s Exact test for proportions, t tests for the continuous variables) to detect statistical significant differences in variables between groups of patients with relative differences between CG and CKD-EPI of less than 10 % (n = 4080, the group of patients considered with equivalent or concordant eGFR estimates) and with relative differences between CG and CKD-EPI of more than 10 % (the group of patients considered with discordant eGFR estimates), subdivided in a subgroup where CG exceeds CKD-EPI by more than 10 % (n = 438) and in a subgroup where the CG result is more than 10 % lower than CKD-EPI (n = 4573). P values are expressed for comparisons of the concordant group with the discordant subgroups.
A multilinear regression model was used to explain the variation in relative differences, using sex, age, weight, height, and SCr levels as independent explanatory variables. R 2 (coefficient of determination) is presented as the percentage of explained variation and as measure for the goodness of fit. Statistical significance was considered at the 5 % significance level.
3 Results
3.1 Theoretical Simulation
Figure 1 shows the potential discordances (1A graph is absolute difference and 1B graph is relative difference) between CKD-EPI and CG at a fixed age of 70 years for men (upper graph) and women (lower graph).
Potential discordances between CKD-EPI and CG at a fixed age of 70 years for men (upper graph) and women (lower graph). Creatinine values are expressed in mg/dL. To convert in µmol/L, multiply by 88. Graphs are (a) absolute difference and (b) relative difference. Red color corresponds to cases where the CG equation gives discordantly lower values than the CKD-EPI equation, blue color corresponds to cases where the CG equation gives higher results, and green color corresponds to cases where results are concordant, i.e., within ±10 % or ±10 mL/min. CG Cockcroft–Gault, CKD-EPI chronic kidney disease epidemiology
For 70-year-old male subjects, the following results were obtained: (1) when weight was above 105 kg, CG was always greater than CKD-EPI (no matter the SCr), and discordantly higher (>10 mL/min) in 75 % of the SCr range (0.5–3.0 mg/dL or 44–264 µmol/L); (2) among subjects with weight between 65 and 100 kg, 86 % of this weight range (no matter the SCr) had differences between CG and CKD-EPI within 10 mL/min, only 8 % showed discordantly higher CG and 6 % showed discordantly lower CG than CKD-EPI; (3) conversely, at low body weight (25–55 kg), CG was always lower than CKD-EPI, with about 50 % of this weight range discordantly lower (no matter the SCr), rising to nearly 100 % of the cases when SCr was in the normal range (0.6–1.2 mg/dL or 53–106 µmol/L).
For 70-year-old female subjects, similar results were obtained: (1) when body weight was above 85 kg, CG was always greater than CKD-EPI (no matter the SCr), and discordantly higher (>10 mL/min) in 74 % of the SCr range (0.5–3.0 mg/dL or 44–264 µmol/L); (2) for body weight between 50 and 80 kg, about 94 % of this weight range (no matter the SCr) had differences between CG and CKD-EPI within 10 mL/min, only 2 % showed discordantly higher CG and 4 % showed discordantly lower CG than CKD-EPI; and (3) conversely, at low weight (25–45 kg), CG was always smaller than CKD-EPI, with about 30 % of this weight range discordantly smaller (no matter the SCr), raising to nearly 100 % of this weight range when SCr was in the normal range (0.5–1.0 mg/dL or 44–88 µmol/L).
In Figs. 2 and 3, we modified age from 50 to 80 years for men and observed absolute and relative differences, respectively. Clearly, concordance between the equations increased with aging (green cases) when absolute differences were considered. The same pattern was observed in women (data not shown). If relative differences were considered, the trend was less impressive. Furthermore, with aging, we observed that the proportion of discordantly lower CG results (red cases) increased whereas the cases with discordantly higher CG results (blue cases) decreased.
In Fig. 3 (relative difference for male subjects), the yellow rectangle corresponds to subjects with normal SCr values (0.6–1.2 mg/dL or 53–106 µmol/L) and normal weights (60–85 kg). It is interesting to note that these ‘normal’ subjects had mostly concordant results (green cases) between the two equations at age 50 years and younger, but that discrepancies between the two equations results increased with aging, the majority of CG results being discordantly lower than the CKD-EPI equations (more red cases in these normal subjects). The same observation was made in women (data not shown).
In CKD patients (SCr 1.5–3 mg/dL or 132–264 µmol/L), the simulations showed, as expected, different results if absolute or relative differences are considered. Globally, when absolute differences were considered, the simulation showed that concordance between the two equations increased with aging, except in male subjects with low weight (<60 kg). If relative differences were considered, the higher concordance between equations with aging remained true but only in subjects with normal weight (within 60–85 kg). The concordance between relative differences was very low (between 0 and 50 %) for female subjects (independent of weight) and for male subjects with extremely low and high body weight.
3.2 Clinical Data
From the two laboratories, 9535 SCr results from subjects aged older than 60 years were available with limited anthropometric information (sex, height, weight, and age). Among these, 9091 samples had SCr measured between 0.5 and 3 mg/dL (44–264 µmol/L) and were thus included in the present analysis. Among these 9091 results, 48 % were from women. Median age was 71 [interquartile range: 66; 78] years. Median weight and height were 72 [62; 82] kg and 167 [160; 173] cm, respectively. Median SCr was 0.95 [0.80; 1.14] mg/dL (84 [70; 100] µmol/L) and median eGFR by CKD-EPI and eClCr by CG were 65 [51; 81] and 74 [59; 88] mL/min, respectively. Among these 9091 results, 4080 (45 %) had CKD-EPI and CG results within ±10 % and were thus considered concordant. The vast majority of discordant results reflected a CG equation result discordantly lower than the CKD-EPI equation (n = 4573, 95 %), whereas only 438 (5 %) subjects had a CKD-EPI equation result lower than the CG equation result. Table 2 shows the characteristics of these subjects. Most analyzed variables are actually significantly different for patients with discordant vs. concordant results, but the most marked difference is the median weight: 78 [70; 87] kg in subjects with concordant results, 95 [85; 109] kg in subjects with CG greater than CKD-EPI and 65 [57; 72] kg in subjects with CKD-EPI greater than CG.
We analyzed the relative difference between CG and CKD-EPI results according to the different anthropometric variables, i.e., sex, height, weight, age, and SCr. By least-squares multiple regression, we showed that all variables explained 88 % of the variation in relative difference between the two equations (R 2-adjusted = 0.88). Among these variables, age (r partial = −0.82) and weight are clearly the most important (r partial = 0.88).
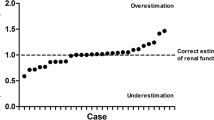
With aging (combining both sexes), the relative difference between CG and CKD-EPI results became more negative. In other words, the CG results were progressively lower in comparison to CKD-EPI results with aging (Fig. 4). On average, the effect was zero at the age of 60 years, but CKD-EPI exceeded CG with a nearly linear increase, reaching an overestimation of 40 % at the age of 95 years.
Regarding body weight (combining both sexes), the relative difference between CG and CKD-EPI results increased when weight increased. In other words, the CG results were lower in comparison to CKD-EPI results at low weight values. When weight increased, the difference between the two equations decreased and, in heavier subjects, the CG result was superior to CKD-EPI results (Fig. 5). On average, the effect was zero around a weight of 90 kg. The majority of subjects had a weight below 90 kg and, for them, CKD-EPI exceeded CG by 0–40 %. However, a minority of the cohort had weight above 90 kg and, in these specific patients, CKD-EPI was less than CG by 0–20 %. People with a very low weight (<50 kg) were most likely to be discordantly classified with a CKD-EPI result >20 % higher than their CG result. The effects of SCr on the discrepancy between CKD-EPI and CG were much less than those of age and weight (Fig. 6). In fact, there was no clear relationship between SCr and the CKD-EPI/CG difference.
4 Discussion
We provide a simple mathematical illustration of potential differences, absolute or relative, between the non-indexed CG equation and the de-indexed CKD-EPI equations (in mL/min), which are recommended for drug dosage adjustment [5, 6, 47]. Our clinical data support the conclusion that differences between the two equations are potentially influenced by each variable included in these equations: sex, age, weight, height, and SCr. Among these variables, age and weight are the most important and will systematically impact the results of the equations. The prevalence of excretory impairment in the older population and their resulting vulnerability to overdosage is a major driver for optimizing dosage adjustment strategies in this population. The assertion, frequently found in the geriatric literature, that CG must be favored because it gives systematically lower results, and thus prevents overdosage, is an oversimplification [20, 21]. We confirm using de-indexed eGFR, that CG results are lower than CKD-EPI in these subjects. However, this assertion is not true in some obese geriatric patients, even if these patients are clearly not the majority. Our clinical database was limited to subjects aged older than 60 years, but as shown by our simulation, the proportion of discordant results increases with younger age and greater body weight. This last point is important as the epidemic of obesity is well known in the general non-geriatric population. Therefore, the general recommendation to favor CG based on geriatric data would potentially have different implications for drug concentrations in younger subjects, especially if weight is high. In the context of drug dosage adjustment strategies, a personalized approach is necessary.
All creatinine-based equations have their own limitations and lack of precision to estimate true GFR [12]. They also require a steady-state situation [61]. For specific therapeutic drugs that are potentially nephrotoxic and have a tight therapeutic window such as cisplatin, it is our opinion that the measurement of real GFR with a reference method has added value, even if proof is still indirect [12, 25–27, 30, 32, 33, 35]. It is also our opinion that drugs that are easily monitored by plasma measurement may be favored in the context of CKD. In other cases, knowing the age, weight, height, and SCr of the patients, the Excel sheet (available in the Supplementary Material) can calculate the absolute and relative difference between the two equations, flagging up discordant cases. If results are concordant, the clinician can reasonably apply drug dosage recommendations available in the literature. If discrepancies occur, it would be important to consider the characteristics of the patients and the safety profile of the drug considered. For highly effective concentration-dependent drugs (such as antibiotics), the risk of under-dosage could be as important as the risk of over-dosage, especially if the risk of nephrotoxicity is relatively low. In such cases, it could be more efficient to consider the equation that gives the higher GFR results. Conversely, it could be better to recommend adjusting the dosage of a drug to the equation, giving the lower result if the prescription concerns potentially nephrotoxic drugs [49, 62].
There are limitations to our study. Without measured GFR data, we are not able to assert which equation must be used for a specific patient. This remains a simulation and our clinical data are probably representative neither of the French general population nor of populations from other countries. Regarding the simulation, we gave both absolute and relative differences but the general conclusions and the relevance of these differences may vary according to the GFR level. Indeed, a relative difference of 10 % is probably more relevant from a practical and clinical point of view at low GFR levels, whereas absolute and relative differences are pertinent (and in fact exactly the same for a GFR value of 100 mL/min) at relatively high GFR. At low GFR, the implications of both relative and absolute differences should be considered. By presenting absolute and relative changes in our analysis, we have illustrated the implications of demographics on CG/CKD-EPI discrepancies across the spectrum of excretory function. The choice of threshold at 10 mL/min or 10 % can be criticized as not relevant for every drug. Indeed, some dosage adjustments are guided simply by CKD stage. However, 10 mL/min is a difference in GFR that will have a substantial effect on plasma concentrations of some drugs. This is especially true in oncologic therapy where the dosage of cisplatin for example can be significantly (under-dosing or over-dosing) modified for a difference in GFR of 10 mL/min or 10 % [32, 33]. Moreover, it would have been impractical to propose simulations for the range of GFR discrepancies relevant to every drug.
Discordances between equations could be theoretically more important in other ethnicities, especially in African-Americans for whom an ethnic coefficient is required in the CKD-EPI equation, but not in the CG equation [63]. Finally, we did not discuss the potential interest of cystatin C-based equations in this context of drug dosage adjustment, as current data are scarce and controversial [23, 35, 64, 65].
5 Conclusion
Age and body weight are the main variables explaining discrepancies between the equations. Obviously, in the context of drug prescription, an individualization is necessary. Our mathematical tool can help physicians, alerting them when large discrepancies exist for a given patient in results calculated for CKD-EPI vs. CG results. Knowing such discrepancies, the clinician can either adjust his/her prescription to balance the risk–benefit of the drug or measure real GFR, especially if the therapeutic window of the drug is narrow. We illustrated potential discrepancies between CKD-EPI and CG with implications for drug dosage adjustment. The European Medicines Agency recommends that pharmacokinetic studies be performed for new drugs with measured GFR by a reference method in the context of CKD [5]. Our findings demonstrate the need to define pharmacokinetics in relation to estimation equations across the spectrum of patients’ age and weight so that appropriate adjustment can be applied in clinical practice.
References
Dreisbach AW, Flessner MF. Drug metabolism and chronic kidney disease. In: Kimmel PL, Rosenberg, MK, editors. Chronic renal disease. Academic Press; 2014. p. 674–81.
Verbeeck RK, Musuamba FT. Pharmacokinetics and dosage adjustment in patients with renal dysfunction. Eur J Clin Pharmacol. 2009;65:757–73.
Aymanns C, Keller F, Maus S, Hartmann B, Czock D. Review on pharmacokinetics and pharmacodynamics and the aging kidney. Clin J Am Soc Nephrol. 2010;5:314–27.
Elinder CG, Barany P, Heimburger O. The use of estimated glomerular filtration rate for dose adjustment of medications in the elderly. Drugs Aging. 2014;31:493–9.
EMA. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/02/WC500162133.pdf. Accessed 8 July 2016.
FDA. 2010. http://www.fda.gov/downloads/Drugs/Guidances/UCM204959.pdf. Accessed 8 July 2016.
Stevens LA, Nolin TD, Richardson MM, Feldman HI, Lewis JB, Rodby R, et al. Comparison of drug dosing recommendations based on measured GFR and kidney function estimating equations. Am J Kidney Dis. 2009;54:33–42.
Park EJ, Wu K, Mi Z, Dong T, Lawrence JP, Ko CW, et al. A systematic comparison of Cockcroft-Gault and modification of diet in renal disease equations for classification of kidney dysfunction and dosage adjustment. Ann Pharmacother. 2012;46:1174–87.
Bouquegneau A, Vidal-Petiot E, Moranne O, Mariat C, Boffa JJ, Vrtovsnik F, et al. Creatinine-based equations for the adjustment of drug dosage in an obese population. Br J Clin Pharmacol. 2016;81:349–61.
Melloni C, Peterson ED, Chen AY, Szczech LA, Newby LK, Harrington RA, et al. Cockcroft-Gault versus modification of diet in renal disease: importance of glomerular filtration rate formula for classification of chronic kidney disease in patients with non-ST-segment elevation acute coronary syndromes. J Am Coll Cardiol. 2008;51:991–6.
Corsonello A, Pedone C, Lattanzio F, Onder G, Inc A. Association between glomerular filtration rate and adverse drug reactions in elderly hospitalized patients: the role of the estimating equation. Drugs Aging. 2011;28:379–90.
Delanaye P, Mariat C. The applicability of eGFR equations to different populations. Nat Rev Nephrol. 2013;9:513–22.
Wargo KA, Eiland EH III, Hamm W, English TM, Phillippe HM. Comparison of the modification of diet in renal disease and Cockcroft-Gault equations for antimicrobial dosage adjustments. Ann Pharmacother. 2006;40:1248–53.
Golik MV, Lawrence KR. Comparison of dosing recommendations for antimicrobial drugs based on two methods for assessing kidney function: Cockcroft-Gault and modification of diet in renal disease. Pharmacotherapy. 2008;28:1125–32.
Hermsen ED, Maiefski M, Florescu MC, Qiu F, Rupp ME. Comparison of the modification of diet in renal disease and Cockcroft-Gault equations for dosing antimicrobials. Pharmacotherapy. 2009;29:649–55.
Okparavero AA, Tighiouart H, Krishnasami Z, Wyatt CM, Graham H, Hellinger J, et al. Use of glomerular filtration rate estimating equations for drug dosing in HIV-positive patients. Antivir Ther. 2013;18:793–802.
Gouin-Thibault I, Pautas E, Mahe I, Descarpentries C, Nivet-Antoine V, Golmard JL, et al. Is Modification of Diet in Renal Disease formula similar to Cockcroft-Gault formula to assess renal function in elderly hospitalized patients treated with low-molecular-weight heparin? J Gerontol A Biol Sci Med Sci. 2007;62:1300–5.
Gill J, Malyuk R, Djurdjev O, Levin A. Use of GFR equations to adjust drug doses in an elderly multi-ethnic group: a cautionary tale. Nephrol Dial Transplant. 2007;22:2894–9.
Healy MF, Speroni KG, Eugenio KR, Murphy PM. Adjusting eptifibatide doses for renal impairment: a model of dosing agreement among various methods of estimating creatinine clearance. Ann Pharmacother. 2012;46:477–83.
Maccallum PK, Mathur R, Hull S a, Saja K, Green L, Morris JK, et al. Patient safety and estimation of renal function in patients prescribed new oral anticoagulants for stroke prevention in atrial fibrillation: a cross-sectional study. BMJ Open 2013;3:e003343.
Helldén A, Odar-Cederlöf I, Nilsson G, Sjöviker S, Söderström A, Von Euler M, et al. Renal function estimations and dose recommendations for dabigatran, gabapentin and valaciclovir: a data simulation study focused on the elderly. BMJ Open. 2013;3:e002686.
Hijazi Z, Hohnloser SH, Oldgren J, Andersson U, Connolly SJ, Eikelboom JW, et al. Efficacy and safety of dabigatran compared with warfarin in relation to baseline renal function in patients with atrial fibrillation: a RE-LY (randomized evaluation of long-term anticoagulation therapy) trial analysis. Circulation. 2014;129:961–70.
Chin PK, Wright DF, Zhang M, Wallace MC, Roberts RL, Patterson DM, et al. Correlation between trough plasma dabigatran concentrations and estimates of glomerular filtration rate based on creatinine and cystatin C. Drugs R D. 2014;14:113–23.
de Lemos ML, Hsieh T, Hamata L, Levin A, Swenerton K, Djurdjev O, et al. Evaluation of predictive formulae for glomerular filtration rate for carboplatin dosing in gynecological malignancies. Gynecol Oncol. 2006;103:1063–9.
Ainsworth NL, Marshall A, Hatcher H, Whitehead L, Whitfield GA, Earl HM. Evaluation of glomerular filtration rate estimation by Cockcroft-Gault, Jelliffe, Wright and Modification of Diet in Renal Disease (MDRD) formulae in oncology patients. Ann Oncol. 2012;23:1845–53.
Craig AJ, Samol J, Heenan SD, Irwin AG, Britten A. Overestimation of carboplatin doses is avoided by radionuclide GFR measurement. Br J Cancer. 2012;107:1310–6.
Hartlev LB, Boeje CR, Bluhme H, Palshof T, Rehling M. Monitoring renal function during chemotherapy. Eur J Nucl Med Mol Imaging. 2012;39:1478–82.
Tsao CK, Moshier E, Seng SM, Godbold J, Grossman S, Winston J, et al. Impact of the CKD-EPI equation for estimating renal function on eligibility for cisplatin-based chemotherapy in patients with urothelial cancer. Clin Genitourin Cancer. 2012;10:15–20.
Kaag D. Carboplatin dose calculation in lung cancer patients with low serum creatinine concentrations using CKD-EPI and Cockcroft-Gault with different weight descriptors. Lung Cancer. 2013;79:54–8.
Dooley MJ, Poole SG, Rischin D. Dosing of cytotoxic chemotherapy: impact of renal function estimates on dose. Ann Oncol. 2013;24:2746–52.
Pal SK, Ruel N, Villegas S, Chang M, DeWalt K, Wilson TG, et al. CKD-EPI and Cockcroft-Gault equations identify similar candidates for neoadjuvant chemotherapy in muscle-invasive bladder cancer. PLoS One. 2014;9:e94471.
Shepherd ST, Gillen G, Morrison P, Forte C, Macpherson IR, White JD, et al. Performance of formulae based estimates of glomerular filtration rate for carboplatin dosing in stage 1 seminoma. Eur J Cancer. 2014;50:944–52.
Cathomas R, Klingbiel D, Geldart TR, Mead GM, Ellis S, Wheater M, et al. Relevant risk of carboplatin underdosing in cancer patients with normal renal function using estimated GFR: lessons from a stage I seminoma cohort. Ann Oncol. 2014;25:1591–7.
Bennis Y, Savry A, Rocca M, Gauthier-Villano L, Pisano P, Pourroy B. Cisplatin dose adjustment in patients with renal impairment, which recommendations should we follow? Int J Clin Pharm. 2014;36:420–9.
Chew-Harris JS, Florkowski CM, George PM, Endre ZH. Comparative performances of the new chronic kidney disease epidemiology equations incorporating cystatin C for use in cancer patients. Asia Pac J Clin Oncol. 2014;11:142–51.
Moranville MP, Jennings HR. Implications of using modification of diet in renal disease versus Cockcroft-Gault equations for renal dosing adjustments. Am J Heal Syst Pharm. 2009;66:154–61.
McFarland MS, Markley BM, Zhang P, Hudson JQ. Evaluation of modification of diet in renal disease study and Cockcroft-Gault equations for sitagliptin dosing. J Nephrol. 2012;25:515–22.
Lessard BA, Zaiken K. Comparison of equations for dosing of medications requiring renal adjustment. J Am Pharm Assoc. 2013;53:54–7.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
KDIGO 2012. Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P. Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol. 2005;16:763–73.
Millar JA. The Cockroft and Gault formula for estimation of creatinine clearance: a friendly deconstruction. N Z Med J. 2012;125:119–22.
Piéroni L, Delanaye P, Boutten A, Bargnoux AS, Rozet E, Delatour V, et al. A multicentric evaluation of IDMS-traceable creatinine enzymatic assays. Clin Chim Acta. 2011;412:2070–5.
Delanaye P, Cavalier E, Cristol JP, Delanghe JR. Calibration and precision of serum creatinine and plasma cystatin C measurement: impact on the estimation of glomerular filtration rate. J Nephrol. 2014;27:467–75.
Earley A, Miskulin D, Lamb EJ, Levey AS, Uhlig K. Estimating equations for glomerular filtration rate in the era of creatinine standardization: a systematic review. Ann Intern Med. 2012;156:785–95.
Matzke GR, Aronoff GR, Atkinson AJ Jr, Bennett WM, Decker BS, Eckardt K-UU, et al. Drug dosing consideration in patients with acute and chronic kidney disease: a clinical update from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2011;80:1122–37.
Spruill WJ, Wade WE, Cobb HH III. Comparison of estimated glomerular filtration rate with estimated creatinine clearance in the dosing of drugs requiring adjustments in elderly patients with declining renal function. Am J Geriatr Pharmacother. 2008;6:153–60.
Nyman HA, Dowling TC, Hudson JQ, Peter WL, Joy MS, Nolin TD. Comparative evaluation of the Cockcroft-Gault equation and the modification of diet in renal disease (MDRD) study equation for drug dosing: an opinion of the Nephrology Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy. 2011;31:1130–44.
Nutescu EA, Spinler SA, Wittkowsky A, Dager WE. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43:1064–83.
Dowling TC, Matzke GR, Murphy JE, Burckart GJ. Evaluation of renal drug dosing: prescribing information and clinical pharmacist approaches. Pharmacotherapy. 2010;30:776–86.
Dufour B, Toussaint-Hacquard M, Kearney-Schwartz A, Manckoundia MD, Laurain MC, Joly L, et al. Glomerular filtration rate estimated by Cockcroft-Gault formula better predicts anti-Xa levels than modification of the diet in renal disease equation in older patients with prophylactic enoxaparin. J Nutr Health Aging. 2012;16:647–52.
Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med. 2012;157:471–81.
Flamant M, Haymann JP, Vidal-Petiot E, Letavernier E, Clerici C, Boffa JJ, et al. GFR estimation using the Cockcroft-Gault, MDRD Study, and CKD-EPI equations in the elderly. Am J Kidney Dis. 2012;60:847–9.
Fotheringham J, Weatherley N, Kawar B, Fogarty DG, Ellam T. The body composition and excretory burden of lean, obese, and severely obese individuals has implications for the assessment of chronic kidney disease. Kidney Int. 2014;86:1221–8.
Du Bois D, Du Bois EF. A formula to estimate the approximative surface area if height and weight be known. Arch Intern Med. 1916;17:863–71.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Advance data from vital and health statistics; no 314. Hyattsville, Maryland: National Center for Health Statistics; 2000. www.cdc.gov/growthcharts.
Delanaye P, Krzesinski JM. Indexing of renal function parameters by body surface area: intelligence or folly? Nephron Clin Pract. 2011;119:c289–92.
Delanaye P, Cavalier E, Froissart M, Krzesinski J-MM. Reproducibility of GFR measured by chromium-51-EDTA and iohexol. Nephrol Dial Transplant. 2008;23:4077–8.
Stevens LA, Levey AS. Measured GFR as a confirmatory test for estimated GFR. J Am Soc Nephrol. 2009;20:2305–13.
Delanaye P, Cavalier E, Morel J, Mehdi M, Maillard N, Claisse G, et al. Detection of decreased glomerular filtration rate in intensive care units: serum cystatin C versus serum creatinine. BMC Nephrol. 2014;15:9.
Pai MP. Treatment of bacterial infections in obese adult patients: how to appropriately manage antimicrobial dosage. Curr Opin Pharmacol. 2015;24:12–7.
Delanaye P, Mariat C, Maillard N, Krzesinski JM, Cavalier E. Are the creatinine-based equations accurate to estimate glomerular filtration rate in african american populations? Clin J Am Soc Nephrol. 2011;6:906–12.
DeCarolis DD, Thorson JG, Marraffa RA, Clairmont MA, Kuskowski MA. Comparison of equations with estimate renal function to predict serum vancomycin concentration in patients with spinal cord injury: does the use of cystatin C improve accuracy? Ther Drug Monit. 2014;36:632–9.
Frazee EN, Rule AD, Herrmann SM, Kashani KB, Leung N, Virk A, et al. Serum cystatin C predicts vancomycin trough levels better than serum creatinine in hospitalized patients: a cohort study. Crit Care. 2014;18:R110.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Pierre Delanaye, Fabrice Guerber, André Scheen, Timothy Ellam, Antoine Bouquegneau, Dorra Guergour, Christophe Mariat, and Hans Pottel declare that they have no conflict of interest that might be relevant to the contents of this manuscript.
Additional information
H. Pottel and C. Mariat equally contributed as last senior author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Delanaye, P., Guerber, F., Scheen, A. et al. Discrepancies between the Cockcroft–Gault and Chronic Kidney Disease Epidemiology (CKD-EPI) Equations: Implications for Refining Drug Dosage Adjustment Strategies. Clin Pharmacokinet 56, 193–205 (2017). https://doi.org/10.1007/s40262-016-0434-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-016-0434-z