Abstract
Lithium has been used for the management of psychiatric illnesses for over 50 years and it continues to be regarded as a first-line agent for the treatment and prevention of bipolar disorder. Lithium possesses a narrow therapeutic index and comparatively minor alterations in plasma concentrations can have significant clinical sequelae. Several drug classes have been implicated in the development of lithium toxicity over the years, including diuretics and non-steroidal anti-inflammatory compounds, but much of the anecdotal and experimental evidence supporting these interactions is dated, and many newer medications and medication classes have been introduced during the intervening years. This review is intended to provide an update on the accumulated evidence documenting potential interactions with lithium, with a focus on pharmacokinetic insights gained within the last two decades. The clinical relevance and ramifications of these interactions are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Research and clinical evidence accumulated over the past 20 years has implicated many medication classes in the development of lithium toxicity, including diuretics, non-steroidal anti-inflammatory drugs, ACE inhibitors, angiotensin II receptor antagonists (blockers), antiepileptic drugs, and possibly antidepressants and antipsychotics. |
The majority of evidence associating medications with lithium toxicity consists of case reports, observational studies, and small prospective trials. Few controlled comparative studies have been published to date. |
Drug interactions with lithium can be somewhat unpredictable and caution is advised whenever any medication is combined with lithium, particularly in elderly populations and those with compromised renal function, electrolyte abnormalities, or dehydration. |
1 Introduction
Lithium salts have been administered for the treatment and prevention of mood disorders for over 60 years [1]. From the outset, it was evident that lithium was associated with a wide variety of potential toxicities but clinicians and researchers also realized that this medication demonstrated unprecedented therapeutic potential for ameliorating episodes of both mania and depression. Over time, other medications were identified that possessed mood-stabilizing properties and appeared to have a wider therapeutic index than lithium, leading to a sharp decline in the popularity of this older compound.
In recent years, the clinical utility of lithium has undergone a renaissance of sorts due, in part, to longitudinal data demonstrating that lithium had a more favorable effect on suicidality than other mood stabilizers [2, 3]. Newfound concerns about the safety and long-term efficacy of these compounds contributed to the ascension of lithium as well [4]. Today, lithium is regarded as a first-line agent for the prophylaxis of bipolar disorder, but the safe and efficacious use of this medication demands a comprehensive understanding of its pharmacokinetic disposition, adverse effect potential, and the relative risk (RR) of drug interactions [5, 6].
2 Pharmacology of Lithium
Lithium is a monovalent cation and the third element featured on the periodic table. It is quite abundant in nature, frequently found in groundwater, and the concentration of lithium circulating in the human body is approximately 2.5 µEq/L or roughly 1/500th of the recommended plasma level for a patient with bipolar disorder [7]. Interestingly, several studies have analyzed a potential association between the concentration of lithium in tap water and the incidence of violent behavior in society, consistently reporting that higher concentrations are correlated with less suicidality, homicidality, and rape [8–10]. Researchers have also uncovered compelling evidence that lithium may have neuroprotective effects, implying that it may have beneficial or prophylactic benefit for Alzheimer’s dementia and other neurodegenerative conditions [11]. Others have theorized that it may aid recovery from traumatic brain injury as well [12].
In spite of the relatively long history of the medicinal use of lithium, a single cogent explanation for its psychiatric effects remains elusive. Researchers laboring under the monoamine hypothesis for mood disorders have reported that lithium enhances serotonin activity by several mechanisms, including increased synthesis of the neurotransmitter, inhibition of presynaptic serotonin 5-HT1A autoreceptors, and downregulation of postsynaptic 5-HT2 receptors [13]. Evidence exists to suggest that lithium may facilitate norepinephrine release and enhance glutamatergic activity as well [14, 15]. Researchers have focused more intently on the effect of lithium on second messenger systems in recent years, reporting an inhibition of inositol monophosphatase and, ultimately, inositol depletion [16]. Lithium is also known to reduce protein kinase C activity, ultimately altering neurotransmission through effects on genomic expression [17]. There is also evidence to suggest that lithium may stimulate neurogenesis through indirect actions on neural growth factors [18].
3 Pharmacokinetics of Lithium
3.1 Absorption
Lithium is generally administered as an oral salt formulation containing either lithium carbonate (tablets or capsules in immediate-release or sustained-release preparations) or lithium citrate (liquid preparation). Both of these salt formulations dissociate in the upper gastrointestinal tract, releasing the lithium ion, which is rapidly and completely absorbed primarily through passive diffusion [19]. The absorption process is slowed somewhat by the presence of food in the stomach, which may explain the decrease in gastrointestinal adverse effects commonly reported when lithium is administered after meals [20]. Maximal concentrations of the immediate-release preparations are usually seen approximately 1–2 h after administration, and sustained-release preparations have been reported to peak 5–6 h after ingestion [21].
3.2 Distribution
As a water-soluble monovalent cation, lithium is not bound to plasma proteins and distributes widely throughout the body following oral absorption. The final volume of distribution for lithium approximates that of total body water (0.79 L/kg), but concentrations of the ion can vary substantially depending on the tissue or compartment sampled. The concentration of lithium in circulation (or the central compartment) is approximately twice that found in red blood cells, muscle or cerebrospinal fluid, and approximately equivalent to concentrations in heart or lung tissue [22, 23]. This complex and prolonged distribution phase is truly multicompartmental. For the purposes of pharmacokinetic modeling, however, lithium’s distribution is described as two-compartment, with the chaotic alpha phase lasting approximately 8 h, and the linear beta phase ensuing thereafter. The practical relevance of this distinction is that clinicians are advised to wait until the alpha phase has been completed until sampling from the central compartment (i.e., 10 h after oral administration).
Lithium must cross the blood–brain barrier to exert therapeutic effects but the process is delayed somewhat, with peak concentrations occurring approximately 24 h after oral administration There is much variability in regards to the ratio of concentrations in the central nervous system (CNS) to plasma, but brain concentrations are roughly 50 % lower than the periphery once steady state has been achieved [22]. Lithium concentrations also vary substantially within CNS compartments but the clinical significance of this phenomenon is unclear. The efflux of lithium out of the CNS is also delayed, resulting in a CNS terminal half-life that is 6–12 h longer than in plasma. This may explain, to some extent, the persistence of neurotoxicities long after plasma concentrations have dropped to subtherapeutic levels.
3.3 Elimination
Lithium is not metabolized and is eliminated almost entirely via renal means. Consequently, plasma concentrations are exquisitely sensitive to physiological factors effecting renal function such as age, dehydration, sodium balance, and hemodynamics. Lithium is filtered entirely by the glomerulus and 75 % of the ion is reabsorbed in the renal tubule [24]. As a result, lithium clearance equates to approximately one-quarter of the glomerular filtration rate (GFR). The majority of this reabsorption occurs in the proximal tubule in a manner very similar to the renal handling of sodium [25]. Lithium also appears to undergo distal reabsorption in the collecting duct [25].
The serum half-life of lithium is approximately 24 h in young healthy subjects, and steady-state dynamics are ordinarily achieved within 3–4 days in the central compartment [26, 27]. Individuals who are elderly or renally impaired may have terminal half-lives of 48 h or longer, and steady-state concentrations may not be achieved for a week or more.
3.4 Therapeutic Drug Monitoring
Due to the prolonged distribution phase, it is recommended that plasma samples be obtained at least 10 h after the last lithium dose [28]. Clinicians are also advised to verify that patients have achieved steady-state dynamics prior to obtaining samples (i.e., lithium dosed at regular intervals for minimum of 3 half-lives).
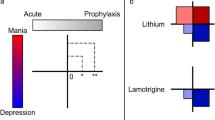
Controversies continue to exist regarding a recommended therapeutic range for lithium concentrations in the plasma [23]. Back in 1967, researchers Schou and Baastrup [29] recommended that clinicians maintain steady-state concentrations within a range of 0.6–1.5 mEq/L. Recent guidelines in Europe (from the National Institute for Health and Clinical Excellence [NICE]) recommend a much narrower plasma concentration of 0.6–0.8 mEq/L, while those published in the USA advocate for slowly titrating into a range of 0.5–1.2 mEq/L [30, 31]. As the risk of adverse effects clearly increases with higher concentrations, a reasonable approach for acute treatment may be to empirically titrate to a target steady-state concentration of 0.8 mEq/L and adjust dosing requirements based on tolerability and therapeutic effects in a patient-specific manner.
Recommendations also differ in regards to acute versus maintenance lithium treatment with some investigators suggesting that lower concentrations be maintained for prophylaxis (as opposed to active treatment). In an effort to resolve this controversy, a large prospective study was conducted that compared relapse rates for patients maintained at a concentration of 0.4–0.6 mEq/L versus those assigned to achieve a concentration of 0.8–1.0 mEq/L [32]. Patients in the lower concentration range were found to be three times more likely to relapse into manic states, supporting the maintenance of comparatively higher concentrations for optimal outcomes.
While there is clearly a correlation between plasma concentrations and both clinical and toxic effects, the therapeutic action of lithium is ultimately mediated in the CNS where quantification of concentrations is impractical at the present time. It is worthwhile to note, however, that researchers have successfully quantified CNS concentrations of lithium through magnetic resonance spectroscopy and reported stronger associations with brain levels than those found in the periphery [33].
As mentioned previously, lithium appears to have a relatively narrow therapeutic index, with symptoms of toxicity often manifest after relatively minor increases in plasma concentrations. Mild symptoms of acute toxicity include a worsening tremor, diarrhea, nausea, sedation, and confusion. These symptoms may progress to dysarthria, ataxia, delirium, arrhythmias, seizures, and acute renal failure as levels continue to increase. Lithium intoxication can be described as either acute or chronic in nature, with acute toxicity often precipitated by an overdose (intentional or accidental), and chronic toxicity developing over a period of several days or weeks as lithium accumulates in the peripheral compartments. Chronic toxicity appears to carry a much worse prognosis due to the saturation of peripheral compartments such as the cerebellum, and irreversible symptoms of toxicity may occur.
There are also pronounced differences in the sensitivity to lithium toxicity among patient populations. Sensitivity is particularly pronounced in elderly patients, who are often unable to tolerate plasma concentrations toward the upper limits of the recommended therapeutic range (e.g., >1.0 mEq/L) [34, 35]. Similarly, pediatric patients are often more inclined to experience adverse effects at plasma concentrations that are generally well-tolerated in adults [36].
4 Drug Interactions with Lithium
Given the remarkable sensitivity of individuals to fluctuating lithium concentrations and the plethora of conditions that may alter lithium disposition, it is not surprising that there is ample concern over the coadministration of medications that may alter lithium disposition and either precipitate toxicity or lead to relapse. As lithium is not metabolized, these interactions do not involve biotransformation through enzyme systems such as cytochrome P450. Most often, lithium interactions occur through the direct effect of other medications upon renal function and GFRs, which ultimately impacts its disposition and renal handling. The remainder of this article is devoted to a summary of the current medical literature documenting drug interactions that have been reported with concurrent lithium administration. Overall, the preponderance of evidence is circumstantial, consisting of case reports, retrospective observations, and a few small comparative trials, but as this body of literature has accumulated over the past 50 years, the RR of drug interactions posed by certain compounds has emerged and may guide us in optimizing the safe and efficacious use of this unique and invaluable psychotherapeutic agent.
For the purposes of this review, the author searched PubMed (1966–2015), EMBASE (1980–2015), Google Scholar®, and the Cochrane Library database using the MeSH terms lithium, toxicity, drug interactions, therapeutic drug monitoring, and their associated medication classes (e.g., diuretics, Non-steroidal anti-inflammatory drugs (NSAIDs), ACE inhibitors, Angiotensin II receptor antagonists (ARBs), Antiepileptic Drugs (AEDs), antidepressants, and antipsychotics). In addition, the author cross-checked references and citations from previous reviews of lithium toxicity, therapeutic drug monitoring, and drug interactions.
A summary of the medication classes and their risk of interactions with lithium is given in Table 1. Table 2 provides a definition of the risk ratings.
4.1 Diuretics
Some of the earliest evidence of drug interactions with lithium can be found with the coadministration of diuretics, though effects vary depending on the class of diuretics in question. Thiazide diuretics have been demonstrated to increase steady-state lithium concentrations by approximately 20–25 %, whereas loop diuretics and potassium-sparing diuretics appear to have less of an effect on lithium disposition under controlled conditions. Osmotic diuretics cause a more robust decrease in lithium concentrations and were once used as an antidote for lithium intoxication. A more indepth discussion of the effects of diuretics on the pharmacokinetics of lithium can be found in Sects. 4.1.1–4.1.5.
4.1.1 Thiazide Diuretics
Initial reports describing lithium intoxication in patients receiving thiazide diuretics began appearing in the 1970s, with chlorothiazide, hydrochlorothiazide, chlorthalidone, and bendrofluazide all implicated in the medical literature [37–40]. The precipitation of lithium toxicity was relatively rapid in these reports, and the symptoms usually reversed within a few days upon discontinuation. One notable exception to this pattern, however, can be found in the case report published by Macfie [38] where a 66-year-old developed serious neurologic sequelae after exposure to a combination diuretic (amiloride and hydrochlorothiazide) that persisted for the duration of the 7-week follow-up. In this case, as well as all others located in the literature, the absolute magnitude of lithium elevation was difficult to determine due to incomplete information reported on oral dosing and plasma sampling.
The impact of thiazide diuretics on lithium disposition was eventually studied in several small investigations that demonstrated a consistent and significant decline of 20–25 % in clearance values [41–45]. Petersen et al. [41] conducted the first open-label prospective trial in human models, describing the effects of long-term thiazide administration. Twenty-two subjects who had been receiving either hydroflumethiazide or bendrofluazide were given 600 mg oral dosages of lithium carbonate on two successive days and clearance values were compared to pharmacokinetic parameters obtained 2 months after stopping thiazides. The authors reported a mean 21 % decrease in lithium clearance (and corresponding 24 % increase in plasma concentrations) among patients receiving concurrent thiazides. Another small investigation examined the impact of chlorothiazide in four healthy volunteers, with a 26 % decrease in lithium clearance reported [42].
Himmelhoch et al. [43] published the results of a retrospective investigation of 12 subjects who had been receiving various dosages of chlorothiazide for nephrogenic diabetes insipidus. The authors calculated a 60 % decrease in lithium clearance values, though plasma sampling was conducted 3–4 h after oral dosing, a timeframe corresponding to the extensive distribution phase of the drug when pharmacokinetic interpretation is compromised.
In 1979, Jefferson and Kalin [44] conducted a more rigorous investigation of the impacts of diuretics on lithium disposition, exposing lithium-treated patients to furosemide and hydrochlorothiazide, respectively, in a crossover, open-label fashion . A total of five healthy young subjects completed the 6-week investigation. Lithium clearance values were not significantly different from baseline when furosemide (40 mg daily) was administered concurrently. However, the combination of hydrochlorothiazide (50 mg daily) and lithium resulted in a 22 % decrease in clearance, which was significantly different from baseline values as well as during concurrent furosemide administration.
From a methodological perspective, Crabtree et al. [45] conducted the most impressive study to date, completing a randomized controlled trial comparing the effects of hydrochlorothiazide and furosemide in 13 healthy young subjects. The results of this investigation were remarkably consistent with the Jefferson and Kalin [44] trial, reporting a 19 % decrease in lithium clearance during hydrochlorothiazide administration (vs. baseline values) and no significant alteration in lithium distribution when furosemide was administered.
Although data documenting the effect of thiazide diuretics on lithium clearance are limited to several published case reports and a few small controlled trials in relatively healthy subjects, the impact on lithium disposition appears to be significant and potentially dangerous. For some patients, this elevation may impose serious clinical consequences due to the narrow therapeutic index of the mood stabilizer, but the identification of individuals who may be uniquely predisposed to this interaction is not yet evident. At the present time, clinicians are best advised to avoid adding thiazide diuretics to patients previously stabilized on lithium treatment. If thiazides must be initiated, it would seem prudent to reduce lithium daily dosages by 25–50 % and obtain plasma concentrations once a new steady-state concentration has been achieved (i.e., approximately 1 week after the initiation of thiazide in younger patients without evidence of renal or hemodynamic compromise).
4.1.2 Loop Diuretics
From a hemodynamic perspective, the pharmacologic effects of loop diuretics are generally considered to be more potent than thiazides. Initial physiology studies in rats, however, actually reported an increase in lithium clearance values when loop diuretics were introduced [46, 47]. In addition, small comparative studies in humans found that thiazides had a more profound effect on decreasing lithium clearance, while furosemide had negligible effects on lithium disposition [44, 45, 48]. One plausible explanation for this apparent discrepancy involves the anatomical site of diuretic activity. Thiazides act by inhibiting sodium reabsorption in the distal tubule, triggering a compensatory increase in sodium and lithium reabsorption in the proximal tubule. In contrast, loop diuretics such as furosemide and bumetanide exert their direct effects more proximally in the ascending limb of the loop of henle and, since distal lithium reabsorption is minimal, compensatory increases in lithium transport are not ordinarily observed [49].
In 1968 Thomsen and Schou [50] examined the effects of several medications on lithium disposition in six healthy human subjects. A single 600 mg oral dose of lithium carbonate was administered and baseline clearance values were calculated. Subjects then sequentially received concurrent medications such as furosemide, bendroflumethiazide, ethacrynic acid, spironolactone, acetazolamide, urea, and theophylline. The authors reported an 11 % decrease in lithium clearance following furosemide exposure (not statistically significant, or NS), as well as a 2 % decrease with bendroflumethiazide (NS), a 2 % increase with ethacrynic acid (NS), a 16 % increase with spironolactone (NS), a 31 % increase with acetazolamide (p < 0.05), a 36 % increase with urea (p < 0.05), and a 58 % increase following theophylline (p < 0.05).
Unfortunately, the safety of combining loop diuretics with lithium in clinical practice cannot be assured. Multiple case reports have been published over the years describing the precipitation of lithium toxicity following exposure to loop diuretics [40, 51, 52]. Interestingly, all of these case reports featured elderly subjects (age range: 63–72 years) with other medical illnesses, suggesting the possibility that loop diuretics may be more likely to impair lithium elimination among individuals with conditions such as hypertension, congestive heart failure, renal compromise, or sodium-restricted diets. More recently, Juurlink et al. [53] conducted a large retrospective case-control study of patients maintained on lithium in the Canadian national health database. Cases were patients who were admitted to hospital for presumed lithium intoxication (3.9 % of the lithium-treated population overall) while controls were beneficiaries stabilized on lithium without evidence of toxicity. After multivariate analysis, researchers reported that the highest RR for lithium toxicity was found in patients starting loop diuretics (RR = 5.5; 95 % confidence interval [CI] 1.9–16.1) and ACE inhibitors (RR = 7.6; 95 % CI 2.6–22.0), while exposure to thiazides or non-steroidal anti-inflammatory drugs (NSAIDs) was not associated with a statistically significant risk. Although study findings were hampered by relatively small sample size for the case cohort, as well as various selection biases, the conclusions did add further evidence that the risk of adding loop diuretics to patients stabilized on lithium therapy may be enhanced in older populations, as well as those with co-morbid medical conditions or sodium-restricted diets.
4.1.3 Potassium-Sparing Diuretics
Amiloride has long been used clinically as an antidote for lithium-induced nephrogenic diabetes insipidus, an adverse effect experienced by nearly 50 % of patients receiving long-term lithium treatment [54, 55]. Two retrospective open-label studies and one recent randomized controlled trial have demonstrated that amiloride is not only effective for decreasing urinary volume but also lacks any appreciable effects on serum concentrations of lithium or other electrolytes [56–58].
The relative safety of administering spironolactone to patients stabilized on lithium has not been extensively explored. In the investigation conducted by Thomsen and Schou [50], spironolactone was reported to increase lithium clearance by 16 % (i.e., decrease the lithium concentration by 20 %), a difference which was not statistically different from baseline values. An earlier study also examined the effect of spironolactone on lithium and reported equivocal findings [59]. While the investigators witnessed a consistent increase in serum lithium concentrations, the urinary excretion rate for lithium remained unchanged, suggesting that these observed outcomes were the result of transient hypovolemia, and it was unclear how continued exposure to spironolactone would impact lithium disposition at steady state.
Published evidence of research or clinical experience with the coadministration of triamterene and lithium could not be found. Given the pharmacological similarities existing between triamterene and amiloride, one would anticipate that changes in the pharmacokinetic parameters of lithium would be minor, but the safety of this combination remains purely speculative at the present time.
4.1.4 Osmotic Diuretics
Osmotic diuretics, such as mannitol and urea, can significantly enhance the clearance of lithium from the body, decreasing plasma concentrations and placing patients at risk for relapse. Presumably, this interaction is due to the creation of an ionic gradient which promotes the excretion of water and electrolytes into the renal tubule. Historically, guidelines for the management of lithium toxicity often advocated for the use of mannitol to abruptly lower the serum concentration, though considerable disparities have been noted in these recommendations, and hydration or extracorporeal removal are more widely advocated today [60].
Thomsen and Schou [50] first demonstrated the impact of urea on lithium disposition in their seminal study discussed in Sects. 4.1.2 and 4.1.3. After subjects were given oral doses of urea ranging from 60 to 83 g, lithium clearance values increased by 36 % on average, a difference deemed to be statistically significant. Obek [61] conducted an open-label study in nine dogs who received a mannitol infusion and reported a 52 % increase in lithium excretion rates. A subsequent case report describing the successful management of lithium toxicity confirmed the benefits of mannitol in facilitating lithium removal in humans, and a prospective study documented this finding as well [49, 62].
4.1.5 Methyl Xanthine Diuretics
Medications such as theophylline, aminophylline, and caffeine belong to another class of diuretics known as methyl xanthines, which can also expedite lithium excretion. While the popularity of theophylline and aminophylline for the treatment of asthma has waned in recent years, the common and often excessive consumption of caffeine among people with mood disorders has the potential to complicate long-term lithium administration.
Aminophylline was found to have the most profound effect on lithium clearance in the aforementioned study by Thomsen and Schou [50]. Individual doses of 500–1000 mg increased excretion rates of lithium by 58 % on average (p < 0.01) [50]. Theophylline was also studied in an open-label investigation of ten healthy subjects stabilized on lithium salt over a period of 9 days. After theophylline was introduced and maintained between plasma concentrations of 5.4–12.7 µg/dL for 5 days, lithium levels fell by 26 % on average, which was both statistically and clinically significant. A further investigation by Holstad et al. [63] analyzed the utility of intravenous theophylline as an antidote for lithium intoxication, reporting a dose-dependent increase of 51 % in lithium clearance. Unfortunately, the administration of theophylline was also associated with an increase in the incidence and severity of acute adverse effects, a finding that was reported by other researchers as well [50].
Caffeine was initially studied by Bikin et al. [64], who failed to uncover any changes in lithium disposition following the introduction of caffeine. Mester et al. [65] and others explored this interaction in a different fashion, measuring lithium concentrations in subjects who drank coffee on a regular basis before discontinuing the stimulant and sampling lithium levels 2 weeks later. Lithium concentrations were increased by 24 % under these conditions, and seven of the 11 subjects experienced classic signs and symptoms of caffeine withdrawal (e.g., headache, malaise, etc.). More recently, the excessive consumption of diet cola was associated with a dramatic decrease in lithium concentrations and subsequent admission to a psychiatric hospital for one adult patient with bipolar disorder [66].
From case reports and a limited number of controlled investigations, it appears that all methyl xanthines are capable of increasing lithium clearance and significantly lowering serum concentrations. This pharmacokinetic interaction appears to be related to the natriuretic effect of methyl xanthines in the proximal tubule, where they are capable of blocking transport of both sodium and lithium [67]. While the practical significance of this interaction is somewhat limited, clinicians should be advised that abrupt changes in caffeine consumption could precipitate substantial variations in plasma lithium concentrations.
4.2 ACE Inhibitors
ACE inhibitors are commonly prescribed for hypertension, congestive heart failure, and the prevention of diabetic nephropathy. Fundamentally, the primary pharmacological action of ACE inhibitors is to prevent the conversion of angiotensin I to angiotensin II, thereby leading to a decrease in aldosterone production, a decrease in sodium reabsorption, and relative volume depletion. This decrease in angiotensin II synthesis also results in peripheral vasodilation and a dose-related decrease in the GFR. Collectively, these physiologic effects would lead to a compensatory increase in lithium reabsorption in the proximal tubule and an increase in circulating lithium concentrations.
Shortly after the introduction of ACE inhibitors in the 1980s, a variety of case reports of lithium toxicity began appearing in the medical literature [68–77]. DasGupta and colleagues [78] subsequently conducted a small prospective study of nine healthy volunteers in an effort to substantiate this potential interaction. Subjects received lithium alone for 10 days, followed by lithium and enalapril for 10 days, and lithium monotherapy once again for the final 6 days. The authors reported that there was no significant change in lithium concentrations following the addition of enalapril, though one subject experienced a 31 % increase in concentrations.
In contrast, a retrospective study of 20 patients stabilized on lithium therapy reported a 36 % increase in concentration following the initiation of various ACE inhibitors, and four individuals presented to the emergency department with symptoms strongly suggestive of lithium intoxication [79]. The authors noted that there was a significant delay in the manifestation of toxicity, which was consistent with previous published case reports where patients generally received concurrent treatment for 3–5 weeks before symptoms emerged. This apparent discrepancy in study findings may be due to the fact that the prospective study recruited healthy volunteers lacking medical co-morbidities, as well as the fact that the investigators employed relatively low doses of lithium and ACE inhibitors to minimize the risk of serious toxicities.
While virtually all ACE inhibitors have been implicated in the precipitation of lithium toxicity, a recent case report suggests that there may differences in the RR posed by specific agents [80]. Meyer et al. [80] described a patient who had a gradual and profound increase in serum lithium concentrations following a change from fosinipril (20 mg daily) to lisinopril (20 mg daily). Over a period of 2 months, lithium concentrations increased from 0.7 to 3.4 mEq/L, resulting in hospitalization and bradycardia. The authors speculated that the differential effect of lisinopril may be due to the fact that it can accumulate under conditions of worsening renal function, but also mentioned that it is the only ACE inhibitor with a linear dose–response curve.
From multiple case reports and other observational data, it appears that the introduction of ACE inhibitors may place patients stabilized on lithium in danger of significant toxicity. Given the delayed nature and variable magnitude of this interaction, the combination of lithium with ACE inhibitors should be avoided if at all possible.
4.3 Angiotensin II Receptor Antagonists
Angiotensin II receptor antagonists (blockers; ARBs) are a relatively new class of antihypertensive medication which act as antagonists at the AT1 receptor subtype. This primary mode of action results in an increase in plasma renin concentrations and angiotensin II levels, and an increase in urinary sodium excretion [81]. Effects on serum aldosterone concentrations appear to be dose dependent and variable. As with ACE inhibitors, the coadministration of ARBs with lithium might be expected to produce a relative natriuresis and potential volume depletion, leading to a compensatory rise in lithium reabsorption in the proximal convoluted tubule, and potential toxicity.
In 1995, Barthelmebs et al. [82, 83] examined the impact of several medications on lithium excretion in rats. While the ACE inhibitor ramipril decreased lithium clearance by 44 % (p < 0.05) and the NSAID indomethacin decreased elimination by 54–57 % (p < 0.05), introduction of the ARB losartan resulted in a non-significant 6 % increase in lithium excretion. However, given the dose-dependent effects that ARBs can have on human renal physiology, it is difficult to determine if exposure in these rat studies approximated dosages typically prescribed in clinical practice. Furthermore, the lack of medical co-morbidities in these models may also discourage the extrapolation of exposure in rats to what might be observed in patients.
Since that time, a total of eight case reports involving four ARBs have been published describing the development of lithium toxicity after initiation of the antihypertensive [84–91]. The ages of patients described in these case reports ranged from 51 to 77 years of age and the indication was hypertension for all. The onset of toxicity was highly variable between patients, but the presentation for most patients occurred between 11 days and 5 weeks after starting the ARB. In each instance, the symptoms of toxicity resolved fairly quickly after concurrent administration had ceased, and in cases where lithium was later reinstated in the absence of the ARB, lithium disposition returned to baseline values.
Although there have not been any prospective studies investigating the safety of combining ARBs with lithium published to date, the presence of multiple case reports describing a significant interaction strongly suggest that caution is advised.
4.4 Non-Steroidal Anti-Inflammatory Drugs
Among all classes of medications, interactions between NSAIDs and lithium may be the best described. Case reports of lithium intoxication following the introduction of NSAIDs have been quite voluminous, and a variety of small, prospective trials have also documented significant increases in lithium concentrations when NSAIDs were coadministered [92]. Given the ubiquitous role that NSAIDs have assumed in the management of common conditions such as febrile illness, acute pain, and chronic inflammation, and the fact that many of these agents are readily available without a prescription, the relative safety of combining NSAIDs with lithium treatment is a pertinent concern.
Review of the prospective studies that have examined the impact of NSAIDs on lithium disposition reveals that most, if not all, of the agents in this class have the potential for decreasing clearance and potentiating toxicity, but the effects are highly variable and less predictable than anticipated. Virtually all of the investigations are quite small, and most recruited healthy volunteers to participate, a patient population that may not be representative of the individuals who are most likely to be exposed to concomitant treatment. As can be seen in Table 3, the mean decrease in lithium clearance was approximately 10–25 % for most investigations, but the range of clearance values was often quite large [93–105]. In addition, individual case reports describing concentration increases of 100 % or more are particularly daunting [106–108]. However, given the narrow therapeutic index of lithium, even a decrease of 20 % in clearance values can have significant clinical ramifications.
The mechanism underlying this important interaction has not been clearly delineated but the common assumption is that the inhibition of prostaglandin synthesis by NSAIDs may decrease renal blood flow and facilitate the reabsorption of sodium and (presumably) lithium [109]. If this hypothesis was accurate, one would anticipate that there would be a predictable hierarchy among the NSAIDs, with agents possessing the strongest inhibitory effects on renal prostaglandin production demonstrating the greatest impact on lithium clearance. Unfortunately, results from prospective trials do not necessarily support this pattern. Aspirin (acetylsalicylic acid) has inhibitory effects on renal prostaglandins that are comparable with other NSAIDs, yet results of two of three studies did not demonstrate a significant effect on lithium elimination, and the results of the third trial reported a small but significant increase in clearance. Similarly, a prospective study comparing the infusion of aspirin to sodium salicylate found that even though aspirin had a much more significant impact upon renal prostaglandin synthesis, only sodium salicylate caused a substantial decrease in lithium clearance values. This discrepancy may be explained, in part, by the fact that most studies of this interaction included healthy young volunteers, and previous research has demonstrated that renal prostaglandins are not influential in the maintenance of sodium and fluid homeostasis for individuals who are normally hydrated and lacking other renal or medical co-morbidities [110]. Clearly, the precise mechanism by which NSAID agents increase lithium retention has yet to be elucidated.
In 2003, researchers from the US Food and Drug Administration presented the results of a pharmacovigilance study examining the safety of concomitant NSAID–lithium treatment which has shed further light on this interaction [92]. The primary aim of the investigation was to explore the potential impact of the cyclo-oxygenase (COX)-2 class of NSAIDs on lithium elimination specifically, but the authors also provided a thorough synthesis of the medical literature describing interactions with any members of the NSAID class. In regards to celecoxib, the only COX-2 inhibitor currently marketed in the USA, the authors were unable to locate any prospective investigations but cited five case reports of lithium intoxication, with serum concentrations increasing from 56 to 99 %. In each case, the symptoms of lithium intoxication resolved following discontinuation of the COX-2 inhibitor, but the authors ultimately concluded that “it must be assumed for patient safety…that any NSAID has the potential to increase serum lithium concentration in any particular patient.”
In summary, virtually all members of the NSAID class have been reported to increase lithium concentrations to a significant extent. Multiple small prospective studies have been published which suggest that lithium clearance values generally decrease by 10–25 %, but most of these studies featured healthy volunteers and there is reason to suspect that patients with alterations in renal function, volume status, or other as yet unidentified co-morbidities may be uniquely at risk for more profound elevations in serum concentrations. It is hoped that further research will be conducted in future years to identify these vulnerable populations, as well as delineating which NSAIDs pose the higher risk and whether occasional use of these medications is permissible.
4.5 Antidepressants
Lithium is often added to antidepressants as an augmentation strategy for treatment-refractory depression [111]. It is also prescribed together with antidepressants for the acute management of bipolar depression. The safety of this combination is, therefore, an obvious concern. Fortunately, only a handful of case reports of acute adverse reactions with this combination have surfaced, and prospective pharmacokinetic studies have failed to demonstrate a significant effect of antidepressants on lithium disposition.
A variety of case reports of purported serotonin syndrome were attributed to the lithium–selective serotonin reuptake inhibitor (SSRI) combination in the 1990s, leading investigators to speculate that the serotonergic activity of lithium may enhance the pharmacologic actions of SSRIs, precipitating acute and excessive serotonin activity [112–116]. Upon further analysis, however, many of these patient presentations include adverse effects that could be attributed to either lithium or SSRIs alone, and it is unclear if the toxicity could reasonably be attributed to the unique combination of agents. Furthermore, many clinicians are unaware of the fact that SSRI monotherapy can precipitate serotonin syndrome in predisposed patients, particularly when patients are exposed to supertherapeutic doses or achieve extremely high concentrations [115].
In 2000, Hawley and others [117] compiled an extensive review of published studies and reports on the combination of lithium with SSRIs, arriving at the conclusion that the two classes of psychotropic agents appeared to be generally well-tolerated together and that verifiable case reports of serious or lethal toxicity could be not identified . These results are consistent with a previous retrospective study by Bauer et al. [118] who compared the adverse effects of fluoxetine alone to those of patients receiving fluoxetine with lithium. Both cohorts contained 110 patients in total and there was no significant increase in adverse effects in general, as well as no differences in a subgroup analysis of ‘serotonergic side effects,’ such as gastrointestinal upset, nervousness, tremor, and sweating. Prospective pharmacokinetic studies have also analyzed the impact of virtually all SSRIs (and many other new antidepressants) on lithium’s parameters and consistently found minimal effects on the disposition of the ion [119–124].
The preponderance of evidence available at the present time seems to suggest that lithium can be safely administered with SSRIs, as well as other classes of antidepressants.
4.6 Antipsychotics
Lithium is commonly administered with antipsychotics, most often for the acute management of manic or mixed manic episodes associated with bipolar disorder. Several case reports have been published describing acute and irreversible neurotoxicity with the combination of lithium and antipsychotics, though these episodes often resemble rare serious events that can be attributed to the administration of either agent alone (e.g., delirium, dysphoria, encephalopathy, dyskinesias, neuroleptic malignant syndrome, etc.) [125–128]. Early case reports featured the combination of lithium with conventional antipsychotics but atypical antipsychotics have been implicated with this interaction as well [129–132].
Since these two classes of psychotropic agents are often prescribed together and case reports of neurotoxicity have been relatively sparse, it would appear that this potential interaction is a rare and idiosyncratic phenomenon. Both retrospective and prospective studies of patients have compared adverse effects with lithium monotherapy, antipsychotic monotherapy, and combination treatment, concluding that there is no significant difference in toxic potential [133–135]. In contrast, a recent review of combination treatments for bipolar disorder concluded that the incidence of adverse effects is higher when lithium is given concomitantly with antipsychotics, though this was primarily in reference to adverse effects of a chronic and less severe nature [136].
In several of the case reports describing serious neurotoxicity, lithium concentrations increased abruptly following the administration of antipsychotics, but prospective pharmacokinetic studies have examined the potential impact of antipsychotics on lithium disposition and reported no significant change in serum lithium concentrations [137–141]. This has led to speculation that the change in lithium concentrations may have been precipitated by acute agitation and associated dehydration, electrolyte abnormalities, or renal compromise (secondary to myoglobinuria and myonecrosis).
Researchers have also theorized that this neurotoxicity may be due to increased intracellular or erythrocyte concentrations of lithium, relative to serum concentrations sampled in the periphery. This hypothesis was supported by several early studies featuring exposure to haloperidol or phenothiazines, but subsequent investigations failed to replicate these findings and actually reported decreases in lithium concentrations intracellularly [142–145]. A recent, preliminary investigation of cell cultures suggests that while lithium alone can decrease oxidative stress (which may be the mechanism underlying its neuroprotective action), the combination of antipsychotics with lithium may actually increase laboratory markers for oxidative stress and neurodegeneration [146]. This notable finding warrants replication and further study.
Although there have been a variety of case reports of severe neurotoxicity induced by the combination of lithium and antipsychotics, it remains unclear if these events are due to the synergistic potential of the two psychotropic medications or if the adverse effects were induced by a single agent alone. From pharmacokinetic studies, one can infer that concomitant antipsychotic treatment is unlikely to increase lithium concentrations, but these investigations have not yet explored the impact of this combination in the effective compartment (i.e., the CNS). Given the documented effectiveness of administering antipsychotics with lithium to acutely manage bipolar episodes, and the relatively rare phenomenon of neurotoxicity, it would not appear that this unique combination should be discouraged. However, clinicians are well-advised to closely monitor neurotoxic sequelae and ensure that adequate hydration and electrolyte status are maintained to minimize toxic potential.
4.7 Antiepileptic Drugs
The successful treatment and prevention of bipolar disorder often entails the utilization of several concurrent psychotropic medications. Anticonvulsants such as valproic acid and carbamazepine were once commonly administered with lithium and, although this practice has become less popular with the introduction of atypical antipsychotics into the psychopharmacological armamentarium, the safety of polypharmacy in this population remains a clinical concern.
Valproic acid rose to prominence as a valuable treatment option for acute mania, rapid cycling bipolar disorder, and schizoaffective illness over two decades ago. It is still commonly prescribed for these purposes, occasionally in combination with lithium, and continues to be a recommended treatment strategy, particularly for patients not responding adequately to initial monotherapy regimens [147]. Over the years there has been a multitude of clinical experience with this combination and it appears to be well-tolerated. Reports of adverse effects from clinical trials are more representative of cumulative toxicities associated with either drug alone than any underlying interactions [148–150]. Only a single prospective pharmacokinetic study has been published in the literature investigating a potential interaction, and the authors reported that a minor increase in valproic acid concentrations was observed (i.e., increased area under the plasma concentration–time curve [AUC] and maximum concentration [C max]) while the disposition of lithium was unaffected [151].
The combination of lithium with carbamazepine was once a fairly popular approach to refractory bipolar disorder and a variety of cases of neurotoxicity were observed [152–154]. In each of the case reports, patients had been stabilized on lithium for an extended period of time prior to receiving carbamazepine and quickly developed symptoms such as ataxia, tremors, hyperreflexia, and nystagmus once combination treatment began. All of the symptoms resolved upon discontinuation of the anticonvulsant. Subsequent pharmacokinetic studies failed to reveal any substantial changes in the disposition of lithium or carbamazepine, leading some researchers to speculate that the latter agent was increasing the lithium concentration intracellularly or in certain unspecified compartments in the CNS [155–157]. Other authors have found that carbamazepine actually improved lithium tolerability, due to the fact that daily doses of the original mood stabilizer were reduced after concomitant treatment improved clinical symptoms [158]. Mixed messages have also been reported on the impact of combination treatment on thyroid function, with some investigators reporting a decrease in thyroid-stimulating hormone concentrations when carbamazepine was added to lithium and others noting a greater decline in free T4 and T3 concentrations [158, 159].
Lamotrigine is often prescribed for the management of bipolar depression or mixed manic episodes. Although some authors have voiced theoretical concerns about additive cognitive deficits when lamotrigine is added to lithium, there are no published case reports of toxicity with this combination available at the present time [160]. A small open-label study investigated the impact of lamotrigine on lithium disposition and reported that there were no significant differences in pharmacokinetic parameters [161]. Conversely, a retrospective study of potential interactions was conducted by a therapeutic drug monitoring service which reported that lithium resulted in a 13 % decline in lamotrigine concentrations, which was deemed to be statistically significant [162] As this study was observational, the authors raised the possibility that temporal changes in medication adherence may have introduced confounding variables.
Topirimate is another antiepileptic drug (AED) that is occasionally used in combination with mood-stabilizing agents. A case report of lithium toxicity was published in 2004 which described the course of a bipolar patient stabilized on lithium and topirimate who increased the dose of her AED to lose weight (from 500 to 800 mg daily) [163]. Five weeks later she reportedly had lost 35 pounds (15.9 kg) but she was also complaining of severe anorexia, nausea, fatigue, and impaired concentration. These symptoms resolved when her topirimate dose was reduced back to the previous regimen. In the only prospective study of this combination published to date, the effects of topirimate were observed in 12 healthy volunteers [164]. The authors measured a 16 % increase in lithium clearance that was reported to be of borderline statistical significance, and they theorized that this interaction may be due to the weak inhibitory effects that the AED has on carbonic anhydrase activity.
4.8 Other Medications
Because lithium toxicity can be precipitated by a host of physiological factors, it is not surprising that many medications have been implicated temporally in the etiology of this phenomenon without clear evidence of causation. For example, antibacterials and antineoplastic agents have been associated with the development of lithium toxicity in various case reports but it is often difficult to control for other related factors encountered with the infection or malignancy being treated, such as hyperpyrexia, dehydration, renal compromise, and electrolyte disturbances [23, 165, 166]. A review of all published case reports of iatrogenic toxicity is beyond the scope of this pharmacokinetic review but there are certain combinations worth highlighting.
From multiple case reports as well as controlled experiments in animal models, it appears that lithium may potentiate or prolong the effects of neuromuscular blocking agents such as pancuronium and succinylcholine [167, 168]. It has been theorized that lithium would be more likely to augment the effects of non-depolarizing neuromuscular blockers (e.g., pancuronium and vecuronium) as it can decrease acetylcholine release, but adverse sequelae have been reported with depolarizing agents as well (e.g., succinylcholine) [169]. A related and controversial concern is the administration of electroconvulsive therapy (ECT) to patients receiving lithium, where multiple case reports of seizures and delirium have been detailed in the medical literature [170, 171]. While some authors believe this to be a contraindication, others have found ECT to be well-tolerated in patients maintained on lithium and advise clinicians to continue the mood stabilizer if clear benefits are evident [172].
The safety of combining lithium with calcium antagonists has also been questioned following multiple case reports of toxicity [173–176]. Although treatment details and chronology were often unclear, classic signs of toxicity were rapidly apparent shortly after initiation of calcium antagonists such as verapamil and diltiazem in spite of the fact that lithium concentrations were not elevated. A subsequent prospective study examined the effects of a single dose of nifedipine on lithium and reported no significant changes in plasma concentrations, prompting researchers to suggest that this may be a rare, idiosyncratic pharmacodynamic interaction of unknown etiology [53, 177].
An additional interaction worthy of mention may occur when sodium bicarbonate is administered to patients stabilized on lithium. Multiple case reports depict patients who are unable to achieve therapeutic concentrations with lithium while ingesting large amounts of antacids containing sodium bicarbonate [178, 179]. This phenomenon would be consistent with the results of the controlled study conducted by Thomsen and Schou [50] where bicarbonate infusion was associated with a 27 % increase in lithium clearance.
Finally, the impact of concurrent ethanol ingestion on lithium disposition is a vital concern, particularly when one considers that 36–61 % of individuals with bipolar disorder will have an alcohol use disorder in their lifetime [180]. Preliminary investigations suggested that lithium may actually serve to discourage drinking in alcoholics, but subsequent studies failed to conclusively demonstrate therapeutic benefits in regards to abstinence or co-morbid depression [181–184]. Unfortunately, study researchers failed to quantify the effects of ethanol on lithium disposition or adequately address potential symptoms of lithium toxicity. In theory, one might anticipate that ethanol ingestion might have significant deleterious effects on lithium treatment. From a pharmacokinetic standpoint, the diuretic effects of acute ethanol ingestion may lead to an increase in lithium reabsorption and an elevation in plasma concentrations. Pharmacodynamically, individuals with a history of chronic alcohol abuse often have neurological impairments such as tremor, memory loss, and confusion that could be exacerbated by lithium administration. In addition, from a psychopathological perspective, chronic alcohol administration may also diminish the mood-stabilizing properties of lithium, engendering future depressive episodes. Unfortunately, none of these effects have been studied in either a prospective or observational fashion and further investigations are clearly warranted [53].
5 Conclusion
In spite of the development and release of novel psychotropic agents, lithium continues to be widely utilized for the maintenance treatment of bipolar affective disorder. Prospective investigations have confirmed and refined our knowledge of a narrow therapeutic range for the mood stabilizer, and any alterations in renal function, hydration status, or electrolyte concentrations can have profound effects on lithium disposition. Over the past 20 years, evidence of potential drug interactions has continued to accumulate. For example, it has become evident that there may be significant differences between individual diuretic agents and NSAID compounds in regards to their impact on lithium concentrations. Furthermore, case reports and observational studies have also emerged to suggest that ACE inhibitors, ARBs, SSRIs, atypical antipsychotics, and newer AEDs may also impart an increased risk for toxicity. At the present time, much of the evidence supporting lithium drug interactions is limited to anecdotal reports, and it is hoped that controlled studies may be conducted in the future to further delineate the risk inherent with specific medications, as well as to identify vulnerable patient populations.
References
Schou M. Lithium treatment at 52. J Affect Disord. 2001;67:21–32.
Goodwin FK, Fireman B, Simon GE, Hunkeler EM, Lee J, Revicki D. Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA. 2003;290:1467–73.
Guzzetta F, Tondo L, Centorrino F, Baldessarini RJ. Lithium treatment reduces suicide risk in recurrent major depressive disorder. J Clin Psychiatr. 2007;68:380–3.
Shulman KI, Rochon P, Sykora K, Anderson G, Mamdani M, Bronskill S, et al. Changing prescription patterns for lithium and valproic acid in old age: shifting practice without evidence. BMJ. 2003;326:960–1.
American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry. 2002;159(4 Suppl):1–50.
Yatham LN, Kennedy SH, Schaffer A, Parikh SV, Beaulieu S, O’Donovan C, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disord. 2009;11:225–55.
Saran BM, Russell GF. The effects of administering lithium carbonate on the balance of Na, K and water in manic-depressive patients. Psychol Med. 1976;6:381–92.
Schrauzer GN, Shrestha KP. Lithium in drinking water and the incidences of crimes, suicides, and arrests related to drug addictions. Biol Trace Elem Res. 1990;25:105–13.
Ohgami H, Terao T, Shiotsuki I, Ishii N, Iwata N. Lithium levels in drinking water and risk of suicide. Br J Psychiatr. 2009;194:464–5.
Fels A. Should we all take a bit of lithium [opinion]. New York Times SundayReview, September 13, 2014: page SR6
Alda M. Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry 2015;20:1–10.
Leeds PR, Yu F, Wang Z, Chiu CT, Zhang Y, Leng Y, et al. A new avenue for lithium: intervention in traumatic brain injury. ACS Chem Neurosci. 2014;5(6):422–33.
Price LH, Heninger GR. Lithium in the treatment of mood disorders. N Engl J Med. 1994;331(9):591–8.
Manji HK, Hsiao JK, Risby ED, Oliver J, Rudorfer MV, Potter WZ. The mechanisms of action of lithium. I. Effects on serotoninergic and noradrenergic systems in normal subjects. Arch Gen Psychiatry. 1991;48(6):505–12.
Nonaka S, Hough CJ, Chuang DM. Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting N-methyl-d-aspartate receptor-mediated calcium influx. Proc Natl Acad Sci. 1998;95(5):2642–7.
Malhi GS, Tanious M, Das P, Coulston CM, Berk M. Potential mechanisms of action of lithium in bipolar disorder: current understanding. CNS Drugs. 2013;27(2):135–53.
Manji HK, Etcheberrigaray R, Chen G, Olds JL. Lithium decreases membrane-associated protein kinase C in hippocampus: selectivity for the alpha isozyme. J Neurochem. 1993;61(6):2303–10.
Fiorentini A, Rosi MC, Grossi C, Luccarini I, Casamenti F. Lithium improves hippocampal neurogenesis, neuropathology and cognitive functions in APP mutant mice. PLoS One. 2010;5(12):e14382.
Sugita ET, Stokes JW, Frazer A, Grof P, Mendels J, Goldstein FJ, et al. Lithium carbonate absorption in humans. J Clin Pharmacol. 1973;13:264–70.
Gai MN, Thielemann AM, Arancibia A. Effect of three different diets on the bioavailability of a sustained release lithium carbonate matrix tablet. Int J Clin Pharmacol Ther. 2000;38(6):320–6.
Carson SW. Lithium. In: Evans WE, Schentag JJ, Jusko WJ, editors. Applied pharmacokinetics: principles of therapeutic drug monitoring, chap 34. Vancouver: Applied Therapeutics; 1990. p. 1–26.
Soares JC, Boada F, Keshavan MS. Brain lithium measurements with (7)Li magnetic resonance spectroscopy (MRS): a literature review. Eur Neuropsychopharmacol. 2000;10(3):151–8.
Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331–49.
Koomans HA, Boer WH, Dorhout Mees EJ. Evaluation of lithium clearance as a marker of proximal tubule sodium handling. Kidney Int. 1989;36(1):2–12.
Kishore BK, Ecelbarger CM. Lithium: a versatile tool for understanding renal physiology. Am J Physiol Renal Physiol. 2013;304(9):F1139–49.
Luisier PA, Schulz P, Dick P. The pharmacokinetics of lithium in normal humans: expected and unexpected observations in view of basic kinetic principles. Pharmacopsychiatry. 1987;20(5):232–4.
Hunter R. Steady-state pharmacokinetics of lithium carbonate in healthy subjects. Br J Clin Pharmacol. 1988;25(3):375–80.
Schou M. Serum lithium monitoring of prophylactic treatment: critical review and updated recommendations. Clin Pharmacokinet. 1988;15(5):283–6.
Schou M, Baastrup PC. Lithium treatment of manic-depressive disorder. Dosage and control. JAMA. 1967;201(9):696–8.
Montgomery DB, European College of Neuropsychopharmacology. ECNP consensus meeting March 2000 NICE: guidelines for investigating efficacy in bipolar disorder. Eur Neuropsychopharmacol. 2001;11:79–88.
Malhi GS, Tanious M, Gershon S. The lithiumeter: a measured approach. Bipolar Disord. 2011;13(3):219–26.
Gelenberg AJ, Kane JM, Keller MB, Lavori P, Rosenbaum JF, Cole K, et al. Comparison of standard and low serum levels of lithium for maintenance treatment of bipolar disorder. N Engl J Med. 1989;321(22):1489–93.
Kato T, Inubushi T, Takahashi S. Relationship of lithium concentrations in the brain measured by lithium-7 magnetic resonance spectroscopy to treatment response in mania. J Clin Psychopharmacol. 1994;14:330–5.
Rej S, Herrmann N, Shulman K. The effects of lithium on renal function in older adults–a systematic review. J Geriatr Psychiatry Neurol. 2012;25(1):51–61.
Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part III: clinical safety. CNS Drugs. 2009;23(5):397–418.
Danielyan A, Kowatch RA. Management options for bipolar disorder in children and adolescents. Paediatr Drugs. 2005;7(5):277–94.
Levy ST, Forrest JN Jr, Heninger GR. Lithium-induced diabetes insipidus: manic symptoms, brain and electrolyte correlates, and chlorothiazide treatment. Am J Psychiatry. 1973;130(9):1014–8.
Macfie AC. Letter: lithium poisoning precipitated by diuretics [letter]. Br Med J. 1975;1(5956):516.
Solomon JG. Lithium toxicity precipitated by a diuretic. Psychosomatics. 1980;21(5):425, 429.
Kerry RJ, Ludlow JM, Owen G. Diuretics are dangerous with lithium. Br Med J. 1980;281(6236):371.
Petersen V, Hvidt S, Thomsen K, Schou M. Effect of prolonged thiazide treatment on renal lithium clearance. Br Med J. 1974;3(5924):143–5.
Poust RI, Mallinger AG, Mallinger J, Himmelhoch JM, Neil JF, Hanin I. Effect of chlorothiazide on the pharmacokinetics of lithium in plasma and erythrocytes. Psychopharmacol Commun. 1976;2(3):273–84.
Himmelhoch JM, Forrest J, Neil JF, Detre TP. Thiazide-lithium synergy in refractory mood swings. Am J Psychiatry. 1977;134(2):149–52.
Jefferson JW, Kalin NH. Serum lithium levels and long-term diuretic use. JAMA. 1979;241(11):1134–6.
Crabtree BL, Mack JE, Johnson CD, Amyx BC. Comparison of the effects of hydrochlorothiazide and furosemide on lithium disposition. Am J Psychiatry. 1991;148(8):1060–3.
Steele TH, Dudgeon KL, Larmore CK. Pharmacological characterization of lithium reabsorption in the rat. J Pharmacol Exp Ther. 1976;196(1):188–93.
Shirley DG, Walter SJ, Sampson B. A micropuncture study of renal lithium reabsorption: effects of amiloride and furosemide. Am J Physiol. 1992;263(6 Pt 2):F1128–33.
Saffer D, Coppen A. Frusemide: a safe diuretic during lithium therapy? J Affect Disord. 1983;5(4):289–92.
Noormohamed FH. Renal handling of lithium and the effects of mannitol and arginine vasopressin in man. Clin Sci (Lond). 1995;89(1):27–36.
Thomsen K, Schou M. Renal lithium excretion in man. Am J Physiol. 1968;215(4):823–7.
Hurtig HI, Dyson WL. Letter: lithium toxicity enhanced by diuresis [letter]. N Engl J Med. 1974;290(13):748–9.
Oh TE. Frusemide and lithium toxicity. Anaesth Intensive Care. 1977;5(1):60–2.
Juurlink DN, Mamdani MM, Kopp A, Rochon PA, Shulman KI, Redelmeier DA. Drug-induced lithium toxicity in the elderly: a population-based study. J Am Geriatr Soc. 2004;52(5):794–8.
Boton R, Gaviria M, Batlle DC. Prevalence, pathogenesis, and treatment of renal dysfunction associated with chronic lithium therapy. Am J Kidney Dis. 1987;10(5):329–45.
Alexander MP, Farag YM, Mittal BV, Rennke HG, Singh AK. Lithium toxicity: a double-edged sword. Kidney Int. 2008;73(2):233–7.
Batlle DC, von Riotte AB, Gaviria M, Grupp M. Amelioration of polyuria by amiloride in patients receiving long-term lithium therapy. N Engl J Med. 1985;312(7):408–14.
Kosten TR, Forrest JN. Treatment of severe lithium-induced polyuria with amiloride. Am J Psychiatry. 1986;143(12):1563–8.
Bedford JJ, Weggery S, Ellis G, McDonald FJ, Joyce PR, Leader JP, Walker RJ. Lithium-induced nephrogenic diabetes insipidus: renal effects of amiloride. Clin J Am Soc Nephrol. 2008;3(5):1324–31. doi:10.2215/CJN.01640408.
Baer L, Platman SR, Kassir S, Fieve RR. Mechanisms of renal lithium handling and their relationship to mineralocorticoids: a dissociation between sodium and lithium ions. J Psychiatr Res. 1971;8(2):91–105.
Decker BS, Goldfarb DS, Dargan PI, Friesen M, Gosselin S, Hoffman RS, et al. Extracorporeal treatment for lithium poisoning: systematic review and recommendations from the EXTRIP Workgroup. Clin J Am Soc Nephrol. 2015;10(5):875–87. doi:10.2215/CJN.10021014.
Obek A. Mannitol infusions and lithium excretion [letter]. Br Med J. 1972;4(5839):550.
Shneerson JM. Acute lithium intoxication. Br J Clin Pract. 1978;32(8):232, 237.
Holstad SG, Perry PJ, Kathol RG, Carson RW, Krummel SJ. The effects of intravenous theophylline infusion versus intravenous sodium bicarbonate infusion on lithium clearance in normal subjects. Psychiatry Res. 1988;25(2):203–11.
Bikin D, Conrad KA, Mayersohn M. Lack of influence of caffeine and aspirin on lithium elimination. Clin Res. 1982;30:249.
Mester R, Toren P, Mizrachi I, Wolmer L, Karni N, Weizman A. Caffeine withdrawal increases lithium blood levels. Biol Psychiatry. 1995;37(5):348–50.
Kralovec K, Fartacek R, Plöderl M, Fartacek C, Aichhorn W. Low serum lithium associated with immoderate use of Coca-Cola Zero. J Clin Psychopharmacol. 2011;31(4):543–4. doi:10.1097/JCP.0b013e318222bb44.
Ludens JH, Willis LR, Williamson HE. The effect of aminophylline on renal hemodynamics and sodium excretion. Arch Int Pharmacodyn Ther. 1970;185(2):274–8.
Douste-Blazy P, Rostin M, Livarek B, Tordjman E, Montastruc JL, Galinier F. Angiotensin converting enzyme inhibitors and lithium treatment. Lancet. 1986;1(8495):144.
Mahieu M, Houvenagel E, Leduc JJ, Choteau P. Lithium-converting enzyme inhibitors: a combination to avoid? Presse Med. 1988;17(6):281.
Pulik M, Lida H. Interaction of lithium and angiotensin-converting enzyme inhibitors. Presse Med. 1988;17(15):75.
Conrad AJ. Ace inhibitors and lithium toxicity [letter]. Mass Gen Hosp Newslett. 1988;2:43.
Navis GJ, de Jong PE, de Zeeuw D. Volume homeostasis, angiotensin converting enzyme inhibition, and lithium therapy. Am J Med. 1989;86(5):621.
Drouet A, Bouvet O. Lithium and converting enzyme inhibitors. Encephale. 1990;16(1):51–2.
Baldwin CM, Safferman AZ. A case of lisinopril-induced lithium toxicity. DICP. 1990;24(10):946–7.
Griffin JH, Hahn SM. Lisinopril-induced lithium toxicity. DICP. 1991;25(1):101.
Correa FJ, Eiser AR. Angiotensin-converting enzyme inhibitors and lithium toxicity. Am J Med. 1992;93(1):108–9.
Teitelbaum M. A significant increase in lithium levels after concomitant ACE inhibitor administration. Psychosomatics. 1993;34(5):450–3.
DasGupta K, Jefferson JW, Kobak KA, Greist JH. The effect of enalapril on serum lithium levels in healthy men. J Clin Psychiatry. 1992;53(11):398–400.
Finley PR, O’Brien JG, Coleman RW. Lithium and angiotensin-converting enzyme inhibitors: evaluation of a potential interaction. J Clin Psychopharmacol. 1996;16(1):68–71.
Meyer JM, Dollarhide A, Tuan IL. Lithium toxicity after switch from fosinopril to lisinopril. Int Clin Psychopharmacol. 2005;20(2):115–8.
Burnier M, Waeber B, Brunner HR. Clinical pharmacology of the angiotensin II receptor antagonist losartan potassium in healthy subjects. J Hypertens Suppl. 1995;13(1):S23–8 (Review).
Barthelmebs M, Grima M, Imbs JL. Ramipril-induced decrease in renal lithium excretion in the rat. Br J Pharmacol. 1995;116(4):2161–5.
Barthelmebs M, Alt-Tebacher M, Madonna O, Grima M, Imbs JL. Absence of a losartan interaction with renal lithium excretion in the rat. Br J Pharmacol. 1995;116(4):2166–9.
Blanche P, Raynaud E, Kerob D, Galezowski N. Lithium intoxication in an elderly patient after combined treatment with losartan. Eur J Clin Pharmacol. 1997;52(6):501.
Leung M, Remick RA. Potential drug interaction between lithium and valsartan. J Clin Psychopharmacol. 2000;20(3):392–3.
Zwanzger P, Marcuse A, Boerner RJ, Walther A, Rupprecht R. Lithium intoxication after administration of AT1 blockers. J Clin Psychiatry. 2001;62(3):208–9.
Su YP, Chang CJ, Hwang TJ. Lithium intoxication after valsartan treatment. Psychiatry Clin Neurosci. 2007;61(2):204.
Aruna AS. Lithium toxicity secondary to lithium-losartan interaction. J Pharm Technol. 2009;25:89–93.
Ma CC, Shiah IS, Chang SW, Kao YC, Lee WK. Telmisartan-induced lithium intoxication in a patient with schizoaffective disorder. Psychiatry Clin Neurosci. 2012;66(2):165–6.
Edokpolo O, Fyyaz M. Lithium toxicity and neurologic effects: probable neuroleptic malignant syndrome resulting from lithium toxicity. Case Rep Psychiatry. 2012;2012:271858. doi:10.1155/2012/271858.
Lazarczyk MJ, Giannakopoulos P. Temporal association as a prerequisite factor of valsartan-induced lithium toxicity. Bipolar Disord. 2014;16(6):662–6. doi:10.1111/bdi.12174.
Phelan KM, Mosholder AD, Lu S. Lithium interaction with the cyclooxygenase 2 inhibitors rofecoxib and celecoxib and other nonsteroidal anti-inflammatory drugs. J Clin Psychiatry. 2003;64(11):1328–34.
Reimann IW, Diener U, Frölich JC. Indomethacin but not aspirin increases plasma lithium ion levels. Arch Gen Psychiatry. 1983;40(3):283–6.
Frölich JC, Leftwich R, Ragheb M, Oates JA, Reimann I, Buchanan D. Indomethacin increases plasma lithium. Br Med J. 1979;1(6171):1115–6.
Rabelink AJ, Koomans HA, Boer WH, Dorhout Mees EJ, van Rijn HJ. Indomethacin increases renal lithium reabsorption in man. Nephrol Dial Transplant. 1989;4(1):27–31.
Kristoff CA, Hayes PE, Barr WH, Small RE, Townsend RJ, Ettigi PG. Effect of ibuprofen on lithium plasma and red blood cell concentrations. Clin Pharm. 1986;5(1):51–5.
Ragheb M. Ibuprofen can increase serum lithium level in lithium-treated patients. J Clin Psychiatry. 1987;48(4):161–3.
Levin GM, Grum C, Eisele G. Effect of over-the-counter dosages of naproxen sodium and acetaminophen on plasma lithium concentrations in normal volunteers. J Clin Psychopharmacol. 1998;18(3):237–40.
Ragheb M, Powell AL. Lithium interaction with sulindac and naproxen. J Clin Psychopharmacol. 1986;6(3):150–4.
Reimann IW, Frölich JC. Effects of diclofenac on lithium kinetics. Clin Pharmacol Ther. 1981;30(3):348–52.
Cold JA, ZumBrunnen TL, Simpson MA, Augustin BG, Awad E, Jann MW. Increased lithium serum and red blood cell concentrations during ketorolac coadministration. J Clin Psychopharmacol. 1998;18(1):33–7.
Hughes BM, Small RE, Brink D, McKenzie ND. The effect of flurbiprofen on steady-state plasma lithium levels. Pharmacotherapy. 1997;17(1):113–20.
Türck D, Heinzel G, Luik G. Steady-state pharmacokinetics of lithium in healthy volunteers receiving concomitant meloxicam. Br J Clin Pharmacol. 2000;50(3):197–204.
Reimann IW, Golbs E, Fischer C, Frölich JC. Influence of intravenous acetylsalicylic acid and sodium salicylate on human renal function and lithium clearance. Eur J Clin Pharmacol. 1985;29(4):435–41.
Ragheb MA. Aspirin does not significantly affect patients’ serum lithium levels. J Clin Psychiatry. 1987;48(10):425.
Harrison TM, Davies DW, Norris CM. Lithium carbonate and piroxicam. Br J Psychiatry. 1986;149:124–5.
Bailey CE, Stewart JT, McElroy RA. Ibuprofen-induced lithium toxicity. South Med J. 1989;82(9):1197.
Jones MT, Stoner SC. Increased lithium concentrations reported in patients treated with sulindac. J Clin Psychiatry. 2000;61(7):527–8.
Brater DC. Effects of nonsteroidal anti-inflammatory drugs on renal function: focus on cyclooxygenase-2-selective inhibition. Am J Med. 1999;107(6A):65S–70S.
Harris RC. COX-2 and the kidney. J Cardiovasc Pharmacol. 2006;47(Suppl 1):S37–42.
Zullino D, Baumann P. Lithium augmentation in depressive patients not responding to selective serotonin reuptake inhibitors. Pharmacopsychiatry. 2001;34(4):119–27.
Salama AA, Shafey M. A case of severe lithium toxicity induced by combined fluoxetine and lithium carbonate. Am J Psychiatry. 1989;146(2):278.
Muly EC, McDonald W, Steffens D, Book S. Serotonin syndrome produced by a combination of fluoxetine and lithium. Am J Psychiatry. 1993;150(10):1565.
Ohman R, Spigset O. Serotonin syndrome induced by fluvoxamine-lithium interaction. Pharmacopsychiatry. 1993;26(6):263–4.
Sobanski T, Bagli M, Laux G, Rao ML. Serotonin syndrome after lithium add-on medication to paroxetine. Pharmacopsychiatry. 1997;30(3):106–7.
Fagiolini A, Buysse DJ, Frank E, Houck PR, Luther JF, Kupfer DJ. Tolerability of combined treatment with lithium and paroxetine in patients with bipolar disorder and depression. J Clin Psychopharmacol. 2001;21(5):474–8.
Hawley CJ, Loughlin PJ, Quick SJ, et al. Efficacy, safety and tolerability of combined administration of lithium and selective serotonin reuptake inhibitors: a review of the current evidence. Hertfordshire Neuroscience Research Group. Int Clin Psychopharmacol. 2000;15(4):197–206.
Bauer M, Linden M, Schaaf B, Weber HJ. Adverse events and tolerability of the combination of fluoxetine/lithium compared with fluoxetine. J Clin Psychopharmacol. 1996;16(2):130–4.
Apseloff G, Wilner KD, von Deutsch DA, et al. Sertraline does not alter steady-state concentrations or renal clearance of lithium in healthy volunteers. J Clin Pharmacol. 1992;32(7):643–6.
Breuel HP, Müller-Oerlinghausen B, Nickelsen T, Heine PR. Pharmacokinetic interactions between lithium and fluoxetine after single and repeated fluoxetine administration in young healthy volunteers. Int J Clin Pharmacol Ther. 1995;33(7):415–9.
Troy SM, Parker VD, Hicks DR, Boudino FD, Chiang ST. Pharmacokinetic interaction between multiple-dose venlafaxine and single-dose lithium. J Clin Pharmacol. 1996;36(2):175–81.
Laroudie C, Salazar DE, Cosson JP, et al. Pharmacokinetic evaluation of co-administration of nefazodone and lithium in healthy subjects. Eur J Clin Pharmacol. 1999;54(12):923–8.
Sitsen JM, Voortman G, Timmer CJ. Pharmacokinetics of mirtazapine and lithium in healthy male subjects. J Psychopharmacol. 2000;14(2):172–6.
Gupta B, Chopra S, Gupta C, Mahajan R, Uppal B, Minocha KB. Effects of fluoxetine, risperidone and alprazolam on pharmacokinetics of lithium in patients with psychiatric illness. Indian J Pharmacol. 2006;38:133–4.
Cohen WJ, Cohen NH. Lithium carbonate, haloperidol, and irreversible brain damage. JAMA. 1974;230(9):1283–7.
Mani J, Tandel SV, Shah PU, Karnad DR. Prolonged neurological sequelae after combination treatment with lithium and antipsychotic drugs. J Neurol Neurosurg Psychiatry. 1996;60(3):350–1.
Goldman SA. Lithium and neuroleptics in combination: is there enhancement of neurotoxicity leading to permanent sequelae? J Clin Pharmacol. 1996;36(10):951–62.
Normann C, Brandt C, Berger M, Walden J. Delirium and persistent dyskinesia induced by a lithium-neuroleptic interaction. Pharmacopsychiatry. 1998;31(5):201–4.
Swartz CM. Olanzapine-lithium encephalopathy. Psychosomatics. 2001;42(4):370.
Tuglu C, Erdogan E, Abay E. Delirium and extrapyramidal symptoms due to a lithium-olanzapine combination therapy: a case report. J Korean Med Sci. 2005;20(4):691–4.
Ali S, Pearlman RL, Upadhyay A, Patel P. Neuroleptic malignant syndrome with aripiprazole and lithium: a case report. J Clin Psychopharmacol. 2006;26(4):434–6.
Miodownik C, Alkatnany A, Frolova K, Lerner V. Delirium associated with lithium-quetiapine combination. Clin Neuropharmacol. 2008;31(3):176–9.
Baastrup PC, Hollnagel P, Sorensen R, Schou M. Adverse reactions in treatment with lithium carbonate and haloperidol. JAMA. 1976;236(23):2645–6.
Garfinkel PE, Stancer HC, Persad E. A comparison of haloperidol, lithium carbonate and their combination in the treatment of mania. J Affect Disord. 1980;2(4):279–88.
Goldney RD, Spence ND. Safety of the combination of lithium and neuroleptic drugs. Am J Psychiatry. 1986;143(7):882–4.
Buoli M, Serati M, Altamura AC. Is the combination of a mood stabilizer plus an antipsychotic more effective than mono-therapies in long-term treatment of bipolar disorder? A systematic review. J Affect Disord. 2014;152–154:12–8.
Apseloff G, Mullet D, Wilner KD, Anziano RJ, Tensfeldt TG, Pelletier SM, et al. The effects of ziprasidone on steady-state lithium levels and renal clearance of lithium. Br J Clin Pharmacol. 2000;49(Suppl 1):61S–4S.
Potkin SG, Thyrum PT, Bera R, Carreon D, Alva G, Kalali AH, et al. Open-label study of the effect of combination quetiapine/lithium therapy on lithium pharmacokinetics and tolerability. Clin Ther. 2002;24(11):1809–23.
Canal M, Legangneux E, van Lier JJ, van Vliet AA, Coulouvrat C. Lack of effect of amisulpride on the pharmacokinetics and safety of lithium. Int J Neuropsychopharmacol. 2003;6(2):103–9.
Demling JH, Huang ML, Remmerie B, Mannaert E, Sperling W. Pharmacokinetics and safety of combination therapy with lithium and risperidone. Pharmacopsychiatry. 2006;39(6):230–1.
Boulton DW, Kollia GD, Mallikaarjun S, Kornhauser DM. Lack of a pharmacokinetic drug-drug interaction between lithium and valproate when co-administered with aripiprazole. J Clin Pharm Ther. 2012;37(5):565–70.
Pandey GN, Goel I, Davis JM. Effect of neuroleptic drugs on lithium uptake by the human erythrocyte. Clin Pharmacol Ther. 1979;26(1):96–102.
von Knorring L, Smigan L, Perris C, Oreland L. Lithium and neuroleptic drugs in combination—effect on lithium RBC/plasma ratio. Int Pharmacopsychiatry. 1982;17(4):287–92.
Ghadirian AM, Nair NP, Schwartz G. Effect of lithium and neuroleptic combination on lithium transport, blood pressure, and weight in bipolar patients. Biol Psychiatry. 1989;26(2):139–44.
Azizabadi-Farahani M, Mirazi N, Azar M, Farsam H, Dehpour AR. The effect of concomitant use of neuroleptic drugs and lithium on the erythrocyte/plasma lithium ratio in Iranian patients with bipolar disorder. J Clin Pharm Ther. 1996;21(1):3–7.
Gawlik-Kotelnicka O, Mielicki W, Rabe-Jabłońska J, Lazarek J, Strzelecki D. Impact of lithium alone or in combination with haloperidol on oxidative stress parameters and cell viability in SH-SY5Y cell culture. Acta Neuropsychiatr. 2015;19:1–7.
Kahn DA, Sachs GS, Printz DJ, Carpenter D, Docherty JP, Ross R. Medication treatment of bipolar disorder 2000: a summary of the expert consensus guidelines. J Psychiatr Pract. 2000;6(4):197–211.
Denicoff KD, Smith-Jackson EE, Bryan AL, Ali SO, Post RM. Valproate prophylaxis in a prospective clinical trial of refractory bipolar disorder. Am J Psychiatry. 1997;154(10):1456–8.
Solomon DA, Keitner GI, Ryan CE, Miller IW. Lithium plus valproate as maintenance polypharmacy for patients with bipolar I disorder: a review. J Clin Psychopharmacol. 1998;18(1):38–49.
Pies R. Combining lithium and anticonvulsants in bipolar disorder: a review. Ann Clin Psychiatry. 2002;14(4):223–32.
Granneman GR, Schneck DW, Cavanaugh JH, Witt GF. Pharmacokinetic interactions and side effects resulting from concomitant administration of lithium and divalproex sodium. J Clin Psychiatry. 1996;57(5):204–6.
Chaudhry RP, Waters BG. Lithium and carbamazepine interaction: possible neurotoxicity. J Clin Psychiatry. 1983;44(1):30–1.
Shukla S, Godwin CD, Long LE, Miller MG. Lithium-carbamazepine neurotoxicity and risk factors. Am J Psychiatry. 1984;141(12):1604–6.
Price WA, Zimmer B. Lithium-carbamazepine neurotoxicity in the elderly. J Am Geriatr Soc. 1985;33(12):876–7.
Rybakowski JK, Lehman W, Kanarkowski R, et al. Possible pharmacokinetic interaction of lithium and carbamazepine. Lithium. 1991;2:183–4.
Yang YY, Deng HC. Influence of carbamazepine on Li+ ratio in healthy volunteers: an in vitro method. Clin Neuropharmacol. 1993;16(3):216–9.
Shopsin D, Johnson G, Gershon S. Neurotoxicity with lithium: differential drug responsiveness. Int Pharmacopsychiatry. 1970;5:170–82.
Bocchetta A, Chillotti C, Severino G, Ardau R, Del Zompo M. Carbamazepine augmentation in lithium-refractory bipolar patients: a prospective study on long-term prophlyactic effectiveness. J Clin Psychopharmacol. 1997;17(2):92–6.
Kramlinger KG, Post RM. Addition of lithium carbonate to carbamazepine: hematological and thyroid effects. Am J Psychiatry. 1990;147(5):615–20.
Sporn J, Sachs G. The anticonvulsant lamotrigine in treatment-resistant manic-depressive illness. J Clin Psychopharmacol. 1997;17(3):185–9.
Chen C, Veronese L, Yin Y. The effects of lamotrigine on the pharmacokinetics of lithium. Br J Clin Pharmacol. 2000;50(3):193–5.
Reimers A, Skogvoll E, Sund JK, Spigset O. Drug interactions between lamotrigine and psychoactive drugs: evidence from a therapeutic drug monitoring service. J Clin Psychopharmacol. 2005;25(4):342–8.
Pinninti NR, Zelinski G. Does topiramate elevate serum lithium levels? J Clin Psychopharmacol. 2002;22(3):340.
Bialer M, Doose DR, Murthy B, et al. Pharmacokinetic interactions of topiramate. Clin Pharmacokinet. 2004;43(12):763–80.
Takahashi H, Higuchi H, Shimizu T. Severe lithium toxicity induced by combined levofloxacin administration. J Clin Psychiatry. 2000;61(12):949–50.
Walker RG. Lithium nephrotoxicity. Kidney Int Suppl. 1993;42:S93–8.
Borden H, Clarke MT, Katz H. The use of pancuronium bromide in patients receiving lithium carbonate. Can Anaesth Soc J. 1974;21(1):79–82.
Hill GE, Wong KC, Hodges MR. Potentiation of succinylcholine neuromuscular blockade by lithium carbonate. Anesthesiology. 1976;44(5):439–42.
Feldman S, Karalliedde L. Drug interactions with neuromuscular blockers. Drug Saf. 1996;15(4):261–73.
Jha AK, Stein GS, Fenwick P. Negative interaction between lithium and electroconvulsive therapy–a case-control study. Br J Psychiatry. 1996;168(2):241–3.
Sartorius A, Wolf J, Henn FA. Lithium and ECT–concurrent use still demands attention: three case reports. World J Biol Psychiatry. 2005;6(2):121–4.
Dolenc TJ, Rasmussen KG. The safety of electroconvulsive therapy and lithium in combination: a case series and review of the literature. J ECT. 2005;21(3):165–70.
Valdiserri EV. A possible interaction between lithium and diltiazem: case report. J Clin Psychiatry. 1985;46(12):540–1.
Dubovsky SL, Franks RD, Allen S. Verapamil: a new antimanic drug with potential interactions with lithium. J Clin Psychiatry. 1987;48(9):371–2.
Price WA, Shalley JE. Lithium-verapamil toxicity in the elderly. J Am Geriatr Soc. 1987;35(2):177–8.
Binder EF, Cayabyab L, Ritchie DJ, Birge SJ. Diltiazem-induced psychosis and a possible diltiazem-lithium interaction. Arch Intern Med. 1991;151(2):373–4.
Bruun NE, Ibsen H, Skøtt P, Toftdahl D, Giese J, Holstein-Rathlou NH. Lithium clearance and renal tubular sodium handling during acute and long-term nifedipine treatment in essential hypertension. Clin Sci (Lond). 1988;75(6):609–13.
Arthur RK. Letter: lithium levels and “Soda Bic” [letter]. Med J Aust. 1975;2(24):918.
McSwiggan C. Interaction of lithium and bicarbonate. Med J Aust. 1978;1(1):38–9.
Cerullo MA, Strakowski SM. The prevalence and significance of substance use disorders in bipolar type I and II disorder. Subst Abuse Treat Prev Policy. 2007;1(2):29.
Merry J, Reynolds CM, Bailey J, Coppen A. Prophylactic treatment of alcoholism by lithium carbonate. A controlled study. Lancet. 1976;4:481–2.
Judd LL, Huey LY. Lithium antagonizes ethanol intoxication in alcoholics. Am J Psychiatry. 1984;141(12):1517–21.
Fawcett J, Clark DC, Aagesen CA, et al. A double-blind, placebo-controlled trial of lithium carbonate therapy for alcoholism. Arch Gen Psychiatry. 1987;44(3):248–56.
Dorus W, Ostrow DG, Anton R, et al. Lithium treatment of depressed and nondepressed alcoholics. JAMA. 1989;262(12):1646–52.
Lexi-Interact Data Fields, Lexicomp®. Indianapolis: Wolters-Kluwer Health Clinical Solutions. http://webstore.lexi.com/Information/Product-Information/Lexi-Interact-Fields. Accessed 23 Jan 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Patrick R. Finley has no potential conflict of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Finley, P.R. Drug Interactions with Lithium: An Update. Clin Pharmacokinet 55, 925–941 (2016). https://doi.org/10.1007/s40262-016-0370-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-016-0370-y