Abstract
The pharmacokinetics of morphine in paediatrics have been widely studied using different approaches and modelling techniques. In this review, we explore advantages and disadvantages of the different data analysis techniques that have been applied, with specific focus on the accuracy of morphine clearance predictions by reported paediatric pharmacokinetic models. Twenty paediatric studies reported a wide range in morphine clearance values using traditional, rather descriptive methods. Clearance values were expressed per kilogram bodyweight, while maturation in clearance was described by comparing mean clearance per kilogram bodyweight between age-stratified subgroups. Population modelling allows for the analysis of sparse data, thereby limiting the burden to individual patients. Using this technique, continuous maturation profiles can be obtained on the basis of either fixed allometric scaling or comprehensive covariate analysis. While the models based on fixed allometric scaling resulted in complex maturation functions, all three paediatric population models for morphine yielded quite similar clearance predictions. The largest difference in clearance predictions between these three population models occurred in the first months of life, particularly in preterm neonates. Morphine clearance predictions by a physiologically based pharmacokinetic model were based on many continuous equations describing changes in underlying physiological processes across the full paediatric age range, and resulted in similar clearance predictions as well. However, preterm neonates could not be integrated in this model. In conclusion, the value of paediatric pharmacokinetic models is mostly dependent on clearance predictions and population concentration predictions, rather than on the individual description of data. For most pharmacokinetic models, however, the assessment of model performance was very limited and the accuracy of morphine clearance predictions as well as population concentration predictions was confirmed by formal evaluation and validation procedures for only one model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Dosing guidelines for children have originally been scaled from adult doses using functions related to body size (i.e. bodyweight). After years of clinical experience, these dosing guidelines are often formalized in (national) formularies. Research necessary to develop evidence-based, rather than consensus-based, dosing algorithms for the paediatric population is complicated by practical, ethical and legal constraints. However, advances in pharmacokinetic and pharmacodynamic analyses and the enormous increase in computing capacities of processors over the past few decades have opened up new possibilities in data analysis and data aggregation, yielding novel opportunities for paediatric pharmacological investigations.
Morphine is commonly prescribed for the paediatric population in hospital settings. Morphine clearance, its variability and the maturation in this parameter have been extensively studied across the paediatric population. This has led to the publication of a wide range of paediatric morphine clearance values, obtained with traditional methods as well as with the new computing-intensive modelling methodologies. Irrespective of the methodology used, reported clearance values should be representative for the studied population, because they provide the basis for paediatric dose adjustments and clinical decision making. Therefore, it is crucial that these values are both accurate and predictive for the next unstudied individual represented by the studied population.
Morphine is predominantly eliminated through glucuronidation by uridine diphosphate glucuronosyltransferase (UGT) 2B7 [1–3], thus morphine clearance directly reflects the formation of its two major metabolites morphine-3-glucuronide (M3G) and morphine-6-glucuronide (M6G). The metabolites are cleared through renal elimination and reduced renal function may result in accumulation of the metabolites. Since M3G and M6G are considered to be pharmacologically active [4], the fate of the metabolites after formation through morphine glucuronidation is of clinical importance. However, as only a limited number of publications have addressed the pharmacokinetics of the morphine metabolites in addition to the pharmacokinetics of morphine, the current review is limited to total morphine clearance.
2 Methods of Literature Search
PubMed was searched in November 2011 for original research on morphine clearance in the paediatric population. The search was limited to the last 20 years, including publications from January 1991 onwards. The following keywords were used: ‘morphine clearance’, ‘morphine metabolism’, ‘morphine glucuronidation’, ‘morphine elimination’ or ‘morphine pharmacokinetics’. Limits were set for age to include children between 0 and 18 years. Case reports were excluded. Only studies with intravenous administration were selected, to avoid confounding issues with bioavailability in the reported clearance values. Since the pharmacokinetics of drugs in patients on extracorporeal membrane oxygenation (ECMO) may depend on various components of the ECMO circuit itself [5, 6], studies in these patients were excluded as well. The obtained publications were categorized as analysed according to (1) traditional methods, (2) population pharmacokinetic modelling or (3) physiologically based pharmacokinetic modelling.
3 Clearance Estimates Obtained with Traditional Methods
3.1 Traditional Methods
Traditional methods to determine pharmacokinetic drug parameters in a population rely on firstly determining individual parameter values, using either compartmental or non-compartmental analysis techniques, after which each parameter is summarized as mean and standard deviation. As such, this yields for each pharmacokinetic parameter a point estimate (mean value) for the population and a measure of variability (standard deviation) in the population. This may be useful in early drug development, when data of a very limited number of patients are available. However, since intra-individual variability, measurement error and model misspecification cannot be distinguished from inter-individual variability with this method, other methods are preferred to describe and quantify trends in a population when more data become available.
As the determination of individual drug clearance values with compartmental methods relies on densely sampled concentration–time profiles for each subject, this method may not always be feasible, especially in the very young. Similarly, non-compartmental methods may not be feasible as they rely either on the area under the plasma concentration–time curve, which also requires dense sampling per individual, or on imprecise measurements of steady-state concentrations. Using traditional methods the maturation patterns in drug clearance are usually studied by expressing individual clearances per kilogram bodyweight, stratifying patients into age groups and comparing mean clearance values per kilogram bodyweight between the age groups. This allows for easy comparisons between studies and between age groups, but this makes findings on maturation dependent on the stratification and precludes the development of continuous maturation profiles. Additionally, it assumes clearance to scale linearly with bodyweight within the age groups, which may be a practical approximation when the range in bodyweight within each stratum is small, but it may not accurately reflect the underlying physiological changes across the entire human lifespan.
3.2 Morphine Clearance Determined with Traditional Methods
Table 1 provides an overview of paediatric morphine clearance values obtained with traditional methods. The reported morphine clearance values in neonates with a postnatal age from 0 to 30 days range from about 0.58 [7] to about 16 mL/min/kg [8], which is a more than 20-fold difference. In infants aged 1 month to 1 year, morphine clearances were reported to range between 7.8 [9] and 69.4 mL/min/kg [8, 10], while in children from 1 to 18 years the range in morphine clearance was reported to vary from about 12 [11] to about 60 mL/min/kg [12]. The wide ranges in reported clearance values within each age group may in part be explained by the differences between studies in terms of patient characteristics, sampling schemes or dosing schemes, but are probably mainly caused by the relative imprecision of the applied data analysis methods. Additionally, most studies are based on a relatively small number of individuals (Table 1), limiting the precision of each finding.
4 Clearance Estimates Obtained with Population Modelling
4.1 Population Modelling
Increases in computing power now allow for the analysis of concentration–time measurements from a population as a whole while considering individuals as constituents of this population. This method is called population or nonlinear mixed-effects modelling. As long as data are sufficiently informative, population modelling can be used for the analysis of dense, sparse and/or unbalanced data. This is especially beneficial for the vulnerable paediatric population as it allows for the analysis of a limited number of blood samples per patient and for the analysis of data obtained during routine clinical practice. Additionally, it may allow for the meta-analysis of data from multiple studies with different designs, thereby reducing the burden for individual paediatric patients. A proper covariate analysis does, however, require information on the same set of covariates in each individual dataset. Since data from various sources can be analysed simultaneously, the precision of the findings may also increase.
Population modelling can also distinguish inter-individual variability from intra-individual variability, measurement error and model misspecification. By identifying which patient characteristics (e.g. age, bodyweight, sex, race, genetics, disease status) are predictors of the inter-individual variability in model parameters, trends in the population can be identified and quantified. These predictors are known as covariates and the relationship between a covariate and a model parameter is known as the covariate relationship. Typically, population pharmacokinetic modelling relies on outcome measures and information on covariates. Concentration data for pharmacokinetic models can be obtained relatively easily from blood samples. Covariate relationships in the population models generally include patient information that can be obtained from medical records or from routine clinical measurements. An important feature of population pharmacokinetic modelling is that it allows for the identification of continuous maturation profiles that do not depend on stratifications and that, when pharmacodynamic relationships remain constant with age, the covariate relationships describing this maturation can be directly used as the basis of evidence-based dosing algorithms. Since steady-state drug concentrations are solely dependent on drug clearance and peak concentrations heavily dependent on distribution volume, the covariate relationships for these parameters can be directly incorporated in the algorithms of paediatric maintenance or loading doses, respectively. However, since the use of sparse data may increase the risk of drawing wrong conclusions, population models require an advanced level of evaluation and validation before a model can be accepted [13].
One of the approaches that can be applied for paediatric population covariate modelling is fixed allometric scaling [14]. Using this approach, bodyweight is included a priori in the model as a covariate on clearance (CL) according to the following allometric equation (Eq. 1):
where BWi is the bodyweight of the individual paediatric patient in kilograms, which is normalized to an average adult bodyweight of 70 kg. The value of the exponent ‘b’ is fixed to 0.75 for clearance, and ‘a’ represents the magnitude of clearance in adults, which is estimated. This fixed allometric equation describes the influence of changes in body size on drug clearance and on average predicts paediatric drug clearances with a fair degree of accuracy in children older than 5 years [15]. In younger children the allometric equation is augmented with an age-based function called the ‘maturation model’ to describe the remaining influence of developmental changes on drug clearance. Additional covariate relationships that reflect the influence of altered function of elimination organs (i.e. liver or kidneys) may be incorporated as well [14].
The fixed allometric scaling approach is frequently applied, despite theoretical and data-driven studies challenging the hypothesis that the allometric equations accurately describe the influence of body size on pharmacokinetic processes [16–23]. Additionally, with the inclusion of bodyweight, part of the influence of age is included as well, due to the strong correlation between bodyweight and age in the paediatric population. This makes the maturation model a mathematical residue of the influence of age that remains after the inclusion of the correlated covariate bodyweight, rather than a descriptor of maturation per se. Moreover, since bodyweight and age are included without formal testing for significance, there is a risk of over-parameterizing the models, leading to imprecise parameter estimates. Finally, special attention is required for the interpretation of these models. Due to the separation of the influence of body size (expressed by bodyweight) and maturation (expressed by age), the statement that maturation is completed at a certain age does not in this context mean that absolute clearance has reached adult values, as body size is usually still increasing. Misinterpretation of such results can lead to over-dosing when used for paediatric dose adjustments, and therefore the expression of the pharmacokinetic parameters per 70 kg may be unwarranted, particularly in neonates.
Another approach in paediatric population pharmacokinetic modelling is the application of a comprehensive covariate analysis, in which all potential covariates for the pharmacokinetic parameter are tested in various relationships and are included in the model based on statistical significance. This procedure can be used to identify demographic factors or co-morbidities that significantly influence drug clearance. In the paediatric population it can also be used to identify covariate relationships that describe functional maturational changes in drug clearance [24]. The paediatric covariate relationships are usually based on bodyweight, age or a combination of both, and may vary in nature (e.g. exponential or linear). It should be noted, however, that these covariate relationships are empirical and that bodyweight or age should not be regarded as the drivers of the observed changes in drug pharmacokinetics, but as surrogate descriptors of the net changes in the underlying physiological system. The descriptive nature of these covariate relationships explicitly preclude extrapolations outside the covariate value range in the learning dataset.
4.2 Morphine Clearance Determined with Population Modelling
4.2.1 Bouwmeester et al. (2004)
The model by Bouwmeester et al. [25] comprises morphine as well as its two main metabolites M3G and M6G. The model is based on data from 184 term neonates to infants up to the age of 3 years from Van Dijk et al. [26].
The Bouwmeester et al. [25] model was developed using fixed allometric scaling principles described in Sect. 4.1. The maturation model for the formation of morphine glucuronides was an exponential model based on postnatal age, and serum bilirubin concentrations were included as a covariate on morphine glucuronidation. Eqs. 2–4 show how total morphine clearance is described by the Bouwmeester et al. [25] model:
where CLtot is the total morphine clearance (L/h), CLM3G and CLM6G are the formation clearance (L/h) of M3G and M6G, respectively, and CLR is the residual clearance (L/h) through alternative pathways. BWi is the bodyweight of the individual paediatric patient in kilograms, PNA is the postnatal age in days, Cbili is the serum bilirubin concentration (μmol/L) and EXP is the exponent. Total morphine clearance is 71.1 L/h/70 kg0.75, and from the maturation model it can be derived that the adult value of morphine glucuronidation is reached between the ages of 6 and 12 months. Absolute morphine glucuronidation is, however, still increasing after that age, as a result of changes in bodyweight, which is described by the allometric function.
Model performance was corroborated by plots of the ratio of observed and individual morphine and metabolite concentrations versus time, which showed limited bias. Results of other diagnostics, in particular plots of population-predicted concentrations versus observed concentrations, were not reported. More recently, this model has been evaluated by our group using both the learning dataset and external datasets [27]. With a condition number of 10,698, the model was shown to be over-parameterized, resulting in imprecise parameter estimates that caused the bootstrapped parameter value for a number of parameters to deviate by more than 10 % from the originally reported values. Plots of predicted concentrations versus observed concentrations revealed accurate individual concentration predictions, suggesting that morphine concentrations can be described accurately when at least one observation per individual is available, although high shrinkage values render the diagnostics based on individual predictions to be potentially misleading. Population concentration predictions were found to be biased. This suggests that model-based concentration predictions based on age, bodyweight and bilirubin concentrations of a child alone are inaccurate. Additionally, simulation-based diagnostics showed bias towards over-prediction of morphine concentrations in the population as a whole. The cause of this bias was diagnosed to originate from structural model misspecification, since plots of individual and population parameter estimates versus the primary covariate bodyweight revealed that the covariate relationships describe the maturational changes in model parameters with bias, which was reflected in mean prediction errors (MPEs) for the predictions of total morphine clearance in the external dataset of 86 and −27 % in term neonates and toddlers, respectively. A claimed advantage of the application of fixed allometric scaling principles is that it allows for predictions outside the studied age range; however, clearance predictions in preterm neonates were found to have an MPE of 192 %, while clearance predictions in older children have never been assessed [27].
4.2.2 Anand et al. (2008)
The population pharmacokinetic model by Anand et al. [28] was based on morphine concentrations obtained from 875 preterm neonates as well as on the data from the 184 term neonates and infants from Van Dijk et al. [26] that were previously analysed by Bouwmeester et al. [25]. The pharmacologically active morphine metabolites were not included in this model.
The Anand et al. [28] model continued to build on the concepts introduced in the publication by Bouwmeester et al. [25]. Fixed allometric scaling was augmented by a maturation model, in which the best fit was obtained with a sigmoidal model based on postmenstrual age, compared to an exponential model. Covariates based on organ function (i.e. serum bilirubin concentrations to reflect hepatic function) were not included, but a scaling factor to adjust morphine clearance in preterm neonates in comparison to term neonates was included. There is some ambiguity on which parameter this fraction for preterm neonates is applied, as both the standard adult value of morphine clearance and the postmenstrual age at which half the allometric adult value of morphine clearance is reached are mentioned. Most probably, the preterm factor was applied to the standard value of morphine clearance, indicating that morphine clearance in preterm neonates is 61 % of the clearance in term neonates. This reduction remains constant throughout the full age range described in the model. Eqs. 6 and 7 show how total paediatric morphine clearance is described by the Anand et al. [28] model:
or
where CLtot,term and CLtot,preterm represent total morphine clearance (L/h) in term and preterm patients, respectively, BWi is the bodyweight of the individual paediatric patient in kilograms and PMA is the postmenstrual age in weeks. According to the maturation model, half the standard adult value of morphine clearance is reached at a postmenstrual age of 54 weeks. Around the postnatal age of 1 year, the influence of the maturation models becomes negligible, after which the increase in absolute clearance is described solely by bodyweight in the allometric equation.
In terms of model evaluation and validation procedures, diagnostics based on individual as well as population concentration predictions are reported, although due to their layout it is difficult to assess the accuracy of the predictions from these plots. No other results on model evaluation and validation were reported. The Anand et al. [28] model was further evaluated by Mahmood [29] using external data. The MPE in total morphine clearance ranged between 8 % in preterm neonates, 19 % in term neonates and 21 % in toddlers between 1 week and 2 months of age, while the MPE was 1.5 % in toddlers between 2 and 10 months of age. The MPE in clearance predictions in children between the age of 3 and 5 years, which was older than the age range in the internal dataset, was 17 %.
4.2.3 Knibbe et al. (2009)
The model by Knibbe et al. [30] was also based on data from the 184 term neonates and infants of Van Dijk et al. [26]. Additionally, data from Simons et al. [31] on 64 preterm and term neonates were added. Both morphine and its main metabolites were included in the model.
Model development of the Knibbe et al. [30] model was based on a comprehensive covariate analysis. Bodyweight, bodyweight at birth, body surface area, sex, postnatal age, postmenstrual age, serum bilirubin concentration, creatinine clearance, mechanical ventilation, surgery versus non-surgery, and type of surgery were investigated as potential covariates on clearance in equations of various forms. Differences in morphine glucuronidation were best described by a bodyweight-based exponential equation with an estimated exponent of 1.44. Within this equation the formation clearance of the morphine glucuronides was found to be reduced in neonates younger than 10 days. This discontinuity did not result from stratification of the data, but from the observed differences in morphine clearance between young neonates and older patients after inclusion of the bodyweight-based covariate relationship. Compared with inclusion of age in a continuous relationship or to age cut-points at 3, 7, 14 or 21 days, inclusion of a discontinuity at the postnatal age of 10 days provided the best mathematical description of this observed difference according to predefined statistical criteria. Physiologically, a rapid but continuous change is, however, more probable. Clearance through pathways other than glucuronidation was found to be not significant and therefore was not included in the model. Equations 8–10 show how total morphine clearance is described by the Knibbe et al. [30] model:
where CLtot is total morphine clearance (mL/min), CLM3G and CLM6G are the formation clearance (mL/min) of M3G and M6G, respectively, with different values for neonates younger than 10 days and older patients, and BWi is the bodyweight (kg) of the individual paediatric patient.
The model was evaluated using various methods with the learning dataset and later also with external datasets [27, 32]. With a condition number of 293 the model was found to be not over-parameterized, which resulted in precise parameter estimates causing the bootstrapped parameter values also to be within 10 % of the originally reported value for all parameters. Plots of individual predicted morphine concentrations versus observed concentrations were minimally biased, although the value of diagnostics based on individual predictions is limited due to high shrinkage. Population-predicted concentrations showed limited bias. Simulation-based diagnostics further confirmed that the model could accurately predict morphine concentrations based on bodyweight and age alone in children under the age of 3 years who, similar to the patients in the learning dataset, had undergone major non-cardiac surgery or were mechanically ventilated. Additionally, it was confirmed that covariate relationships describe individual parameter values accurately, with MPEs for total morphine clearance in the external datasets of 17 % for preterm neonates and 30 % for term neonates and toddlers [11]. The exponential increase in morphine clearance with bodyweight explicitly precludes this model from making clearance predictions in children older than 3 years.
Table 2 summarizes the details of the pharmacokinetic population models discussed in Sect. 4. For comparison, Table 3 lists the absolute clearance values and clearance values per kilogram bodyweight for nine hypothetical patients, predicted by each of these three population models. The largest differences in predicted morphine clearance values between the models are observed at the extremes of the age ranges of the models, with a difference of almost a factor 2 in the first month of life and around a 30 % difference at the age of 3 years. Particularly large differences were found for preterm neonates aged 1 day to 2 weeks, and term neonates aged 2 weeks.
5 Clearance Estimates Obtained with Physiologically Based Pharmacokinetic Modelling
5.1 Physiologically Based Pharmacokinetic Modelling
In physiologically based pharmacokinetic models, an exhaustive set of mathematical equations mechanistically describe and quantify the interaction between a drug molecule with specific physicochemical properties and the underlying physiological system. Additionally, interactions within the physiological system are described and quantified. These equations and the constants within these equations thereby aggregate compound-specific information with anatomical measurements and in vitro or in vivo physiological information. So, while population modelling yields models for a specific drug in a specified population, physiologically based models are more generalizable and nonspecific for particular drugs.
Physiologically based pharmacokinetic models require a wider variety of information than population modelling. Some of this information may be difficult to obtain, but since a substantial part of this information relates to underlying (patho)physiological processes, rather than to specific drugs, this information needs to be obtained only once. With the current gaps in our knowledge on human physiology and maturation, years of research are still required to properly describe and quantify all physiological parameters and interactions. However, the influence of some parameters or interactions on the overall drug pharmacokinetics may be negligible and with the major physiological determinants of pharmacokinetic processes currently being well described, physiologically based models have already been proven useful to make inferences about the changes in the pharmacokinetics of drugs that have not yet been studied in a particular population [33–35]. The additional research in this area is successively refining these models or extending their application to special populations.
The paediatric population can be included in this approach by integrating information on maturational changes in the physiological system into the model. Maturation of drug clearance is not defined for specific drugs, but for specific elimination routes such as glomerular filtration or biotransformation through various phase I and phase II enzymes. As morphine is mainly eliminated through hepatic glucuronidation by the UGT2B7 isoenzyme [1–3], information on ontogeny (i.e. expression and function) of this enzyme system is required, as well as maturational changes in liver size, hepatic blood flow and perfusion, plasma protein binding and active hepatic transport mechanisms. As maturation profiles in physiologically based pharmacokinetic models are established for all of the underlying physiological changes, the developmental changes in pharmacokinetic parameters are described by a wide variety of mostly nonlinear equations. This enables the determination of pharmacokinetic parameters for drugs with specific properties in individuals for which certain key demographics (e.g. bodyweight and age) are known, which may be helpful in the development of first-in-child doses. However, the net maturation profile of pharmacokinetic parameters in a population as a whole cannot be directly derived. This complicates the establishment of evidence-based dosing guidelines from physiologically based pharmacokinetic models.
5.2 Morphine Clearance Determined with Physiologically Based Pharmacokinetic Modelling
5.2.1 Edginton et al. (2006)
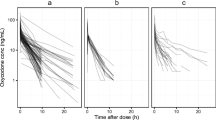
The publication by Edginton et al. [36] is the only publication that we retrieved that compares overall in vivo morphine clearance predictions by a physiologically based pharmacokinetic model to observed in vivo morphine clearances in the paediatric population. In the Edginton et al. [36] model, hepatic UGT2B7 ontogeny profiles were derived from literature values of in vivo clearance as well as from in vitro determinations of enzyme activity for morphine and lorazepam. First, in vitro determinations of paediatric UGT2B7 enzyme activity were expressed as a percentage of adult activity. This information was subsequently combined with maturational changes in the underlying physiological processes and in vivo adult morphine clearance values, to obtain model-predicted in vivo paediatric clearance parameters. The in vivo maturation profile of morphine glucuronidation over the entire paediatric age range was obtained by determining mean morphine clearance per kilogram of bodyweight at 17 distinct ages and generating a cubic spline of mean morphine clearance versus age. Available paediatric in vivo clearance values for morphine and lorazepam were used to further adjust the UGT2B7 ontogeny profile to provide the best visual fit of in vivo predicted drug clearances to the observed clearances. This yielded a bi-phasic maturation profile describing the net influence of underlying physiological changes on in vivo morphine clearance expressed per kilogram of bodyweight.
Optimization of the in vivo maturation profiles was based on visual improvement of how well the predicted profile described in vivo literature data, but this model fit was not numerically quantified. Age was selected as the descriptor for the UGT2B7 ontogeny profile in the Edginton et al. [36] model, but the ambiguity about how to quantify maturation in the first few days of life, especially comparing preterm and term neonates, could not be resolved. Therefore, this model used one single clearance value for all premature neonates, irrespective of postnatal or postmenstrual age. Additionally, since the maturation profile was not compared to individual clearance data, but to mean study values in stratified age ranges, the quality of model fit could not be assessed properly. In the manuscript, the predictive performances of the enzyme ontogeny models are tested on paediatric data from test compounds that are eliminated through multiple elimination pathways. However, this is not an ideal method to test the prediction of the clearance profiles of individual elimination routes. Alternatively, the UGT2B7 ontogeny profile was later used in a full physiologically based pharmacokinetic model to assess the accuracy of morphine concentration predictions [34]. It was found that the predicted morphine concentrations were on average within a factor 2.06 from the observed value. However, in preterm neonates, a clear trend towards under-prediction of concentrations, and thus over-prediction of clearance, was observed.
6 Discussion
Morphine pharmacokinetics have been widely studied in the paediatric population, with a relatively large amount of this research being performed in children in the first few days to months of life. The majority of traditional pharmacokinetic studies in Sect. 3 were performed in the younger age ranges and the three population pharmacokinetic models in Sect. 4 only included patients up to the age of 3 years. This is probably not only because most developmental changes occur in the early life stages but also because these very young patients are encountered most frequently in hospital settings and paediatric intensive care units. Only the physiologically based pharmacokinetic model in Sect. 5 covers the entire paediatric age range.
As can be seen in Table 1, there is a 20-fold difference in the reported morphine clearances by traditional methods in neonates, which narrows down to about a 3-fold difference in older children and adolescents. The predicted clearance values from the three population models fall within the range of morphine clearance values obtained with the traditional methods. When the three population models are compared, the difference in morphine clearance predictions is most prominent in preterm neonates (which were not included in the Bouwmeester et al. [25] model) and in patients in the first few months of life, as illustrated in Table 3. The morphine clearance predictions by the Edginton et al. [36] model are also in the same range as the other studies, but an explicit relationship describing the developmental changes in morphine clearance in the paediatric population is lacking, as the maturation of underlying physiological processes instead of clearance are quantified.
The three paediatric population pharmacokinetic models for morphine discussed in Sect. 4 were assessed for the accuracy of both their population concentration predictions and clearance predictions. The model by Knibbe et al. [30] was the only model for which accurate concentration predictions were confirmed as bias in individual as well as population concentration-predicted versus observed concentration plots was found to be minimal. Especially the Bouwmeester et al. [25] model proved to have poor population concentration predictions, while the population concentration predictions by the Anand et al. [28] model were difficult to assess. With regards to MPEs of the population predictions of total morphine clearance, the error of the Bouwmeester et al. [25] model reached up to 85 % [27]. For the Anand et al. [28] model the MPE of total morphine clearance ranged between 8 and 21 % [29], while for the Knibbe et al. [30] model this ranged between 17 and 30 % [27]. The MPEs reported for the Anand et al. [28] model cannot be directly compared to the reported MPEs of the Bouwmeester et al. [25] model and the Knibbe et al. [30] model, as different external data were used as well as different age ranges of the paediatric subsets and different methods were used to determine individual morphine clearances. However, these results suggest the accuracy of total morphine clearance predictions by the Anand et al. [28] and Knibbe et al. [30] models to be in a similar range, despite the fact that the Anand et al. [28] model was based on data from a larger number of preterm neonates than the Knibbe et al. [30] model. This illustrates that model performance not only depends on data density, but also on the quality of that data, showing that data should be obtained at timepoints that are informative for the various pharmacokinetic processes.
Concerning the physiologically based model by Edginton et al. [36], the method to assess the model predictions was not quantitative and the visual tools were not optimal, making it difficult to assess the morphine clearance predictions by this model. However, morphine concentration predictions by this model were on average within a factor 2 from the observed value, which could be regarded as acceptable for determining first-in-child doses or inter-drug scaling of new drugs in the paediatric population.
As biased clearance predictions can be harmful when used for paediatric dose adjustments or clinical decision making, we would like to emphasize that proper model evaluation and validation for all paediatric population pharmacokinetic models is of utmost importance. It should, however, be noted that most evaluation and validation procedures assess the accuracy of model predictions for a population as a whole. As mentioned by Mahmood [29], the inter-individual variability in paediatric morphine clearance is high, causing the prediction error in individual clearances to be high even with the most accurate population model. As a result, clinical monitoring is still important in paediatric patients receiving morphine treatment.
As illustrated in Fig. 1, population modelling and physiologically based modelling approach the study of the pharmacokinetics of a drug from opposite perspectives, and are therefore often referred to as the ‘top-down’ and ‘bottom-up’ approach, respectively. Inherent to these different perspectives is a difference in the nature of the data that are required for these models. Physiologically based pharmacokinetic models require a vast amount of data, which are generalizable but may not always prove to significantly influence net pharmacokinetic parameters, while population pharmacokinetic models only allow for the quantification of rate-limiting processes that are not always generalizable and have to be repeated for every new drug studied in every new population. Future endeavours in paediatric pharmacology will therefore benefit from using the physiological insight and generalizability of physiologically based models while restricting the focus to significant and rate-limiting processes, as is done with population modelling. This will yield hybrid models that meet in between the top-down and bottom-up approaches and expedite paediatric model development [37, 38].
Population pharmacokinetic modelling and physiologically based pharmacokinetic modelling are often referred to as the ‘top-down’ and ‘bottom-up’ approach, respectively. Population modelling derives in vivo pharmacokinetic parameters from clinically observed drug concentrations, whereas physiologically based modelling derives this information by aggregating physiochemical information of the drug with anatomical and physiological information of the biological system [bottom part of figure reproduced from Johnson et al. [33], with permission from Springer International Publishing Switzerland (© Adis Data Information BV [2006]. All rights reserved.)]. τ dosage interval, B/P blood plasma ratio, CL apparent total body clearance of the drug from plasma, CL/F oral clearance, CL H hepatic clearance of the drug from plasma, CL int intrinsic clearance, CL R renal clearance, CYP cytochrome P450, f Gut fraction of the dose that escapes gut wall metabolism, f H fraction escaping liver extraction, f u fraction unbound in plasma, f uGut unbound fraction in gut (enterocyte), f uMic unbound fraction in microsomes, k a absorption rate constant, Km Michaelis–Menten constant, MW molecular weight, Q Gut drug-specific nominal blood flow/permeability descriptor, V d volume of distribution, V max maximum rate of metabolism
One of the disadvantages of both population modelling and physiologically based modelling is that they require specialized software and skilled professionals to design studies and perform the analyses. Additionally, with the mathematical equations that describe and quantify maturational changes in clearance values in the paediatric population becoming more complex, reported clearance values also become more difficult to interpret and compare. Particularly, the use of fixed allometric scaling principles in combination with age-based maturation functions [14] results in a combined function of two highly nonlinear relationships for the maturation of morphine clearance in the Bouwmeester et al. [25] and Anand et al. [28] models. Since the analysis of data generated in population pharmacokinetic studies often yields complex covariate relationships, evidence-based dosing algorithms also grow increasingly complex. As dosing algorithms should be as simple as possible, but not simpler, special attention is required to implement these regimens in clinical practice. This may require a closer involvement of the hospital pharmacist in patient care to optimize and individualize drug dosing and to avoid dosing errors [39].
To date, most paediatric pharmacological research has focused on drug pharmacokinetics. This is because clearance is generally believed to be the main driver of required dose adjustments in the paediatric population [40]. When pharmacokinetic models are used to derive evidence-based paediatric dosing algorithms, it is implicitly assumed that the pharmacodynamics remain constant. This assumption is acceptable when (1) pathophysiological processes are similar in adults and children, (2) the exposure-effect relationship can be assumed independent of age based on the mechanism of action and (3) the clinical endpoints for treatment are the same in both populations [41]. Morphine does not meet these criteria as the expression of the μ-opioid receptor may differ between age groups, and as the clinical endpoints for pain differ in adults and children. This implies that morphine pharmacodynamics need to be studied as well to establish age-appropriate target concentrations. Future paediatric pharmacodynamic studies are therefore necessary to derive final dosing algorithms in this population that account for both pharmacokinetic and pharmacodynamic changes.
7 Conclusion
Traditional compartmental and non-compartmental analysis approaches, population modelling and physiologically based pharmacokinetic modelling have been applied to study morphine clearance and the maturational changes in this parameter in the paediatric population. This has led to a variety of reported values for paediatric morphine clearance and functions for the maturation profiles of this parameter. However, absolute predicted clearance values obtained with the different methods seem to be in good agreement, except in preterm and term born neonates and infants in the first 3 months of life. The predictive value of models is determined by accurate clearance predictions (quantified by MPE values) and concentration predictions (assessed in population-predicted vs. observed plots). The Knibbe et al. [30] model was the only model for which accurate concentration predictions on the individual as well as population level were corroborated throughout the full age range of the model and for both morphine and its metabolites. With regards to the prediction of total morphine clearance, the Anand et al. [28] model and Knibbe et al. [30] model have similar accuracies, although the Anand model did not include the pharmacologically active metabolites.
References
Coffman BL, Rios GR, King CD, Tephly TR. Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Dispos. 1997;25:1–4.
Court MH, Krishnaswamy S, Hao Q, Duan SX, Patten CJ, Von Moltke LL, et al. Evaluation of 3′-azido-3′-deoxythymidine, morphine, and codeine as probe substrates for UDP-glucuronosyltransferase 2B7 (UGT2B7) in human liver microsomes: specificity and influence of the UGT2B7*2 polymorphism. Drug Metab Dispos. 2003;31:1125–33.
Morrish GA, Foster DJR, Somogyi AA. Differential in vitro inhibition of M3G and M6G formation from morphine by (R)- and (S)-methadone and structurally related opioids. Br J Clin Pharmacol. 2006;61:326–35.
Osborne R, Thompson P, Joel S, Trew D, Patel N, Slevin M. The analgesic activity of morphine-6-glucuronide. Br J Clin Pharmacol. 1992;34:130–8.
Buck ML. Pharmacokinetic changes during extracorporeal membrane oxygenation: implications for drug therapy of neonates. Clin Pharmacokinet. 2003;42:403–17.
Bhatt-Meht V, Annich G. Sedative clearance during extracorporeal membrane oxygenation. Perfusion. 2005;20:309–15.
Roka A, Melinda KT, Vasarhelyi B, Machay T, Azzopardi D, Szabo M. Elevated morphine concentrations in neonates treated with morphine and prolonged hypothermia for hypoxic ischemic encephalopathy. Pediatrics. 2008;121:e844–9.
Lynn AM, Nespeca MK, Bratton SL, Shen DD. Intravenous morphine in postoperative infants: intermittent bolus dosing versus targeted continuous infusions. Pain. 2000;88:89–95.
Scott CS, Riggs KW, Ling EW, Fitzgerald CE, Hill ML, Grunau RV, et al. Morphine pharmacokinetics and pain assessment in premature newborns. J Pediatr. 1999;135:423–9.
Lynn A, Nespeca MK, Bratton SL, Strauss SG, Shen DD. Clearance of morphine in postoperative infants during intravenous infusion: the influence of age and surgery. Anesth Analg. 1998;86:958–63.
Dagan O, Klein J, Bohn D, Barker G, Koren G. Morphine pharmacokinetics in children following cardiac surgery: effects of disease and inotropic support. J Cardiothorac Vasc Anesth. 1993;7:396–8.
Dampier CD, Setty BN, Logan J, Ioli JG, Dean R. Intravenous morphine pharmacokinetics in pediatric patients with sickle cell disease. J Pediatr. 1995;126:461–7.
Tod M, Jullien V, Pons G. Facilitation of drug evaluation in children by population methods and modelling. Clin Pharmacokinet. 2008;47:231–43.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24:25–36.
Mahmood I. Theoretical versus empirical allometry: facts behind theories and application to pharmacokinetics. J Pharm Sci. 2010;99:2927–33.
Dodds PS, Rothman DH, Weitz JS. Re-examination of the “3/4-law” of metabolism. J Theor Biol. 2001;209:9–27.
Agutter PS, Wheatley DN. Metabolic scaling: consensus or controversy? Theor Biol Med Model. 2004;1:13.
Bokma F. Evidence against universal metabolic allometry. Funct Ecol. 2004;18:184–7.
Glazier DS. Beyond the ‘3/4-power law’: variation in the intra- and interspecific scaling of metabolic rate in animals. Biol Rev. 2005;80:611–62.
White CR, Cassey P, Blackburn TM. Allometric exponents do not support a universal metabolic allometry. Ecology. 2007;88:315–23.
Kolokotrones T, Van S, Deeds EJ, Fontana W. Curvature in metabolic scaling. Nature. 2010;464:753–6.
Mahmood I. Prediction of drug clearance in children from adults: a comparison of several allometric methods. Br J Clin Pharmacol. 2006;61:545–57.
Mahmood I. Prediction of drug clearance in children: impact of allometric exponents, body weight, and age. Ther Drug Monit. 2007;29:271–8.
De Cock RF, Piana C, Krekels EH, Danhof M, Allegaert K, Knibbe CA. The role of population PK–PD modelling in paediatric clinical research. Eur J Clin Pharmacol. 2011;67:5–16.
Bouwmeester NJ, Anderson BJ, Tibboel D, Holford NH. Developmental pharmacokinetics of morphine and its metabolites in neonates, infants and young children. Br J Anaesth. 2004;92:208–17.
Van Dijk M, Bouwmeester NJ, Duivenvoorden HJ, Koot HM, Tibboel D, Passchier J, et al. Efficacy of continuous versus intermittent morphine administration after major surgery in 0–3-year-old infants; a double-blind randomized controlled trial. Pain. 2002;98:305–13.
Krekels EH, van Hasselt JG, Tibboel D, Danhof M, Knibbe CA. Systematic evaluation of the descriptive and predictive performance of paediatric morphine population models. Pharm Res. 2011;28:797–811.
Anand KJ, Anderson BJ, Holford NH, Hall RW, Young T, Shephard B, et al. Morphine pharmacokinetics and pharmacodynamics in preterm and term neonates: secondary results from the NEOPAIN trial. Br J Anaesth. 2008;101:680–9.
Mahmood I. Evaluation of a morphine maturation model for the prediction of morphine clearance in children: how accurate is the predictive performance of the model? Br J Clin Pharmacol. 2011;71:88–94.
Knibbe CA, Krekels EH, van den Anker JN, DeJongh J, Santen GW, van Dijk M, et al. Morphine glucuronidation in preterm neonates, infants and children younger than 3 years. Clin Pharmacokinet. 2009;48:371–85.
Simons SH, van Dijk M, Van Lingen RA, Roofthooft D, Duivenvoorden HJ, Jongeneel N, et al. Routine morphine infusion in preterm newborns who received ventilatory support: a randomized controlled trial. JAMA. 2003;290:2419–27.
Krekels EH, DeJongh J, Van Lingen RA, Van der Marel CD, Choonara I, Lynn AM, et al. Predictive performance of a recently developed population pharmacokinetic model for morphine and its metabolites in new datasets of (preterm) neonates, infants and children. Clin Pharmacokinet. 2011;50:51–63.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45:931–56.
Edginton AN, Schmitt W, Willmann S. Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet. 2006;45:1013–34.
Fagerholm U. Prediction of human pharmacokinetics: evaluation of methods for prediction of hepatic metabolic clearance. J Pharm Pharmacol. 2007;59:803–28.
Edginton AN, Schmitt W, Voith B, Willmann S. A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet. 2006;45:683–704.
Krekels EH, Panoilia E, Neely M, Tibboel D, Capparelli E, Danhof M, et al. Maturation of glucuronidation; a system specific property [poster]. PAGE 20th meeting; 2011 Jun 7–10; Athens.
De Cock RFW, Allegaert K, Sherwin CMT, de Hoog M, van den Anker JN, Danhof M, et al. Maturation of GFR in preterm and term neonates reflected by clearance of different antibiotics [abstract no. 2096]. PAGE 20th meeting; 2011 Jun 7–10; Athens.
Knibbe CA, Danhof M. Individualized dosing regimens in children based on population PKPD modelling: are we ready for it? Int J Pharm. 2011;415:9–14.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part I. Clin Pharmacokinet. 2002;41:959–98.
Knibbe CA, Krekels EH, Danhof M. Advances in paediatric pharmacokinetics. Expert Opin Drug Metab Toxicol. 2011;7:1–8.
Hartley R, Green M, Quinn M, Levene MI. Pharmacokinetics of morphine infusion in premature neonates. Arch Dis Child. 1993;69:55–8.
Saarenmaa E, Neuvonen PJ, Rosenberg P, Fellman V. Morphine clearance and effects in newborn infants in relation to gestational age. Clin Pharmacol Ther. 2000;68:160–6.
Barrett DA, Barker DP, Rutter N, Pawula M, Shaw PN. Morphine, morphine-6-glucuronide and morphine-3-glucuronide pharmacokinetics in newborn infants receiving diamorphine infusions. Br J Clin Pharmacol. 1996;41:531–7.
Chay PC, Duffy BJ, Walker JS. Pharmacokinetic-pharmacodynamic relationships of morphine in neonates. Clin Pharmacol Ther. 1992;51:334–42.
Mikkelsen S, Feilberg VL, Christensen CB, Lundstrom KE. Morphine pharmacokinetics in premature and mature newborn infants. Acta Paediatr. 1994;83:1025–8.
Barrett DA, Elias-Jones AC, Rutter N, Shaw PN, Davis SS. Morphine kinetics after diamorphine infusion in premature neonates. Br J Clin Pharmacol. 1991;32:31–7.
Pokela ML, Olkkola KT, Seppala T, Koivisto M. Age-related morphine kinetics in infants. Dev Pharmacol Ther. 1993;20:26–34.
Choonara I, Lawrence A, Michalkiewicz A, Bowhay A, Ratcliffe J. Morphine metabolism in neonates and infants. Br J Clin Pharmacol. 1992;34:434–7.
Haberkern CM, Lynn AM, Geiduschek JM, Nespeca MK, Jacobson LE, Bratton SL, et al. Epidural and intravenous bolus morphine for postoperative analgesia in infants. Can J Anaesth. 1996;43:1203–10.
McRorie TI, Lynn AM, Nespeca MK, Opheim KE, Slattery JT. The maturation of morphine clearance and metabolism. Am J Dis Child. 1992;146:972–6.
Hain RD, Hardcastle A, Pinkerton CR, Aherne GW. Morphine and morphine-6-glucuronide in the plasma and cerebrospinal fluid of children. Br J Clin Pharmacol. 1999;48:37–42.
Mashayekhi SO, Ghandforoush-Sattari M, Routledge PA, Hain RD. Pharmacokinetic and pharmacodynamic study of morphine and morphine 6-glucuronide after oral and intravenous administration of morphine in children with cancer. Biopharm Drug Dispos. 2009;30:99–106.
Kopecky EA, Jacobson S, Joshi P, Koren G. Systemic exposure to morphine and the risk of acute chest syndrome in sickle cell disease. Clin Pharmacol Ther. 2004;75:140–6.
Robieux IC, Kellner JD, Coppes MJ, Shaw D, Brown E, Good C, et al. Analgesia in children with sickle cell crisis: comparison of intermittent opioids vs. continuous intravenous infusion of morphine and placebo-controlled study of oxygen inhalation. Pediatr Hematol Oncol. 1992;9:317–26.
Van Lingen RA. Pain assessment and analgesia in the newborn: an integrated approach [thesis]. Rotterdam: Erasmus University; 2000.
Van der Marel CD, Peters JW, Bouwmeester NJ, Jacqz-Aigrain E, van den Anker JN, Tibboel D. Rectal acetaminophen does not reduce morphine consumption after major surgery in young infants. Br J Anaesth. 2007;98:372–9.
Peters JW, Anderson BJ, Simons SH, Uges DR, Tibboel D. Morphine pharmacokinetics during venoarterial extracorporeal membrane oxygenation in neonates. Intensive Care Med. 2005;31:257–63.
Peters JW, Anderson BJ, Simons SH, Uges DR, Tibboel D. Morphine metabolite pharmacokinetics during venoarterial extra corporeal membrane oxygenation in neonates. Clin Pharmacokinet. 2006;45:705–14.
Hanekamp MN. Short and long term studies in neonates treated with extracorporeal membrane oxygenation (ECMO) [thesis]. Rotterdam: Erasmus University; 2005.
Vandenberghe H, Mac LS, Chinyanga H, Endrenyi L, Soldin S. Pharmacokinetics of intravenous morphine in balanced anesthesia: studies in children. Drug Metab Rev. 1983;14:887–903.
Dahlstrom B, Bolme P, Feychting H, Noack G, Paalzow L. Morphine kinetics in children. Clin Pharmacol Ther. 1979;26:354–65.
Olkkola KT, Maunuksela EL, Korpela R, Rosenberg PH. Kinetics and dynamics of postoperative intravenous morphine in children. Clin Pharmacol Ther. 1988;44:128–36.
Acknowledgments
This study was performed within the framework of Top Institute Pharma project number D2-104. The work of C.A.J. Knibbe is supported by the Innovational Research Incentives Scheme (Veni Grant, July 2006) of the Dutch Organization for Scientific Research NWO.
Conflict of interest
All authors declare no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krekels, E.H.J., Tibboel, D., Danhof, M. et al. Prediction of Morphine Clearance in the Paediatric Population. Clin Pharmacokinet 51, 695–709 (2012). https://doi.org/10.1007/s40262-012-0006-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-012-0006-9