Abstract
Background and Objective
Clinical guidelines recommend monotherapy with antidepressants for the treatment of major depression. This study examined prescription patterns with regard to both duration and type of treatment used among patients with newly diagnosed non-psychotic major depression based on a claims database from health insurance societies between 2008 and 2011 in Japan.
Methods
A retrospective cohort (N = 600,000) followed up for 4 years was used to identify patients (age ≥18 years) with newly diagnosed non-psychotic major depression. The prescription patterns and polypharmacy were examined. Four different types of pharmaceutical drugs were defined as possible psychotropic agents for major depression: (1) first- and/or second-generation antidepressants; (2) benzodiazepines; (3) sulpiride; and (4) antipsychotics. The data were analyzed by an intent-to-treat approach at months 0, 1, 3, 6, and 12 from the date of diagnosis.
Results
A total of 7,338 patients (3,684 males and 3,654 females, mean age 36.8 ± 10.9 years) with newly diagnosed non-psychotic major depression were identified. The median duration of treatment was 122 days. The proportion of patients in the cohort prescribed at least one type of defined psychotropic agents was 75.6 % (month 0), 47.3 % (month 1), 36.0 % (month 3), 26.8 % (month 6), and 17.4 % (month 12). The proportion of patients in the cohort prescribed at least one first- and/or second-generation antidepressant was 50.2 % (month 0), 34.9 % (month 1), 27.5 % (month 3), 20.3 % (month 6), and 12.5 % (month 12). The proportion of patients receiving at least one benzodiazepine was 58.0 % (month 0), 36.7 % (month 1), 27.1 % (month 3), 20.0 % (month 6), and 12.0 % (month 12). The proportion of patients receiving an antidepressant as monotherapy was only 12.0 % (month 0), 7.8 % (month 1), 6.5 % (month 3), 4.8 % (month 6), and 2.9 % (month 12), whereas the proportion of patients treated with a benzodiazepine alone was 13.5 % (month 0), 6.9 % (month 1), 4.6 % (month 3), 3.5 % (month 6), and 2.7 % (month 12). Various combinations of polypharmacy were observed. The most common was a combination of at least one antidepressant and benzodiazepine, which was prescribed to 36.7 % (month 0), 25.8 % (month 1), 19.9 % (month 3), 14.9 % (month 6), and 9.2 % (month 12) of the cohort.
Conclusions
Based on analysis of prescription patterns and type of treatment used for treating non-psychotic major depression, a majority of patients were not treated according to the recommended guidelines in Japan. Various patterns of prescription and use of polypharmacy were observed over time. The median duration of treatment was shorter than the recommendation (6 months) in the guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background and Objective
In the past decade, the treatment of major depression in Japan has undergone changes due to the increased number of patients with major depression and the introduction of new-generation antidepressants, such as selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, and noradrenergic and specific serotonergic antidepressants. The estimated number of patients treated for major depression was reported to be 430,000 in 1996, which more than doubled to 1,041,000 in 2008 in Japan [1]. In 1999, fluvoxamine was the first second-generation antidepressant to be introduced into Japan. Since then, paroxetine (2000), milnacipran (2000), sertraline (2006), mirtazapine (2009), duloxetine (2010), and escitalopram (2011) have been introduced into the Japanese market. The annual sales of antidepressants have been steadily expanding, reaching 120 billion yen (1.5 billion US dollars) in 2009 from 15 billion yen (190 million US dollars) in 1999. Nearly 89 % of these revenues were due to second-generation antidepressants [2].
The clinical guidelines recommend monotherapy with a second-generation antidepressant for acute-phase treatment of major depression [3–6]. The Japanese Society of Mood Disorders (JSMD) released the Treatment Guideline II: Major Depressive Disorder, 2012 Ver. 1 in 2012 [7]. According to the guidelines, polypharmacy of antidepressants is not recommended, benzodiazepines should not be administered irresponsibly for a long term, and attention should be paid to problems with dependence, cognitive dysfunction, obstructive sleep apnea, and paradoxical reactions [7]. Furthermore, monotherapy with either benzodiazepines, sulpiride, or antipsychotics is not recommended for treating major depression [7].
In clinical practice, however, these recommended guidelines do not appear to be respected in Japan. Sawada et al. [8] reported a higher rate of concomitant use of anxiolytic benzodiazepines for patients with major depression despite the similar continuation rate on monotherapy with a second-generation antidepressant after 4 weeks. Several studies reported frequent prescriptions for sulpiride as an antidepressant in Japan [9]. This was because sulpiride was approved in Japan with an indication for depression (150–300 mg/day) [10]. Ueshima et al. [11] conducted an internet survey of psychiatrists in Japan and only 26 % of the responders treated patients with major depression with monotherapy.
In previous studies, the type of drug investigated was focused on only first- and/or second- generation antidepressants [12] or on the limited number of combinations for multiple drugs [8]. In addition, previous studies were conducted at a limited number of medical institutions and only included new patients or patients already undergoing treatment [8, 9, 12].
Despite recent changes in treatment, such as newly introduced antidepressants, there is only limited information on the treatment of patients with major depression in Japan with respect to treatment patterns, such as duration and types of treatment. Furthermore, a comprehensive treatment evaluation of patients with major depression based on a large database has yet to be conducted.
The objective of this study was therefore to examine prescription patterns with regard to duration and type of treatment by patients diagnosed with major depression based on the claims database of health insurance societies between 2008 and 2011 in Japan. To eliminate prevalent-user bias, which may cause different medication-taking behaviors from new psychotropic users [13], only patients newly diagnosed with major depression were analyzed in this study.
2 Methods
2.1 Study Design
This was a retrospective and observational cohort study using the claims database to identify a cohort of patients newly diagnosed with major depression. Characteristics of prescription patterns with regard to both duration and type of treatment used for major depression based on four types of defined psychotropic drugs were examined at selected time points from the index date (the first date of diagnosis) and all patients were followed for 1 year by an intention-to-treat (ITT) approach.
2.2 Data Source
The claims data from the Japan Medical Data Center (JMDC) Ltd. (Tokyo, Japan) were used for the analyses [14]. The JMDC data consist of monthly claims information submitted to health insurance societies from medical institutions for both corporate employees and their dependents [15]. The claims data include information on disease, medical procedures and materials, prescriptions (at either a pharmacy or hospital), and in- or out-patient status [15]. Since hospital prescriptions were claimed on a monthly basis without specific information on the actual date, these claims were analyzed as if they occurred on the 15th day of each month. The diseases database includes ICD-10 (International Classification of Disease, 10th Revision) diagnosis codes [16] and the diseases and injuries codes defined by the Medical Information System Development Center (MEDIS-DC), which are the standardized names of diseases and injuries for reimbursement by the National Health Insurance [17]. The claims database from January 2008 to December 2011, which includes 600,000 beneficiaries (employees and their dependents), was analyzed to identify patients with newly diagnosed non-psychotic major depression. A confidential enrollee identifier to track and link records across data files was used to ensure confidentiality. The study was approved by the Kyoto University Graduate School and Faculty of Medicine Ethics Committee (Kyoto, Japan).
2.3 Study Cohort Selection
A flowchart with the detailed process of patient selection for the analysis population is shown in Fig. 1. The first date of diagnosis was defined as the index date. One year before the index date was defined as the pre-index period. Patients who were newly diagnosed with major depression without psychotic disorder were selected for the analysis population. At first, patients who were diagnosed with at least one disease term related to unipolar depression were extracted. To identify unipolar depression, the criteria were defined by the combination of both the ICD-10 diagnosis code and the name of diseases and injuries codes defined by MEDIS-DC (Electronic Supplementary Material, Appendix 1). Secondly, patients who were diagnosed with bipolar affective disorder (F319) or organic mental disorder, including symptomatic mental disorder (F0) or schizophrenia, schizotypal, and delusional disorders (F2) up to 30 days after the index date were excluded. Thirdly, patients prescribed antidepressants, antipsychotics, or mood stabilizers up to 15 days before the index date were excluded. Lastly, patients who lost their insurance eligibility within less than 12 months after the index date were excluded. Patients 18 years and over on the day of diagnosis between 1 January 2009 and 31 December 2010 were defined as the analysis population. Patients meeting all of the inclusion and exclusion criteria were followed up for 12 months after their index dates to examine the prescription patterns and type of treatment used, including antidepressant polypharmacy.
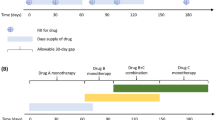
2.4 Duration of Treatment
The duration of treatment was analyzed among patients who were prescribed at least one defined psychotropic drug. It was calculated for any defined psychotropic drug as the number of days between the date of first prescription and the date of last prescription plus dispensing day during a 12-month follow-up period. Gaps longer than 90 days were considered to constitute a new episode and were not included for the treatment duration in this study.
2.5 Drug Utilization Patterns
Psychotropic drugs used for treating major depression were defined and categorized into four types: (1) first- and/or second-generation antidepressants; (2) benzodiazepine; (3) sulpiride; and 4) antipsychotics (Electronic Supplementary Material, Appendix 2). Prescription patterns were examined at months 0, 1, 3, 6, and 12 after the index date. At least one prescription of the defined psychotropic drugs used for treating major depression was examined for each analysis month. Polypharmacy for major depression was evaluated based on each combination of the four types of defined drugs used for treating major depression, while polypharmacy within the same class was not counted (e.g. two or more benzodiazepines prescribed on the same day). The proportion of the patients prescribed first- and/or second-generation antidepressants was examined as a separate analysis.
2.6 Statistical Analysis
Descriptive statistics were used summarizing the demographics of the cohort, prescription patterns, and polypharmacy. Analysis was conducted using SAS version 9.2 (SAS institute Inc., Cary, NC, USA).
In this study, the time window for analyzing prescription patterns was 30 days, which was ±15 days from the analysis point (months 0, 1, 3, 6, and 12). The shorter time window was set at 14 days (i.e., ±7 days from the analysis point) for prescriptions to evaluate the robustness of the main analysis.
3 Results
The patient characteristics of the analysis population are described in Table 1. A total of 7,338 patients were identified. The mean age of the population was 36.8 years (standard deviation: 10.9) and 50.2 % were male. Of the analysis population, 48.8 % were aged between 18 and 34 years, and 38.3 % were between 35 and 49 years. Insurance status as enrollees was 75.1 %. Hospitalization during the pre-index period was 5.7 % and hospitalization at index date was 1.9 %. The majority of the diagnoses for unipolar major depression by ICD-10 was depressive episode, unspecified (F329) [n = 7,182], dysthymia (F341) [n = 839], mixed anxiety and depressive disorder (F412) [n = 163], mild depressive episode (F320) [n = 83], and other depressive disorders (F328) [n = 50].
The median duration of treatment by prescriptions was 122 days. Of the total analysis population, 827 (11.3 %) were not prescribed any of the defined psychotropic drugs used for the treatment of major depression during the analysis period. 1,426 (19.4 %) patients were prescribed at least one defined psychotropic drug for less than 90 days, whereas 2,247 (30.6 %) patients were prescribed at least one defined psychotropic drug for a year or more.
At least one defined psychotropic drug was prescribed to 5,546 patients (75.6 %) of the identified cohort at month 0, 3,470 (47.3 %) at month 1, 2,644 (36.0 %) at month 3, 1,965 (26.8 %) at month 6, and 1,279 (17.4 %) at month 12.
At least one first- and/or second-generation antidepressant was prescribed to 3,684 (50.2 %) patients at month 0, 2,563 (34.9 %) at month 1, 2,021 (27.5 %) at month 3, 1,489 (20.3 %) at month 6, and 918 (12.5 %) at month 12. At least one second-generation antidepressant was prescribed to 3,094 (42.2 %) patients at month 0, 2,237 (30.5 %) at month 1, 1,749 (23.8 %) at month 3, 1,315 (17.9 %) at month 6, and 807 (11.0 %) at month 12. The number of patients who were prescribed a combination of at least one first- and/or second-generation antidepressant was 346 (4.7 %) at month 0, 317 (4.3 %) at month 1, 290 (4.0 %) at month 3, 235 (3.2 %) at month 6, and 164 (2.2 %) at month 12. The prescription patterns of first- and/or second-generation antidepressants by the analysis month are shown in Fig. 2.
At least one benzodiazepine was prescribed to 4,254 (58.0 %) patients at month 0, 2,692 (36.7 %) at month 1, 1,989 (27.1 %) at month 3, 1,469 (20.0 %) at month 6, and 939 (12.0 %) at month 12. Benzodiazepine as monotherapy was prescribed to 988 (13.5 %) patients at month 0, 508 (6.9 %) at month 1, 340 (4.6 %) at month 3, 258 (3.5 %) at month 6, and 198 (2.7 %) at month 12. Prescription patterns and polypharmacy of defined psychotropic drugs by month are shown in Fig. 3. The detailed breakdown figures are described in Table 2.
Prescription patterns and polypharmacy of defined psychotropic drugs by month (n = 7,338). “Other at least defined AD prescription” includes AD + AP; AD + sulpiride + AP; AD + BZD + AP; AD + BZD + sulpiride + AP; BZD + AP; BZD + AP + sulpiride; AP; sulpiride + AP. AD antidepressant, AP antipsychotic, BZD benzodiazepine
Various combinations of polypharmacy were observed. The most common polypharmacy was a combination of first- and/or second-generation antidepressants and benzodiazepines. The first- and/or second-generation antidepressants and benzodiazepines were prescribed to 2,077 (28.3 %) patients at month 0, 1,433 (19.5 %) at month 1, 1,080 (14.7 %) at month 3, 794 (10.8 %) at month 6, and 484 (6.6 %) at month 12. The first- and/or second-generation antidepressants and benzodiazepines, with or without other defined psychotropic drugs, were prescribed to 2,691 (36.7 %) patients at month 0, 1,894 (25.8 %) at month 1, 1,463 (19.9 %) at month 3, 1,094 (14.9 %) at month 6, and 676 (9.2 %) at month 12.
Among patients who were prescribed at least one defined psychotropic drug, more than 70 % (76.7 % at month 0, 77.6 % at month 1, 75.2 % at month 3, 74.8 % at month 6, and 73.4 % at month 12) were prescribed benzodiazepines through the analysis period. A benzodiazepine alone was prescribed to 13.5 % of the cohort at month 0. Among those who were prescribed at least one defined psychotropic drug, the prescription rate of a benzodiazepine alone stayed between 13 and 18 % throughout the year of analysis.
The number of antidepressant prescriptions for each analysis month was evaluated using a shorter analysis window (14 days and 7 days before and after the analysis point). The results did not vary by more than 5 % between 30 days and 14 days of the analysis windows on the prescriptions at either the pharmacy or the hospital, which accounted for 71.2 % of all prescriptions. Therefore, the same conclusions were reached (data not shown).
4 Discussion
In our study, the prescription patterns and polypharmacy were examined among newly diagnosed patients with major depression based on the claims database using an ITT approach. This was the first study using the large claims database in Japan to investigate the use of psychotropic drugs among patients who were newly diagnosed with major depression in the real-world setting.
The median duration of treatment was 122 days. Almost half of the patients received at least one defined psychotropic drug of interest for 4 months or less, which is below the 6-month treatment time recommended in the clinical guidelines [18]. A sex-related disparity in median treatment duration was observed (female: 98 days and male: 142 days). Further investigation is needed to explain this difference.
Almost half of patients, who were prescribed at least one defined psychotropic drug received it for less than 6 months. These findings are similar to previously reported data [19–21]. In addition, 11.3 % of the cohort was not prescribed any defined psychotropic drug for 1 year from the index date. Despite the guideline recommendation for a minimal treatment duration of 9–12 months, our findings indicated that patients newly diagnosed with major depression did not receive the treatment for the recommended duration for major depression.
Only one of eight patients in this study was solely prescribed first- and/or second-generation antidepressants at the time of diagnosis. At least one first- and/or second-generation antidepressant was prescribed to nearly half of the cohort at month 0. Inagaki investigated the prescription patterns among patients who were prescribed at least one antidepressant at three psychiatric hospitals (n = 1,456) [12]. The data demonstrated that 67.9 % of the patients were prescribed at least one second-generation antidepressant. In our study, among patients who were prescribed at least one first- or second-generation antidepressant, more than 85 % were prescribed a second-generation antidepressant through the analysis period. This may suggest that newly diagnosed patients with major depression are more likely to be prescribed a second-generation antidepressant. It should be noted that Inagaki’s cohort included patients with ongoing treatment [12]. In our study, among those who were prescribed at least one antidepressant, the proportion of patients who were prescribed both first- and second-generation antidepressants increased from 9.3 % at month 0 to 15.2 % at month 6. An increase in combination therapy with first- and second-generation antidepressants may reflect some of the proposed treatment strategies for treatment-refractory depression.
Of those who were prescribed at least one antidepressant, approximately three-quarters were prescribed at least one psychotropic drug from another defined drug class. The most common one was first- and/or second-generation antidepressants, and a benzodiazepine was prescribed for approximately half of the patients among those prescribed at least one defined psychotropic drug. Meta-analysis of antidepressants plus benzodiazepines for major depression showed a limited treatment effect of benzodiazepines for major depression after 6–12 weeks [19]. In addition, benzodiazepine treatment is at risk of problems with abuse, dependence, and withdrawal symptoms upon discontinuation, particularly with long-term use [4]. Despite the limited treatment effect and the guidelines in Japan, our findings suggested a wide gap between the guidelines and the actual treatment. Pfeiffer et al. [20] investigated the adequacy of antidepressant treatment with benzodiazepines using a clinical database from the Veteran Health Administration in the USA. These investigators reported that 7.6 % of patients diagnosed with depression were prescribed benzodiazepines commencing on the same date as their initial antidepressant treatment [20]. In comparison with the study by Pfeiffer et al., our study suggests that the majority of patients with major depression were prescribed benzodiazepines in Japan. Considering the risk and benefit of benzodiazepines, they seem to be over-prescribed for the treatment of major depression in Japan.
Lai et al. [21] reported that less than 2 % of patients receiving treatment for major depression were prescribed benzodiazepines for more than 30 days in Taiwan. Our study suggested that a substantial minority of patients were prescribed benzodiazepines alone for treating major depression. Since long-term use of benzodiazepines could aggravate the symptoms of depression [22] and lead to a psychological dependence and discontinuation syndrome [23, 24], the stand-alone prescription of benzodiazepines should be avoided.
Maeda et al. [25] reported that 33 % of patients who were newly diagnosed with unipolar depression in a psychiatric unit at a university hospital were prescribed sulpiride. In our study, among patients who were prescribed at least one defined psychotropic drug, approximately one-quarter of the patients were prescribed sulpiride. In addition, monotherapy of sulpiride was observed in a small percentage of patients over the analysis period. This result indicates that sulpiride is still commonly prescribed for the treatment of major depression despite that fact that it is not recommended for treating major depression in the JSMD guidelines [7].
Antipsychotics were increasingly prescribed among patients who were prescribed at least one defined psychotropic drug over the analysis period. This suggests that the treatment pattern was in line with guideline recommendations of adding antipsychotics in the case of non-response [4, 5].
Anxiety disorder is frequently diagnosed with major depression [26, 27]. It may cause poorer mental health outcomes [28], including a longer time to recover than patients with major depression without anxiety disorders [29]. Wu et al. reported that patients with major depression with a co-morbid anxiety were more likely to use antidepressants than those not having a co-morbid anxiety [30]. In addition, sleep disturbance may affect the treatment outcome among patients with major depression. Further study is needed to examine co-morbidities such as anxiety and sleep disturbance [31].
This is the first study comprehensively examining prescription patterns and the use of more than one drug for major depression for four types of psychotropic agents in a cohort from a clinical database. Additional studies are needed to confirm our findings.
The limitations of the study are as follows. The JMDC database is based on data from health insurance companies from a number of corporations with 600,000 beneficiaries (employees and their dependents). Therefore, their socioeconomic and demographic status may not represent the overall Japanese population. The JMDC database did not include a significant number of patients over 65 years of age. The average age of our cohort was 36.6 years old, and our results therefore apply generally to younger populations. Secondly, newly diagnosed patients with major depression were identified based on the first date of diagnosis as an index date in the claims database. Since the first date of diagnosis is set by each medical institution, patients with recurrent episodes could have been included in our study. In our study, however, patients who were prescribed an antidepressant before the index date were excluded from the analysis population. Therefore, we think that the chance of including patients with a previous or recurrent episode was minimized. Furthermore, the index date was set at the first date of diagnosis and the results did not follow the duration of the treatment on an individual basis. Thirdly, due to the nature of the claims database, the disease code might not reflect the patient’s actual diagnosis. Lastly, again due to the nature of the claims database, the prescription data do not indicate whether the medications were consumed.
5 Conclusion
This is the first study comprehensively examining prescription patterns and polypharmacy for four types of pharmaceutical agents in a cohort of patients newly diagnosed with major depression. The study showed that the majority of prescription patterns and trends for treating major depression in a Japanese claims database did not follow guideline recommendations. Various patterns of prescriptions and polypharmacy were observed over time. The median duration of treatment was shorter than that recommended in the guidelines. Further studies using different types of clinical databases and a prospective design are required to determine the validity of these findings.
References
Ministry of Health, Labor and Welfare, Tokyo, Japan. Patient survey 2008. Tokyo: Ministry of Health, Labor and Welfare; 2008.
Furukawa TA, Akechi T, Shimodera S, et al. Strategic use of new generation antidepressants for depression: SUN(^_^)D study protocol. Trials. 2011;11(12):116.
Motohashi N, editor. Pharmacotherapy algorithms for mood disorders. Tokyo: Jihou; 2003.
National Collaborating Centre for Mental Health (UK). Depression: the treatment and management of depression in adults (updated edition). Leicester: British Psychological Society; 2010. NICE Clinical Guidelines, no. 90.
Lam RW, Kennedy SH, Grigoriadis S, The Canadian Network for Mood and Anxiety Treatments (CANMAT), et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord. 2009;117(Suppl 1):S26–43.
Texas Department of State Health Services. Texas medication algorithm project procedural manual: major depressive disorder algorithms, USA. 2008 http://www.pbhcare.org/pubdocs/upload/documents/TMAP%20Depression%202010.pdf. Accessed 12 Jan 2013.
Treatment guideline II: major depressive disorder, 2012, ver. 1. Tokyo: The Japanese Society of Mood Disorders (JSMD); 2012.
Sawada N, Uchida H, Suzuki T, et al. Persistence and compliance to antidepressant treatment in patients with depression: a chart review. BMC Psychiatry. 2009;16(9):38.
Uchida N, Chong MY, Tan CH, et al. International study on antidepressant prescription pattern at 20 teaching hospitals and major psychiatric institutions in East Asia: analysis of 1,898 cases from China, Japan, Korea, Singapore and Taiwan. Psychiatry Clin Neurosci. 2007;61(5):522–8.
National Health Insurance (NHI) price dictionary, 2012 April version. Tokyo: Jiho; 2012.
Ueshima K, Higuchi T, Kanba S, et al. Views on drug therapy for depression: proposals based on the field survey [in Japanese]. Jpn Med J. 2005;4262:18–62.
Inagaki A. Prescription patterns of antidepressant. Health and labour sciences research 2002 [in Japanese]. http://www.ncnp.go.jp/tmc/pdf/22_report03.pdf. Accessed 20 Jan 2013.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Japan Medical Data Center Co. Ltd. Tokyo, Japan [in Japanese]. http://www.jmdc.co.jp/en/srv_pharma/jdm.html. Accessed 21 Jan 2013.
Kimura S, Sato T, Ikeda S, et al. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20(5):413–9.
International Classification of Disease, 10th revision (ICD-10) diagnosis codes, vol. 2. Geneva: World Health Organization; 2004.
Master of diseases and injuries names version 3 [in Japanese]. Tokyo: Medical Information System Development Center (MEDIS-DC); 2011.
Davidson JR. Major depressive disorder treatment guidelines in America and Europe. J Clin Psychiatry. 2010;71(Suppl E1):e04.
Furukawa TA, Streiner DL, Young LT. Antidepressant and benzodiazepine for major depression. Cochrane Database Syst Rev. 2002;(1):CD001026.
Pfeiffer P, Ganoczy D, Zivin K, et al. Benzodiazepines and adequacy of initial antidepressant treatment for depression. Clin Psychopharmacol. 2011;31(3):360–4.
Lai IC, Wang MT, Wu BJ, et al. The use of benzodiazepine monotherapy for major depression before and after implementation of guidelines for benzodiazepine use. J Clin Pharm Ther. 2011;36(5):577–84.
Lader MH, Petursson H. Benzodiazepine derivatives—side effects and dangers. Biol Psychiatry. 1981;16:1195–201.
Pecknold JC. Discontinuation reaction to alprazolam in panic disorder. J.Psychiatr. Res. 1993;27(Suppl. 1):155–70.
Richels K, Case WG, Dowing RW, et al. Long-term diazepam therapy and clinical outcome. JAMA. 1983;250:767–71.
Maeda H, Egami H, Tomita M, et al. How does sulpiride work and how is it utilized? Jpn J Clin Psychopharmacol. 2007;10(10):1853–60.
Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on alcoholism and related conditions. Arch Gen Psychiatry. 2005;62(10):1097–106.
Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–105.
Felker BL, Hedrick SC, Chaney EF, et al. Identifying depressed patients with a high risk of comorbid anxiety in primary care. Prim Care Companion J Clin Psychiatry. 2003;5(3):104–10.
Clayton PJ, Grove WM, Coryell W, et al. Follow-up and family study of anxious depression. Am J Psychiatry. 1991;148(11):1512–7.
Wu CH, Erickson SR, Piette JD, et al. The association of race, comorbid anxiety, and antidepressant adherence among Medicaid enrollees with major depressive disorder. Res Social Adm Pharm. 2012;8(3):193–205.
Morehouse R, Macqueen G, Kennedy SH. Barriers to achieving treatment goals: a focus on sleep disturbance and sexual dysfunction. J Affect Disord. 2011;132(Suppl 1):S14–20.
Acknowledgment
No sources of funding were used to assist in the conduct of this study or the preparation of the manuscript. TAF has received honoraria for speaking at CME meetings sponsored by Asahi Kasei, Eli Lilly, GlaxoSmithKline, Mochida, MSD, Otsuka, Pfizer Shionogi, and Tanabe-Mitsubishi. He is a diplomate of the Academy of Cognitive Therapy. He has received royalties from Igaku-Shoin, Seiwa-Shoten, and Nihon Bunka Kagaku-sha. He is on the advisory board for Sekisui Chemicals and Takeda Science Foundation. The Japanese Ministry of Education, Science, and Technology, the Japanese Ministry of Health, Labor and Welfare, and the Japan Foundation for Neuroscience and Mental Health have funded his research projects. SH has received honoraria for a luncheon meeting as a speaker at the Annual Meeting of Japanese Cancer Association by Sanofi K.K. He has received honoraria for speaking at the J-CaPURE joint meeting supported by Takeda Pharmaceutical Co. Ltd. He has received honoraria for an evening seminar at Annual Meeting of the Japanese Society of Urolithiasis Research sponsored by Astra Zeneca K.K. He has received honoraria for an educational lecture at the Japanese Society of BCG Instillation Therapy sponsored by Japan BCG Laboratory. The Japanese Ministry of Education, Science, and Technology, and the Japanese Ministry of Health, Labor and Welfare have funded his research projects. KK has received a grant from Dainippon Sumitomo Pharma Co., Ltd, Kyowa Hakko Kirin Co., Ltd, Olympus Corporation, and Taiho Pharmaceuticals Co., Ltd. He has received honoraria from Daiichi Sankyo Company, Ltd, Behringer Ingelheim Japan, Inc., Senju Pharmaceuticals Co., Ltd, Toray industries Inc., Maruho Co., Ltd, Canon Inc., Olympus Corporation, Kyowa Hakko Kirin Co., Ltd, Kaken Pharmaceutical Co., Ltd, Novartis K.K., Otsuka Pharmaceuticals Co., Ltd, and Eisai Co., Ltd. He has received honoraria for lectures from the Japan Medical Data Center Co., Ltd. YO is an employee at Sanofi.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Onishi, Y., Hinotsu, S., Furukawa, T.A. et al. Psychotropic Prescription Patterns Among Patients Diagnosed With Depressive Disorder Based on Claims Database in Japan. Clin Drug Investig 33, 597–605 (2013). https://doi.org/10.1007/s40261-013-0104-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0104-y