Abstract
Background and Objective
Ustekinumab, a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody against interleukin-12/23p40, has been reported to be significantly efficacious in treating patients with moderate-to-severe plaque psoriasis. Although the efficacy and safety of ustekinumab have been previously studied in Asian patients with psoriasis, the pharmacokinetics of ustekinumab has not been reported for Asian patients. The objective of this analysis was to compare the pharmacokinetics of ustekinumab in Chinese and non-Chinese subjects.
Subjects and Methods
Two Phase 1, open-label, single-period, inpatient/outpatient studies were conducted to evaluate the pharmacokinetics of ustekinumab following a single subcutaneous (SC) injection. In Study 1, non-Chinese healthy male subjects (n = 31) received a single SC injection of ustekinumab 90 mg. In Study 2, Chinese healthy male subjects (n = 24) were randomized (1:1) to receive a single SC injection of ustekinumab 45 mg or 90 mg. Serum ustekinumab concentrations were measured using validated immunoassays. The pharmacokinetic parameters were calculated using non-compartmental analyses. After data collection, a linear mixed model approach was used to compare the log-transformed maximum observed serum concentration (Cmax) and area under the serum concentration–time curves (AUCs) generated from the 90-mg dose groups in the two studies. The ratios of the geometric means of the Cmax and AUCs in Chinese subjects (Test) to those in non-Chinese subjects (Reference) along with the 90 % confidence intervals (CIs) were calculated.
Results
The mean body weight was 80.3 kg in non-Chinese (Caucasian: 77.4 %; black: 12.9 %; Asian: 0.0 %; other: 9.7 %) and 65.7 kg in Chinese subjects, with an overall mean of 74 kg. Across studies and dose groups, the median time corresponding to the Cmax (tmax) was 4.0–8.5 days, the mean terminal half-life (t½) was approximately 3 weeks, and the mean apparent volume of distribution based on the terminal phase (Vz/F) was 80.3–97.3 mL/kg. In the 90-mg groups, mean exposure parameters of ustekinumab were 1.1- to 1.3-fold higher in Chinese versus non-Chinese subjects. However, exposure parameters were not significantly different between the two study populations when individual parameters were adjusted to a subject weighing 74 kg: the 90 % CIs of the geometric mean ratios (Chinese versus non-Chinese) for weight-adjusted Cmax, AUC from time zero to time of last measurable concentration (AUClast), and AUC from time zero to infinity (AUC∞) were (0.76–1.09), (0.85–1.16) and (0.88–1.22), respectively. Ustekinumab was generally well tolerated, with no unexpected adverse events; one subject (non-Chinese) developed anti-drug antibodies to ustekinumab.
Conclusion
The pharmacokinetics of ustekinumab were comparable between Chinese and non-Chinese healthy male subjects when exposure parameters were adjusted by subject body weight.
Clinical Trial Registration
Study 1, conducted with non-Chinese subjects (March–July 2006), was completed before the 7th revision of the Declaration of Helsinki and was therefore exempt from registration under the existing guidelines. The clinical trial registration number for Study 2, conducted with Chinese subjects (October 2009–June 2010), is NCT01081704.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Interleukin (IL)-12 and IL-23 are key cytokines in the pathogenesis of psoriasis [1, 2]. Treatment with ustekinumab, a human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody (mAb) that binds to the p40 subunit common to IL-12 and -23, has demonstrated significant efficacy in treating patients with moderate-to-severe plaque psoriasis [3–7]. Currently, ustekinumab has been approved in the USA, the EU, Japan and many other countries for the treatment of adult patients (18 years or older) with moderate-to-severe plaque psoriasis who are candidates for phototherapy or systemic therapy.
The pharmacokinetic properties of ustekinumab have been characterized in population pharmacokinetic analyses using data from global Phase 2–3 trials in patients with psoriasis [8] or psoriatic arthritis (PsA) [9]. Systemic exposure to ustekinumab was reported to be associated with efficacy in patients with psoriasis [10, 11]. Although the efficacy and safety of ustekinumab have been studied in Asian patients with psoriasis [12, 13], the pharmacokinetics of ustekinumab has not been reported for Asian subjects. A bridging pharmacokinetic study in Chinese subjects was required by the State Food and Drug Administration (SFDA) of China for a local new drug application. The objective of the current analysis was to assess the pharmacokinetics of ustekinumab in a Phase 1 study in healthy Chinese male subjects and to compare these findings with those obtained from a previous Phase 1 study in healthy non-Chinese male subjects. In addition, tolerability was monitored and immunogenicity was assessed in these two studies.
2 Subjects and Methods
2.1 Study Designs
2.1.1 Study 1 (Non-Chinese)
This was a Phase 1, single-centre, open-label, single-dose, inpatient/outpatient study conducted at PRACS Institute, Ltd. (Fargo, ND, USA) from March 2006 to July 2006. In this study, healthy adult male subjects (non-Chinese; mostly Caucasian and black) received a single subcutaneous (SC) injection of ustekinumab 90 mg. Approximately 30 subjects were planned to be enrolled into the study such that at least 24 subjects were to complete the study. The total duration of subject participation was up to 16 weeks, including a screening visit up to 30 days prior to injection, an inpatient period in the study unit from 1 day before to 14 days after injection, and an outpatient period during which subjects returned to the study unit for scheduled visits from 17 days through 84 days (12 weeks) after injection. The study protocol and amendments were reviewed and approved by the Institutional Review Board, Inc., PRACS Institute, Ltd.
2.1.2 Study 2 (Chinese)
This was a Phase 1, single-centre, randomized, parallel, open-label, single-dose, inpatient/outpatient study conducted at Peking University First Hospital (PUFH) [Beijing, China] from October 2009 to June 2010. In this study, healthy Chinese male subjects were randomly assigned in a 1:1 ratio to receive a single SC injection of ustekinumab 45 mg or 90 mg. At least 12 subjects per group were planned to be enrolled into the study such that at least eight subjects per group were to complete the study. The total duration of subject participation was up to 16 weeks, including a screening visit up to 30 days prior to injection, an inpatient period consisting of 5 consecutive nights/6 days in the study unit from 1 day before to 4 days after injection, and an outpatient period during which subjects returned to the study unit for scheduled visits from 5 days through 84 days (12 weeks) after injection. The study protocol and amendments were reviewed and approved by the Ethics Committee of PUFH.
Treatment compliance was monitored by the study site personnel. Site personnel administered the study agent and recorded injection date and time on the case report form (CRF). All CRFs were to be overseen by the site monitors designated by the sponsor: PRA International (Raleigh, NC, USA) for Study 1 and Quintiles (Shanghai, China) for Study 2. During these visits, all procedures were evaluated for compliance with the protocol. Both studies were conducted in accordance with applicable laws and regulations, the current International Conference on Harmonisation guidelines for Good Clinical Practices (http://www.ich.org), and the principles of the Declaration of Helsinki [14].
2.2 Subjects
In both studies, healthy male subjects aged 18–45 years with a body weight of 60–90 kg were eligible. In Study 1, only subjects who lived in the USA were enrolled. In Study 2, however, only subjects who lived in China and had Chinese ancestry were enrolled.
During the screening period, subjects must not have had any clinically relevant abnormalities, which were determined by medical history, physical examination, blood chemistry, complete blood count (CBC), urinalysis, vital signs, chest radiograph and electrocardiogram (ECG). Subjects must have had no history of latent or active tuberculosis (TB) prior to screening; had no signs or symptoms suggestive of active TB upon review of the medical history and/or physical examination; had no recent close contact with a person with active TB; had a negative tuberculin skin test result (Study 1) or had both a negative tuberculin skin test and a negative QuantiFERON®-TB Gold test (Study 2) within 30 days prior to injection; and had a chest radiograph (both posterior–anterior and lateral views) taken within 3 months prior to injection with no evidence of current active TB or old inactive TB. Subjects with any malignancy, history of malignancies, history of latent or active granulomatous infections, recent non-tuberculous mycobacterial infections, or opportunistic infections were not eligible. All subjects were informed about the nature and purpose of the study, participation/termination conditions, and risks and benefits of treatment. Subjects provided written informed consent before any protocol-specific procedures were undertaken.
Any prescription, over-the-counter, herbal or natural medications were prohibited during the 14 days prior to injection and through completion of the studies, with the exception of paracetamol (acetaminophen) or pre-existing multivitamins that could be used at recommended doses. Subjects could not receive any live virus or bacterial vaccinations within 30 days before screening or during the trials.
2.3 Dosage and Administration
Ustekinumab was supplied as a sterile solution in either a single-use 2-mL type-I glass vial (Study 1) or a single-use 1-mL prefilled syringe (Study 2). It was administered via SC injection into the abdominal area. Both the vial and prefilled-syringe products have been approved by the US Food and Drug Administration (FDA) and European Medicines Agency for human use at two dose strengths: 45 mg in 0.5 mL or 90 mg in 1 mL.
2.4 Sample Collections
In both studies, blood samples of ≥5 mL each were collected from the antecubital vein via direct venipuncture or indwelling catheter into a serum separator tube at 1 h before injection, 12 h after injection, and also at 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 17, 21, 28, 35, 42, 49, 56, 63, 70 and 84 days (12 weeks) after injection for measuring serum ustekinumab concentrations. Blood samples collected at 1 h before injection and 84 days after injection were also evaluated for the presence of anti-drug antibodies (ADAs) in serum. Subjects who terminated study participation early had their last blood samples collected at the termination visits. The tubes were gently inverted 5–6 times to afford mixing with the polymer gel and silica clot activator before processing. The blood samples were allowed to clot at room temperature for approximately 30 min and centrifuged at room temperature (minimum 1,500×g) for 15–20 min. All separated sera were transferred immediately with a clean, disposable glass or polyethylene pipette into pre-labeled storage tubes (1.8-mL NUNC™ Cryovial™ with skirted bottom) with approximately 1 mL of serum in each tube. Serum samples were stored in an upright position at approximately −20 °C or below in non-automatically defrosting freezers. Samples were kept frozen during shipping to the study sponsor’s clinical pharmacology laboratory (Radnor, PA, USA) for bioanalyses.
2.5 Bioanalytical Methods
In Study 1, serum ustekinumab concentrations were quantified using a validated enzyme-linked immunosorbent assay (ELISA). The lowest quantifiable concentration in a sample for this ELISA was 0.0844 μg/mL [lower limit of quantification (LLOQ) of 0.00844 μg/mL multiplied by the minimum required 1:10 dilution]. Inclusive of all calibration standards, the mean inter-assay accuracy (% relative error) was 91.1–101.8 % and the mean inter-assay precision (% coefficient of variation) was 2.9–12.1 %. Inclusive of all three quality control (QC) samples, the mean intra-assay precision ranged from 4.7 to 7.1 %, the mean inter-assay accuracy ranged from 84.4 to 101.1 %, the mean inter-assay precision ranged from 3.7 to 11.3 %, and the total error (mean inter-assay accuracy plus mean inter-assay precision) ranged from 4.8 to 26.9 %. In Study 2, serum ustekinumab concentrations were measured using a validated electrochemiluminescent immunoassay (ECLIA). The lowest quantifiable concentration in a sample for this ECLIA was 0.1688 μg/mL (LLOQ of 0.01688 μg/mL multiplied by the minimum required 1:10 dilution). Inclusive of all calibration standards, the mean inter-assay accuracy ranged from 96.3 to 102.1 % and the mean inter-assay precision ranged from 2.3 to 5.3 %. Inclusive of all five QC samples, the mean intra-assay precision ranged from 2.6 to 9.5 %; the mean inter-assay accuracy ranged from 84.7 to 100.9 %; the mean inter-assay precision ranged from 6.7 to 8.9 %; and the total error ranged from 7.6 to 24.2 %. The ELISA and ECLIA assays were cross-validated to ensure the obtained data were reliable and could be compared.
In both studies, the presence of ADAs was determined using a validated bridging enzyme immunoassay [15] with a sensitivity of 24 ng/mL at a minimum required 1:10 dilution. The accuracy was 94.9 and 99.0 %, respectively, for the 2.4 and 312.5 ng/mL positive-control concentrations. The intra-assay precision was 5.3 % for the human-positive and 17.5 % for the human-negative serum pools. The inter-assay precision was 14.1 % for the human-positive and 18.4 % for the human-negative serum pools.
2.6 Pharmacokinetic Analyses
The pharmacokinetic parameters of ustekinumab were calculated using non-compartmental analyses [16] implemented in WinNonlin® Enterprise (Version 5.2.1, Pharsight Corporation, Mountain View, CA, USA). All calculations were based on actual sampling times. For estimation of pharmacokinetic parameters, serum ustekinumab concentrations below the lowest quantifiable concentration were assigned a value of zero if they preceded the first quantifiable sample in the profile. Any other values below the lowest quantifiable concentration were set to missing. If any individual concentration value was deemed to be anomalous, and a clear justification could be provided, the anomalous data point could be excluded from pharmacokinetic analyses. The derived pharmacokinetic parameters included the maximum observed serum concentration (Cmax); time to reach Cmax (tmax); area under the serum concentration versus time curve from time zero to time of last measurable concentration (AUClast); AUC from time zero to infinity (AUC∞); terminal half-life (t½); apparent clearance (CL/F); and apparent volume of distribution based on the terminal phase (Vz/F). The terminal rate constant associated with the terminal portion of the serum concentration versus time curve (λz) was determined by a least-squared regression analysis of the log-linear portion of the terminal phase (including at least three timepoints) with a coefficient of determination (R2) value of at least 0.90, a goodness of fit criterion.
The t½ was calculated as ln(2)/λz. The AUClast was calculated using a combination of linear and logarithmic trapezoidal methods: the linear trapezoidal rule was employed before the Cmax, and the logarithmic trapezoidal rule was used after the Cmax. The AUC∞ value was determined as AUClast + Clast/λz, where Clast represents the last measurable serum concentration of ustekinumab. In addition, in order to have an accurate estimation of the AUC∞ value, the extrapolated AUC after the Clast must not exceed 20 % of the AUC∞ value. Some or all of the specified pharmacokinetic parameters were not evaluable for subjects who discontinued early and did not have fully characterized concentration–time profiles of ustekinumab.
Body weight-adjusted serum ustekinumab concentrations and exposure parameters (Cmax and AUCs) were obtained using the following equation:
where WTindividual represents the body weight of an individual subject and WTmean represents the mean body weight of the two study populations.
2.7 Statistical Analyses
Descriptive statistics were used to summarize serum ustekinumab concentrations at each scheduled sampling timepoint. Concentrations below the lowest quantifiable concentration were assigned a value of zero for the purpose of computing descriptive statistics. Missing data remained missing, and no data imputations were performed. Descriptive statistics were also used to summarize the derived pharmacokinetic parameters of ustekinumab.
No formal hypothesis testing was planned in either study, and, therefore, no formal sample size determination was performed. In this cross-study comparison, a linear mixed model approach (SAS 9.1, SAS Institute Inc., Cary, NC, USA) was used to compare the log-transformed exposure parameters, Cmax and AUCs (either the original or body weight-adjusted values) generated from the 90-mg dose groups in the two studies. The ratios of the geometric means of the Cmax and AUCs in Chinese subjects (Test) to those in non-Chinese subjects (Reference) along with the 90 % parametric confidence intervals (CIs) were calculated. According to the criteria specified by the SFDA of China [17, 18], the comparability of the pharmacokinetics of ustekinumab between the two study populations could be concluded if the 90 % CI for the ratio of the geometric means for AUCs was within the range of 0.80–1.25 and the 90 % CI for the ratio of the geometric means for Cmax was within the range of 0.70–1.43. The t½ values between Chinese and non-Chinese subjects were also compared using a two-sided Student’s t-test at a statistical significance level α = 0.05. The t½ of ustekinumab was assumed to be dose-independent, and all individual t½ values generated from both dose groups (45 mg and 90 mg) in Study 2 (Chinese) were used in the statistical comparison.
2.8 Immunogenicity Assessment
Subjects were classified as having a positive ADA status if ADAs were detected in the sample evaluated after exposure to ustekinumab. If ADAs were not detected in the sample evaluated after exposure to ustekinumab, subjects were classified as having a negative ADA status.
2.9 Safety and Tolerability Assessments
In both studies, subjects were monitored for type, incidence and severity of any AEs and serious AEs (SAEs) that occurred throughout the study period. The severity of each AE was graded by investigators as mild, moderate or severe, and the relationship between the AEs and the study agent was indicated by investigators (with the possibility from low to high) as not related, unlikely/doubtfully related, possibly related, probably related, or very likely/definitely related. AEs of special interest included bacterial (especially TB), viral and fungal infections, malignancies and hypersensitivity reactions (including angioedema and possible anaphylaxis). Other tolerability assessments included clinical laboratory tests (e.g., routine haematology, biochemistry, immunology and urinalysis measurements, and TB tests), physical examinations, ECG measurements and vital signs (sitting systolic and diastolic blood pressure, heart rate and oral temperature after a minimum of approximately 5 min of rest). Measurements of vital signs were performed at screening, check-in (1 day before injection), within 1 h before injection, and at 1, 7, 14, 42 and 84 days (12 weeks) after injection in Study 1 or at 4, 7, 42 and 84 days (12 weeks) after injection in Study 2.
3 Results
3.1 Study Subjects
In Study 1, a total of 31 healthy non-Chinese (Caucasian: 77.4 %; black: 12.9 %; Asian: 0.0 %; other: 9.7 %) male subjects, with a mean age of 24.6 years (range 19–43 years), received a single dose of ustekinumab 90 mg. Among these, 26 completed the study through 84 days (12 weeks), and five subjects discontinued early due to reasons unrelated to AEs (two subjects withdrew consent to continue participation in the study, two subjects were discharged for using unacceptable concomitant medications, and one subject discontinued the study due to a deviation from the protocol-specified procedures) (Fig. 1a). In Study 2, a total of 24 healthy Chinese male subjects, with a mean age of 25.1 years (range 18–43 years), received a single dose of ustekinumab 45 mg (n = 12) or 90 mg (n = 12) (Fig. 1b). All of the 24 subjects completed the study through 84 days (12 weeks).
Although the weight inclusion criterion (60–90 kg) was the same in both studies, the mean weight and body mass index (BMI) were significantly lower in Study 2 (Chinese) than in Study 1 (non-Chinese) (65.7 vs. 80.3 kg and 22.4 vs. 26.3 kg/m2; p < 0.001 for both; Table 1). The overall mean body weight was 74.1 kg in the combined study population. Most of the Chinese subjects (23/24, 95.8 %) weighed <74 kg, while most of the non-Chinese subjects (25/31, 80.6 %) weighed ≥74 kg.
3.2 Pharmacokinetics
The mean [standard deviation (SD)] serum concentration–time profiles of ustekinumab 45 mg and 90 mg following a single SC injection are presented in Fig. 2. The mean serum ustekinumab concentrations peaked approximately 4–7 days after injection and then declined in an apparently mono-exponential manner through the end of the studies. Within Study 2, serum ustekinumab concentrations increased in an approximately dose-proportional manner at each sampling timepoint: a 2.0-fold increase in dose from 45 mg to 90 mg resulted in an average 2.0-fold (range 1.7- to 2.4-fold) increase in mean serum ustekinumab concentrations. Between studies, however, the mean serum ustekinumab concentrations at each sampling timepoint appeared to be approximately 1.3-fold higher (range 1.0- to 1.7-fold) for Chinese subjects in the 90-mg group than those for non-Chinese subjects who received the 90-mg dose.
Among the 31 subjects enrolled in Study 1, 30 had evaluable samples for Cmax and tmax, 29 had samples evaluable for AUClast, and 23 had evaluable samples for all other pharmacokinetic parameters; all 24 subjects in Study 2 had samples evaluable for all pharmacokinetic parameters (Table 2). After a single SC injection of 45 mg or 90 mg, ustekinumab was absorbed into the systemic circulation with a median tmax ranging from 4.0 to 8.5 days (overall median tmax = 7.0 days). The individual tmax values ranged from 3.0 to 28.0 days in the 45-mg group in Study 2 and from 3.0 to 17.0 days in the two 90-mg groups. Ustekinumab was eliminated from the circulation with an overall mean t½ of approximately 3 weeks. The mean Vz/F values ranged from 80.3 to 97.3 mL/kg.
The data suggested linear pharmacokinetics of ustekinumab following a single SC injection at the dose levels studied. In Study 2, the systemic exposure (Cmax and AUCs) increased in an approximately dose-proportional manner while CL/F, Vz/F and t½ appeared to be dose independent. However, the systemic exposure (mean Cmax and AUCs) of ustekinumab 90 mg was approximately 1.1- to 1.3-fold higher in Chinese subjects than in non-Chinese subjects (Table 2).
3.3 Statistical Comparisons
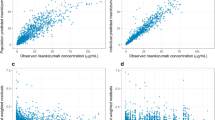
The systemic exposure (Cmax and AUCs) of ustekinumab appeared to be associated with subject body weight with a trend toward lower systemic exposure in subjects with higher body weight (Fig. 3). The AUClast and AUC∞ values were statistically higher in Chinese subjects who received the 90-mg dose compared with non-Chinese subjects who received the 90-mg dose. The geometric mean ratios (90 % CI) for AUClast and AUC∞ in Chinese versus non-Chinese subjects were 1.24 (1.04–1.48) and 1.31 (1.09–1.58), respectively, the upper bounds of which were all outside the comparability acceptance interval of 0.80–1.25. The geometric mean ratio (90 % CI) for Cmax in Chinese versus non-Chinese subjects was 1.13 (0.94–1.36), which was within the comparability acceptance interval of 0.70–1.43 [17, 18].
Individual systemic exposure [Cmax (a), AUClast (b), and AUC∞ (c)] versus body weight in the 90-mg groups in healthy Chinese and non-Chinese male subjects. AUC area under the serum concentration versus time curve, AUC ∞ AUC from time zero to infinity, AUC last AUC from time zero to time of last measurable concentration, C max maximum observed serum concentration
Serum ustekinumab concentrations in the 90-mg groups appeared to be comparable between the two study populations when individual serum concentrations were adjusted to a subject with a weight of 74 kg, which was the overall mean body weight of the combined study population (Fig. 4).
Individual exposure parameters were also adjusted to a subject with a weight of 74 kg. The log-transformed weight-adjusted Cmax and AUC values were approximately normally distributed. The distribution of the weight-adjusted exposure parameters overlapped between the two study populations (Fig. 5). Specifically, the ratios of geometric means of the weight-adjusted AUClast and AUC∞ were both around 1 (0.99 and 1.04, respectively), and the 90 % CIs of the geometric mean ratios (0.85–1.16 and 0.88–1.22, respectively) were all within the stringent comparability acceptance interval of 0.80–1.25 (Table 3). Although the lower bound of the 90 % CI for the geometric mean ratio of weight-adjusted Cmax fell slightly below 0.80, it was still within the less stringent comparability acceptance interval of 0.70–1.43 for Cmax specified by the SFDA of China [17, 18]. The totality of these results suggests that the systemic exposure of ustekinumab was statistically comparable between Chinese and non-Chinese healthy male subjects when adjusted by subject body weight.
Box plots of body-weight adjusted systemic exposure [Cmax (a), AUClast (b) and AUC∞ (c)] of ustekinumab in the 90-mg groups in healthy Chinese and non-Chinese male subjects. The solid and dashed lines inside each box represent the median and mean, respectively; the lower and upper bounds of the box represent the 25th and 75th percentiles, respectively; the whiskers (error bars) represent the bounds of 1.5 times the interquartile range; and the open circles represent the outlier values. AUC area under the serum concentration versus time curve, AUC ∞ AUC from time zero to infinity, AUC last AUC from time zero to time of last measurable concentration, C max maximum observed serum concentration
In addition, the t½ values were approximately normally distributed. The mean (SD) t½ values were 21.6 (4.3) days in Chinese subjects (n = 24) and 22.4 (7.0) days in non-Chinese subjects (n = 23) and were not significantly different (p > 0.05).
3.4 Immunogenicity
In Study 1, of the 29 non-Chinese subjects who had appropriate samples, one subject (3.4 %) tested positive for ADAs during the study period. In Study 2, none of the 24 Chinese subjects tested positive for ADAs during the study period.
3.5 Safety and Tolerability
All subjects who received ustekinumab were monitored for AEs through 84 days following injection. Overall, single SC injections of ustekinumab were well tolerated in both Chinese (45 mg or 90 mg doses) and non-Chinese (90 mg dose) healthy male subjects. There were no deaths, SAEs or withdrawals from the studies due to AEs. There were no clinically significant changes or abnormalities in clinical laboratory values, vital signs, ECGs or physical examinations. No AEs of special interest, including TB infections, malignancies or hypersensitivity reactions, were observed.
In Study 1, 23 (74.2 %) non-Chinese subjects experienced at least one AE: 12 subjects (38.7 %) had AEs of mild intensity, 11 (35.5 %) had AEs of moderate intensity, and no subjects had any AEs of severe intensity. Overall, the most common AEs were in the system-organ classes of respiratory, thoracic and mediastinal disorders (25.8 %) and nervous system disorders (22.6 %). AEs that were reported by more than one subject were headache (seven; 22.6 %), pharyngolaryngeal pain (five; 16.1 %), arthralgia (four; 12.9 %), cough (three; 9.7 %), toothache (three; 9.7 %), diarrhoea (two; 6.5 %), musculoskeletal chest pain (two; 6.5 %), feeling hot (two; 6.5 %) and nasopharyngitis (two; 6.5 %). One subject (3.2 %) had an AE (infective conjunctivitis) that was considered to be probably related to the study agent, nine subjects (29.0 %) had AEs that were considered to be possibly related to the study agent, three subjects (9.7 %) had AEs that were considered to be unlikely to be related to the study agent, and ten subjects (32.3 %) had AEs that were considered to be not related to the study agent. A mild injection-site reaction (bruising) was observed in one subject (3.2 %). The subject who tested positive for ADAs did not have any injection-site reactions or other AEs.
In Study 2, two (16.7 %) Chinese subjects who received the 45-mg dose and one (8.3 %) who received the 90-mg dose experienced one AE each during the study period: an upper respiratory tract infection and an ear injury in the 45-mg group and epistaxis in the 90-mg group. All three AEs were mild. One AE was considered to be unlikely to be related to the study agent, and two AEs were considered to be not related to the study agent. In addition, no injection-site reactions were observed.
4 Discussion
The pharmacokinetics of ustekinumab have been characterized in these two Phase 1 studies in healthy Chinese and non-Chinese male subjects. After a single SC injection of 45 mg or 90 mg, ustekinumab was slowly absorbed into the systemic circulation with an overall median tmax of approximately 1 week. Following the Cmax, the mean serum concentration–time of ustekinumab declined in an apparently mono-exponential manner through the end of the study, which was consistent with the one-compartment open model reported for ustekinumab in the population pharmacokinetic analyses in patients with psoriasis or PsA [8, 9]. The relatively fast distribution phase might be masked by the slow absorption phase following SC injection. Notably, the individual tmax values ranged from 3.0 to 28.0 days, indicating a large inter-subject variability in drug absorption. In the population pharmacokinetic analysis in patients with PsA [9], the absorption rate constant (ka) was estimated to be 0.427/day with an inter-subject variability of 82.4 %, suggesting that it would take approximately 1.6 days (range 0.9–9.2 days) for 50 % of the administered dose to be absorbed from the injection site into the systemic circulation.
The mean Vz/F values were approximately 80.3–97.3 mL/kg, which is consistent with the volume of distribution values reported for other therapeutic mAbs [20]. Given an absolute bioavailability (F) of 57.2 % [21], the mean Vz is estimated to be approximately 48–56 mL/kg, suggesting that ustekinumab is primarily confined to the circulatory system with limited extravascular tissue distribution.
Ustekinumab was eliminated from the circulation with a mean t½ of approximately 3 weeks, consistent with the t½ values reported previously in patients with psoriasis (21.6 days) [8] or PsA (21.2 days) [9] and those for other fully human IgG1 therapeutic mAbs [19, 20] or an endogenous IgG [19, 22].
The higher Cmax and AUC values for the 90-mg dose in Chinese subjects versus non-Chinese subjects may be attributable to a variety of factors including difference in subject weight between the two study populations. Although a weight of 60–90 kg was specified as an inclusion criterion for both studies, the distributions of subject body weight were different between the two study populations, with the Chinese subjects having a significantly lower mean body weight than the non-Chinese subjects (p < 0.001). The possibility that body weight was an important factor that contributed to the difference in systemic exposure between the two study populations is supported by the population pharmacokinetic analyses in patients with psoriasis or PsA, in which the CL/F increased with increases in body weight, and the systemic exposure to ustekinumab was predicted to decrease with increasing body weight [8, 9]. Race was not a significant factor that contributed to the inter-subject variability in the pharmacokinetics of ustekinumab after the differences in body weight across races were considered. Body size (body weight or body surface area) has been reported as a significant covariate for the clearance of many other IgG-based mAbs [19, 20].
When individual concentrations and exposure parameters were adjusted by subject body weight, the pharmacokinetics of ustekinumab were statistically comparable between Chinese and non-Chinese healthy male subjects. The ratios of geometric means of weight-adjusted AUCs met the stringent comparability acceptance criteria of 0.80–1.25. Although the lower bound of the 90 % CI for the geometric mean ratio of weight-adjusted Cmax fell slightly below 0.80, it was still within the less stringent comparability acceptance criteria of 0.70–1.43 specified by the China SFDA. Therefore, the slightly lower weight-adjusted Cmax in Chinese-subjects was not considered statistically significant or clinically meaningful. The numeric differences in exposure parameters that remained after weight adjustment might be attributable to the small sample size, cross-study comparison, assay variability and inter-subject variability typically observed with therapeutic mAbs.
Systemic exposure of ustekinumab was reported to be associated with clinical response in patients with moderate-to-severe plaque psoriasis. Patients with higher systemic exposure generally had a greater clinical response than patients with lower systemic exposure [11]. Because the pharmacokinetics of ustekinumab are comparable between Chinese and non-Chinese healthy male subjects, Chinese and non-Chinese patients with psoriasis who have the same weight are expected to achieve comparable efficacy when treated with the same dose and dosing regimen that are approved by the US FDA [23, 24]. Comparable efficacy and safety profiles of ustekinumab have been reported between Asian (Korean and Taiwanese) and non-Asian (predominantly Caucasian) patients with moderate-to-severe plaque psoriasis [13]. The efficacy and safety profiles of ustekinumab are being evaluated in a Phase 3 study in Chinese patients with moderate-to-severe plaque psoriasis (Clinical trial registration: NCT01008995).
Single SC injections of ustekinumab 45 mg or 90 mg were generally well tolerated in both Chinese and non-Chinese healthy male subjects. However, the incidence of AEs appeared to be higher in non-Chinese subjects, which may be due to potential differences between the healthcare cultures in the USA and China. Non-Chinese subjects in the USA may have been more likely to report suspected AEs, while Chinese subjects may have been more conservative in reporting any minor discomforts. Also, these studies were Phase 1 studies that included only a small number of healthy male subjects. As a result, the AE data should be interpreted with caution and should not be directly compared. More comprehensive AE data are being evaluated in large-scale Phase 3 studies in Chinese and non-Chinese patients with psoriasis [25, 26].
In these two Phase 1 studies, one subject (non-Chinese) developed ADAs during the study period. The incidence of ADAs could have been underestimated with only a single-dose injection of ustekinumab. In three Phase 3 studies in patients with psoriasis (n = 2,899), the incidence rates of ADAs were reported to be approximately 5 % and remained stable through up to 3 years with maintenance therapy every 12 or 8 weeks [27].
4.1 Limitations
Both studies had small sample sizes and were not originally designed for a statistical comparison. In addition, none of the non-Chinese subjects in Study 1 received a 45-mg SC injection of ustekinumab, which prevented a direct comparison between the two study populations of the pharmacokinetics of ustekinumab 45 mg, which is the recommended dose for patients with psoriasis who weigh ≤100 kg [23]. Therefore, the results from this analysis should be interpreted with caution.
5 Conclusions
The pharmacokinetics of ustekinumab following a single 45-mg or 90-mg SC injection were compared across two Phase 1 studies in Chinese and non-Chinese healthy male subjects. The data suggest that subject body weight was an important factor contributing to the difference in systemic exposure between the two study populations. No statistically significant ethnic differences in the systemic exposure of ustekinumab were observed when the difference in subject weight was considered.
References
Nair RP, Ruether A, Stuart PE, et al. Polymorphisms of the IL12B and IL23R genes are associated with psoriasis. J Invest Dermatol. 2008;128(7):1653–61.
Torti DC, Feldman SR. Interleukin-12, interleukin-23, and psoriasis: current prospects. J Am Acad Dermatol. 2007;57(6):1059–68.
Gottlieb AB, Cooper KD, McCormick TS, et al. A phase 1, double-blind, placebo-controlled study evaluating single subcutaneous administrations of a human interleukin-12/23 monoclonal antibody in subjects with plaque psoriasis. Curr Med Res Opin. 2007;23(5):1081–92.
Griffiths CE, Strober BE, van de Kerkhof P, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010;362(2):118–28.
Krueger GG, Langley RG, Leonardi C, et al. A human interleukin-12/23 monoclonal antibody for the treatment of psoriasis. N Engl J Med. 2007;356(6):580–92.
Leonardi CL, Kimball AB, Papp KA, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008;371(9625):1665–74.
Papp KA, Langley RG, Lebwohl M, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet. 2008;371(9625):1675–84.
Zhu Y, Hu C, Lu M, et al. Population pharmacokinetic modeling of ustekinumab, a human monoclonal antibody targeting IL-12/23p40, in patients with moderate to severe plaque psoriasis. J Clin Pharmacol. 2009;49(2):162–75.
Zhu YW, Mendelsohn A, Pendley C, et al. Population pharmacokinetics of ustekinumab in patients with active psoriatic arthritis. Int J Clin Pharmacol Ther. 2010;48(12):830–46.
Zhou H, Hu C, Zhu Y, et al. Population-based exposure-efficacy modeling of ustekinumab in patients with moderate to severe plaque psoriasis. J Clin Pharmacol. 2010;50(3):257–67.
Zhu Y, Yan H, Yeilding N, et al. Exposure–response relationship of ustekinumab in two phase 3 studies in patients with moderate-to-severe plaque psoriasis [abstract]. AAPS J. 2009;11(Suppl 2). http://www.aapsj.org/abstracts/AM_2009/AAPS2009-002128.PDF.
Igarashi A, Kato T, Kato M, et al. Efficacy and safety of ustekinumab in Japanese patients with moderate-to-severe plaque- type psoriasis: long-term results from a phase 2/3 clinical trial. J Dermatol. 2012;39(3):242–52.
Tsai TF, Ho JC, Song M, et al. Efficacy and safety of ustekinumab for the treatment of moderate-to-severe psoriasis: a phase III, randomized, placebo-controlled trial in Taiwanese and Korean patients (PEARL). J Dermatol Sci. 2011;63(3):154–63.
Declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. Br Med J. 1996;313(7070):1448.
Geng D, Shankar G, Schantz A, et al. Validation of immunoassays used to assess immunogenicity to therapeutic monoclonal antibodies. J Pharm Biomed Anal. 2005;39(3–4):364–75.
Gabrielsson J, Weiner D. Pharmacokinetic and pharmacodynamic data analysis: concepts and applications. 4th ed. Stockholm: Swedish Pharmaceutical Press; 2007.
Guidance for bioavailability and bioequivalence studies of chemical drug products: China State Food and Drug Administration, Center for Drug Evaluation; 2005.
Liu YM, Pu HH, Liu GY, et al. Pharmacokinetics and bioequivalence evaluation of two different atorvastatin calcium 10-mg tablets: a single-dose, randomized-sequence, open-label, two-period crossover study in healthy fasted Chinese adult males. Clin Ther. 2010;32(7):1396–407.
Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(10):633–59.
Keizer RJ, Huitema AD, Schellens JH, et al. Clinical pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49(8):493–507.
Weber J, Keam SJ. Ustekinumab. BioDrugs. 2009;23(1):53–61.
Mascelli MA, Zhou H, Sweet R, et al. Molecular, biologic, and pharmacokinetic properties of monoclonal antibodies: impact of these parameters on early clinical development. J Clin Pharmacol. 2007;47(5):553–65.
Stelara [package insert]. Horsham: Janssen Biotech Inc.; 2013.
Lebwohl M, Yeilding N, Szapary P, et al. Impact of weight on the efficacy and safety of ustekinumab in patients with moderate to severe psoriasis: rationale for dosing recommendations. J Am Acad Dermatol. 2010;63(4):571–9.
Gordon KB, Papp KA, Langley RG, et al. Long-term safety experience of ustekinumab in patients with moderate to severe psoriasis (Part II of II): results from analyses of infections and malignancy from pooled phase II and III clinical trials. J Am Acad Dermatol. 2012;66(5):742–51.
Lebwohl M, Leonardi C, Griffiths CE, et al. Long-term safety experience of ustekinumab in patients with moderate-to-severe psoriasis (Part I of II): results from analyses of general safety parameters from pooled phase 2 and 3 clinical trials. J Am Acad Dermatol. 2012;66(5):731–41.
Zhu Y, Shankar G, Yeilding N, et al. Immunogenicity assessment of ustekinumab in Phase 3 studies in patients with moderate to severe plaque psoriasis [abstract]. AAPS J. 2010;12(Suppl 1). http://www.aapsj.org/abstracts/NBC_2010/NBC10-000360.PDF.
Acknowledgments
The authors would like to thank the healthy volunteers, investigators and study personnel who made these two Phase 1 studies successful. They are indebted to Dr Dion Chen of Janssen Research & Development, LLC for his statistical analysis support. They also thank Dr Rebecca Clemente, Kirsten Schuck and Dr Mary Whitman of Janssen Biotech, Inc. for their assistance in preparing the manuscript.
Competing Interests
This study was funded by Janssen Research & Development, LLC. All authors are employed by Janssen Research & Development, LLC and own stock in Johnson & Johnson.
Role of the Funding Source
Employees of the study sponsor, Janssen Research & Development, LLC, participated in the study design, collection, analysis and interpretation of the data, and writing the manuscript. Additional writing support was provided by employees of Janssen Biotech, Inc. All authors reviewed and approved the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, Y., Wang, Q., Frederick, B. et al. Comparison of the Pharmacokinetics of Subcutaneous Ustekinumab between Chinese and Non-Chinese Healthy Male Subjects across Two Phase 1 Studies. Clin Drug Investig 33, 291–301 (2013). https://doi.org/10.1007/s40261-013-0072-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0072-2