Abstract
Background
Although suicide-prevention campaigns have been implemented in numerous countries, Canada has yet to implement a strategy nationally. This is the first study to examine the cost utility of the implementation of a multidimensional suicide-prevention program that combines several interventions over a 50-year time horizon.
Methods
We used Markov modeling to capture the dynamic changes to health status and estimate the incremental cost per quality-adjusted life-year gained over a 50-year period for Ontario residents for a suicide-prevention strategy compared to no intervention. The strategy consisted of a package of interventions geared towards preventing suicide including a public health awareness campaign, increased identification of individuals at risk, increased training of primary-care physicians, and increased treatment post-suicide attempt. Four health states were captured by the Markov model: (1) alive and no recent suicide attempt; (2) suicide attempt; (3) death by suicide; (4) death (other than suicide). Analyses were from a societal perspective where all costs, irrespective of payer, were included. We used a probabilistic analysis to test the robustness of the model results to both variation and uncertainty in model parameters.
Results
Over the 50-year period, the suicide-prevention campaign had an incremental cost-effectiveness ratio (ICER) of $18,853 (values are in Canadian dollars) per QALY gained. In all one-way sensitivity analyses, the ICER remained under $50,000/QALY. In the probabilistic analysis, there was a probability of 94.8% that the campaign was cost effective at a willingness-to-pay of $50,000/QALY (95% confidence interval of ICER probabilistic distribution: 2650–62,375). Among the current population, the intervention was predicted to result in the prevention of 4454 suicides after 50 years (1033 by year 10; 2803 by year 25). A healthcare payer perspective sensitivity analysis showed an ICER of $21,096.14/QALY.
Interpretation
These findings demonstrate that a suicide-prevention campaign in Ontario is very likely a cost-effective intervention to reduce the incidence of suicide and suggest suicide-prevention campaigns are likely to be cost effective for some other Canadian provinces and potentially other countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
This is the first study to examine the cost utility of the implementation of a multidimensional suicide-prevention program that combines several strategies finding an ICER of $18,853 per QALY gained over a 50-year time horizon. |
These findings demonstrate that suicide-prevention campaigns in Ontario are a cost-effective intervention to reduce the incidence of suicide and along with other evidence suggest similar suicide-prevention campaigns are likely to be cost effective for all Canadian provinces and potentially other countries. |
1 Introduction
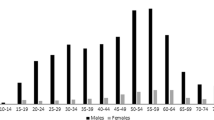
The global burden of suicide and suicide attempts is considerable, with 3.2 million incident-treated intentional self-harm injuries, an estimated 842,000 suicides annually, and 34.9 million years of life lost [1]. Self-harm is highest among those age 15–24 years and is generally higher among younger age groups but rates of suicide are highest among those aged 40–59 years [2], likely due to greater lethality of the chosen methods. In Canada, the burden of suicide is high and it is the ninth leading cause of death, responsible for 3926 deaths per year [3]. However, in part due to low non-suicide-related mortality, suicide is the second or third leading cause of death for individuals 10–44 years of age [2]. Self-harm is also very costly, with $2.95 billion in total costs due to productivity losses and medical care each year in the USA [4].
Suicide prevention campaigns were initiated in 11 Organisation for Economic Co-operation and Development (OECD) countries between 1992 and 2005, including the UK and USA [5]. These national campaigns have varied slightly, but have often included components similar to those investigated in the European Nuremberg Alliance against Depression (NAD) trial [6]. This trial investigated the use of community-based suicide-prevention strategies that involve training of family physicians to detect and treat depression, population campaigns aimed at increasing awareness of depression and suicide, and clinical follow-up of high-risk patients who have attempted suicide [6]. Despite the large humanistic and economic burden and numerous calls to action by medical journals and the media, Canada has yet to implement a national suicide campaign, although numerous elements have been incorporated into a Quebec campaign that began in 1999 [4, 7, 8].
Therefore, our primary objective was to assess from a societal perspective the incremental cost-effectiveness of a suicide-prevention campaign targeting the entire population of Ontario, which is the largest province in Canada, to inform the broader implementation of such a policy across Canada.
2 Methods
2.1 Study Setting and Intervention
We developed a Markov model to estimate the costs and effects of a suicide-prevention campaign in Ontario, Canada, compared to no intervention (Fig. 1). This intervention was modeled after suicide campaigns that have been previously implemented in Quebec and at the national level in other OECD countries and have been shown to be effective at reducing the rate of suicide [5, 8, 9]. The overall aim of these suicide-prevention programs was to improve treatment for patients with depression and lower suicidal behaviour. These programs were generally composed of four main components. First, there was an annual public health campaign to spread awareness and reduce stigma towards treatment. Second, training to assist in the identification of individuals at risk for suicide was provided to volunteers or community workers, such as police officers and teachers. Third, training on detection and treatment of depression and suicidal behaviour was provided to primary-care physicians. Additionally, health professionals were trained to effectively assess the suicidal intentions of individuals. Fourth, a high-risk psychosocial intervention was established that targeted those who attempted suicide and were treated in a hospital setting.
There were 11,478,804 adults age 16 + years in Ontario in 2016, with an average age of 46 years [10, 11]. We created a hypothetical cohort matching the size and average age of this population. We projected their costs and outcomes, and estimated the incremental cost-effectiveness ratio (ICER) over a life-time horizon of 50 years, to capture the long-term dynamics of suicide attempts, suicides, and suicide-prevention.
2.2 Model Design
We used a four-state Markov model (Fig. 1): (1) alive and no recent suicide attempt (ANRSA); (2) suicide attempt (i.e. also referred to as “suicide attempt and survive”); (3) suicide; and (4) death (other than suicide) consistent with states included in another suicide model [12]. All individuals started in the ANRSA state. If an individual attempts suicide and survives, they enter the “suicide attempt” state. This is a tunnel state in which individuals must remain for 5 years, after which they return to the ANRSA state. Risks of “re-attempting suicide and surviving” and “re-attempting suicide and dying” are elevated in the tunnel state for 5 years given the available evidence, given the lack of availability of most parameters beyond 5 years, and plateauing rates [13]. Death from other causes is elevated given the excess risk of accidental, undetermined, and other non-suicide deaths post attempt [14]. If individuals in the tunnel state re-attempt suicide and survive, they return to year one of the “suicide attempt” tunnel state. Two psychiatrists (J.Z. and P.K.) provided guidance on the development and clinical face validation of the model structure. The model does not assume that self-harm necessarily leads to suicide but does capture the fact that self-harm greatly elevates the risk of eventual suicide even if the initial self-harm was not of suicidal intent. Furthermore, the model allows individuals to die by suicide without first entering the attempted suicide and survived state. Our model did not include a depression state due to the lack of data on transition parameters. Each state was associated with a cost and utility weight obtained from the literature described in the following paragraphs.
2.3 Model Parameters
Model parameters for each state (i.e., including transition rates, costs, and utilities) were gathered from administrative databases, literature, and government reports. The “suicide attempt” tunnel state enabled year-specific utilities, costs, and transition rates following a suicide attempt. The model parameters were highest in year one of the tunnel [13]. We used age-specific values for costs, utilities, employment rates, and transition probabilities where available using the Ontario population.
2.3.1 Transition Probabilities
Our model had six transition probabilities: (1) ANRSA to “suicide attempt and survive”; (2) ANRSA to “suicide”; (3) ANRSA to “other death”; (4) “suicide attempt” to “suicide re-attempt and survive” (non-fatal re-attempts); (5) “suicide attempt” to “suicide re-attempt and suicide” (fatal re-attempt); and (6) “suicide attempt” to “other death” (Table 1). Transition probabilities were derived using data from existing literature, ICES, and Statistics Canada [13,14,15]. Rate values for suicide and suicide attempts were derived for the year 2012. We converted rates to probabilities using the formula p = 1 − e−rt and probabilities to rates using \( r = \,-\frac{1}{t} \times ln(1\, - \,p) \) [16].
Given the availability of data, we proxied the transition rate from the ANRSA to “suicide attempt and survive” with the rate of individuals with an emergency department visit for intentional self-harm. Although using emergency department visits for intentional self-harm may underestimate the true suicide attempt rate, many self-harm interventions including the interventions examined in this study target individuals with self-harm who present to hospital [17].
The probability of fatal (“suicide re-attempt and suicide”) and non-fatal re-attempts (“suicide re-attempt and survive”) was derived from a published systematic review and meta-analysis [13]. Given that cumulative probabilities for non-fatal and fatal re-attempts were available only for 1 and 5 years, year-specific probabilities between years 2 and 5 were calculated [13]. These year-specific probabilities were calculated by starting with the year 1 cumulative probability [13] [non-fatal (NF) = 0.163, fatal (F) = 0.016] and converting it into a rate. Then a recovery rate (R) for all years was applied to the rate and these rates were converted back to probabilities (i.e., FY2–5 = 0.016 × RY−1, R = 0.64; NF = 0.1630 × RY−1, R = 0.3). R was chosen such that the year-specific probabilities applied to a population would result in the same year five cumulative probability from the review (suicide attempts calculated: 22.4, review: 22.4; suicide calculated: 3.9, review: 3.9) [13]. These year-specific probabilities were used for the time-dependent probabilities of the tunnel.
Rates of deaths due to other causes were obtained from Statistics Canada for 2011–2013 [15]. The rate of other death among individuals in the “suicide attempt and survive” state was multiplied by 3.6, estimated based the excess risk of non-suicide death among individuals with an emergency department visit for self-harm in Ontario [14].
The overall population suicide rate was available from ICES for 2012 [18]. Although official suicide rates are an underestimate, prior Canadian research suggests these underestimates are not substantial (male:12%; female: 17.5%) and do not influence most epidemiologic conclusions [19]. The overall population rate includes suicides from both the ANRSA and the “Suicide attempt and survive” state. Given no estimates of the transition rate from ANRSA to suicide and the overall population rate would overestimate this rate, we used the model to estimate an adjustment to the overall population rate such that the model-generated number of suicides is less than 1% off of expected number of suicides (~ 43 K) (i.e. \( {\text{Adjustment}} = \frac{{\# {\text{suicides}}_{\text{total}} - \# {\text{suicides}}_{{{\text{SA}} \to {\text{S}}}} }}{{\# {\text{suicides}}_{\text{total}} }} \); #suicidestotal = population alive at all cycles × overall population suicide rate).
2.3.2 Costs
Costs were divided into three types: healthcare sector costs, non-medical costs, and costs of productivity losses estimated using the friction cost method [20] and were derived or estimated based on past studies and reports [9, 21,22,23] (Table 2). Healthcare sector costs included visits to the hospital, emergency department, and family physicians that are covered by the Ontario provincial government [9, 21, 23]. Age-specific mean healthcare costs were available for the overall population [21] and for the last year of life [23]. The overall population healthcare costs are a weighted average where overall = (probability of death × cost of death) + (probability of not death × cost of not death). Therefore, age-specific healthcare costs for the ANRSA were calculated as follows: (overall cost − (probability of death × cost of death))/probability of not death. Non-health-care sector costs included autopsy, police investigation, and funeral services [9]. Costs due to productivity losses due to premature death were calculated using a friction cost method with an average replacement value of 3 months [20]. The friction cost method takes the employer’s perspective and captures only the lost hours of work until a replacement employee is hired [20]. We chose the friction method over the human-capital method, which captures the lost hours of work for entire life of the patient, to provide a more conservative and realistic cost estimate given significant unemployment [20]. Productivity loss per suicide or death was calculated as one-fourth of the annual wage (i.e., $50,625.12), adjusted for age-specific employment rates from 2016 from Statistics Canada [22, 24]. We also included estimated productivity losses due to suicide attempts that resulted in admission ($9726) or not ($1015) in 2000 US currency from a prior study calculated based on probabilities of short- or long-term disability [4]. Although their inclusion introduces additional uncertainty, societal costs (i.e., non-medical costs and productivity losses) were included given that most countries recommend societal costs as a primary analysis or to be included as a secondary analysis and to avoid underestimating potential cost-offsets due to averted attempts and deaths given the high productivity losses due to these events [25]. There is trade-off that a societal perspective may be less relevant to the health payer who will be covering most of the costs of the intervention. Therefore, we included a sensitivity analysis conducted from the healthcare perspective only including intervention and medical costs. Each of the U.S. costs were converted to Canadian dollars using the Purchasing Power Parity (PPP) (i.e. $1.00 USD = $1.23 CAD) [26]. All costs in our model were inflated to 2016 CAN dollars using the appropriate component of the Consumer Price Index (CPI) [27].
2.3.3 Utilities
Utilities among the general population were age-specific estimates based on EQ-5D values from the US Medical Expenditure Panel Survey (Table 3) [28]. Using the person trade-off method, the utility for the suicide attempt state was estimated as 0.54 (i.e. disability weight = 0.46) by 16 Dutch medical practitioners familiar with suicidality as the utility weight for being in a state related to a suicide attempt for 1 year and converted to age-specific values by Pil et al. [12, 29]. Disability weights for another study were very similar (0.447) [30]. Given the utility values were available for the first year post-suicide attempt, we assumed that the individuals recovered to full utility after the first year. Any additional utility decrements beyond year 1 missed would result in the model findings becoming more conservative.
2.3.4 Intervention Model Parameters
We used two estimates to capture the effect of the intervention (Table 4). First, we used the estimated mean effect of a suicide campaign implemented at the national level from a study of 21 Organisation for Economic Co-operation and Development (OECD) countries, 11 of which implemented a suicide campaign [5]. The estimated mean effect from the study used fixed effects panel regression methods, which eliminate time-invariant heterogeneity and also controlled for a number of time-variant characteristics reflecting the political features of the country (e.g., welfare generosity), economic characteristics (e.g., unemployment rate), and socio-demographic variables (e.g., level of development). Given Canada and other OECD countries were included in the control group, and the countries most similar to Canada including the USA, UK, and Australia (i.e., British or former British colonies from the OECD) were included in the intervention group, this effect estimate is likely generalizable to Canada. We have also varied the effect of this intervention in sensitivity analyses to explore possible violations of this assumption. We converted the absolute reduction in suicide rates to a relative rate reduction, which we applied to the transition from ANRSA to “suicide”. We also applied the same relative reduction to the transition from ANRSA to “suicide attempt and survive”.
Second, the suicide-prevention campaign we modeled included a psychosocial intervention targeting individuals who attempted suicide. Given available evidence from a systematic review and meta-analysis, we applied this intervention effect as a relative risk reduction in the transition rate from “suicide attempt” to “suicide re-attempt” [17]. Since there is only evidence of effectiveness at 1 year post-suicide attempt, we assumed the effect lasted 1 year and afterwards there were no effects from years 2–5 of the tunnel [17].
2.4 Base-Case Analysis
We conducted a cost-utility analysis using the societal perspective. Outcomes included quality-adjusted life-years (QALYs) and costs. The costs and QALYs are incurred as individuals transition between the different health states of the model. The 50-year time horizon was chosen to capture a life-time perspective and given that the mean age of the Ontario adult population was 46 years old. In our probabilistic simulations, cohort members moved between health states in yearly cycles, due to a lack of data on parameters less than 1 year and requirement of additional assumptions to incorporate shorter cycles. Future costs and health benefits were discounted at 1.5% annually in accordance with Canadian Agency for Drugs and Technologies in Health (CADTH) guidelines [31].
2.5 Sensitivity Analysis
We conducted one-way sensitivity analyses setting the ranges of the confidence intervals where available or otherwise used ± 30%, given prior studies have often used a range of 10–30% when confidence intervals were not available or used [32,33,34]. The results of the deterministic one-way sensitivity analyses are presented as a Tornado diagram (Fig. 2), which shows the value of the incremental cost-effectiveness ratio (ICER) based on the ranges of the input parameters and ranks the variables based on the degree of uncertainty in impacting the resulting ICER. We conducted additional sensitivity analyses using a discount rate of 0% and 3% as recommended by CADTH [31] and with 5% given common use internationally [35]. We also analyzed the model with a time horizon of 10 and 25 years, and using the healthcare payer perspective without loss of productivity costs or other non-medical costs (i.e., autopsy, funeral, police, etc.).
We conducted a probabilistic analysis by re-running the model 100,000 times to examine the impact of uncertainty in all parameters on our conclusions and to estimate the probability of being cost effective at different societal willingness to pay (WTP) thresholds (i.e., for an additional unit of effect). The 95% interval was assessed from the 2.5% and 97.5% percentiles of the distribution of the ICER estimates. We used beta distributions for probabilities, log-normal distributions for intervention effects, and gamma distributions for costs, and used established formulas (Tables 1, 2, 3, 4) [36]. Where the standard deviation was unknown, we estimated it as 0.33 times the mean in accordance with other Canadian research; prior studies have used between 0.1 and one times the mean as the standard deviation [37,38,39,40]. Although we simulated random draws from an age distribution (mean = 46, SD 20% mean), probabilistic sensitivity analysis was conducted only for non-age-specific variables due to the limitation of TreeAge [41]. One-way sensitivity analyses were conducted for all age-specific variables instead. We presented the results as an ICER scatterplot with the 95% confidence interval (CI) ellipse and WTP threshold and as a cost-effectiveness acceptability curve, which plots the proportion of the simulations with an ICER below each WTP threshold. Due to dense clustering of individual simulation estimates, we have reduced the ICER scatter plot to only 1000 simulations. All analyses were conducted with a half-cycle correction in TreeAge Pro 2016 software [42].
3 Results
3.1 Base Case
Our model showed that the introduction of a suicide campaign had discounted incremental costs and QALYs per capita of $144 and 0.008, respectively. This resulted in an ICER of $18,853 per QALY (Table 5). After 10 years, there would be 9379 suicides in the intervention arm and 10,412 suicides in the non-intervention arm, resulting in 1033 prevented suicides (9.9% decrease). Over 50 years, the model estimated that the campaign would have resulted in 4454 suicides prevented (10.3% decrease) (Table 6).
3.2 Sensitivity Analyses
Figure 2 shows a tornado diagram displaying the impact of a range of values for each variable on the ICER. The variables having the largest impact on the ICER were the intervention cost and the effect of the intervention on suicide rates. Other key variables were the utility of the suicide attempt state, the probability of suicide attempt from the ANRSA state, and the cost of medical care in the ANRSA state. However, in all one-way sensitivity analyses, the ICER remained under $50,000/QALY. The ICER scatterplot demonstrating the clustering of simulation estimates is presented in Fig. 3a. The probabilistic sensitivity analyses show that 94.8% of the simulation trials were found to be cost effective at a WTP of $50,000 per QALY, and this percentage increased to 99.2% at a WTP threshold of $100,000 per QALY (Fig. 3b). We found an ICER of $20,802, $17,010 and $14,809 at a discount rate of 0, 3, and 5%, respectively (Table 5). The ICER was $8623 at 10 years and $8784 at 25 years (Table 7). We found that the ICER was $21,096.14 from the healthcare payer perspective.
a Incremental cost-effectiveness ratio scatter-plot with 1000 simulations—base case (50 years, 1.5% discount rate, societal perspective). b Cost-effectiveness acceptability curve—base case. Due to dense clustering of estimates, the scatter-plot shows the first 1000 simulations; campaign intervention vs. no-intervention
4 Discussion
This is the first study examining the cost utility of the implementation of a multidimensional suicide-prevention program. We found a cost-effectiveness ratio of $18,853 per QALY, with a 94.8% chance of being cost effective at a WTP threshold of $50,000 per QALY and resulting in a large number of suicides (4454; 10.3% decrease) prevented over a 50-year period. The cost and effect of the intervention were the most important parameters; however, in all one-way sensitivity analyses the ICER was less than $50,000 per QALY.
Our base-case results show that the differences in the costs and effects were relatively small across the two groups. The small difference in costs reflects the relatively small cost of implementation (i.e., ~ $3 per capita) [9], while the difference in effects reflects the rarity of the events under consideration (i.e., suicide rate and intentional self-harm rate are 11 and 128 per 100,000 person-years, respectively). Changes to these rates would result in relatively small changes in the QALYs when examined among all individuals in a population rather than only those at high risk for suicide.
To our knowledge, there are only four published studies to date that have performed an economic evaluation of suicide-prevention programs or policies for the general population [9, 12, 43, 44]. These studies modeled the effects of a telephone hotline [12], multi-dimensional suicide campaign [9], bridge barrier [43], or several different interventions including media regulations, gun legislation and buybacks, and follow-up of patients who attempted suicide with cognitive behavioral therapy [44]. With the exception of gun legislation and buybacks, all interventions were considered cost effective at conventional benchmarks and demonstrate that there are other cost-effective interventions to be considered in future policy discussions of multidimensional suicide campaigns [9, 12, 43, 44]. More recently, two studies have published results focusing exclusively on the cost effectiveness of interventions targeting similar high-risk populations in the emergency department [45, 46]. These studies have found these interventions to be highly cost effective or cost saving, which suggests that this component of the campaign will be particularly important to implement.
Vasiliadis et al. examined the cost effectiveness of a multidimensional suicide-prevention program implemented in Quebec similar to the one we modeled, and found an ICER of $3979 per life-year saved [9]. We have extended the work of Vasiliadis et al. [9] in several ways. Key differences in methods included the use of a 1-year study period in comparison to the use of Markov models with a 50-year time horizon in this study, examination of cost effectiveness (i.e., $ per life year saved) rather than cost utility (i.e., $ per QALY). Furthermore, this study used a more conservative estimate of the effects of the intervention on suicides and suicide attempts based on econometric evidence from numerous countries that implemented suicide campaigns compared to the 27% for suicide attempts and 16% for suicides that were previously used as estimated from the Nuremberg Alliance against Depression (NAD) trial [5, 6, 9]. These differences in methodology may have led to the higher ICER estimate in our study [9]. However, regardless of the methodological differences, both studies demonstrated these interventions to be cost effective in Canada’s largest provinces.
4.1 Policy Implications
Although suicide-prevention strategies have been implemented in Quebec and in some jurisdictions as pilot projects, such as the Zero suicide campaign in London, Ontario, no national suicide-prevention strategy has been implemented in Canada. This paper is a response to calls for the implementation of a national suicide-prevention strategy in an editorial in Canada’s Leading Medical Journal (CMAJ) [7] and articles in several Canadian newspapers. Our study adds to a growing literature examining the effectiveness and cost effectiveness of suicide-prevention interventions. In 1999, Quebec implemented a campaign that was similar to the campaign modelled in our study. It included starting a provincial hotline and opening suicide-prevention centres, initiating better mental health treatment for those attempting suicide, installing bridge and railway barriers, and improving staff training at youth protection agencies. This strategy was followed by a 45% reduction in the rate of suicides in the following decade from 26.5 per 100,000 people to 14.6 per 100,000 people in 2009 [8]. However, to our awareness there have not been any formal reviews of this intervention published, and this estimate does not make use of a control group or account for pre-existing time trends [8]. Although this Canadian measure of effectiveness is a before-after comparison without reference to a control group, evidence across 21 OECD countries also demonstrated decreasing suicide rates post-implementation of suicide campaigns with considerably more robust methods including panel econometric methods [5]. Given evidence from our Ontario study and Vasiliadis et al.’s [9] study in Quebec, suggesting multidimensional suicide-prevention campaigns are cost effective in Canada’s largest provinces, the current evidence base suggests that the introduction of a suicide-prevention campaign across Canada is likely to be both effective and cost effective. Greater resources should be allocated towards suicide-prevention in order to prevent a considerable number of deaths for a minimal cost per-capita.
4.2 Strengths and Limitations
A strength of this study was the design and use of a Markov model, tunnel states, and a 50-year time horizon. We were able to take into account the long-term dynamics of suicide attempts and time-dependent probabilities, and account for the greater healthcare costs among individuals who do not commit suicide. Furthermore, this study used high-quality inputs including estimates of the effect of suicide-prevention campaigns and psychosocial interventions [5, 17] and several transitions rates derived from high-quality government-collected administrative and statistical data. Lastly, we made use of both deterministic and probabilistic sensitivity analyses to examine the role of variability and uncertainty in model parameters, thereby testing the robustness and enhancing the generalizability of our study findings.
Our study had several limitations. The model was constructed for the general adult population and does not take into account the high variability of suicide rates known to exist regionally and among individuals of different ethnic origins or ancestries (e.g., indigenous populations). Assumptions about the cost or effects of interventions might not apply universally to all aspects of Canada’s population. Future work should explore this heterogeneity and examine cost effectiveness of suicide prevention for these key subpopulations.
Second, there were limitations to the states and parameters used in the model. The model used intentional self-harm presenting to emergency departments (EDs) as the estimate of suicide attempts. These events are less common and more severe than suicide attempts that do not present to hospitals and may be non-suicidal. However, most parameters for re-attempts and intervention effects were for intentional self-harm that presented to hospital [13, 29], and individuals who self-harm without suicidal intent presenting to healthcare are similar to those with suicidal intent, including the eventual risk of suicide [47]. Furthermore, we did not include costs associated with caregiver burden. Given the lack of data on transition parameters, we were not able to model suicide attempts that did not require hospital care and did not include a depression state. It has been previously assumed that the intervention would have identified and treated an additional 7% individuals with depression [9]. Although we may have missed some of the increased costs of treating self-harm and depression in primary care, we did not account for the effects of the intervention on productivity costs or utility among these patient groups. Although we cannot be certain, we believe that the exclusion of self-harm not requiring hospital care and a depression state would largely not have altered our results and would likely result in more conservative findings. Furthermore, any potential underestimation of treatment costs would have been covered in our one-way sensitivity analyses, which varied intervention costs to a much greater extent. Additionally, the utility parameters for the self-harm state was estimated by Dutch healthcare professionals rather than patients or the general population, given the unavailability of patient reported utilities.
Third, the model was for a closed population, which gradually lost members over time to suicide and other deaths. Furthermore, this model reflects the population as is and did not incorporate future changes in population structure (i.e., migration) or economic conditions (i.e., GDP, unemployment). Future work should consider open populations that that take into account new population members and factor in potential demographic and economic changes.
Lastly, given many of these inputs were from Ontario or Quebec and there are differences in the levels of suicide and in mental healthcare systems across countries, the results may not be generalizable beyond a single-payer healthcare setting. Given that suicide-prevention campaigns have been shown to be effective across countries [5], the cost-effectiveness in other jurisdictions will depend greatly on the ability of jurisdictions to implement these interventions at a low cost per capita.
5 Conclusion
We found that the introduction of a suicide-prevention campaign may be cost effective in Ontario. Given parameters reflecting the cost and effects of the policy were the most important in sensitivity analyses, this suggests the need to learn from existing suicide campaigns implemented elsewhere. Cost-effectiveness modeling of suicide prevention is feasible and may help inform policy discussions of suicide prevention in Canada.
Data availability
Data are available from the authors upon request.
References
Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22:3–18.
Skinner R, McFaull S, Draca J, Frechette M, Kaur J, Pearson C, et al. Suicide and self-inflicted injury hospitalizations in Canada (1979 to 2014/15). Health Promot Chronic Dis Prev Can. 2016;36:243–51.
Statistics Canada. Health Fact Sheets—the ten leading causes of death, 2012 [Internet]. 2015. http://www.statcan.gc.ca/pub/82-625-x/2015001/article/14296-eng.htm. Accessed 29 Aug 2019.
Corso PS, Mercy JA, Simon TR, Finkelstein EA, Miller TR. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32:474–82.
Matsubayashi T, Ueda M. The effect of national suicide-prevention programs on suicide rates in 21 OECD nations. Soc Sci Med. 2011;73:1395–400.
Hegerl PDU, Wittmann M, Arensman E, van Audenhove C, Bouleau J-H, van der Feltz-Cornelis C, et al. The ‘European Alliance Against Depression (EAAD)’: a multifaceted, community-based action programme against depression and suicidality. World J Biol Psychiatry. 2008;9:51–8.
Eggertson L, Patrick K. Canada needs a national suicide-prevention strategy. CMAJ. 2016;188:E309–10.
Eggertson L. Quebec cuts suicide rates despite lack of a national prevention strategy. iPolitics [Internet]. https://ipolitics.ca/2015/06/19/quebec-cuts-suicide-rates-despite-lack-of-a-national-prevention-strategy/. Accessed 29 Aug 2019.
Vasiliadis H-M, Lesage A, Latimer E, Seguin M. Implementing suicide prevention programs: costs and potential life years saved in Canada. J Ment Health Policy Econ. 2015;18:147–55.
Statistics Canada. Population by year, by province and territory (CANSIM table 051-0001) [Internet]. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo02a-eng.htm. Accessed 22 June 2019.
Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K, Bulloch AG. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can J Psychiatry. 2015;60:23–30.
Pil L, Pauwels K, Muijzers E, Portzky G, Annemans L. Cost-effectiveness of a helpline for suicide-prevention. J Telemed Telecare. 2013;19:273–81.
Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS One. 2014;9:e89944.
Finkelstein Y, Macdonald EM, Hollands S, Sivilotti ML, Hutson JR, Mamdani MM, et al. Risk of suicide following deliberate self-poisoning. JAMA Psychiatry. 2015;72:570–5.
Statistics Canada. Elements of the life table, Canada, provinces and territories (CANSIM Table 053-0003) [Internet]. http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=530003. Accessed 22 June 2019.
Fleurence RL, Hollenbeak CS. Rates and probabilities in economic modelling: transformation, translation and appropriate application. PharmacoEconomics. 2007;25:3–6.
Hawton K, Witt KG, Salisbury TLT, Arensman E, Gunnell D, Hazell P, et al. Psychosocial interventions following self-harm in adults: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:740–50.
MHASEF Research Team. Mental health and addictions system performance in Ontario: a baseline scorecard. Toronto: Institute for Clinical Evaluative Sciences; 2018.
Speechley M, Stavraky KM. The adequacy of suicide statistics for use in epidemiology and public health. Can J Public Health Rev Can Sante Publique. 1991;82:38–42.
Van den Hout W. The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis. 2010;69:i89–91.
Canadian Institute for Health Information. National Health Expenditure Trends|CIHI [Internet]. 2018. https://www.cihi.ca/en/national-health-expenditure-trends. Accessed 22 June 2019.
Statistics Canada. Average weekly earnings (including overtime), by province and territory [Internet]. 2017. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/labr79-eng.htm. Accessed 22 June 2019.
Tanuseputro P, Wodchis WP, Fowler R, Walker P, Bai YQ, Bronskill SE, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLoS One. 2015;10:e0121759.
Statistics Canada. Labour Force Survey estimates (LFS), by provinces, territories and economic regions based on 2011 Census boundaries [Internet]. http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=2820123&&pattern=&stByVal=1&p1=1&p2=37&tabMode=dataTable&csid=. Accessed 22 June 2019.
Krol M, Papenburg J, Tan SS, Brouwer W, Hakkaart L. A noticeable difference? Productivity costs related to paid and unpaid work in economic evaluations on expensive drugs. Eur J Health Econ. 2016;17:391–402.
Organisation for Economic Co-operation and Development. Purchasing Power Parity [Internet]. 2018. https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm. Accessed 22 June 2019.
Statistics Canada. Consumer Price Index, health and personal care, by province (Canada) [Internet]. 2018. https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1810000501#timeframe. Accessed 22 June 2019.
Fleishman JA. Demographic and clinical variations in health status [Internet]. Agency for healthcare research and quality. 2005. https://meps.ahrq.gov/data_files/publications/mr15/mr15.shtml. Accessed 22 June 2019.
van Spijker BA, van Straten A, Kerkhof AJ, Hoeymans N, Smit F. Disability weights for suicidal thoughts and non-fatal suicide attempts. J Affect Disord. 2011;134:341–7.
Mathers C, Vos T, Stevenson C. The burden of disease and injury in Australia. Canberra: Australian Institute of Health and Welfare; 1999.
Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies, 4th ed. Canada, Ottawa. 2017.
Manchanda R, Legood R, Burnell M, McGuire A, Raikou M, Loggenberg K, et al. Cost-effectiveness of population screening for BRCA mutations in Ashkenazi jewish women compared with family history-based testing. JNCI J Natl Cancer Inst. 2015;107:dju380.
Marra CA, Esdaile JM, Anis AH. Practical pharmacogenetics: the cost effectiveness of screening for thiopurine s-methyltransferase polymorphisms in patients with rheumatological conditions treated with azathioprine. J Rheumatol. 2002;29:2507–12.
You JH, Tam L, Lee NL. Cost-effectiveness of molecular point-of-care testing for influenza viruses in elderly patients at ambulatory care setting. PLoS One. 2017;12:e0182091.
International Society for Pharmacoeconomics and Outcomes Research. Pharmacoeconomic guidelines around the world [Internet]. 2017. https://tools.ispor.org/peguidelines/. Accessed 29 Aug 2019.
Gray A, Clarke P, Wolstenholme J, Wordsworth S. Applied methods of cost-effectiveness analysis in healthcare. Oxford: Oxford University Press; 2010.
Singh SM, Micieli A, Wijeysundera HC. An economic evaluation of percutaneous left atrial appendage occlusion: dabigatran and warfarin for stroke prevention in patients with non-valvular atrial fibrillation. Circulation. 2013;127:2414–23.
Abdel-Qadir H, Roifman I, Wijeysundera HC. Cost-effectiveness of clopidogrel, prasugrel and ticagrelor for dual antiplatelet therapy after acute coronary syndrome: a decision-analytic model. CMAJ Open. 2015;3:E438.
Butt T, Patel PJ, Tufail A, Rubin GS. Modelling cost effectiveness in neovascular age-related macular degeneration: the impact of using contrast sensitivity vs. visual acuity. Appl Health Econ Health Policy. 2014;12:289–97.
Yang NH, Dharmar M, Yoo B-K, Leigh JP, Kuppermann N, Romano PS, et al. Economic evaluation of pediatric telemedicine consultations to rural emergency departments. Med Decis Making. 2015;35:773–83.
Munzer A. Probabilistic Sensitivity Analysis (PSA) on values that change by cycle [Internet]. 2014. http://treeage.zendesk.com/hc/en-us/articles/222718208-Probabilistic-Sensitivity-Analysis-PSA-on-values-that-change-by-cycle. Accessed 22 June 2019.
TreeAge Software Inc. TreeAge Pro [Internet]. Williamstown, Massachusetts, USA. 2016. https://www.treeage.com/. Accessed 22 June 2019.
Whitmer DA, Woods DL. Analysis of the cost effectiveness of a suicide barrier on the Golden Gate Bridge. Crisis. 2013;34:98–106.
Mihalopoulos C, Vos T, Pirkis J, Carter R. The economic analysis of prevention in mental health programs. Annu Rev Clin Psychol. 2011;7:169–201.
Park A-L, Gysin-Maillart A, Müller TJ, Exadaktylos A, Michel K. Cost-effectiveness of a brief structured intervention program aimed at preventing repeat suicide attempts among those who previously attempted suicide: a secondary analysis of the ASSIP randomized clinical trial. JAMA Netw Open. 2018;1:e183680.
Denchev P, Pearson JL, Allen MH, Claassen CA, Currier GW, Zatzick DF, et al. Modeling the cost-effectiveness of interventions to reduce suicide risk among hospital emergency department patients. Psychiatr Serv. 2017;69:23–31.
Kapur N, Cooper J, O’Connor RC, Hawton K. Non-suicidal self-injury vs attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry. 2013;202:326–8.
Author information
Authors and Affiliations
Contributions
JC and ML are dual first authors for this article. JC and ML conceived the study, undertook the analysis, and wrote the manuscript. All authors assisted with the interpretation of the results and critically reviewed the manuscript.
Corresponding authors
Ethics declarations
Funding
The research presented in this article was not funded by any study-specific Grant funding. Michael Lebenbaum is funded by a Vanier Canada Graduate Scholarship.
Conflict of interest
Joyce Cheng, Michael Lebenbaum, Claire de Oliveira, Paul Kurdyak, Juveria Zaheer, and Peter C. Coyte have no conflicts of interests to declare. Rebecca Hancock-Howard was previously employed as a consultant at Amaris, a private firm; clients include pharmaceutical companies and medical device manufacturers.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lebenbaum, M., Cheng, J., de Oliveira, C. et al. Evaluating the Cost Effectiveness of a Suicide Prevention Campaign Implemented in Ontario, Canada. Appl Health Econ Health Policy 18, 189–201 (2020). https://doi.org/10.1007/s40258-019-00511-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-019-00511-5