Abstract
Objectives
To analyse the cost effectiveness of community-based case management for patients suffering from chronic obstructive pulmonary disease (COPD).
Methods
The study took place in the third largest municipality in Denmark and was conducted as a randomised controlled trial with 12 months of follow-up. A total of 150 patients with COPD were randomised into two groups receiving usual care and case management in addition to usual care. Case management included among other things self care proficiency, medicine compliance, and care coordination. Outcome measure for the analysis was the incremental cost-effectiveness ratio (ICER) as cost per quality-adjusted life year (QALY) from the perspective of the healthcare sector. Costs were valued in British Pounds (£) at price level 2016. Scenario analyses and probabilistic sensitivity analyses were conducted in order to assess uncertainty of the ICER estimate.
Results
The intervention resulted in a QALY improvement of 0.0146 (95% CI −0.0216; 0.0585), and a cost increase of £494 (95% CI −1778; 2766) per patient. No statistically significant difference was observed either in costs or effects. The ICER was £33,865 per QALY gained. Scenario analyses confirmed the robustness of the result and revealed slightly lower ICERs of £28,100–£31,340 per QALY.
Conclusions
Analysis revealed that case management led to a positive incremental QALY, but were more costly than usual care. The highly uncertain ICER somewhat exceeds for instance the threshold value used by the National Institute of Health and Care Excellence (NICE). No formally established Danish threshold value exists.
ClinicalTrials.gov Identifier: NCT01512836.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The results reveal that providing case management for patients suffering from COPD leads to a small gain in QALY but at an additional cost when compared to usual care. | |
The cost per QALY exceeds the cost-effectiveness threshold value set by NICE. | |
The question of cost effectiveness of case management for COPD patients depends on decisions-makers’ valuation of a QALY for this patient group. |
1 Introduction
The growing number of patients suffering from chronic obstructive pulmonary disease (COPD) calls for effective and cost-effective care management strategies. Case management, i.e. a form of integrated care where “the patient is navigated through a complex health-related process by an individual case manager or a small case management team” [1], is believed to be an efficient method to manage patients with chronic and/or complex healthcare needs [2], e.g. patients with COPD. Despite evidence showing that case management can lead to significant health benefits in COPD [3–11], the associated costs of providing case management is less well established. In order to provide decision-makers with evidence on whether the resources currently being invested in this area represent an efficient use of scarce public resources, the net costs of providing case management needs to be measured in relation to its relevant health effect.
This paper reports the methods and results of a cost-effectiveness analysis conducted alongside a randomised controlled trial (RCT) of community-based case management, focusing on support for self-care, medicine compliance, and care coordination for patients with COPD within the context of the Danish National Healthcare sector. We hypothesised that the intervention led to a reduction in hospital admissions and improved health-related quality of life while potentially being cost saving—mainly due to a decrease in inpatient hospital costs. The objective of this article is the reporting of the results of the economic analysis from this RCT. A detailed description of the study design can be found elsewhere [1].
2 Methods
2.1 Study Design
Power analysis was based on a clinical outcome measure (rate of COPD hospitalisations) and resulted in a required sample size of approximately 75 participants in each group when including an expected loss to follow-up of 20% [1]. Clinical results will be published in another paper. Patients with COPD were recruited from Aalborg municipality—the third largest municipality in Denmark. Patients were eligible for study participation if they had been referred by their general practitioner or respiratory specialist to pulmonary rehabilitation at Aalborg rehabilitation centre during 2011. Based on random, permuted blocks of five to ensure approximate balance over time, the participants were randomised to the case management intervention or to usual care and were followed for 12 months. All participants continued to be managed by their regular healthcare providers and had access to their usual healthcare services and medications. As caseloads of approximately 70 COPD patients per case manager have been recommended [12], only one case manager was affiliated with the study. The intervention group received case management by a dedicated COPD nurse with more than 20 years of experience. She had previously worked at both in- and outpatient pulmonary hospital clinics and had most recently worked as a community-based COPD rehabilitation nurse. Prior to trial initiation, the case manager completed a health promotion coaching course focusing on motivational dialogue.
Table 1 describes the components of the intervention. Intensity and focus of the intervention was based on individual participant needs and hence not homogenous. The case manager was not to have any direct role in disease treatment, and was not to take over the function and responsibility of other healthcare providers. All healthcare providers caring for each participant were informed about the case manager’s role and existence. The RCTs were pre-registered at clinicaltrial.gov (ClinicalTrials.gov Identifier: NCT01512836).
2.2 Outcome Measure and Data Collection
The trial was analyzed as a standard cost-utility analysis, where the incremental cost-effectiveness ratio (ICER) was calculated as the cost per quality-adjusted life year (QALY). The outcome was measured at the individual level and data were gathered alongside the trial. The perspective of the study was that of the healthcare sector, hence, all costs to healthcare providers involved in treating, caring for, and monitoring the participants were accounted for. Costs incurred by the participants and their caregivers were not included in the analysis due to the healthcare sector perspective chosen. All costs were calculated in 2014 Danish Kroner (DDK) by use of the consumer price index, but were converted to Pound Sterling (£) by using an exchange rate of 9.67 DKK = 1 £, as per 9 March 2016. As in accordance with the RCT, the time horizon of the analysis was 12 months, hence no discounting was carried out.
2.2.1 QALYs
The generic questionnaire EuroQol 5-dimensions 3-level (EQ-5D-3L) was applied to obtain a measure of health-related quality of life (HRQoL), and the questionnaire was administered at baseline and after 12 months. Responses from the questionnaire were converted into the EQ-5D-3L index score using Danish societal weights [13]. Participants dying during the follow-up period received an EQ-5D-3L index score equal to the health state for death. The number of QALYs for each participant was calculated by summing the days of participation weighted by the EQ-5D-3L index score using linear interpolation.
2.2.2 Costs
The analysis included the following costs: direct disease-related costs in the primary healthcare sector (general practitioner contacts), the secondary healthcare sector (in- and outpatient hospital treatment), cost for community care (home nurse care, practical in-home assistance, household cleaning, training, stay at nursing home), costs for prescription medication, and intervention costs (case manager salary, costs for coaching course, and mileage costs, etc.). Only costs related to COPD were included in the analysis. However, for primary healthcare and community care it was not possible to distinguish between disease-specific costs and costs in general, and all costs concerning each participant were therefore included.
Data on study participants were extracted by the patients’ 10-digit registration number in various registers. The regional register of North Denmark was used to obtain data in the primary and secondary healthcare sector and sales of prescription medicine. Primary healthcare service use is registered on the date the service was received, type of service, and the reimbursement fee paid by the National Health Insurance to the healthcare provider. GPs are paid by a mixture of capitation and fee for service and both were included in the analysis. Use of secondary healthcare was classified in accordance with the Danish diagnosis-related grouping (DRG) system and Danish ambulatory grouping system (DAGS), where charges reflect the average costs for treating patients with similar conditions and processes at Danish hospitals [14] providing the relevant services. Data on number of admissions, length of stay, number of outpatient visits, and emergency room visits and their associated DRG/DAGS charge were extracted.
Data on use of prescription medicine were based on information from the dispensing pharmacies and contained information on the date the medicine was retrieved, package identifier and number of packages issued. In accordance with the perspective of the analysis, the costs for prescription medicine only covered the reimbursement fees paid by the National Health Insurance and the local health authorities, and not the out-of-pocket expenses paid by the participants.
Data on use of community care were collected from the local health authority of Aalborg municipality. Data were registered as hours of received care and each care parameter was combined with a unit cost to obtain a cost per participant. National wage rates were used to estimate the cost for home nurse care, home assistance and household cleaning [15, 16]. The local health authority provided a mean unit cost per hour for training, and an average cost for nursing-home care in Danish municipalities was used [17].
As for intervention costs, the efficient hourly wage rate for the case manager was estimated based on actual gross salary and under the assumption of 1500 efficient work-hours per year. Total kilometres of driving to and from participant homes were collected for the intervention group as a whole and divided by the number of intervention participants. Kilometres per participant was added a unit cost according to the reimbursement rate in municipalities. The coaching course was depreciated over a 5-year period at a 3% interest. An overhead cost due to rent, heating and lighting expenses of the case manager’s office throughout the study period was included in the intervention costs. Trial protocol driven costs were not included in the analysis. Table 2 lists the applied unit costs.
2.2.3 Other
A questionnaire covering demographic, disease-specific, and psychosocial topics was administered to the participants at baseline and at follow-up, as individual participant characteristics may influence on the outcome of the intervention.
2.3 Statistical Analysis
Data were analyzed according to the principle of intention to treat. Baseline charateristics were analyzed using Student’s t test for normally distributed continous data, Mann–Whitney U test for non-normally distributed data, and Pearson’s χ 2 test for categorical data. Data on HRQoL and costs were presented as mean ± SD, despite not being normally distributed, as the mean is the measure being used in cost-utility analysis (CUA). All baseline variables were presented with the associated p value, with a significance level set at p < 0.05. Missing data were present in 2–4% of the cases. Assuming data were missing at random (MAR), the method of multiple imputation was used according to guidelines [18, 19]. An exposition of the imputation model used can be found as supplemental material.
2.4 Regression Analysis of QALYs and Costs
The cost-utility of case management was assessed by calculating a point estimate of the ICER after 12 months’ follow-up. When calculating the ICER, the difference in arithmetic mean costs between the case management intervention and usual care is divided by the arithmetic mean effects between the same two interventions [20]. Regression analysis was applied to assess the incremental estimates of QALYs and costs. A seemingly unrelated regression model (SUR) was chosen as it took into account the high correlation between error terms for QALYs and costs [21]. Baseline covariates were applied to the regression model in order to improve precision and to adjust for treatment group imbalances. QALYs were adjusted for baseline HRQoL as a patient’s baseline utility is likely to be highly correlated with HRQoL at follow-up. Failure to do so may bias the QALY estimates in case of imbalance in baseline HRQoL scores [22]. Potential cost differences between the two groups at baseline were accounted for by adjusting the cost outcome for baseline total cost [23]. Furthermore, both outcomes were adjusted for the following baseline covariates: gender, forced expiratory volume in 1 s (FEV1), number of comorbidities, presence of cancer and whether or not the participants were living alone. Gender was chosen as a covariate, as female gender has been associated with lower HRQoL scores and a greater utilization of healthcare services [24, 25]. In addition, low FEV1, comorbidities and presence of cancer have been found to influence negatively on HRQoL and most likely will result in increased healthcare resource use [26, 27]. Co-habitation status was added as a covariate as living alone increases mortality, risk of depression, and admission to hospital in patients with COPD, and thereby potentially affecting both the QALY and cost estimate [28–30]. The CUA was analyzed and presented according to best practice for cost-effectiveness analysis alongside clinical trials [31, 32].
2.5 Assessment of Uncertainty
The uncertainty surrounding the point estimates of mean QALYs and costs were assessed by use of two scenario analyses. Both scenario analyses were conducted by use of SUR modelling of QALYs and costs and adjusted for the same baseline covariates as the primary analysis. The first scenario analysis was conducted in order to test the effect of mortality on the cost-effectiveness result, as it was considered questionable that death was related to treatment allocation. Therefore, all deceased participants were removed from the imputed dataset. The second scenario analysis consisted of a complete case analysis and was conducted in order to assess the impact of the multiple imputation model on the estimate of incremental QALYs and costs.
In order to test robustness of the cost-effectiveness results, probabilistic sensitivity analysis (PSA) was performed on the primary analysis and both scenarios by drawing 10,000 trial simulations. PSA captures the uncertainty in all parameters jointly and enables the reader of the analyses to get an understanding of the impact different uncertainties can have on the probability of case management being cost-effective at a given cost-effectiveness threshold [20]. The variance–covariance matrices from the SUR models were extracted and Cholesky’s decomposition was applied to obtain correlated draws. Cost-effectiveness acceptability curves were performed for all scenarios to assess the probability of case management being cost effective at different cost-effectiveness thresholds for a gain in QALYs. As according to recommendations from the National Institute of Health and Care Excellence (NICE), the results of the PSA were presented at political cost-effectiveness thresholds of £20,000–£30,000 [33].
3 Results
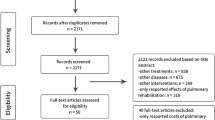
Participants: Figure 1 shows the flow diagram of the progress through the phases of the RCT. A participation rate of 63% was obtained in the study. In total, 74 participants were randomised to usual care, whereas 76 participants were randomised to the case management intervention. Six participants died during the study period. Of these, two died shortly after randomisation and before receiving any case management. To enhance the precision of the CUA estimate, the two participants were excluded from further analysis according to guideline on post-randomisation exclusion [34], as their deaths were assumed not to have been inflicted by the intervention. Common for the remaining four deceased participants was that they suffered from at least two other comorbidities besides their diagnosis of COPD. Another five participants were lost to follow-up during the study period.
Flowchart of participants. The figure illustrates the course of participants throughout the study. Two participants assigned to the case-management intervention unexpectantly died shortly following randomisation and before they had received any case management. The two participants were excluded from further analysis as according to guideline [34]. The remaining participants were analysed according to the intention-to-treat principle. The figure is reproduced from a previously published paper with permission from the copyright holder [1]
Non-imputed baseline characteristics are listed in Table 3. No significant differences were seen between the two groups. However, differences were seen for the distribution of gender, employment status, comorbidities, EQ-5D-3L index scores and costs. The baseline variables with missing data had no more than 2% missing.
Intervention intensity: Originally, the case manager was to provide follow-up phone calls every month as well as an in-person meeting every 3 months. However, it turned out that some participants had good self-care and did not need to be monitored so closely, whereas others needed much more intense follow-up to manage their health issues. Therefore, follow-up was arranged as needed, but still with an in-person meeting at least every 3 months. As can be seen in Table 4, the participants received on average 6.46 case-manager contacts during the follow-up period, of which the majority were face-to-face meetings. In contrast, the case manager had on average 0.16 contacts per participant to other healthcare providers regarding coordination of care, which was quite a bit lower than anticipated.
Outcomes and costs: Data on EQ-5D-3L index scores were complete at baseline but had 4% missing values at follow-up. There were no problems with missing data on costs as they were drawn from personally identifiable registers. As listed in Table 4, the case management intervention resulted in a mean unadjusted significant increase in HRQoL of 0.08 [95% confidence interval (CI) 0.05;0.09], but had an additional mean unadjusted significant rise in total costs of £1005 (95% CI 385.75; 1624.20).
3.1 Cost Effectiveness
3.1.1 Primary Analysis
When regression adjusting for baseline imbalances in the primary analysis, case management resulted in a non-significant increase in mean total costs as well as a non-significant rise in QALYs, see Table 5. The adjusted incremental mean total cost of case management per participant was £494 (95% CI −1778; 2766) over the 12 months of follow-up, which were mainly due to intervention costs. The adjusted regression of QALY revealed that case management participants had an average rise of 0.0146 QALYs (95% CI −0.0216; 0.0585) more per participant than usual care participants, leading to an ICER of £33,865 per QALY gained. The PSA revealed that case management was a cost-effective strategy in only 43% of the simulations at a cost-effectiveness threshold of £20,000, whereas case management was cost effective in 49% of the simulations at a threshold of £30,000, as demonstrated in Fig. 2.
Incremental cost-effectiveness scatterplot (left) and cost-effectiveness acceptability curve (right) for the primary analysis. The figure on the left illustrates the cost-effectiveness scatterplot with 10,000 simulations of incremental costs and QALYs of the case-management intervention as compared to usual care for the primary analysis. The cost-effectiveness threshold of £20,000 is illustrated by the black line running through (0.0) in the scatterplot. Forty-three percent of the simulations fall under the threshold line, indicating that case management is a cost-effective strategy compared to usual care in 43% of the simulations. The simulations fall in all four quadrants indicating the uncertainty surrounding the ICER estimate. The figure on the right illustrates the probability of the case management intervention being cost effective at different cost-effectiveness thresholds as compared to usual care. QALY quality-adjusted life year
3.1.2 Scenario Analyses
Excluding all participants who died during the study period resulted in anadjusted incremental mean non-significant cost of £832 (95% CI −1425; 3090).The adjusted incremental mean QALYs rose to 0.0296 (95% CI 0.0004; 0.0580) and the difference was significant. The rise in QALY in the case management group was higher than in the primary analysis, as three out of the four participants, who died during follow-up, were allocated to the case management group. However, the adjusted incremental mean cost for the case management group rose simultaneously, resulting in an ICER of £28,100 per QALY gained. The PSA revealed the case management intervention to be cost-effective in 42–51% of the simulations at cost-effectiveness thresholds of £20,000–£30,000/QALY, respectively.
Complete case analysis revealed a moderate increase in both incremental mean total costs and incremental mean QALYs compared to the primary analysis. The adjusted incremental mean cost of case management per participant was £664 (95% CI −1700; 3028), whereas the adjusted mean incremental QALY was 0.0212 (95% CI −0.0126; 0.0550). Both differences were non-significant. The ICER was £31,340 with a 41–48% chance of being cost effective at thresholds of £20,000–£30,000/QALY.
4 Discussion
This pragmatic RCT compared the costs and health effects of community-based case management for patients suffering from COPD with usual care in Denmark. Our results showed that when correcting for baseline scores, community-based case management for COPD led to improvements in QALY but with a concurrent rise in costs. The differences, however, were not significant at conventional significance levels, 5%. With an ICER of £33,865 per QALY gained and a probability of being a cost-effective strategy in 43–47% of the simulations at a threshold of £20,000–30,000 per QALY gained, the intervention appears more unlikely than likely to be cost-effective under the given assumptions.
An analysis adjusting only for baseline HRQOL and baseline cost was conducted; however, it did not change the conclusion of cost effectiveness (see supplementary material). The scenario analyses were consistent with the findings in the primary analysis. Exclusion of deceased participants in both groups only affected the cost per QALY moderately and led to an ICER of £28,100 per QALY gained. In line with the primary analysis and the analysis excluding all deceased participants, the complete case analysis revealed an ICER of £31,340, which might be attributable to the low rate of participants discontinuing their participation.
In the primary analysis, the difference in QALY was not significant, and thus it cannot be distinguished statistically, whether the intervention is more effective than usual care. The study was not powered to detect a significant difference in QALY, but the case-managed group did, however, obtain a rise in QALY compared to usual care. It is up to decision makers to determine if this difference is of clinical importance. Whether the intervention offers sufficient value for money to warrant resources being allocated to it depends on decision-makers’ valuation of a QALY for COPD patients. No political threshold values for a QALY have yet been established in Denmark, and decision of cost effectiveness is therefore case dependent, if considered at all. In England, however, NICE has set a threshold of £20,000–30,000 per QALY gained. In light of NICEs threshold the cost-effectiveness estimate of case management for COPD was borderline, and the uncertainty around the ICER estimate was substantial. Previously, healthcare interventions with comparable and significantly higher ICERs have been financed in Denmark [35], indicating that the ratio found in the current study could be considered acceptable for financing. Whether a healthcare service should be financed or not depends on various factors, such as budget constraints, necessity of care, moral values, patient responsibility, etc. [36]. However, as revealed in the sensitivity analysis, this requires that decision makers are willing to accept a high degree of uncertainty regarding the cost effectiveness of the intervention.
The study followed the intention-to-treat principle; however, as noted above two participants were excluded from analysis since they never received the intervention. It should be noted that inclusion of these two participants would have led to a considerably higher cost per QALY, albeit that estimate of cost effectiveness is believed highly erroneous by the authors for the reason indicated earlier.
The use of QALY for the outcome measure of the study is a strength—assuming that EQ-5D is also suitable for rehabilitative treatment strategies—as it provides a common measure for assessing the extent of the benefits gained from a variety of interventions in terms of quantity and quality of life. When combined with the costs associated with the interventions, this information can help inform decision makers in allocating resources within and across therapy areas. Evidence of validity and reliability supports the use of EQ-5D-3L in obtaining HRQoL scores for COPD patients [37], and the obtained estimates of HRQoL are believed representative of the patient group. Since HRQoL estimates have been gathered at baseline and after 12 months only, it is not clear how the participants’ HRQoL fluctuated within that time period. Additionally, this study only includes the costs and effects in the 12-month period where the case-manager was employed and had contact with the participants. It cannot be ruled out that the QALY outcome needs a longer follow-up period in order to reveal the ‘stable effect’ of case management. In such situations economic modelling is often employed to simulate long-term outcomes. Economic modelling has not been performed; however, the authors plan to evaluate the long-term outcomes in the future. Access to the Danish registries provides the opportunity to follow each participant’s use of healthcare services beyond the 12 months of follow-up, which could be supplemented with a EQ-5D-3L questionnaire. An important strength of the study was the high degree of data completeness. Throughout the study period special attention was paid to missing data, and this, together with the low drop-out rate, led to nearly complete data. Especially the Danish registries have a high degree of completeness and validity, which adds precision to the cost-effectiveness estimate.
The intervention was pre-defined to include both support for self-care and care coordination; however, registrations show that the case manager mainly interacted with the participants and only to a limited degree cooperated with other healthcare providers regarding coordination of care. Previous research has shown that coordination across health professions can be a challenging task when conducting case management, in particular due to difficulties of acknowledgement and becoming integrated in daily practice [38, 39]. The causes and potential consequences of the limited involvement with other healthcare providers will prospectively be evaluated by use of interviews with the case manager obtained during and following study completion. The case manager was appointed due to her dedication and experience as a COPD nurse, and it cannot be rejected that the obtained differences in QALYs are influenced by her skills and motivation. If the service is implemented, in practice the level of education, experience and training of case managers should be emphasized. Furthermore, it should be noted that given the nature of case management, blinding of participants and the case manager was not feasible. As knowledge of group assignment might affect the behaviour of both parties involved as well as the participants’ responses to subjective outcome measures, this poses an inevitable limitation of the study design.
The total mean cost for the case management group at follow-up was higher than for the usual-care group. This was mainly attributed to intervention costs and cost differences in inpatient hospital care, with the latter of the two being unexpectantly higher for the case managed group. The difference in total mean cost may be a coincidence, but could also be related to the frequent contact between the participants and the case manager, potentially resulting in earlier detection of insufficient improvements and worsening in symptoms. Additionally, the difference might also indicate that the effects of learned self-management skills can take longer than 12 months to settle, and that potential cost savings might not reveal themselves until after a longer period of time. As for intervention costs, it should be noted that the intervention costs were not variable by participant. For example, in practice it turned out that it was not possible to obtain the number of driven kilometers per participant. Instead the total number of driven kilometers for the group as a whole was used and divided by the number of intervention participants. The lack of variability of the intervention costs poses a limitation as it underestimates the uncertainty around the cost estimates and associated ICERs.
SUR was used for the analysis of cost effectiveness due to a strong correlation between the error terms for costs and QALYs. However, the use of SUR poses a potential limitation, as this form of analysis assumes bivariate normality, which is often not the case for either costs or QALYs. Alternatively, generalised linear models (GLM) can be applied, as this analysis can take into account the right and left skewed nature of costs and QALYs, respectively. GLM analysis with different distributions was therefore applied to costs and to QALY decrements (not reported here); however SUR modelling was found to fit data best.
Of the eligible participants, 37% refused to participate, which may have an influence on the generalisability of the study. No baseline values were obtained for these participants, and it is therefore unknown to what extent the results are generalisable to the reference population. Eligible participants were recruited from one large municipality in Denmark, which might introduce bias if the COPD patients living there, and/or the organization of their care, deviated from other municipalities in Denmark. The municipality covered both urban and rural areas, and the study population contained patients with all degrees of severity of COPD due to broad inclusion criteria. This, together with the fact that COPD care in Denmark follows standardised guidelines [40], heightens generalisability, which is believed reasonable for Denmark. Generalisability of the study to other countries depends, among other things, on the healthcare systems organisational structure, the reimbursement system, COPD healthcare service costs, population characteristics and geographical circumstances [41]. It is believed that this paper, together with the published protocol for the study [1], will enable the reader to determine whether the result is transferable to their setting due to the reporting of methods and results following best practice.
Only a limited number of studies have evaluated the costs of providing case management and similar care strategies for COPD [7, 12, 42]. A study by Koff et al. [7] reported the change in HRQoL, as measured by the St George’s Respiratory Questionnaire (SGRQ), and healthcare costs for a 3-month long RCT evaluating integrated care for COPD patients. The intervention focused on disease-specific education and teaching of self-management techniques in combination with telemonitoring, and was compared to usual care. The study found that the intervention significantly improved HRQoL while at the same time being cost saving. Another RCT study by Bourbeau et al. [12], examined the cost per prevented hospitalisation of a 12-month intervention consisting of self-management education along with ongoing supervision by a case manager. Compared to usual care, the intervention resulted in an ICER of $4214 per hospitalisation prevented. Lastly, a RCT study by Hoogendoorn et al. [42] evaluated the cost effectiveness of a community-based COPD management programme over a 2-year follow-up period. The intervention mainly consisted of self-management education and focused on patients with less severe airflow obstruction than those traditionally included in such studies. The study found an ICER of €9078 per additional patient with a relevant improvement in SGRQ and €32,425 per QALY gained. Of the three studies, the study by Hoogendoorn et al. methodogically resembles our study the most, and the cost per QALY is somewhat alike. However, comparison of the studies with our study is generally difficult due to heterogeneity such as differences in setting, type of intervention, outcome measures and patient population characteristics.
In light of the presented findings, it is concluded that our intervention of case management resulted in a positive incremental QALY; however, the incremental cost rose simultaneously. The highly uncertain ICER, with a point estimate above the cost-effectiveness threshold set by NICE, makes it difficult to determine whether case management is a cost-effective alternative to usual care.
References
Storgaard Sørensen S, Møller Pedersen K, Weinreich UM, Ehlers LH. Design, and participant enrollment, of a randomized controlled trial evaluating effectiveness and cost-effectiveness of a community-based case management intervention, for patients suffering from COPD. Open Access J Clin Trials. 2015;7:53–62.
Schaefer J, Davis C. Case management and the chronic care model: a multidisciplinary role. Lippincott’s Case Manag. 2004;9:96–103.
Casas A, Troosters T, Garcia-Aymerich J, Roca J, Hernández C, Alonso A, et al. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur Respir J. 2006;28:1130–230.
Leung AC, Liu C, Chow NW, Chi I. Cost-benefit analysis of a case management project for the community-dwelling frail elderly in Hong Kong. J Appl Gerontol. 2004;23:70–85.
Bourbeau J, Julien M, Maltais F, Rouleau M, Beaupré A, Bégin R, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:585–91.
Rice KL, Dewan N, Bloomfield HE, Grill J, Schult TM, Nelson DB, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182:890–6.
Koff PB, Jones RH, Cashman JM, Voelkel NF, Vandivier RW. Proactive integrated care improves quality of life in patients with COPD. Eur Respir J. 2009;33:1031–8.
Moullec G, Lavoie KL, Rabhi K, Julien M, Favreau H, Labrecque M. Effect of an integrated care programme on re-hospitalization of patients with chronic obstructive pulmonary disease. Respirology. 2012;17:707–14.
Bird S, Noronha M, Sinnott H. An integrated care facilitation model improves quality of life and reduces use of hospital resources by patients with chronic obstructive pulmonary disease and chronic heart failure. Aust J Prim Health. 2010;16:326–33.
Poole PJ, Chase B, Frankel A, Black PN. Case management may reduce length of hospital stay in patients with recurrent admissions for chronic obstructive pulmonary disease. Respirology. 2001;6:37–42.
Efraimsson EO, Hillervik C, Ehrenberg A. Effects of COPD self-care management education at a nurse-led primary health care clinic. Scand J Caring Sci. 2008;22:178–85.
Bourbeau J, Collet J-P, Schwartzman K, Ducruet T, Nault D, Bradley C. Economic benefits of self-management education in COPD. Chest. 2006;130:1704–11.
Wittrup-Jensen KU, Lauridsen J, Gudex C, Pedersen KM. Generation of a Danish TTO value set for EQ-5D health states. Scand J Public Health. 2009;37:459–66.
Danish Ministry of Health. Takstsystem 2015—vejledning (in Danish) [Internet]. http://www.ssi.dk/~/media/Indhold/DK-dansk/Sundhedsdataogit/NSF/Sundhedsokonomiogfinansiering/Sundhedokonomi/Takster/Takster2015/Takstvejledning2015.ashx. Accessed 7 June 2015.
Danish Nursing Council. Løn-og ansættelsesvejledning (in Danish) [Internet]. 2013. p. 1–40. http://www.dsr.dk/Lederforeningen/Din-løn/Documents/14-90_lønvejledning_A4_low.pdf. Accessed 7 June 2015.
FOA. Lønmagasin (in Danish) [Internet]. Copenhagen; 2015. p. 1–27. http://www.e-pages.dk/foa/463/. Accessed 7 June 2015.
Ministry of Finance. Frit valg og kvalitet—afregningsmodeller på de kommunale serviceområder (in Danish) [Internet]. Albertslund; 2003. p. 186. http://www.fm.dk/publikationer/2003/frit-valg-og-kvalitet. Accessed 7 June 2015.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99.
Manly CA, Wells RS. Reporting the use of multiple imputation for missing data in higher education research. Res High Educ [Internet] Springer Neth. 2014;56:397–409. doi:10.1007/s11162-014-9344-9.
Gray AM, Clarke PM, Wolstenholme JL, Wordsworth S. Applied methods of cost-effectiveness analysis in health care. 1st ed. New York: Oxford University Press; 2011.
Willan AR, Briggs AH, Hoch JS. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ. 2004;13:461–75.
Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–96.
Van Asselt ADI, Van Mastrigt GAPG, Dirksen CD, Arntz A, Severens JL, Kessels AGH. How to deal with cost differences at baseline. Pharmacoeconomics. 2009;27:519–28.
Katsura H, Yamada K, Wakabayashi R, Kida K. Gender-associated differences in dyspnoea and health-related quality of life in patients with chronic obstructive pulmonary disease. Respirology. 2007;12:427–32.
Redondo-Sendino A, Guallar-Castillón P, Banegas JR, Rodríguez-Artalejo F. Gender differences in the utilization of health-care services among the older adult population of Spain. BMC Public Health. 2006;6:155.
Jones PW, Brusselle G, Dal Negro RW, Ferrer M, Kardos P, Levy ML, et al. Health-related quality of life in patients by COPD severity within primary care in Europe. Respir Med. 2011;105:57–66.
Tan Z, Liang Y, Liu S, Cao W, Tu H, Guo L, et al. Health-related quality of life as measured with EQ-5D among populations with and without specific chronic conditions: a population-based survey in Shaanxi Province, China. PLoS One. 2013;8:e65958.
van Manen JG, Bindels PJE, Dekker FW, Ijzermans CJ, van der Zee JS, Schadé E. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002;57:412–6.
Crockett AJ, Cranston JM, Moss JR, Alpers JH. The impact of anxiety, depression and living alone in chronic obstructive pulmonary disease. Qual Life Res. 2002;11:309–16.
Wing QBJ. Outcomes and health-related quality of life following hospitalitzation for an acute exacerbation of COPD. Respirology. 2005;10:334–40.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)—explanation and elaboration : a report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Heal. 2013;16:231–50.
Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials : the ISPOR RCT-CEA task force report. Value Health. 2005;8:521–33.
National Institute of Clinical Excellence. Methods for the development of NICE public health guidance (third edition) [Internet]. 2012. p. 1–286. https://www.nice.org.uk/article/pmg4/resources/non-guidance-methods-for-the-development-of-nice-public-health-guidance-third-edition-pdf. Accessed 7 June 2015.
Fergusson D, Aaron SD, Guyatt G, Hébert P. Post-randomisation exclusions: the intention to treat principle and excluding patients from analysis. BMJ. 2002;325:652–4.
Barzey V, Atkins MB, Garrison LP, Asukai Y, Kotapati S, Penrod JR. Ipilimumab in 2nd line treatment of patients with advanced melanoma: a cost-effectiveness analysis. J Med Econ. 2013;16:202–12.
Culyer AJ. Cost-effectiveness thresholds in health care: a bookshelf guide to their meaning and use [Internet]. 2015. Report No.: 121. http://www.york.ac.uk/media/che/documents/papers/researchpapers/CHERP121_Cost-Effectiveness_thresholds_Health_Care.pdf.
Simon Pickard A, Wilke C, Jung E, Patel S, Stavem K, Lee TA. Use of a preference-based measure of health (EQ-5D) in COPD and asthma. Respir Med. 2008;102:519–36.
Ellen Netting F, Williams FG. Case manager-physician collaboration: implications for professional identity, roles, and relationships. Health Soc Work. 1996;21:216–24.
Bourbeau J, Van Der Palen J. Promoting effective self-management programmes to improve COPD. Eur Respir J. 2009;33:461–3.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [Internet]. p. 117. http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Feb18.pdf. Accessed 17 Aug 2015.
Welte R, Feenstra T, Jager H, Leidl R. A decision chart for assessing and improving the transferability of economic evaluation results between countries. Pharmacoeconomics. 2004;22:857–76.
Hoogendoorn M, Van Wetering CR, Schols AM, Rutten-van Mölken MPMH. Is INTERdisciplinary COMmunity-based COPD management (INTERCOM) cost-effective? Eur Respir J. 2010;35:79–87.
Danish Regions and Danish Medical Association. Overenskomst om almen praksis (in Danish) [Internet]. 2014. p. 99. http://www.laeger.dk/portal/pls/portal/!PORTAL.wwpob_page.show?_docname=10623107.PDF. Accessed 20 Aug 2015.
Statens Seruminstitut. DRG takster (in Danish) [Internet]. 2015. http://www.ssi.dk/Sundhedsdataogit/Sundhedsokonomiog-finansiering/SundhedsoekonomiogDRG/DRG-takster.aspx. Accessed 20 Aug 2015.
SKAT. Kørselsgodtgørelse—skattepligtig og skattefri (in Danish) [Internet]. 2014. https://www.skat.dk/SKAT.aspx?oId=2064181. Accessed 20 Aug 2015.
Acknowledgements
The authors would like to thank Thomas Mulvad from The North Denmark Region, Denmark, and Tommi Vorbeck Nielsen from Aalborg Municipality, Denmark, for their cooperation in extraction of register data used in the study.
Author contributions
SSS conceived the study design; acquired the data; performed the analyses and interpretation of data; and drafted the manuscript for publication. KMP, UMW and LE contributed to the study design and interpretation of the results, and reviewed and recommended revisions to the submitted manuscript to ensure accuracy. All authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the RCT were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors Sabrina Storgaard Sørensen, Kjeld Møller Pedersen, Ulla Møller Weinreich and Lars Ehlers declare that they have no conflict of interest.
Funding
The research project received support from The North Denmark Region, Denmark. The sponsors of the study had no role in data analysis, data interpretation, or writing of the paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sørensen, S.S., Pedersen, K.M., Weinreich, U.M. et al. Economic Evaluation of Community-Based Case Management of Patients Suffering From Chronic Obstructive Pulmonary Disease. Appl Health Econ Health Policy 15, 413–424 (2017). https://doi.org/10.1007/s40258-016-0298-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-016-0298-2