Abstract
Background
Hospital outpatient orthopaedic services traditionally rely on medical specialists to assess all new patients to determine appropriate care. This has resulted in significant delays in service provision. In response, Orthopaedic Physiotherapy Screening Clinics and Multidisciplinary Services (OPSC) have been introduced to assess and co-ordinate care for semi- and non-urgent patients.
Objectives
To compare the efficiency of delivering increased semi- and non-urgent orthopaedic outpatient services through: (1) additional OPSC services; (2) additional traditional orthopaedic medical services with added surgical resources (TOMS + Surg); or (3) additional TOMS without added surgical resources (TOMS − Surg).
Methods
A cost-utility analysis using discrete event simulation (DES) with dynamic queuing (DQ) was used to predict the cost effectiveness, throughput, queuing times, and resource utilisation, associated with introducing additional OPSC or TOMS ± Surg versus usual care.
Results
The introduction of additional OPSC or TOMS (±surgery) would be considered cost effective in Australia. However, OPSC was the most cost-effective option. Increasing the capacity of current OPSC services is an efficient way to improve patient throughput and waiting times without exceeding current surgical resources. An OPSC capacity increase of ~100 patients per month appears cost effective (A$8546 per quality-adjusted life-year) and results in a high level of OPSC utilisation (98 %).
Conclusion
Increasing OPSC capacity to manage semi- and non-urgent patients would be cost effective, improve throughput, and reduce waiting times without exceeding current surgical resources. Unlike Markov cohort modelling, microsimulation, or DES without DQ, employing DES-DQ in situations where capacity constraints predominate provides valuable additional information beyond cost effectiveness to guide resource allocation decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Economic modelling predicts that increasing OPSC capacity is an efficient use of resources compared to usual care in the example hospital. |
Increasing OPSC capacity by ~100 patients per month results in a high level of OPSC utilisation without exceeding current surgical resources in the example hospital. |
DES-DQ has the ability to capture the effect of capacity constraints on the provision of health services. Therefore, this modelling method is ideal for providing information on waiting times, throughput, resource utilisation and cost effectiveness under capacity constraints to help guide resource allocation decisions. |
1 Introduction
Hospital outpatient orthopaedic services have traditionally relied on medical specialists to assess and screen all new patients referred to the service before directing them to the most appropriate (conservative or surgical) care. This model of service delivery has resulted in significant delays in service provision [1–3]. In response, advanced practice physiotherapy-led models have been developed such as the Orthopaedic Physiotherapy Screening Clinic and Multidisciplinary Services (OPSC) in Queensland, which employ experienced musculoskeletal physiotherapists to assess and co-ordinate multidisciplinary care for semi- and non-urgent patients. In Australia, referrals to orthopaedic outpatient services are categorised as: Category 1 (urgent; target time frame 30 days, usually not appropriate for OPSC service), Category 2 (semi-urgent; target time frame 90 days), and Category 3 (non-urgent; target time frame 365 days). Typically, patients categorised as semi- and non-urgent (Category 2 or 3) are considered for referral to OPSC. Services such as OPSC have been shown to reduce waiting times and staff costs while maintaining quality of service in Canada, the UK and Australia [1, 4–7].
In traditional orthopaedic medical services (TOMS), in the hospital of interest, patients are initially assessed by an orthopaedic specialist, they may then be: directed back to their general practitioner for continuing management; referred to conservative management which could include physiotherapy or other medical management (e.g. corticosteroid injections); placed on a surgical waiting list; or continue to be monitored for the need for surgery and called back for review at a later date.
In OPSC, patients are initially screened by a physiotherapist who has postgraduate qualifications in musculoskeletal physiotherapy. Following this assessment, patients may be referred for co-ordinated multidisciplinary non-surgical management. This can include physiotherapy, occupational therapy, dietetics and psychology as well as other allied health intervention when indicated (e.g. podiatry). In addition to services tailored to individual patients, group-based programmes are used to support ongoing self-management, knowledge and skill development. Alternatively, following screening the patient may be referred back to an orthopaedic specialist. This may occur if issues are identified that indicate the need for urgent medical attention or suggest a strong need for surgical review.
Although the OPSC is operational in 14 hospital facilities in Queensland it is estimated that only a modest proportion (around 38 % in the hospital of interest; hospital data collection and expert review of OPSC suitable patients) of the total orthopaedic patient population suitable for such an intervention has access to the service. It is proposed that increasing the capacity of OPSC to manage semi- and non-urgent orthopaedic patients would be an efficient way to address unmet demand in public orthopaedic outpatients. The aim of this research is to explore the potential impact of altering the mix of OPSC and TOMS compared with usual care (UC) through economic modelling using discrete event simulation (DES) with dynamic queueing (DQ).
Unlike Markov cohort modelling, microsimulation, or DES without DQ, employing DES with DQ (DES-DQ) is ideal for modelling health services delivery where demand for services often exceeds supply and capacity constraints predominate [8]. DES-DQ allows the prediction of queuing times as a function of the demand for resources (i.e. orthopaedic patients requiring initial assessment, review or surgery) and resource availability (e.g. orthopaedic specialist to assess, review and perform surgery on patients and physiotherapists to assess, review and treat patients). Furthermore, DES with DQ has the flexibility to investigate real-world complex systems where waiting times are growing or declining during the analysis period rather than relying on assumptions of steady-state queuing times.
Using real-world data from a large public teaching hospital in Australia this research provides a practical example of how economic modelling using DES with DQ can support rational resource allocation decisions to help ameliorate capacity constraints faced in orthopaedic services. Furthermore, we anticipate the general modelling methods and analysis approach presented in this study may be applicable to other healthcare settings where capacity constraints predominate.
2 Objectives
The objective of this research was to compare the efficiency of delivering increased semi- and non-urgent orthopaedic outpatient services through providing: (1) additional OPSC; (2) additional TOMS with additional surgical resources (TOMS + Surg); or (3) additional TOMS without additional surgical resources (TOMS − Surg) in a large public teaching hospital in Australia (Logan Hospital, Metro South Health) compared with UC.
3 Methods
3.1 Research Question and Context
In the hospital of interest, UC currently consists of service provision through TOMS in combination with a smaller advanced practice physiotherapy-led OPSC. Currently, TOMS and OPSC conduct around 62 and 27 new patient assessments in the eligible patient population per month, respectively. This UC was then compared with a range of service provision alternatives, including: (1) increasing the capacity of OPSC services (without additional surgical capacity) by an additional 25–125 patients per month (OPSC); (2) increasing the capacity of TOMS (with additional surgery capacity; TOMS + Surg) by 25–125 patients per month; and (3) increasing the capacity of TOMS (without additional surgery capacity; TOMS − Surg) by 25–125 patients per month. The choice of new levels of capacity tested in the economic analysis was made in conjunction with experts in the delivery of these services to ensure that they spanned feasible changes in future resourcing and capacity. For each alternative service option, the cost effectiveness, throughput, waiting times and percentage utilisation of resources were compared with UC.
3.2 Perspective
The cost-effectiveness analysis was conducted using a healthcare payer perspective including direct healthcare costs.
3.3 Modelling Software
The economic model was developed using the Simul8© 2014 software package.
3.4 Input Data
Detailed data describing the current number of patients waiting for orthopaedic assessment and surgery, and the rate of new patient presentations, and orthopaedic medical specialist and OPSC throughput from July 2013–November 2014 was obtained from the large public teaching hospital of interest (Table 1). The number of patients who were currently undergoing orthopaedic review was not available, so it was estimated through expert opinion (MR, SO and TC). Other data were taken from a retrospective chart audit of 980 patients attending an OPSC with a primary diagnosis involving the knee (34.4 %), shoulder (37.6 %) or lumbar (28.1 %) spine as described by Comans et al. (Table 1) [9]. The chart audit captured data from seven public hospitals throughout Queensland, including the hospital of interest (i.e. Logan hospital). These retrospective data were obtained from patients who were considered to be typical and generalisable to the OPSC service at the hospital of interest. Patients with low back, knee or shoulder conditions considered to be unlikely to require surgery were the three most frequently treated conditions seen by the OPSC service. From 2012–2016 these three conditions represented around 82.9 % of all conditions treated by the service at the hospital of interest. Other conditions treated by this service included foot/ankle (6.1 %), cervical spine (4.7 %), hip (2.5 %), elbow (2.0 %), thoracic spine (1.2 %), and wrist/hand (0.6 %).
The surgical success rates applied in the economic model were taken from the literature and weighted by the proportion of surgical procedures performed for the knee, shoulder or lumbar spine recorded in the retrospective chart audit [9–14]. All costs are presented in Australian Dollars ($A1.00 ≈ US$0.76) and were applied at 2014 values. Costs and benefits were discounted at 5 % per annum as specified in pharmacoeconomic guidelines from the Pharmaceutical Benefits Advisory Committee in Australia [15].
The derivation of the preference-based health-related quality of life (utility values) applied in the economic model have been described previously [9]. In brief, utility values were calculated from data collected in the retrospective chart audit, with measurements taken at baseline and post-management using the Assessment of Quality of Life four dimensions (AQoL-4D), a generic health-related quality of life instrument [16]. These measurements were taken over approximately a 24-week period, which was considered an appropriate duration to assess the patients’ response to the interventions administered. Follow-up utility estimates were calculated for responders (i.e. those who met a clinically important difference on a low back, knee, or shoulder questionnaire) and non-responders, allowing these values to be applied appropriately to the economic model’s health states.
The model was pre-populated with simulated patients to match the prevalent population waiting for services as recorded in the large public teaching hospital data collection (e.g. patients waiting for TOMS review or orthopaedic surgery). Where these data were not available, expert opinion was used to estimate the size of these populations (i.e. patient requiring ongoing review with TOMS or OPSC). The impact of altering this assumption was tested in sensitivity analyses. The rate of newly presenting or incident patients requiring orthopaedic care was taken directly from the large public teaching hospital data collection.
Full details of the input parameters applied in the economic model, by parameter type [e.g. costs, preference-based health-related quality of life (utility), and probabilities] are presented in Table 1.
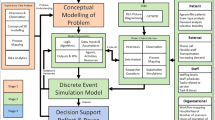
3.5 Model Structure
A conceptualised version of the structure of the DES-DQ economic model is presented in Fig. 1. Both UC and each new service provision alternative were assessed using the same model structure with modifications to throughput data used to represent changes in health service capacity.
Conceptualised structure of the DES-DQ model. DES-DQ discrete event simulation with dynamic queueing, GP general practitioner, MDS multidisciplinary service, NR non-responder, OPSC orthopaedic physiotherapy screening clinic, Q queue, RES responder, TOMS traditional service provision through orthopaedic medical specialists
3.6 Time Horizon
The time horizon applied in the economic model was set to the same duration as that used in the original economic analysis by Comans et al., and to the duration over which the introduction of the new intervention was to be assessed (i.e. 5.25 years) [9]. The time horizon of the original model was guided by clinical experts who identified the duration in which the main differences in costs and effects between treatment arms were likely to be realised. Further, a longer time frame has the potential to introduce more uncertainty in the results as the type of care may change over time. Orthopaedic treatment is primarily expected to affect patient quality of life and not life span, therefore, this time horizon was considered appropriate.
3.7 Queuing Methods
The DES-DQ model employed queues with exponential inter-arrival times, which assumes that each inter-arrival time is independent of the next. Each queue used a simple single server structure to reflect the total throughput of the health service being modelled (e.g. TOMS, OPSC). The queues used in the DES-DQ model employed a first-in, first-out (FIFO) scheduling discipline. The DES queues allowed baulking or reneging due to patient refusal to wait for treatment (i.e. drop out) or patient mortality.
3.8 Stochastic Uncertainty
Average cost, effect, incremental cost-effectiveness ratio (ICER), waiting time and throughput values were calculated as the mean of 10 model runs each using unique random number streams with approximately 23,000 simulated patients per run.
3.9 Model Validation
The DES-DQ economic model described herein was based on a previously published Markov cohort model (MM) which compared OPSC and TOMS alone [9]. The DES model and the MM generated almost identical outcomes when the DES model was calibrated to the MM outcomes, thereby cross-validating the results using two separate modelling methods [17, 18]. The DES model was then modified to suit the single hospital of interest and to compare the efficiency of different combinations of TOMS and OPSC with UC.
3.10 Sensitivity Analyses
A series of univariate and multivariate sensitivity analyses were conducted by varying the input parameters across plausible ranges to test the model’s sensitivity to parameter uncertainty.
4 Results
Table 2 shows the ICERs generated for each service provision option when compared to UC. OPSC generates the lowest ICERs at around A$7900–A$9350 per additional quality-adjusted life-year (QALY) or less. TOMS + Surg generated higher ICERs than OPSC at around A$21,400–A$21,900 per additional QALY. TOMS − Surg generated similar ICERs to TOMS + Surg when capacity was increased up to 50 additional patients per month. When capacity was increased to 75 or 125 additional patients per month the ICER for TOMS − Surg decreased to around A$18,200 and A$13,200 per additional QALY, respectively.
Figure 2a presents the total number of initial assessments performed through OPSC or TOMS for each service provision alternative over the model period. It is estimated that around 5600 patients will be managed with UC over the modelled time horizon. As the maximum capacity of each service provision alternative is increased from 25–100 additional patients per month, the total number of patients receiving an initial assessment increased in a similar linear fashion in all analyses. When the service capacity was increased to an additional 125 patients per month the number of patients receiving an initial OPSC assessment in the OPSC service alternative declines in comparison to the TOMS alternatives, because at this point OPSC capacity begins to exceed the number of patients suitable for OPSC management.
a Patient initial assessment throughput over model period. b Patient surgical throughput over model period. Nb. Rounding has been applied. Average throughput values were calculated as the mean of 10 model runs each using unique random number streams with approximately 23,000 simulated patients per run. Asterisk indicates initial assessment by TOMS or OPSC. CI credible interval, OPSC Orthopaedic Physiotherapy Screening Clinic and Multidisciplinary Service, TOMS – Surg traditional service provision through orthopaedic medical specialists without additional surgical resources, TOMS + Surg traditional service provision through orthopaedic medical specialists with additional surgical resources
Figure 2b presents the total number of patients receiving surgery over the model period for each service provision alternative. It is estimated that around 2000 patients will receive surgery under UC over the modelled time horizon. The total number of patients predicted to receive surgery increases in a similar fashion as the maximum capacity of TOMS + Surg and TOMS − Surg is increased from 25–50 additional patients per month. When the capacity of each service provision alternative is increased to an additional 50–125 patients per month the number of patients receiving surgery plateaus in the TOMS − Surg alternative, whereas the number of patients receiving surgery in the TOMS + Surg alternative continues to rise. In all analyses, the increase in the number of patients receiving surgery is lower in the OPSC option than the TOMS + Surg option. Similarly, when the capacity of each service provision alternative is increased from 25–100 patients the increase in the number of patients receiving surgery is lower in the OPSC option than the TOMS − Surg option. This indicates that fewer patients are referred to surgery in the OPSC treatment pathway. When the capacity of OPSC is further increased to 125 patients per month the number of patients receiving surgery in the OPSC and TOMS − Surg options are equal indicating that current surgical capacity has been reached.
Figure 3a shows the average time patients are predicted to wait before receiving an initial assessment by TOMS or OPSC over the model period for each service provision alternative. Patient waiting times reduce in the same way for TOMS − Surg and TOMS + Surg over the various increases in service capacity tested. Increasing the service capacity of OPSC decreases initial assessment waiting times by a larger amount than TOMS. However, waiting times start to converge for OPSC and TOMS when service capacity is increased to 125 additional patients per month.
a Average time to initial assessment over model period. b Average surgical waiting times over model period. Nb. Mean waiting time values were calculated as the mean of 10 model runs each using unique random number streams with approximately 23,000 simulated patients per run. Asterisk indicates initial assessment by TOMS or OPSC. CI credible interval, OPSC orthopaedic physiotherapy screening clinic and multidisciplinary service, TOMS – Surg traditional service provision through orthopaedic medical specialists without additional surgical resources, TOMS + Surg traditional service provision through orthopaedic medical specialists with additional surgical resources
Figure 3b shows the average time patients are predicted to wait before receiving surgery over the model period for each service provision alternative. Increasing the service capacity of TOMS + Surg decreases surgical waiting times by the largest amount. Increasing the service capacity of OPSC from 25–100 additional patients per month has little effect on surgical waiting times; however, waiting times start to increase more rapidly when the capacity of OPSC is increased to 125 patients per month. Increasing the service capacity of TOMS − Surg by 25 additional patients per month has little effect on surgical waiting times. However, when TOMS − Surg capacity is increased beyond this point surgical waiting times are predicted to increase markedly over the model period.
Table 3 presents the levels of resource utilisation (defined as the average percentage service capacity used over the modelled time horizon) for surgery and initial assessment by OPSC or TOMS predicted by the economic model for each service provision alternative. In the analyses where TOMS capacity (±surgery) is increased by 25–100 additional patients per month, 100 % resource utilisation for TOMS is predicted. When TOMS capacity is further increased by 125 patients per month, TOMS resource utilisation decreases to 94 %. Resource utilisation for OPSC is predicted to be 100 % when OPSC patient capacity is increased from 25–75 patients per month. When OPSC capacity is increased by an additional 100–125 patients per month, resource utilisation declines indicating OPSC capacity over the modelled time horizon is beginning to exceed the number of patients suitable to be managed through this pathway. Surgical resource utilisation increases from around 76–99 % as the maximum capacity of OPSC is increased by 0–125 additional patients per month. Surgical resource utilisation increases to 100 % as TOMS − Surg is increased by 75 additional patients per month or greater. Average surgical resource utilisation declines as TOMS + Surg capacity is increased.
Table 4 presents a series of univariate and multivariate sensitivity analyses showing how the incremental cost, incremental effects, ICER and net monetary benefit (NMB) results are affected by alterations in the base-case parameter values using the OPSC + 100 patient capacity analysis as an example. The ICER and incremental NMB results appear reasonably stable across each of the sensitivity analyses conducted.
5 Discussion
This research evaluated the efficiency of different methods of delivering orthopaedic outpatient services in an example hospital where demand exceeds capacity and waiting times are beyond clinical recommendations. The study compared the cost effectiveness, patient throughput and waiting times of various combinations of specialist orthopaedic outpatient services and advanced practice physiotherapy-led services using a DES model with DQ.
Modelling of current demand over 5 years demonstrates that current levels of orthopaedic service provision in the example hospital are inadequate. The model indicates that if services remain unchanged from current practice, queues for orthopaedic services will continue to increase creating unacceptable delays beyond those timeframes recommended for orthopaedic consultation in Australia (i.e. 90 days for urgency category 2 and 365 days for urgency category 3 patients). Unchanged over the 5-year modelled time horizon, waiting times may grow to around 2.7 years. In Australia, revealed preferences show that the willingness-to-pay (WTP) per QALY is around A$50,000–A$64,000 [19, 20]. In the current analyses, the ICER values for both TOMS and OPSC fall well below these WTP thresholds in all scenarios tested and would, therefore, be considered cost effective. However, the analysis suggests that increasing the capacity of OPSC is a more cost-effective option when compared to TOMS, generating more QALYs per health-care dollar spent. Furthermore, if the perspective of this analysis was expanded to a societal level, then these ICERs would likely further improve as the broadened analysis would capture the reduction in patient productivity over the protracted patient waiting times.
Unlike Markov-cohort modelling, microsimulation, or DES without DQ, employing DES with DQ in situations where capacity constraints predominate provides valuable additional information beyond cost effectiveness to guide resource allocation decisions. For instance, in the analyses where TOMS − Surg capacity is increased by 75–125 patients per month the ICER for these service provision options improves (Table 2). However, this improvement comes at the cost of rapidly increasing surgical waiting times which are unlikely to be desirable (Fig. 3b). In contrast, as OPSC capacity is increased (also without altering surgical capacity) the demand for surgery rises but does not generate increased and protracted surgical waiting times (Fig. 3b). This contrast is further demonstrated by comparing the average resource utilisation data generated by the model. As TOMS − Surg capacity is increased by 75–125 patients per month, demand for surgery equals, or exceeds, supply leading to 100 % resource utilisation rates (Table 3). However, when OPSC capacity is increased from 75–100 patients, surgical resource demand increases but does not exceed supply, increasing surgical resource utilisation to around 94–98 % of current capacity (Table 3).
The model also indicates that at a 100 patient per month increase in OPSC capacity, OPSC resource utilisation would be high (98 %) indicating little unused OPSC resources over the modelled period (Table 3). However, given the current demand, if OPSC capacity was increased beyond this level to 125 additional patients per month, OPSC resource utilisation would decrease to 85 % over the modelled period (Table 3). This indicates that supply of OPSC would exceed demand and potentially lead to underutilised OPSC resources in this scenario.
There are limitations of this study. This economic analysis is based on non-randomised evidence and, therefore, it is possible that the data used in it may be affected by confounding factors. Nevertheless, any confounders should affect each analysis in a similar manner. In addition, like many such analyses, data were not available which would allow the comparison of the model’s output with the historical performance of the hospital of interest (i.e. external validation was not possible given the available data) [18].
In summary, in the hospital of interest, the model indicates that increasing the capacity of the current advanced practice physiotherapy-led service to manage semi- and non-urgent patients would be cost effective, improve patient throughput and reduce patient waiting times without exceeding current surgical resources. An increase of OPSC capacity of around 100 patients per month is predicted to result in a high level of OPSC resource utilisation. However, it is important to note that only approximately 60 % of the semi- and non-urgent orthopaedic patient population were deemed suitable for OPSC intervention, the remaining patients require intervention with TOMS. The model shows that even when all patients suitable for OPSC are managed by OPSC, TOMS remains at 100 % utilisation, indicating that demand for TOMS remains high and exceeds supply. This situation could be ameliorated by parallel increases in the capacity of TOMS.
References
Oldmeadow LB, Bedi HS, Burch HT, Smith JS, Leahy ES, Goldwasser M. Experienced physiotherapists as gatekeepers to hospital orthopaedic outpatient care. Med J Aust. 2007;186(12):625–8 (Epub 2007/06/20. eng).
Schoch PA, Adair L. Successfully reforming orthopaedic outpatients. Aust Health Rev Publ Aust Hosp Assoc. 2012;36(2):233–7 (Epub 2012/05/26. eng).
Blackburn MS, Cowan SM, Cary B, Nall C. Physiotherapy-led triage clinic for low back pain. Aust Health Rev Publ Aust Hosp Assoc. 2009;33(4):663–70 (Epub 2010/02/20. eng).
Daker-White G, Carr AJ, Harvey I, Woolhead G, Bannister G, Nelson I, et al. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J Epidemiol Community Health. 1999;53(10):643–50 (Epub 2000/01/05. eng).
Hattam P. The effectiveness of orthopaedic triage by extended scope physiotherapists. Clin Gov Int J. 2004;9:244–52.
Desmeules F, Toliopoulos P, Roy JS, Woodhouse LJ, Lacelle M, Leroux M, et al. Validation of an advanced practice physiotherapy model of care in an orthopaedic outpatient clinic. BMC Musculoskelt Disord. 2013;14:162 (Epub 2013/05/10. eng).
Smith DRM. Orthopaedic physiotherapy screening clinics—an approach to managing overburdened orthopaedic services (Abstract). Physiotherapy. 2007;93(S1):S746.
Standfield L, Comans T, Scuffham P. Markov modeling and discrete event simulation in health care: a systematic comparison. Int J Technol Assess Health Care. 2014;30(2):165–72 (Epub 2014/04/30. eng).
Comans T, Raymer M, O’Leary S, Smith D, Scuffham P. Cost-effectiveness of a physiotherapist-led service for orthopaedic outpatients. J Health Serv Res Policy. 2014 (Epub 12 May 2014).
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435 (Epub 2012/02/24. eng).
Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev. 2008;1:CD005619 (Epub 2008/02/07. eng).
Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F. Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine. 2013;38(7):E409–22 (Epub 2013/01/22. eng).
Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Therapy. 2003;83(8):696–706 (Epub 2003/07/29. eng).
Rahme H, Solem-Bertoft E, Westerberg CE, Lundberg E, Sorensen S, Hilding S. The subacromial impingement syndrome. A study of results of treatment with special emphasis on predictive factors and pain-generating mechanisms. Scand J Rehabil Med. 1998;30(4):253–62 (Epub 1998/11/24. eng).
PBAC. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (Version 4.4). Department of Health. Canberra: Australian Government; 2013.
Hawthorne G, Richardson J, Osborne R. The Assessment of Quality of Life (AQoL) instrument: a psychometric measure of health-related quality of life. Qual Life Res Int J Qual Life Aspects Treat Care Rehabil. 1999;8(3):209–24 (Epub 1999/09/03. eng).
Standfield LB, Comans TA, Scuffham PA. An empirical comparison of Markov cohort modeling and discrete event simulation in a capacity-constrained health care setting. Eur J Health Econ HEPAC Health Econ Prevent Care. 2015 (Epub 2015/12/31. Eng).
Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM, Wong JB. Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-7. Med Decis Making. 2012;32(5):733–43 (Epub 2012/09/20. eng).
Henry DA, Hill SR, Harris A. Drug prices and value for money: the Australian Pharmaceutical Benefits Scheme. JAMA. 2005;294(20):2630–2 (Epub 2005/11/24. eng).
Shiroiwa T, Sung YK, Fukuda T, Lang HC, Bae SC, Tsutani K. International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ. 2010;19(4):422–37 (Epub 2009/04/22. eng).
Acknowledgments
The authors gratefully acknowledge Orthopaedic Physiotherapy Screening Clinic and Multidisciplinary Services Program Manager, David Smith, research staff, Elise Gane, Peter Window, Zoe Michaleff, and Erin Pitt, for their contribution to this study and the Physiotherapy and Orthopaedic Department Directors and staff from the participating hospitals.
Authors contributions
L. Standfield and T. Comans: economic model development, guided and conducted the analyses, developed the manuscript. M. Raymer, S. O’Leary: collection, provision and interpretation of key clinical data, expert advice on service delivery methods and manuscript development. N. Moretto: collection, provision and interpretation of key clinical data and manuscript development. P. Scuffham: expert economic advice and review, manuscript development and oversight.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
L. Standfield, T. Comans, M. Raymer, S. O’Leary, N. Moretto, and P. Scuffham had no conflicts of interest to disclose.
Financial support for this study was provided by the Australian Centre for Health Services Innovation (AusHSI) and by an Australian Postgraduate Award Scholarship grant from the Australian government. The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Rights and permissions
About this article
Cite this article
Standfield, L., Comans, T., Raymer, M. et al. The Efficiency of Increasing the Capacity of Physiotherapy Screening Clinics or Traditional Medical Services to Address Unmet Demand in Orthopaedic Outpatients: A Practical Application of Discrete Event Simulation with Dynamic Queuing. Appl Health Econ Health Policy 14, 479–491 (2016). https://doi.org/10.1007/s40258-016-0246-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-016-0246-1