Abstract
The incidence of malignant melanoma (MM) continues to rise in the United States. While sun protection and full body skin examinations remain the mainstay of preventative care, chemoprevention of the deadly disease has become an increasingly popular field of study. In this focused review, we discuss current findings and analyze the risks and benefits of various agents investigated for the primary and secondary chemoprevention of MM. Such agents include topical retinoids, vitamins, and supplements, Polypodium leucotomas extracts, non-steroidal anti-inflammatory agents (NSAIDs), statins, sunscreens, and field therapy with topical imiquimod for primary and secondary chemoprevention. We further identify a need for expanded high quality human research on the topic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chemoprevention, the use of natural, synthetic, or biologic agents to prevent carcinogenic progression, has been more widely studied in the context of keratinocyte carcinomas compared with malignant melanomas. |
Topical retinoids, vitamins and minerals, Polypodium leucotomas extracts, non-steroidal anti-inflammatory agents, sunscreens, and topical imiquimod have been investigated in human models for use in protecting against malignant melanoma. |
Further research involving human subjects is needed to better elucidate which agents are suitable for clinical use. |
1 Introduction
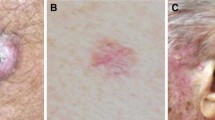
Skin cancer is the most common cancer in the United States (US), and its incidence currently exceeds that of breast, prostate, lung, and colon cancer combined [1]. Malignant melanoma (MM, shown in Fig. 1), which accounts for a minority of skin cancer cases, results in the overwhelming majority of deaths [2]. Risk factors for MM are similar to those of other skin cancers, but also include history of numerous dysplastic or congenital melanocytic nevi, or a family or personal history of MM [3].
Malignant melanoma is associated with repeated and sporadic ultraviolet (UV) exposure, and more often occurs in people who have had multiple sunburns as children or adolescents. UV radiation causes suppression of the immune response and release of mediators that affect antigen-presenting cells at a local and systemic level. It can also lead to the dimerization of pyrimidines on DNA, which can replicate and result in mutations [4].
Despite increased awareness of UV avoidance and sun protective measures, incidence of melanoma continues to rise [3]. The CDC Skin Cancer Prevention Progress Report for 2016 estimated a US$8.1 billion cost for skin cancer treatment in the US; furthermore, melanoma is the most lethal skin cancer and leads to 9000 deaths each year [5]. Chemoprevention, also known as therapeutic prevention, or precision prevention, has become widely investigated as a complementary or alternative method of decreasing the incidence of skin cancer. It refers to the administration of an agent in order to prevent disease. Primary, secondary, and tertiary chemoprevention aim to decrease the risk of disease occurrence in healthy individuals, pre-malignant to malignant transformations, and disease recurrence, respectively [6]. Effective chemoprevention of melanoma reduces incidence of melanomas and associated treatment costs [7]. Nevertheless, there are unique challenges associated with the study of potential chemopreventive agents in that they most often involve treatment of asymptomatic or healthy individuals.
A number of agents have been extensively studied in vivo and in vitro. While an abundance of research on the topic of chemoprevention of MM exists, this article aims to provide a focused review of those agents that have been clinically investigated in humans between 1985 and 2016.
2 Primary and Secondary Chemoprevention
2.1 Vitamins, Minerals, and other Supplements
2.1.1 Vitamin A
Retinol (vitamin A), its precursor (beta-carotene), and its derivatives (retinoids) have been studied for their effects against MM and keratinocyte carcinomas (KCs). Though their exact mechanism of action on the skin is unknown, they are thought to play a role in influencing growth factors, down-regulating proto-oncogenes, and elevating ceramide levels within the skin [8]. Retinoids may also inhibit tumor growth, angiogenesis, and metastasis [9]. The basis for melanoma chemoprevention with retinoids stems from studies that reveal inhibitory effects of retinoids on the in vitro growth of murine melanoma cell lines [10]. In vitro studies in human cell lines of melanoma treated with retinoids showed mixed results, with some cell lines showing inhibition of growth, no growth, or even stimulation of growth [11].
A preliminary study on two human subjects with metastatic cutaneous melanoma treated with topical β-all-trans-retinoic acid showed complete remission in one patient with a partial response in the other [12]. In 1986, Meyskens et al. conducted a pilot trial on the role of topical tretinoin in three subjects with dysplastic nevus syndrome, a possible precursor of MM. Pre- and post-treatment biopsies were interpreted by a pathologist and dermatologist unaware of the experimental protocol. The authors noted a regression to benign compound nevi in some of the subjects, sparking continued interest in research on the agent [13]. A randomized, double-blind, placebo-controlled study examined the effects of topical tretinoin on 21 patients with dysplastic nevi. Post-treatment comparative photographs showed marked fading or elimination of some dysplastic nevi clinically, and histologic examination showed disappearance or reversion to benign nevi in many treated lesions [14]. Another study of five male subjects with dysplastic nevi revealed a histologic and clinical improvement after 6-month treatment with topical tretinoin. The authors reported that its use for chemoprevention was limited by its associated irritation and difficulty of application [15]. Following this, a prospective double-blind randomized control trial (RCT) of 30 patients with atypical nevi revealed that after 4 months of treatment with either topical tretinoin 0.1 %, tretinoin 0.1 % with hydrocortisone 1 %, or a placebo cream once weekly under a hydrocolloid dressing occlusion, most of the treated nevi still met criteria for histological atypia [16]. Table 1 includes a summary of literature on chemopreventive agents. Systemic retinoids produce a multitude of potential adverse effects, which limit studies on their use in the chemoprevention of MM. While numerous studies demonstrate their chemopreventive properties against KCs in high-risk patients, literature on their role against MM is scarce [17].
2.1.2 Vitamin B3 (Nicotinamide)
UV radiation-induced DNA damage requires adenosine triphosphate (ATP)-dependent DNA repair enzymes to avoid genetic mutations and carcinogenesis. Since nicotinamide is an essential co-factor for the production of ATP, its chemopreventative properties may stem from maintaining an adequate ATP pool in addition to reducing the immunosuppressive effects of UV radiation [18]. Phase II and III randomized, double-blind, placebo-controlled clinical trials suggest an efficacious role of oral nicotinamide in the prevention of KCs [18, 19]. Although clinical studies on human melanocytic tumors are lacking, a preclinical study investigating the effects of nicotinamide on UV-irradiated primary human melanocytes revealed that nicotinamide significantly enhanced repair of cyclobutane pyrimidine dimers and oxidative DNA photolesions [20].
2.1.3 Polypodium leucotomas Extracts
Extracts from the tropical fern Polypodium leucotomas (PL) have been used by indigenous peoples in the treatment of inflammatory disorders [21]. A study on the safety of one product containing PL extract found no mutagenic/genotoxic activity, and no target organ or treatment-related toxicological effects in vitro and in vivo with Wistar rats using a maximum dose of 1200 mg/kg daily for a 90-day study period [22]. Additionally, a randomized, double-blinded, placebo-controlled trial on human subjects taking two doses of PL extract (240 mg) daily for 60 days found no changes in safety assessments (physical examination, vital signs, complete blood count with differential, comprehensive metabolic panel, and prothrombin time–partial thromboplastin time) compared with baseline measures with no reports of adverse events. The authors of this study also found a decreased number of sunburns and an increased minimal erythema dose (MED) in participants taking PL extract [23]. Some of the potential chemopreventive effects of PL extract may be related to its anti-inflammatory and antioxidant properties, activation of the tumor suppressor p53, inhibition of COX-2 expression, and enhanced DNA repair following UV exposure [24]. One preclinical study of topical PL extract applied to hairless albino mice exposed to UVB radiation showed treated mice had a reduction in skinfold thickness, lower degrees of histological parameters of photoaging damage and decreased numbers of skin tumors following cessation of the UVB exposure compared with controls [25].
A preliminary human study of 21 healthy volunteers either treated or untreated with oral psoralens and exposed to solar radiation were evaluated before and after topical or oral administration of PL extract. This study revealed that both topical and oral PL extract significantly increased the UV dose required for various markers of cutaneous phototoxicity [26]. A more recent human study of nine healthy participants exposed to varying doses of artificial UV radiation with and without oral administration of PL extract (7.5 mg/kg) found significant decreases in erythema, sunburn cells, cyclobutane pyrimidine dimers, proliferating epidermal cells and dermal mast cell infiltration among treated participants [27]. Furthermore, a 2009 RCT found decreased levels of the UVA-induced ‘common deletion’ in healthy volunteers following oral PL extract supplementation [28].
The most recent study including 61 high-risk MM patients (25 with familial and/or multiple MM, 20 with sporadic MM, and 16 with dysplastic nevus syndrome without history of MM) found that oral PL extract (1080 mg total dose) significantly increased the MED in all patients (0.123–0.161 J/cm2, p < 0.05). This study also went further to evaluate patients for mutation status on the cyclin-dependent kinase inhibitor 2A gene (CDKN2A), the best established high-risk locus for MM; in addition to polymorphism status on the melanocortin 1 receptor gene (MC1R), variants of which lead to differing levels of pheomelanin production and moderate risk for the development of MM. The authors found that patients in the familial MM group with a CDKN2A and/or MC1R polymorphism had larger responses in MED following treatment. Lastly, patients with dark hair and lower basal MED benefited most from treatment with PL extract [29].
While none of these human studies specifically evaluated patients for the development of MM, the surrogate markers of phototoxicity provide a helpful glimpse into PL extract as a potential chemopreventive agent since UVR is the most important etiologic factor in the development of MM.
2.1.4 Antioxidant Combinations
UV radiation results in the production of reactive oxygen species for hours following UV exposure [30]. Antioxidants have thus been thought to reduce the burden of DNA damage secondary to reactive oxygen species produced with UV exposure. The SU.VI.MAX (Supplémentation en Vitamines et Minéraux Antioxydants) trial tested the efficacy of a combination of vitamins in reducing the risk of skin cancer in a randomized, double-blinded, placebo-controlled, primary prevention study including 7876 and 5141 healthy French women and men, respectively. The daily antioxidant combination of 120 mg vitamin C, 30 mg vitamin E, 6 mg beta carotene, 100 μg selenium, and 20 mg zinc was tested against a placebo with a median follow-up time of 7.5 years. While no difference in MM incidence was found between the groups among men, there was a surprising increase in incidence of MM in the women treated with antioxidants. This study raised the question of whether antioxidants have different roles in the pathogenesis of MM in men and women. No differences in KCs were reported between groups [31]. A subsequent publication using the data from this study revealed that the risk of skin cancer declined following interruption of supplementation, which supported a causative role for antioxidants in the evolution of skin cancer [32].
2.2 Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
Numerous studies have shown that chronic aspirin and/or other NSAID use can decrease the risk of certain cancers [33–36]. Following UV exposure, higher levels of cyclo-oxygenase (COX)-2 are found in the epidermis and are thought to contribute to sunlight-induced skin cancers. NSAIDs are COX enzyme blockers [37]. Proposed mechanisms for NSAID chemoprevention include decreased catalytic production of prostaglandins and subsequent inflammation, inhibition of nuclear factor-κB (a pathway involved in apoptosis inhibition), reduction of vascular endothelial growth factor (VEGF) production, and inhibition of angiogenesis [38, 39].
A case–control study investigating 400 cutaneous melanoma patients and 600 age- and gender-matched controls revealed that the use of any NSAID for >5 years reduced the risk of melanoma (adjusted odds ratio [OR] 0.57; 95 % confidence interval [CI] 0.43–0.77) [40]. Another case–control study of a prescription database determined that the use of NSAIDs in 3242 patients from Northern Denmark who developed MM from 1991–2009 was associated with a decreased incidence rate ratio (IRR) of MM (IRR 0.87; 95 % CI 0.80–0.95). The authors observed greater benefits in individuals taking NSAIDs for longer periods of time [41]. Contrastingly, a similarly sized case–control study of a prescription database found no association between the use of COX-2 inhibitors and melanoma incidence in 3249 patients with MM and 16,000 matched controls (OR 1.05; 95 % CI 0.75–1.47) [42].
An observational prospective study assessing NSAID use among 59,806 postmenopausal Caucasian women revealed 548 incidents of melanoma during a median follow-up period of 12 years. Aspirin use was associated with a 21 % lower risk of melanoma (hazard ratio [HR] 0.79; 95 % CI 0.63–0.98) when compared with non-users. Furthermore, increased duration of use was also associated with decreased melanoma risk. Notably, non-aspirin NSAIDs and acetaminophen use did not reduce melanoma risk [43]. Another large observational prospective study of 92,125 Caucasian women revealed an increased risk of MM in current aspirin users (relative risk [RR] 1.32; 95 % CI 1.03–1.70), although the lack of a dose–response effect and a similar increase in past aspirin users did not support a pharmacologic mechanism. After adjustment for risk factors, the aspirin results were only mildly attenuated. The authors failed to detect an association between current non-aspirin NSAID use and MM (RR 0.96; 95 % CI 0.76–1.20) [44].
The only RCT to date on aspirin and the primary chemoprevention of MM randomized women to receive either 100 mg aspirin (n = 19,934) or placebo (n = 19,942) every other day for an average follow up of 10 years. The trial found no significant risk reduction for MM (RR 0.97) or other cancers [45].
A recent study of 50 patients with atypical nevi treated with either 150 mg sulindac or placebo daily for 8 weeks revealed an increase in the concentration of a pro-apoptotic metabolite (sulindac sulfone) in benign nevi [46]. This group had previously demonstrated that dysplastic nevi and primary melanoma expression of VEGF was significantly increased in comparison with benign nevi [47]. However, no changes in levels of either VEGF or cleaved caspase-3 expression were found following treatment with sulindac [46]. The short course of treatment and small sample size were limitations in the study, and further work must be done to reach a meaningful conclusion.
2.3 Statins
Statins (3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors) are used widely to treat hypercholesterolemia and have been shown to reduce morbidity and mortality related to cardiovascular events. A massive observational case–control study performed in the Netherlands revealed that statin users had a lower incidence of cancer (3129), identified through electronic ICD9-CM (International Classification of Disease, 9th revision, clinical modification) codes, when compared with controls (16,976) with an OR of 0.80 (95 % CI 0.66–0.96), with the OR for patients using statins for more than 4 years being 0.64 (95 % CI 0.44–0.93) [48]. A secondary analysis of tolerability and safety in a study comparing lovastatin with a placebo (n = 3304 and n = 3301, respectively) for the primary prevention of acute coronary events revealed a significant decrease in incidence of melanoma in the lovastatin group compared with the placebo group (n = 14 vs n = 27, respectively; p = 0.04) [49]. These findings led to additional studies specifically examining the effects of statin use on melanocytic neoplasms.
A prospective analysis of association between statin use and melanoma risk followed 199,726 postmenopausal women. At baseline, 7.4 % of women used statins, and the annualized rate of melanoma incidence was 0.09 % in both statin users and nonusers. The authors concluded no significant association between statin use and melanoma risk among postmenopausal women existed [41]. A meta-analysis of 20 RCTs of statins and fibrates for heart disease prevention found that the incidence of melanoma was not significantly associated with the use of either statins (OR 0.87; 95 % CI 0.61–1.23) or fibrates (OR 0.45; 95 % CI 0.20–1.01) [50]. Furthermore, a randomized, double-blind, placebo-controlled phase II clinical trial studied the effects of a 6-month course of lovastatin versus placebo on clinically atypical nevi (n = 34 and n = 32, respectively). Lovastatin did not induce changes in molecular biomarkers of biopsied lesions, or decrease histopathologic atypia, clinical atypia, or nevus number [51].
2.4 Sunscreen
Numerous studies support the role of UV radiation in skin carcinogenesis. Application of 2 and 7 % octyldimethyl p-aminobenzoic acid (PABA) significantly reduced the incidence of skin cancers in hairless albino mice and mice with slight pigmentation by blocking UV radiation [52]. Furthermore, Noonan et al. revealed that a single dose of burning UV radiation to neonatal mice induced tumors with high penetrance similar to human melanomas [53]. This preclinical evidence suggests the regular use of sunscreen starting in early life decreases the risk of melanoma.
Numerous studies have investigated the role of sunscreen in preventing the cutaneous effects of solar radiation including erythema, induction of histological atypia, and local or systemic immunosuppression [54]. A human study including 34 healthy subjects examined sunscreen’s protective effect on the systemic immunosuppressive effects of UV radiation. Subjects applied either sunscreen with a sun protection factor (SPF) of 15 (including 8 % octyl dimethyl PABA, 2 % 2-hydroxy-4-methyl oxybenzophenone, and 2 % butyl methoxydibenzoyl methane in an emulsion base) or a vehicle cream. They then received UV radiation in 12 half-hour exposures on consecutive days from a Wolf ‘Karibik’ solarium bed that emitted approximately 1.03 % UVB radiation (wavelength 280–315 nm) with the remainder being UVA radiation (peak emission of wavelength 350–360 nm). Blood tests performed prior to UV exposure and on days 1, 7, 14, and 21 after exposure measured systemic immune effects of exposure. A Chromium-51 release assay measured natural killer (NK) cell activity against the melanoma target cell MM200 and the K562 myeloid line. The study revealed that sunscreen application prior to solarium lamp exposure did not protect against the depression in NK cell activity against melanoma cells when compared with a vehicle control. The authors of this 1987 paper concluded that further studies on the role of sunscreen in melanoma needed to be conducted [55].
A randomized Australian trial assigned participants to daily broad-spectrum sunscreen containing 8 % 2-ethyl hexyl-p-methoxycinnamate and 2 % 4-tert-butyl-4 methoxy-4-dibenzoylmethane (SPF 16) and 30 mg beta-carotene supplements (n = 404) or discretionary use of sunscreen with placebo supplements (n = 416) from 1992 to 1996. Compliance was assessed by weight of returned sunscreen bottles, surveys asking average frequency of use, and remaining supplement tablet counts. Risk factor assessment at baseline included history of skin cancer, skin color, outdoor behavior, and sunburn history. Sun exposure and protection behavior was updated throughout the trial. Ten years after trial cessation, 11 primary melanomas had been identified in the daily sunscreen group, and 22 in the discretionary group (HR 0.50; 95 % CI 0.24–1.02; p = 0.05). Furthermore, only three invasive melanomas were identified in the daily sunscreen group compared with 11 invasive melanomas in the discretionary group (HR 0.27; 95 % CI 0.08–0.97), despite similar outdoor behavior between groups both during and after the trial [56].
More recently, a study by Carrera et al. [57] compared the effects of a physical barrier to sunscreen in protecting against UV-B radiation. Twenty-three clinically similar nevi from 20 patients were studied. Half of each nevus was covered with either an application of sunscreen or an opaque physical barrier then irradiated with a single dose of 2 MED UV-B light (UV800, Waldmann) to a 2 cm2 area centered on the nevus, and followed up histologically 7 days later. Both physical opaque barrier and sunscreen including broad-spectrum SPF 50 containing octocrylene, avobenzone (Parsol 1789), titanium dioxide, ecamsul (Mexoryl SX), and Mexoryl XL applied 30 min prior to UV exposure only partially protected against UV-B effects on nevi. While visible and dermoscopic changes were not always appreciated, subclinical protection occurred with both sunscreen and a physical barrier. These subclinical effects were measured by blinded histopathologic and immunohistochemical (IHC) evaluation. At the histopathological level, sunscreen was less effective than a physical barrier against melanocyte activation as evidenced by intensity and percentage of Melan-A staining. Interestingly, IHC stains for human melanoma black-45 antigen (HMB-45) and melanoma antigen recognized by T-cells-1 (Melan-A monoclonal antibody) revealed that neither sunscreen nor a physical barrier prevented inflammation. The authors concluded that while weak differences between the forms of protection existed, the protective role of sunscreen in avoiding UV radiation-induced effects on nevi was similar to a physical barrier [57]. It is important to note that 2 MED of UV-B light is a very low and easily achievable dose. The comparison of an SPF 50 sunscreen to a physical barrier against this low UV dose may not be clinically significant.
2.5 Imiquimod Field Therapy
Field therapy consists of topical agents including 5-fluorouracil, diclofenac, imiquimod, ingenol mebutate, as well as photodynamic therapy. With regard to MM, imiquimod modifies the immune response modifier by binding to Toll-Like Receptors 7 and 8 on dendritic cells, macrophages, and neutrophils, and up-regulates interferon-α, tumor necrosis factor-α, as well as other cytokines, leading to cell-mediated immunity (Th1) and inflammation. It further recruits cytotoxic T-cells (CD8+) and CD68+ macrophages [58]. In a single-blinded study, ten patients with atypical nevi and at least eight nevi >5 mm on their trunks treated their lesions with 5 % imiquimod cream three times weekly for 16 weeks. Clinical response was gauged with standardized photographs of the nevi and histologic assessment of each patient’s four largest nevi. No obvious changes in size and morphology were detected, but the authors reported that subtle changes in nevus color could not be assessed due to imperfect spectral registration of images. Histologically, 4 of 14 treated nevi and 0 of 14 untreated nevi showed significant relative reduction of junctional and intraepidermal nevocytes along with papillary fibrosis and variable inflammation (p = 0.03). The authors concluded that the histologic changes observed suggested a possible role for imiquimod in the treatment of atypical nevi with the intent of melanoma chemoprevention [59]. In a smaller study, three subjects applied imiquimod to atypical nevi five nights weekly for 12 weeks. Imiquimod use led to a dense inflammatory infiltrate in two of three of the atypical nevi treated and failed to produce lesion resolution [60]. The authors suggested these inflammatory changes may be misinterpreted as severe melanocytic atypia or melanoma.
3 Discussion
The number of studies on chemoprevention of melanoma has continued to grow in recent years. The major challenge in conducting these studies stems from the need to treat healthy subjects for long periods of time including a significant follow-up period in order to establish whether an agent is protective. Researchers have developed a multitude of shortcuts to estimate potential chemopreventive properties of an agent through evaluation of visible and histologic skin changes following UV exposure. While these surrogate measures are helpful in the short term they are not without pitfalls. For instance, the inherent subjectivity when evaluating tissue histologically could influence results when the study design relies on histologic ranking criteria to establish chemopreventive properties. In this paper we discussed numerous agents that have been clinically investigated in humans.
The studies on topical vitamin A derivatives are contradictory, with the most robust study showing persistent histologic atypia following treatment [16]. The most positive study suggested a regression of histologic atypia in dysplastic nevi, but these are not immediate precursors to MM lesions [14]. Furthermore, some of the studies that suggested an effect on tumorigenesis underappreciated the heterogeneity of dysplastic nevi and failed to appropriately stratify and randomize lesions by clinical appearance [15]; the lesions may have been histologically distinct prior to treatment. Lastly, due to the known anti-inflammatory properties of topical retinoids, the authors may have misinterpreted the overall decrease in inflammatory response as histologic improvements. Overall, topical vitamin A is locally irritating, and its role in the prevention of MM is inconclusive. While oral retinoid treatments may play a chemopreventive role against KCs in immunocompromised patients, their potentially severe adverse effects (teratogenicity, hyperlipidemia, nyctalopia, and mucocutaneous dryness) limit their use in healthy patient chemoprevention, or even in tertiary chemoprevention given the effective adjuvant immunotherapies in use with fewer side effects.
Nicotinamide is safe and efficacious in chemoprevention of KCs in clinical studies, through a mechanism thought to involve an enhancement of DNA repair and reduction in UV-induced immunosuppression. While human clinical trials on its potential chemopreventive effect against melanoma have not yet occurred, a preclinical study suggests nicotinamide is also efficacious in enhancing DNA repair in primary human melanocytes [20]. Future studies involving human subjects are likely on the horizon.
Extracts from the fern Polypodium leucotomos (PL) have been used historically by indigenous peoples and recently have been shown to be safe for human consumption and possess photoprotective properties in multiple preclinical and human studies [22, 23, 25–29]. This agent is unique and attractive in chemoprevention because its oral absorption leads to diffuse skin distribution, which enhances protection particularly when combined with topical sunscreen. Additionally, PL extract may be used as an adjunct in patients receiving PUVA or UVB as part of their treatment, especially when cutaneous phototoxicity is the limiting factor [26]. While clinical trials investigating the role of PL extract on the incidence and severity of MM are lacking, the availability and increased usage of this agent should stimulate further study on its role in preventing MM.
The strongest study investigating the role of a combination of antioxidants in the chemoprevention of melanoma (SU.VI.MAX trial) found an increase in the incidence of melanoma in women treated with the antioxidant combination [31], and a decline in overall skin cancer incidence following cessation of antioxidant treatment [32]. The major limitation of this study was the relatively low number of events, due to the low overall incidence of melanoma; thus, differences in risk among women and men should be interpreted with caution. Furthermore, the authors report it was not possible to measure voluntary antioxidant intake following the treatment period. A recent study revealed that oxidative stress has an inhibitory effect on distant metastasis in human melanoma cells in NOD-SCID-II2rg (−/−) mice, potentially implicating a role for antioxidants in the malignant spread of existing melanomas [61].
Several case–control studies on the long-term use of NSAIDs found a decreased risk of MM and led to further studies. These studies were not without limitations, including small sample sizes in the Curiel-Lewandrowski et al. study [40], and an assumption that dispensed medications were in fact taken regularly by the individual visiting the pharmacy in the Johannesdottir et al. study [41]. The subsequent two largest prospective, observational, case–control studies revealed conflicting results. The Gamba et al. study, which was limited by self-reported drug administration and a non-generalizable study population (postmenopausal women), found a protective effect of regular aspirin use on melanoma risk [43]. A similarly sized study by Jeter et al., which only studied Caucasian women, identified an increased risk of MM in women taking aspirin, and no association with risk of melanoma in women taking non-aspirin NSAIDs [44]. Furthermore, the interventional study conducted by Cook et al. found no association between aspirin use and MM risk [45]. Since the results of NSAID use in the chemoprevention of MM are largely mixed, we identify a need for expanded research on the efficacy of specific NSAIDs in chemoprevention of MM.
The study of statins as potential chemopreventive agents against melanoma began after secondary analyses of large-scale cardiovascular clinical trials suggested lower rates of melanoma in the treatment arm [49, 62]. Large-scale observational studies have demonstrated decreased incidence of cancer in statin users [48]. Contrastingly, an association study [63] and a meta-analysis of 20 RCTs including statin treatment [50] did not find any significant association between statin use and melanoma incidence. The strongest experimental study, a randomized, placebo-controlled, double-blind clinical trial that investigated the effects of a 6-month course of lovastatin on clinically atypical nevi, failed to identify any changes indicative of reversal of atypia or regression [51]. Thus, the authors concluded that if lovastatin has an effect on melanoma incidence, it does so through an alternative mechanism to the reversal of atypia, or a longer treatment course was needed to appreciate changes in atypia. It is important to note that reversal of atypia in an atypical nevus with a 6-month course of a statin may be too high a bar, and potentially not even a relevant bar when evaluating the chemopreventative effects of statins.
Numerous studies also investigate the role of sunscreen in the chemoprevention of melanoma. The study by Hersey et al. revealed that sunscreen application prior to solarium lamp exposure did not protect against UV-induced decreases in NK cell numbers [55]. At the same time, suppression of NK cell numbers and activity during UV exposure has not been shown to reduce melanoma development in humans, making the significance of this finding unclear. The Green et al. RCT found that daily application of sunscreen protected against melanoma compared with discretionary sunscreen use [56]. Taken together, sunscreen’s safe and preventive role against skin cancer stands clear, and its use in protecting against skin cancer is strongly encouraged.
Imiquimod has been found to lead to regression of atypical nevi [59]. At the same time, a study involving only three patients raised the concern that imiquimod might confound histologic evaluation of atypical nevi as a result of the dense inflammatory infiltrate it produces [60]. Given the supporting evidence, further studies investigating the chemoprevention of MM with topical imiquimod are warranted.
4 Conclusion
Chemoprevention, the use of chemical agents in order to prevent progressive or invasive disease, has the potential to reduce the complexity and cost of treating advanced-stage malignant melanoma. From this review, we conclude that while studies have explored numerous agents for their chemopreventive properties against MM, only some of these agents may effectively work in humans. Agents with more robust investigation include topical retinoids, Polypodium leucotomos extract, sunscreen, NSAIDs, statins, and topical imiquimod.
Studies most strongly support regular sunscreen use. Topical vitamin A derivatives have not been investigated in humans for their role in regression of histologic atypia since 1998 due to a preclinical study that showed some melanoma cell lines were stimulated to grow following application of a retinoid, and a human clinical trial that showed no effect on histologic atypia. Nicotinamide, while shown in multiple clinical trials to be of benefit in the chemoprevention of non-melanoma skin cancer, particularly among immunocompromised individuals, has not been studied in the chemoprevention of melanocytic neoplasms in humans. Polypodium leucotomos extract has been shown in preclinical and human studies to provide safe photoprotection, but there are no studies investigating its role in chemoprevention of MM. NSAIDs and statins have been investigated as a result of data available from large clinical trials investigating their cardioprotective properties. Large studies examining their impact on the incidence of melanoma are largely mixed, and they have not been shown to reduce atypia in preliminary studies. These drugs offer a unique opportunity for further study in melanoma chemoprevention due to their current FDA indications for reducing morbidity and mortality related to cardiovascular disease. Since the available data is not sufficient to draw meaningful conclusions on the majority of investigated agents, further research must be conducted before chemoprevention can be recommended for clinical use.
References
Society AC. Cancer Facts & Figures 2015. 2015.
Howlader N NA, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations). Bethesda: National Cancer Institute 2012 December 23, 2015.
Society AC. Melanoma Skin Cancer; 2015.
Constantinou M. Melanoma Genomics and Immunotherapy. R I Med J (2013). 2015;98(11):31–4.
Skin Cancer Prevention Progress Report 2016. Atlanta: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2016.
Hong WK, Spitz MR, Lippman SM. Cancer chemoprevention in the 21st century: genetics, risk modeling, and molecular targets. J Clin Oncol. 2000;18(21 Suppl):9s–18s.
Einspahr JG, Stratton SP, Bowden GT, Alberts DS. Chemoprevention of human skin cancer. Crit Rev Oncol Hematol. 2002;41(3):269–85.
Wright TI, Spencer JM, Flowers FP. Chemoprevention of nonmelanoma skin cancer. J Am Acad Dermatol. 2006;54(6):933–46 (quiz 47–50).
Alizadeh F, Bolhassani A, Khavari A, Bathaie SZ, Naji T, Bidgoli SA. Retinoids and their biological effects against cancer. Int Immunopharmacol. 2014;18(1):43–9.
Lotan R, Giotta G, Nork E, Nicolson GL. Characterization of the inhibitory effects of retinoids on the in vitro growth of two malignant murine melanomas. J Natl Cancer Inst. 1978;60(5):1035–41.
Lotan R. Different susceptibilities of human melanoma and breast carcinoma cell lines to retinoic acid-induced growth inhibition. Cancer Res. 1979;39(3):1014–9.
Levine N, Meyskens FL. Topical vitamin-A-acid therapy for cutaneous metastatic melanoma. Lancet (London, England). 1980;2(8188):224–6.
Meyskens FL Jr, Edwards L, Levine NS. Role of topical tretinoin in melanoma and dysplastic nevi. J Am Acad Dermatol. 1986;15(4 Pt 2):822–5.
Edwards L, Jaffe P. The effect of topical tretinoin on dysplastic nevi. A preliminary trial. Arch Dermatol. 1990;126(4):494–9.
Halpern AC, Schuchter LM, Elder DE, Dt Guerry, Elenitsas R, Trock B, et al. Effects of topical tretinoin on dysplastic nevi. J Clin Oncol. 1994;12(5):1028–35.
Stam-Posthuma JJ, Vink J, le Cessie S, Bruijn JA, Bergman W, Pavel S. Effect of topical tretinoin under occlusion on atypical naevi. Melanoma Res. 1998;8(6):539–48.
Bettoli V, Zauli S, Virgili A. Retinoids in the chemoprevention of non-melanoma skin cancers: why, when and how. J Dermatol Treat. 2013;24(3):235–7.
Chen AC, Martin AJ, Choy B, Fernandez-Penas P, Dalziell RA, McKenzie CA, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373(17):1618–26.
Chen AC, Martin AJ, Dalziell RA, McKenzie CA, Lowe PM, Eris JM, et al. A phase 2 randomised controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients. Br J Dermatol. 2016. doi:10.1111/bjd.14662.
Thompson BC, Surjana D, Halliday GM, Damian DL. Nicotinamide enhances repair of ultraviolet radiation-induced DNA damage in primary melanocytes. Exp Dermatol. 2014;23(7):509–11.
Horvath A, Alvarado F, Szocs J, de Alvardo ZN, Padilla G. Metabolic effects of calagualine, an antitumoral saponine of Polypodium leucotomos. Nature. 1967;214(5094):1256–8.
Murbach TS, Beres E, Vertesi A, Glavits R, Hirka G, Endres JR, et al. A comprehensive toxicological safety assessment of an aqueous extract of Polypodium leucotomos (Fernblock((R))). Food Chem Toxicol. 2015;86:328–41.
Nestor MS, Berman B, Swenson N. Safety and efficacy of oral Polypodium leucotomos extract in healthy adult subjects. J Clin Aesthet Dermatol. 2015;8(2):19–23.
Zattra E, Coleman C, Arad S, Helms E, Levine D, Bord E, et al. Polypodium leucotomos extract decreases UV-induced Cox-2 expression and inflammation, enhances DNA repair, and decreases mutagenesis in hairless mice. Am J Pathol. 2009;175(5):1952–61.
Alcaraz MV, Pathak MA, Rius F, Kollias N, Gonzalez S. An extract of Polypodium leucotomos appears to minimize certain photoaging changes in a hairless albino mouse animal model. A pilot study. Photodermatol Photoimmunol Photomed. 1999;15(3–4):120–6.
Gonzalez S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucotomos prevents acute sunburn and psoralen-induced phototoxic reactions as well as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13(1–2):50–60.
Middelkamp-Hup MA, Pathak MA, Parrado C, Goukassian D, Rius-Diaz F, Mihm MC, et al. Oral Polypodium leucotomos extract decreases ultraviolet-induced damage of human skin. J Am Acad Dermatol. 2004;51(6):910–8.
Villa A, Viera MH, Amini S, Huo R, Perez O, Ruiz P, et al. Decrease of ultraviolet A light-induced “common deletion” in healthy volunteers after oral Polypodium leucotomos extract supplement in a randomized clinical trial. J Am Acad Dermatol. 2010;62(3):511–3.
Aguilera P, Carrera C, Puig-Butille JA, Badenas C, Lecha M, Gonzalez S, et al. Benefits of oral Polypodium Leucotomos extract in MM high-risk patients. J Eur Acad Dermatol Venereol. 2013;27(9):1095–100.
Premi S, Wallisch S, Mano CM, Weiner AB, Bacchiocchi A, Wakamatsu K, et al. Photochemistry. Chemiexcitation of melanin derivatives induces DNA photoproducts long after UV exposure. Science (New York, NY). 2015;347(6224):842–7.
Hercberg S, Ezzedine K, Guinot C, Preziosi P, Galan P, Bertrais S, et al. Antioxidant supplementation increases the risk of skin cancers in women but not in men. J Nutr. 2007;137(9):2098–105.
Ezzedine K, Latreille J, Kesse-Guyot E, Galan P, Hercberg S, Guinot C, et al. Incidence of skin cancers during 5-year follow-up after stopping antioxidant vitamins and mineral supplementation. Eur J Cancer (Oxford, England : 1990). 2010;46(18):3316–22.
Chan AT, Arber N, Burn J, Chia WK, Elwood P, Hull MA, et al. Aspirin in the chemoprevention of colorectal neoplasia: an overview. Cancer Prev Res (Philadelphia, Pa). 2012;5(2):164–78.
Ye X, Fu J, Yang Y, Gao Y, Liu L, Chen S. Frequency-risk and duration-risk relationships between aspirin use and gastric cancer: a systematic review and meta-analysis. PLoS One. 2013;8(7):e71522.
Swede H, Mirand AL, Menezes RJ, Moysich KB. Association of regular aspirin use and breast cancer risk. Oncology. 2005;68(1):40–7.
Salinas CA, Kwon EM, FitzGerald LM, Feng Z, Nelson PS, Ostrander EA, et al. Use of aspirin and other nonsteroidal antiinflammatory medications in relation to prostate cancer risk. Am J Epidemiol. 2010;172(5):578–90.
Clouser MC, Roe DJ, Foote JA, Harris RB. Effect of non-steroidal anti-inflammatory drugs on non-melanoma skin cancer incidence in the SKICAP-AK trial. Pharmacoepidemiol Drug Saf. 2009;18(4):276–83.
Monnier Y, Zaric J, Ruegg C. Inhibition of angiogenesis by non-steroidal anti-inflammatory drugs: from the bench to the bedside and back. Curr Drug Targets Inflamm Allergy. 2005;4(1):31–8.
Goodman JR, Grossman D. Aspirin and other NSAIDs as chemoprevention agents in melanoma. Cancer Prev Res (Philadelphia, Pa). 2014;7(6):557–64.
Curiel-Lewandrowski C, Nijsten T, Gomez ML, Hollestein LM, Atkins MB, Stern RS. Long-term use of nonsteroidal anti-inflammatory drugs decreases the risk of cutaneous melanoma: results of a United States case-control study. J Invest Dermatol. 2011;131(7):1460–8.
Johannesdottir SA, Chang ET, Mehnert F, Schmidt M, Olesen AB, Sorensen HT. Nonsteroidal anti-inflammatory drugs and the risk of skin cancer: a population-based case-control study. Cancer. 2012;118(19):4768–76.
Vinogradova Y, Coupland C, Hippisley-Cox J. Exposure to cyclooxygenase-2 inhibitors and risk of cancer: nested case-control studies. Br J Cancer. 2011;105(3):452–9.
Gamba CA, Swetter SM, Stefanick ML, Kubo J, Desai M, Spaunhurst KM, et al. Aspirin is associated with lower melanoma risk among postmenopausal Caucasian women: the Women’s Health Initiative. Cancer. 2013;119(8):1562–9.
Jeter JM, Han J, Martinez ME, Alberts DS, Qureshi AA, Feskanich D. Non-steroidal anti-inflammatory drugs, acetaminophen, and risk of skin cancer in the Nurses’ Health Study. Cancer Causes Control. 2012;23(9):1451–61.
Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial. JAMA. 2005;294(1):47–55.
Curiel-Lewandrowski C, Swetter SM, Einspahr JG, Hsu CH, Nagle R, Sagerman P, et al. Randomized, double-blind, placebo-controlled trial of sulindac in individuals at risk for melanoma: evaluation of potential chemopreventive activity. Cancer. 2012;118(23):5848–56.
Einspahr JG, Thomas TL, Saboda K, Nickolof BJ, Warneke J, Curiel-Lewandrowski C, et al. Expression of vascular endothelial growth factor in early cutaneous melanocytic lesion progression. Cancer. 2007;110(11):2519–27.
Graaf MR, Beiderbeck AB, Egberts AC, Richel DJ, Guchelaar HJ. The risk of cancer in users of statins. J Clin Oncol. 2004;22(12):2388–94.
Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279(20):1615–22.
Freeman SR, Drake AL, Heilig LF, Graber M, McNealy K, Schilling LM, et al. Statins, fibrates, and melanoma risk: a systematic review and meta-analysis. J Natl Cancer Inst. 2006;98(21):1538–46.
Linden KG, Leachman SA, Zager JS, Jakowatz JG, Viner JL, McLaren CE, et al. A randomized, double-blind, placebo-controlled phase II clinical trial of lovastatin for various endpoints of melanoma pathobiology. Cancer Prev Res (Phila). 2014;7(5):496–504.
Kligman LH, Akin FJ, Kligman AM. Sunscreens prevent ultraviolet photocarcinogenesis. J Am Acad Dermatol. 1980;3(1):30–5.
Noonan FP, Recio JA, Takayama H, Duray P, Anver MR, Rush WL, et al. Neonatal sunburn and melanoma in mice. Nature. 2001;413(6853):271–2.
Drolet BA, Connor MJ. Sunscreens and the prevention of ultraviolet radiation-induced skin cancer. J Dermatol Surg Oncol. 1992;18(7):571–6.
Hersey P, MacDonald M, Burns C, Schibeci S, Matthews H, Wilkinson FJ. Analysis of the effect of a sunscreen agent on the suppression of natural killer cell activity induced in human subjects by radiation from solarium lamps. J Invest Dermatol. 1987;88(3):271–6.
Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29(3):257–63.
Carrera C, Puig-Butille JA, Aguilera P, Ogbah Z, Palou J, Lecha M, et al. Impact of sunscreens on preventing UVR-induced effects in nevi: in vivo study comparing protection using a physical barrier vs sunscreen. JAMA Dermatol. 2013;149(7):803–13.
Michalopoulos P, Yawalkar N, Bronnimann M, Kappeler A, Braathen LR. Characterization of the cellular infiltrate during successful topical treatment of lentigo maligna with imiquimod. Br J Dermatol. 2004;151(4):903–6.
Dusza SW, Delgado R, Busam KJ, Marghoob AA, Halpern AC. Treatment of dysplastic nevi with 5 % imiquimod cream, a pilot study. J Drugs Dermatol. 2006;5(1):56–62.
Somani N, Martinka M, Crawford RI, Dutz JP, Rivers JK. Treatment of atypical nevi with imiquimod 5 % cream. Arch Dermatol. 2007;143(3):379–85.
Piskounova E, Agathocleous M, Murphy MM, Hu Z, Huddlestun SE, Zhao Z, et al. Oxidative stress inhibits distant metastasis by human melanoma cells. Nature. 2015;527(7577):186–91.
Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group. N Engl J Med. 1999;341(6):410–8.
Jagtap D, Rosenberg CA, Martin LW, Pettinger M, Khandekar J, Lane D, et al. Prospective analysis of association between use of statins and melanoma risk in the Women’s Health Initiative. Cancer. 2012;118(20):5124–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this review.
Conflict of interest
Jessica Mounessa, Talayesa Buntinx-Krieg, Rosie Qin, Cory A. Dunnick, and Robert P. Dellavalle have no conflicts of interest to disclose.
Additional information
J. Mounessa and T. Buntinx-Krieg are co-first authors.
Rights and permissions
About this article
Cite this article
Mounessa, J., Buntinx-Krieg, T., Qin, R. et al. Primary and Secondary Chemoprevention of Malignant Melanoma. Am J Clin Dermatol 17, 625–634 (2016). https://doi.org/10.1007/s40257-016-0221-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-016-0221-5