Abstract
Background
No studies have directly compared the effectiveness and safety of dabigatran and rivaroxaban using US Medicare data.
Objective
Our objective was to compare effectiveness and safety between rivaroxaban 20 mg/dabigatran 150 mg and rivaroxaban 15 mg/dabigatran 75 mg among patients with atrial fibrillation (AF).
Methods
Using 2010–2013 US Medicare Part D data, we selected patients with AF initiating dabigatran 150/75 mg or rivaroxaban 20/15 mg between 4 November 2011 (when rivaroxaban was approved) and 31 December 2013. Our sample included 7322 patients receiving dabigatran 150 mg, 5799 patients receiving rivaroxaban 20 mg, 1818 receiving dabigatran 75 mg, and 2568 receiving rivaroxaban 15 mg. We followed them until stroke, other thromboembolic events, bleeding, discontinuation or switch of an anticoagulant, death, or 31 December 2013. We constructed Cox proportional hazard models with propensity score weighting to compare clinical outcomes between groups.
Results
There was no difference in the risk of stroke between dabigatran 150 mg and rivaroxaban 20 mg (hazard ratio [HR] 1.05; 95 % confidence interval [CI] 0.97–1.13) or between dabigatran 75 mg and rivaroxaban 15 mg (HR 1.05; 95 % CI 0.94–1.18). Compared with dabigatran 150 mg, rivaroxaban 20 mg was associated with a higher risk of other thromboembolic events (HR 1.28; 95 % CI 1.14–1.44), major bleeding (HR 1.32; 95 % CI 1.17–1.50), and death (HR 1.36; 95 % CI 1.19–1.56). The risk of thromboembolic events other than stroke (HR 1.37; 95 % CI 1.15–1.62), major bleeding (HR 1.51; 95 % CI 1.25–1.82), and death (HR 1.21; 95 % CI 1.04–1.41) was also higher for rivaroxaban 15 mg than for dabigatran 75 mg.
Conclusions
There was no difference in stroke prevention between rivaroxaban and dabigatran; however, rivaroxaban was associated with a higher risk of thromboembolic events other than stroke, death, and bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We used 2010–2013 Medicare Part D data for patients with atrial fibrillation to compare the effectiveness and safety of two doses of dabigatran and rivaroxaban. |
We found no difference in stroke prevention between rivaroxaban and dabigatran; however, the risk of bleeding and the risk of thromboembolic events other than stroke were higher with rivaroxaban. |
Dabigatran showed a superior benefit–risk ratio than rivaroxaban in the prevention of stroke among a sample of Medicare beneficiaries with atrial fibrillation. |
1 Introduction
Dabigatran 150 mg and 75 mg were approved by the US FDA in October 2010 for the prevention of stroke among patients with non-valvular atrial fibrillation (AF), with 75 mg indicated for patients with creatinine clearance <30 ml/min [1]. Rivaroxaban 20 mg and 15 mg gained FDA approval for the same indication in November 2011, with 15 mg indicated for patients with creatinine clearance <50 ml/min [2]. Both doses of dabigatran are administered twice daily, whereas rivaroxaban follows a once-daily regimen [1, 2]. The RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) clinical trial found that dabigatran 150 mg was similar to warfarin in the risk of bleeding, but superior in the prevention of stroke [3]; the ROCKET-AF (Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) showed that rivaroxaban 20 mg/15 mg was similar to warfarin in both the risk of bleeding and the prevention of stroke [4, 5]. Since the approval of rivaroxaban, two new non-vitamin K antagonist oral anticoagulants (NOACs) have gained FDA approval for the same indication: apixaban in December 2012 and edoxaban in January 2015 [6, 7].
Because no clinical trials have directly compared NOACs, previous researchers have used the results of the RE-LY [3] and ROCKET-AF [4] trials to compare the effectiveness and safety of dabigatran and rivaroxaban [8, 9]. In these indirect comparisons, rivaroxaban 20 mg/15 mg was predicted to be less effective in the prevention of stroke and systemic embolism than dabigatran 150 mg, but similar in the risk of bleeding [8, 9]. Because the validity of indirect comparisons is limited by inter-trial population differences, and the subjects enrolled in the ROCKET-AF trial were considerably sicker than those in the RE-LY trial [3, 4], it is important to perform direct analyses to compare the effectiveness and safety of dabigatran and rivaroxaban using the same population.
Although several observational studies have compared the real-world effectiveness and safety of dabigatran or rivaroxaban with those of warfarin [10–15], only one study has directly compared the risk of bleeding between dabigatran and rivaroxaban; it found no differences in the risk of bleeding [16]. However, the authors used medical records from only two hospitals and did not separately examine the risk of bleeding by dose of anticoagulant [16]. Because the risk of bleeding varies with the strength of anticoagulant, it is also necessary to separately examine the risk of bleeding by dose [17–19]. To the best of our knowledge, no observational studies have conducted a head-to-head comparison of the effectiveness of dabigatran and rivaroxaban in the prevention of stroke in AF.
We used 2010–2013 pharmacy and medical claims data from a 5 % random sample of Medicare beneficiaries with AF to compare the risk of stroke, other thromboembolic events, death, and bleeding following the initiation of dabigatran and rivaroxaban at high doses (dabigatran 150 mg and rivaroxaban 20 mg) and low doses (dabigatran 75 mg and rivaroxaban 15 mg).
2 Methods
2.1 Data Source and Study Population
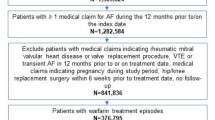
We obtained 2010–2013 pharmacy and medical data for a 5 % random sample of US Medicare beneficiaries from the Centers for Medicare and Medicaid Services (CMS). First, we identified patients who filled a prescription for dabigatran or rivaroxaban between 4 November 2011 (the approval date for rivaroxaban) and 31 December 2013 (n = 44,621) (Fig. 1). The index date was defined as the day of the first prescription filled for dabigatran or rivaroxaban in this time window. Second, we required that patients had a diagnosis of AF any time before the index date according to the CMS Chronic Condition Warehouse definition of AF (n = 22,292) [20]. Third, we excluded patients who had a claim for dabigatran or rivaroxaban in the 3 months before the index date to ensure we identified patients who initiated dabigatran or rivaroxaban treatment during our study period, when the risk of bleeding is higher [21]. We used a 3-month wash-out period because anticoagulants used in AF are usually prescribed as 30-day or 90-day supply prescriptions. Our final sample included 7322 patients receiving dabigatran 150 mg, 5799 receiving rivaroxaban 20 mg, 1818 receiving dabigatran 75 mg, and 2568 receiving rivaroxaban 15 mg. In our study, we did not include patients receiving rivaroxaban 10 mg because this dose has not been approved for the prevention of stroke and systemic embolism in AF [2]. Since apixaban was approved in December 2012, the follow-up period available for this treatment group in our dataset was shorter than 1 year; therefore, we did not include apixaban in our study.
We followed each individual from the index date until discontinuation of treatment, defined as a gap in anticoagulant treatment of over 60 days, switch of an anticoagulant or dose, death, or 31 December 2013 [13]. This study was approved by the Institutional Review Board at the University of Pittsburgh.
2.2 Outcomes
Effectiveness outcomes included ischemic stroke, other thromboembolic events, and all-cause mortality. Ischemic stroke was defined as having one inpatient, emergency room, or outpatient claim with primary or secondary International Classification of Diseases, Ninth Revision (ICD-9) codes 433, 434, or 436 [22, 23]. Other thromboembolic events included inpatient, emergency room, or outpatient claims for systemic embolism (ICD-9 = 444), transient ischemic attack (ICD-9 = 435), and pulmonary embolism (ICD-9 = 415.1) [22, 23]. Safety outcomes included any bleeding event and major bleeding; we also specifically reported safety outcomes for two anatomical locations: intracranial hemorrhage and gastrointestinal bleeding. Major bleeding events included intracranial hemorrhage, hemoperitoneum, and inpatient or emergency room stays for gastrointestinal, hematuria, or not otherwise specified hemorrhage (Table 1 in the Electronic Supplementary Material [ESM]) [13].
2.3 Covariates
We adjusted for demographic variables and clinical characteristics, all of which were measured at the index date. Demographic variables included age, race, and Medicaid eligibility. Clinical characteristics included CHADS2 (congestive heart failure, hypertension, aged ≥75 years, diabetes mellitus, stroke/transient ischemic attack [TIA]) score [24], chronic kidney disease, hypertension, a history of stroke or TIA, prior acute myocardial infarction, diabetes, congestive heart failure, acquired hypothyroidism, number of other CMS priority comorbidities (listed in Table 1), a history of bleeding, concomitant use of non-steroidal anti-inflammatory drugs (NSAIDs), and concomitant use of antiplatelet drugs (definitions are listed in Table 1).
2.4 Statistical Analysis
We compared patient characteristics between patients initiating dabigatran 150 mg and those initiating rivaroxaban 20 mg and between patients initiating dabigatran 75 mg and those initiating rivaroxaban 15 mg using Chi squared tests. To compare the unadjusted cumulative incidence of effectiveness and safety outcomes at 1-year follow-up, we constructed Kaplan–Meier time-to-event curves.
One of the limitations of using observational data to conduct comparative effectiveness studies is that individuals in one treatment group may not be comparable to individuals in the other group. To mitigate this problem, we used propensity score weighting, which was conducted in two steps. First, we constructed a logistic regression controlling for all covariates listed in the Covariates Section to calculate the probability of initiating rivaroxaban (propensity score). We used the Toolkit for Weighting and Analysis of Nonequivalent Groups (TWANG) in statistical software R to find the best logistic regression model to calculate the propensity score. We calculated standardized differences in covariate means between two treatment groups to evaluate whether covariates were balanced between treatment groups after propensity score weighting [25]. Standardized differences with absolute values <10 % indicate a good balance between treatment groups [26]. Second, we constructed Cox proportional hazards models to compare effectiveness and safety outcomes between groups, using the inverse of the propensity score for each individual as a weight. Cox models included one indicator variable for rivaroxaban initiation as well as all pre-defined covariates listed in the Covariates Section. Because one of the limitations of this methodology is the presence of large weights, we checked the distribution of weights and found that none of the subjects had weights >10. For all time-to-event analyses except those that compared the risk of all-cause mortality between treatment groups, the time at risk was censored at the end of the study period (31 December 2013) or at switch of anticoagulant or dose, discontinuation of anticoagulant therapy, or death. Time-to-event analyses built to compare the risk of all-cause mortality between treatment groups had the same censoring events except death. All analyses were conducted with statistical software SAS 9.4 (Cary, NC, USA).
We further compared the effectiveness and safety of dabigatran and rivaroxaban among three subgroups of patients: those aged >75 years, patients with chronic kidney disease, or those with at least seven CMS priority conditions other than AF [27]. For each subgroup identified, we re-calculated the propensity score and constructed Cox models to compare effectiveness and safety outcomes following the same methodology as with the overall sample.
2.5 Sensitivity Analyses
One may argue that some of our study participants may have initiated anticoagulation therapy for an indication other than AF. To examine whether this may have affected our results, we re-ran our analyses after excluding study participants who had claims in the 3 months before the index date with a diagnosis of venous thromboembolism, pulmonary embolism, phlebitis, and hip- or knee-replacement surgery. Subjects who used warfarin before the initiation of dabigatran or rivaroxaban may have had remaining warfarin at the time of dabigatran or rivaroxaban initiation, which may have affected the occurrence of bleeding events soon after the initiation of dabigatran or rivaroxaban. To analyze whether our results for safety outcomes were affected by this problem, we ran our analyses after excluding subjects who filled a prescription for warfarin 6 months before index date. It can sometimes be difficult to differentiate new events from prior diagnoses of strokes in patients with a history of stroke, so we conducted sensitivity analyses by including and excluding patients who had a history of stroke or TIA before the index date. Finally, we also examined the robustness of our results after excluding patients who filled a prescription for NSAIDs or antiplatelet agents after the index date.
3 Results
3.1 Patient Characteristics
The mean follow-up period was 385 days for patients receiving dabigatran 150 mg, 251 days for those receiving rivaroxaban 20 mg, 357 days for those receiving dabigatran 75 mg, and 239 for those receiving rivaroxaban 15 mg (Table 2 in the ESM). Before propensity score weighting, patients initiating rivaroxaban 20 mg were more likely to also be eligible for Medicaid benefits and have chronic kidney disease and acquired hypothyroidism than those initiating dabigatran 150 mg (Table 1). The mean age of patients receiving dabigatran 150 mg was 75.64 years, and the mean age of those receiving rivaroxaban 20 mg was 75.44 years. On average, patients receiving dabigatran 75 mg and those receiving rivaroxaban 20 mg were aged 82.00 and 81.71 years, respectively. Although low-dose dabigatran and rivaroxaban are only indicated in patients with AF with reduced kidney function, only 52.6 % of patients receiving dabigatran 75 mg and 51.5 % of those receiving rivaroxaban 15 mg had a diagnosis of chronic kidney disease. After propensity score weighting, all patient characteristics were balanced between rivaroxaban and dabigatran groups for both high- and low-dose initiators.
3.2 Unadjusted Incidence of Effectiveness and Safety Outcomes
Before adjustment, dabigatran 150 mg was associated with a lower risk of all-cause mortality, major bleeding, gastrointestinal bleeding, and any bleeding events than was rivaroxaban 20 mg (Table 2). The unadjusted incidence of clinical outcomes did not differ between patients receiving dabigatran 75 mg and those receiving rivaroxaban 15 mg except for any bleeding event, which was higher with rivaroxaban 15 mg than with dabigatran 75 mg.
3.3 Adjusted Hazard Ratio of Effectiveness and Safety Outcomes
Figure 2 shows the adjusted hazard ratios (HRs) for effectiveness and safety outcomes after propensity score weighting. The risk of ischemic stroke did not differ between rivaroxaban 20 mg and dabigatran 150 mg (HR 1.05; 95 % confidence interval [CI] 0.97–1.13); however, rivaroxaban 20 mg was associated with a higher risk of other thromboembolic events (HR 1.28; 95 % CI 1.14–1.44) and all-cause mortality (HR 1.36; 95 % CI 1.19–1.56) than dabigatran 150 mg. The risk of major bleeding (HR 1.32; 95 % CI 1.17–1.50), any bleeding event (HR 1.17; 95 % CI 1.10–1.24), and gastrointestinal bleeding (HR 1.19; 95 % CI 1.03–1.30) was also higher among patients initiating rivaroxaban 20 mg than among those initiating dabigatran 150 mg. The risk of intracranial hemorrhage did not differ between high-dose dabigatran and high-dose rivaroxaban.
Hazard ratios for effectiveness and safety outcomes, by treatment and dose. Hazard ratios were estimated with Cox proportional hazard models with propensity score weighting that controlled for treatment, age, sex, race, Medicaid eligibility, CHADS2 score, chronic kidney disease, hypertension, previous stroke or transient ischemic attack, acute myocardial infarction, diabetes mellitus, congestive heart failure, acquired hypothyroidism, number of other Centers for Medicare and Medicaid Services priority conditions, a history of bleeding, use of non-steroidal anti-inflammatory drugs (NSAIDs), and use of antiplatelet agents. CI confidence interval
Our results for the comparative risk of effectiveness and safety outcomes among low-dose initiators are consistent with the findings from high-dose initiators: there was no difference in the risk of ischemic stroke and intracranial bleeding between rivaroxaban 15 mg and dabigatran 75 mg; however, the risk of other thromboembolic events (HR 1.37; 95 % CI 1.15–1.62), all-cause mortality (HR 1.21; 95 % CI 1.04–1.41), major bleeding (HR 1.51; 95 % CI 1.25–1.82), any bleeding event (HR 1.39; 95 % CI 1.27–1.53), and gastrointestinal bleeding (HR 1.25; 95 % CI 1.09–1.44) was higher with rivaroxaban 15 mg than with dabigatran 75 mg.
3.4 Subgroup and Sensitivity Analyses
For patients with more than seven CMS priority chronic conditions other than AF, we found the risk of ischemic stroke to be higher with rivaroxaban 20 mg than with dabigatran 150 mg (HR 1.12; 95 % CI 1.01–1.25) (Fig. 3). Other results for selected effectiveness and safety outcomes in three high-risk subgroups were consistent with the findings from the overall sample. After excluding patients with a diagnosis of an indication for anticoagulation other than AF, there was no difference in the risk of thromboembolic events other than stroke between rivaroxaban and dabigatran, but other outcomes were similar to those from the overall sample (Table 3 in the ESM). The HRs of bleeding events did not vary much after recent warfarin-experienced subjects were excluded from the study sample (Table 4 in the ESM). The exclusion of patients with a history of stroke or TIA did not impact our results for the comparative risk of effectiveness outcomes between two anticoagulants (Table 5 in the ESM). Our results were also consistent after the exclusion of patients who used NSAIDs or antiplatelet agents after the index date (Table 6 in the ESM).
Hazard ratios for effectiveness and safety outcomes, by subgroup, treatment, and dose. Hazard ratios were estimated with Cox proportional hazard models with propensity score weighting that controlled for all the covariates listed in the Covariates Section except for the one defining the subgroup. CI confidence interval
4 Discussion
To the best of our knowledge, our study is the first to compare effectiveness and safety outcomes between dabigatran and rivaroxaban, separately by dose, among Medicare patients with AF. Our study yielded two main findings. First, we found no difference in stroke prevention between dabigatran and rivaroxaban; however, rivaroxaban was associated with higher rates of thromboembolic events other than stroke and all-cause mortality than dabigatran. Second, we observed that the risk of major bleeding, gastrointestinal bleeding, and any bleeding events was higher with rivaroxaban than with dabigatran, but there was no difference in the risk of intracranial bleeding between dabigatran and rivaroxaban.
Previous researchers have conducted indirect comparisons of the results from RE-LY and ROCKET-AF, predicting that dabigatran would be associated with a lower combined risk of stroke and systemic embolism than rivaroxaban (HR 1.35; 95 % CI 1.02–1.78), but that the risk of ischemic stroke (HR 1.33; 95 % CI 0.98–1.78) and bleeding (HR 1.12; 95 % CI 0.92–1.37) would be similar with two drugs [8, 9]. We found no difference in the risk of ischemic stroke with two NOACs (HR 1.05; 95 % CI 0.97–1.13), but we observed that the risk of thromboembolic events other than stroke (HR 1.28; 95 % CI 1.14–1.44) and the risk of bleeding (HR 1.32; 95 % CI 1.17–1.50) was higher with rivaroxaban. The differences between our results for the comparative risk of bleeding with two NOACs and those reported in indirect comparisons may be explained by the differences in patient characteristics of subjects enrolled in the two clinical trials [8, 9]. For example, 55 % and 62 % of the subjects enrolled in ROCKET-AF had a prior stroke/TIA and heart failure compared with 20 % and 35 % of those enrolled in RE-LY, respectively [3, 4]. Laliberte et al. [10] used US commercial insurance data to compare the effectiveness and safety of rivaroxaban and warfarin, estimating the annual risk of major bleeding for patients receiving rivaroxaban as 3.3 %. Our estimate for the rate of major bleeding while receiving rivaroxaban 20 mg (5 %) is higher than that reported by Laliberte et al. [10], partially because of the higher prevalence of risk factors for bleeding among our study sample. For instance, 28.6 % of our study participants receiving rivaroxaban 20 mg had a diagnosis of kidney disease compared with only 7.5 % of those included by Laliberte et al. [10]. To the best of our knowledge, only one study has directly compared the risk of bleeding with dabigatran and rivaroxaban. To do so, Sherid et al. [16] used medical records from two community hospitals and found no difference in the risk of bleeding with the two NOACs. However, the sample size in this study was very small (dabigatran = 227, rivaroxaban = 147), which may have prevented the authors from finding significant differences.
Our study is subject to six main limitations. First, propensity score weighting did not adjust for unobserved patient characteristics, such as laboratory test results, because they are not available in Medicare claims data. Thus, some unobserved risk factors for clinical outcomes, such as creatinine clearance, may have been unbalanced between treatment groups. However, we balanced the proportion of patients with chronic kidney disease between treatment groups using propensity score weighting, and we also included this as a covariate in our Cox proportional hazards models. Second, we could not calculate the HAS-BLED risk score, a tool for predicting the risk of bleeding, because data on international normalized ratio (INR) were unavailable [28, 29]. Nevertheless, we balanced all components of HAS-BLED score except for labile INR between treatment groups and also included them as separate covariates in our analytical models. Third, we used 2010–2013 Medicare data, so our study period represents the first 2 years after rivaroxaban entered the US market. Prescribing patterns for NOACs may change over time as prescribers become more familiar with these agents [18, 19]. Fourth, our study did not include apixaban, which was approved in December 2012, because we would not have had a follow-up period long enough to study effectiveness outcomes. As a result, it will be informative to repeat our analyses as newer Medicare Part D data become available and to study the effectiveness and safety of dabigatran and rivaroxaban compared with apixaban. Fifth, we censored patients when they switched anticoagulation treatments or discontinued anticoagulation for >60 days; however, short interruptions of anticoagulation may not have been captured in our analysis. In addition, we observed that the rates of discontinuation and switching during our study period were higher in the dabigatran groups than in the rivaroxaban groups, which may be partially due to the longer follow-up time available for the dabigatran cohorts. Nevertheless, these differences in discontinuation and switching rates should not affect our results because, for each of the outcomes analyzed, we used a time-to-first event analysis. Sixth, claims data do not capture information on patients’ adherence to therapy, which may have been higher in the rivaroxaban groups because of the once-daily regimen. In fact, a recent analysis of US commercial insurance claims data found that patients receiving rivaroxaban were more adherent than patients receiving dabigatran [30]. However, this is not especially concerning because our study aimed to compare effectiveness and safety outcomes under real-world conditions, where adherence to rivaroxaban is likely to be higher. In doing so, we found no difference in the prevention of stroke with two new oral anticoagulants, yet rivaroxaban was associated with a higher risk of bleeding. This implies that despite the twice-daily regimen, dabigatran still presents a better benefit–risk ratio in real-world clinical practice than rivaroxaban.
Rivaroxaban 15 mg and dabigatran 75 mg are indicated in the prevention of stroke or systemic embolism in renally impaired patients with AF; however, we observed that half of the study participants who initiated rivaroxaban 15 mg or dabigatran 75 mg did not have a diagnosis of chronic kidney disease. Although our study did not specifically examine the off-label use of low-dose dabigatran and rivaroxaban, we hypothesize that these low doses of anticoagulants were prescribed off-labelly in 2011–2013 for patients with normal kidney function who did have other risk factors for bleeding, such as hypertension or a history of stroke or bleeding. These prescribing patterns may have been motivated by concerns about severe bleeding events with NOACs, the unavailability of dabigatran 110 mg in the USA, and the lack of an antidote to reverse the anticoagulation effects of rivaroxaban and dabigatran in case of emergency in 2011–2013, the period our study represents. Idarucizumab, the specific antidote for dabigatran, was approved in October 2015 [31]. It will be informative to further characterize this off-label use of low-dose anticoagulants and analyze how it changes over time as clinicians become more familiar with NOACs. In addition, it will be relevant to compare post-hemorrhage outcomes of patients who bled while receiving rivaroxaban and dabigatran in future analyses. These outcomes are likely to differ between the two drugs because, in addition to idarucizumab, hemodialysis can also reverse the effects of dabigatran, and this is not available for rivaroxaban [32]. Evaluating how post-hemorrhage outcomes compare between the two drugs would be particularly relevant for subgroups at high risk of bleeding events, such as patients aged >75 years or with kidney disease [24, 29].
5 Conclusion
We found that dabigatran was superior in safety to rivaroxaban; however, we found no differences in stroke prevention between the two oral anticoagulants. Our findings have important implications for the use of NOACs among patients with AF.
References
Ridgefield CT. Pradaxa prescribing information. Boehringer Ingelheim Pharmaceuticals. 2015. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022512s028lbl.pdf. Accessed 12 Jan 2016.
Titusville NJ. Prescribing information for Xarelto. Janssen Pharmaceuticals, Inc. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022406s012lbl.pdf. Accessed 14 May 2015.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Goodman SG, Wojdyla DM, Piccini JP, White HD, Paolini JF, Nessel CC, et al. Factors associated with major bleeding events: insights from the ROCKET AF trial (rivaroxaban once-daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation). J Am Coll Cardiol. 2014;63(9):891–900.
Prescribing information for Eliquis. New York: Bristol-Myers Squibb Company. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/202155s011lbl.pdf. Accessed 12 Jan 2016.
Prescribing information for Savaysa. Tokyo: Daiichi Sankyo Co. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206316s002lbl.pdf. Accessed 12 Jan 2016.
Mantha S, Ansell J. An indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillation. Thromb Haemost. 2012;108(9):476–84.
Lip GY, Larsen TB, Skjoth F, Rasmussen LH. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J Am Coll Cardiol. 2012;60(8):738–46.
Laliberte F, Cloutier M, Nelson WW, Coleman CI, Pilon D, Olson WH, et al. Real-world comparative effectiveness and safety of rivaroxaban and warfarin in nonvalvular atrial fibrillation patients. Curr Med Res Opin. 2014;30(7):1317–25.
Chang HY, Zhou M, Tang W, Alexander GC, Singh S. Risk of gastrointestinal bleeding associated with oral anticoagulants: population based retrospective cohort study. BMJ. 2015;350:h1585.
Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly medicare patients treated with dabigatran or warfarin for non-valvular atrial fibrillation. Circulation. 2015;131(2):157–64.
Hernandez I, Baik SH, Pinera A, Zhang Y. Risk of bleeding with dabigatran in atrial fibrillation. JAMA Intern Med. 2015;175(1):18–24.
Larsen TB, Rasmussen LH, Skjoth F, Due KM, Callreus T, Rosenzweig M, et al. Efficacy and safety of dabigatran etexilate and warfarin in “real-world” patients with atrial fibrillation: a prospective nationwide cohort study. J Am Coll Cardiol. 2013;61(22):2264–73.
Maura G, Blotiere PO, Bouillon K, Billionnet C, Ricordeau P, Alla F, et al. Comparison of the short-term risk of bleeding and arterial thromboembolic events in nonvalvular atrial fibrillation patients newly treated with dabigatran or rivaroxaban versus vitamin K antagonists: a French nationwide propensity-matched cohort study. Circulation. 2015;132(13):1252–60.
Sherid M, Sifuentes H, Sulaiman S, Samo S, Husein H, Tupper R, et al. Risk of gastrointestinal bleeding with dabigatran: a head-to-head comparative study with rivaroxaban. Digestion. 2014;90(2):137–46.
Liu S, Kim CO, Lucyk SN. Dosage of dabigatran as a risk factor for bleeding in atrial fibrillation. JAMA Intern Med. 2015;175(7):1244–5.
Miyares MA. One-year risk of bleeding with dabigatran in patients with atrial fibrillation: placing real-world results into perspective. JAMA Intern Med. 2015;175(7):1242–3.
Hernandez I, Zhang Y. Risk of bleeding with dabigatran in 2010–2011 Medicare data. JAMA Intern Med. 2015;175(7):1245–7.
Center for Medicare and Medicaid Services. Chronic Conditions Data Warehouse. 27 Chronic Condition Algorithms. 2014. https://www.ccwdata.org/cs/groups/public/documents/document/ccw_condition_categories.pdf. Accessed 8 July 2015.
Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115(21):2689–96.
Thigpen JL, Dillon C, Forster KB, Henault L, Quinn EK, Tripodis Y, et al. Validity of international classification of disease codes to identify ischemic stroke and intracranial hemorrhage among individuals with associated diagnosis of atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2015;8(1):8–14.
Lichtman JH, Jones SB, Watanabe E, Allen NB, Wang Y, Howard VJ, et al. Elderly women have lower rates of stroke, cardiovascular events, and mortality after hospitalization for transient ischemic attack. Stroke. 2009;40(6):2116–22.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke. J Am Med Assoc. 2001;285(22):2864–70.
d’Agostino RB. Tutorial in biostatistics: propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–81.
Cohen J. Statistical power analysis. Cur Dir Psychol Sci. 1992;1(3):98–101.
Center for Medicare and Medicaid Services. Chronic conditions data warehouse (CCW). Medicare beneficiary prevalence for chronic conditions for 2002 through 2011. https://www.ccwdata.org/cs/groups/public/documents/document/wls_ucm1-000774.pdf. Accessed 5 Jan 2015.
Singer DE, Chang Y, Borowsky LH, Fang MC, Pomernacki NK, Udaltsova N, et al. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J Am Heart Assoc. 2013;2(3):000250.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
McHorney CA, Crivera C, Laliberte F, Nelson WW, Germain G, Bookhart B, et al. Adherence to non-vitamin-K-antagonist oral anticoagulant medications based on the Pharmacy Quality Alliance measure. Curr Med Res Opin. 2015;31(12):2167–73.
Pollack CV Jr, Reilly PA, Bernstein R, Dubiel R, Eikelboom J, Glund S, et al. Design and rationale for RE-VERSE AD: A phase 3 study of idarucizumab, a specific reversal agent for dabigatran. Thromb Haemost. 2015;114(1):198–205.
Fawole A, Daw HA, Crowther MA. Practical management of bleeding due to the anticoagulants dabigatran, rivaroxaban, and apixaban. Cleve Clin J Med. 2013;80(7):443–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors acknowledge funding from the Commonwealth Fund (Grants 20150380 and 20130660), the Agency for Healthcare Research and Quality (No. R01 HS018657), and from the National Institute of Mental Health (No. R21 MH100721). IH has received a scholarship from “La Caixa” Foundation (Spain).
Conflict of interest
IH and YZ have no conflicts of interest that are directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hernandez, I., Zhang, Y. Comparing Stroke and Bleeding with Rivaroxaban and Dabigatran in Atrial Fibrillation: Analysis of the US Medicare Part D Data. Am J Cardiovasc Drugs 17, 37–47 (2017). https://doi.org/10.1007/s40256-016-0189-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-016-0189-9