Abstract
Especially during thoracic surgery, anesthesiologists have to cope with both the drastic alteration of normal pulmonary physiology and the mechanical stress on the lung tissue induced by ventilation. These problems result from the total collapse of the lung being operated on and the partial collapse of the ventilated other lung. In addition, technical factors inherent to thoracic surgery and the patient’s condition potentiate such adverse effects. Traditional ventilatory settings described for thoracic surgery have not led to a decrease in the incidence of hypoxemia or perioperative atelectasis. However, lung recruitment maneuvers and ventilatory strategies are aimed at resolving lung collapse in mechanically ventilated patients, improving lung function, and decreasing the rate of post-operative pulmonary complications directly related to lung collapse. This article summarizes recent evidence for the role that lung recruitment maneuvers play during one-lung ventilation anesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One-lung ventilation (OLV)—a technique that excludes the operated lung from ventilation—is one of the most challenging procedures for anesthesiologists. OLV must assure an optimal surgical field while at the same time maintaining an adequate gas exchange and minimizing the mechanical injury to the ventilated lung [1, 2]. Individualized positive-pressure mechanical ventilation is the key to accomplishing the above goals but very much depends on how well the operated non-ventilated lung is isolated from the other, ventilated lung.Footnote 1 However, mechanical ventilation under these circumstances is a two-edged sword: it is life-saving and injurious at the same time. To date, it is well known that ventilator-induced lung injury (VILI) has a negative impact on patient outcome [2–5, 6•, 7••].
Increasing evidence suggests that mechanical ventilation induces VILI even in patients with healthy lungs, such as during general anesthesia [5, 6•, 7••]. The origin of VILI resides in the high stress that mechanical breaths induce within collapsed lung zones and the high strain on normally ventilated areas which receive excessive ventilation [5, 8]. VILI is clearly associated with post-operative complications such as atelectasis, hypoxemia, pneumonia, or acute respiratory distress syndrome (ARDS) [4, 7••]. VILI has an even higher adverse impact on critically ill patients undergoing complex surgery like thoracic interventions performed under OLV [2, 4].
This new knowledge calls for the intra-operative use of protective ventilatory strategies based on low tidal volume ventilation and limited airway pressures [5, 6•, 7••]. However, the main shortcoming of such protective concepts is that the root cause of lung injury—mechanical ventilation of a partially collapsed lung—although attenuated is not totally abolished. Therefore, an optional ventilator treatment necessarily consists of a deliberate combination of the above protective ventilation with a lung recruitment maneuver (RM) [9, 10••].
RMs are ventilatory strategies aimed at restoring a normal functional residual capacity even during adverse circumstances such as thoracic anesthesia [11–13]. RM re-aerate atelectasis and areas of airway closure thereby increasing the alveolar surface for gas exchange and decreasing the mechanical stresses which are the origin of VILI.
The objective of this paper is to analyze the impact that RMs have on gas exchange and lung injury during thoracic surgery with OLV.
Gas Exchange During Thoracic Surgeries with One-Lung Ventilation
The mechanisms leading to an impaired gas exchange during OLV are depicted in Fig. 1. The unfavorable ratios of local ventilation to perfusion (V/Q) created by both the total collapse of the operated/non-ventilated lung and the different states of aeration and perfusion in the ventilated lung lead to inefficiencies of gas exchange, witnessed clinically as hypoxemia and hypercapnia of different degrees [14, 15].
Schematic representation of the mechanisms behind deficiencies in exchange and lung injury in thoracic surgeries with one-lung ventilation. In thoracic surgery, the operated lung is totally collapsed and the ventilated lung becomes compressed by abdominal viscera through a dysfunctional diaphragm, by the mediastinal weight, and by the surgeon’s activity (arrows). Causes of a deterioration of gas exchange are schematically depicted on the left. These range from pulmonary areas without ventilation (shunt = V/Q 0) to overinflated areas (dead space = V/Q ∞). Main potential causes of lung injury during thoracic surgeries are listed on the right
The incidence of hypoxemia during OLV ranges from 1 to 24 % and depends, among other factors, on the correct placement of the double-lumen tube, the use of bronchoscopes, the patient’s underlying disease, the body position during surgery, the kind of surgery performed, the ventilatory settings used, and anesthesiologist’s experience in thoracic surgery [16, 17]. Originally, shunting through the non-ventilated lung was thought to be the main reason for hypoxemia [18], although a considerable part of the total shunting also results from the perfusion of atelectatic areas within the ventilated lung [14, 19]. Beyond pure atelectasis, areas with a low V/Q due to airway collapse also contribute significantly to the deficiencies in arterial oxygenation typically seen during OLV [20].
Hypercapnia is another common problem of gas exchange observed in 10–30 % of all thoracic surgeries [21]. Nowadays, the incidence of hypercapnia is increasing due to the use of low tidal volumes for reasons of lung protection. Hypercapnia depends on the same factors already described above for hypoxemia but with another confounding factor, the re-inhalation of CO2 from the large instrumental dead space of typical double-lumen tubes. Although hypercapnia induces respiratory acidosis, a slight increase in PaCO2 might even be beneficial for most patients, as it is known to augment the hypoxic pulmonary vasoconstriction reflex, to increase oxygen delivery to tissues, to protect the lungs from injury, and to decrease the hospital length of stay after major surgery [22].
Lung Injury in Thoracic Surgeries with One-Lung Ventilation
A non-cardiogenic protein-rich inflammatory edema is characteristic for the injured alveolar-capillary membrane after thoracic surgery with OLV [23]. The mechanisms leading to this lung injury are complex and are present in both the ventilated and the non-ventilated lung (Fig. 1; Table 1). The synergistic negative effects of these damaging mechanisms support the multiple hit theory which tries to link the local inflammation process within the lungs with the systemic inflammatory response [24]. Both these inflammations can potentiate each other and may even lead to an ARDS in 1–7 % of lung resections [2, 3].
These multiple insults affect the lungs in different ways and to different degrees. The operated lung has to cope with an injury that is related to the extent of the surgical trauma [25, 26]. In general, the degree of lung injury is proportional to the surgical aggression which has already been described for all kind of thoracic procedures including minimally invasive ones. Thus, Yim et al. [25] demonstrated that video-assisted surgery is related to lower plasmatic cytokine concentrations when compared to open surgeries. More invasive surgeries for cancer may directly affect the pulmonary lymphatic drainage which aggravates non-cardiogenic edema formation.
Another important mechanism of lung injury during OLV is the ischemia of the non-ventilated lung and its sequential reperfusion when ventilation is restored [27]. Hyperoxia in the ischemic operated lung at the onset of ventilation leads to an increase in reactive oxygen species, in cell damage, and in local leukocyte infiltration. The generation of free oxygen radicals is proportional to the duration of OLV [27–29].
The re-expansion of the operated lung at the end of surgery—a kind of lung recruitment “maneuver” commonly performed by manual bagging—could be an additional cause of lung injury beyond the one caused by ischemia reperfusion. There are a few reports showing that RMs enhance the expression of inflammatory mediators [30, 31, 32••, 33]. However, the potentially deleterious effect of RMs is related to the way they are performed and especially to their timing, the driving pressures, and volumes applied [9, 34••]. There is evidence that “fast” lung recruitments induced local inflammation in an experimental model of ARDS. Recruitment maneuvers performed as sustained inflation (SI) typically increase airway pressures and lung volumes abruptly, and by their non-physiological nature create stress on the fragile lung tissue. Such stresses can be minimized by applying cyclic step-wise RMs [30, 31, 32••, 33, 34••].
The local hypoxia observed in atelectatic areas also induces a mild lung injury with an inflammatory response mediated by macrophages [35]. Duggan et al. [36] described histological damage and increased lung permeability in atelectatic areas of rat lungs, which are attenuated by oxygen.
The chance of developing lung injury after major surgery increases with a positive fluid balance [37]. This is also true for thoracic surgery as described by Licker et al. [38], who found that a positive fluid balance was an independent risk factor for developing ARDS. A positive fluid balance augments edema formation in previously injured lungs due to both an increased hydrostatic capillary pressure and a decreased plasmatic oncotic pressure. In addition, the endothelial glycocalix—an internal protective layer that prevents plasmatic proteins and water from leaving the vascular system—can be damaged in thoracic surgery by fluid overload as well as by lung trauma, ischemia reperfusion, local hypoxia, and inflammatory response [39].
Transfusion-related lung injury is a known entity that can especially affect critically ill patients undergoing thoracic surgery. Even if euvolemia is maintained, blood products are known to cause neutrophil sequestration and activation within the lungs [40].
A sudden increase in pulmonary blood flow with hyperperfusion of the ventilated lung during OLV can damage the lungs by a capillary stress failure [41]. Temporary hyperperfusion is commonly observed in thoracic surgery [20], especially during the clamping and de-clamping of the pulmonary artery and with the abuse of inotropic and vasoactive drugs. López-Aguilar et al. [41] determined the role that capillary blood flow and pressure play in inducing lung damage. They found in an animal model that high pulmonary capillary blood flow and pressure increased the score of histological alveolar and endothelial injury when compared to low flow and pressure conditions.
The main mechanism of lung damage in the ventilated lung is the mechanical injury that the ventilator induces—in the true sense of the term ventilator-induced lung injury. However, the concept of VILI has changed over the last 30 years [9]. Initially, the main causes of VILI were thought to be barotrauma and volutrauma, and thus the damage caused by high airway pressures and VTs, respectively. Despite the fact that airway pressures and tidal volumes have progressively been reduced over past decades, to date, VILI remains an important issue. It is now considered to be mainly due to tidal recruitment and tidal overdistension [42–44]. Tidal recruitment refers to the cyclic opening and closing of unstable airways and alveoli during a breathing cycle. This repetitive opening and closing of lung units induces shear stress within the boundary between stable and unstable units. Such damage can thus occur whenever ventilated lungs are partially collapsed. Tidal overdistension, on the other hand, can be observed whenever excessive inspiratory flows are directed primarily towards normally ventilated areas. Such airflow strains these areas beyond their elastic limit.
Ventilatory Management During OLV Anesthesia
Protective Ventilation
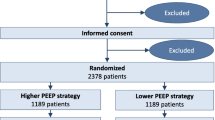
Radical changes in the way patients with acute lung injury are ventilated in intensive care medicine have been observed during the last years. It is now an accepted fact that mortality and ventilator-free days in ARDS patients are lower if they are ventilated with 6 rather than 12 mL/kg predicted body weight (31 vs. 40 %, respectively; p = 0.07) [45]. In many institutions throughout the world, such protective ventilation with low VT and plateau pressures with an associated permissive hypercapnea and the use of PEEP are considered standard treatment for ARDS patients.
The legacy of such novel insights was delayed in the anesthesia world since the traditional opinion was that “healthy” lungs do not need any special attention. However, new evidence unequivocally shows that even healthy lungs can be damaged by inadequate mechanical ventilation. Thus, Gagic et al. reported that 24 % of 332 patients without ARDS who received mechanical ventilation in the ICU developed acute lung injury after a few days. The main risk factor associated with such lung injury was the size of the VT applied (odds ratio 1.3 for each mL above 6 mL/kg of predicted body weight; p < 0.001) [5]. Similarly, Serpa Neto et al. [6•] in a meta-analysis of 2.822 ICU patients without ARDS showed a decrease in lung injury, pulmonary infection, hospital length of stay, and mortality with low VT ventilation. Comparable findings were observed in the operating theatre in patients with healthy lungs. In a recent meta-analysis including 1.669 anesthetized patients, Hemmes et al. [7••] showed that low VT at high PEEP ventilation (with and without RM) decreased the risk of lung injury, atelectasis, and pulmonary infection compared with high VT ventilation at low PEEP.
Of all ventilated lungs, those treated with OLV during thoracic surgeries are the ones most prone to VILI, mainly because the traditional ventilatory strategies still commonly used in clinical practice are not only “non-protective” but must be considered potentially injurious, as they employ relatively high VTs for just one single lung together with high FiO2 and low or no PEEP at all. Thus, studies could show a pulmonary production of pro-inflammatory cytokines during OLV [46, 47], which was more pronounced in the ventilated than in the operated lung [48••, 49]. This local inflammation in thoracic surgery was associated with a high incidence of postoperative pulmonary complications [50].
The latest evidence suggests that protective ventilation decreases VILI during OLV. Schilling et al. [51] demonstrated that ventilation during OLV with low VT (5 mL/kg) compared to high VT (10 mL/kg) partially decreases the pulmonary expression of pro-inflammatory cytokines and neutrophil infiltration. Similarly, Michelet et al. [52] found that patients undergoing esophagectomies with OLV who were ventilated with VT 5 mL/kg at 5 cm H2O of PEEP showed lower cytokine levels than those ventilated with a VT of 9 mL/kg without PEEP.
The attenuation of the pulmonary inflammatory response by using protective ventilation during OLV has important positive clinical repercussions. Protective ventilation during OLV compared with high VT and ZEEP showed fewer postoperative pulmonary dysfunctions and a more satisfactory gas exchange [53••]. In a retrospective analysis, Licker et al. [2] showed that ventilation with VT of 5 but not 7 mL/kg during OLV was associated with a lower incidence of atelectasis and acute lung injury, fewer admissions to the ICU, and a shorter hospital stay.
Although ventilation with low VT, plateau pressures, and PEEP decreases the pulmonary inflammatory response, such a ventilatory strategy cannot totally abolish VILI during OLV [48••, 49]. This is because protective ventilation inherently promotes lung collapse due to the use of low VT and high FiO2 [54], and thus the damaging effects of tidal recruitment can still act in the partially collapsed ventilated lung.
Recruitment Maneuvers and the Open Lung Concept
Lachmann proposed another ventilatory strategy for ARDS patients, which consists of two main components: (1) an active opening up of collapsed lung units by a RM, and (2) the use of sufficiently high levels of PEEP to keep lung units open [55]. The rationale of any RM is to restore the FRC in order to normalize lung function and to avoid the mechanisms of VILI. Amato et al. [56] described an improved outcome of patients with ARDS when protective ventilation was combined with a RM.
The adoption of such a kind of protective ventilation in the field of anesthesia was delayed compared to intensive care medicine. Already in 1993, Hedenstierna’s group in Sweden had described the patho-physiology around lung collapse and the physiological basis of sustained inflations—then called vital capacity maneuvers [11]. Shortly thereafter, our group demonstrated the beneficial clinical effect of a cycling RM on anesthesia-induced atelectasis [12, 13]. RM has been demonstrated to be safe in a wide variety of species, patients, and surgical procedures, including thoracic ones performed under OLV [13, 57••].
Information about RMs as potential triggers of the local inflammatory response or VILI is scarce. Only a few experimental and clinical studies provide first hints. On the one hand, experimental reports showed an increased expression of inflammatory mediators [30, 31, 32••, 33] with the SI-type RM but not with the cyclic type of RM (see below). On the other hand, additional experimental and clinical data showed that RM did not affect or even decreased the inflammatory response. Schilling et al. [57••] recently demonstrated that repetitive RMs did not induce any significant pro-inflammatory responses in healthy pigs undergoing OLV anesthesia. These data fit with clinical studies which showed that RM had no effect on the level of systemic inflammatory cytokines in critically ill ventilated patients with and without ARDS [58, 59]. Other experimental studies even showed a decreased inflammatory response when using RMs [60–62]. The cytokine attenuation during a RM could be due to the abolition of VILI as demonstrated by Kozian et al. [63••]. The authors showed that a RM combined with protective ventilation decreased tidal recruitment on CT images when compared to high VT ventilation in pigs undergoing OLV. Similar findings were obtained in cardiac surgery patients. Reis Miranda et al. [64] demonstrated that a RM associated with low VT and high PEEP decreased cytokines release as compared to a ventilation at VT 6–8 mL/kg and 5 cm H2O of PEEP.
These positive effects of RM on VILI could be responsible for the decreased rate of post-operative complications in anesthetized patients. A recent meta-analysis showed that the risk of lung injury, atelectasis, and pulmonary infection decreased with protective ventilation during anesthesia [7••]. However, this analysis included studies with and without RM and, therefore, a final conclusion in favor of RM cannot be drawn. Recently, Futier et al. [10••] described that protective ventilation combined with RM improved clinical outcomes and reduced health care utilization in patients undergoing major abdominal surgery. Taking all this encouraging evidence together, it seem that cycling of RMs have a complementary protective effect on the lung tissue not only in thoracic surgery with OLV but in all mechanically ventilated patients.
The management of OLV has changed over the last decades. In the early days of thoracic anesthesia, awareness and knowledge about VILI were rare and, thus, ventilation with high VT and FiO2 without PEEP was promoted [18]. Later on, reduced tidal volumes and PEEP of no more than 5 cm H2O became popular, while RM was still considered a rescue intervention in case of severe hypoxemia [65].
RM can eliminate approx. 1/3 of the total venous admixture that comes from the ventilated lungs [19]. Restoring the FRC of the ventilated lung by actively recruiting it improves gas exchange, although it will never be entirely normalized because the second lung is totally collapsed and not ventilated at all. However, in nearly all cases, maintaining the ventilated lung in a perfectly open condition suffices to prevent hypoxemia and to avoid complementary CPAP in the operated lung. According to our group’s experience, RM in conjunction with the use of 4 mL/kg VT provides an optimal arterial oxygenation at a slight hypercapnea (personal unpublished data). RM with sufficient PEEP should avoid tidal recruitment because the ventilated lung is no longer collapsed. At the same time, they minimize tidal overdistension because the inspiratory flow is more homogeneously distributed within the more compliant lung.
A summary of the main published clinical studies on the use of RM in thoracic surgeries is given in Table 2. The first clinical report of a lung recruitment procedure in thoracic surgery was in 2002 [19]. A cycling RM was successfully applied and the clinical results during OLV were similar to the one already described in other kinds of surgery: improved arterial oxygenation and respiratory system compliance at decreased dead spaces [19, 66]. Subsequent studies confirmed these results. Cinella et al. [67] performed a RM in the ventilated lung and showed a higher PaO2 and a reduced respiratory elastance. Garutti et al. [68] showed similar effects on arterial oxygenation after RM in pulmonary resections with OLV lasting longer than 1 h. Park et al. [69] also confirmed the benefits of a RM performed before OLV on PaO2 and lung mechanics. Unzueta et al. described a reduction in alveolar dead space and a better PaO2 during OLV after RM [70••].
Some questions remain regarding the way RM should be performed. One of the key questions is related to the level of recruitment pressures recommended. Details of published RMs before or during OLV are summarized in Table 2. Since most of the lungs during OLV may be considered “healthy” with respect to their recruitability, they usually require no more than 40 cm H2O to be fully expanded. In order to limit the shear stresses between open and closed lung units during the cycling recruitment, a PEEP of 20 cm H2O appears appropriate.
Another question is related to the way such pressures are best delivered to the lungs. Thus, inappropriate timing is an important factor associated with negative RM effects. Alveolar recruitment per se is a rapid phenomenon which happens quickly during the intervention. However, shear stresses within the fragile lung tissue and hemodynamic side effects are mainly associated with “fast” RM and not with “slow” cycling RM [33]. This way, one-step SI maneuvers are more harmful than cycling step-wise RMs because SIs abruptly change pressures and volumes within lungs [30, 31, 32••]. Riva et al. [30] showed in an experimental model of ARDS that a slow RM caused less stress for the lung tissue than a fast RM. In another experimental study, Silva et al. [32••] found that SI showed more hyperinflation and activation of pro-inflammatory and pro-fibrogenic mediators than cycling RMs. Based on these data, Marini recently suggested that RMs of the SI-type in ARDS patients must be eradicated from clinical practice and replaced by slow, step-wise RMs [34••]. It is only logical that such advice from the ICU world should also be followed in thoracic anesthesia because the risk for VILI and non-cardiogenic inflammatory edema—although of different magnitude and clinical repercussions—is present in all mechanically ventilated patients irrespective of the reason for such ventilator treatment.
An important issue is the duration of the application of high airway pressures needed to reach an optimal therapeutic effect. The time required is proportional to the lung condition: it is as short as a few seconds in healthy lungs and increases up to 2–5 min in ARDS patients [9]. Therefore, 10 breaths at highest recruitment pressure should be enough to open up the lungs during OLV anesthesia (Table 2).
Furthermore, the question of how many RM should be used during thoracic surgery needs to be answered. The answer depends on the details of the surgery and should be planned strategically. Some authors apply RMs during two lung ventilation and others only during OLV (Table 2). An initial RM must be performed immediately after anesthesia induction before OLV to make the patients benefit from the positive RM effects during the entire anesthesia time. In critically ill patients, in whom hemodynamic side effects of the RM are expected, such a maneuver can be applied during OLV, because one report demonstrated that a RM on the ventilated lung alone was hemodynamically well tolerated [68]. However, in general, the hemodynamic tolerance is related to a patient’s preload status and is rarely a problem in normovolemic patients [9, 13, 71].
It must be emphasized that, in most cases, one single maneuver is enough to expand the lungs and to keep the lungs “open” during the entire anesthesia time provided sufficient PEEP is used [9, 13]. A second RM (or even more RMs) becomes necessary whenever the operated lung must be re-expanded, which is usually the case only once at the end of surgery. Following the reasoning described in this paper, a controlled and step-wise increase in lung volume and airway pressure performed using a ventilator should be safer than the traditional manual re-expansions with the anesthesia bag. A manual RM cannot control timing, volumes, or pressures and could thus be potentially harmful for the lungs [30, 31, 32••, 33, 34••].
The number of RMs needed to be performed in thoracic surgery also depends on how efficient such maneuvers are and on the level of PEEP chosen. The level of PEEP used after a RM must exceed the lung’s closing pressure to keep the lungs “open” and free from collapse [9, 13]. Most studies conclude that RM effects are self-limited, and therefore RMs must be performed repetitively. However, according to Young–Laplace’s law and our own experience, lung re-collapse after RM can only occur if the pressure within the lung is insufficient to keep them expanded. In other words, PEEP plays a central role in keeping the lungs expanded during the surgery. While sufficient PEEP is essential, it must be taken into account that too high levels of PEEP overdistend the ventilated lung and will increase its resistance to blood flow, which in turn shifts blood flow towards the shunting non-ventilated lung. As the lung’s closing pressure varies among patients, it must be selected carefully to avoid de-recruitment. The optimum PEEP after RM is very difficult to determine at the bedside. We suggest using higher PEEP levels than the ones typically recommended for OLV (0–5 cm H2O). In a recent study, Ferrando et al. [72] have determined in 15 patients that the optimum PEEP after a RM for OLV varies from 6 to 12 cm H2O (mean 10 ± 2 cm H2O). These personalized levels of PEEP improved arterial oxygenation and decreased dead space compared to patients receiving a RM but only 5 cm H2O of PEEP.
Conclusions
The paradigm of lung recruitment during anesthesia has shifted away from strategies primarily devised to improve gas exchange by re-aerating hypoventilated and collapsed areas towards ventilatory maneuvers that are aimed at protecting the lungs from VILI by reducing tidal recruitment and tidal overdistension. This is particularly important in thoracic surgery in which the risk for severe derangements of gas exchange and lung injury is particularly high. VILI is one of the causes of lung injury on which anesthesiologists can have a positive therapeutic impact. Beyond the clear benefits of alveolar recruitment maneuvers on VILI, its impact on patient outcome after thoracic surgery is as yet unknown and warrants further clinical studies.
Notes
Nowadays, many thoracic surgeries are performed with different body positioning besides the classical lateral decubitus. Therefore, in this paper, we write about ventilated or non-ventilated lungs instead dependent or non-dependent ones.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Brodsky JB. The evolution of thoracic anesthesia. Thorac Surg Clin. 2005;15:1–10.
Licker M, Fauconnet P, Villiger Y, Tschopp JM. Acute lung injury and outcomes after thoracic surgery. Curr Opin Anaesthesiol. 2009;22:61–7.
Jeon K, Yoon JW, Suh GY, et al. Risk factors for post-pneumonectomy acute lung injury/acute respiratory distress syndrome in primary lung cancer patients. Anaesth Intensive Care. 2009;37:14–9.
Tusman G, Böhm SH, Warner DO, Sprung J. Atelectasis and perioperative pulmonary complications in high-risk patients. Curr Opin Anaesthesiol. 2012;25:1–10.
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sauver JL, Lymp JF, Afessa B, Hubmayr RD. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32:1817–24.
• Serpa Neto A, Oliveira Cardoso S, Manetta JA, Moura Pereyra VG, Crepaldi Espósito D, Oliveira M, Toledo Damasceno MC, Schultz MJ. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA 2012;308:1651–9. This meta-analysis showed that protective ventilation improved outcome in patients without ARDS.
•• Hemmes SNT, SerpaNeto A, Schultz MJ. Intraoperative ventilator strategies to prevent postoperative pulmonary complications: a meta-analysis. Curr Opin Anesthesiol 2013;26:126–33. Lung protective ventilation during anesthesia decreases postoperative pulmonary complications.
Pavone LA, Albert S, Carney D, Gatto LA, Halter JM, Nieman GF. Injurious mechanical ventilation in the normal lung causes a progressive pathologic change in dynamic alveolar mechanics. Crit Care. 2007;11:R64.
Tusman G, Bohm SH, Suarez-Sipmann F. Alveolar recruitment during mechanical ventilation—where are we in 2013? Trends Anesth Crit Care. 2013;3:238–45.
•• Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low tidal volume ventilation in abdominal surgery. N Engl J Med 2013;369:428–37. Protective ventilation with recruitment maneuvers improved clinical outcome and reduced health care utilization in high-risk patients.
Rothen HU, Sporre B, Wegenius G, et al. Reexpansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth. 1993;71:788–95.
Tusman G, Böhm SH, Vazquez de Anda GF, do Campo JL, Lachmann B. Alveolar recruitment strategy improves arterial oxygenation during general anaesthesia. Br J Anaesth. 1999;82:8–13.
Tusman G, Bohm SH. Prevention and reversal of lung collapse during the intra-operative period. Best Prac Res Clin Anaesth. 2010;24:183–97.
Klingstedt C, Hedenstierna G, Baehrendtz S, Lundqvist H, Strandberg A, Tockis L, Brismar B. Ventilation-perfusion relationships and atelectasis formation in the supine and lateral positions during conventional mechanical and differential ventilation. Acta Anaesthesiol Scand. 1990;34:421–9.
Levin AI, Coetzee JF, Coetzee A. Arterial oxygenation and one-lung anesthesia. Curr Opin Anaesthesiol. 2008;21:28–36.
Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation. Prediction, prevention and treatment. Anesthesiology. 2009;110:1402–11.
Ishikawa S, Lohser J. One-lung ventilation and arterial oxygenation. Curr Opin Anesth. 2011;24:24–31.
Benumof JL. One-lung ventilation and hypoxic pulmonary vasoconstriction: implications for anesthetic management. Anesth Analg. 1985;64:821–33.
Tusman G, Bohm SH, Melkun F, Staltari D, Quinzio C, Nador C, Turchetto E. Alveolar recruitment strategy increases arterial oxygenation during one-lung ventilation. Ann Thorac Surg. 2002;73:1204–9.
Kozian A, Schilling T, Schütze H, Heres F, Hachenberg T, Hedenstierna G. Lung computed tomography density distribution in a porcine model of one-lung ventilation. Br J Anaesth. 2009;102:551–60.
Akca O, Doufas AG, Morioka N, et al. Hypercapnia improves tissue oxygenation. Anesthesiology. 2002;97:801–6.
Wax DB, Lin HM, Hossain S, Porter SB. Intraoperative carbon dioxide management and outcomes. Eur J Anaesthesiol. 2010;27:819–23.
Jordan S, Mitchell JA, Quilan GJ, Goldstraw P, Evans TW. The pathogenesis of lung injury following pulmonary resection. Eur Respir J. 2000;15:790–9.
Schultz MJ, Haitsma JJ, Slutsky AS, Gagic O. What tidal volumes should be used in patients without acute lung injury? Anesthesiology. 2007;106:1226–31.
Yim APC, Wan S, Wai T, Arifi AA. VATS lobectomy reduces cytokine responses compared with conventional surgery. Ann Thorac Surg. 2000;70:243–7.
Whitson BA, D’Cunha J, Andrade RS, et al. Thoracoscopy versus thoracotomy approaches to lobectomy: differential impairment of cellular immunity. Ann Thorac Surg. 2008;86:1735–44.
De Perrot M, Liu M, Waddel TK, Keshavjee S. Ischemia-reperfusion induced lung injury. Am J Respir Crit Care Med. 2003;167:490–511.
Cheng YJ, Chan KC, Chien CT, Sun WZ, Lin CJ. Oxidative stress during 1-lung ventilation. J Thorac Cardiovasc Surg. 2006;132:513–8.
Misthos P, Katsaragakis S, Milingos N, et al. Postresectional pulmonary oxidative stress in lung cancer patients. The role of one-lung ventilation. Eur J Cardiothorac Surg. 2005;27:370–83.
Riva DR, Contador RS, Baez-Garcia CSN, Xisto DG, Cagido VR, Martini SV, Morales MM, Rocco PRM, Faffe DS, Zin WA. Recruitment maneuver: RAMP versus CPAP pressure profile in a model of acute lung injury. Respir Physiol Neurobiol. 2009;169:62–8.
Rzezinski AF, Oliveira GP, Santiago VR, Santos RS, Ornellas DS, Morales MM, et al. Prolonged recruitment manoeuvre improves lung function with less ultrastructural damage in experimental mild acute lung injury. Respir Physiol Neurobiol. 2009;169:271–81.
•• Silva PL, Moraes L, Santos RS, Samary C, Ornellas DS, Saddy F, Capelozzi VL, Pelosi P, Marini JJ, Gama de Abreu M, Rocco PR. Impact of pressure profile and duration of recruitment maneuvers on morphofunctional and biochemical variables in experimental lung injury. Crit Care Med 2011;39:1074–81. Longer duration RM with slower airway pressure increment minimized the biological impact on lungs.
Arnal JM, Paquet J, Wysocki M, Demory D, Donati S, Granier I, Corno G, Durand-Gasselin J. Optimal duration of a sustained inflation recruitment maneuver in ARDS patients. Intensive Care Med. 2011;37:1588–94.
•• Marini JJ. Recruitment by sustained inflation: time for a change. Intensive Care Med 2011; 37:1572–4. This editorial suggests that sustained inflation RM must be deleted from the clinical practice.
Madjdpour C, Jewell UR, Kneller S, et al. Decreased alveolar oxygen induces lung inflammation. Am J Physiol. 2003;284:L360–7.
Duggan M, McNamara PJ, Engelberts D, et al. Oxygen attenuates atelectasis-induced injury in the in vivo rat lung. Anesthesiology. 2005;103:522–31.
Hughes CG, Weavind L, Banerjee A, Mercaldo ND, Schildcrout JS, Pandharipande PP. Intraoperative risk factors for acute respiratory distress syndrome in critically ill patients. Anesth Analg. 2010;111:464–7.
Licker M, de Perrot M, Spiliopoulos A, Robert J, Diaper J, Chevalley C, Tschopp JM. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth Analg. 2003;97:1558–65.
Chappel D, Jacob M, Hofmann-Kiefer K, Bruegger D, Rehm M, Conzen P, Welsch U, Becker BF. Hydrocortisone preserves the vascular barrier by protecting the endothelial glycocalyx. Anesthesiology. 2007;107:776–84.
Triulzi DJ. Transfusion-related acute lung injury: current concepts for the clinician. Anesth Analg. 2009;108:770–6.
López-Aguilar J, Piacentini E, Villagrá A, Murias G, Pascotto S, Saenz-Valiente A, Fernandez-Segoviano P, Hotchkiss JR, Blanch L. Contributions of vascular flow and pulmonary capillary pressure to ventilator-induced lung injury. Crit Care Med. 2006;34:1106–12.
Protti A, Andreis DT, Monti M, et al. Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med. 2013;41:1046–55.
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, Gandini G, Herrmann P, Mascia L, Quintel M, Slutsky AS, Gattinoni L, Ranieri VM. Tidal hyperinflation during low tidal volumen ventilation in acute respiratory distress síndrome. Am J Respir Crit Care Med. 2007;175:160–6.
Bellani G, Guerra L, Musch G, Zanella A, Patroniti N, Mauri T, Messa C, Pesenti A. Lung regional metabolic activity and gas volumen changes induced by tidal ventilation in patients with acute lung injury. Am J Respir Crit Care Med. 2011;183:1193–9.
The National Heart, Lung, and blood Institute ARDS Clinical Trials Network. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8.
Sato N, Koedo K, Kimura Y, et al. Cytokines profile of serum and bronchoalveolar lavage fluids following thoracic esophageal cancer surgery. Eur Surg Res. 2001;33:279–84.
Abe T, Oka M, Tangoku A, et al. Interleukin-6 production in lung tissue after transthoracic esophagectomy. J Am Coll Surg. 2001;192:322–9.
•• Zingg U, Forberger J, Frey DM, Esterman AJ, Oertli D, Beck-Schimmer B, Zollinger A. Inflammatory response in ventilated left and collapsed right lungs, serum and pleural fluid, in transthoracic esophagectomy for cancer. Eur Cytokine Netw 2010;21:50–7. This study showed that VILI in the ventilated lung caused more cytokines release than that observed in the operated lung in patients undergoing OLV.
Sugasawa Y, Yamaguchi K, Kumakura S, Murakami T, Kugimiya T, Suzuki K, Nagaoka I, Inada E. The effect of one lung ventilation upon pulmonary inflammatory responses during lung resection. J Anesth. 2011;25:170–7.
Fernandez-Perez ER, Keegan MT, Brown DR, Hubmayr RD, Gagic O. Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Anesthesiology. 2006;105:14–8.
Schilling T, Kozian A, Huth C, Bühling F, Kretzschmar M, Welte T, Hachenberg T. The pulmonary immune effects of mechanical ventilation in patients undergoing thoracic surgery. Anesth Analg. 2005;101:957–65.
Michelet P, D’Juorno XB, Roch A, Doddoli C, Marin V, Papazian L, et al. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology. 2006;105:911–9.
•• Yang M, Ahn HJ, Kim K, Kim JA, Yi CA, Kim MJ, Kim HJ. Does a protective ventilation strategy reduce the risk of pulmonary complications after lung cancer surgery? A randomized controlled trial. Chest 2011;139:530–7. This study showed that the application of low VT and PEEP during OLV was related to lower incidence of postoperative dysfunction than non-protective ventilatory settings.
Putensen C, Wrigge H. Tidal volumes in patients with normal lungs: one for all or the less the better? Anesthesiology. 2007;106:1085–7.
Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18:319–21.
Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi Filho G, Kairalla RA, Deheinzelin D, Munoz C, Olivera R, Takagaki T, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54.
•• Schilling T, Kretzschmar M, Hachenberg T, Hedenstierna G, Kozian A. The immune response to one-lung ventilation is not affected by repeated alveolar recruitment maneuvers in pigs. Minerva Anestesiol 2013;79:590–603. Repetitive recruitment maneuvers did not induce a local proinflammatory effect.
Puls A, Pollok-Kopp B, Wrigge H, Quintel M, Neumann P. Effects of a single-lung recruitment maneuver on the systemic release of inflammatory mediators. Intensive Care Med. 2006;32:1080–5.
Talmor D, Sarge T, Legedza A, O‘Donnel CR, Ritz R, Loring SH, Malthotra A. Cytokine release following recruitment maneuvers. Chest. 2007;132:1434–9.
Ko SC, Zhang H, Haitsma JJ, et al. Effects of PEEP levels following repeated recruitment maneuvers on ventilator-induced lung injury. Acta Anaesth Scand. 2008;52:514–21.
Reiss LK, Kowallik A, Uhlig S. Recurrent recruitment maneouvres improve lung mechanics and minimize lung injury during mechanical ventilation of healthy mice. PLoS ONE. 2011;6:e24527. doi:10.1371.
Van Kaam AH, Dik WA, Haitsma JJ, de Jaegere A, Naber BA, Van Aalderen WM, Kok JH, Lachmann B. Application of the open lung concept during positive-pressure ventilation reduces pulmonary inflammation in new-born piglets. Biol Neonate. 2003;83:273–80.
•• Kozian A, Schilling T, Schütze H, Senturk M, Hachemberg T, Hedenstierna G. Ventilatory protective strategies during thoracic surgery. Effects of alveolar recruitment maneuver and low tidal volume ventilation on lung density distribution. Anesthesiology 2011;114:1025–35. Lung recruitment improved aeration and decreased tidal recruitment in an animal model of OLV.
Reis Miranda D, Gommers D, Struijs A, Dekker R, Mekel J, Feelders R, Lachmann B, Bogers JJC. Ventilation according to the open lung concept attenuates pulmonary inflammatory response in cardiac surgery. Eur J Cardiothorac Surg. 2005;28:889–95.
Sentkur M. New concepts of the management of one-lung ventilation. Curr Opin Anaesthsiol. 2006;19:1–4.
Tusman G, Böhm SH, Suarez-Sipmann F, et al. Lung recruitment improves the efficiency of ventilation and gas exchange during one-lung ventilation anesthesia. Anesth Analg. 2004;98:1604–9.
Cinella G, Grasso S, Natale C, Sollitto F, Cacciapaglia M, Angiolillo M, Pavone G, Mirabella L, Dambrosio M. Physiological effects of a lung-recruiting strategy applied during one-lung ventilation. Acta Anaesthesiol Scand. 2008;52:766–75.
Garutti I, Martinez G, Cruz P, Piñeiro P, Olmedilla L, de la Gala F. The impact of lung recruitment on hemodynamics during one-lung ventilation. J Cardiothorac Vasc Anesth. 2009;23:506–8.
Park SH, Jeon YT, Hwang JW, Do SH, Kim JH, Park HP. A preemptive alveolar recruitment strategy before one-lung ventilation improves arterial oxygenation in patients undergoing thoracic surgery: a prospective randomized study. Eur J Anaesthesiol. 2011;28:298–302.
•• Unzueta C, Tusman G, Suarez-Sipmann F, Bohm SH, Moral V. Alveolar recruitment improves ventilation during thoracic surgery: a randomized controlled trial. Br J Anaesth 2012;108:517–24. This randomized controlled study showed that lung recruitment improves arterial oxygenation and decreases dead space in patients undergoing OLV.
Bohm SH, Thamm OC, von Sandersleben A, Bangert K, Langwieler TE, Tusman G, Strate TG, Standl TG. Alveolar recruitment strategy and high positive-end expiratory pressure levels do not affect hemodynamics in morbidly obese intravascular volume-loaded patients. Anesth Analg. 2009;109:160–3.
Ferrando C, Mugarra A, Gutierrez A, Carbonell JA, Garcia M, Soro M, Tusman G, Belda FJ. Setting individualized PEEP level with a decremental PEEP trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesth Analg (in press).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tusman, G., Bohm, S.H. & Suarez-Sipmann, F. Alveolar Recruitment Maneuvers for One-Lung Ventilation During Thoracic Anesthesia. Curr Anesthesiol Rep 4, 160–169 (2014). https://doi.org/10.1007/s40140-014-0054-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-014-0054-9